Abstract
This study aims to analyze the prevalence and likelihood of overweight, obesity, and elevated body mass index (BMI) among sexual minority men (i.e., men who have sex with men [MSM], men who have sex with men and women [MSMW], and all sexual minority men), using men who have sex with women (MSW) as the reference group. Studies reporting mean BMIs or prevalence or likelihood of obesity, overweight, or elevated BMI categorized by sexual orientation were included. Data were pooled and analyzed to report mean differences (MDs) of BMIs, prevalence rates, odds ratios (ORs), and their respective 95% confidence intervals (CIs). Forty-three studies were included, with a median of 26,507 participants (median 3.37% sexual minority men). The respective mean overweight, obesity, and elevated BMI prevalence rates among MSM (36%, 23%, and 39%) and MSMW (33%, 27%, and 47%) were lower than those of MSW (44%, 26%, and 55%). This finding was consistent with a significantly lower BMI (MD −1.50 [−1.93, −1.08] kg/m2) and a decreased likelihood of overweight (OR 0.75 [0.64, 0.88]) and obesity (OR 0.84 [0.78, 0.90]). Sexual minority men present with a lower prevalence and likelihood of obesity and overweight than their heterosexual counterparts. The obesity paradox—a sustained catabolic state presenting with lower BMI—is a feasible explanation for this phenomenon, although further research exploring paradoxical cardiovascular findings is granted.
Keywords: obesity, overweight, elevated BMI, men who have sex with men, sexual minorities, prevalence, obesity paradox, meta-analysis
Introduction
Obesity is a complex, multidimensional, metabolic disease associated with serious cardiovascular diseases (CVDs), including hypertension, dyslipidemias, and type 2 diabetes mellitus (Flegal et al., 2013; Singh-Manoux et al., 2018). CVD continues to be the leading cause of morbidity and mortality worldwide (Caceres et al., 2020). The body mass index (BMI) is the weight-for-height index most widely used to assess weight status in clinical and epidemiological settings. Despite a better understanding of obesity pathogenesis and management, the prevalence rate of elevated BMI (≥25.0 kg/m2, i.e., combined overweight and obesity) has shown an upward global trend (Dai et al., 2020). Since 1975, worldwide prevalence rates of elevated BMI have tripled; and estimates from 2016 show that 39% of adults had an elevated BMI while 13% were obese (BMI ≥30.0 kg/m2; WHO, 2020). In the United States, the crude prevalence rate of obesity among adults was estimated at 39.8%, an increase by 9.1% from 1999 (Hales et al., 2017).
Obesity prevalence rates peak between 40 and 60 years of age. Adult women in the United States are more likely to be obese than men (Hales et al., 2017; Purnell, 2000). Worldwide, men present with higher mortality rates and more disability-adjusted life years (DALYs) associated with elevated BMI (Dai et al., 2020). Data from the United States indicate that since 1960, the prevalence rate of overweight (BMI ≥25.0 and <30.0 kg/m2) slowly decreased, while the prevalence of obesity and severe obesity (BMI ≥40.0 kg/m2) increased for both genders, more noticeably for men (Fryar et al., 2018).
Among men, a handful of studies have addressed the issue of weight disparities by sexual orientation. Caceres et al. (2017) reviewed 15 studies reporting weight disparities among sexual minority men. The review identified two-thirds of the studies reporting a decreased likelihood of elevated BMI among sexual minority men compared with their heterosexual counterparts (Caceres et al., 2017). The reasons for these disparities can be framed within the Minority Stress Theory, which posits that sexual minority health disparities result in large part from life of stressors induced by nonconformity to a heteronormative environment (Meyer, 2003). These life stressors include general life events (e.g., financial adversity), structural and institutional factors (e.g., laws, policies, and social norms), interpersonal factors (e.g., discrimination, stigma, and violence), and intrapersonal factors (e.g., self-stigma and concealment; Meyer, 2003). Flentje et al. (2020) conducted a systematic review that identified three studies associating 13 minority stressors with changes in the BMI in 31% of these comparisons. Changes in cortisol levels have been posited as a plausible biobehavioral mechanism linking life stressors to poor cardiovascular outcomes (Huebner et al., 2021). The impact of life stressors on biopsychosocial drivers of CVD in general—and obesity in particular—is such that the American Heart Association incorporated them in the conceptual model for cardiovascular health disparities among sexual minority adults (Caceres et al., 2020), and the disparities in obesity prevalence and CVD outcomes are subject of a growing research agenda (cf. VanKim & Laska, 2021).
Sexual minority men seem to present with an overall decreased prevalence of elevated BMI (VanKim & Laska, 2021), which does not necessarily translate into a healthier cardiometabolic status. The obesity paradox in CVD asserts that overweight or class I obese (BMI ≥30.0 but <35.0 kg/m2) persons may have better CVD outcomes compared with normal-weight (18.5 ≤ BMI <25.0 kg/m2) or underweight (BMI <18.5 kg/m2) persons (Antonopoulos & Tousoulis, 2017; Carbone et al., 2019). The poor prognosis for individuals with normal or underweight may be a result of a progressive and sustained catabolic state, with weight loss resulting from disproportionate loss of lean mass (Elagizi et al., 2018). Among sexual minority men, cardiovascular outcomes often associated with obesity—such as hypertension, diabetes, and dyslipidemias (Caceres et al., 2017; López Castillo et al., 2021)—are more prevalent. A first explanation of this paradoxical phenomenon is consistent with life stressors. Sexual minority men report an increased drive for muscularity (Calzo et al., 2013) and more weight-related stigma (Fulton & Srinivasan, 2021; Puhl et al., 2019), which partially explain motivations and behaviors to actively avoid an elevated BMI. A second explanation involves a higher prevalence of HIV infection among sexual minority men. Man-to-man sexual contact continues to be the dominant HIV transmission mechanism (81% of new infections in 2018), with an all-time-high linkage to and retention in antiretroviral therapy (ART; 65% and 49%, respectively) (Centers for Disease Control and Prevention [CDC], 2022). Approximately half of people living with HIV will develop central fat accumulation soon after starting ART (Grunfeld et al., 2010) and both HIV infection and ART are associated with significantly increased BMI, waist circumference, overweight and obesity, and prevalence of abdominal obesity (Nduka et al., 2016; Sarkar & Brown, 2000; Shlay et al., 2007). Cortisol has also been described as a mediator of obesity among people living with HIV receiving ART and developing this Cushing syndrome–like reaction (Stanley & Grinspoon, 2012).
Although previous descriptive work reported disparate prevalence rates of overweight and obesity among sexual minorities (Caceres et al., 2017; Flentje et al., 2020), to date, these disparities have not been quantified using meta-analytic techniques. Given the importance of accurate estimates to advance efforts preventing CVD in populations at increased risk, such as sexual minority men, the current meta-analysis aims to summarize the prevalence and likelihood of overweight, obesity, and elevated BMI among sexual minority men, using men who have sex with women (MSW) as the reference group.
Method
Protocol and Registration
The full keyword search and study research questions were prospectively published in the International Prospective Register of Systematic Reviews (PROSPERO; University of York, United Kingdom; Registration CRD42020213163). The Institutional Review Board (IRB) at the University of Central Florida reviewed the PROSPERO study protocol and determined it did not meet the definition of research involving human subjects and, thus, IRB review and approval were not required (STUDY00002927).
Data Sources and Keyword Search
The keyword search was created, reviewed, and conducted in the following four databases using the native search interface from their date of inception until December 2020: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, the Web of Science, and PubMed. Keyword variants for the MSM population ([[gay OR bisexual OR homosexual OR heterosexual] AND men] OR [“men who have sex with men” OR MSM]) and for the outcome of interest the keywords “obesity” and “overweight” were used. The reference lists of the selected articles were also manually searched for additional relevant records.
Inclusion Criteria
Only original research articles in peer-reviewed publications were included for analysis. Besides this criterion, the search was not restricted by dates, language, geographic area, participants’ age, or analytic methods as long as the studies complied with the inclusion criteria. Abstracts from the records obtained were reviewed for relevance and included for data extraction if (a) the article analyzed primary or secondary data sources; (b) the population studied included sexual minority men (either as a single, aggregated category or categorized as men who have sex with men [MSM] and/or men who have sex with men and women [MSMW] as separate categories) defined by either behavior, identity, attraction, or a combination of these; (c) the article reported analyses or subanalyses of obesity, overweight, or elevated BMI specific to sexual minority men; (d) the article included a quantifiable population of MSW, defined by either behavior, identity, attraction, or a combination of these, that could be used as a reference group; and (d) regardless of statistical significance, the article reported at least one measure of prevalence, aggregated descriptive measures of obesity, overweight, or elevated BMI (including, but not limited to BMI or abdominal circumference), or inverse variance measures (i.e., odds ratio [OR], prevalence ratio [PR], or their respective regression coefficients [β] in the case of generalized linear regression models). Because nonbinary and/or transgender populations are both small and diverse, records focusing exclusively on these populations were excluded to reduce the risk of misclassification and to avoid underpowered comparisons.
Abstraction Process
Articles were reviewed, extracted, synthesized, and study quality was assessed by four reviewers (SC, DV, NN, and IB). Every record was independently reviewed by at least two reviewers to calculate agreement metrics (i.e., Holsti’s percentage concordance and Cohen’s kappa; Cohen, 1968; Holsti, 1969). Disagreements were resolved by a fifth reviewer (HLC) in consultation with the original reviewers.
When reported, demographic measures of the studies’ samples (including, but not limited to, proportion of men and women included, sampling methods, data source, and distribution by age, race/ethnicity, geographic location, and sexual orientation) were extracted for context to understand the role of potential biases and confounders. The keyword search, data abstraction, and study inclusion followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Liberati et al., 2009).
Measures
Sexual Orientation
Self-reported sexual identity and attraction (whether romantic or sexual) often—although not always—align with self-reported sexual behavior (Wolff et al., 2017). Thus, the sexual minority populations to be included (i.e., sexual minority men, MSM, and/or MSMW) were defined preferably through behavioral measures of sexual orientation and, when other measures of sexual orientation were available (i.e., self-reported sexual identity, sexual or romantic attraction, or a combination of these), these were included and assumed to be mostly concordant.
Overweight, Obesity, and Elevated BMI
The authors extracted data from studies reporting mean (standard deviation [SD]) values for BMI (in kg/m2) or mean abdominal circumference (in cm). Prevalence measures of overweight, obesity, and elevated BMI were extracted from self-reported lifetime diagnosis of overweight or obesity (yes/no), crude and/or adjusted measures of prevalence, and inverse variance measures. All studies used the standard calculation for BMI (weight in kg/[height in m]2) and the agreed-upon categories for overweight (BMI ≥25.0 and <30.0 kg/m2), obesity (BMI ≥30.0 kg/m2), severe obesity (BMI ≥40.0 kg/m2), and elevated BMI (≥25.0 kg/m2, i.e., combined overweight and obesity).
Bias Assessment
Recommendations for bias assessment in observational studies (Hammer et al., 2009) were followed by using a bias assessment tool evaluating the risk of selection, information, and response bias in each article included. In addition, the risk of confounding by four factors (namely, age, education, income, and HIV serostatus) was assessed for each study.
Statistical Analyses
Three, separate meta-analyses were conducted for studies reporting crude or adjusted mean BMI; crude or adjusted prevalence rates of overweight, obesity, or elevated BMI; and crude or adjusted measures of inverse variance. Mean BMIs were pooled and compared using mean differences (MD) with their respective 95% CIs. Prevalence and inverse variance measures were pooled, and weights were assigned to each study using the reciprocal of their variance. All meta-analyses were conducted assuming random effects. As age can operate as a confounder, we conducted an exploratory meta-regression of prevalence and inverse variance measures on age for those studies reporting mean age.
Forest plots were generated by Review Manager v. 5.4.1 (The Cochrane Collaboration; Copenhagen, Denmark) and are presented as supplementary figures following the best practices for forest plots (Higgins et al., 2011). Meta-regressions of prevalence estimates by age were generated with Comprehensive Meta-Analyses v. 3.0 (Biostat, Inc.; Englewood, NJ). Heterogeneity for study comparisons was determined through I2 (Lin & Chu, 2018), and funnel plot analyses were conducted to assess for study heterogeneity, reporting bias, and chance (Sterne et al., 2011).
Results
The keyword and manual search strategy identified 325 unique records. Titles and abstracts independently screened by four reviewers were found with moderate Holsti’s concordance (r = .750) and moderate Cohen’s κ (mean κ = .513; range .445–.578). After resolution of disagreements through discussion and consensus, the full text of 111 records was reviewed for compliance with inclusion criteria. Sixty-eight studies were excluded, mostly due to lack of specific subanalyses of sexual minority men (n = 27) or lack of original research with primary or secondary data sources (n = 17). Supplementary Figure S1 summarizes the PRISMA sequence for screening steps, concluding with the inclusion of 43 studies for meta-analytic comparisons.
The 43 studies included (Table 1) were published between 1996 and 2020; and almost half of them (n = 21) were published within the last five years of that date range (i.e., 2016-2020). Despite the lack of language restriction in this search, all studies were published in English and used secondary data from country- or state-level surveys. Most studies (n = 38) were conducted in the United States, two in the United Kingdom (Calzo et al., 2018; Conner et al., 2004), one each in Canada (Brennan et al., 2010) and Denmark (Frisch & Zdravkovic, 2010), and one multinational study across Brazil, Mexico, and the United States (Nyitray et al., 2019). Twenty-five of the 38 studies conducted in the United States were nationally representative; 12 were conducted at the state level (7 in California, 2 in Washington, and 1 each in Massachusetts, Minnesota, and Oregon), and one at an unspecified northeastern university college. All studies had an observational design and analyzed cross-sectional, single-timepoint data.
Table 1.
Characteristics of the 43 Studies Included in the Meta-Analysis.
| Author(s), year | Study site | Data source | Objective | Measure of obesity | Measure of sexual orientation | Gender | Male participants a | ||
|---|---|---|---|---|---|---|---|---|---|
| Sexual orientation | Age (y) | Race/ethnicity | |||||||
| Austin et al., 2009 b | United States | 1998–2005 GUTS | To describe how sexual orientation–related weight-status patterns may vary by gender and age from early through middle to late adolescence. | BMI calculated from self-reported height and weight.
c
Reported as likelihood of elevated BMI. d |
Combined sexual identity and attraction. Reported as H, mostly H, B, G, or not sure. |
22,161 M 34,829 W |
93.85% H 4.26% mostly H 0.51% B 1.30% G |
12–14: 24.83% 15–16: 23.00% 17–18: 20.44% 19–20: 15.99% 21–23: 10.60% |
NR |
| Azagba et al., 2019 | United States | 2014–2017 BRFSS | To examine whether overweightness and obesity vary by sexual minority subgroup. | BMI calculated from self-reported height and weight. Reported as likelihood of obesity f and elevated BMI. d |
Sexual identity. Reported as H, G, B, and other/don’t know/not sure. |
346,681 M 369,928 W |
Total
g
48.5% H 60.9% LG 35.4% B 41.6% other |
Total
g
18–24: 11.86% 25–34:15.80% 35–44: 16.04% 45–54: 17.65% 55–64:17.64% ≥65: 20.98% |
Total
g
White: 65.17% H/L: 15.20% AA/B: 11.52% Others: 8.11% |
| Bankoff et al., 2016 | United States | Knowledge Networks-GfK Research Panel | To examine the associations between sexual orientation, BMI, disordered eating behaviors, and food addiction in a sample of male veterans. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI. |
Sexual identity. Reported at H and sexual minority (G, B, and other). |
642 M | 96.26% H 3.74% sexual minority |
X– (SD) 64.11 (11.20) min 22 max 89 |
White: 85.5% |
| Beach et al., 2018 | United States | 2014 BRFSS | To compare the prevalence of self-reported diabetes and diabetes risk factors among adult sexual minority and heterosexual populations. | BMI calculated from self-reported data. Reported as prevalence of overweight e and obesity. f |
Sexual identity. Reported as H, G, and B. |
60,689 M 85,939 W |
97.13% H 1.75%G 1.12% B |
18–29: 10.41% 30–39: 10.32% 40–49: 13.84% 50–64: 33.76% ≥65: 31.03% Missing 0.64% |
White: 81.94% AA/B: 5.85% H/L: 3.45% Others: 7.27% Missing: 1.49% |
| Blosnich et al., 2014 | 10–state sample in the United States | 2010 BRFSS | To compare health indicators by gender and sexual orientation statuses. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI and prevalence and likelihood of overweight e and obesity. f |
Sexual identity. Reported as H, G, and B. |
34,124 M | 97.40% H 1.92% G 0.68% B |
H X–(SD) 45.1 (0.19) G X– (SD) 42.7 (1.22) B X–(SD) 41.9 (2.08) |
White: 79.85% AA/B: 2.24% H/L: 9.82% Others: 7.02% |
| Blosnich et al., 2016 | United States | 2003–2011 MEPS | To examine associations between sexual minority status and medical conditions. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of overweight, e obesity, f and elevated BMI. d |
Partnership or marriage. Reported as same- and opposite-sex partnerships or marriages. |
496 M 492 W |
50.00% opposite-sex partnered 50.00% same-sex partnered |
NR | NR |
| Boehmer et al., 2012 | California, United States | 2001, 2003, & 2005 CHIS | To identify differences by sexual orientation in health behaviors of cancer survivors. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI and prevalence and likelihood of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
3,690 M 7,252 W |
94.20% H 4.39% G 1.41% B |
H X– (SD) 59.9 (0.3) GX– (SD) 49.8 (1.2) B X– (SD) 57.4 (1.5) |
White: 84.36% H/L: 6.61% Asian: 3.01% AA/B: 2.90% Other: 3.06 |
| Boehmer et al., 2014 | California, United States | 2001, 2003, 2005, & 2007 CHIS | To estimate the prevalence of health conditions among young, middle age, and older age groups to examine sexual orientation differences while stratifying by gender. | BMI calculated from self-reported height and weight. Reported as prevalence of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
66,109 M 93,242 W |
95.78% H 3.06% G 1.16% B |
20–39: 46.39% 40–59: 41.25% ≥60: 12.37% |
White: 50.51% H/L: 26.14% Asian: 11.69% AA/B: 5.20% Other: 6.07% |
| Brennan et al., 2010 | Canada | 2003 CCHS | To determine whether health status and health risk behaviors of Canadian men vary based on sexual orientation identity. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
49,901 M | 98.32% H 1.07% G 0.60% B |
HX–(95% CI) 44.4 (44.3, 44.5) G X– (95% CI) 39.9 (38.4, 41.4) B X–(95% CI) 39.3 (36.5, 42.1) |
NR |
| Brown & Keel, 2015 | Northeastern United States | Waves 3 and 4 of a longitudinal study at a northeastern university in 1982, 1992, and 2002 and followed at 10-year intervals. | To examine how romantic relationships impact the trajectory of eating pathology in gay and bisexual versus heterosexual men. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI. |
Sexual identity. Reported as H, G, and B. |
573 M | 91.10% H 8.90% GB |
H X– (SD): 29.41 (8.65) GB X– (SD): 27.40 (9.09) |
NR |
| Caceres et al., 2018 | United States | 2001–2012 NHANES | To examine sexual orientation differences in modifiable risk factors for CVD and CVD diagnoses in men. | BMI calculated from measured height and weight. Reported as prevalence and likelihood of obesity. f |
Combined sexual identity and behavior. Reported as exclusively H, H-identified MSM, G, and B. |
7,731 M | 94.31% exclusively H 2.32% H-identified MSM 1.90% G 1.51% B |
20–29: 24.8% 30–39: 24.9% 40–49: 26.3% 50–59: 23.9% |
White: 70.4% AA/B: 10.2% H/L: 14.1% Other: 5.3% |
| Caceres et al., 2019 | United States | 2014–2016 BRFSS | To investigate sexual orientation differences in CVD risk and CVDs. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of obesity. f |
Sexual identity. Reported as H, G, and B. |
177,096 M 218,058 W |
97.03% H 2.03% G 1.25% B |
18–24: 10.63% 25–34: 16.46% 35–44: 16.81% 45–54: 19.13% 55–64: 18.88% ≥65: 18.65% |
White: 69.90% AA/B: 10.41% H/L: 12.31% Other: 7.37% |
| Caceres et al., 2022 | United States | 2001–2016 NHANES | To examine racial/ethnic differences in physiological risk factors for CVD among sexual minority and heterosexual adults. | BMI calculated from measured height and weight. Reported as X– (SD) BMI and prevalence of overweight e and obesity. f |
Sexual identity. Reported as H, G, B, and not sure/something else. |
11,310 M 10,995 W |
95.5% H 1.94% G 1.48% B 1.34% not sure |
H X– (SD) 38.8 (0.2) G X– (SD) 40.5 (1.2) B X– (SD) 38.6 (1.2) Not sure X– (SD) 40.6 (1.3) |
White: 66.91% AA/B: 11.62% H/L: 17.05% |
| Calzo et al., 2018 | United Kingdom | 1991–1992 ALSPC | To examine the associations of sexual orientation and eating disorder symptoms among adolescents. | BMI calculated from measured height and weight. Reported as prevalence of overweight e and obesity. f |
Combined sexual identity and attraction. Reported as: completely H, mostly H, and combined GB. |
2,367 M 2,681 W |
91.30% completely H 6.17% mostly H 2.53% GB |
NR | White: 93% |
| Conner et al., 2004 | England, United Kingdom | Primary data collection in bars in Leeds, England | To examine the impacts of gender and sexual orientation on eating motives and eating styles in addition to body image. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI. |
Sexual identity. Reported as H and G. |
58 M 63 W |
51.72% H 28 48.28% G |
H X– (SD) 23.1 (3.27) G X– (SD) 23.9 (4.41) |
NR |
| Conron et al., 2010 | Massachusetts, United States | 2001–2008 State BRFSS | To provide estimates of several leading US adult health indicators by sexual orientation identity and gender. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of overweight e and obesity. f |
Sexual identity. Reported as H, G, and B. |
26,507 M 40,852 W |
95.77% H 3.48% G 0.73% B |
18–33: 22.20% 34–49: 41.31% 50–64: 36.49% |
White: 82.17% AA/B: 4.92% H/L: 8.34% Asian: 2.92% Other: 1.66% |
| Davids & Green, 2011 | United States | Online Survey from various recruitment sites | To examine psychological predictors of body dissatisfaction and eating disorder symptoms among gay, bisexual, and heterosexual men. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI. |
Sexual identity. Reported as H, G, and B. |
167 M 272 W |
20.36% H 57.49% G 22.16% B |
H X– (SD) 23.74 (7.08) G X– (SD) 26.28 (8.53) B X– (SD) 33.22(13.95) |
Lost due to error in software data collection program. |
| Deputy & Boehmer, 2010 | California, United States | 2005 CHIS | To investigate eating habits and exercise behaviors as mediators in the relationship between sexual orientation and BMI in men. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of overweight e and obesity. f |
Sexual identity. Reported as H and sexual minority (GB). |
14,982 M, unweighted 11,767,858 M, weighted |
96.39% H 3.61%14 sexual minority men |
H X– 40.5 Sexual minority men X– 39.9 |
White 58.46% Non-White 41.64% |
| Deputy & Boehmer, 2014 | California, United States | 2007–2011 CHIS | To determine differences in weight at age 18 y and at current age and weight change by sexual orientation within different racial/ethnic populations, stratifying by gender. | BMI calculated from self-reported height and weight. Reported as likelihood of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
54,095 M 66,179 W |
95.89% H 3.03% G 8.08% B |
H X– (SE) 40.7 (60.0) G X– (SE) 40.7 (60.4) B X– (SE) 40.1 (60.9) |
White: 55.68% H/L: 27.81% Asian: 10.57% AA/B: 6.31% |
| Dilley et al., 2010 | Washington, United States | 2003–2006 State BRFSS | To identify health disparities for a statewide population of LGB men and women compared with their heterosexual counterparts. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
30,845 M 48,655 W |
97.62% H 1.61% G 0.76% B |
18–29: 22.14% 30–39: 20.09% 40–49: 20.96% 50–59: 17.68% 60–69: 4.45% ≥70: 0.90% |
White: 83.76% AA/B: 2.19% Asian/PI: 4.07% NA: 1.41% Other: 0.40% Multi: 0.20% H/L 8.04% |
| Epel et al., 1996 | United States | Random sample of 500 personal ads published in 1992 from 7 publications serving the groups of interest. | To assess body shape ideals across gender, sexual orientation, race, SES, and age. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI and prevalence of elevated BMI. d |
Sexual identity. Reported as H, G, and B. |
140 M
h
48 W |
75.71% H 24.29% G |
Total
g
X– (SD) 42.3 (14.0) |
White or mostly white |
| Everett & Mollborn, 2013 | United States | Wave IV AddHealth | To determine if gay and bisexual persons are more likely to be hypertensive than heterosexual-identified persons and to assess if indicators of victimization and discrimination, cardiovascular risk factors explain differences in hypertension by sexual orientation. | BMI calculated from measured height and weight data. Reported as prevalence of overweight e and obesity.f,i |
Combined sexual identity and attraction. Reported as H, B/mostly H, and G/mostly G. |
6,678 M 7,555 W |
93.41% completely H 4.06% B/mostly H 2.67% G/mostly G |
NR | NR |
| Frederick & Essayli, 2016 | United States | Five surveys posted on the official news website of for two weeks each in 2003, 2006, 2010, 2011, and 2012. j | To examine the extent to which gay and heterosexual men differed on measures related to body image. | BMI calculated from self-reported height and weight. Reported as X– (SD) BMI and prevalence of elevated BMI d and obesity. f |
Sexual identity. Reported as H and G. |
Study 1. 2003 Sex and Body Image Survey. 27 237 M |
94.41% H 5.59% G |
H X– (SD) 37 (12) G X– (SD) 35 (10) |
NR |
|
Study 2. 2010 Sex, Stress, and Success Survey. 11 470 M |
97.11% H 2.89% G |
H X– (SD) 45 (12) G X– (SD) 40 (12) |
NR | ||||||
|
Study 3. 2012 TV Viewing Habits Survey. 3237 M |
87.12% H 12.88% G |
H X– (SD) 50 (11) G X–SD) 47 (11) |
NR | ||||||
|
Study 4. 2006 Sex and Relationship Survey. 32,080 M |
97.72% H 2.28% G |
HV(SD) 40 (11) G X– (SD) 38 (10) |
White: 89.98% AA/B: 2.98% H/L 3.02% Asian 2.00% Other 2.02% |
||||||
| Fredriksen-Goldsen et al., 2013 | Washington, United States | 2003–2010 State BRFSS | To investigate health disparities among LGB adults aged ≥50 y. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of obesity. f |
Sexual identity. Reported as H, G, B, and something else. |
37,820 M 58,319 W |
98.21% H 1.22% G 0.57% B |
Range 50–98 H X– (SD) 62.35 (0.07) G X– (SD) 59.26 (0.45) B X– (SD) 60.22 (0.75) |
White: 90.45% |
| Fricke et al., 2019 | California, United States | 2008, 2011, and 2014–2015 Kaiser Permanente Northern California Member Health Surveys | To test if sexual minorities were less likely than heterosexuals to meet the physical activity guidelines. | BMI calculated from measured height and weight. Reported as prevalence of obesity. f |
Sexual identity. Reported as H or sexual minority (GB). |
19,392 M 23,142 W |
95.51% H 4.49% sexual minority men |
20–44: 25.07% 45–64: 33.16% 65–79: 35.59% ≥80: 6.18% |
White: 65.08% AA/B: 5.35% H/L: 10.77% Asian: 15.93% Other: 2.68% |
| Fricke & Sironi, 2020 | United States | Waves III and IV of AddHealth | To analyze the effect of depression on sexual identity change and BMI, obesity, and physical activity. | BMI calculated from self-reported height and weight. Reported as prevalence of obesity. f |
Combined sexual identity and attraction. Reported at H, mostly H, B, mostly G, and G. |
5,400 M 5,949 W |
93.6% H 3.5% mostly H 0.5% B 0.7% mostly G 1.7% G |
X– 28.9 | White: 66.5% AA/B: 13.8% H/L: 12.0% Asian: 3.8% Other: 3.9% |
| Frisch & Zdravkovic, 2010 | Denmark | Civil Registration System | To study the associations between weight, length, and body mass index (BMI) at birth and same-sex marriage in young adulthood. | BMI calculated from measured height and weight. Reported as X– (SD) BMI. |
Partnership or marriage. Reported as same- and opposite-sex partnerships or marriages. |
419,112 M 399,400 W |
99.93% opposite-sex partnered 0.07% same-sex partnered |
NR | NR |
| Garland-Forshee et al., 2014 | Oregon, United States | 2005–2008 State BRFSS | To examine health-related disparities among LGB men and women compared with heterosexual men and women. | BMI calculated from self-reported height and weight. Reported as likelihood of obesity. f |
Sexual identity. Reported as H, G, B, and other. |
16,475 M 26,271 W |
97.63% H 1.63% G 0.75% B |
18–34: 31.86% 35–54: 38.26% >55: 29.89% |
White: 85.93% All other races & H/L: 14.07% |
| Gonzales & Henning-Smith, 2017 | United States | 2014–2015 BRFSS | To examine differences by sexual orientation in an array of health outcomes and health risk factors. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of obesity. f |
Sexual identity. Reported as H, G, and B. |
129,343 M 179,203 W |
97.01% H 1.83% G 1.16% B |
18–24: 13.07% 25–34: 16.20% 35–44: 16.21% 45–54: 18.25% 55–64: 17.31% ≥65: 18.57% |
White: 70.59% AA/B: 11.20% H/L: 10.16% Other/multi: 6.42% |
| Gorman et al., 2015 | United States | 2005–2010 BRFSS | To evaluate how health reports and social advantage operate before and after adjustment for established health risk factors by sexual orientation. | BMI calculated from self-reported height and weight. Reported as prevalence of overweight e and obesity. f |
Sexual identity. Reported as H, G, B, and other/don’t know |
162,475 M 252,798 W |
97.20% H 2.09% G 0.72% B |
H X– (SD) 43.9 (15.2) G X– (SD) 42.7 (13.5) B X– (SD) 38.0 (13.9) |
White: 63.29% AA/B: 4.80% H/L: 20.86% Asian: 8.45% Other: 2.60% |
| Hatzenbuehler et al., 2013 | United States | Wave IV AddHealth | To determine whether sexual orientation disparities in biomarkers of early CVD risk are present among young adults. | BMI calculated from measured height and weight. Reported as X– (SD) BMI. |
Sexual identity. Reported as H and GB. |
6,438 M 6,013 W |
96.69% H 3.31% GB |
H X– (SD) 29.03 (0.12) GB X– (SD) 29.04 (0.19) |
AA/B: 14.45% Asian: 3.11% H/L: 11.23% Multi, NA, other: 5.56% White 65.64% |
| Heck & Jacobson, 2006 | United States | 1997 – 2004 NHIS | To examine ever and current asthma diagnosis among persons in same-sex relationships. | BMI calculated from self-reported height and weight. Reported as prevalence of overweight e and obesity. f |
Partnership or marriage. Reported as same- and opposite-sex partnerships or marriages. |
61,298 M 68,196 W |
99.30% opposite-sex partnership 0.70% same sex partnership |
18–29 11.64% 30–39: 23.08% 40–49: 24.32% ≥50: 41.06% |
White: 77.42% AA/B: 8.60% H/L: 10.49% Other: 4.00% |
| Jackson et al., 2016 | United States | 2013–2014 NHIS | To investigate the relationship between sexual orientation identity and health among US women and men. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of overweight e and obesity. f |
Sexual identity. Reported as H, G, B, and something else/don’t know. |
30,961 M 38,309 W |
96.79% H 2.02% G 0.52% B 067% something else/don’t know |
Range 18 to >85 | White: 62.55% AA/B: 12.97% H/L: 15.84% NA: 1.31% Asian/PI: 6.19% |
| Laska et al., 2015 | United States | 2007–2011 CSHS | To assess disparities in weight and weight-related behaviors among college students by sexual orientation and gender. | BMI calculated from self-reported height and weight. Reported as prevalence of overweight e and obesity.f,g,h |
Combined sexual identity and behavior. Reported as H, discordant H, G, B, and unsure. |
12,498 M 21,384 W |
93.05% H 0.85% discordant H 2.89% G 1.61% B 1.60% unsure |
18–20: 32.83% 21–24: 33.89% ≥25: 33.31% |
White: 80.76% AA/B: 4.27% Asian: 7.08% H/L: 2.26% Multi/other: 4.02% |
| Newlin Lew et al., 2018 | United States | 2014 BRFSS | To assess the prevalence and related ORs for obesity, prediabetes, and diabetes in sexual minority men compared with straight men. | BMI calculated from self-reported height and weight. Reported as prevalence and likelihood of obesity. f |
Sexual identity. Reported as H, G, and B. |
53,542 M | 97.00% H 2.00% G 1.00% B |
18–24: 10.87% 25–34: 16.85% 35–44: 16.10% 45–54: 19.51% 55–64: 18.13% ≥65: 18.54% |
White: 80.24% AA/B: 11.99% H/L: 7.71% |
| Nyitray et al., 2019 | Brazil, Mexico, and United States | Anal canal specimens from men, ages 18–70 y | To study the association between HPV infection and BMI. | BMI calculated from measured height and weight. Reported as prevalence of overweight e and obesity. f |
Sexual behavior. Reported as MSM and MSW. |
1,676 M | 80.43% MSW 19.57% MSM |
18–24: 25.95% 25–34: 31.92% 35–44: 26.91% 45–70: 15.21% |
Race
White: 46.60% AA/B: 14.44% Other: 37.89% Refuse/missing: 1.07% Ethnicity H/L = 46.36% Non-Hispanic: 52.57% Refuse/missing: 1.07% |
| Rosario et al., 2016 | United States | 1999–2010 GUTS | To examine sexual-orientation disparities in frequent engagement in cancer-related risk indicators of tobacco, alcohol, diet and physical activity, ultraviolet radiation, and STIs. | BMI calculated from self-reported height and weight.
b
Reported as prevalence and likelihood of elevated BMI. d |
Combined sexual identity and behavior. Reported as completely H, mostly H, G, and B. |
3,797 M 6,161 W |
90.25% completely H 6.45% mostly H 2.66% G 0.63% B |
NR | Total
f
White: 95.4% Minorities: 4.6% |
| Strutz et al., 2015 | United States | Wave IV AddHealth 2008 | To describe a wide range of health status and healthcare access characteristics of sexual minorities in comparison with those of the majority population. | BMI calculated from measured height and weight. Reported as prevalence and likelihood of overweight e and obesity. f |
Combined sexual attraction, behavior, and identity. Sexual minorities were reported as those having all three indicators, attraction plus any other indicator, and any one indicator of sexual minority status. |
6,020 M 7,068 W |
90.50% H 9.50% any one indicator 3.32% all three indicators 3.14% attraction plus |
24–27: 34.17% 28–29: 33.16% ≥30: 32.66% |
White: 67.16% AA/B: 14.60% H/L: 11.98% Other: 6.36% |
| Stupplebeen et al., 2019 | California, United States | 2003–2012 CHIS | To examine whether the association between weight status and four chronic diseases (heart disease, hypertension, lifetime asthma, and type 2 diabetes) varied by sexual orientation identity among adult men. | BMI calculated from self-reported height and weight.
b
Reported as X– (SD) BMI and prevalence of overweight e and obesityf,i,k |
Sexual identity. Reported as H and GB. |
72,214 M | 95.96% H 4.04% GB |
X– (SE) 40.66 (0.09) | H/L: 35.51% White: 46.54% AA/B: 5.6% Asian: 12.35% |
| Trinh et al., 2017 | United States | 2013–2015 NHIS | To analyze the health behaviors and outcomes and use of health care services by sexual and racial/ethnic minorities compared with white heterosexuals. | BMI calculated from self-reported height and weight.
b
Reported as prevalence of overweight e and obesity. f |
Sexual identity. Reported as H and sexual minority (GB). |
41,059 M 50,854 W |
97.9% H 2.1% sexual minority |
Total
g
X– (SD) 47 (0.14) |
White: 68.56% AA/B: 13.35% H/L: 18.09% |
| Tuthill et al., 2020 | United States | 2005–2010 BRFSS | To examine how health status and health behavior vary within and across LGB men and women. | BMI calculated from self-reported height and weight.
b
Reported as prevalence of obesity. f |
Sexual identity. Reported as H, G, B, and other/don’t know |
223,675 M 334,098 W |
97.39% H 1.91% G 0.70% B |
NR | White: 81.82% AA/B: 5.91% H/L: 8.38% Asian/PI: 2.10% NA: 1.79% |
| VanKim et al., 2020 | Minnesota, United States | 2009–2013 State CSHS | To examine the relationship between the college LGB climate, including campus-based policies and resources, and obesity across sexual orientation groups. | BMI calculated from self-reported height and weight.
b
Reported as prevalence and likelihood of overweight e and obesity. f |
Combined sexual identity and behavior. Reported as H, discordant H, G, B, and unsure. |
10,368 M 18,219 W |
92.85% H 0.68% discordant H 3.24% G 1.53% B 1.70% unsure |
NR | NR |
| Wolstein et al., 2018 l | United States | 2011–2014 CHIS | To examine differences in health care access, health behaviors, and health outcomes by sexual orientation among California adults. | BMI calculated from self-reported height and weight.
b
Reported as prevalence and likelihood of obesity. f |
Sexual identity. Reported as H, G, B, and other. |
14,489, 000 M 15,344,000 W |
93.6% H 3.4% G 2.6% B 0.4% other |
Range: 18–70 | NR |
Note. GUTS = growing up today study; BMI = body mass index; H = heterosexual; B = bisexual; G = gay; M = men; W = women; NR = not reported; BRFSS = behavioral risk factor surveillance system; H/L = Hispanic/latinx; AA/B = African American/black; GfK = growth from knowledge; = mean; SD = standard deviation; min = minimum; max = maximum; MEPS = medical expenditure panel survey; CHIS = California health interview survey; CCHS = Canadian community health survey; CI = confidence intervals; NHANES = national health and nutrition examination survey; CVD = cardiovascular disease; MSM = men who have sex with men; ALSPC = Avon longitudinal study of parents and children; NA = native American; SES = socioeconomic status; AddHealth, The National Longitudinal Study of Adolescent to Adult Health; NHIS = national health interview survey; CSHS = college student health survey; OR = odds ratio; HPV = human papillomavirus; MSW = men who have sex with women; STIs = sexually transmitted infections; SE = standard error; CDC = centers for disease control and prevention; FPL = federal poverty level; L = lesbian; Multi = multiracial; PI = pacific islander; y = years.
Percentages with one decimal place were directly reported in the study, while percentages with two decimal places were calculated from data reported in the study. bAll numbers reported correspond to observations from repeated-measures longitudinal data. cFor participants 12–20 y, BMI was converted to age- and sex-specific BMI Z-scores using CDC standards. dDefined as BMI ≥25 kg/m2. eDefined as BMI ≥25 kg/m2 but <30 kg/m2. fDefined as BMI ≥30 kg/m2. gCombined for men and women. hFor valid data points reporting BMI; the forest plot in Supplementary Figure 1 only includes the comparisons for 57 H vs. 34 G men reported, and excludes 26 H White and 23 H Black men whose. i Obesity was subclassified as Grade 1 (BMI≥30 kg/m2 but <35 kg/m2), Grade 2 (BMI≥35 kg/m2 but <40 kg/m2), or Grade 3 (BMI≥40 kg/m2). jThe 2011 Money, Sex, and Love Survey (Study 5) does not report measures relevant to this meta-analysis and, thus, was excluded. kGrade 2 and Grade 3 obesity were combined as a single category. l Authors were contacted to verify the absolute numbers of M and W participants.
The number of male participants ranged between 58 (Conner et al., 2004) and 11,767,858 (Deputy & Boehmer, 2010) with a median (interquartile range [IQR]) of 26,507 (5,710, 63,704) participants. The percentage of sexual minority men included in the studies as a proportion of all male participants ranged from 0.07% (Frisch & Zdravkovic, 2010) to 79.64% (Davids & Green, 2011), with a median (IQR) of 3.37% (2.63%, 4.70%).
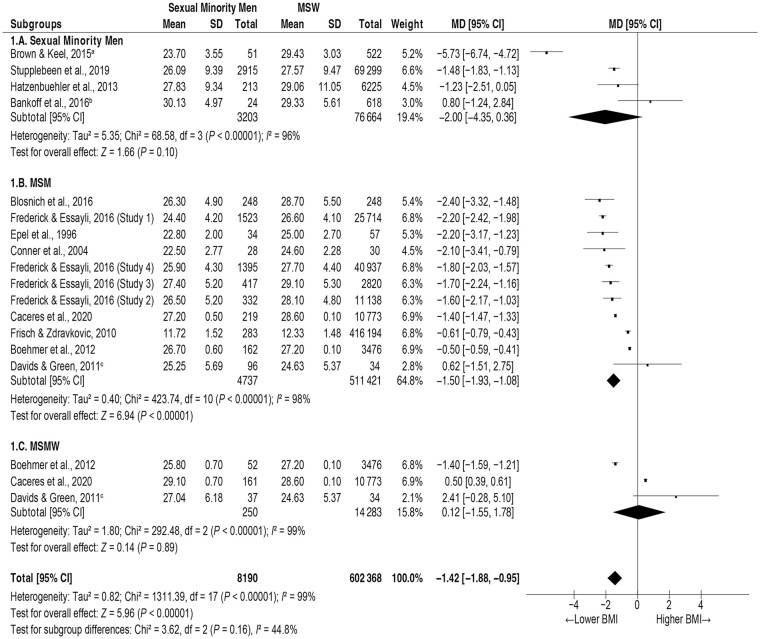
Mean BMI
Figure 1 presents the forest plot from the 12 studies reporting BMI means and their respective variance for the populations of interest. For these studies, the overall MDs (95% CIs) by subgroups were −2.00 (−4.35, 0.36) kg/m2 for all sexual minority men (Subgroup 1.A), −1.50 (−1.93, −1.08) kg/m2 for MSM (Subgroup 1.B), and 0.12 (−1.55, 1.78) kg/m2 for MSMW (Subgroup 1.C.). Overall, heterogeneity for the subgroup comparisons was high (I2=99%) with a statistically significantly lower BMI (MD −1.42; 95% CI [−1.88, −0.95 kg/m]2) for the pooled subgroup analysis.
Figure 1.
Forest Plot of Studies Reporting Mean Values of BMI Among Sexual Minority Men.
Note. BMI = body mass index; CI = confidence interval; df = degrees of freedom; MD = mean difference; MSM = men who have sex with men; MSMW = men who have sex with men and women; MSW = men who have sex with women; SD = standard deviation.
aParticipants were diagnosed with eating disorders. bUnweighted means. cParticipants were diagnosed with body dissatisfaction disorder.
Prevalence Estimates
Table 2 presents a summary of the point estimates of prevalence rates for overweight, obesity, and elevated BMI by sexual orientation for all studies included. Study-by-study forest and funnel plots are presented in Supplementary Figures S2 and S3, respectively.
Table 2.
Prevalence Estimates of Overweight, Obesity, and Elevated BMI by Sexual Orientation.
| Studies a (n) | Prevalence estimate | 95% Confidence interval | Z | P | ||
|---|---|---|---|---|---|---|
| Subgroups analyzed | Lower bound | Upper bound | ||||
| Overweight (N = 16) | ||||||
| All sexual minority men | 4 | 34.13% | 27.61% | 41.32% | −4.2039 | <.001 |
| MSM | 15 | 35.64% | 32.13% | 39.31% | −7.3903 | <.001 |
| MSMW | 8 | 33.46% | 28.66% | 38.62% | −6.0053 | <.001 |
| MSW | 19 | 44.00% | 40.75% | 47.31% | −3.5405 | <.001 |
| Obesity (N = 26) | ||||||
| All sexual minority men | 6 | 20.65% | 17.82% | 0.2379 | −14.4861 | <.001 |
| MSM | 23 | 20.01% | 18.55% | 0.2156 | −28.8903 | <.001 |
| MSMW | 16 | 26.60% | 24.38% | 0.2895 | −16.9734 | <.001 |
| MSW | 29 | 25.73% | 24.32% | 0.2720 | −27.6044 | <.001 |
| Elevated BMI (N = 5) | ||||||
| MSM | 5 | 38.80% | 23.60% | 56.55% | −1.2420 | .21 |
| MSMW | 5 | 46.71% | 29.52% | 64.72% | −0.3493 | .73 |
| MSW | 5 | 54.75% | 37.31% | 71.09% | 0.5261 | .60 |
Note. BMI = body mass index; MSM = men who have sex with men; MSMW = men who have sex with men and women; MSW = men who have sex with women.
Frederick and Essayli (2016) is a single report on four independent studies (denoted as Studies 1-4 in Supplementary Figure S2, Panel B), and thus, the number of data points is greater than the number of studies for the categories where this study is included.
Crude prevalence rates were calculated from the studies reporting sexual orientation-specific data for overweight (n = 16), obesity (n = 26), and elevated BMI (n = 5). Crude prevalence estimates for all three outcome categories (i.e., overweight, obesity, and elevated BMI) for sexual minority men, MSM, and MSMW were consistently lower than the respective outcome estimates for MSW. Statistically significant lower crude prevalence rates were identified for overweight and obesity estimates but not for the crude prevalence rate of elevated BMI.
Given that age can confound prevalence estimates of the outcomes of interest, crude prevalence estimates were adjusted through an exploratory meta-regression across studies reporting mean age using random-effects estimation (Table 3). Meta-regression showed that the effect of age increases with BMI. While age did not show a tangible overall effect on the prevalence of overweight (R2 analog = 0), small and moderate effects were observed for age on the respective prevalence rates of overweight (R2 analog = .27) and elevated BMI (R2 analog = .42). It must be noted, however, that only a small proportion of studies reported age as a mean value that could be incorporated in the meta-regression.
Table 3.
Meta-Regression Models of Prevalence Rates of Overweight, Obesity, and Elevated BMI Regressed on Mean Age.
| Subgroups analyzed | Coefficient | Standard error | 95% CI | Z | P | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Overweight | ||||||
| Intercept | −1.6847 | 0.7295 | −3.1145 | −0.2550 | −2.31 | .02 |
| Mean age | 0.0297 | 0.0174 | −0.0044 | 0.0639 | 1.71 | .09 |
| Model fit | τ² = 0.0614, τ = 0.2477, I² = 99.92%, Q = 19342.82, df = 15, p < .001, R2 analog = .00 | |||||
| Obesity | ||||||
| Intercept | −2.2538 | 0.4719 | −3.1788 | −1.3288 | −4.78 | <.001 |
| Mean age | 0.0227 | 0.0106 | 0.0019 | 0.0435 | 2.13 | .03 |
| Model fit | τ² = 0.1322, τ = 0.3635, I² = 99.84%, Q = 10760.39, df = 17, p < .001, R2 analog = .27 | |||||
| Elevated BMI | ||||||
| Intercept | −1.9249 | 0.8333 | −3.5581 | −0.2916 | −2.31 | .02 |
| Mean age | 0.0424 | 0.0171 | 0.0088 | 0.0760 | 2.48 | .01 |
| Model fit | τ² = 0.1686, τ = 0.4106, I² = 98.42%, Q = 316.53, df = 5, p <.001, R2 analog = .42 | |||||
Note. BMI = body mass index; CI = confidence interval.
Likelihood Estimates
Table 4 presents the summary of the likelihood estimates for overweight, obesity, and elevated BMI by sexual orientation. The respective forest and funnel plots can be found in Supplementary Figures S4 and S5, respectively.
Table 4.
Prevalence Estimates of Overweight, Obesity, and Elevated BMI by Sexual Orientation.
| Subgroups analyzed | Studies (n) | OR b | 95% CI | χ2 | df | P | I 2 | |
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Overweight | 0.68 | 0.58 | 0.80 | 89.56 | 12 | <.001 | 87% | |
| All sexual minority men | 2 | 0.68 | 0.55 | 0.83 | 0.13 | 1 | .72 | 0% |
| MSM b | 6 | 0.63 | 0.50 | 0.79 | 49.92 | 5 | <.001 | 90% |
| MSMW b | 5 | 0.75 | 0.52 | 1.08 | 31.92 | 4 | <.001 | 87% |
| Obesity | 0.84 | 0.78 | 0.90 | 87.58 | 22 | <.001 | 75% | |
| All sexual minority men | 3 | 0.67 | 0.57 | 0.80 | 1.77 | 2 | .41 | 0% |
| MSM b | 11 | 0.79 | 0.71 | 0.88 | 50.32 | 10 | <.001 | 80% |
| MSMW b | 9 | 0.98 | 0.92 | 1.04 | 9.27 | 8 | .32 | 14% |
| Elevated BMI | 0.84 | 0.56 | 1.25 | 332.10 | 12 | <.001 | 96% | |
| MSM | 7 | 0.88 | 0.53 | 1.48 | 237.01 | 6 | <.001 | 97% |
| MSMW | 6 | 0.72 | 0.53 | 0.98 | 9.56 | 5 | .09 | 48% |
Note. BMI = body mass index; df = degrees of freedom; CI = confidence interval; MSM = men who have sex with men; MSMW = men who have sex with men and women; MSW = men who have sex with women; OR = odds ratio.
The reference group is MSW. bDeputy and Boehmer (2014) reported four unadjusted ORs by race/ethnicity for MSM and MSW, which were weighted and averaged as a single estimate using the same meta-analytic assumptions in this study.
Seven studies presented data on the likelihood of being overweight, either as crude or as adjusted ORs or PRs. The meta-analysis shows that two of the sexual minority men subgroups were significantly less likely to be overweight, namely all sexual minority men (32% less likely) and MSM (37% less likely), while MSMW were not significantly different from MSW in their likelihood of being overweight (OR 0.75, 95% CI [0.52, 1.08]). Overall, all subgroups of sexual minority men were significantly less likely to be overweight (OR 0.68; 95% CI [0.58, 0.80]). Heterogeneity for studies on overweight was variable and most effects operated in the same direction.
Fourteen studies presented data on the likelihood of obesity, either as crude or adjusted ORs (Table 4). Again, sexual minority men and MSM were 33% and 21% less likely to be obese, while MSMW did not reach statistical significance for this comparison. Two were identified as significant outliers (Azagba et al., 2019; Caceres et al., 2018). After removal, the analysis reached statistical significance for the MSM (OR 0.79, 95% CI [0.71, 0.88]) subgroup but not for the MSMW subgroup (OR 0.98, 95% CI [0.92, 1.04]). Removal of outliers yielded an overall lower likelihood of obesity among all sexual minority subgroups pooled (OR 0.84, 95% CI [0.78, 0.90]), not shown in Table 4.
Seven studies presented data on the likelihood of elevated BMI. None of the subgroup comparisons reached statistical significance. Funnel plot analyses did not identify studies that would operate as outliers among these subgroups. Pooled analyses did not reach statistical significance and heterogeneity between studies was important (I2 = 96%).
Risk of bias
Supplementary Table S1 summarizes the bias assessment for the 43 studies included. Most showed a very low risk of participant selection or response biases (n = 40 [93%] and n = 35 [81%], respectively). The risk of information or misclassification biases was less clear, with most studies assessed as uncertain (n = 33 [77%]). While almost half of the studies presented a low risk of confounding by income (n = 19), education (n = 21), or age (n = 26), only three studies included information on HIV serostatus of participants (Blosnich et al., 2014, 2016; Nyitray et al., 2019).
Discussion
The purpose of this meta-analysis was to examine disparities in the prevalence and likelihood of obesity and overweight among sexual minority men. Based on the extensive review employed, it is believed this is the first study to use meta-analytic techniques to achieve this goal, although a narrative systematic review with comparable findings has been published (Caceres et al., 2017). Forty-three studies, mostly conducted in the United States between 1996 and 2020, were included, although representation from other countries must be noted.
This meta-analysis demonstrated a consistently lower mean BMI among all analytic subgroups of sexual minority men compared with MSW, which was also replicated when analyzing crude prevalence rates and the adjusted likelihood of obesity, overweight, and elevated BMI (≥25 kg/m2) overall and across most analytic subgroups.
Various explanations have been posited for the BMI disparities observed among sexual minority men. First, compared with heterosexual men, sexual minority men have more awareness of their body image and watch their weight more closely (Warren et al., 2016). Recent studies suggest sexual minority men and heterosexual women are significantly more prone to body dissatisfaction, which may be due to sustained and pervasive social pressure on body image (Conner et al., 2004; Meneguzzo et al., 2021). Besides awareness of body image, obesity-related stigma and the underlying psychological conditions—such as depression, anxiety, and stress—have been demonstrated as important predictors of obesity among gay men (Conner et al., 2004; Fulton & Srinivasan, 2021; Meneguzzo et al., 2021; Warren et al., 2016). These conditions may ultimately be a result of nonconformity stress—a key element within the Minority Stress Theory (Frost et al., 2015; Meyer, 2003). Although the studies included did not specifically assess for psychological conditions, the significantly lower prevalence rates of obesity among sexual minority men are in agreement with this first explanation.
Although weight status can be evaluated via several methods, all the studies included in this meta-analysis used BMI to determine weight status. Thus, a second plausible explanation for the disparities observed is BMI’s lower predictive value for cardiovascular disease, especially when compared with other anthropometric measures alone or in combination with imaging techniques that have validated cutoff values for men (e.g., waist circumference, waist-to-hip ratio, waist-to-height ratio, sagittal abdominal diameter, or body fat percentage; (Antonopoulos & Tousoulis, 2017). This lower predictive value derives from the fact that BMI does not measure body fat distribution, which in turn varies by sex, age, and race and ethnicity (Deurenberg et al., 2002; Flegal et al., 2013; Jackson et al., 2002). BMI does not accurately distinguish body composition of lean and fat mass, and individuals classified as overweight or obese may indeed have increased muscle mass (Jackson et al., 2002; Oreopoulos et al., 2010), which does not necessarily translate into increased risk of CVD. Studies examining obesity could triangulate multiple assessments of body weight and composition to improve analytic accuracy. In addition, biomarkers associated with obesity, such as markers of chronic low-grade inflammation (e.g., cortisol and high-sensitivity C-reactive protein), markers in the insulin/insulin-like growth factor axis, and certain adipokines (e.g., leptin, adiponectin, and resistin), can also be incorporated to better understand the context of CVD risk (Nimptsch et al., 2019).
While most studies included a reported demographic status of the participants, the intersectional effect of sexual minorities and other statuses on weight cannot be estimated. Thus, the third explanation of weight disparities observed arises from an intersectional framework with other demographic variables. In their systematic review on health outcomes within the Minority Stress Theory, VanKim et al. (2020) identified studies demonstrating plausible interaction effects of sexual minority status with race, ethnicity, age, and educational attainment. These effects were consistent across most health outcomes, including BMI differences when compared with heterosexual populations.
A fourth hypothesis for the weight disparities observed in this study is based on the population study design. All studies included in this meta-analysis used survey data, and most participants self-reported weight and height. Therefore, self-report biases (i.e., recall bias and social desirability bias) cannot be ruled out (Althubaiti, 2016). Two systematic literature reviews analyzed the accuracy of self-reported weight, height, and BMI derived from self-reported measures in studies published between 1982–2005 and 2005–2017 (Connor Gorber et al., 2007; Maukonen et al., 2018). Both reviews concluded that both men and women underestimate self-reported weight and overestimate self-reported height, with the ultimate effect of underestimating BMI calculations. Thus, data collection efforts at the population level should rely only on anthropometry rather than self-report to avoid underestimation of weight and BMI and overestimation of height.
Last, and perhaps most importantly, a lower prevalence of obesity and overweight among sexual minority men may not necessarily translate into a healthier cardiovascular status. The obesity paradox in CVD asserts that overweight or class I obese persons may have a better prognosis after CVD ensues (Antonopoulos & Tousoulis, 2017; Carbone et al., 2019), while individuals presenting with normal weight or underweight have a poorer prognosis from CVD as a result of a progressive and sustained catabolic state with loss of lean mass (Elagizi et al., 2018). A meta-analysis reported that, compared with people having normal BMIs, people with obesity presented with significantly higher all-cause mortality, while people with overweight presented lower all-cause mortality (Flegal et al., 2013). Although the obesity paradox in CVD has been studied in the general population, the current study is the first quantitative study demonstrating the plausibility of this phenomenon among sexual minority men.
We assessed the risk of selection, information or misclassification, and response biases. Misclassification bias is always a possibility given the lack of standardization in research measuring the sexual orientation of participants. Biases associated with self-reported data, such as height and weight, are also potential threats to study validity. Among the four potential confounders included in this study, the role of HIV serostatus is by far the most uncertain, followed by the risk of confounding by education level.
Limitations
This study has some limitations worth noting. First, as it has been stated, several studies relied on self-reported height and weight to estimate BMI, which may drive over- or underestimation of key variables due to social desirability and to idealized body image—especially among sexual minority populations. Second, there are two possible sources of misclassification in the studies included. On the one hand, while population representative samples accurately represent sexual minorities (Grasso et al., 2019), scholarly inquiries are limited due to a recognized lack of clarity and consistency in defining specific sexual minority groups (Legate & Rogge, 2019; Wolff et al., 2017). Studies reported either well-known sexual orientation measures of behavioral, identity, or attraction items or reported new measures, such as same-sex partnership. This heterogeneity introduces the possibility of misclassification bias. On the contrary, some studies estimated the likelihood of elevated BMI, combining overweight and obesity as a single measure. This may partially explain the nonsignificant findings in this comparison. Third, while other potential confounders—such as educational attainment and HIV serostatus—were reported among the publications assessed, only a handful of studies indeed controlled for these differences. It must also be noted that only a small number of studies reports age as a mean value that can be incorporated in meta-regression analyses to understand the effect of sampling distribution by age on the BMI estimates.
Limitations aside, this study has important strengths worth mentioning. Our analyses demonstrated that, compared with heterosexual men, sexual minority men present with a significantly lower prevalence of overweight, obesity, and elevated BMI. This finding has important implications for CVD prevention, which should encourage a healthy control of body weight and composition as one of the American Heart Association’s Life Simple Seven. This study also provides plausible evidence for the presence of the obesity paradox in CVD among sexual minority men, warranting further research efforts to understand CVD outcomes among sexual minorities across diverse BMI statuses.
Conclusion
Compared with heterosexual men, sexual minority men present a significantly lower prevalence of obesity and overweight, as measured by BMI. Several plausible explanations exist for this phenomenon, including increased awareness of body image, predictive limitations of BMI as the only measure of weight-to-height, interaction effects with other demographic minority status, and the obesity paradox of cardiovascular disease. Future studies should address the fact this apparently better cardiovascular health status in sexual minority men may actually be driven by a sustained catabolic state that presents with lower BMI than in MSW but may result in poorer CVD outcomes in the long term. The role of proposed biobehavioral markers, such as cortisol, should be explored among sexual minority populations presenting with the obesity paradox.
Supplemental Material
Supplemental material, sj-pdf-1-jmh-10.1177_15579883221095387 for Paradoxical Obesity and Overweight Disparities Among Sexual Minority Men: A Meta-Analysis by Humberto López Castillo, Christopher W. Blackwell and Eric W. Schrimshaw in American Journal of Men’s Health
Acknowledgments
One of the contributors who met the criteria for authorship did not wish to accept authorship of this article citing religious beliefs and has been excluded from authorship at their request and after agreement with the Publisher and author group. The authors would like to thank volunteer students Daniel Vitellaro, Alex Zamora, and Fabiola Ayala-Cardona for their help validating the initial keyword search. The authors also thank Ivan Bahamon, MPH; Noé Navarro, Jr., BS; and Daniel Vitellaro, BS, for their valuable help during the final manuscript screening process. The authors also would like to acknowledge Kim Hong and Camila Diez for their role conducting external data quality assurance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Humberto López Castillo  https://orcid.org/0000-0003-4604-0887
https://orcid.org/0000-0003-4604-0887
Supplemental Material: Supplemental material for this article is available online.
References
References marked with an asterisk (*) correspond to studies included in the meta-analysis.
- Althubaiti A. (2016). Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 9, 211–217. 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonopoulos A. S., Tousoulis D. (2017). The molecular mechanisms of obesity paradox. Cardiovascular Research, 113(9), 1074–1086. 10.1093/cvr/cvx106 [DOI] [PubMed] [Google Scholar]
- *Austin S. B., Ziyadeh N. J., Corliss H. L., Haines J., Rockett H. R., Wypij D., Field A. E. (2009). Sexual orientation disparities in weight status in adolescence: Findings from a prospective study. Obesity, 17(9), 1776–1782. 10.1038/oby.2009.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Azagba S., Shan L., Latham K. (2019). Overweight and obesity among sexual minority adults in the United States. International Journal of Environmental Research and Public Health, 16(10), 1828. 10.3390/ijerph16101828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bankoff S. M., Richards L. K., Bartlett B., Wolf E. J., Mitchell K. S. (2016). Examining weight and eating behavior by sexual orientation in a sample of male veterans. Comprehensive Psychiatry, 68, 134–139. 10.1016/j.comppsych.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Beach L. B., Elasy T. A., Gonzales G. (2018). Prevalence of self-reported diabetes by sexual orientation: Results from the 2014 Behavioral Risk Factor Surveillance System. LGBT Health, 5(2), 121–130. 10.1089/lgbt.2017.0091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Blosnich J. R., Farmer G. W., Lee J. G., Silenzio V. M., Bowen D. J. (2014). Health inequalities among sexual minority adults: Evidence from ten U.S. states, 2010. American Journal of Preventive Medicine, 46(4), 337–349. 10.1016/j.amepre.2013.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Blosnich J. R., Hanmer J., Yu L., Matthews D. D., Kavalieratos D. (2016). Health care use, health behaviors, and medical conditions among individuals in same-sex and opposite-sex partnerships: A cross-sectional observational analysis of the Medical Expenditures Panel Survey (MEPS), 2003-2011. Medical Care, 54(6), 547–554. 10.1097/MLR.0000000000000529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Boehmer U., Miao X., Linkletter C., Clark M. A. (2014). Health conditions in younger, middle, and older ages: are there differences by sexual orientation? LGBT Health, 1(3), 168–176. 10.1089/lgbt.2013.0033 [DOI] [PubMed] [Google Scholar]
- *Boehmer U., Miao X., Ozonoff A. (2012). Health behaviors of cancer survivors of different sexual orientations. Cancer Causes & Control, 23(9), 1489–1496. 10.1007/s10552-012-0023-x [DOI] [PubMed] [Google Scholar]
- *Brennan D. J., Ross L. E., Dobinson C., Veldhuizen S., Steele L. S. (2010). Men’s sexual orientation and health in Canada. Canadian Journal of Public Health, 101(3), 255–258. 10.1007/bf03404385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Brown T. A., Keel P. K. (2015). Relationship status predicts lower restrictive eating pathology for bisexual and gay men across 10-year follow-up. The International Journal of Eating Disorders, 48(6), 700–707. 10.1002/eat.22433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Caceres B. A., Ancheta A. J., Dorsen C., Newlin-Lew K., Edmondson D., Hughes T. L. (2022). A population-based study of the intersection of sexual identity and race/ethnicity on physiological risk factors for CVD among U.S. adults (ages 18-59). Ethnicity & Health, 27, 617–638. 10.1080/13557858.2020.1740174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Caceres B. A., Brody A. A., Halkitis P. N., Dorsen C., Yu G., Chyun D. A. (2018). Sexual orientation differences in modifiable risk factors for cardiovascular disease and cardiovascular disease diagnoses in men. LGBT Health, 5(5), 284–294. 10.1089/lgbt.2017.0220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caceres B. A., Brody A. A., Luscombe R. E., Primiano J. E., Marusca P., Sitts E. M., Chyun D. (2017). A systematic review of cardiovascular disease in sexual minorities. American Journal of Public Health, 107(4), e13–e21. 10.2105/AJPH.2016.303630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Caceres B. A., Makarem N., Hickey K. T., Hughes T. L. (2019). Cardiovascular disease disparities in sexual minority adults: An examination of the Behavioral Risk Factor Surveillance System (2014-2016). American Journal of Health Promotion, 33(4), 576–585. 10.1177/0890117118810246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caceres B. A., Streed C. G., Jr., Corliss H. L., Lloyd-Jones D. M., Matthews P. A., Mukherjee M., Poteat T., Rosendale N., Ross L. M., & American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Hypertension; Council on Lifestyle and Cardiometabolic Health; Council on Peripheral Vascular Disease; and Stroke Council. (2020). Assessing and addressing cardiovascular health in LGBTQ adults: A scientific statement from the American Heart Association. Circulation, 142(19), e321–e332. 10.1161/CIR.0000000000000914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Calzo J. P., Austin S. B., Micali N. (2018). Sexual orientation disparities in eating disorder symptoms among adolescent boys and girls in the UK. European Child & Adolescent Psychiatry, 27(11), 1483–1490. 10.1007/s00787-018-1145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzo J. P., Corliss H. L., Blood E. A., Field A. E., Austin S. B. (2013). Development of muscularity and weight concerns in heterosexual and sexual minority males. Health Psychology, 32(1), 42–51. 10.1037/a0028964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbone S., Canada J. M., Billingsley H. E., Siddiqui M. S., Elagizi A., Lavie C. J. (2019). Obesity paradox in cardiovascular disease: Where do we stand? Vascular Health and Risk Management, 15, 89–100. 10.2147/VHRM.S168946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022, January 12). HIV and men. https://www.cdc.gov/hiv/group/gender/men/index.html
- Cohen J. (1968). Weighted kappa: Nominal scale agreement with provision for scaled disagreement or partial credit. Psychological Bulletin, 70(4), 213–220. 10.1037/h0026256 [DOI] [PubMed] [Google Scholar]
- *Conner M., Johnson C., Grogan S. (2004). Gender, sexuality, body image and eating behaviours. Journal of Health Psychology, 9(4), 505–515. 10.1177/1359105304044034 [DOI] [PubMed] [Google Scholar]
- Connor Gorber S., Tremblay M., Moher D., Gorber B. (2007). A comparison of direct vs. Self-report measures for assessing height, weight and body mass index: A systematic review. Obesity Reviews, 8(4), 307–326. 10.1111/j.1467-789X.2007.00347.x [DOI] [PubMed] [Google Scholar]
- *Conron K. J., Mimiaga M. J., Landers S. J. (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100(10), 1953–1960. 10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H., Alsalhe T. A., Chalghaf N., Ricco M., Bragazzi N. L., Wu J. (2020). The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PLOS MEDICINE, 17(7), Article e1003198. 10.1371/journal.pmed.1003198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Davids C. M., Green M. A. (2011). A preliminary investigation of body dissatisfaction and eating disorder symptomatology with bisexual individuals. Sex Roles, 65(7–8), 533–547. 10.1007/s11199-011-9963-y [DOI] [Google Scholar]
- *Deputy N. P., Boehmer U. (2010). Determinants of body weight among men of different sexual orientation. Preventive Medicine, 51(2), 129–131. 10.1016/j.ypmed.2010.05.010 [DOI] [PubMed] [Google Scholar]
- *Deputy N. P., Boehmer U. (2014). Weight status and sexual orientation: Differences by age and within racial and ethnic subgroups. American Journal of Public Health, 104(1), 103–109. 10.2105/AJPH.2013.301391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deurenberg P., Deurenberg-Yap M., Guricci S. (2002). Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obesity Reviews, 3(3), 141–146. 10.1046/j.1467-789x.2002.00065.x [DOI] [PubMed] [Google Scholar]
- *Dilley J. A., Simmons K. W., Boysun M. J., Pizacani B. A., Stark M. J. (2010). Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. American Journal of Public Health, 100(3), 460–467. 10.2105/AJPH.2007.130336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elagizi A., Kachur S., Lavie C. J., Carbone S., Pandey A., Ortega F. B., Milani R. V. (2018). An Overview and update on obesity and the obesity paradox in cardiovascular diseases. Progress in Cardiovascular Diseases, 61(2), 142–150. 10.1016/j.pcad.2018.07.003 [DOI] [PubMed] [Google Scholar]
- *Epel E. S., Spanakos A., Kasl-Godley J., Brownell K. D. (1996). Body shape ideals across gender, sexual orientation, socioeconomic status, race, and age in personal advertisements. The International Journal of Eating Disorders, 19(3), 265–273. [DOI] [PubMed] [Google Scholar]
- *Everett B., Mollborn S. (2013). Differences in hypertension by sexual orientation among U.S. young adults. Journal of Community Health, 38(3), 588–596. 10.1007/s10900-013-9655-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K. M., Kit B. K., Orpana H., Graubard B. I. (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. Journal of the American Medical Association, 309(1), 71–82. 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flentje A., Heck N. C., Brennan J. M., Meyer I. H. (2020). The relationship between minority stress and biological outcomes: A systematic review. Journal of Behavioral Medicine, 43(5), 673–694. 10.1007/s10865-019-00120-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Frederick D. A., Essayli J. H. (2016). Male body image: The roles of sexual orientation and body mass index across five national U.S. studies. Psychology of Men & Masculinity, 17(4), 336–351. 10.1037/men0000031 [DOI] [Google Scholar]
- *Fredriksen-Goldsen K. I., Kim H. J., Barkan S. E., Muraco A., Hoy-Ellis C. P. (2013). Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health, 103(10), 1802–1809. 10.2105/AJPH.2012.301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Fricke J., Gordon N., Downing J. (2019). Sexual orientation disparities in physical activity: Results from insured adults in California. Medical Care, 57(2), 138–144. 10.1097/MLR.0000000000001017 [DOI] [PubMed] [Google Scholar]
- *Fricke J., Sironi M. (2020). Sexual fluidity and BMI, obesity, and physical activity. SSM Population Health, 11, 100620. 10.1016/j.ssmph.2020.100620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Frisch M., Zdravkovic S. (2010). Body size at birth and same-sex marriage in young adulthood. Archives of Sexual Behavior, 39(1), 117–123. 10.1007/s10508-008-9408-z [DOI] [PubMed] [Google Scholar]
- Frost D. M., Lehavot K., Meyer I. H. (2015). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 38(1), 1–8. 10.1007/s10865-013-9523-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryar C. D., Carroll M. D., Ogden C. L. (2018). Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960-1962 through 2015-2016. https://www.cdc.gov/nchs/data/hestat/obesity_adult_15_16/obesity_adult_15_16.pdf
- Fulton M., Srinivasan V. N. (2021). Obesity, stigma and discrimination. StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/32119458 [PubMed]
- *Garland-Forshee R. Y., Fiala S. C., Ngo D. L., Moseley K. (2014). Sexual orientation and sex differences in adult chronic conditions, health risk factors, and protective health practices, Oregon, 2005-2008. Preventing Chronic Disease, 11, 140126. 10.5888/pcd11.140126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gonzales G., Henning-Smith C. (2017). Health disparities by sexual orientation: Results and implications from the Behavioral Risk Factor Surveillance System. Journal of Community Health, 42(6), 1163–1172. 10.1007/s10900-017-0366-z [DOI] [PubMed] [Google Scholar]
- *Gorman B. K., Denney J. T., Dowdy H., Medeiros R. A. (2015). A new piece of the puzzle: Sexual orientation, gender, and physical health status. Demography, 52(4), 1357–1382. 10.1007/s13524-015-0406-1 [DOI] [PubMed] [Google Scholar]
- Grasso C., Goldhammer H., Funk D., King D., Reisner S. L., Mayer K. H., Keuroghlian A. S. (2019). Required sexual orientation and gender identity reporting by US health centers: First-year data. American Journal of Public Health, 109(8), 1111–1118. 10.2105/AJPH.2019.305130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunfeld C., Saag M., Cofrancesco J., Jr., Lewis C. E., Kronmal R., Heymsfield S., Tien P. C., Bacchetti P., Shlipak M., Scherzer R., & Study of Fat Redistribution Metabolic Change in HIV Infection (FRAM). (2010). Regional adipose tissue measured by MRI over 5 years in HIV-infected and control participants indicates persistence of HIV-associated lipoatrophy. AIDS, 24(11), 1717–1726. 10.1097/QAD.0b013e32833ac7a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C. M., Carroll M. D., Fryar C. D., Ogden C. L. (2017). Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief, (288), 1–8. https://www.ncbi.nlm.nih.gov/pubmed/29155689 [PubMed]
- Hammer G. P., du Prel J. B., Blettner M. (2009). Avoiding bias in observational studies: Part 8 in a series of articles on evaluation of scientific publications. Deutsches Ärzteblatt International, 106(41), 664–668. 10.3238/arztebl.2009.0664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hatzenbuehler M. L., McLaughlin K. A., Slopen N. (2013). Sexual orientation disparities in cardiovascular biomarkers among young adults. American Journal of Preventive Medicine, 44(6), 612–621. 10.1016/j.amepre.2013.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Heck J. E., Jacobson J. S. (2006). Asthma diagnosis among individuals in same-sex relationships. The Journal of Asthma, 43(8), 579–584. 10.1080/02770900600878289 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Altman D. G., Gotzsche P. C., Juni P., Moher D., Oxman A. D., Savovic J., Schulz K. F., Weeks L., Sterne J. A., Cochrane Bias Methods G., Cochrane Statistical Methods G. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holsti O. R. (1969). Content analysis for the social sciences and humanities. Addison-Wesley. [Google Scholar]
- Huebner D. M., McGarrity L. A., Perry N. S., Spivey L. A., Smith T. W. (2021). Cardiovascular and cortisol responses to experimentally-induced minority stress. Health Psychology, 40(5), 316–325. 10.1037/hea0001067 [DOI] [PubMed] [Google Scholar]
- Jackson A. S., Stanforth P. R., Gagnon J., Rankinen T., Leon A. S., Rao D. C., Skinner J. S., Bouchard C., Wilmore J. H. (2002). The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. International Journal of Obesity and Related Metabolic Disorders, 26(6), 789–796. 10.1038/sj.ijo.0802006 [DOI] [PubMed] [Google Scholar]
- *Jackson C. L., Agénor M., Johnson D. A., Austin S. B., Kawachi I. (2016). Sexual orientation identity disparities in health behaviors, outcomes, and services use among men and women in the United States: A cross-sectional study. BMC Public Health, 16(1), Article 807. 10.1186/s12889-016-3467-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Laska M. N., VanKim N. A., Erickson D. J., Lust K., Eisenberg M. E., Rosser B. R. (2015). Disparities in weight and weight behaviors by sexual orientation in college students. American Journal of Public Health, 105(1), 111–121. 10.2105/AJPH.2014.302094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legate N., Rogge R. D. (2019). Identifying basic classes of sexual orientation with latent profile analysis: Developing the multivariate sexual orientation classification system. Archives of Sexual Behavior, 48(5), 1403–1422. 10.1007/s10508-018-1336-y [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gotzsche P. C., Ioannidis J. P., Clarke M., Devereaux P. J., Kleijnen J., Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Journal of Clinical Epidemiology, 62(10), e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- Lin L., Chu H. (2018). Quantifying publication bias in meta-analysis. Biometrics, 74(3), 785–794. 10.1111/biom.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Castillo H., Tfirn I. C., Hegarty E., Bahamon I., Lescano C. M. (2021). A meta-analysis of blood pressure disparities among sexual minority men. LGBT Health, 8(2), 91–106. 10.1089/lgbt.2019.0121 [DOI] [PubMed] [Google Scholar]
- Maukonen M., Männistö S., Tolonen H. (2018). A comparison of measured versus self-reported anthropometrics for assessing obesity in adults: A literature review. Scandinavian Journal of Public Health, 46(5), 565–579. 10.1177/1403494818761971 [DOI] [PubMed] [Google Scholar]
- Meneguzzo P., Collantoni E., Bonello E., Vergine M., Behrens S. C., Tenconi E., Favaro A. (2021). The role of sexual orientation in the relationships between body perception, body weight dissatisfaction, physical comparison, and eating psychopathology in the cisgender population. Eating and Weight Disorders, 26(6), 1985–2000. 10.1007/s40519-020-01047-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nduka C. U., Uthman O. A., Kimani P. K., Stranges S. (2016). Body fat changes in people living with HIV on antiretroviral therapy. AIDS Reviews, 18(4), 198–211. [PubMed] [Google Scholar]
- *Newlin Lew K., Dorsen C., Long T. (2018). Prevalence of obesity, prediabetes, and diabetes in sexual minority men: Results from the 2014 Behavioral Risk Factor Surveillance System. The Diabetes Educator, 44(1), 83–93. 10.1177/0145721717749943 [DOI] [PubMed] [Google Scholar]
- Nimptsch K., Konigorski S., Pischon T. (2019). Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism, 92, 61–70. 10.1016/j.metabol.2018.12.006 [DOI] [PubMed] [Google Scholar]
- *Nyitray A. G., Peng F., Day R. S., Carvalho Da, Silva R. J., Baggio M. L., Salmerón J., Quiterio M., Abrahamsen M., Lazcano-Ponce E., Villa L. L., Giuliano A. R. (2019). The association between body mass index and anal canal human papillomavirus prevalence and persistence: The HIM study. Human Vaccines & Immunotherapeutics, 15(7–8), 1911–1919. 10.1080/21645515.2019.1593083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreopoulos A., Kalantar-Zadeh K., McAlister F. A., Ezekowitz J. A., Fonarow G. C., Johnson J. A., Norris C. M., Padwal R. S. (2010). Comparison of direct body composition assessment methods in patients with chronic heart failure. Journal of Cardiac Failure, 16(11), 867–872. 10.1016/j.cardfail.2010.06.416 [DOI] [PubMed] [Google Scholar]
- Puhl R. M., Himmelstein M. S., Pearl R. L., Wojtanowski A. C., Foster G. D. (2019). Weight stigma among sexual minority adults: Findings from a matched sample of adults engaged in weight management. Obesity, 27(11), 1906–1915. 10.1002/oby.22633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purnell J. Q. (2000). Definitions, classification, and epidemiology of obesity. In Feingold K. R., Anawalt B., Boyce A., Chrousos G., de Herder W. W., Dhatariya K., Dungan K., Grossman A., Hershman J. M., Hofland J., Kalra S., Kaltsas G., Koch C., Kopp P., Korbonits M., Kovacs C. S., Kuohung W., Laferrere B., McGee E. A., McLachlan R., Morley J. E., New M., Purnell J., Sahay R., Singer F., Stratakis C. A., Trence D. L., Wilson D. P. (Eds.), Endotext. https://www.ncbi.nlm.nih.gov/pubmed/25905390
- *Rosario M., Li F., Wypij D., Roberts A. L., Corliss H. L., Charlton B. M., Frazier A. L., Austin S. B. (2016). Disparities by sexual orientation in frequent engagement in cancer-related risk behaviors: A 12-year follow-up. American Journal of Public Health, 106(4), 698–706. 10.2105/AJPH.2015.302977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S., Brown T. T. (2000). Lipid disorders in people with HIV. In Feingold K. R., Anawalt B., Boyce A., Chrousos G., de Herder W. W., Dhatariya K., Dungan K., Grossman A., Hershman J. M., Hofland J., Kalra S., Kaltsas G., Koch C., Kopp P., Korbonits M., Kovacs C. S., Kuohung W., Laferrère B., McGee E. A., McLachlan R., Morley J. E., New M., Purnell J., Sahay R., Singer F., Stratakis C. A., Trence D. L., Wilson D. P. (Eds.), Endotext. https://www.ncbi.nlm.nih.gov/books/NBK567198/
- Shlay J. C., Bartsch G., Peng G., Wang J., Grunfeld C., Gibert C. L., Visnegarwala F., Raghavan S. S., Xiang Y., Farrough M., Perry H. E., Kotler D., El-Sadr W. M. (2007). Long-term body composition and metabolic changes in antiretroviral naive persons randomized to protease inhibitor-, nonnucleoside reverse transcriptase inhibitor-, or protease inhibitor plus nonnucleoside reverse transcriptase inhibitor-based strategy. Journal of Acquired Immune Deficiency Syndromes, 44(5), 506–517. 10.1097/QAI.0b013e31804216cf [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A., Fayosse A., Sabia S., Tabak A., Shipley M., Dugravot A., Kivimaki M. (2018). Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: A cohort study. PLOS MEDICINE, 15(5), Article e1002571. 10.1371/journal.pmed.1002571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley T. L., Grinspoon S. K. (2012). Body composition and metabolic changes in HIV-infected patients. The Journal of Infectious Diseases, 205(Suppl. 3), S383–S390. 10.1093/infdis/jis205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne J. A. C., Sutton A. J., Ioannidis J. P. A., Terrin N., Jones D. R., Lau J., Carpenter J., Rücker G., Harbord R. M., Schmid C. H., Tetzlaff J., Deeks J. J., Peters J., Macaskill P., Schwarzer G., Duval S., Altman D. G., Moher D., Higgins J. P. T. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. British Medical Journal, 343, d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- *Strutz K. L., Herring A. H., Halpern C. T. (2015). Health disparities among young adult sexual minorities in the U.S. American Journal of Preventive Medicine, 48(1), 76–88. 10.1016/j.amepre.2014.07.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Stupplebeen D. A., Eliason M. J., LeBlanc A. J., Sanchez-Vaznaugh E. V. (2019). Differential influence of weight status on chronic diseases by reported sexual orientation identity in men. LGBT Health, 6(3), 126–133. 10.1089/lgbt.2018.0167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Trinh M. H., Agénor M., Austin S. B., Jackson C. L. (2017). Health and healthcare disparities among U.S. women and men at the intersection of sexual orientation and race/ethnicity: A nationally representative cross-sectional study. BMC Public Health, 17(1), Article 964. 10.1186/s12889-017-4937-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tuthill Z., Denney J. T., Gorman B. (2020). Racial disparities in health and health behaviors among gay, lesbian, bisexual and heterosexual men and women in the BRFSS-SOP. Ethnicity & Health, 25(2), 177–188. 10.1080/13557858.2017.1414157 [DOI] [PubMed] [Google Scholar]
- *VanKim N. A., Eisenberg M. E., Erickson D. J., Lust K., Laska M. N. (2020). College climate and sexual orientation differences in weight status. Prevention Science, 21(3), 422–433. 10.1007/s11121-019-01061-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanKim N. A., Laska M. N. (2021). Sexual orientation and obesity: What do we know? Current Obesity Reports, 10(4), 453–457. 10.1007/s13679-021-00454-w [DOI] [PubMed] [Google Scholar]
- Warren J. C., Smalley K. B., Barefoot K. N. (2016). Differences in psychosocial predictors of obesity among LGBT subgroups. LGBT Health, 3(4), 283–291. 10.1089/lgbt.2015.0076 [DOI] [PubMed] [Google Scholar]
- WHO. (2020). Obesity and overweight: Key facts. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Wolff M., Wells B., Ventura-DiPersia C., Renson A., Grov C. (2017). Measuring sexual orientation: A review and critique of U.S. data collection efforts and implications for health policy. Journal of Sex Research, 54(4–5), 507–531. 10.1080/00224499.2016.1255872 [DOI] [PubMed] [Google Scholar]
- *Wolstein J., Charles S. A., Babey S. H., Diamant A. L. (2018). Disparities in health care access and health among lesbians, gay men, and bisexuals in California. Policy Brief (UCLA Center for Health Policy Research), 2018(9), 1–8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jmh-10.1177_15579883221095387 for Paradoxical Obesity and Overweight Disparities Among Sexual Minority Men: A Meta-Analysis by Humberto López Castillo, Christopher W. Blackwell and Eric W. Schrimshaw in American Journal of Men’s Health