Abstract
Background:
Several environmental factors are associated with the risk of acute lower respiratory infections (ALRIs) and upper respiratory infections (URIs) in children under 5 years of age (YOA). Evidence implicating chemical pesticides remains equivocal. There are also no data on this subject in these children in Ghana. This study investigated the association between urinary pesticide residual levels and the risk for ALRIs/URIs in children under 5 YOA.
Methods:
The participants for this study were from the Offinso North Farm Health Study, a population-based cross-sectional study. Two hundred and fifty four parents/guardians who had answered affirmatively to the question “Has your child ever accompanied you to the farm?” were interviewed on household socio-demographic and environmental factors, being breastfed, child education, age, gender, and respiratory infection. One hundred fifty children were randomly selected to provide the first void urine.
Results:
The proportion of children with ALRI was 22.1% and those with URI was 35.8%. We observed a statistically significant exposure-response relation of p,p′-DDE (tertile) with ALRI (1.7-3.2 µg/L urine: prevalence ratio [PR] = 1.22 [1.05-1.70], ⩾3.2 µg/L urine: 1.50 [1.07-3.53] [P-for trend = .0297]). This observation was in children older than two YOA (P-for trend = .0404). Delta-HCH and beta-HCH (2-levels) were significantly associated with ALRI but not URI. The risk of ALRI increased with deltamethrin levels in an exposure-response manner (2.5-9.5 µg/L urine: 2.10 [1.37-3.24], ⩾9.5 µg/L urine: 4.38 [1.87-10.32] [P-for trend = .0011]) and this was also observed in children older than two YOA. Similar observation was noted for URI. Bifenthrin (>0.5 µg/L urine) was positively associated with ALRI and URI whereas permethrin (⩾1.2 µg/L urine) was not associated only with URI.
Conclusions:
The present study supports the hypothesis that exposure to chemical pesticides is associated with respiratory infections in children under 5 YOA.
Keywords: Ghana, Offinso North District, respiratory infection, urinary pesticides residual levels, children under 5 years of age
Introduction
Acute respiratory infections are one of the most important risk factors for morbidity and mortality in children under 5 years of age (YOA). 1 Acute lower respiratory tract infections (ALRIs), mainly pneumonia, bronchiolitis, and acute laryngitis are the major contributors that account for the global burden of ALRIs-related mortality in children under 5 YOA. 2 Lower respiratory infection is the second most important cause of morbidity and mortality in Ghana and the Offinso North district. 3
Several risk factors are known to increase vulnerability to ALRIs in children and these include exposure to tobacco smoke, household air pollution, lack of breastfeeding, familial history of atopy or allergic asthma, and sociocultural-related factors.4,5 Children’s hand-to-mouth and object-to-mouth behavior in contaminated areas may also increase their risk and degree of pesticide exposure. 6 These factors may act independently or in concert with other variables to increase the incidence and severity of ALRIs. 7 There is evidence associating chemical pesticides exposures to adverse health outcomes.
The demand for vegetables by the growing Ghanaian population has resulted in an increase of importation and utilization of chemical pesticides to manage the pests on the farm. 8 Many of these pesticides belong to Class II (moderately hazardous) or Class III (slightly hazardous).8,9 In addition some persistent, banned, or restricted pesticides smuggled into the country are used by farmers. 10 The short and long-term adverse health outcomes among adults following the use of these pesticides are well documented.11 -13 However, evidence linking chemical pesticides exposures to ALRIs in children under 5 years of age remains equivocal. Dallaire et al 14 investigated the effect of prenatal exposure to pesticides on the incidence of acute infections in Inuit infants. Maternal plasma collected during delivery was sampled and assayed for total polychlorinated biphenyl congeners (PCBs), PCB-153, and dichlorodiphenyldichloroethylene (DDE). There was no association of prenatal levels of PCBs/DDEs with a respiratory infection. A Swedish study failed to establish any significant relationship between maternal serum concentration of DDE sampled during pregnancy and ALRI and wheezing. 15 In a Menorcan birth cohort study, DDE was found to increase the risk of wheezing and asthma at ages four and seven YOA, but neither wheezing nor ALRI incidence increased during the first year of life. 16 However, in Spain, Sunyer et al 17 sampled the serum of 584 women during pregnancy and assayed for p, p-DDE, p,p-DDT find, PCB congeners 28, 118, 138, 153, and 180, hexachlorobenzene, and -hexachlorocyclohexane. The authors did not find any association of p,p-DDE with recurrent ALRI. Adjusting for PCBs and the organochlorines did not change the results. This finding was also confirmed in a much bigger population consisting of 1455 mother-child pairs in 3 regions in Spain (Gipuzkoa, Sabadell, and Valencia), 18 in Mexico, in Japan, and in Costa Rica.19 -22 Previous studies on this subject were are conducted in Europe, and North and South America and they vary widely in the way in which the studies were conducted. Evidence from Asia and Africa is lacking. There also no data on the health effect of pesticides in children under 5 YOA in Ghana. Understanding pesticide exposures and health effects in children in Ghana will inform corrective control programs in the event it is a real problem.
In Ghana individuals living in farming communities are exposed to high concentrations of a variety of pesticides, including fumigants, fungicides, herbicides, insecticides, and banned pesticides.11,22,23 The Offinso North district is a major vegetable-growing area in Ghana and has one of the highest pesticide usage rates. Previously, we have reported high concentrations of OCs and organophosphate in adult farmers in the Offinso North district. 24 The current study determines the association between urinary pesticide residual levels and respiratory infections in children under 5 YOA.
Materials and Methods
Study participants, study design, and setting
The participants for this study are children under 5 YOA from the Offinso North Farm Health Study (ONFAHS). The ONFAHS is a population-based cross-sectional study in the Offinso North District of the Ashanti Region, Ghana. Offinso North district is a major vegetable farming community, located about 95 km Northwest of Kumasi, the administrative capital of the Ashanti Region. The district is made up of 17 small and 3 large farming communities.11,12 The communities are socio-culturally and economically homogenous. The population of the North Offinso district is 83 440 of which about 32 210 live in Akumadan, Nkenkenson, and Afrancho. Study participants were selected from the 3 large farming communities, namely Akumadan, Nkenkenson, and Afrancho (Figure 1).
Figure 1.
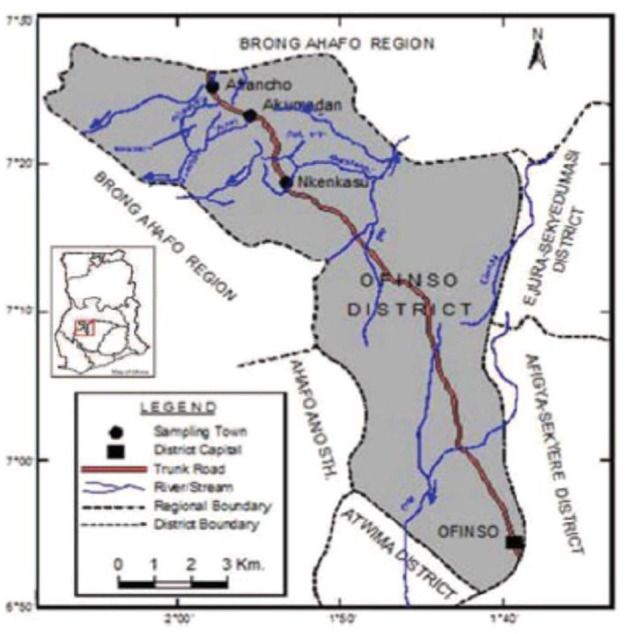
Map showing the Offinso North District and the study areas-Afrancho, Akumadan, and Nkenkasu.
Data collection
Data collection began before the spraying season. A detailed description of this study including eligibility criteria, study design, and sampling are reported elsewhere.11,24 Briefly, between May and July 2017, 330 households in the 3 major farming communities in the district were conveniently sampled into the study. Trained local agriculture extension officers scheduled interview appointments with parents/guardians of the children at approximately 05:00 at their homes because most parents leave their homes for their farms around 06:00. The interviewers asked questions about household socio-demographic and environmental factors, questions related to the children such as, if the child was or is being breastfed, child education, age, gender, and so on. Much other information was taken from the parents/guardians of the children but were not included in this analysis. In the current analysis, the study population included 254 children under 5 YOA whose parents had answered affirmatively to the question “Has your child ever accompanied you to the farm?”
Upon recruitment, 150 children were randomly selected to provide urine samples. Their parents were provided sterile, metal-free plastic urine containers (50 mL) (Sarstet S-monovette, Germany) or commode inserts for children who were unable to urinate into the specimen tube (usually females). If the insert was used, the parent transferred the urine into the specimen cup. Urine samples were collected after the interview. Parents were advised to use clean water and soap to wash their hands before handling the sterile metal-free plastic urine containers. They were also instructed to void out the first portion of the urine stream before the collection of 50 mL midstream urine. The protocol for urine handling, and procedure used for laboratory analysis of pesticide residues is explained in detail elsewhere. 11 Briefly, ten mL of the urine were drawn into each of 4 sterile sample tubes (Sarstedt, S-monovette, Germany) and stored in refrigerated boxes containing ice packs (at 4°C-8°C) and shipped to the Ghana Standards Authority for analysis with a gas chromatograph (CP-3800, Varian, Inc., Walnut Creek, CA) equipped with an electron capture detector (CP-3800, Varian, Inc.) (GC-ECD) and a capillary column (VF—5 mS, 40 m × 0.25 mm × 0.25 mm, also from Varian, Inc.). The GC-ECD operation conditions were: temperature program, 70°C (for 2 minutes) to 180°C (for 1 minutes) increasing at 25°C/minute, to 300°C increasing at 5°C/minute; injector temperature, 270°C; detector temperature, 300°C; carrier gas, nitrogen at 1.0 mL/minute, and makeup gas, nitrogen at 29 mL/minute. Approval for this study was provided by the Ghana Health Services Ethical Review Board. Informed consent was obtained from parents on behalf of the children.
Main determinants of interest
The main determinants of interest were the concentrations of four organochlorines, eight pyrethroids, and seven organophosphates pesticides in hexane extracts of 24 hours urine samples collected in the early hour of the morning.
Health outcome
Our health outcome was acute respiratory infection defined as symptoms of acute lower respiratory infection (ALRI) and upper respiratory infection (URI) at any time in the 2 weeks period preceding the survey interview. ALRI here is defined as cough accompanied by short and rapid breathing and feverish condition. URI is defined as the experience of runny nose, nasal congestion, sore throat, sneezing, watery eyes, and/or ache in the ears. These definitions were consistent with other studies in terms of the symptoms considered relevant.25,26
Confounders
Potential confounders included the gender of the child, parental education, marital status, cooking fuel type, child fed exclusively on breast milk, ethnicity, age of the child, and zonal community and were retrieved from the questionnaire. The definition of these confounders is shown in Table 1. The selection of these variables was informed by literature4,11,16-21 and their significant association with the outcomes of interest at P < .05.
Table 1.
Personal and environmental characteristics of the study population of children below 5 years of age, the North Offinso Farm Health study (NOFAHS) (n = 254).
| Characteristics of the study population | N | % |
|---|---|---|
| Child gender | ||
| Male | 167 | 65.75 |
| Female | 87 | 34.25 |
| Age of child (y) | ||
| ⩾1 | 31 | 12.20 |
| 2 | 41 | 16.14 |
| 3 | 96 | 37.80 |
| 4 | 86 | 33.86 |
| Child education | ||
| Do not attend school | 119 | 46.85 |
| Crèche | 21 | 8.27 |
| Kindergarten | 114 | 44.88 |
| Child exclusive breastfeeding | ||
| Yes | 35 | 13.78 |
| No | 219 | 86.22 |
| Age of parent who filled the questionnaire (y) | ||
| <30 | 9 | 3.54 |
| 35-45 | 58 | 22.83 |
| 45-55 | 114 | 56.69 |
| >55 | 45 | 16.93 |
| Marital status of the parent who filled the questionnaire | ||
| Single | 65 | 25.59 |
| Married | 189 | 74.41 |
| Ethnic origin | ||
| Akan | 109 | 42.91 |
| Ewe | 28 | 11.02 |
| Ga | 15 | 5.91 |
| Hausa | 96 | 37.80 |
| Others* | 6 | 2.36 |
| Parental education | ||
| Have not been to school | 167 | 65.75 |
| JSS/middle school/primary school | 78 | 30.71 |
| SSS/secondary school/vocational or technical training | 9 | 3.54 |
| Father’s smoking habit | ||
| Never smoker | 219 | 86.22 |
| Past smoker | 19 | 7.48 |
| Current smoker | 16 | 6.30 |
| Mother’s smoking habit | ||
| Never smoker | 244 | 96.44 |
| Past smoker | 6 | 1.98 |
| Current smoker | 4 | 1.58 |
| Father’s drinking habit | ||
| Current drinker | 193 | 75.98 |
| Past drinker | 41 | 16.14 |
| Never drinker | 20 | 7.87 |
| Mother’s drinking habit | ||
| Current drinker | 226 | 89.33 |
| Past drinker | 8 | 3.16 |
| Never drinker | 19 | 7.51 |
| Fuel type used | ||
| Low pollution fuel | 4 | 1.57 |
| Medium pollution fuel | 139 | 54.72 |
| High pollution fuel | 111 | 43.70 |
| The location where pesticides are stored at home | ||
| Kitchen | 86 | 33.86 |
| Bedroom | 36 | 14.17 |
| Designated storeroom inside a home | 46 | 18.11 |
| Designated storeroom outside a home | 55 | 21.65 |
| Animal house | 31 | 12.21 |
| Zonal communities | ||
| Akumadan | 109 | 42.91 |
| Nkenkenso | 80 | 31.50 |
| Afrancho | 65 | 25.59 |
Kusasi, dagati, dagomba, and Komkumba.
Statistical methods
For continuous variables, mean, standard deviation, median, minimum, maximum, lower quartile, upper quartile, 90th, 95th, and 99th percentile were computed. Proportions were computed for categorical variables. The generalized linear models (SAS PROC GENMOD) with a binomial distribution and log link function were used to assess the association of urinary pesticide residual levels (eg, organophosphate, pyrethroids, and organochlorines) and acute respiratory infection. The trend was investigated with Cochran-Armitage test for trend (significance level of .05), and we controlled for potential confounders as shown above. The analysis was further stratified by age (⩽2 years vs >2 years). Prevalence ratio (PR) was the effect measure. The analysis was performed with the SAS statistical software package (SAS, version 9.3, SAS Institute, Cary, NC).
Results
Participants characteristics
The characteristics of the study population are shown in Table 1. Most of the children were males (167, 65.8%), were3 YOA (96, 37.8%), did not attend school (119, 46.9%), were not fed exclusively on breast milk (219, 86.2%), and belong to ethnic groups such as the Gas, the Kokonbas, the Sisala, and the Moshi (172, 67.7%). Most of the parents of these children had no formal education (167, 65.8%), never smoked (219, 86.2 vs 244, 96.4%: father vs mother, respectively), and currently drinking alcohol (193, 76.0% vs 226, 89.3%: father vs mother, respectively). In homes of most of these children (139, 54.7%), medium polluted fuel (ie, charcoal) is the primary source for daily energy needs. Pesticides were stored in different locations including designated storehouses outside the home (55, 21.7.0%) or animal houses (31, 12.2%) or kitchens (86, 33.9%) or bedrooms (36, 14.2%).
Prevalence of ALRI/URI
The prevalence of ALRI and URI in the PSAC surveyed was 22.1% and 35.8%, respectively. The prevalence of ALRI was found to decrease with age (41.9% at 1 YOA vs 17.4% at <4 YOA, Somers D = −0.28) and to be significantly higher in girls (29.9%) than in boys (17.3%), (Somers D = 0.18) P < .0001. The proportion of children with ALRI was higher (Somers D = 0.22) in children on exclusive breastfeeding (42.9%) compared to those who were not on exclusive breastfeeding (18.7%). The risk of ALRI decreases with parental education with ALRI higher in children whose parent(s) had no formal education compared to those children whose parent(s) had secondary/vocational/technical training (16.2% vs 44.4%, Somers D = 0.16). The remaining results are shown in Table 2.
Table 2.
Prevalence of self-reported respiratory infection in children below the age of 5 years, the Offinso North Farm Health Study (ONFAHS) (N = 254).
| Characteristics of study population | Acute respiratory infection | |||
|---|---|---|---|---|
| Acute lower respiratory infection (ALRI) | Upper respiratory infection (URI) | |||
| ALRI n (%) | No ALRI n (%) | URI n (%) | No URI n (%) | |
| Total | 56 (22.05) | 198 (77.95%) | 91 (35.83) | 163 (64.17) |
| Age | ||||
| <1 | 13(41.94) | 18 (58.06) | 28 (90.32) | 3 (9.68) |
| 2 | 14 (34.15) | 27 (65.85) | 16 (39.02) | 25 (60.98) |
| 3 | 14 (14.59) | 82 (85.41) | 24 (25.00) | 72 (75.00) |
| 4 | 15 (17.44) | 71 (82.56) | 23 (26.74) | 63 (73.26) |
| Tau c = −0.28 | Somers D = −0.39 | |||
| Sex of child | ||||
| Boy | 30 (17.96) | 137 (82.04) | 43 (25.75) | 124 (74.25) |
| Girl | 26 (29.89) | 61 (70.11) | 48 (55.17) | 39 (44.83) |
| Somers D = 0.18 | Somers D = 0.31 | |||
| Child’s education | ||||
| Do not go to school | 23 (19.33) | 96 (80.67) | 46 (38.66) | 73 (61.34) |
| Crèche or Kindergarten | 33 (24.44) | 102 (75.56) | 45 (33.33) | 90 (66.67) |
| Somers D = 0.08 | Somers D = 0.03 | |||
| Child on exclusive breastfeeding | ||||
| Yes | 15 (42.86) | 20 (57.14) | 30 (85.71) | 5 (14.29) |
| No | 41 (18.72) | 178 (81.28) | 61 (27.85) | 158 (72.15) |
| Somers D = 0.22 | Somers D = 0.33 | |||
| Any parent a full-time or part-time farmer | ||||
| Full-time farmer | 40 (23.39) | 131 (76.61) | 73 (42.69) | 98 (57.31) |
| Part-time farmer | 15 (18.29) | 67 (81.71) | 17 (20.73) | 65 (79.27) |
| Missing | 1 | Somers D = −0.03 | 1 | Somers D = −0.14 |
| Parental education | ||||
| Have not been to school | 27 (16.17) | 140 (83.83) | 37 (22.16) | 130 (77.84) |
| JSS/middle school/primary school | 25 (32.05) | 53 (67.95) | 50 (64.10) | 28 (35.90) |
| SSS/secondary school/vocational or technical training | 4 (44.44) | 5 (55.56) | 4 (44.44) | 5 (55.55) |
| Somers D = 0.16 | Somers D = 0.35 | |||
| Father’s smoking habit | ||||
| Never smoker | 5 (31.25) | 11 (68.75) | 10 (62.50) | 6 (37.50) |
| Past smoker | 4 (21.05) | 15 (78.95) | 4 (21.05) | 15 (78.95) |
| Current smoker | 47 (21.46) | 172 (78.54) | 77 (35.16) | 142 (64.84) |
| Somers D = 0.02 | Somers D = 0.06 | |||
| Mother’s smoking habit | ||||
| Never smoker | 1 (25.00) | 3 (75.00) | 2 (5.00) | 2 (50.00) |
| Past smoker | 1 (20.00) | 4 (80.00) | 2 (40.00) | 3 (60.00) |
| Current smoker | 54 (22.13) | 190 (77.87) | 87 (35.66) | 157 (64.34) |
| Missing | 1 | Somers D = −0.01 | Somers D = 0.02 | |
| Father’s drinking habit | ||||
| Current drinker | 7 (35.00) | 13 (65.00) | 12 (60.00) | 8 (40.00) |
| Past drinker | 8 (19.51) | 33 (80.49) | 23 (56.10) | 18 (43.90) |
| Never drinker | 41 (21.24) | 152 (78.76) | 56 (29.02) | 137 (70.98) |
| Somers D = −0.03 | Somers D = −0.16 | |||
| Mother’s drinking habit | ||||
| Current drinker | 1 (5.26) | 18 (94.74) | 7 (36.84) | 12 (63.16) |
| Past drinker | 4 (5.00) | 4 (5.00) | 4 (50.00) | 4 (50.00) |
| Never drinker | 50 (22.12) | 176 (77.88) | 79 (34.96) | 147 (65.04) |
| Missing | 1 | Somers D = −0.02 | 1 | Somers D = −0.01 |
| Fuel type used | ||||
| Low pollution fuel | 1 (25.00) | 3 (75.00) | 3 (75.00) | 1 (25.00) |
| Medium pollution fuel | 31(22.30) | 108 (77.70) | 43 (30.94) | 96 (69.06) |
| High pollution fuel | 24 (21.62) | 87 (78.38) | 45 (40.54) | 66 (59.46) |
| Somers D = 0.01 | Somers D = −0.05 | |||
On the other hand, the prevalence of URI decreases with the increasing age of the child and this difference was significant (⩽1 YOA vs 2 YOA vs 3 YOA vs 4 YOA: 90.3% vs 39.0% vs 25.0% vs 26.7%, respectively; Somers D = −0.39). The prevalence of URI was higher in girls compared to boys (girl vs boy: 55.2% vs 25.8%; Somers D = 0.31). URI was higher in children who were exclusively breastfeed compared to those who were not (85.7% vs 27.9%; Somers D = 0.33). Children of full-time farmers compared to part-time farmers (42.7% vs 20.7%; Somers D = −0.14) had higher URI. The remaining results is in Table 2.
Concentrations of urinary pesticide residues
Mean, median and lower, and upper quartile concentrations of 8 pyrethroid, 4 organochlorine, and 7 organophosphate insecticide residues identified in urine from children are reported in Table 3. The limit of detection of all residues was 0.01 µg/L of urine.
Table 3.
Concentrations of pesticides residues in urine of children under the age of 5, the Offinso North Farm Health Study (ONFAHS) (n = 150).
| Pesticide | LOD | Min | LQ | UQ | Mean | Median | SD | 90th percentile | 95th percentile | 99th percentile | Max |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Organochlorines | |||||||||||
| PP DDE | 0.01 | 0.01 | 0.80 | 3.20 | 2.28 | 1.70 | 2.67 | 4.50 | 6.20 | 12.60 | 23.10 |
| Dieldrin | 0.01 | 0.01 | 0.40 | 8.70 | 5.53 | 3.40 | 6.11 | 14.70 | 16.30 | 24.10 | 28.80 |
| Delta-HCH | 0.01 | 0.01 | 0.01 | 0.01 | 0.11 | 0.01 | 0.36 | 0.27 | 0.80 | 2.4 | 2.4 |
| Beta-HCH | 0.01 | 0.01 | 0.01 | 0.31 | 0.53 | 0.01 | 1.36 | 1.40 | 4.10 | 6.80 | 7.6 |
| Pyrethroid | |||||||||||
| Cyfluthrin | 0.01 | 0.01 | 2.80 | 15.40 | 9.68 | 6.20 | 8.37 | 23.00 | 24.10 | 30.20 | 30.20 |
| Deltamethrin | 0.01 | 0.01 | 1.60 | 11.20 | 8.15 | 5.60 | 10.83 | 16.15 | 31.40 | 57.00 | 69.50 |
| Allethrin | 0.01 | 0.01 | 0.40 | 2.40 | 1.47 | 1.25 | 1.27 | 3.20 | 3.50 | 5.40 | 5.40 |
| Fenvalerate | 0.01 | 0.01 | 0.01 | 0.31 | 0.61 | 0.01 | 1.66 | 2.00 | 4.00 | 9.00 | 12.40 |
| Cypermethrin | 0.01 | 0.01 | 2.00 | 12.80 | 8.05 | 6.50 | 7.09 | 20.90 | 22.40 | 24.00 | 26.80 |
| Lambda cyhalothrin | 0.01 | 0.01 | 0.01 | 3.40 | 2.44 | 1.40 | 4.14 | 6.45 | 8.40 | 11.60 | 40.80 |
| Bifenthrin | 0.01 | 0.01 | 0.01 | 1.30 | 0.79 | 0.01 | 1.37 | 2.65 | 3.50 | 5.40 | 8.00 |
| Permethrin | 0.01 | 0.01 | 0.01 | 1.20 | 4.17 | 0.01 | 10.75 | 17.85 | 35.50 | 45.60 | 47.00 |
| Organophosphate | |||||||||||
| Methamidophos | 0.01 | 0.01 | 0.01 | 2.40 | 1.63 | 1.45 | 2.57 | 3.20 | 3.60 | 19.60 | 21.20 |
| Chlorpyrifos | 0.01 | 0.01 | 0.01 | 7.20 | 5.95 | 2.10 | 14.15 | 16.00 | 23.00 | 35.20 | 156.00 |
| Profenofos | 0.01 | 0.01 | 0.01 | 3.60 | 2.53 | 2.25 | 2.61 | 6.40 | 7.60 | 10.80 | 11.60 |
| Diazinon | 0.01 | 0.01 | 0.01 | 1.60 | 0.96 | 0.80 | 1.09 | 2.40 | 3.20 | 4.40 | 4.80 |
| Parathion ethyl | 0.01 | 0.01 | 0.01 | 2.40 | 1.76 | 1.35 | 1.84 | 4.05 | 5.40 | 8.60 | 9.60 |
| Dimethoate | 0.01 | 0.01 | 0.01 | 1.60 | 1.54 | 0.01 | 2.74 | 6.80 | 7.60 | 8.50 | 10.80 |
| Malathion | 0.01 | 0.01 | 0.40 | 3.40 | 2.34 | 1.80 | 2.12 | 5.35 | 6.40 | 9.10 | 9.10 |
Urinary residual levels of insecticides and self-reported respiratory infection
ALRI
Trace concentrations of pesticide residues were detected in the urine of the children (Table 4). For p,p′-DDE (continuous), no significant association was observed with ALRI (PR = 1.02; 0.98-1.11) (Table 4). But for p,p′-DDE (tertile) an increased risk with ALRI (P-for trend = .0297) was noted. The PRs for second tertile and third tertile vrs first tertile were 1.22 (1.05-1.77) and 1.50 (1.07-3.13), respectively. Delta-HCH (continuous) was significantly associated with ALRI (1.95; 1.69-2.26); and as a categorical variable was associated with ALRI (2.40; 1.30-4.42) and not confirmed in the subgroup analysis. Beta-HCH (continuous) had no significant association with ALRI, but the categorical variable was associated with ALRI (1.90; 1.03-3.52) and not confirmed in the subgroup analysis. The urinary concentration of deltamethrin (continuous) was associated with ALRI (1.03; 1.02-1.05). There was an increased risk of ALRI with deltamethrin concentration (P for trend = .0011). The PRs for second tertile and third tertile versus first tertile was 2.10 (1.37-3.24) and 4.38 (1.87-10.32), respectively. In a subgroup analysis, increasing risk of deltamethrin with ALRI (P-for trend = .0404) was also observed in children, 3, or 4 YOA but not in those below 3 YOA. The PRs for second tertile and third tertile versus first tertile were 2.48 (1.01-5.81) and 4.85 (1.15-10.98), respectively. Bifenthrin (continuous) was not associated with ALRI, but bifenthrin (>0.5 µg/L urine) was associated with ALRI (2.04; 1.11-3.74) and this was confirmed in children 3 or 4 YOA but the estimate was inconclusive. Dieldrin, cyfluthrin, allethrin, fenvalerate, cypermethrin, lambda-cyhalothrin, methamidophos, profenofos, diazinon, parathion ethyl, dimethoate, malathion, and permethrin were not significantly associated with ALRI (Table 4).
Table 4.
Association between the concentration of organochlorine, pyrethroid, and organophosphate insecticides in urine with ALRI in in children below 5 YOA, the North Offinso Farm Health study (NOFAHS) (n = 150).
| Pesticide level | ALRI | ||||||
|---|---|---|---|---|---|---|---|
| All ages | ⩽2 y | >2 y | |||||
| N* | Crude PR (95% CI) | Adjusted PR* a (95% CI) | Crude PR (95% CI) | Adjusted PR* b (95% CI) | Crude PR (95% CI) | Adjusted PR* a (95% CI) | |
| Organochlorines | |||||||
| PP DDE (continuous) | 50 | 1.01 (0.92-1.10) | 1.02 (0.93-1.11) | 1.02 (0.84-1.54) | 1.01 (0.77-1.32) | 1.01 (0.77-1.57) | 1.04 (0.94-1.16) |
| PP DDE | |||||||
| <1.70 18 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1-7-3.2 6 | 21 | 1.20 (1.03-1.73) | 1.22 (1.05-1.77) | 0.89 (0.63-3.26) | 0.67 (0.59-6.71) | 2.41 (1.09-5.62) | 3.01 (0.98-7.75) |
| ⩾ 3.2 10 | 15 | 1.44 (1.06-2.99) | 1.50 (1.07-3.13) | 0.66 (0.55-4.67) | 0.52 (0.45-7.02) | 4.02 (1.15-8.35) | 5.10 (1.03-9.11) |
| P for trend | .0345 | .0296 | .5029 | .6102 | .0218 | .0404 | |
| Delta-HCH (continuous) | 47 | 2.02 (1.75-2.34) | 1.95 (1.69-2.26) | 0.93 (0.62-1.40) | 0.92 (0.51-1.46) | 0.92 (0.88-1.48) | 0.93 (0.68-1.28) |
| Delta-HCH | |||||||
| <0.22 | 22 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.22 | 15 | 2.26 (1.18-4.33) | 2.40 (1.30-4.42) | 0.74 (0.17-3.66) | 0.72 (0.16-3.25) | 2.22 (0.61-8.05) | 2.61 (0.64-10.56) |
| Beta-HCH (continuous) | 48 | 1.00 (0.83-1.22) | 0.98 (0.81-1.20) | 0.99 (0.38-2.55) | 1.56 (0.67-3.66) | 1.56 (0.67-3.75) | 1.37(0.72-2.66) |
| Beta-HCH | |||||||
| <0.22 | 21 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.22 | 14 | 1.93 (1.04-3.57) | 1.90 (1.03-3.52) | 0.29 (0.04-2.12) | 0.73 (0.16-3.25) | 1.62 (0.45-5.90) | 2.61 (0.64-10.56) |
| Dieldrin (continuous) | 50 | 1.04 (0.99-1.08) | 1.03 (0.98-1.08) | 0.97 (0.90-1.06) | 1.04 (0.57-1.13) | 1.04 (0.97-1.13) | 1.01 (0.96-1.07) |
| Dieldrin | |||||||
| <0.55 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 0.55-8.70 | 16 | 1.50 (0.95-2.37) | 1.24 (0.84-1.85) | 0.79 (0.52-1.21) | 0.78 (0.47-1.33) | 1.81 (0.86-3.80) | 1.34 (0.73-2.48) |
| ⩾8.70 | 10 | 2.25 (0.90-5.63) | 1.54 (0.70-3.41) | 1.05 (0.67-3.45) | 0.89 (0.57-3.35) | 3.09 (0.46-8.67) | 2.35 (0.39-7.99) |
| P for trend | .4342 | .2968 | .4758 | .3154 | .1379 | .2979 | |
| Pyrethroid | |||||||
| Cyfluthrin (continuous) | 48 | 1.01 (0.91-1.05) | 1.01 (0.97-1.05) | 0.97 (0.92-1.03) | 0.98 (0.91-1.06) | 0.98 (0.91-1.06) | 0.98 (0.94-1.03) |
| Cyfluthrin | |||||||
| <6.20 | 13 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 6.20-16.0 | 22 | 1.05 (0.70-1.58) | 1.07 (0.73-1.59) | 0.79 (0.53-1.20) | 0.80 (0.43-1.50) | 1.14 (0.61-2.11) | 1.20 (0.62-2.34) |
| ⩾16 | 13 | 1.11 (0.50-2.49) | 1.15 (0.53-2.52) | 0.89 (0.41-3.01) | 0.92 (0.39-4.85) | 2.10 (0.56-4.44) | 3.11 (0.81-6.71) |
| P for trend | .8090 | .7346 | .2550 | .4869 | .6871 | .5923 | |
| Deltamethrin (continuous) | 47 | 1.03 (1.02-1.04) | 1.03 (1.02-1.05) | 1.01 (0.98-1.04) | 1.04 (1.00-1.09) | 1.05 (1.03-1.10) | 1.02 (1.00-1.05) |
| Deltamethrin | |||||||
| <2.5 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2.5-9.5 | 23 | 2.08 (1.36-3.21) | 2.10 (1.37-3.24) | 1.21 (0.96-1.75) | 1.20 (0.66-2.18) | 2.10 (1.04-4.26) | 2.48 (1.01-5.81) |
| ⩾9.5 | 14 | 4.35 (1.84-10.27) | 4.38 (1.87-10.32) | 4.04 (0.89-4.35) | 3.96 (0.69-5.01) | 4.11 (1.17-12.18) | 4.85 (1.15-10.98) |
| P for trend | .0013 | .0011 | .3232 | .5454 | .0321 | .0349 | |
| Allethrin (continuous) | 49 | 0.96 (0.73-1.26) | 0.98 (0.76-1.26) | 1.08 (0.71-1.05) | 0.95 (0.64-1.31) | 0.95 (0.64-1.39) | 0.94 (0.71-1.26) |
| Allethrin | |||||||
| <0.90 | 22 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 0.90-1.6 | 14 | 0.90 (0.63-1.28) | 0.95 (0.66-1.35) | 1.21 (0.85-1.72) | 1.44 (0.79-2.62) | 1.90 (0.65-2.16) | 0.96 (0.45-2.02) |
| ⩾1.60 | 13 | 0.81 (0.40-1.63) | 0.90 (0.44-1.83) | 1.35 (0.74-2.59) | 1.65 (0.68-4.44) | 2.10 (0.45-6.23) | 1.94 (0.26-10.45) |
| P for trend | .5510 | .7603 | .2587 | .2131 | .5694 | .9101 | |
| Fenvalerate (continuous) | 49 | 0.93 (0.74-1.18) | 0.91 (0.72-1.16) | 1.08 (0.77-1.65) | 0.95 (0.64-1.31) | 0.95 (0.64-1.39) | 0.94 (0.71-1.26) |
| Fenvalerate | |||||||
| <0.30 | 25 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.30 | 24 | 0.98 (0.76-1.26) | 1.19 (0.61-2.35) | 0.94 (0.47-1.90) | 1.02 (0.35-2.98) | 1.77 (0.56-5.59) | 1.74 (0.48-6.32) |
| Cypermethrin (continuous) | 49 | 1.01 (0.97-1.06) | 1.00 (0.96-1.06) | 1.01 (0.95-1.08) | 1.04 (0.96-1.12) | 1.03 (0.90-1.06)) | 1.02 (0.57-1.07) |
| Cypermethrin | |||||||
| <3.00 | 22 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 3.00-10.50 | 14 | 1.19 (0.79-1.79) | 1.16 (0.77-1.75) | 1.08 (0.76-1.54) | 1.21 (0.68-2.17) | 1.59 (0.79-3.20) | 1.52 (0.68-3.36) |
| ⩾10.50 | 13 | 1.42 (0.63-3.21) | 1.35 (0.56-4.01) | 1.21 (0.44-2.15) | 1.31 (0.32-2.89) | 1.41 (0.59-4.32) | 1.39 (0.47-4.41) |
| P for trend | .4176 | .3245 | .6717 | .5118 | .1779 | .2963 | |
| Lambda-cyhalothrin (continuous) | 47 | 0.99 (0.92-1.06) | 0.98 (0.91-1.06) | 1.02 (0.97-1.07) | 0.99 (0.78-1.25) | 0.99 (0.78-1.25) | 1.01 (0.95-1.37) |
| Lambda-cyhalothrin | |||||||
| <1.50 | 29 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.50 | 18 | 1.28 (0.68-2.41) | 1.33 (0.69-2.55) | 0.92 (0.51-1.64) | 0.93 (0.38-2.24) | 1.00 (0.34-2.91) | 1.05 (0.32-3.44) |
| Bifenthrin (continuous) | 40 | 1.02 (0.86-1.22) | 1.07 (0.88-1.22) | 1.17 (0.79-1.77) | 1.16 (0.75-1.83) | 1.33 (1.04-1.71) | 1.45 (1.04-1.97) |
| Bifenthrin | |||||||
| <0.5 | 24 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.5 | 16 | 1.88 (1.01-3.47) | 2.04 (1.11-3.74) | 1.02 (0.57-1.67) | 0.99 (0.38-2.58) | 6.00 (1.73-20.81) | 10.97 (1.85-65.11) |
| Permethrin (continuous) | 40 | 1.02 (0.99-1.05) | 1.02 (0.97-1.08) | 0.97 (0.91-1.09) | o.97 (0.91-1.57) | 1.05 (1.02-1.08) | 1.05 (1.01-1.17) |
| Permethrin | |||||||
| <1.2 | 24 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.2 | 16 | 1.41 (0.72-2.74) | 1.26 (0.57-2.79) | 9.58 (0.22-1.53) | 0.58 (0.16-2.06) | 2.14 (0.71-6.49) | 1.52 (0.40-5.80) |
| Organophosphate | |||||||
| Methamidophos (continuous) | 49 | 1.03 (0.95-1.11) | 1.02 (0.95-1.11) | 0.92 (0.65-1.32) | 0.92 (0.64-1.34) | 1.07 (0.86-1.21) | 1.07 (0.97-1.33) |
| Methamidophos | |||||||
| <1.00 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.00-2.00 | 21 | 1.30 (0.89-1.91) | 1.32 (0.90-1.92) | 0.88 (0.63-1.23) | 0.88 (0.52-1.49) | 1.76 (0.92-3.39) | 1.90 (0.89-4.09) |
| ⩾2.00 | 14 | 1.70 (0.80-3.63) | 1.73 (0.81-3.76) | 0.76 (0.32-1.34) | 0.72 (0.24-1.65) | 1.92 (0.87-7.52) | 2.13 (0.72-11.01) |
| P for trend | .1785 | .1789 | .4634 | .6344 | .0768 | .0895 | |
| Chlorpyrifos (continuous) | 50 | 1.01 (1.00-1.04) | 1.01 (1.00-1.05) | 0.99 (0.92-1.08) | 0.98 (0.91-1.06) | 1.01 (0.98-1.03) | 1.01 (0.98-1.04) |
| Chlorpyrifos | |||||||
| <1.00 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.00-4.00 | 21 | 0.99 (0.66-1.49) | 1.02 (0.69-1.52) | 0.87 (0.62-1.24) | 0.83 (0.48-1.46) | 1.39 (0.71-2.72) | 1.50 (0.75-2.99) |
| ⩾4.00 | 15 | 0.98 (0.43-2.22) | 1.05 (0.47-2.34) | 0.71 (0.54-1.89) | 0.68 (0.42-2.15) | 1.23 (0.69-3.21) | 1.42 (0.54-3.52) |
| P for trend | .9629 | .9103 | .4598 | .5229 | .3218 | .2496 | |
| Profenofos (continuous) | 47 | 1.02 (0.91-1.14) | 1.01 (0.92-1.15) | 1.00 (0.56-1.116) | 1.00 (0.55-1.79) | 1.03 (0.82-1.28) | 1.03 (0.83-1.28) |
| Profenofos | |||||||
| <2.20 | 29 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾2.20 | 18 | 1.07 (0.57-2.00) | 1.11 (0.61-2.020 | 1.21 (0.68-2.15) | 1.25 (0.52-2.98) | 1.86 (0.59-5.80) | 2.04 (0.58-7.13) |
| Diazinon (continuous) | 48 | 1.23 (0.96-1.58) | 0.96 (0.91-1.55) | 1.05 (0.76-1.45) | 1.04 (0.75-1.46) | 0.47 (0.19-1.16) | 0.40 (0.15-1.09) |
| Diazinon | |||||||
| <0.7 | 20 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.7 | 28 | 1.01 (0.54-1.90) | 0.96 (0.52-1.80) | 1.00 (0.56-1.78) | 1.00 (0.40-2.50) | 0.44 (0.14-1.40) | 0.34 (0.09-1.33) |
| Parathion ethyl (continuous) | 49 | 1.00 (0.84-1.20) | 1.02 (0.86-1.20) | 0.97 (0.80=1.18) | 0.97 (0.79-1.24) | 1.04 (0.74-1.47) | 1.09 (0.72-1.65) |
| Parathion ethyl | |||||||
| <1.0 | 13 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.0-2.0 | 22 | 0.90 (0.62-1.29) | 0.85 (0.59-1.21) | 0.96 (0.68-1.34) | 0.96 (0.57-1.61) | 1.62 (0.85-3.08) | 1.52 (0.75-3.04) |
| ⩾2.0 | 14 | 0.81 (0.39-1.66) | 0.72 (0.31-1.57) | 0.76 (0.32-2.87) | 0.73 (0.29-4.30) | 1.98 (0.65-5.62) | 2.06 (0.58-6.83) |
| P for trend | .5741 | .3744 | .7921 | .8734 | .1233 | .2308 | |
| Dimethoate (continuous) | 47 | 1.00 (0.88-1.14) | 0.98 (0.86-1.12) | 1.01 (0.56-1.19) | 1.02 (0.86-1.21) | 1.15 (0.94-1.35) | 1.10 (0.91-1.55) |
| Dimethoate | |||||||
| <1.7 | 27 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.7 | 20 | 1.25 (0.58-2.71) | 1.14 (0.52-2.49) | 1.06 (0.56-2.00) | 1.17 (0.43-3.19) | 2.14 (0.74-6.20) | 1.64 (0.47-5.78) |
| Malathion (continuous) | 50 | 0.92 (0.76-1.04) | 0.94 (0.78-1.14) | 0.97 (0.80-1.18) | 0.97 (0.79-1.25) | 1.06 (0.82-1.37) | 1.09 (0.82-1.47) |
| Malathion | |||||||
| <1.30 | 14 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.30-3.20 | 21 | 0.82 (0.56-1.22) | 0.83 (0.57-1.21) | 1.03 (0.72-1.45) | 1.03 (0.60-1.76) | 1.40 (0.72-2.72) | 1.51 (0.73-3.14) |
| ⩾3.20 | 15 | 0.68 (0.31-1.48) | 0.70 (0.33-1.48) | 0.96 (0.68-2.48) | 0.95 (0.61-3.12) | 2.15 (0.65-4.57) | 3.21 (0.54-5.76) |
| P for trend | .3357 | .3394 | .8871 | .9193 | .3161 | .2632 | |
Case number of ALRI; *a Sex of the child, parental education, marital status, cooking fuel type, fed exclusively on breast milk, ethnicity, age of the child, and zonal community; *b Sex of the child, parental education, marital status, cooking fuel type, fed exclusively on breast milk, ethnicity, and zonal community. Bolded point estimate and confidence mean they are significant.
URI
Urinary concentration of p,p′-DDE, delta-HCH, beta-HCH, dieldrin, cyfluthrin, allethrin, fenvalerate, cypermethrin, lambda-cyhalothrin, bifenthrin, methamidophos, chlorpyrifos, profenofos, diazinon, parathion ethyl, dimethoate, malathion, and permethrin were not significantly associated with URI (Table 5). Bifenthrin (continuous) was associated with URI in children 3 or 4 YOA (1.33, 1.07-1.65), but the association of bifenthrin (⩾0.5 µg/L urine) with URI was inconclusive in these children (8.68; 2.26-33.42). Deltamethrin (continuous) was significantly associated with URI (PR = 1.02, 1.00-1.04). A trend (P = .0027) was observed with tertile deltamethrin and URI. The PRs for urinary concentrations of deltamethrin between 2.5 and 9.5 µg/L and for ⩾9.5 µg/L vrs <2.5 µg/L were 1.73 (1.22-2.45) and 2.98 (1.49-5.98), respectively (Table 5). Permethrin (continuous) was associated with URI in children 3 or 4 YOA (1.33, 1.07-1.65), but the association of permethrin (⩾1.2 µg/L urine) with URI was inconclusive
Table 5.
Association between the concentration of organochlorine, pyrethroid, and organophosphate insecticides in urine with URI risk in children below 5 YOA, the Offinso North Farm Health Study (ONFAHS) (n = 150).
| Pesticide level | URI | ||||||
|---|---|---|---|---|---|---|---|
| All ages | ⩽2 y | >2 y | |||||
| N* | Crude PR (95% CI) | Adjusted PR* a (95% CI) | Crude PR (95% CI) | Adjusted PR* b (95% CI) | Crude PR (95% CI) | Adjusted PR* a (95% CI) | |
| Organochlorines | |||||||
| PP DDE (continuous) | 63 | 1.00 (0.88-1.14) | 1.00 (0.88-1.14) | 0.99 (0.89-1.11) | 1.01 (0.90-1.13) | 1.07 (0.90-1.37) | 1.13 (0.86-1.25) |
| PP DDE | |||||||
| <1.70 | 33 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1-7-3.2 | 17 | 1.16 (0.85-1.58) | 1.16 (0.85-1.58) | 0.78 (0.57-1.07) | 0.87 (0.54-1.42) | 1.60 (1.02-2.51) | 1.54 (0.90-2.62) |
| ⩾3.2 | 13 | 1.35 (0.73-2.49) | 1.35 (0.73-2.49) | 1.02 (0.67-2.34) | 1.43 (0.76-3.03) | 2.14 (1.24-3.18) | 2.03 (0.75-5.42) |
| P for trend | .3600 | .3600 | .1026 | .5834 | .0461 | .1144 | |
| Delta-HCH (continuous) | 54 | 1.64 (0.96-2.82) | 1.64 (0.96-2.82) | 0.83 (0.30-2.47) | 0.41 (0.34-2.48) | 1.11 (0.47-2.63) | 1.12 (0.46-2.73) |
| Delta-HCH | |||||||
| <0.22 | 30 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.22 | 24 | 1.83 (1.03-3.23) | 1.23 (0.46-3.25) | 0.51 (0.16-1.63) | 0.67 (0.15-2.96) | 1.17 (0.40-3.40) | 1.14 (0.33-3.99) |
| Beta-HCH (continuous) | 52 | 0.94 (0.76-1.18) | 0.94 (0.76-1.18) | 0.86 (0.38-1.09) | 0.97 (0.63-1.45) | 0.84 (0.34-1.33) | 0.82 (0.52-1.37) |
| Beta-HCH | |||||||
| <0.22 | 29 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.22 | 23 | 1.46 (0.87-2.45) | 1.46 (0.87-2.45) | 0.75 (0.43-1.31) | 0.88 (0.36-2.19) | 1.46 (0.69-3.09) | 1.42 (0.58-3.48) |
| Dieldrin (continuous) | 60 | 1.03 (1.00-1.07) | 1.03 (1.00-1.07) | 0.99 (0.93-1.06) | 0.99 (0.92-1.97) | 1.02 (0.96-1.08) | 1.03 (0.95-1.09) |
| Dieldrin | |||||||
| <0.55 | 30 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 0.55-8.70 | 17 | 1.45 (0.99-2.13) | 1.45 (0.99-2.13) | 0.90 (0.63-1.28) | 0.94 (0.49-1.80) | 1.35 (0.80-2.27) | 1.29 (0.70-2.38) |
| ⩾8.70 | 13 | 2.10 (0.97-4.53) | 2.10 (0.97-4.53) | 0.78 (0.34-2.31) | 0.89 (0.34-3.56) | 3.16 (0.96-4.23) | 2.11 (0.75-4.32) |
| P for trend | .0789 | .0789 | .5564 | .8521 | .2643 | .4111 | |
| Pyrethroid | |||||||
| Cyfluthrin (continuous) | 60 | 1.00 (0.97-1.04) | 1.00 (0.97-1.04) | 1.00 (0.95-1.04) | 0.99 (0.94-1.04) | 0.96 (0.91-1.02) | 0.97 (0.91-1.03) |
| Cyfluthrin | |||||||
| <6.20 | 30 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 6.20-16.0 | 17 | 0.95 (0.68-1.33) | 0.95 (0.68-1.33) | 0.90 (0.67-1.21) | 0.94 (0.50-1.42) | 0.63 (0.39-1.06) | 0.70 (0.39-1.20) |
| ⩾16 | 13 | 0.90 (0.46-1.77) | 0.90 (0.46-1.77) | 0.89 (0.32-1.89) | 0.93 (0.41-2.01) | 0.48 (0.12-1.12) | 0.57 (0.11-2.56) |
| P for trend | .7718 | .7718 | .4607 | .5130 | .7120 | .1676 | |
| Deltamethrin (continuous) | 61 | 1.02 (1.01-1.03) | 1.02 (1.00-1.04) | 1.00 (0.98-1.03) | 1.00 (0.97-1.03) | 1.04 (1.01-1.07) | 1.04 (1.02-1.09) |
| Deltamethrin | |||||||
| <2.5 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2.5-9.5 | 16 | 1.79 (1.28) | 1.73 (1.22-2.45) | 1.24 (0.90-1.71) | 1.14 (0.67-1.96) | 2.07 (1.25-3.42) | 2.08 (1.09-3.96) |
| ⩾9.5 | 13 | 3.21 (1.63-6.30) | 2.98 (1.49-5.98) | 2.23 (0.78-2.89) | 2.17 (0.53-2.90) | 4.24 (1.57-4.38) | 4.26 (1.21-4.89) |
| P for trend | .0012 | .0027 | .1963 | .6276 | .0030 | .0201 | |
| Allethrin (continuous) | 51 | 1.08 (0.88-1.33) | 1.10 (0.91-1.34) | 1.18 (0.85-1.63) | 1.23 (0.86-1.78) | 1.03 (0.84-1.53) | 1.08 (0.78-1.50) |
| Allethrin | |||||||
| <0.90 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 0.90-1.6 | 16 | 1.04 (0.77-1.40) | 1.11 (0.88-1.40) | 1.22 (0.91-1.64) | 1.32 (0.70-2.49) | 0.91 (0.55-1.48) | 0.70 (0.37-1.33) |
| ⩾1.60 | 13 | 1.08 (0.59-1.96) | 1.23 (0.78-1.95) | 1.34 (0.89-2.01) | 1.48 (0.92-2.89) | 0.98 (0.67-2.10) | 0.86 (0.46-2.01) |
| P for trend | .8113 | .4881 | .1403 | .3823 | .6914 | .2706 | |
| Fenvalerate (continuous) | 54 | 0.88 (0.68-1.13) | 0.88 (0.70-1.11) | 0.99 (0.69-1.37) | 0.98 (0.69-1.39) | 0.94 (0.70-1.26) | 0.94 (0.69-1.29) |
| Fenvalerate | |||||||
| <0.30 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.30 | 22 | 1.00 (0.56-1.82) | 0.92 (0.52-1.63) | 1.05 (0.60-1.93) | 1.47 (0.39-5.88) | 2.25 (0.97-5.25) | 2.93 (0.97-8.81) |
| Cypermethrin (continuous) | 63 | 1.04 (1.01-1.07) | 1.04 (1.00-1.08) | 1.01 (0.96-1.07) | 1.92 (0.96-1.09) | 1.01 (0.95-1.07) | 1.02 (0.96-1.08) |
| Cypermethrin | |||||||
| <3.00 | 33 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 3.00-10.50 | 17 | 1.37 (0.99-1.93) | 1.32 (0.97-1.81) | 1.06 (0.81-1.38) | 1.31 (0.73-2.38) | 1.27 (0.74-2.17) | 1.36 (0.72-2.55) |
| ⩾10.50 | 13 | 1.92 (0.99-3.74) | 1.75 (0.94-3.27) | 0.93 (0.71-1.98) | 1.04 (0.56-2.67) | 2.03 (0.65-2.77) | 2.65 (0.63-2.04) |
| 0.0567 | 0.0852 | 0.6670 | 0.3648 | 0.3861 | 0.3423 | ||
| Lambda-cyhalothrin (continuous) | 57 | 0.99 (0.93-1.06) | 1.00 (0.94-1.07) | 1.01 (0.96-1.06) | 1.01 (0.94-1.08) | 1.02 (0.87-1.19) | 1.05 (0.88-1.24) |
| Lambda-cyhalothrin | |||||||
| <1.50 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.50 | 25 | 1.11 (0.66-1.87) | 1.08 (0.94-1.07) | 0.92 (0.59-1.42) | 0.96 (0.40-2.30) | 1.14 (0.46-2.73) | 1.40 (0.51-3.82) |
| Bifenthrin (continuous) | 53 | 1.01 (0.85-1.21) | 1.00 (0.83-1.21) | 1.10 (0.76-1.69) | 1.13 (0.74-1.74) | 1.35 (1.13-1.62) | 1.33 (1.07-1.65) |
| Bifenthrin | |||||||
| <0.5 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.5 | 21 | 1.57 (0.94-2.62) | 1.43 (0.85-2.39) | 1.12 (0.72-1.74) | 1.14 (0.41-3.21) | 6.50 (2.30-18.39) | 8.68 (2.25-33.42) |
| Permethrin (continuous) | 54 | 1.01 (0.96-1.04) | 1.01 (0.99-1.06) | 0.97 (0.91-1.04) | 0.92 (0.91-1.04) | 1.03 (1.01-1.06) | 1.64 (1.01-1.07) |
| Permethrin | |||||||
| <1.2 | 36 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.2 | 18 | 1.21 (0.61-2.38) | 1.07 (0.53-2.16) | 0.81 (0.38-1.71) | 1.14 (0.41-3.21) | 1.66 (0.67-4.11) | 8.68 (2.25-33.42) |
| Organophosphate | |||||||
| Methamidophos (continuous) | 61 | 1.02 (0.98-1.09) | 1.03 (0.96-1.10) | 0.93 (0.67-1.29) | 0.92 (0.65-1.31) | 0.99 (0.95-1.16) | 1.01 (0.84-1.21) |
| Methamidophos | |||||||
| <1.00 | 27 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.00-2.00 | 18 | 1.29 (0.95-1.76) | 1.29 (0.94-1.77) | 1.06 (0.84-1.33) | 1.08 (0.64-1.83) | 1.38 (0.83-2.27) | 1.40 (0.78-2.52) |
| ⩾2.00 | 16 | 1.67 (0.89-3.10) | 1.65 (0.87-3.12) | 1.21 (0.73-2.33) | 1.24 (0.70-2.98) | 2.04 (0.60-2.78) | 2.14 (0.57-3.35) |
| P for trend | .1145 | .1254 | .6263 | .2103 | .2556 | ||
| Chlorpyrifos (continuous) | 61 | 1.01 (0.99-1.02) | 1.01 (0.99-1.03) | 1.00 (0.95-1.06) | 0.98 (0.93-1.05) | 1.00 (0.98-1.03) | 1.01 (0.96-1.05) |
| Chlorpyrifos | |||||||
| <1.00 | 27 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.00-4.00 | 18 | 0.95 (0.68-1.33) | 0.97 (0.85-1.10) | 1.04 (0.81-1.33) | 1.05 (0.60-1.84) | 1.12 (0.66-1.90) | 1.11 (0.61-2.01) |
| ⩾4.00 | 16 | 0.91 (0.47-1.77) | 0.94 (0.72-1.22) | 0.89 (0.23-1.98) | 0.88 (0.21-2.03) | 1.43 (0.55-2.10) | 1.39 (0.52-2.89) |
| P for trend | .7898 | .8177 | .7481 | .8568 | .6713 | .7291 | |
| Profenofos (continuous) | 53 | 1.04 (0.93-1.16) | 1.03 (0.57-1.16) | 1.00 (0.85-1.16) | 0.99 (0.85-1.17) | 1.08 (0.92-1.26) | 1.06 (0.90-1.25) |
| Profenofos | |||||||
| <2.20 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾2.20 | 21 | 1.05 (0.57-1.94) | 1.05 (0.57-1.96) | 0.87 (0.23-1.12) | 0.92 (0.34-1.22) | 1.63 (0.58-4.60) | 1.71 (0.67-6.43) |
| Diazinon (continuous) | 54 | 1.07 (0.82-1.41) | 1.06 (0.80-1.32) | 1.08 (0.80-1.48) | 1.04 (0.76-1.43) | 0.62 (0.38-1.02) | 0.57 (0.30-1.05) |
| Diazinon | |||||||
| <0.7 | 33 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾0.7 | 21 | 0.82 (0.44-1.41) | 0.78 (0.42-1.44) | 0.87 (0.56-1.36) | 0.93 (0.37-2.34) | 1.73 (0.69-4.30) | 1.63 (0.58-4.60) |
| Parathion ethyl (continuous) | 61 | 0.98 (0.83-1.17) | 0.98 (0.82-1.17) | 1.01 (0.86-1.09) | 0.99 (0.82-1.12) | 1.26 (1.03-1.54) | 1.28 (1.01-1.63) |
| Parathion ethyl | |||||||
| <1.0 | 27 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.0-2.0 | 18 | 0.86 (0.64-1.16) | 0.83 (0.65-1.07) | 0.99 (0.76-1.28) | 0.98 (0.58-1.68) | 1.86 (1.07-3.23) | 1.73 (0.94-3.17) |
| ⩾2.0 | 16 | 0.74 (0.41-1.35) | 0.69 (0.42-1.15) | 1.05 (0.87-2.34) | 0.99 (0.62-2.76) | 2.78 (1.22-5.61) | 2.65 (0.96-4.08) |
| P for trend | .3407 | .9185 | .9385 | .9528 | .0181 | .0638 | |
| Dimethoate (continuous) | 54 | 1.02 (0.92-1.14) | 1.01 (0.90-1.12) | 1.03 (0.89-1.20) | 1.05 (0.90-1.23) | 1.06 (0.93-1.22) | 1.04 (0.90-1.21) |
| Dimethoate | |||||||
| <1.7 | 32 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ⩾1.7 | 22 | 1.42 (0.73-2.74) | 1.30 (0.67-2.53) | 1.17 (0.76-1.79) | 1.48 (0.55-3.96) | 1.61 (0.67-3.91) | 1.36 (0.46-3.98) |
| Malathion (continuous) | 61 | 0.95 (0.82-1.11) | 0.98 (0.83-1.14) | 0.96 (0.79-1.14) | 0.96 (0.79-1.16) | 0.92 (0.78-1.21) | 0.98 (0.78-1.24) |
| Malathion | |||||||
| <1.30 | 22 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.30-3.20 | 23 | 0.83 (0.60-1.15) | 0.84 (0.63-1.11) | 1.07 (0.84-1.38) | 1.02 (0.62-1.62) | 1.10 (0.64-1.87) | 1.14 (0.63-2.09) |
| ⩾3.20 | 16 | 0.69 (0.36-1.32) | 0.70 (0.40-1.23) | 0.94 (0.32-2.04) | 0.94 (0.15-1.94) | 2.31 (0.75- 3.98) | 2.35 (0.72-3.12) |
| P for trend | .2726 | .2682 | .5675 | .9375 | .7345 | .664 | |
Case number of URI; *a Sex of the child, parental education, marital status, cooking fuel type, fed exclusively on breast milk, ethnicity, age of the child, and zonal community; *b Sex of the child, parental education, marital status, cooking fuel type, fed exclusively on breast milk, ethnicity, and zonal community. Bolded point estimate and confidence mean they are significant.
Discussions
Main findings
This study explores the association of exposure of children under five YOA to trace concentrations of 4 organochlorine, 8 pyrethroid, and 7 organophosphate insecticide residues with respiratory infection in the Offinso North District of Ghana. The specific pesticides and their concentrations in the first void urine of the children are shown in Figure 1. The findings show that in this community, the proportion of children with ALRI was 22.1% and that with URI were 35.8%. Urinary residue analysis demonstrated significant exposure-response relation of urinary concentrations of p, p′-DDE with ALRI; association of delta-HCH, beta-HCH, and bifenthrin with ALRI. An exposure-response relation of urinary concentrations of deltamethrin with a respiratory infection was observed. These findings are important for many farm communities in developing countries, where children continued to be exposed to high levels of pesticides and related chemicals.
Methodological validity
Our study has several strengths. The data for this analysis were derived from a population-based cross-sectional study in the Offinso North District, Ghana. We measure direct exposure to 19 pesticides by their analysis in hexane extfacts of urine. Findings from these data sources suggested positive associations with ALRI/URI in some cases. Thus, information bias is not likely or is minimal in our study. Moreover, confounding factors controlled for in our analysis were based on their statistical significance (P < .05) with our outcomes of interest and were consistent with the literature.4,11,16-21 We received overwhelming support and interest for the project from the local communities, thus, increasing the participation rate and minimizing selection bias. Whilst acknowledging the relevance of the current study, a few limitations were also noted. A selection bias might have occurred in the way in which sampling was carried out in this study (ie, convenience sampling). In the community, farmers go to their farms incredibly early in the morning and it was not possible to reach out to all farmers. Thus, only those who delayed were included in this study and this could be a source of selection bias. It is important to note that the application of a probabilistic sampling strategy was not feasible in this study. It is also important to note that the current analysis was restricted to high exposed children and the findings cannot be generalized to all the children. Differential misclassification of ALRI was unlikely in the present study because participants and interviewers were not privileged to the laboratory results. Another concern in the present study is the lack of clinical diagnosis or confirmation of reported cases of respiratory infection. The definitions of ALRI/URI applied in this study were consistent with other similar studies in terms of the symptoms considered relevant,25,26 but the quality of the ascertainment of symptoms is perhaps not as good, as there was not clinical confirmation.
The cross-sectional design applied in the current study restricts our ability to establish any temporality. Nevertheless, an exposure-response relation between exposure to some pesticides and ALRI/URI was observed, suggesting plausible causal links. Besides, some residual confounding such as birth weight (⩽2500 g), non-exclusive breastfeeding, measles immunization, housing conditions, malnutrition, and ambient air pollution were not considered in the analysis. Mothers/guardians provided 1 urine sample per child, and it was not possible to determine within-child differences, which could have resulted in misclassification and an imprecise estimate of the regression parameter. Finally, some associations of urinary pesticide residue with URI/ALRI lacks the power to detect any associations and will increase the margin of error; and thus, compromising the precision of the parameter estimates.
Comparison of our findings with previous studies
Children are more susceptible to pesticide exposure because of their mouthing behavior, eating, drink, and breathing pattern, and their lack of height which brings them close to contaminated sites/surfaces on the ground. 6 Our systematic search of the literature did not retrieve any study on the relation between organophosphate/pyrethroids and URI/ALRI, but we identified 15 studies reporting on a wide range of organochlorines and URI (n = 4), ALRI (n = 13), general infection (n = 1), and chest infections (n = 1). Findings from these studies were largely inconsistent. For instance, in Sabadell (Spain), Sunyer et al 17 measured organochlorine levels in maternal serum in the first trimester. Maternal levels of p, p-DDE, p, p-DDT, PCBs 28, 118, 138, 153, and 180, hexachlorobenzene, and β-hexachlorocyclohexane. DDE was the only organochlorine compound that was significantly associated with recurrent ALRI (relative risk (RR) 2.40, 95% confidence interval 1.19-4.83), ALRI at 6 months (RR = 1.68; CI = 1.06-2.66), and ALRI at 14 months (1.52, 1.05-2.21). In a follow-up study in a much bigger population consisting of 1455 mother-child pairs from 3 regions in Spain (Gipuzkoa, Sabadell, and Valencia), prenatal DDE concentrations were associated with ALRI risk (1.11, 1.00-1.22). Adjusting for PCBs and HCB did not materially change the results. There was an exposure-response association of DDE with the risk of ALRI. 27 These observations were confirmed in Japanese children 28 and Dutch PSAC. 29 However, studies among PSAC in Sweden, 14 in Mexico, 30 in Canada,31,32 in Japan, 33 in Costa Rica, 21 and the USA 33 did not confirm these associations. A respiratory infection has been reported among infants exposed to high levels of HCB and DDE combined. 27 A study by Okada et al 20 in Sapporo, Japan, failed to establish any association between prenatal perfluorooctanoic acid (PFOA)/perfluorooctane sulfonate (PFOS) levels and otitis media in children. Previous studies have evaluated a wide range of Persistent Organic Pollutants (POPs) including, PCB congeners, DDE, HCB, and HCHs. In environmental health studies, exposure to POPs was determined by sampling maternal blood or breast milk during pregnancy, or sampling of maternal diet or children’s serum.15,28,29 Breast milk sampled after delivery is used as a marker of perinatal exposure. Other studies 30 used maternal blood serum and diet as markers of prenatal exposure and children’s serum as indicators of post-natal exposure. The data source for ALRI/URI includes the use of questionnaires9 -12,14,15,25,26,29 -32 or medical records.26,33 Due to cultural beliefs and community perception related to blood sampling, the current study sampled urine. The experiences of ALRI/URI of PSAC, 2 weeks before the study were reported by parents. We collected data on direct exposure to organochlorines, pyrethroid, and organophosphate residues in urine. Like previous studies,27-29 we noted a consistent exposure-response relationship between levels of exposure p, p′-DDE, and the risk for ALRI. None of the organochlorine POPs considered in our study was found to be associated with URI, a finding consistent with those of Rogan et al 30 and Dallaire et al. 14 We also reported on a wide range of urinary pyrethroids/organophosphate residues, and we noted exposure-response relations for deltamethrin with ALRI/URI. We also observed a significant positive association of bifenthrin with ALRI. These findings have not been reported previously, but in our earlier study among 300 vegetable farmers, we observed an exposure-response relationship of beta-HCH with wheezing.
We further tested for the first time the association of pyrethroid and organophosphate insecticides with a respiratory infection. Our study further suggested that delta-and beta-HCHs at concentrations >0.22 µg/L of urine or bifenthrin concentration of >0.5 µg/L in urine increased the risk of ALRI. Deltamethrin concentration above 2.5 µg/L in urine increases the risk of respiratory infection in an exposure-response manner. Our findings have important public health implications for children living in farm communities in developing countries given the fact that ALRI (particularly, pneumonia) is the number one killer of children under 5 YOA worldwide 34 and the fact that these children will continuously be exposed to high levels of pesticides because of the increasing demand for pesticides to boost vegetable production. 8 Our findings again suggested the need for public health intervention measures that could minimize the use and exposure to pesticides to have a marked public health impact on children living in farming communities in developing countries. Governments in these countries should demonstrate a commitment to prudent measures that ensures efficient utilization and management of chemical pesticides.
Conclusions
The present study supports the hypothesis that exposure to chemical pesticides is associated with respiratory infections in children under 5 YOA. Specifically, we observed an increased risk of p,p′-DDE with ALRI (P-for trend = .0297) and this was noted in children, 3, or 4 YOA (P-for trend = .0404). Delta-HCH and beta-HCH had a significant association with ALRI but not URI. The risk of ALRI increased with deltamethrin levels (P-for trend = .0011) and this was also observed in children, 3, or 4 YOA. Bifenthrin (>0.5 µg/L) was associated with ALRI and URI.
Acknowledgments
We are grateful to the Chiefs and elders of the Offinso North District, agriculture extension officers in the communities, the agriculture officer-in-charge, and the communities at large for their support of this project.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: RQ: Conceptualization, RQ, FAA, ODY: Methodology, RQ, SI: Formal analysis, All: Resources, RQ: Data curation, RQ, EA: Writing-original draft, All: Writing review & editing, SI: Visualization, RQ: Supervision, project administration.
Availability of Data and Materials: We are still publishing from the dataset that supported these findings. Nevertheless, the data is with the corresponding author and will be made available upon request.
Ethics Approval and Consent to Participate: Informed consent was obtained from parents on behalf of the children. Participants were free to participate with or without reservation. Consent to publish this data in any form was obtained from parents/guidance of the children.
ORCID iDs: David Kofi Essumang  https://orcid.org/0000-0002-0589-7895
https://orcid.org/0000-0002-0589-7895
Reginald Quansah  https://orcid.org/0000-0002-7318-4192
https://orcid.org/0000-0002-7318-4192
References
- 1. Goodarzi E, Sohrabivafa M, Darvishi I, Naemi H, Khazaei Z. Epidemiology of mortality induced by acute respiratory infections in infants and children under the age of 5 years and its relationship with the Human Development Index in Asia: an updated ecological study. J Public Health. 2021;29:1047-1054. [Google Scholar]
- 2. GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Infect Dis. 2018;18:1191-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seidu AA, Ameyaw EK, Ahinkorah BO, Baatiema L, Appiah F. Ecological zone and symptoms of acute respiratory infection among children under five in Ghana: 1993-2014. SSM Popul Health. 2019;8:100414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ramani VK, Pattankar J, Puttahonnappa SK. Acute respiratory infections among under-five age group children at urban slums of Gulbarga City: a longitudinal study. J Clin Diagn Res. 2016;10:LC08-LC13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med. 2018;18:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Black K, Shalat SL, Freeman NCG, Jimenez M, Donnelly KC, Calvin JA. Children’s mouthing and food-handling behavior in an agricultural community on the US/Mexico border. J Expo Anal Environ Epidemiol. 2005;15:244-251. [DOI] [PubMed] [Google Scholar]
- 7. Winans B, Humble MC, Lawrence BP. Environmental toxicants and the developing immune system: a missing link in the global battle against infectious disease? Reprod Toxicol. 2011;31:327-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dinham B. Growing vegetables in developing countries for local urban populations and export markets: problems confronting small-scale producers. Pest Management Science. 2003;59:575-582. [DOI] [PubMed] [Google Scholar]
- 9. Bruce-Vanderpuije P, Megson D, Reiner EJ, Bradley L, Adu-Kumi S, Gardella JA, Jr. The state of POPs in Ghana- A review on persistent organic pollutants: Environmental and human exposure. Environmental Pollution. 2019;245:331-342. [DOI] [PubMed] [Google Scholar]
- 10. Darko G, Acquaah SO. Levels of organochlorine pesticides residues in dairy products in Kumasi, Ghana. Chemosphere. 2008;71(2):294-298. [DOI] [PubMed] [Google Scholar]
- 11. Quansah R, Bend JR, Abdul-Rahaman A, Armah FA, Luginaah I, Essumang DK, Iddi S, Chevrier J, Cobbina SJ, Nketiah-Amponsah E, Adu-Kumi S, Darko G, Afful S. Associations between pesticide use and respiratory symptoms: a cross-sectional study in southern Ghana. Environmental Research. 2016;150:245–254. [DOI] [PubMed] [Google Scholar]
- 12. Niu C, Liu Y, Wang J, Liu Y, Zhang S, Zhang Y, Zhang L, Zhao D, Liu F, Chao L, Wang X, Zhang C, Song G, Zhang Z, Li Y, Yan Z, Wen Y, Ge Y, Zang Z, Feng W, Zhang H, Tao L, Nakyeyune R, Shen Y, Shao Y, Guo X, Miles T, Yang A, Liu F, Wang G. Risk factors for esophageal squamous cell carcinoma and its histological precursor lesions in China: a multicenter cross-sectional study. BMC Cancer. 2021;21(1):1034. doi: 10.1186/s12885-021-08764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karmaus W, Kuehr J, Kruse H. Infections and atopic disorders in childhood and organochlorine exposure. Arch Environ Health. 2001;56:485-492. [DOI] [PubMed] [Google Scholar]
- 14. Dallaire F, Dewailly E, Muckle G, et al. Acute infections and environmental exposure to organochlorines in Inuit infants from Nunavik. Environ Health Perspect. 2004;112:1359-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glynn A, Thuvander A, Aune M, et al. Immune cell counts and risks of respiratory infections among infants exposed pre- and postnatally to organochlorine compounds: a prospective study. Environ Health. 2008;7:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gascon M, Vrijheid M, Martínez D, et al. Prenatal exposure to dichlorodiphenyldichloroethylene and infant lower respiratory tract infections and wheeze. Eur Respir J. 2012;39:1188-1196. [DOI] [PubMed] [Google Scholar]
- 17. Sunyer J, Garcia-Esteban R, Alvarez M, et al. DDE in mothers’ blood during pregnancy and lower respiratory tract infections in their infants. Epidemiology. 2010;21:729-735. [DOI] [PubMed] [Google Scholar]
- 18. Cupul-Uicab LA, Terrazas-Medina EA, Hernández-ávila M, Longnecker MP. Prenatal exposure to p,p′-DDE and p,p′-DDT in relation to lower respiratory tract infections in boys from a highly exposed area of Mexico. Environ Res. 2014;132:19-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Miyashita C, Sasaki S, Saijo Y, et al. Effects of prenatal exposure to dioxin-like compounds on allergies and infections during infancy. Environ Res. 2011;111:551-558. [DOI] [PubMed] [Google Scholar]
- 20. Okada E, Sasaki S, Saijo Y, et al. Prenatal exposure to perfluorinated chemicals and relationship with allergies and infectious diseases in infants. Environ Res. 2012;112:118-125. [DOI] [PubMed] [Google Scholar]
- 21. Mora AM, Hoppin JA, Córdoba L, et al. Prenatal pesticide exposure and respiratory health outcomes in the first year of life: results from the infants’ Environmental Health (ISA) study. Int J Hyg Environ Health. 2020;225:113474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ntow WJ. Organochlorine pesticides in water, sediment, crops, and human fluids in a farming community in Ghana. Arch Environ Contam Toxicol. 2001;40:557-563. [DOI] [PubMed] [Google Scholar]
- 23. Ntow WJ, Gijzen HJ, Kelderman P, Drechsel P. Farmer perceptions and pesticide use practices in vegetable production in Ghana. Pest Manag Sci. 2006;62:356-365. [DOI] [PubMed] [Google Scholar]
- 24. Quansah R, Bend JR, Armah FA, et al. Respiratory and non-respiratory symptoms associated with pesticide management practices among farmers in Ghana’s most important vegetable hub. Environ Monit Assess. 2019;191:716. [DOI] [PubMed] [Google Scholar]
- 25. Bautista LE, Correa A, Baumgartner J, Breysse P, Matanoski GM. Indoor charcoal smoke and acute respiratory infections in young children in the Dominican Republic. Am J Epidemiol. 2009;169:572-580. [DOI] [PubMed] [Google Scholar]
- 26. Mishra V. Indoor air pollution from biomass combustion and acute respiratory illness in preschool age children in Zimbabwe. Int J Epidemiol. 2003;32:847-853. [DOI] [PubMed] [Google Scholar]
- 27. Gascon M, Vrijheid M, Martínez D, et al. Infancia y Medio Ambiente Environment and Childhood Project. Prenatal exposure to dichlorodiphenyldichloroethylene and infant lower respiratory tract infections and wheeze. Eur Respir J. 2012. May;39(5):1188-96. doi: 10.1183/09031936.00011711. [DOI] [PubMed] [Google Scholar]
- 28. Dewailly E, Ayotte P, Bruneau S, Gingras S, Belles-Isles M, Roy R. Susceptibility to infections and immune status in Inuit infants exposed to organochlorines. Environ Health Perspect. 2000;108:205-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. ten Tusscher GW, Steerenberg PA, van Loveren H, et al. Persistent hematologic and immunologic disturbances in 8-year-old Dutch children associated with perinatal dioxin exposure. Environ Health Perspect. 2003;111:1519-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rogan WJ, Gladen BC, McKinney JD, et al. Polychlorinated biphenyls (PCBs) and dichlorodiphenyl dichloroethene (DDE) in human milk: effects on growth, morbidity, and duration of lactation. Am J Public Health. 1987;77:1294-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jusko TA, Klebanoff MA, Brock JW, Longnecker MP. In-utero exposure to dichlorodiphenyltrichloroethane and cognitive development among infants and school-aged children. Epidemiology. 2012;23:689-698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sunyer J, Antó JM, Plana E, et al. Maternal atopy and changes in parity. Clin Exp Allergy. 2005;35:1028-1032. [DOI] [PubMed] [Google Scholar]
- 33. Stølevik SB, Nygaard UC, Namork E, et al. Prenatal exposure to polychlorinated biphenyls and dioxins is associated with increased risk of wheeze and infections in infants. Food Chem Toxicol. 2011;49:1843-1848. [DOI] [PubMed] [Google Scholar]
- 34. Institute for Health Metrics and Evaluation. Pushing the Pace: Progress and Challenges in Fighting Childhood Pneumonia. IHME; 2014. [Google Scholar]


