Abstract
Background
This study examines the 20-year trend of suicide in 46 Muslim-majority countries throughout the world and compares their suicide rates and trends with the global average. Ecological-level associations between the proportion of the Muslim population, the age-standardized suicide rates, male-to-female suicide rate ratio, and the Human Development Index (HDI) in 2019 were examined.
Methods
Age-standardized suicide rates were extracted from the WHO Global Health Estimates database for the period between 2000 and 2019. The rates in each country were compared with the age-standardized global average during the past 20 years. The countries were further grouped according to their regions/sub-regions to calculate the regional and sub-regional weighted age-standardized suicide rates involving Muslim-majority countries. Correlation analyses were conducted between the proportion of Muslims, age-standardized suicide rate, male: female suicide rate ratio, and the HDI in all countries. Joinpoint regression was used to analyze the age-standardized suicide rates in 2000-2019.
Results
The 46 countries retained for analysis included an estimated 1.39 billion Muslims from a total worldwide Muslim population of 1.57 billion. Of these countries, eleven (23.9%) had an age-standardized suicide rate above the global average in 2019. In terms of regional/sub-regional suicide rates, Muslim-majority countries in the Sub-Saharan region recorded the highest weighted average age-standardized suicide rate of 10.02/100,000 population, and Southeastern Asia recorded the lowest rate (2.58/100,000 population). There were significant correlations between the Muslim population proportion and male-to-female rate ratios (r=-0.324, p=0.028), HDI index and age-standardized suicide rates (r=-0.506, p<0.001), and HDI index and male-to-female rate ratios (r=0.503, p<0.001) in 2019. Joinpoint analysis revealed that seven Muslim-majority countries (15.2%) recorded an increase in the average annual percentage change regarding age-standardized suicide rates during 2000-2019.
Conclusions
Most Muslim-majority countries had lower age-standardized suicide rates than the global average, which might reflect religious belief and practice or due to Muslim laws in their judicial and social structure which may lead to underreporting. This finding needs further in-depth country and region-specific study with regard to its implication for public policy.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-022-13101-3.
Keywords: Suicide rate, WHO Global Health Estimates, Islam, Joinpoint
Background
In 2019, the World Health Organization (WHO) estimated over 700,000 suicide deaths globally, equalling an average age-standardized suicide rate of 9.0 per 100,000 population [1]. There are more than 20 suicide attempts per suicide [2]. Furthermore, it is estimated that 135 people are exposed to a suicide death [3]. The shared goal of the United Nations Sustainable Development Goals (SDGs) and the WHO’s Comprehensive Mental Health Action Plan 2013-2030 is to reduce the global suicide mortality rate by one-third by 2030 [1, 4, 5].
The global average suicide rate has been declining steadily for the past 20 years from 14.0 per 100,000 in 2000 to 9.0 in 2019 [1]. This decrease is partly explained by a notable decline in suicides in populous countries such as China and India, specifically from 14.9 in 2000 to 6.7 in 2019 (decline of 55.0%), and from 19.1 in 2000 to 12.9 in 2019 (decline of 32.5%), respectively. Furthermore, there was also a reduction of suicides in Europe. For example, a high suicide rate in Russia dropped by 55.8% from 48.9 per 100,000 in 2000 to 21.6 in 2019. However, suicide rates in the Americas increased. Nevertheless, a majority of suicide deaths (77%) still occur in Lower- and Middle-Income Countries (LMICs), including the majority of Muslim countries [1, 6, 7].
Religion has been identified as one of the protective factors of suicidality [8]. Lawrence et al. [9] argued that the protective effect of religion against suicidality depends on different dimensions of religion and may differ by type of suicidality (e.g., suicidal ideation vs. suicide attempt). A meta-analysis by Wu et al. [10] found that religion was protective against death by suicide, with greater protectiveness found in areas of higher religious homogeneity, western cultures, and older population. Lester’s review of the literature suggested that intrinsic religiosity was protective against suicidal ideation and attempt [11]. Dadfar et al. found that religiosity may have a positive impact on the suicidal behavior of Iranian psychiatric outpatients [12]. Another study among Malaysian adolescents found that those who reported higher spiritual well-being had lower levels of suicidal ideation [13].
There have been many studies indicating that suicide rates in Muslim (or Muslim-majority) countries are lower than in non-Muslim-majority countries. Lester [14] reviewed research in Muslim countries and found that the suicide rate was consistently lower in countries where Islam was the predominant religion, which has been further confirmed [15–18]. A recent study showed that Muslims have the lowest permissiveness level toward suicide among the major religions of the world independent of religiosity level, and permissiveness was correlated with national suicide rates [19]. In Shah and Chandia’s [20] cross-national study, countries with a lower proportion of Muslims were found to exhibit higher suicide rates in both males and females, which suggests the protective effect of Islam against suicide. However, Alothman and Fogarty [21] found that the median male-to-female suicide rate ratio among Muslim predominant countries was 2.5 in 2015, which was the second-highest after Christian predominant countries, at 3.3. It is unclear, however, whether there is a correlation between the proportion of Muslims and the male-to-female suicide rate ratio. There are exceptions to the low suicide rates recorded in Muslim-majority countries. Countries belonging to the former Soviet Union in Central Asia, despite being predominantly Muslim, have recorded high suicide rates, attributed to adverse economic, health service-related, and other societal factors [22].
In summary, previous research highlights that there may be a variety of factors associated with the suicide rates and male-to-female suicide rate ratios in Muslim majority countries. Nevertheless, there is a lack of studies on suicides in Muslim-majority countries, particularly on an aggregated level.
In 2020, the WHO made the estimates of age-standardized suicide rates from 2000 to 2019 available for its member states under the Global Health Estimates [1]. The WHO Global Health Estimates of suicide rates utilized information from the Global Burden of Disease study, the WHO Mortality Database, and other data sources to provide the best possible estimates. Bias from potential misclassification of suicide deaths was minimized by considering the potential contribution of undetermined and accidental deaths [23]. This information allows comparisons between Muslim-majority countries and with global and regional averages across two decades. Furthermore, we can further examine ecological-level associations between the age-standardized suicide rates, male-to-female suicide rate ratio, and other environmental factors. Therefore, the present study aimed to: (1) analyze the 20-year suicide trend in 46 Muslim majority countries and compare the trends with the global average; (2) compare the 2019 country suicide rates with the global average and their respective regions/sub-regions; (3) examine the association between the age-standardized suicide rates and the male-to-female suicide rate ratio, the proportion of Muslim population in a country, and the Human Development Index (HDI) in 2019. Based on previous research, we hypothesized that Muslim majority countries will have lower age-standardized suicide rates in comparison with the global and regional suicide rates. Further, we expected the proportion of Muslims in a country would be negatively correlated with the suicide rate.
Methods
Data source
The age-standardized suicide rates were extracted from the WHO Global Health Estimates database [1]. Age-standardized suicide rates were available for the period between 2000 and 2019. Population data were extracted from the United Nations Population Division in order to provide information regarding the population size of each country [24]. Index of each country on the Human Development Index (HDI) in 2019 was obtained from the United Nations Development Programme (UNDP) [25]. The HDI reflects the socioeconomic development of a country beyond just Gross Domestic Income, including also dimensions such as life expectancy, education index, and standard of living [25].
Muslim majority countries were identified if at least 50% of the population identified as Muslim [26]. The proportion of the Muslim population in a country was derived from World Population Review data [27]. A total of 49 countries were classified as Muslim majority countries based on the criterion above. Countries that were not simultaneously listed as UN member states and WHO member states were omitted. This resulted in the omission of three Muslim majority countries – Palestine, Western Sahara, and Mayotte (French protectorate).
The remaining 46 Muslim-majority countries were further grouped according to the United Nations geoscheme, a system dividing 249 countries and territories of the world into six regional and 22 sub-regional groups [28] (Table 1).
Table 1.
List of 46 Muslim-majority countries, age-standardized suicide rate per 100,000 population, male-to-female suicide rate ratio, and Human Development Index ranking in 2019
| Country | Estimated Muslim Population n (%)a |
Suicide rate (both sexes) c | Male to female suicide rate ratioc | Human Development Index (HDI)d | Regional age-standardized suicide rate (Muslim-majority countries only) | Regional age-standardized suicide rate (Other countries) | Regional age-standardized suicide rate (All countries) |
|---|---|---|---|---|---|---|---|
| Total | 1392957160 | - | - | - | |||
| Central Asiab | 7.96 | - | 7.96 | ||||
| Uzbekistan | 31827355 (96.5) | 8.28 | 2.41 | 0.720 | |||
| Kazakhstan | 13023102 (70.2) | 18.05 | 4.48 | 0.825 | |||
| Tajikistan | 9013429 (96.7) | 5.32 | 2.15 | 0.668 | |||
| Turkmenistan | 5543974 (93.3) | 6.07 | 3.24 | 0.715 | |||
| Kyrgyzstan | 5132681 (80.0) | 8.28 | 3.86 | 0.697 | |||
| South Asiab | 2.82 | 5.46 | 3.93 | ||||
| Pakistan | 208985531 (96.5) | 9.77 | 3.11 | 0.557 | |||
| Bangladesh | 147393740 (90.4) | 3.85 | 3.53 | 0.632 | |||
| Afghanistan | 37889590 (99.6) | 5.96 | 1.09 | 0.511 | |||
| Maldives | 522462 (98.4) | 2.76 | 4.56 | 0.740 | |||
| Southeastern Asiab | 2.58 | 7.29 | 3.31 | ||||
| Indonesia | 235985494 (87.2) | 2.55 | 3.33 | 0.718 | |||
| Malaysia | 19585221 (61.3) | 5.77 | 3.75 | 0.810 | |||
| Brunei | 341437 (78.8) | 2.54 | 5.25 | 0.838 | |||
| Western Asiab | 4.87 | 3.94 | 4.47 | ||||
| Iran | 82416410 (99.4) | 5.13 | 2.78 | 0.783 | |||
| Turkey | 82762170 (99.2) | 2.34 | 3.00 | 0.820 | |||
| Iraq | 37619468 (95.7) | 4.74 | 3.04 | 0.674 | |||
| Saudi Arabia | 33274742 (97.1) | 5.43 | 4.11 | 0.854 | |||
| Yemen | 28899465 (99.1) | 7.06 | 1.70 | 0.470 | |||
| Syria | 15875223 (93.0) | 2.11 | 4.38 | 0.567 | |||
| Jordan | 9818849 (97.2) | 1.98 | 3.33 | 0.729 | |||
| Azerbaijan | 9736240 (96.9) | 3.97 | 4.40 | 0.756 | |||
| UAE | 7425600 (76.0) | 5.24 | 2.42 | 0.890 | |||
| Lebanon | 3955744 (57.7) | 2.76 | 2.29 | 0.744 | |||
| Oman | 4273518 (85.9) | 4.47 | 5.82 | 0.813 | |||
| Kuwait | 3138479 (74.6) | 2.66 | 5.43 | 0.806 | |||
| Qatar | 2194855 (77.5) | 4.66 | 3.35 | 0.848 | |||
| Bahrain | 1209538 (73.7) | 7.20 | 4.30 | 0.852 | |||
| North Africab | 4.23 | - | 4.23 | ||||
| Egypt | 92758582 (92.4) | 3.41 | 2.09 | 0.707 | |||
| Algeria | 42622523 (99.0) | 2.60 | 1.74 | 0.748 | |||
| Sudan | 41528840 (97.0) | 4.76 | 1.91 | 0.510 | |||
| Morocco | 36107048 (99.0) | 7.29 | 2.15 | 0.686 | |||
| Tunisia | 11671332 (99.8) | 3.18 | 2.56 | 0.740 | |||
| Libya | 6574129 (97.0) | 4.49 | 2.10 | 0.724 | |||
| Sub-Saharan Africab | 10.02 | 10.79 | 10.68 | ||||
| Niger | 22914437 (98.3) | 10.15 | 2.20 | 0.394 | |||
| Mali | 18675122 (95.0) | 7.96 | 1.84 | 0.434 | |||
| Senegal | 15660804 (96.1) | 10.99 | 3.56 | 0.512 | |||
| Burkina Faso | 12497651 (61.5) | 14.38 | 3.77 | 0.452 | |||
| Somalia | 15412020 (99.8) | 14.66 | 3.21 | - | |||
| Guinea | 11379180 (89.1) | 12.33 | 2.30 | 0.477 | |||
| Chad | 9249192 (58.0) | 13.22 | 2.93 | 0.398 | |||
| Sierra Leone | 6141181 (78.6) | 11.25 | 1.80 | 0.452 | |||
| Mauritania | 4525698 (100.0) | 5.47 | 1.90 | 0.546 | |||
| Gambia | 2246745 (95.7) | 9.64 | 2.15 | 0.496 | |||
| Djibouti | 944350 (97.0) | 11.95 | 2.14 | 0.524 | |||
| Comoros | 836426 (98.3) | 8.46 | 1.95 | 0.554 | |||
| Southern Europeb | 5.83 | 10.02 | 9.53 | ||||
| Bosnia & Herzegovina | 1673606 (50.7) | 8.25 | 3.97 | 0.780 | |||
| Albania | 1693977 (58.8) | 3.72 | 2.41 | 0.795 |
Note. aWorld Population Review. bUnited Nations, SDG Indicators: Regional groupings used in report and Statistical Annex. cWHO Global Health Observatory data. dUnited Nations Development Programme
Statistical analysis
In order to calculate regional average age-standardized suicide rates, the country-specific weight was calculated by using the country-specific population divided by the total population size for the region. Next, for each region, the weighted average age-standardized suicide rate was calculated as the sum of all suicide rates multiplied by their weights [29].
As the data were normally distributed (based on skewness and kurtosis values of < ±2 and < ±7 respectively [30]), Pearson’s correlation coefficients were calculated between the proportion of Muslims in a country, the suicide rate, male-to-female suicide rate ratio, and HDI in 2019.
Trend analyses of country suicide rates were conducted using Joinpoint regression, using Joinpoint version 4.8.0. Joinpoint regression was used to identify the occurrence of statistically significant changes in the trend, i.e. age-standardized suicide rate, where the slope of the linear function changes [31]. Joinpoint regression provides an estimate of the annual percentage change (APC) and the average annual percentage change (AAPC) to assess the annual change in the age-standardized suicide rates in the 46 Muslim-majority countries from 2000 to 2019, with 95% confidence intervals (95%CIs). A p-value of less than 0.05 was used to determine statistical significance for all two-tailed tests.
This study did not require approval by an ethics committee as published population-based data were used.
Results
The 46 countries included for analysis have an estimated 1.39 billion Muslims from a total population of about 1.57 billion. The average proportion of Muslims making up the 46 countries was 89.4%, with a range of 50.7% to 100.0%. Seven UN regions/subregions were represented, with the greatest number of countries from Western Asia (14 countries) and least from Southern Europe (two countries) (Table 1).
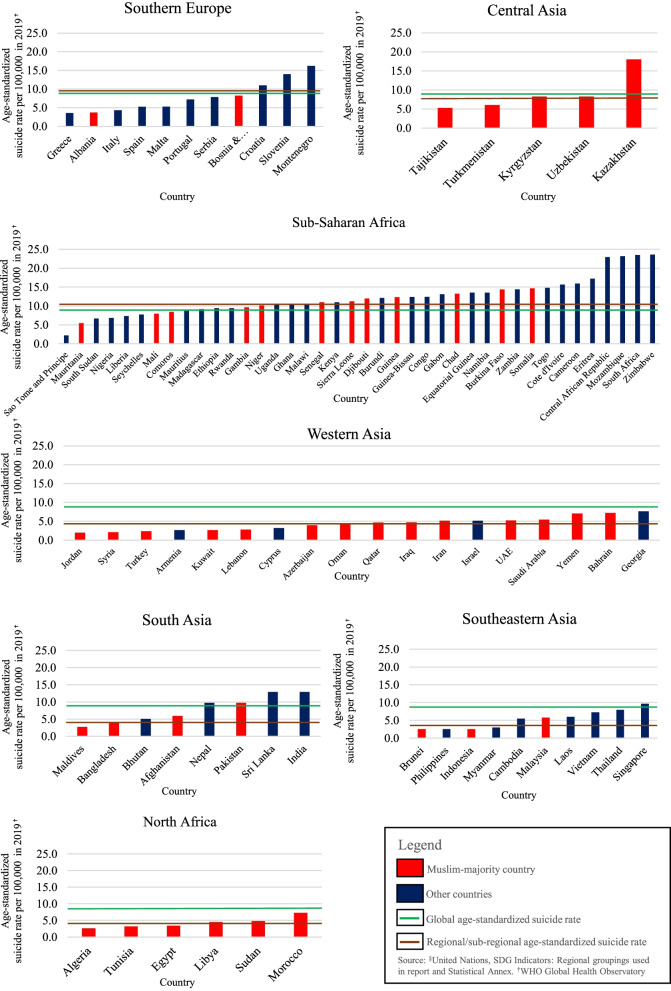
Regarding the suicide rates of the Muslim-majority countries by region/sub-region, the Muslim-majority countries in the Sub-Saharan region recorded the highest weighted average age-standardized suicide rate of 10.02 per 100,000 population, followed by Central Asia (7.96), Southern Europe (5.83), Western Asia (4.87), North Africa (4.23), South Asia (2.82), and Southeastern Asia (2.58). In comparison with the global average, only Sub-Saharan Africa had an average rate that was higher than the global average. In terms of regional average, only Western Asia had an average rate that was higher than the regional average. In comparison with other (non-Muslim) countries in the region, only Western Asia recorded a higher average rate (Fig 1).
Fig. 1.
Age-standardized suicide rates of Muslim-majority and other countries based on region/sub-region in 2019. Source: WHO Global Health Observatory
The relationship between the proportion of Muslims, age-standardized suicide rate, male-to-female suicide rate ratio, and HDI in 2019
The results of the Pearson’s correlation showed that there was no relationship between the proportion of the Muslim population and the age-standardized suicide rate in Muslim-majority countries (r=-0.178 p=0.237). However, there was a significant correlation between the Muslim population proportion and male-to-female suicide rate ratio (r=-0.324, p=0.028). HDI index was significantly correlated with both, and age-standardized suicide rates (r=-0.506, p<0.001) and male-to-female suicide rate ratio (r=0.503, p<0.001).
Suicide trends of Muslim-majority countries during the past 20 years
Globally, age-standardized suicide rates declined from 14.0 per 100,000 in year 2000 to 9.0 in year 2019, a decrease of 35.7%. Based on the Joinpoint analysis, the global trend had two Joinpoints in 2011 and 2015, where the trend showed a decline (AAPC: -2.3; 95%CI:-2.6, -2.0), with the decline becoming slower after 2015. Among the Muslim-majority countries analyzed, seven countries (Azerbaijan, Brunei, Guinea, Niger, Saudi Arabia, Sierra Leone, and Somalia; 15.2%) recorded a significant increase in AAPC.
Muslim-majority countries in the Central Asia Sub-Region (6 countries)
Most of the Muslim-majority countries in Central Asia had a significant decrease in AAPC, except for Tajikistan which had a slight non-significant increase in AAPC of 0.3 (95%CI -0.1, 0.7). The largest decrease was recorded by Turkmenistan, with AAPC of –4.5 (95%CI -5.2, -3.9), and an overall decrease of 56.2%. Kazakhstan had one of the world’s highest suicide rates, and even though it recorded a decrease (AAPC: -3.8; 95%CI:-4.3 to -3.3), the rate of 18.1 in 2019 was still the highest among all the 46 Muslim-majority countries included for analysis.
Muslim-majority countries in the South Asia Sub-Region (3 countries)
All Muslim-majority countries in the South Asia Sub-Region recorded a negative AAPC, and the suicide rates were below the global average over the past 20 years. Maldives had the greatest decline in suicide rate (47.9%) during the past 20 years (AAPC -3.4; 95% CI: -4.5, -2.4). Bangladesh had been recording a significant overall decrease in its suicide rate during the past 20 years (AAPC-3.0; 95%CI: -3.5, -2.6). However, an upward trend was detected from 2014 to 2019 (APC 1.6; 95%CI 0.7, 2.4).
Muslim-majority countries in the Southeastern Asia Sub-Region (3 countries)
Muslim-majority countries in Southeastern Asia recorded the lowest suicide rates in comparison with the other six regions/sub-regions and all countries had rates below the world average. While Indonesia recorded a decline (AAPC -2.0; 95%CI: -2.2, -1.8), Brunei recorded an overall upward trend (AAPC 2.6; 95%CI:0.7, 4.5) from 2000 to 2019.
Muslim-majority countries in the Western Asia Sub-Region (14 countries)
The suicide rate decreased significantly for all Muslim-majority countries in Western Asia, except for Azerbaijan (AAPC: 0.8; 95%CI:0.3 to 1.2) and Saudi Arabia (AAPC: 1.9; 95%CI:1.5 to 2.2). Saudi Arabia recorded the greatest increase in the past 20 years (41.4%) among all Western Asian Muslim-majority countries. All countries, however, trended below the global average rate during the past 20 years. Turkey recorded the largest decrease in suicide rate in the region (-44.4%). Kuwait and Syria recorded an upward trend for the years 2011-2019 and 2006-2019 respectively, even though Kuwait recorded an overall decrease of -14.2% during the past 20 years, whilst Syria recorded an overall increase of 5.0% during the same time period.
Muslim-majority countries in the North Africa Sub-Region (6 countries)
All the Muslim-majority countries in the North Africa sub-region trended below the global average. Morocco had the highest suicide rates in this region during the 20 years of observation. Most countries recorded a decline in the AAPC, except for Libya, which recorded a non-significant AAPC of 0.1 (95%CI:-0.6, 0.9).
Muslim-majority countries in the Sub-Saharan Africa Sub-Region (12 countries)
In 2019, the majority of Sub-Saharan African Muslim-majority countries recorded suicide rates above the global average, except Comoros (8.5), Mali (8.0), and Mauritania (5.5). Guinea and Niger both recorded an overall increase in AAPC (1.3; 95%CI: 1.0, 1.6 and 0.2; 95%CI: 0.0, 0.4 respectively), with an upward trend between 2000 to 2013, and a downward trend between 2013 to 2019. Similarly, Sierra Leone had an overall increase in suicide rates (AAPC 0.5; 95%CI: 0.0, 1.0), with multiple fluctuations.
Muslim-majority countries in the Southern Europe Sub-Region (2 countries)
Albania showed a long-term decrease in the suicide rate from 5.2 in 2000 to 3.7 in 2019; a decrease of -28.9%. Bosnia and Herzegovina had a stable trend showing a small growth from 8.1 in 2000 to 8.3 in 2019, an increase of 1.5%. It fluctuated between 8.1 and 9.0 during this period, having two Joinpoints and showed an increasing trend in initial years until 2007 after which it declined for a few years before flattening from 2010 onward (AAPC: 0.0; 95%CI:-0.8 to 0.8) (Table 2; Fig S1 in Supplementary Material).
Table 2.
Joinpoint analysis of the suicide trend of the global average and Muslim-majority countries from 2000 to 2019
| Global Average | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2011 | -2.2* | -2.4 | -2.1 | -29.0 | < 0.001 |
| 2 | 2011 | 2015 | -3.6* | -4.8 | -2.4 | -6.4 | < 0.001 |
| 3 | 2015 | 2019 | -0.9* | -1.7 | -0.1 | -2.6 | 0.024 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.3* | -2.6 | -2.0 | -15.1 | < 0.05 |
|
Central Asia Kazakhstan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2005 | 0.0 | -1.8 | 1.9 | 0.0 | 0.990 |
| 2 | 2005 | 2019 | -5.2* | -5.5 | -4.8 | -29.4 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.8* | -4.3 | -3.3 | -14.9 | < 0.05 |
| Kyrgyzstan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2014 | -2.9* | -3.2 | -2.6 | -18.7 | < 0.001 |
| 2 | 2014 | 2019 | -5.9* | -7.4 | -4.3 | -8.0 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.7* | -4.1 | -3.3 | -16.4 | < 0.05 |
| Tajikistan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2002 | -5.2* | -9.0 | -1.2 | -2.7 | 0.015 |
| 2 | 2002 | 2019 | 1.0* | 0.8 | 1.1 | 14.4 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.3 | -0.1 | 0.7 | 1.5 | >0.05 |
| Turkmenistan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2006 | 1.4* | 0.2 | 2.6 | 2.6 | 0.024 |
| 2 | 2006 | 2011 | -13.4* | -15.3 | -11.5 | -14.2 | < 0.001 |
| 3 | 2011 | 2019 | -3.0* | -3.7 | -2.2 | -8.6 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -4.5* | -5.2 | -3.9 | -13.2 | < 0.05 |
| Uzbekistan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2009 | -4.0* | -4.6 | -3.4 | -14.0 | < 0.001 |
| 2 | 2009 | 2016 | 1.4* | 0.3 | 2.6 | 2.7 | 0.020 |
| 3 | 2016 | 2019 | -3.6* | -6.8 | -0.2 | -2.3 | 0.042 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.9* | -2.6 | -1.3 | -5.6 | < 0.05 |
|
South Asia Pakistan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | 0.8 | -0.2 | 1.7 | 1.8 | 0.101 |
| 2 | 2003 | 2011 | -1.5* | -1.8 | -1.3 | -13.2 | < 0.001 |
| 3 | 2011 | 2019 | -0.2* | -0.4 | -0.0 | -2.4 | 0.034 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.6* | -0.8 | -0.4 | -6.6 | < 0.05 |
| Bangladesh | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | -5.9* | -7.6 | -4.1 | -7.2 | < 0.001 |
| 2 | 2003 | 2008 | -1.3* | -2.5 | -0.1 | -2.5 | 0.035 |
| 3 | 2008 | 2014 | -6.7* | -7.5 | -5.9 | -18.5 | < 0.001 |
| 4 | 2014 | 2019 | 1.6* | 0.7 | 2.4 | 4.2 | 0.002 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.0* | -3.5 | -2.6 | -12.5 | < 0.05 |
| Afghanistan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2006 | -0.4 | -1.1 | 0.3 | -1.3 | 0.223 |
| 2 | 2006 | 2012 | -3.5* | -4.4 | -2.7 | -8.8 | < 0.001 |
| 3 | 2012 | 2019 | -0.6* | -1.1 | -0.1 | -2.5 | 0.027 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.5* | -1.8 | -1.1 | -8.1 | < 0.05 |
| Maldives | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2004 | -7.1* | -9.0 | -5.2 | -8.1 | < 0.001 |
| 2 | 2004 | 2013 | -4.1* | -4.8 | -3.4 | -13.4 | < 0.001 |
| 3 | 2013 | 2016 | 4.9 | -1.7 | 12.0 | 1.7 | 0.130 |
| 4 | 2016 | 2019 | -4.3* | -7.4 | -1.1 | -3.0 | 0.014 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.4* | -4.5 | -2.4 | -6.2 | < 0.05 |
|
Southeastern Asia Indonesia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2014 | -2.7* | -2.8 | -2.5 | -36.4 | < 0.001 |
| 2 | 2014 | 2019 | -0.3 | -1.0 | 0.5 | -0.8 | 0.439 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.0* | -2.2 | -1.8 | -19.1 | < 0.05 |
| Malaysia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2013 | -1.4* | -1.7 | -1.1 | -11.3 | < 0.001 |
| 2 | 2013 | 2019 | 2.3* | 1.5 | 3.2 | 5.7 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.2 | -0.5 | 0.1 | -1.5 | >0.05 |
| Brunei | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2019 | 2.6* | 0.7 | 4.5 | 2.9 | 0.010 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 2.6* | 0.7 | 4.5 | 2.9 | < 0.05 |
|
Western Asia Iran | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2006 | -5.6* | -6.7 | -4.5 | -10.8 | < 0.001 |
| 2 | 2006 | 2015 | 0.8* | 0.1 | 1.6 | 2.4 | 0.036 |
| 3 | 2015 | 2019 | -4.1* | -6.2 | -2.0 | -4.2 | 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.3* | -2.9 | -1.7 | -7.4 | < 0.05 |
| Turkey | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2007 | -6.2* | -7.1 | -5.2 | -14.0 | < 0.001 |
| 2 | 2007 | 2012 | -2.8* | -5.0 | -0.4 | -2.6 | 0.024 |
| 3 | 2012 | 2019 | 0.3 | -0.7 | 1.3 | 0.6 | 0.586 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.0* | -3.7 | -2.2 | -8.1 | < 0.05 |
| Iraq | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2008 | -0.7* | -1.2 | -0.3 | -3.7 | 0.003 |
| 2 | 2008 | 2013 | 2.9* | 1.6 | 4.2 | 4.9 | < 0.001 |
| 3 | 2013 | 2019 | -3.1* | -3.7 | -2.4 | -10.0 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.6* | -0.9 | -0.2 | -2.7 | < 0.05 |
| Saudi Arabia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2005 | 1.0* | 0.1 | 1.9 | 2.5 | 0.026 |
| 2 | 2005 | 2012 | 7.1* | 6.4 | 7.8 | 23.3 | < 0.001 |
| 3 | 2012 | 2019 | -2.5* | -3.0 | -2.0 | -11.0 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 1.9* | 1.5 | 2.2 | 10.7 | < 0.05 |
| Yemen | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2015 | -1.4* | -1.5 | -1.3 | -23.7 | < 0.001 |
| 2 | 2015 | 2019 | 0.8 | -0.2 | 1.7 | 1.7 | 0.113 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.0* | -1.2 | -0.8 | -9.1 | < 0.05 |
| Syria | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2006 | -1.8 | -3.8 | 0.2 | -1.9 | 0.072 |
| 2 | 2006 | 2019 | 1.3* | 0.7 | 1.9 | 4.4 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.3 | -0.4 | 1.0 | 0.9 | >0.05 |
| Jordan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2004 | -3.8* | -5.2 | -2.4 | -6.1 | < 0.001 |
| 2 | 2004 | 2009 | -7.2* | -8.5 | -5.8 | -11.8 | < 0.001 |
| 3 | 2009 | 2015 | -1.6* | -2.6 | -0.6 | -3.7 | 0.005 |
| 4 | 2015 | 2019 | 1.2 | -0.3 | 2.6 | 1.9 | 0.096 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.0* | -3.5 | -2.4 | -10.5 | < 0.05 |
| Azerbaijan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2006 | 6.5* | 5.7 | 7.4 | 18.1 | < 0.001 |
| 2 | 2006 | 2016 | -2.5* | -2.9 | -2.1 | -13.3 | < 0.001 |
| 3 | 2016 | 2019 | 0.7 | -1.6 | 3.0 | 0.6 | 0.536 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.8* | 0.3 | 1.2 | 3.5 | < 0.05 |
| United Arab Emirates | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | -5.1* | -7.3 | -2.9 | -5.1 | 0.001 |
| 2 | 2003 | 2011 | -1.0* | -1.6 | -0.4 | -3.6 | 0.005 |
| 3 | 2011 | 2017 | -4.7* | -5.7 | -3.7 | -10.6 | < 0.001 |
| 4 | 2017 | 2019 | 4.0 | -0.7 | 9.0 | 1.9 | 0.085 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.3* | -3.0 | -1.7 | -7.2 | < 0.05 |
| Lebanon | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2019 | -0.2 | -0.6 | 0.1 | -1.3 | 0.199 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.2 | -0.6 | 0.1 | -1.3 | >0.05 |
| Oman | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2010 | -0.8* | -1.5 | -0.2 | -2.8 | 0.016 |
| 2 | 2010 | 2013 | -8.2* | -15.6 | -0.0 | -2.2 | 0.049 |
| 3 | 2013 | 2019 | -1.0 | -2.4 | 0.5 | -1.5 | 0.168 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.1* | -3.3 | -0.8 | -3.1 | < 0.05 |
| Kuwait | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2005 | -2.4* | -4.6 | -0.2 | -2.5 | 0.036 |
| 2 | 2005 | 2008 | 2.7 | -7.1 | 13.5 | 0.6 | 0.561 |
| 3 | 2008 | 2011 | -7.9 | -16.7 | 1.8 | -1.9 | 0.096 |
| 4 | 2011 | 2019 | 2.3* | 1.2 | 3.4 | 4.7 | 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.6 | -2.6 | 1.5 | -0.5 | 1 |
| Qatar | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2005 | -4.4* | -5.8 | -2.9 | -6.5 | < 0.001 |
| 2 | 2005 | 2008 | 4.1 | -2.9 | 11.5 | 1.3 | 0.222 |
| 3 | 2008 | 2015 | -5.3* | -6.4 | -4.2 | -10.6 | < 0.001 |
| 4 | 2015 | 2019 | -1.2 | -3.3 | 1.0 | -1.3 | 0.241 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.8* | -3.9 | -1.6 | -4.8 | < 0.05 |
| Bahrain | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | 11.5* | 3.5 | 20.2 | 3.2 | 0.008 |
| 2 | 2003 | 2013 | -4.9* | -6.2 | -3.6 | -8.0 | < 0.001 |
| 3 | 2013 | 2019 | 2.3 | -0.2 | 4.9 | 2.0 | 0.071 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.2 | -1.6 | 1.2 | -0.3 | 1 |
|
North Africa Egypt | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2008 | -0.7* | -1.4 | -0.1 | -2.5 | 0.027 |
| 2 | 2008 | 2013 | 1.6 | -0.3 | 3.5 | 1.8 | 0.090 |
| 3 | 2013 | 2019 | -2.2* | -3.1 | -1.2 | -4.8 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.6* | -1.1 | -0.0 | -2.0 | < 0.05 |
| Algeria | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2011 | -4.4* | -4.6 | -4.1 | -39.9 | < 0.001 |
| 2 | 2011 | 2014 | -1.0 | -4.7 | 2.8 | -0.6 | 0.552 |
| 3 | 2014 | 2017 | -3.9* | -7.4 | -0.2 | -2.4 | 0.041 |
| 4 | 2017 | 2019 | 2.2 | -1.6 | 6.1 | 1.3 | 0.225 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -3.1* | -3.9 | -2.3 | -7.6 | < 0.05 |
| Sudan | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2008 | -0.8* | -1.2 | -0.4 | -5.0 | 0.001 |
| 2 | 2008 | 2011 | 0.4 | -3.0 | 3.9 | 0.3 | 0.795 |
| 3 | 2011 | 2016 | -1.7* | -2.8 | -0.7 | -3.6 | 0.005 |
| 4 | 2016 | 2019 | -0.1 | -1.8 | 1.7 | -0.1 | 0.913 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.8* | -1.4 | -0.2 | -2.5 | < 0.05 |
| Morocco | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2011 | -1.2* | -1.4 | -0.9 | -10.2 | < 0.001 |
| 2 | 2011 | 2015 | -5.6* | -7.4 | -3.9 | -6.7 | < 0.001 |
| 3 | 2015 | 2019 | -0.8 | -2.0 | 0.4 | -1.4 | 0.174 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -2.1* | -2.5 | -1.6 | -9.2 | < 0.05 |
| Tunisia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | -0.1 | -1.3 | 1.2 | -0.1 | 0.929 |
| 2 | 2003 | 2016 | -2.1* | -2.2 | -1.9 | -30.3 | < 0.001 |
| 3 | 2016 | 2019 | 2.3* | 1.0 | 3.6 | 4.0 | 0.002 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.1* | -1.3 | -0.8 | -7.7 | < 0.05 |
| Libya | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2019 | 0.1 | -0.6 | 0.9 | 0.4 | 0.670 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.1 | -0.6 | 0.9 | 0.4 | 1 |
|
Sub-Saharan Africa Niger | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2013 | 0.8* | 0.6 | 1.0 | 8.9 | < 0.001 |
| 2 | 2013 | 2019 | -0.9* | -1.5 | -0.3 | -3.3 | 0.005 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.2* | 0.0 | 0.4 | 2.2 | < 0.05 |
| Mali | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2013 | 0.1 | -0.1 | 0.3 | 0.8 | 0.453 |
| 2 | 2013 | 2019 | -1.8* | -2.4 | -1.2 | -6.3 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.5* | -0.7 | -0.3 | -4.8 | < 0.05 |
| Senegal | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2019 | -1.3* | -1.4 | -1.2 | -27.2 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.3* | -1.4 | -1.2 | -27.2 | < 0.05 |
| Burkina Faso | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2002 | -3.0* | -4.4 | -1.7 | -5.0 | 0.001 |
| 2 | 2002 | 2010 | -0.1 | -0.3 | 0.1 | -1.4 | 0.195 |
| 3 | 2010 | 2013 | 0.6 | -0.8 | 2.1 | 1.0 | 0.330 |
| 4 | 2013 | 2019 | -1.8* | -2.0 | -1.6 | -17.3 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-P-Value~ |
| Full Range | 2000 | 2019 | -0.8* | -1.1 | -0.6 | -6.6 | < 0.05 |
| Somalia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2010 | 1.8* | 1.4 | 2.2 | 10.4 | < 0.001 |
| 2 | 2010 | 2015 | -2.8* | -4.2 | -1.3 | -4.1 | 0.002 |
| 3 | 2015 | 2019 | 1.5* | 0.0 | 3.1 | 2.2 | 0.047 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.5* | 0.0 | 1.0 | 2.1 | < 0.05 |
| Guinea | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2013 | 2.6* | 2.3 | 2.9 | 21.3 | < 0.001 |
| 2 | 2013 | 2019 | -1.4* | -2.3 | -0.6 | -3.8 | 0.002 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 1.3* | 1.0 | 1.6 | 8.8 | < 0.05 |
| Chad | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2012 | 0.0 | -0.2 | 0.2 | 0.1 | 0.937 |
| 2 | 2012 | 2015 | -3.9* | -6.7 | -1.0 | -2.9 | 0.013 |
| 3 | 2015 | 2019 | -1.2* | -2.2 | -0.3 | -2.9 | 0.014 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.9* | -1.3 | -0.4 | -3.7 | < 0.05 |
| Sierra Leone | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2010 | 1.8* | 1.4 | 2.2 | 10.4 | < 0.001 |
| 2 | 2010 | 2015 | -2.8* | -4.2 | -1.3 | -4.1 | 0.002 |
| 3 | 2015 | 2019 | 1.5* | 0.0 | 3.1 | 2.2 | 0.047 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.5* | 0.0 | 1.0 | 2.1 | < 0.05 |
| Mauritania | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2011 | -1.4* | -1.7 | -1.2 | -10.8 | < 0.001 |
| 2 | 2011 | 2019 | 0.1 | -0.3 | 0.6 | 0.6 | 0.548 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.8* | -1.0 | -0.5 | -6.5 | < 0.05 |
| Gambia | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2003 | 1.4 | -0.7 | 3.5 | 1.5 | 0.169 |
| 2 | 2003 | 2013 | -0.8* | -1.2 | -0.5 | -4.9 | < 0.001 |
| 3 | 2013 | 2019 | -1.9* | -2.6 | -1.3 | -6.2 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -0.8* | -1.2 | -0.5 | -4.2 | < 0.05 |
| Djibouti | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2004 | 0.4 | -0.9 | 1.7 | 0.7 | 0.512 |
| 2 | 2004 | 2008 | -1.5 | -3.6 | 0.5 | -1.7 | 0.124 |
| 3 | 2008 | 2013 | 1.2 | -0.1 | 2.6 | 2.1 | 0.063 |
| 4 | 2013 | 2019 | 0.0 | -0.6 | 0.7 | 0.2 | 0.879 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.1 | -0.5 | 0.7 | 0.3 | 1 |
| Comoros | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2005 | -3.9* | -5.1 | -2.7 | -6.9 | < 0.001 |
| 2 | 2005 | 2019 | -0.4* | -0.7 | -0.2 | -3.4 | 0.004 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.3* | -1.7 | -1.0 | -7.7 | < 0.05 |
|
Southern Europe Bosnia and Herzegovina | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2007 | 1.6* | 0.9 | 2.3 | 5.2 | < 0.001 |
| 2 | 2007 | 2010 | -3.3 | -8.1 | 1.7 | -1.4 | 0.174 |
| 3 | 2010 | 2019 | -0.1 | -0.5 | 0.4 | -0.4 | 0.711 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | 0.0 | -0.8 | 0.8 | 0.1 | 1 |
| Albania | |||||||
| Segment | Lower Endpoint | Upper Endpoint | APC | Lower CI | Upper CI | Test Statistic (t) | Prob > |t| |
| 1 | 2000 | 2008 | 8.1* | 3.4 | 12.9 | 3.7 | 0.002 |
| 2 | 2008 | 2019 | -7.9* | -10.4 | -5.3 | -6.4 | < 0.001 |
| Range | Lower Endpoint | Upper Endpoint | AAPC | Lower CI | Upper CI | Test Statistic~ | P-Value~ |
| Full Range | 2000 | 2019 | -1.5 | -3.7 | 0.8 | -1.3 | >0.05 |
Note. APC Average Percent of Change. AAPC Annual Average Percentage of Change. CI Confidence Intervals. UAE United Arab Emirates. *significant at p < 0.05
Discussion
The release of the new WHO estimates provided an opportunity to examine suicide rates across the globe including countries with relatively limited information. Therefore, the aim of this paper was to analyze the age-standardized suicide rates in 46 Muslim-majority countries from 2000 to 2019, and to compare the suicide trends with the global average. In addition, we compared the 2019 suicide rates with the global average and their respective regions/sub-regions; and examined the association between the age-standardized suicide rates and the male-to-female suicide rate ratio, with the proportion of Muslim population in a country, and the Human Development Index (HDI) in 2019. Our study found that the majority of the Muslim-majority countries (76.1%) had their average suicide rates below the global average in 2019. Despite some fluctuations, most of the countries (63.0%) showed an overall decline during the past 20 years (2000-2019).
Suicide rates in Muslim-majority countries across regions and sub-regions
Of the 46 Muslim-majority countries analyzed, 11 (23.9%) had an age-standardized suicide rate above the global average in 2019. Of the 11 countries, nine are located in Sub-Saharan Africa, including Burkina Faso, Chad, Comoros, Djibouti, Gambia, Guinea, Mali, Mauritania, Niger, Senegal, Sierra Leone, and Somalia. The other two are in South Asia and Central Asia, i.e., Pakistan and Kazakhstan. These 11 countries are estimated to have about 318.5 million Muslims out of the total Muslim population of about 1,393.0 million (22.9%). The remaining 35 Muslim-majority countries have age-standardized suicide rates below the global average, and they consist of about 1,074.5 million Muslim populations comprising 77.1% of total Muslim populations located in the Muslim majority countries included in the analysis.
Traditionally, Kazakhstan has had high suicide rates and showed a twice higher rate compared to the global average in 2019. A recent study found that unemployment was the factor most strongly correlated with suicide rates in Kazakhstan between 2000 and 2019 [32]. The suicide rate estimated in Pakistan was also slightly above the global average. A scoping review on suicidal behavior and self-harm in Pakistan found that individuals below 30 years old and males to be at higher risk of suicide in Pakistan [33]. There is a lack of suicide research from Africa to explain the high suicide rates of nine Muslim majority countries in Africa, however, the WHO estimates show that the African region has the highest average suicide rate in 2019 [34].
Based on the country-level comparisons, the age-standardized suicide rates of most Muslim-majority countries were consistently lower than the global average during the past 20 years. This could be partly explained by the role of their religion and may also be due to some countries integrating Islamic principles into their governance and social systems. Suicide is prohibited under Islamic law, based on evidence from the Qur’an, the Sunnah, and the consensus of Muslim scholars. The person who dies by suicide is liable to be eternally condemned and experience God’s wrath. According to the Qur’an, in the 4th surah, verse 29, “You shall not kill yourselves. Surely Allah is ever compassionate to you.” Apart from condemning suicide, the Qur’an emphasizes the sanctity of life, providing instructive guidance on the value of life and fulfilling the role as a human in this world whilst maintaining steadfastness, patience, and stability in all aspects of life (Qur’an, 17:33) [35]. In addition, adherence to the normative structures of collectivism such as cohesive communities, familial support, and collective goals together with religious commitment is important, and these may be protective against suicide [20]. Based on the above, the low suicide rates in most of the Muslim-majority countries may be related to the understanding of the Islamic concept of life within the matrix of Islamic thought such as legal thought, the Qur’an, and Prophetic Traditions. The findings are consistent with other studies reporting the protective effects of Islam in terms of reducing country- or region-wide suicide rates in Muslim countries [14–18].
On the other hand, suicide is also a major stigma in Muslim countries, which may lead to a reluctance to report a suicide death, and this may lead to the lower suicide rates in these countries [6, 36, 37]. The low rates of suicide in Muslim-majority countries which can be seen as a result of Islamic thought condemning taking one’s own life is not necessarily indicative of lower levels of suicidal ideation [38]. The suicidal ideation can manifest itself as non-fatal suicidal behavior or might be repressed by one’s religious belief. This is supported by higher attempted suicide rates in Ankara, Turkey [39], a high percentage of Turkish students considering suicide [40], and higher scores obtained in the suicide probability scale by Turkish university students compared to their American counterparts [38].
There were considerable cross-regional differences in the average age-standardized suicide rates in the seven regions and sub-regions of Central Asia, South Asia, Southeastern Asia, Western Asia, North Africa, Sub-Saharan Africa, and Southern Europe examined here. As a region, Sub-Saharan Africa recorded the highest average suicide rate among all the regions examined. According to Lester et al., gender inequalities may play a role in higher suicide rates in Africa and family power dynamics and domestic violence may contribute to this [41]. A narrative synthesis by Vijayakumar et al. further suggested that the suicide rate among African refugees was higher [42]. As Africa is home to the largest number of refugees, suicide among refugees might be an important factor behind the increasing overall rate of suicide deaths in African countries. In Sub-Saharan Africa, a meta-analysis among young people revealed that the median lifetime prevalence estimate of self-harm was 10.3% [43]. The high prevalence of self-harm may translate into a high suicide rate in this region.
In Western Asia, Muslim-majority countries recorded a higher average suicide rate than the overall Western Asia regional average, which included Muslim-majority and other countries. Of note, six out of 14 countries in this region recorded a male-to-female suicide rate ratio of more than 4.0. Future studies could expand on these preliminary findings to examine the reason behind the relatively higher suicide rates in Muslim-majority countries in the Western Asia region in comparison with other countries.
We found no association between the proportion of Muslims and age-standardized suicide rates. This finding is not consistent with Shah and Chandia’s [20] study on suicide rates of 27 countries based on WHO data between 1991-2002, where the higher proportion of Muslims was associated with lower suicide rates for both males and females. The difference may be because Shah and Chandia’s [20] study included countries where Muslims were not the majority. Therefore, further studies are needed to establish the protective effect of Islam for males and females. However, we found that the higher the proportion of Muslims in a country, the lower the male-to-female suicide rate ratio. This means females had a relatively higher risk of dying by suicide in Muslim-majority countries with a higher Muslim population proportion.
We also found that a higher HDI index was associated with a higher male-to-female suicide rate ratio, i.e. females had a lower risk of dying by suicide in countries with better quality of life and economic development. The findings were consistent with another study of 91 countries where a higher HDI was associated with higher suicide rates among males [44]. Factors contributing to higher female suicide rates such as greater gender inequality and lack of education and economic freedom [45] may be lower in Muslim-majority countries with a higher HDI. Our study also found that the higher the HDI index, the lower the age-standardized suicide rate in Muslim-majority countries. The results were dissimilar with another study in which high and very high HDI countries had significantly higher suicide rates in comparison with medium HDI countries [44]. However, the aforesaid study [44] did not include low HDI countries, which are more prevalent in our study. Therefore, HDI may be more protective of suicide among low and middle HDI countries in comparison with high and very high HDI countries, but this needs to be further investigated in future studies.
Suicide trends in Muslim-majority countries across regions
Overall, the suicide trend in a majority of Muslim-majority countries indicated a significant decrease in 2000-2019. This was shown for countries in Central Asia which have traditionally recorded very high suicide rates and, nevertheless, even after a significant decrease, they still recorded higher rates than the global average. However, a few countries in Western Asia (Azerbaijan and Saudi Arabia) and Brunei in Southeastern Asia recorded an overall increase in the AAPCs during the past 20 years. In addition, a few countries experienced an upward trend after an initial decrease, which were Bangladesh (2014 onwards), Kuwait (2011 onwards), and Syria (2006 onwards). Syria recorded an upward trend between 2000-2010, a downward trend between 2010-2015, and an upward trend between 2015-2019. While it is difficult to determine the causes of these trends, a number of legal, health, and psychosocial events may be contributing factors. In Bangladesh, the ban of class I pesticides in 2000 was successful in decreasing suicide deaths attributable to pesticide poisoning between 2001 and 2014 [46]. However, a psychological autopsy study conducted on suicide deaths between July 2019 to July 2020 in Dhaka, Bangladesh showed that pesticide poisoning was still the most prevalent suicide method [47]. The upward trend in suicide rates in Syria between 2006 to 2019 may be partly explained by the Syrian civil war which began in 2011 and was a factor contributing to between 16% to 84% of Syrians suffering from post-traumatic stress disorder, and 11% to 49% from depression [48]. Sierra Leone recorded an upward trend in suicide rates between 2015 and 2019, and this may be related to the increased incidence of grief, post-traumatic stress, depression, and unexplained somatic symptoms owing to the Ebola outbreak between 2015 and 2017 [49]. These may have stemmed from the social ramifications of the disease such as the loss of loved ones, and stigma and violence against those presumed infected, depriving affected individuals of the traditional social support needed to overcome the crisis [50, 51].
The results of this study have implications for suicide prevention in Muslim-majority countries. First of all, based on the WHOMiNDBank, only Uzbekistan has a national suicide prevention policy [52]. In Kazakhstan, the Adolescent Mental Health and Suicide Prevention (AMHSP) program was implemented in two regions and incorporated within the 2015-2020 National Action Plan. The multisectoral collaboration with UNICEF Kazakhstan and a strong national agenda on suicide prevention resulted in falling suicide rates among adolescents aged 15-19 years old and is now being scaled nationally [53, 54]. There is a need for similar national suicide prevention activities to be developed and implemented in the other Muslim-majority countries. In addition, the considerable differences in suicide rates between the Muslim-majority countries studied should encourage further research on the multifaceted influence (or limitations) of religion in affecting the country- and region-level suicide rates [55]. For example, the countries represented in this study are from different socio-economic stages of development. How religious influence interacts with socio-economic and other factors is still far from definitive. Hence, any endeavor which attempts to provide a common explanation is bound to suffer from shortcomings and criticism. Future research can benefit from investigating the underlying mechanisms behind the decrease of suicide rates in countries that recorded a significant decrease in suicide rates during the past 20 years.
Limitations
This was an analysis based on WHO estimated suicide data for each country. Of the 46 Muslim-majority countries surveyed, only three countries (Kazakhstan, Kuwait, and Kyrgyzstan) had vital registration data which was ranked high-quality, whilst 56.5% of the Muslim-majority countries, and all Muslim-majority countries from the Sub-Saharan Africa region, had death registration data which were either unavailable or deemed unusable due to their low quality. Therefore, these data need to be interpreted with caution [1]. Certain countries not listed as UN and WHO member states, such as Palestine, were not included in this study, as data on suicide rates were not available. Important insights from these countries may therefore be left out, and future studies are required. There was a wide range in the proportion of the population in each country that had a Muslim affiliation. No research has been done on the level of belief-specific practices followed in each country, which was beyond the scope of this paper. In addition, we did not disaggregate the 20-year suicide trend data by gender, age cohort, and other demographic indicators. This is recommended for future studies, which could contribute to a greater understanding of groups that contributed most to the changes, and therefore prevention initiatives could be tailored. The correlation analyses conducted between the proportion of the Muslim population, age-standardized suicide rate, male-to-female suicide rate ratio, and HDI did not control for other variables and was limited to 2019. Future studies should conduct panel analyses using multiple sources spanning several years.
The influence of Islamic culture or Islamic laws on gender roles was also not examined. Some countries may be governed by Syariah (Islamic) laws that may prohibit attempted suicide, including some which may criminalize attempted suicide. Effects of this on suicide rates were not investigated. Some countries may have under-reported suicide due to different levels of development and accuracy in their suicide reporting system. It is a custom for a Muslim to be buried early before decay sets in [56], normally, before the next day prayer. This practice may create pressure on the proper recording of suicide data as sometimes it limits the time available for the police, coroners, or pathologists to confirm the cause of death. Sudden death among women was also found to be less frequently reported as a suicide, in comparison with male suicide, due to the need to preserve family honor [57]. The WHO classified the mortality data quality of some countries as “poor”, and these need to be interpreted with caution [58].
Conclusions
In conclusion, not all Muslim-majority countries have a lower suicide rate than the global average. This might be a reflection of the variations in the religious practice or the implementation of Syariah laws in judicial and social structures. This important finding needs further in-depth country- or region-specific exploration with policy analysis.
Supplementary Information
Additional file 1: Fig S1. Age-standardized suicide rate in Muslim-majority countries in 2000-2019 and comparison with the global average.
Acknowledgements
Not applicable
Abbreviations
- AAPC
Average annual percentage change
- APC
Annual percentage change
- GHO
Global Health Observatory
- HDI
Human Development Index
- UNICEF
United Nations Children’s Fund
- WHO
World Health Organization
Authors’ contributions
BL, DL, and KK conceptualized the study. BL, KK, WSC, ZZW, and CSS analyzed and/or interpreted the data. All authors were involved in writing and reviewing the manuscript drafts. All authors read and approved the final manuscript.
Funding
This study was funded by the Geran Galakan Penyelidik Muda (GGPM-2021-031) and the Skim Insentif Penerbitan Jurnal 2021 (GP-2021-K023687 (02), Universiti Kebangsaan Malaysia. The funding body did not have a role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the WHO Global Health Estimates repository, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/age-standardized-suicide-rates-(per-100-000-population)
Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The data used in the study were anonymized/deidentified.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bob Lew, Email: boblew@asiacrux.com.
David Lester, Email: David.Lester@stockton.edu.
Kairi Kõlves, Email: k.kolves@griffith.edu.au.
Paul S. F. Yip, Email: sfpyip@hku.hk
Ying-Yeh Chen, Email: catriona.cordelia@gmail.com.
Won Sun Chen, Email: wchen@swin.edu.au.
M. Tasdik Hasan, Email: tasdikhdip@yahoo.com.
Harold G. Koenig, Email: harold.koenig@duke.edu
Zhi Zhong Wang, Email: wzhzh_lion@126.com.
Muhamad Nur Fariduddin, Email: fariduddin@uitm.edu.my.
Emek Yuce Zeyrek-Rios, Email: eyz200@nyu.edu.
Caryn Mei Hsien Chan, Email: caryn@ukm.edu.my.
Feisul Mustapha, Email: feisulidzwan@gmail.com.
Mimi Fitriana, Email: Mimifitriana@iumw.edu.my.
Housseini Dolo, Email: hdolo@icermali.org.
Burak M. Gönültaş, Email: mburakgonultas@gmail.com
Mahboubeh Dadfar, Email: dadfar.m@iums.ac.ir, Email: mahboubehdadfar@yahoo.com.
Mojtaba Davoudi, Email: davoudi85@gmail.com.
Ahmed M. Abdel-Khalek, Email: aabdel-khalek@hotmail.com
Lai Fong Chan, Email: laifchan@ppukm.edu.my.
Ching Sin Siau, Email: chingsin.siau@ukm.edu.my.
Norhayati Ibrahim, Email: yatieibra@ukm.edu.my.
References
- 1.WHO . Age-Standardised Suicide Rates for 2000-2019. 2021. [Google Scholar]
- 2.WHO. Suicide Prevention. https://www.who.int/health-topics/suicide#tab=tab_1. Accessed 19 Oct 2021.
- 3.Cerel J, Brown MM, Maple M, Singleton M, Van de Venne J, Moore M, Flaherty C. How many people are exposed to suicide? Not six. Suicide Life Threat Behav. 2019;49(2):529–534. doi: 10.1111/sltb.12450. [DOI] [PubMed] [Google Scholar]
- 4.WHO . One in 100 Deaths is by Suicide. 2021. [Google Scholar]
- 5.WHO . Live Life: An implementation guide for suicide prevention in countries. 2021. [Google Scholar]
- 6.Eskin M, Baydar N, Harlak H, Hamdan M, Mechri A, Isayeva U, Abdel-Khalek AM, Rezaeian M, Asad N, El-Nayal M, Al BF. Cultural and interpersonal risk factors for suicide ideation and suicide attempts among Muslim college students from 11 nations. J Affect Disord. 2021;294:366–374. doi: 10.1016/j.jad.2021.07.050. [DOI] [PubMed] [Google Scholar]
- 7.Yip PSF, Zheng Y, Wong C. Demographic and epidemiological decomposition analysis of global changes in suicide rates and numbers over the period 1990–2019. Inj Prev. 2022;28:117–24. [DOI] [PubMed]
- 8.Gearing RE, Alonzo D. Religion and suicide: new findings. J Relig Health. 2018;57(6):2478–2499. doi: 10.1007/s10943-018-0629-8. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence RE, Oquendo MA, Stanley B. Religion and suicide risk: a systematic review. Arch Suicide Res. 2016;20(1):1–21. doi: 10.1080/13811118.2015.1004494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu A, Wang JY, Jia CX. Religion and completed suicide: A meta-analysis. PloS One. 2015;10(6):e0131715. doi: 10.1371/journal.pone.0131715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lester D. Does religiosity predict suicidal behavior? Religions. 2017;8(11):238. [Google Scholar]
- 12.Dadfar M, Lester D, Turan Y, Beshai JA, Unterrainer HF. Religious spiritual well-being: results from Muslim Iranian clinical and non-clinical samples by age, sex and group. J Relig Spiritual Aging. 2021;33(1):16–37. [Google Scholar]
- 13.Ibrahim N, Din NC, Ahmad M, Amit N, Ghazali SE, Wahab S, Kadir NB, Halim FW, Halim MR. The role of social support and spiritual wellbeing in predicting suicidal ideation among marginalized adolescents in Malaysia. BMC Public Health. 2019;19(4):1–8. doi: 10.1186/s12889-019-6861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lester D. Suicide and Islam. Arch Suicide Res. 2006;10(1):77–97. doi: 10.1080/13811110500318489. [DOI] [PubMed] [Google Scholar]
- 15.Klomek AB, Nakash O, Goldberger N, Haklai Z, Geraisy N, Yatzkar U, Birnai A, Levav I. Completed suicide and suicide attempts in the Arab population in Israel. Soc Psychiatry Psychiatr Epidemiol. 2016;51(6):869–876. doi: 10.1007/s00127-016-1219-2. [DOI] [PubMed] [Google Scholar]
- 16.Mirhashemi S, Motamedi MH, Mirhashemi AH, Taghipour H, Danial Z. Suicide in Iran. Lancet. 2016;387(10013):29. doi: 10.1016/S0140-6736(15)01296-9. [DOI] [PubMed] [Google Scholar]
- 17.Naveed S, Qadir T, Afzaal T, Waqas A. Suicide and its legal implications in Pakistan: a literature review. Cureus. 2017;9(9):e1665. [DOI] [PMC free article] [PubMed]
- 18.Snowdon J, Saberi SM, Moazen-Zadeh E. A comparison between the age patterns and rates of suicide in the Islamic Republic of Iran and Australia. East Mediterr Health J. 2020;26(6):748–54. [DOI] [PubMed]
- 19.Saiz J, Ayllón-Alonso E, Sánchez-Iglesias I, Chopra D, Mills PJ. Religiosity and suicide: a large-scale international and individual analysis considering the effects of different religious beliefs. J Relig Health. 2021:60;2503–26. [DOI] [PubMed]
- 20.Shah A, Chandia M. The relationship between suicide and Islam: a cross-national study. J Inj Violence Res. 2010;2(2):93. doi: 10.5249/jivr.v2i2.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alothman D, Fogarty A. Global differences in geography, religion and other societal factors are associated with sex differences in mortality from suicide: an ecological study of 182 countries. J Affect Disord. 2020;260:67–72. doi: 10.1016/j.jad.2019.08.093. [DOI] [PubMed] [Google Scholar]
- 22.Savani S, Gearing RE, Frantsuz Y, Sozinova M. Suicide in Central Asia. Suicidology. Online. 2020;11:1. [Google Scholar]
- 23.World Health Organization . WHO Methods and Data Sources for Country-Level Causes of Death 2000-2019. WHO; 2020. [Google Scholar]
- 24.United Nations Development Programme. Human Development Report 2019. Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century. https://hdr.undp.org/sites/default/files/hdr2019.pdf. Accessed 19 Jan 2022.
- 25.United Nations Department of Social and Economic Affairs. World Population Prospects 2019. https://population.un.org/wpp/Download/Standard/Population/. Accessed 19 Jan 2022.
- 26.Pew Research Centre. Table: Muslim Population by Country. https://www.pewforum.org/2011/01/27/table-muslim-population-by-country/. Accessed 19 Oct 2021.
- 27.World Population Review. Muslim majority countries. https://worldpopulationreview.com/country-rankings/muslim-majority-countries. Accessed 19 Oct 2021.
- 28.United Nations . SDG Indicators: Regional groupings used in Report and Statistical Annex. 2021. [Google Scholar]
- 29.WHO. Suicide mortality rate (per 100 000 population). https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4664. Accessed 31 Dec 2021.
- 30.Kim HY. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod. 2013;38:52–54. doi: 10.5395/rde.2013.38.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ryan SE, Porth LS. A Tutorial on the Piecewise Regression Approach Applied to Bedload Transport Data. Gen Tech Rep. Fort Collins, CO: U.S. Department of Agriculture, Forest Service, Rocky Mountain Research Station;2007.
- 32.Inoue K, Seksenbayev N, Chaizhunusova N, Moldagaliyev T, Ospanova N, Tokesheva S, Zhunussov YT, Takeichi N, Noso Y, Hoshi M, Kawano N. An exploration of the labor, financial, and economic factors related to suicide in the Republic of Kazakhstan. Int J Env Res Public Health. 2021;18(13):6992. doi: 10.3390/ijerph18136992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shekhani SS, Perveen S, DeS H, et al. Suicide and deliberate self-harm in Pakistan: a scoping review. BMC Psychiatry. 2018;18:44. doi: 10.1186/s12888-017-1586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. Suicide worldwide in 2019: Global health estimates. https://www.who.int/publications/i/item/9789240026643. Accessed 19 Jan 2022.
- 35.Ali AY. The Holy Quran: Text, Translation, and Meaning. Maryland; 1989. [Google Scholar]
- 36.Pritchard C, Iqbal W, Dray R. Undetermined and accidental mortality rates as possible sources of underreported suicides: population-based study comparing Islamic countries and traditionally religious Western countries. BJPsych Open. 2020;6(4);E56. [DOI] [PMC free article] [PubMed]
- 37.Pritchard C, Amanullah S. An analysis of suicide and undetermined deaths in 17 predominantly Islamic countries contrasted with the UK. Psychol Med. 2007;37:421–430. doi: 10.1017/S0033291706009159. [DOI] [PubMed] [Google Scholar]
- 38.Zeyrek EY, Gençöz F, Bergman Y, Lester D. Suicidality, problem-solving skills, attachment style, and hopelessness in Turkish students. Death Stud. 2009;33(9):815–827. doi: 10.1080/07481180903142407. [DOI] [PubMed] [Google Scholar]
- 39.Sayil I, Berksun OE, Palabiyikoğlu R, Oral A, Haran S, Güney S, Binici S, Geçim S, Yücat T, Beder A, Özayar H. Attempted suicides in Ankara in 1995. Crisis. 1998;19(1):47. doi: 10.1027/0227-5910.19.1.47. [DOI] [PubMed] [Google Scholar]
- 40.Lester D, Castromayor IJ, Içli T. Locus of control, depression, and suicidal ideation among American, Philippine, and Turkish students. J Soc Psychol. 1991;131(3):447–449. doi: 10.1080/00224545.1991.9713873. [DOI] [PubMed] [Google Scholar]
- 41.Lester D. Women and suicide in Islamic sub-Saharan Africa. Psychol Rep. 2008;102(3):734–738. doi: 10.2466/pr0.102.3.734-738. [DOI] [PubMed] [Google Scholar]
- 42.Vijayakumar L, Ray S, Fernandes TN, Pathare S. A descriptive mapping review of suicide in vulnerable populations in low and middle countries. Asia Pac Psychiatry. 2021;13:e12472. doi: 10.1111/appy.12472. [DOI] [PubMed] [Google Scholar]
- 43.Quarshie EN, Waterman MG, House AO. Self-harm with suicidal and non-suicidal intent in young people in sub-Saharan Africa: a systematic review. BMC Psychiatry. 2020;20(1):1–26. doi: 10.1186/s12888-020-02587-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen YY, Chen M, Lui CS, Yip PS. Female labour force participation and suicide rates in the world. Soc Sci Med. 2017;195:61–67. doi: 10.1016/j.socscimed.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 45.Khazaei S, Armanmehr V, Nematollahi S, Rezaeian S, Khazaei S. Suicide rate in relation to the Human Development Index and other health related factors: A global ecological study from 91 countries. J Epid Glob Health. 2017;7(2):131–134. doi: 10.1016/j.jegh.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chowdhury FR, Dewan G, Verma VR, Knipe DW, Isha IT, Faiz MA, Gunnell DJ, Eddleston M. Bans of WHO class I pesticides in Bangladesh—suicide prevention without hampering agricultural output. Int J Epidemiol. 2018;47(1):175–184. doi: 10.1093/ije/dyx157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arafat SY, Mohit MA, Mullick MS, Kabir R, Khan MM. Risk factors for suicide in Bangladesh: case–control psychological autopsy study. BJPsych Open. 2021;7(1). [DOI] [PMC free article] [PubMed]
- 48.Hendrickx M, Woodward A, Fuhr DC, Sondorp E, Roberts B. The burden of mental disorders and access to mental health and psychosocial support services in Syria and among Syrian refugees in neighboring countries: a systematic review. J Public Health. 2020;42(3):e299–e310. doi: 10.1093/pubmed/fdz097. [DOI] [PubMed] [Google Scholar]
- 49.Hopwood H, Sevalie S, Herman MO, Harris D, Collet K, Bah AJ, Beynon F. The burden of mental disorder in Sierra Leone: a retrospective observational evaluation of programmatic data from the roll out of decentralised nurse-led mental health units. Int J Ment Health Syst. 2021;15(1):1–27. doi: 10.1186/s13033-021-00455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yadav S, Rawal G. The current mental health status of Ebola survivors in Western Africa. J Clin Diag Res. 2015;9(10):LA01. doi: 10.7860/JCDR/2015/15127.6559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Secor A, Macauley R, Stan L, Kagone M, Sidikiba S, Sow S, Aronovich D, Litvin K, Davis N, Alva S, Sanderson J. Mental health among Ebola survivors in Liberia, Sierra Leone and Guinea: results from a cross-sectional study. BMJ Open. 2020;10(5):e035217. doi: 10.1136/bmjopen-2019-035217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO . MiNDbank: Suicide Prevention. 2021. [Google Scholar]
- 53.UNICEF . Mainstreaming Adolescent Mental Health and Suicide Prevention in Kazakhstan’s Educational and Health Systems. 2019. [Google Scholar]
- 54.Wasserman C, Darky T. Assessment of suicide preventative activities in Kazakhstan: Kyzylorda and East Kazakhstan regions. 2014. [Google Scholar]
- 55.Chelmardi AK, Rashid S, Dadfar M, Lester D. Understanding Suicidal Behavior Using a Comprehensive Approach. Illn Crisis Loss. 2021;10541373211051058.
- 56.Sarhill N, LeGrand S, Islambouli R, Davis MP, Walsh D. The terminally ill Muslim: death and dying from the Muslim perspective. Am J Hosp Palliat Med. 2001;18(4):251–255. doi: 10.1177/104990910101800409. [DOI] [PubMed] [Google Scholar]
- 57.Canetto SS. Suicidal Behaviors Among Muslim Women. Crisis. 2015;36(6):447–458. doi: 10.1027/0227-5910/a000347. [DOI] [PubMed] [Google Scholar]
- 58.Knipe DW, Metcalfe C, Gunnell D. WHO suicide statistics–a cautionary tale. Ceylon Med J. 2015;60(1):35. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig S1. Age-standardized suicide rate in Muslim-majority countries in 2000-2019 and comparison with the global average.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the WHO Global Health Estimates repository, https://www.who.int/data/gho/data/indicators/indicator-details/GHO/age-standardized-suicide-rates-(per-100-000-population)