Summary
In 2014, Buysse published a novel definition of sleep health, raising awareness for the importance of this construct for individuals, populations, clinical care, and research. However, the original definition focused on adults, with the recommendation that it should be adapted for children and adolescents. As children live within a complex and dynamic system, and may not always have control over their own sleep, this theoretical review will examine and apply Buysse’s five dimensions of sleep health within the context of pediatrics. In addition, using examples from the pediatric sleep literature we introduce a modified definition that takes into consideration the influence of the socio-ecological system within which children live, and the sleep-related behaviors that are critical in supporting or hindering sleep health. Finally, we discuss how the proposed theoretical framework, Peds B-SATED, can be applied to clinical practice, research, and training in the field of pediatric sleep.
Keywords: Infant, Toddler, School-age children, Adolescents, Duration, Timing, Sleep-efficiency, Sleepiness, Sleep-related behaviors
Introduction
In 2014, Buysse published his seminal paper titled “Sleep Health: Can We Define It? Does It Matter?“ [1] He defined sleep health as “a multidimensional pattern of sleep-wakefulness, adapted to individual, social, and environmental demands, that promotes physical and mental wellbeing. Good sleep health is characterized by subjective satisfaction, appropriate timing, adequate duration, high efficiency, and sustained alertness during waking hours” (p. 12). This definition expresses sleep as a positive attribute, with a focus on how well an individual or population sleeps rather than on sleep disorders or sleep disturbances. It provides targets for health promotion and prevention, again in contrast to treatment of disorders that aims to reduce symptoms. Sleep health also can be considered within the broader context of population health and allows for a focus on health promotion at many levels, including individuals, communities, and populations. Finally, it can be measured both subjectively and objectively, along a continuum from low to high levels, and acknowledges that sleep health may be different across situations and individuals.
Notably, Buysse (2014) states that this definition is “most appropriate for adults, but could be adapted to infants, children, and adolescents” (p. 12). This is an important point as, unlike adults who may have significant control over their sleep health, children and adolescents (birth to 18 years) live within a complex and dynamic system that exerts significant influence over their sleep health of which they have minimal control. In this theoretical review we examine and apply Buysse’s five dimensions of sleep health within the context of pediatrics, and then introduce a modified definition that includes the influence of the socio-ecological system within which children live and the sleep-related behaviors that are critical in supporting or hindering sleep health.
Researchers have previously used socio-ecological and systems frameworks to understand the etiology of sleep patterns and problems in children [2–4]. Within a socio-ecological framework [5] (Fig. 1), factors at different levels of the social ecology, including characteristics of the individual child (microsystem), the family and school environments (mesosystem), and the broader neighborhood and socio-cultural context (macrosystem), may independently or interactively contribute to aspects of pediatric sleep health, as well as the development of pediatric sleep problems [6]. Contributing factors at each socio-ecological level shown in Fig. 1 are not an exhaustive list, but reflect a growing body of research on correlates of and contributors to poor pediatric sleep health. These factors may be conceptualized as being proximally or distally linked to pediatric sleep health domains. Individual factors, such as neurodevelopmental or behavioral health status [7,8], and family factors, including parenting behaviors and family functioning [3,9], may be more proximal factors influencing child sleep health, compared to distal factors such as neighborhood amenities, green space, light, and noise [10]. However, factors at multiple socio-ecological levels likely interact in nuanced and complex ways to influence pediatric sleep health over time. For instance, living in a disadvantaged neighborhood or being of lower socioeconomic status (SES) have been cross-sectionally and longitudinally associated with insufficient and poor-quality pediatric sleep [10–13], but these linkages can vary in magnitude and direction according to additional individual and family factors [14].
Fig. 1.
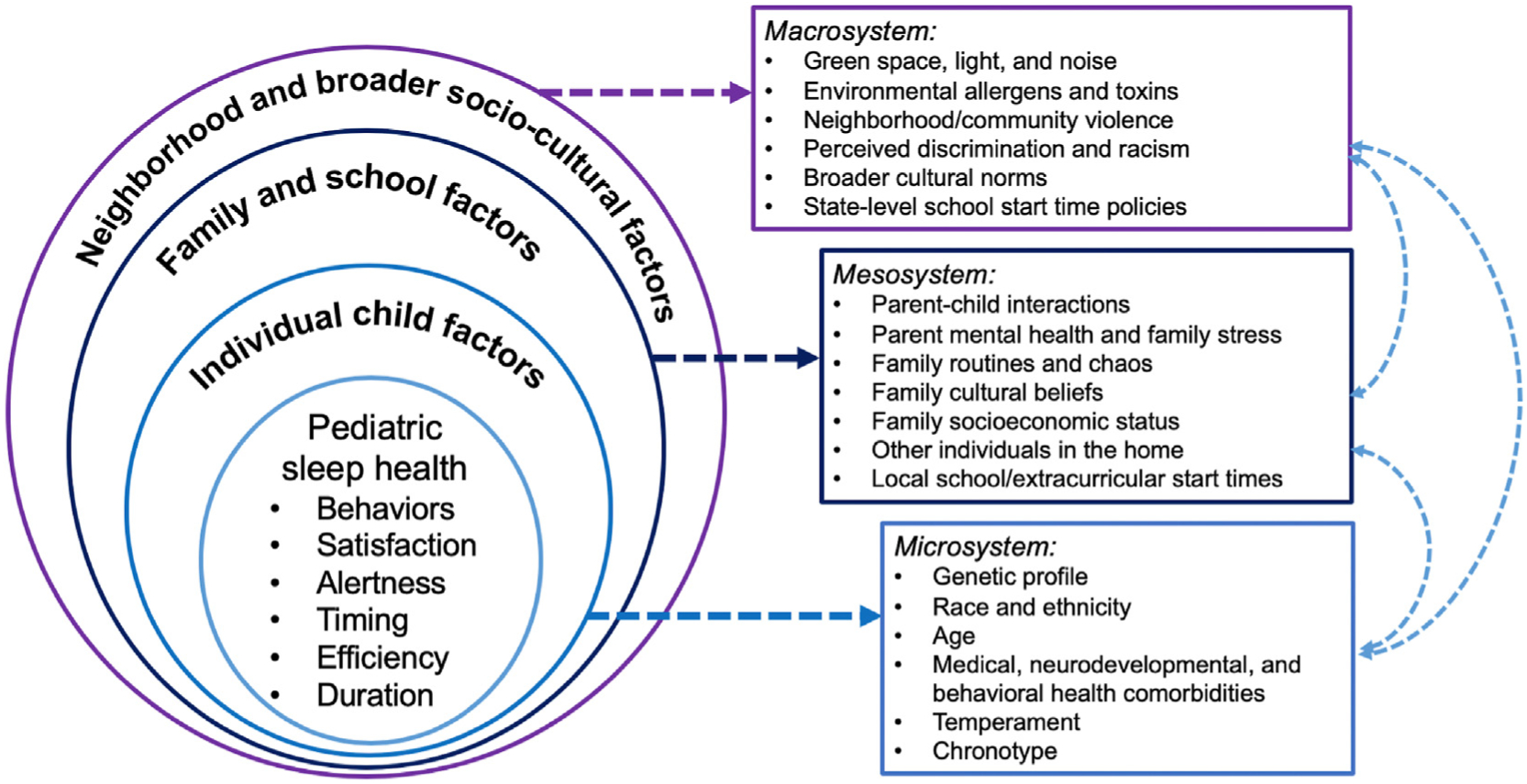
Socio-ecological factors hypothesized to contribute to pediatric sleep health domains.
Furthermore, the salience of different socio-ecological factors may change across developmental stage. For example, a difficult temperament or medical conditions such as reflux in infancy could contribute to challenging parent–child interactions around sleep and sleep disruption in early childhood [3], but these factors are less likely to be a concern in school-aged children or adolescents. In contrast, a later secondary school start time policy may directly increase the sleep duration of adolescents [15], with little to no impact on infants and toddlers. Factors may also interact differently or synergistically at various points in development. For instance, both parental enforcement of bedtimes [16–18] and later school start times [19, 20] benefit adolescent sleep, which in turn impacts adolescent mood, whereas pathways between parenting practices, the school setting, and child sleep and mood outcomes may differ earlier in development.
In addition to considering sleep across different developmental stages, child development is also a dynamic process, with critical and sensitive periods from infancy through adolescence. As such, there may be cascading and bidirectional effects among sleep problems, socio-ecological factors, and child well-being. For example, longitudinal research suggests that self-regulation deficits and sleep problems may interact during early childhood with downstream impacts on attention and school functioning [21,22]. Although more research is needed, it is also possible that the consequences of insufficient sleep, such as emotion-regulation deficits [23] and irritability [24], may impact how youth interact with their social ecology (e.g., peers, teachers, caregivers), leading to cascading adverse outcomes.
Dimensions of pediatric sleep health
With the socio-ecological framework in mind, we now turn to the sleep health dimensions proposed by Buysse. In his paper, he proposes the acronym SATED as a way to quickly assess the different dimensions of sleep health: Satisfaction with sleep, Alertness during waking hours, Timing of sleep, sleep Efficiency, and sleep Duration. He also argues that Regularity is important for treatment, but is less clearly associated with poor health outcomes. Recent studies have examined the psychometric properties of both the five-item SATED questionnaire [25] and the six-item RU SATED questionnaire, which was modified to also include sleep regularity [26,27]. However, two of these studies reported weak psychometric findings [26,27]. Other studies have created operational definitions for the dimensions of Buysse’s sleep health dimensions, including one for adolescents [28], as well as explored potential new measures of different sleep health dimensions [29,30].
In the following sections, we highlight how all five dimensions as initially described by Buysse are also applicable for pediatric sleep health, providing considerations and differences for pediatrics (with a summary found in Table 1). This is followed by our proposal that regularity is part of a larger dimension that is highly relevant for pediatrics, namely sleep-related Behaviors, resulting in a six-factor model: Peds B-SATED. Because sleep duration is the first aspect of sleep most people consider when thinking about sleep health, and sleep duration is increasingly being viewed as a public health outcome [15,31–33], we will start with a discussion of how this dimension of pediatric sleep health is similar to and different from adults.
Table 1.
Reconceptualizing sleep health for pediatric populations.
| Sleep health domains | Buysse (2014) definition | Pediatric considerations |
|---|---|---|
| Satisfaction/quality | A subjective assessment of “good” or “poor” sleep |
|
| Alertness/Sleepiness/Napping | The ability to maintain attentive wakefulness |
|
| Timing | The placement of sleep within the 24-h day |
|
| Efficiency (continuity) | The ease of falling asleep and returning to sleep |
|
| Duration | The total amount of sleep obtained per 24 h |
|
| Behaviors (*additional dimension not included in Buysse’s 2014 paper) | Not applicable |
|
Sleep duration: The total amount of sleep obtained per 24 h
Similar to adults there is a recommended optimal range of sleep duration to promote health in pediatrics. As seen in Table 2, optimal sleep duration has been linearly associated with health outcomes across psychological/social, cognitive/academic, and physical health domains in a number of studies. Unlike adults, however, recommended hours of sleep changes across development, as highlighted by pediatric guidelines from the American Academy of Sleep Medicine [34]. This consensus statement describes how sufficient sleep duration (within the recommended range for age) is associated with optimal physical and mental health outcomes, including improved attention, behavior, learning, memory, emotion regulation, and quality of life; while sleep duration outside this range (not enough sleep or too much sleep) is associated with inattention, behavior and learning problems, increased risk of accidents and injuries, hypertension, obesity, diabetes, and mental health problems [34].
Table 2.
Examples of research investigating pediatric sleep health and well-being domains.
| Sleep health domains | Example citations linking sleep and well-being domains(126) | |
|---|---|---|
| Satisfaction/quality (subjective) | Psychological/social | Kelly & El-Shiekh [148]; Lovato & Gradisar [149] |
| Cognitive/academic | Bub et al. [150]; Friedman et al. [151] | |
| Physical health | Dutil & Chaput; [152] Matthews & Pantesco [52] | |
| Alertness/sleepiness/napping | Psychological/social | Berger et al. [23]; El-Shiekh et al., 2013 [153]; Hash et al. [154] |
| Cognitive/academic | Cremone et al. [155]; Dewald et al.; [51] Miller et al. [156] | |
| Physical health | Matthews & Pantesco [52] | |
| Timing | Psychological/social | Short et al. [16]; Gangswisch et al. [17]; Peltz et al. [18] |
| Cognitive/academic | Hoyniak et al. [157] | |
| Physical health | Hart et al. [158]; Matthews & Pantesco [52] | |
| Efficiency (continuity) | Psychological/social | Reynaud et al. [49] |
| Cognitive/academic | Astill et al. [50]; Dewald et al. [51] | |
| Physical health | Matthews & Pantesco [52] | |
| Duration | Psychological/social | Astill et al. [50]; Chaput et al., 2016 [159] & 2017 [160]; Reynaud et al. [49] |
| Cognitive/academic | Astill et al.; [50] Dewald et al.; [51] Short et al. [161] | |
| Physical health | Chaput et al., 2016 [159] & 2017 [160]; Magee & Hale [162]; Matthews & Pantesco [52]; Quist et al. [163] | |
| Behaviors | Psychological/social | Becker et al. [IIV] [89]; Lemola et al. [electronics] [164]; Mindell et al. [bedtime routines] [165] |
| Cognitive/academic | Becker et al. [IIV] [89] | |
| Physical health | Becker et al. [IIV] [89]; Lee et al. [bedtime routines/schedules] [166]; Seifert et al. [caffeine] [167] |
Note. Where possible, we cite meta-analytic research on these linkages, which appears in bold. As in Buysse’s(1) table illustrating associations between adult sleep health domains and relevant outcomes, this table is not meant to serve as an exhaustive list. Psychological/social domain includes social-emotional functioning, behavioral functioning, and internalizing/externalizing conditions; cognitive/academic domain include executive functioning skills, intelligence, and academic/school performance; physical domain includes weight gain, adiposity, and cardiometabolic risks. IIV = intraindividual variability. “Efficiency” domain includes studies referring to actigraphic sleep efficiency as an indicator of “quality.”
One of the striking differences between sleep duration in adults and pediatrics is the wide range of recommended hours, from 12 to 16 h for infants to 8–10 h for adolescents [34], and that sleep duration needs are constantly changing, with 5 different guidelines between the ages of 4 months and 18 years [34]. Increased family education around sleep duration guidelines and how these change as children age is necessary to promote healthy sleep over time [34]. In addition, 24-h sleep duration in young children includes both developmentally-appropriate daytime naps and nighttime sleep. Thus, it is essential for health care providers and families to have a strong understanding of what is age-appropriate not only for total sleep duration, but also for the frequency and duration of naps in early development.
One shortcoming of the recommended hours of sleep duration in pediatrics is that these values are based on either studies of actual sleep (how much sleep children and adolescents are currently getting) or, more often, sleep opportunity (the amount of time between bedtime and wake time that children try to sleep). While it has been shown that adolescents have an average biological sleep need of ~9.3 h per night [35], no controlled studies have examined the sleep need of pre-pubertal children. Thus, additional research is essential that clearly defines sleep need in order to provide the most accurate recommendations of sleep duration in pediatrics. Indeed, there is a growing body of research suggesting that both insufficient sleep and excessive sleep duration are associated with poor functioning [36–39]. For instance, studies have found a curvilinear association between sleep duration and child outcomes, such that children with longer sleep durations, outside the recommended range [37,38], demonstrate poorer cognitive and behavioral functioning. Research that better identifies optimal thresholds for child sleep duration and examines the impact of both short and long sleep on functioning is needed.
Additionally, as seen in Fig. 1, it is important to recognize that current sleep recommendations that are based on actual sleep are likely influenced by individual (e.g., neurodevelopment [7], race/ethnicity [40, 41]), family/school (e.g., parent set bedtimes [16,17], school start times) and broader socio-cultural and environmental factors (e.g., perceived discrimination [42], neighborhood violence [43, 44]).
Finally, it is not clear that the current recommendations for sleep duration are representative of all children. For example, racial differences in napping patterns have been found (e.g., Black or African American children stop napping at an older age than non-Latinx White children [45]). However, there is some question about whether 24-h sleep duration actually differs between Black or African American and non-Latinx White children, as the increase in naps may be associated with decreased nocturnal sleep, potentially in a bidirectional relationship [46]. Furthermore, there are racial/ethnic disparities in pediatric sleep duration, such that non-Latinx white youth are more likely to obtain sufficient sleep relative to their Black or African American and Latinx peers [40,41]. Examining additional cultural and socio-ecological factors that may account for these noted disparities is important to better understand sleep needs across different pediatric populations. Similarly, it is unclear if there are different sleep needs for children around the world, or whether differences in sleep duration are more a result of cultural practices rather than biological need. For example, studies have found differences of up to 1.5 h in obtained sleep in young children in countries such as Japan and Korea compared to New Zealand and United Kingdom [47]. Finally, while children with neurodevelopmental disorders have a shorter sleep duration compared to children who are typically developing, it is not clear if this is a shorter sleep need or some type of abnormality in neural organization [48]. More research is needed to better understand variation in physiological sleep needs in these groups.
Sleep efficiency and continuity: The ease of falling asleep and returning to sleep
The primary definition of sleep efficiency is the ratio of time sleeping to time in bed trying to sleep, thus accounting for sleep onset latency (time between lights out and falling asleep) and wake after sleep onset (time spent awake after falling asleep). Several reviews have examined the relationship between sleep efficiency and health outcomes (see Table 2) [49–52]. While objective measures of sleep can provide a more accurate measure of sleep efficiency, the subjective report of sleep continuity relies on an individual to estimate both sleep onset latency and wake after sleep onset. Studies of adults have found only a modest association between self-reported sleep and objective measures (e.g., [53, 54]).
In pediatrics, sleep efficiency and continuity can be more challenging to capture than with adults, especially as it is often based on parental report. Few studies have considered at what age children can accurately report on sleep onset latency and wake after sleep onset. In one qualitative study with sleep experts, there was disagreement on the specific age when children become accurate self-reporters; however, there was consensus that there may be wide variability, with some children as young as 6 years able to describe their sleep efficiency, and some pre-adolescents who still do not have a sense of sleep onset latency or wake after sleep onset [55]. Thus, a significant amount of what we know about sleep continuity in pediatrics relies on parental report. But as children get older, parents become less involved with sleep routines [56–58]. Thus, parents of a middle or high school aged child (i.e., 11–17 years) may not be aware of how long a child spends trying to fall asleep, or how long he/she is awake during the night if the child does not wake the parent [59].
On the other end of the age spectrum, it is important to consider developmental differences in infant sleep continuity. For example, studies have shown that all infants have frequent night wakings, but many return to sleep quickly without signaling their parents [60–62]. Thus, parental report may underestimate sleep continuity compared to more objective measures. Also, the construct of whether night wakings, which can be normative in infants, is problematic needs to be considered within the larger context of the family. For example, treatment is usually sought based on parental report of concerns, rather than objective report of wakings. The duration of these night wakings may also need to be considered within this basis of parental report. For example, studies indicate that adults typically need to be awake for an average of 4 min to report middle of the night awakenings, with individual differences ranging from 30 s to 10 min [63]. Should a similar construct be implemented for parental report of night wakings, differentiating between normative night wakings versus those that are problematic? Furthermore, the quality of these wakings will affect parental report. For instance, although two infants each may wake briefly and return to sleep quickly, it is qualitatively different when the first one returns to sleep independently, compared to the second infant who cries, and parents respond to help the infant return to sleep. The second scenario is more likely to be deemed problematic, although there may be substantial variation within and across cultures in how parents define a sleep problem and in their expectations for infant sleep consolidation in particular [64,65].
There are also questions about how to define “sleeping through the night,” as well as consideration of the age when sleeping for long stretches is developmentally appropriate. Studies have investigated the definition of sleeping through the night as it pertains to infants. Henderson and colleagues concluded that the most developmentally and socially valid criterion for sleeping through the night is from 10:00 pm to 6:00 am [65,66], after comparing three definitions [1]: sleeping from midnight to 5:00 am [2], 8-h criterion (sleeping uninterrupted for 8 h minimum between sleep onset and morning waking), or [3] family congruent criterion (sleeping uninterrupted from 10:00 pm to 6:00 am). The majority of infants met the family congruent criterion at two and 3 months of age.
Sleep timing: The placement of sleep within the 24-h d
For most people, sleep occurs at night, as human circadian rhythms are regulated by the release of melatonin when it gets dark outside, and the cessation of melatonin production with the exposure to daytime light. Extrinsic factors, such as work schedules, also play a significant role in the timing of adult sleep.
In pediatrics, both intrinsic (e.g., the circadian rhythm) and extrinsic factors (e.g., family, school) play a critical role in determining the timing of sleep (Fig. 1), with some research showing that the timing of sleep is in turn related to child outcomes (Table 2). In newborn infants, the circadian rhythm is not fully detectable until around eight–12 weeks of age [67], starting with the day–night rhythm of cortisol secretion and followed by melatonin rhythmicity one week later, contributing to nighttime sleep consolidation. It is further impacted by light exposure, with one study finding that increased duration of daily exposure to >100 lux of illumination, as well as increased amplitude of circadian rhythm of light, were associated with stronger circadian patterns in young infants [68]. Thus, both intrinsic and extrinsic factors impact the regular timing of sleep in the first few months.
Studies clearly show the importance of parent set bedtimes and consistent early bedtimes for sleep health in children and adolescents [16–18,69]. However, in many families, parent work and childcare schedules play a role in the timing of sleep for children under 10 years [70–72]. For example, in order to spend time with children in the evenings after work, parents or other caregivers may delay child bedtimes, or children may attempt to remain awake later to see their parent/caregiver. In the mornings, when parents/caregivers need to be at work early, many children need to be awakened to get to daycare or before school care, resulting in shortened sleep duration. Weekend schedules may also be shifted to prioritize family activities, although there is limited research on weekday to weekend shifts in preschool and school-aged children. Another external factor that can influence the timing of sleep in younger children is the presence of older children and adolescents in the home. Older siblings who have evening activities, or other adults in the home who remain awake later and/or share the child’s sleep space, can also result in a delayed bedtime for younger children [9,73]. Similarly, naps may be affected by daytime activities of older siblings. In addition, there may be practices that differ across cultures and influence the timing of sleep, such as later mealtimes and a designated siesta or rest period in the afternoon [1].
With the onset of puberty, the circadian timing of dim light melatonin onset is delayed by 1–2 h [74], resulting in later sleep onset times. Weekend social jetlag (the significant delay of bedtime and wake time on non-school days) can also result in poorly timed sleep when the weekend is over [75]. Adolescence is a time that also includes increases in homework, extracurricular activities, and social interactions that can further delay the timing of sleep onset. However, early school start times are common in the United States [15,76], resulting in early rise times for many adolescents. The intersection between normal circadian changes, irregular sleep schedules on weekends, and external restrictions on sleep timing can result in poorer sleep health for youth [77].
Alertness/sleepiness: The ability to maintain attentive wakefulness
Along with the circadian rhythm that helps to drive sleep timing, homeostatic sleep pressure (or the drive for sleep) helps to regulate daytime alertness [78,79], which is important for optimal health and well-being (Table 2). Good sleep health should contribute to decreased sleep pressure through most of the day, resulting in increased feelings of alertness and decreased feelings of sleepiness. The homeostatic drive also factors into when someone begins to feel sleepy, with changes across development. Although 16 h of wakefulness is needed to build sufficient sleep pressure in adults, homeostatic sleep pressure builds more quickly in infants, toddlers, and preschoolers [79]. This helps to explain why naps are developmentally appropriate in infants and young children, while most school-aged children and adolescents remain alert through the day, without feeling sleepy in school or during activities. In contrast, there is a slower build-up of homeostatic sleep pressure during wakefulness in post-pubertal adolescents, resulting in a greater ability to delay bedtimes [80].
In young children, there are a number of factors that affect the timing and the presence of naps. As noted above, development of underlying circadian rhythms of cortisol, melatonin, and core body temperature does not develop until eight–12 weeks of age. Throughout infancy, naps are affected by both sleep pressure and homeostatic drive, resulting in naps occurring in individual infants either when sleep pressure is high (e.g., 2–3 h of wakefulness) or based on their circadian clock (e.g., napping at 9:00 a.m. and 2:00 p.m.). Initial studies indicate great variability in the time of day for naps across early infancy [81], however between about eight and 12 months old, parental report of daytime sleep develops into the following two distinct times: one nap at about 9:00 am and a second nap at about 2:00 pm. Although most toddlers still need to nap [82], one study found that napping toddlers had later bedtimes, shorter nighttime sleep duration, and napping frequency was positively correlated with melatonin onset time [83].
There are also cultural differences in napping. Prior to age 3 years, a study of infants in predominantly-Asian countries/regions found minimal variation in the number and duration of daytime naps compared to infants in predominantly non-Latinx White countries [47]. However, vast differences in napping occur after age 3 years, as a result of racial and cultural differences. One study found significant racial differences in napping in the United States, beginning as early as age 2 years and extending to at least 8 years [45]. At age 8 years, almost 40% of Black or African-American children were reported to nap, compared with only 5% of non-Latinx White children. Looking at cross-cultural differences, preschoolers in countries such as China and Philippines continue to nap until ages 5 and 6 years, in comparison to the cessation of the majority of napping in countries such as Australia, United States, and the United Kingdom [84]. For older school-aged children in China, midday napping has been associated with improved daytime functioning, including cognitive, mood, and behavior [85]. Further research, however, still needs to be conducted on individual, family, and socio-cultural differences within these contexts in both nap timing and duration to determine whether daytime sleepiness and naps are clinically concerning.
When considering alertness/sleepiness in pediatrics, it is critical to understand that presenting symptoms can differ between children and adults. For example, while irritability can be a sign of increased sleepiness across development, some children have increased energy when sleepy (as opposed to most adults who report decreased energy) [86]. Other significant signs of sleepiness in children and adolescents include difficulties with behavior and emotion regulation, as well as poor concentration and academic performance [19,87]. It is also important to recognize the role of attribution in understanding alertness/sleepiness. Most adults can report that they are sleepy because of poor quality or insufficient quantity of sleep. However, it is not clear at what age children are able to attribute their daytime functioning to their previous night of sleep [55]. In addition, reliance on parent report may not always provide a complete picture as parents can only report on observable behaviors (e.g., increased hyperactivity, reports of child falling asleep in school, irritability). Child report is needed to better recognize internal symptoms, such as feelings of fatigue or anhedonia that may result from poor quality sleep.
During adolescence, a number of other factors affect daytime alertness beyond insufficient sleep and underlying sleep disrupters, such as obstructive sleep apnea and narcolepsy. As noted above, studies also indicate that there is a slower accumulation of homeostatic sleep pressure in older adolescents, which contributes to an ability to delay bedtimes [80]. The intersection of later bedtimes and early high school start times in the United States create what is referred to as the “perfect storm,“ [77] contributing to significant daytime sleepiness. Napping may be used in some countries to decrease daytime sleepiness, with associations between midday napping and improved neurocognitive functioning for adolescents in China [88]. There are likely individual differences in the response to decreased sleep that impact daytime alertness and functioning [89], similar to observed phenotypic and intra-individual differences in response to insufficient sleep in adults [90].
Satisfaction/quality: The subjective assessment of “good” or “poor” sleep
Of all five dimensions, satisfaction/quality is the most difficult to quantify [1]. All other dimensions of sleep health can be measured by behavioral or physiological data, but satisfaction/quality relies solely on the reporter to provide an interpretation of their sleep. Further, this interpretation is often made within the context of other environmental and social contexts. Thus, two individuals may have the same sleep duration, sleep continuity, and sleep timing, but one feels as if their sleep was “good” while the other reports their sleep to be “poor.”
In pediatrics, as with other aspects of sleep, there remain questions about when a child might be able to differentiate between good and poor sleep quality. For older children and adolescents, if not queried directly, satisfaction/quality is the dimension of sleep health least likely to be accurate when provided by parents because sleep quality is so subjective. Thus, when possible it is essential to obtain reports of sleep quality from both the parent and the child/adolescent. Further, the parent’s perception of sleep heavily influences their own report of the child’s sleep quality/satisfaction [91], and parents may misattribute daytime behavioral issues to poor sleep quality. Finally, although subjective reports of satisfaction/quality are related to health and well-being outcomes (Table 2), research studies have vastly differed in how they define sleep quality.
Sleep-related behaviors: Actions and activities that may promote or inhibit sleep health
Sleep-related behaviors are an important consideration in pediatric sleep health, and are being added to the original model proposed by Buysse [1]. Sleep-related behaviors is a broader category of factors that promote sleep, including a consistent sleep schedule (regularity as defined by Buysse [1]) and a nightly bedtime routine, as well as factors that inhibit sleep health, such as caffeine intake and technology use in the hour prior to sleep. Additionally, parent–child interactions prior to bedtime and at sleep onset can impact sleep duration, consolidation, and quality. While more research is needed, these different aspects of sleep behaviors (e.g., routines, caffeine, electronics) have also been associated with health outcomes across development in pediatrics (Table 2).
Unlike adults, children and adolescents may or may not have sole control over many of these factors, with parents or other external factors (e.g., use of computers required for homework) often driving the choice of sleep-related behaviors. Thus, we propose sleep-related behaviors as a sixth sleep health dimension for pediatrics, expanding the sixth dimension of regularity (or variability) in adults. While we agree that regularity is a critical aspect of sleep health for pediatrics, we argue that it is part of the sleep-related behaviors dimension.
In pediatrics, regularity can be applied to multiple dimensions of sleep health, but is most critical for the timing of sleep, which in turn ensures sufficient sleep duration. As previously discussed, the regularity of bedtimes and wake times helps to maintain a healthy sleep rhythm for children and adolescents. It is common for adolescents and many school-aged children to have variable sleep-wake schedules, with differences noted between weekdays, weekends, and school holidays. The variability in weekend sleep time in particular is problematic, as previously described, resulting in social jetlag.57 For example, a youth who does not obtain sufficient sleep during the school week because of a late bedtime and an early wake time will further delay his bedtime on weekend nights, and attempt to “catch up” on sleep by sleeping until noon. However, come Sunday night he will have difficulty falling asleep, impairing his ability to obtain sufficient sleep duration and feel alert during the day.
In addition to a regular sleep schedule, it is important to have a consistent bedtime routine to facilitate sleep onset and broad sleep health. Defined as the predictable activities that occur in the hour or so prior to sleep onset [92], a bedtime routine is essential for children of all ages. In early childhood, there is a dose–response relationship between bedtime routine consistency and healthy sleep outcomes, with increased bedtime routine consistency linearly associated with earlier bedtimes, a shorter sleep onset latency, reduced nighttime awakenings, and longer sleep duration [93]. Even in school-aged children, following a consistent bedtime routine is associated with better sleep, including longer nighttime sleep duration [56]. Having a consistent routine is hypothesized to facilitate sleep onset by creating positive sleep associations, with the steps of the routine serving as part of a behavioral chain leading to sleep [92].
Sleep-onset associations, behaviors that occur at the time of sleep onset, are common and often the result of parent behaviors. Parental presence is the most common sleep–onset association that can impact the ability to fall asleep or return to sleep following a naturally occurring night waking. Parental presence at sleep onset is common in young children (68% of infants, 43% of toddlers and preschoolers) [56]. It also is important to note that sleep onset associations are not limited to children <5 years, with over 20% of school-age children and 6% of adolescents requiring parental presence to fall asleep at bedtime at least some of the time [55,56].
Socio-ecological factors may play a role in the association between parental presence at sleep onset and child sleep outcomes, and as such must be considered in light of whether or not families are bed- or room-sharing, and whether this is an intentional choice, a necessity due to limited space or economic resources, or in reaction to a child sleep problem. For example, cross-cultural research has demonstrated that there is variation in parenting behaviors at bedtime according to region, with over half (57%) of young children from predominantly-Caucasian countries falling asleep independently compared to only 4% of those from predominantly-Asian regions/countries [94]. Parent presence at sleep onset was more robustly associated with poor nighttime sleep in predominantly-Caucasian regions and also contributed to the association between bed- or room-sharing and poor sleep outcomes. Although there are few studies of parental presence and co-sleeping at bedtime in older children, some research indicates that co-sleeping was more common in school-aged children with anxiety disorders, and was also linked to an increased sleep onset latency and more variable nighttime sleep duration [95]. Parents of children with special needs may also be more likely to be present at bedtime, contributing to poor sleep outcomes. For example, in one study parents of children with Down syndrome were significantly more likely to report being present at bedtime than parents of typically developing children [96]. Additional research focused on parental presence at bedtime and pediatric sleep outcomes should include an assessment of pre-bedtime parenting practices, parent–child interactions, and co-sleeping preferences and arrangements, in both children who are typically developing and those with comorbid behavioral health and neurodevelopmental conditions.
Transition objects are another type of sleep–onset association commonly seen in pediatrics (especially in younger children) and not in adults to facilitate sleep. Objects can include pacifiers, stuffed animals, or other comfort items. These are typically considered positive sleep onset associations as a child can utilize these objects without parental assistance. Studies have found that stuffed animals can reduce stress and fears at bedtime in younger and school age children [69,97,98].
Extrinsic sleep-related behaviors, including caffeine use and technology, often interfere with sleep health and may be impacted by parents/caregivers or other environmental factors, such as availability and social norms. As a stimulant, caffeine has a physiological impact that can result in delayed and disrupted sleep in both children and adults. Although it is recommended that children under 12 years have no caffeine, and adolescents have limited caffeine (<100 mg) [99], caffeine is widely available and consumed by a substantial proportion of youth, with studies showing that 28–58% of preschoolers, 41–87% of school-aged children, and 75–86% of adolescents regularly consuming caffeine [56,100–102]. Household norms, parental rule enforcement, and family practices play an important role in child caffeine consumption and the subsequent impact on sleep. In particular, parental limit setting around child caffeine consumption has been shown to benefit both sleep quality and sleep duration in children and adolescents [103].
The use of electronics prior to sleep onset is discouraged, however it is a common behavior, with an estimated 25% of 1–3 year olds [104] to over 70% of children and adolescents having electronic devices in the bedroom and/or using electronics prior to bedtime [104–107]. Although most research is correlational (and not causal), there is consistent evidence that the presence of electronic items in the child’s bedroom or the use of electronics at bedtime is associated with shorter sleep duration across development [56,104–107]. From this growing literature, several findings stand out as important to consider for pediatric sleep health. First, recent research shows a correspondence between child and parent habits around electronics usage, as children who use electronics at bedtime are more likely to have parents using electronics at bedtime as well [103]. This finding suggests that parental limit setting around the use of electronics may need to be bolstered by parents and other family members monitoring their own electronics usage at bedtime. Second, studies have shown that over one-third of young adolescents report waking during the night to use social media at least once a week, with over one in 5 youth waking almost every night to send or check social media messages [108]. For teenagers in particular, parental-limit setting in relation to social media engagement is likely necessary to prevent electronics from interfering in healthy sleep. Finally, in line with broader racial/ethnic disparities in sleep health, the presence of a television in the bedroom is associated with shorter sleep duration among racial/ethnic minority children ages 6 months to 7 years, but not among non-Latinx white children [109]. Finally, it needs to be noted that a total ban of electronics use at bedtime needs to be considered within the individual and family context [110]. For example, some electronics use by some children with neurodevelopmental conditions may result in an easier time settling down at bedtime, although this has not been studied to date. Further research related to variation in family and socio-cultural norms and limit-setting around electronics usage, as well as causal research examining the impact of electronics usage on sleep, is necessary to better inform pediatric sleep health recommendations related to electronics devices across different pediatric populations.
Peds B-SATED: Revised definition and application of the model
Based on this review and the Peds B-SATED model, we propose a revised version of Buysse’s definition of sleep health for pediatrics (with additions italicized). Good sleep in pediatrics is characterized by subjective or caregiver-rated satisfaction, appropriate timing, adequate duration for age, high efficiency, sustained alertness during waking hours, and healthy sleep behaviors. The proposed Peds B-SATED model provides an applicable framework for clinicians and researchers in pediatric sleep, both in terms of current application and the development of future directions for clinical practice, research, and training.
Clinicians
For clinicians, screening for sleep health should be on par with screening for diet and exercise [111]. Although sleep duration might be the easiest question to screen given recommended age-based guidelines, duration alone, as we have discussed, does not define sleep health. Such screening and assessment, however, needs to be done across all identified domains. Additionally it needs to include assessment of both perception of sleep by caregivers and children/adolescents, as well as specific questions about sleep patterns and sleep disturbances. Starting with a broader question (e.g., “Do you/does your child have any sleep problems? Is there anything you wish to change about your child’s sleep?“), in addition to asking about snoring as recommended by the American Academy of Pediatrics [112], may be needed to initiate the conversation between patients/families and clinicians, with a set of developmentally-tailored follow-up questions used depending upon the family’s responses.
Clinical screening tools for sleep disorders have been developed, including the BEARS [113] and the Sleep Disturbances Scale for Children (SDSC) [114]. However, these measures are not ideal for screening sleep health, with the BEARS screening tool only capturing four of the six domains (missing Satisfaction and Behaviors), and the SDSC only including two sleep health dimensions (Sleepiness and Duration).
There are hundreds of pediatric sleep questionnaires that have been developed over the years that do include different domains of sleep health; however, a comprehensive review of these is beyond the scope of this theoretical review [115–117]. Instead in Table 3 we provide a list of commonly used questionnaires, as well as measures that include different aspects of sleep health across different developmental groups. Of these, one measure per age group assesses all domains of sleep health: the parent-reported Children’s Sleep Habits Questionnaire (ages 2–10) [118], the self-reported Children’s Report of Sleep Patterns (ages 8–18) [119–121], and the self-report School Sleep Habits Survey (ages 13–19) [122]. The Brief Infant Sleep Questionnaire-Revised assesses all domains except for sleepiness/alertness, as warranted given the focus on infants and toddlers (birth to 3 years) [123,124]. However, none of these measures assesses all aspects of each domain. Thus, one comprehensive measure that includes all aspects of the Peds B-SATED sleep health domains should be developed, including multiple versions to appropriately assess sleep health at different ages/stages.
Table 3.
Examples of subjective pediatric questionnaires and the domains of sleep health measured.
| Subjective Measures | Satisfaction | Alertness/Sleepiness | Timing | Efficiency | Duration | Behaviors | Age | Items | Reporter |
|---|---|---|---|---|---|---|---|---|---|
| Children’s Sleep Habits Questionnaire [118] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 2–10 yrs | 33/45 | Parent |
| Children’s Report of Sleep Patterns [119–121] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8–18 yrs | 60 | Self |
| School Sleep Habits Survey [122] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13–19 yrs | 45 | Self |
| Brief Infant Sleep Questionnaire [123, 124] | ✓ | ✓ | ✓ | ✓ | ✓ | 0–3 yrs | 13/25a | Parent | |
| BEARS [113] | ✓ | ✓ | ✓ | ✓ | 2–18 yrs | 7–8 | Parent/Self | ||
| PROMIS Pediatric Sleep Disturbance [168] | ✓ | 8–18 yrs | 4/8/15 | Self | |||||
| 5–18 yrs | 4/8/15 | Parent-proxy | |||||||
| Sleep Disturbance Scale for Children [114] | ✓ | ✓ | 6–15 yrs | 27 | Parent | ||||
| Modified Epworth Sleepiness Scale [169]/Epworth Sleepiness Scale for Children and Adolescents [170] | ✓ | 12–18 yrs | 8 | Self | |||||
| 2–18 yrs | 8 | Parent-proxy | |||||||
| Pediatric Sleep Questionnaire [171] | ✓ | 2–18 yrs | 22 | Parent | |||||
| Pediatric Daytime Sleepiness Scale [172] | ✓ | 11–15 yrs | 8 | Self | |||||
| PROMIS Pediatric Sleep Related Impairment [168] | ✓ | 8–18 yrs | 4/8/15 | Self | |||||
| 5–18 yrs | 4/8/15 | Parent-proxy | |||||||
| Morningness-Eveningness Questionnaire for Children [173] | ✓ | 11–12 yrs | 10 | Self |
Finally, incorporating sleep health within the context of intervention for specific sleep disorders enables a clinician to more appropriately treat individuals. One study found that within an interdisciplinary pediatric sleep center almost 25% of presenting patients had more than one diagnosed sleep disorder, such as sleep apnea and insomnia, and over one-third received a behavioral recommendation, such as implementation of a consistent sleep schedule or bedtime routine [125]. For example, obstructive sleep apnea (OSA) and other disorders can contribute to poor sleep health, but as noted above, sleep health is a broader construct and is more than just the absence of a sleep disorder. A practitioner can treat the sleep disorder, such as prescribing positive airway pressure (PAP) therapy for the treatment of OSA, but the child may only sleep 5 h a night or the adolescent may sleep during the day which interferes with school performance. Thus, the dimensions of sleep health are distinct but complementary to the treatment of pediatric sleep disorders and should be assessed with all patients. Furthermore, the valid definition and characterization of sleep health in children will strengthen the reciprocal and bi-directional relationships between sleep health and sleep medicine.
Researchers
There is a need for additional research across a number of the domains indicated. For example, more work needs to be done to identify actual sleep need for school-aged and younger children, as opposed to relying on studies of obtained sleep. In addition, research examining each of these sleep health constructs, as well as how the underlying domains may be related over time, is necessary to better understand all aspects of this pediatric sleep health model. Despite the availability of well-validated pediatric sleep measures (examples in Table 3), additional research on how such measures or broader screening questions can be used to efficiently and accurately screen the Peds B-SATED domains in clinical practice is needed.
Further, more information is needed about how each domain of Peds B-SATED is related to important child well-being outcomes [126], including psychological/social functioning, cognitive skills and academic performance, and physical health. Although there is a growing body of research linking sleep health domains and child well-being (a review of which is beyond the scope of this paper), including a recent meta-review on sleep and child outcomes that included 39 review papers examining such linkages [127], there are critical gaps in this research. As shown in Table 2 research on the consequences of variation in sleep timing, alertness/sleepiness/napping, and sleep behaviors is lacking. Research that examines the ways in which specific sleep health behaviors may be associated with or lead to adverse child outcomes is especially sparse. By contrast, there are a number of meta-analytic and systematic reviews available on research linking insufficient sleep and multiple domains of child well-being. In addition, it is notable that there is heterogeneity in the terms used to describe sleep domains, with some research using actigraphy-derived sleep efficiency as an index of sleep quality, which may contribute to mixed findings in the literature for several linkages between sleep quality and child outcomes. Finally, whereas many studies of pediatric sleep and physical health explore outcomes such as weight gain, adiposity, and cardiometabolic risks, few studies have examined other physical health outcomes, such as illnesses and injuries/accidents [127].
Finally, additional research that takes both a developmental and a socio-ecological approach to understanding the multifaceted construct of sleep health, and how the domains of pediatric sleep health may vary by individual and contextual factors, is critical. This work can inform efforts to promote sleep health and well-being across multifaceted populations of children and adolescents.
Training
The key to identification of sleep issues and promotion of positive sleep health is adequate training of pediatric clinicians, including those involved with children on a regular basis such as in childcare settings and schools. A number of studies have noted the lack of knowledge of sleep and sleep medicine by health care clinicians [128,129], as well as a lack of training in medical school [130, 131] and pediatric residency programs [132]. Furthermore, a survey of 346 members of the American Academy of Pediatrics found that few of these pediatricians (18%) had ever received formal training on sleep disorders and less than 15% were very confident in their abilities to counsel pediatric patients on sleep issues [133]. This training is critical not only for primary care clinicians, but is needed for all types of clinicians, including pediatric specialists (e.g., psychiatry, neurology, developmental and behavioral pediatrics), psychologists, and nurses/nurse-practitioners [134,135]. Along with identifying sleep-related issues, the education of primary care physicians and other front-line clinicians about sleep health is necessary to give families the support and information needed to improve sleep health across all domains.
Training is also important for those involved with children and adolescents on a regular basis outside of healthcare settings, including those in early childhood education programs and in schools. A study of sleep health literacy in 63 staff members at a Head Start program found that although 87% reported feeling comfortable discussing healthy sleep with parents, less than half felt comfortable counseling them [136]. Thus, there was a gap in the perception of staff between their competencies to promote healthy sleep in families and their capacity to address sleep problems. There have been calls for school psychologists to receive preservice and continuing education in the assessment, prevention, and intervention for pediatric sleep, as well as development of practice guidelines for assessment and intervention, similar to those for medical practice [137]. Little, if any, attention has been paid to the need for teachers to receive education about pediatric sleep. Development of educational programs regarding the domains of Peds B-SATED will not only help them identify children with sleep issues, but more importantly integrate this information into the education of children and adolescents about the importance of sleep and understanding of sleep health.
Public education
Although we have outlined suggestions for how clinicians can evaluate and provide interventions for sleep health directly to patients, there remains a significant need for broader, population-based dissemination of sleep health information directly to families and the general public. Sleep education programs for children and adolescents have been primarily school based, with studies showing an increase in sleep knowledge, and in some cases sleep duration, but no long term changes in sleep health [138,139]. Parent sleep education programs have been studied primarily as prevention for infant sleep disturbances [140], or in the context of treatment for specific populations (e.g., autism, head start programs) [141–144]. In addition, there have been endeavors to provide publicly-available education about sleep, such as the website Babysleep.com developed and disseminated by the Pediatric Sleep Council that has resulted in global outreach to 223 countries (99% of the world’s countries) [145]. Finally, although there have been campaigns to promote awareness about sleep health in older youth and adults, such as the National Healthy Sleep Awareness Project, which was supported by the American Academy of Sleep Medicine, the Centers for Disease Control and Prevention, and the Sleep Research Society [146], as well as Baby Sleep Day promoted by the Pediatric Sleep Council, there have been no concerted public health campaigns to improve sleep health in children of all ages. There is also a need for continued development of publicly-available sleep education websites, smartphone apps, and toolkits. There have been some developments in this area, including sleep toolkits developed by the Autism Treatment Network for parents, but more are needed, especially ones that are created to be directly accessed by children or adolescents.
The Peds B-SATED framework can provide a foundation for such campaigns and public education endeavors, with direct-to-consumer information about the importance of sleep health and specific behaviors families can take to encourage it. In light of significant sleep health disparities in pediatrics and among adults, it is especially important that public health efforts to promote healthy sleep awareness are implemented and disseminated in a manner that is responsive to the many socio-ecological factors that shape sleep health outcomes and target reduction of sleep health disparities [147].
Peds B-SATED: Conceptual model
As we have described throughout this paper, sleep health is critical across development, from infancy through adolescents. The Peds B-SATED framework allows us to conceptualize the different aspects of sleep health, including the additional component of sleep health behaviors, which may be especially important in pediatrics. Although this framework has significant overlap with the adult RU-SATED framework, there are also distinct characteristics that need to be considered from both a developmental perspective and a socio-ecological model. Children and adolescents are not simply small adults, and thus the unique features of pediatric sleep health must be considered by clinicians and researchers to ensure successful physiological, cognitive, and emotional development.
It is important to understand that sleep health is not a uni-dimensional construct, but includes different domains: specifically Behaviors, Satisfaction/Quality, Alertness/Sleepiness, Timing, Efficiency, and Duration. Further, while some domains are essential for all children regardless of age (e.g., bedtime routine, consistent bedtime schedule), other aspects of these domains do not remain consistent across development (e.g., sleep duration is greater in infants than adolescents). Thus, clinicians and researchers need to be aware of the differences of sleep across development. In addition, while these pediatric sleep health domains may be related, it is also important to recognize they may not always be associated. For example, children who experience poor quality sleep or who have a caregiver-identified child sleep problem may or may not consume any caffeine or have bedroom electronics. In the same way, some youth may consume caffeine and use electronics but obtain adequate sleep duration and report no daytime sleep-related impairments. Furthermore, there are likely significant individual differences, potentially influenced by other socio-ecological factors, in sleep health needs and profiles across pediatric populations. The multidimensional Peds B-SATED conceptualization is similar to how one might characterize individual nutritional needs and profiles, with individuals in need of supplementation in some areas (e.g., protein) but not others (e.g., vegetables) in order to achieve optimal sleep health.
Practice points.
Sleep health should be considered at every well-child visit, on par with diet and exercise.
The Peds B-SATED theoretical model provides clinicians a framework to evaluate the different dimensions of sleep that impact health outcomes.
Sleep health should be integrated into the treatment of all pediatric sleep disorders, whether behavioral or physiological in etiology.
Research agenda.
Identify actual sleep needs for school-aged and younger children, rather than relying on studies that only measure obtained sleep or sleep opportunity.
Develop a validated screening measure that includes all Peds B-SATED domains that can be used in both primary care and specialty care practice.
Conduct additional research that links the Peds B-SATED domains with child and adolescent well-being, including physical health, mental health, and academic outcomes.
Include both developmental and socio-ecological factors in future research to understand individual and contextual factors that contribute to sleep health.
Acknowledgements
Dr. Williamson was supported during this project by a career development award from the Sleep Research Society Foundation and K23 HD094905 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
References
* The most important references are denoted by an asterisk.
- *[1].Buysse DJ. Sleep health: can we define it? Does it matter? Sleep 2014;37(1):9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Sadeh A, Anders TF. Infant sleep problems: origins, assessment, interventions. Infant Ment Health J 1993;14(1):17–34. [Google Scholar]
- [3].Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev 2010;14(2):89–96. [DOI] [PubMed] [Google Scholar]
- [4].Newton AT, Honaker SM, Reid GJ. Risk and protective factors and processes for behavioral sleep problems among preschool and early school-aged children: a systematic review. Sleep Med Rev 2020;52:101303. [DOI] [PubMed] [Google Scholar]
- [5].Bronfenbrenner U The ecology of human development: experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. p. 1979. [Google Scholar]
- [6].Williamson AA, Mindell JA, Hiscock H, Quach J. Sleep problem trajectories and cumulative socio-ecological risks: birth to school-age. J Pediatr 2019;215:229–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tietze AL, Blankenberg M, Hechler T, Michel E, Koh M, Schluter B, et al. Sleep disturbances in children with multiple disabilities. Sleep Med Rev 2012;16:117–27. [DOI] [PubMed] [Google Scholar]
- [8].Quach JL, Nguyen CD, Williams KE, Sciberras E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr 2018;172(2): e174363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Spilsbury JC, Patel SR, Morris N, Ehayaei A, Intille SS. Household chaos and sleep-disturbing behavior of family members: results of a pilot study of African American early adolescents. Sleep Health 2017;3(2):84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disord 2013;2013:394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bottino CJ, Rifas-Shiman SL, Kleinman KP, Oken E, Redline S, Gold D, et al. The association of urbanicity with infant sleep duration. Health Place 2012;18(5):1000–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol 2014;33(3):301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sheehan C, Powers D, Margerison-Zilko C, McDevitt T, Cubbin C. Historical neighborhood poverty trajectories and child sleep. Sleep Health 2018;4(2):127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: multiple indicators and moderation of effects. Health Psychol 2013;32(8):849–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].American Academy of Pediatrics. School start times for adolescents. Pediatrics 2014;134(3):642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Short MA, Gradisar M, Wright H, Lack LC, Dohnt H, Carskadon MA. Time for bed: parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. Sleep 2011;34(6):797–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep 2010;33(1):97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Peltz JS, Rogge RD, Connolly H. Parents still matter: the influence of parental enforcement of bedtime on adolescents’ depressive symptoms. Sleep 2020;43(5). [DOI] [PubMed] [Google Scholar]
- [19].Owens J Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics 2014;134(3):e921–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wahlstrom KL, Owens JA. School start time effects on adolescent learning and academic performance, emotional health and behaviour. Curr Opin Psychiatr 2017;30(6):485–90. [DOI] [PubMed] [Google Scholar]
- [21].Williams KE, Berthelsen D, Walker S, Nicholson JM. A developmental cascade model of behavioral sleep problems and emotional and attentional self-regulation across early childhood. Behav Sleep Med 2017;15(1): 1–21. [DOI] [PubMed] [Google Scholar]
- [22].Williams KE, Nicholson JM, Walker S, Berthelsen D. Early childhood profiles of sleep problems and self-regulation predict later school adjustment. Br J Educ Psychol 2016;86(2):331–50. [DOI] [PubMed] [Google Scholar]
- [23].Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. J Sleep Res 2012;21(3):235–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. JCPP (J Child Psychol Psychiatry) 2014;55(2):180–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Benitez I, Roure N, Pinilla L, Sapina-Beltran E, Buysse DJ, Barbe F, et al. Validation of the satisfaction, alertness, timing, efficiency and duration (SATED) questionnaire for sleep health measurement. Ann Am Thorac Soc 2020;17(3):338–43. [DOI] [PubMed] [Google Scholar]
- [26].Ravyts SG, Dzierzewski JM, Perez E, Donovan EK, Dautovich ND. Sleep health as measured by RU SATED: a psychometric evaluation. Behav Sleep Med 2019:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Becker NB, Martins RIS, Jesus SN, Chiodelli R, Stephen RM. Sleep health assessment: a scale validation. Psychiatr Res 2018;259:51–5. [DOI] [PubMed] [Google Scholar]
- [28].Dong L, Martinez AJ, Buysse DJ, Harvey AG. A composite measure of sleep health predicts concurrent mental and physical health outcomes in adolescents prone to eveningness. Sleep Health 2019;5(2):166–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Knutson KL, Phelan J, Paskow MJ, Roach A, Whiton K, Langer G, et al. The national sleep foundation’s sleep health index. Sleep Health 2017;3(4): 234–40. [DOI] [PubMed] [Google Scholar]
- [30].Ohayon MM, Paskow M, Roach A, Filer C, Hillygus DS, Chen MC, et al. The national sleep foundation’s sleep satisfaction tool. Sleep Health 2019;5(1): 5–11. [DOI] [PubMed] [Google Scholar]
- [31].U.S. Department of Health and Human Services. Healthy people 2020 2010 [updated 2010]. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health/objectives.
- [32].U.S. Department of Health and Human Services. Healthy people 2030 2020 [updated 2020]. Available from: https://www.healthypeople.gov/sites/default/files/ObjectivesPublicComment508.pdf.
- [33].Centers for Disease Control and Prevention. Sleep and Health [updated 2019]. Available from: https://www.cdc.gov/healthyschools/sleep.htm; 2019.
- [34].Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the american academy of sleep medicine. J Clin Sleep Med 2016;12(6):785–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Carskadon MA, Orav EJ, Dement WC. Evolution of sleep and daytime sleepiness in adolescents. In: Guilleminault C, Lugaresi E, editors. Sleep/wake disorders: natural history, epidemiology, and long-term evolution. New York: Raven Press; 1983. p. 201–16. [Google Scholar]
- [36].Bei B, Manber R, Allen NB, Trinder J, Wiley JF. Too long, too short, or too variable? Sleep intraindividual variability and its associations with perceived sleep quality and mood in adolescents during naturalistically unconstrained sleep. Sleep 2017;40(2). [DOI] [PubMed] [Google Scholar]
- [37].El-Sheikh M, Philbrook LE, Kelly RJ, Hinnant JB, Buckhalt JA. What does a good night’s sleep mean? Nonlinear relations between sleep and children’s cognitive functioning and mental health. Sleep 2019;42(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].James S, Hale L. Sleep duration and child well-being: a nonlinear association. J Clin Child Adolesc Psychol 2017;46(2):258–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Richards A, Inslicht SS, Metzler TJ, Mohlenhoff BS, Rao MN, O’Donovan A, et al. Sleep and cognitive performance from teens to old age: more is not better. Sleep 2017;40(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Guglielmo D, Gazmararian JA, Chung J, Rogers AE, Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health 2018;4(1):68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Smith JP, Hardy ST, Hale LE, Gazmararian JA. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health 2019;5(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].El-Sheikh M, Tu KM, Saini EK, Fuller-Rowell TE, Buckhalt JA. Perceived discrimination and youths’ adjustment: sleep as a moderator. J Sleep Res 2016;25(1):70–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Bagley EJ, Tu KM, Buckhalt JA, El-Sheikh M. Community violence concerns and adolescent sleep. Sleep Health 2016;2(1):57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Heissel JA, Sharkey PT, Torrats-Espinosa G, Grant K, Adam EK. Violence and vigilance: the acute effects of community violent crime on sleep and cortisol. Child Dev 2018;89(4):e323–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics 2005;115(1 Suppl):225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lavigne JV, Arend R, Rosenbaum D, Smith A, Weissbluth M, Binns HJ, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr 1999;20(3):164–9. [DOI] [PubMed] [Google Scholar]
- [47].Mindell JA, Sadeh A, Wiegand B, How TH, Goh DY. Cross-cultural differences in infant and toddler sleep. Sleep Med 2010;11(3):274–80. [DOI] [PubMed] [Google Scholar]
- [48].Buckley AW, Rodriguez AJ, Jennison K, Buckley J, Thurm A, Sato S, et al. Rapid eye movement sleep percentage in children with autism compared with children with developmental delay and typical development. Arch Pediatr Adolesc Med 2010;164(11):1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Reynaud E, Vecchierini MF, Heude B, Charles MA, Plancoulaine S. Sleep and its relation to cognition and behaviour in preschool-aged children of the general population: a systematic review. J Sleep Res 2018;27(3): e12636. [DOI] [PubMed] [Google Scholar]
- *[50].Astill RG, Van der Heijden KB, van Ijzendoorn MH, Van Someren EJ. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull 2012;138(6):1109–38. [DOI] [PubMed] [Google Scholar]
- *[51].Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev 2010;14(3):179–89. [DOI] [PubMed] [Google Scholar]
- *[52].Matthews KA, Pantesco EJ. Sleep characteristics and cardiovascular risk in children and adolescents: an enumerative review. Sleep Med 2016;18: 36–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology 2008;19(6):838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Jackson CL, Patel SR, Jackson WB, Lutsey PL, Redline S. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: multi-Ethnic Study of Atherosclerosis. Sleep 2018;41(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Meltzer LJ, Forrest CB, de la Motte A, Mindell JA, Bevans KB. Development and validation of the Pediatric Sleep Practices Questionnaire: a self-report measure for youth ages 8–17 years. Behav Sleep Med 2021;19(1):126–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 national sleep foundation sleep in America poll. Sleep Med 2009;10(7):771–9. [DOI] [PubMed] [Google Scholar]
- [57].Waters E, Stewart-Brown S, Fitzpatrick R. Agreement between adolescent self-report and parent reports of health and well-being: results of an epidemiological study. Child Care Health Dev 2003;29(6):501–9. [DOI] [PubMed] [Google Scholar]
- [58].Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev 1998;69(4):875–87. [PubMed] [Google Scholar]
- [59].Poulain T, Vogel M, Meigen C, Spielau U, Hiemisch A, Kiess W. Parent-child agreement in different domains of child behavior and health. PloS One 2020;15(4):e0231462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Anders TF, Halpern LF, Hua J. Sleeping through the night: a developmental perspective. Pediatrics 1992;90(4):554–60. [PubMed] [Google Scholar]
- [61].Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry Allied Discip 2002;43(6):713–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Sadeh A, Lavie P, Scher A, Tirosh E, Epstein R. Actigraphic home-monitoring of sleep-disturbed and control infants and young children: a new method for pediatric assessment of sleep-wake patterns. Pediatrics 1991;87:494–9. [PubMed] [Google Scholar]
- [63].Winser MA, McBean AL, Montgomery-Downs HE. Minimum duration of actigraphy-defined nocturnal awakenings necessary for morning recall. Sleep Med 2013;14(7):688–91. [DOI] [PubMed] [Google Scholar]
- [64].Sadeh A, Mindell J, Rivera L. My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med 2011;12(5): 478–82. [DOI] [PubMed] [Google Scholar]
- [65].Henderson JM, Motoi G, Blampied NM. Sleeping through the night: a community survey of parents’ opinions about and expectations of infant sleep consolidation. J Paediatr Child Health 2013;49(7):535–40. [DOI] [PubMed] [Google Scholar]
- [66].Henderson JMT, France KG, Owens JL, Blampied NM. Sleeping through the night: the consolidation of self-regulated sleep across the first year of life. Pediatrics 2010;126(5):e1081–7. [DOI] [PubMed] [Google Scholar]
- [67].Thomas KA, Burr RL, Spieker S. Light and maternal influence in the entrainment of activity circadian rhythm in infants 4–12 weeks of age. Sleep Biol Rhythm 2016;14(3):249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Tsai SY, Thomas KA, Lentz MJ, Barnard KE. Light is beneficial for infant circadian entrainment: an actigraphic study. J Adv Nurs 2012;68(8): 1738–47. [DOI] [PubMed] [Google Scholar]
- [69].Golem D, Eck KM, Delaney CL, Clark RL, Shelnutt KP, Olfert MD, et al. “My stuffed animals help me”: the importance, barriers, and strategies for adequate sleep behaviors of school-age children and parents. Sleep Health 2019;5(2):152–60. [DOI] [PubMed] [Google Scholar]
- [70].Martinez SM, Thompson-Lastad A. Latino parents’ insight on optimal sleep for their preschool-age child: does context matter? Acad Pediatr 2015;15(6):636–43. [DOI] [PubMed] [Google Scholar]
- [71].Kalil A, Dunifon R, Crosby D, Su JH. Work hours, schedules, and insufficient sleep among mothers and their young children. J Marriage Fam 2014;76: 891–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Lee S, Hale L, Berger LM, Buxton OM. Maternal perceived work schedule flexibility predicts child sleep mediated by bedtime routines. J Child Fam Stud 2019;28:245–59. [Google Scholar]
- [73].Boles RE, Halbower AC, Daniels S, Gunnarsdottir T, Whitesell N, Johnson SL. Family chaos and child functioning in relation to sleep problems among children at risk for obesity. Behav Sleep Med 2017;15(2):114–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Hagenauer MH, Perryman JI, Lee TM, Carskadon MA. Adolescent changes in the homeostatic and circadian regulation of sleep. Develomental Neuroscience 2009;31(4):276–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int 2006;23(1–2): 497–509. [DOI] [PubMed] [Google Scholar]
- [76].Wheaton AG, Ferro GA, Croft JB. School start times for middle school and high school students - United States, 2011–12 School Year. MMWR Morb Mortal Wkly Rep 2015;64(30):809–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA. An update on adolescent sleep: new evidence informing the perfect storm model. J Adolesc 2018;67:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Jenni OG, Carskadon MA. Normal human sleep at different ages: infants to adolescents. In: SRS basics of sleep guide. Westchester, IL: Sleep Researcher Society; 2005. p. 11–9. [Google Scholar]
- [79].Jenni OG, LeBourgeois MK. Understanding sleep-wake behavior and sleep disorders in children: the value of a model. Curr Opin Psychiatr 2006;19(3):282–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Jenni OG, Achermann P, Carskadon MA. Homeostatic sleep regulation in adolescents. Sleep 2005;28(11):1446–54. [DOI] [PubMed] [Google Scholar]
- [81].Mindell JA, Leichman ES, Composto J, Lee C, Bhullar B, Walters RM. Development of infant and toddler sleep patterns: real-world data from a mobile application. J Sleep Res 2016;25(5):508–16. [DOI] [PubMed] [Google Scholar]
- [82].Staton S, Rankin PS, Harding M, Smith SS, Westwood E, LeBourgeois MK, et al. Many naps, one nap, none: a systematic review and meta-analysis of napping patterns in children 0–12 years. Sleep Med Rev 2019;50: 101247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Akacem LD, Simpkin CT, Carskadon MA, Wright KP Jr, Jenni OG, Achermann P, et al. The timing of the circadian clock and sleep differ between napping and non-napping toddlers. PloS One 2015;10(4): e0125181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Mindell JA, Sadeh A, Kwon R, Goh DY. Cross-cultural differences in the sleep of preschool children. Sleep Med 2013;14(12):1283–9. [DOI] [PubMed] [Google Scholar]
- [85].Liu J, Feng R, Ji X, Cui N, Raine A, Mednick SC. Midday napping in children: associations between nap frequency and duration across cognitive, positive psychological well-being, behavioral, and metabolic health outcomes. Sleep 2019;42(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol 1996;3(1):44–50. [DOI] [PubMed] [Google Scholar]
- [87].Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin 2011;58(3): 649–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Ji X, Li J, Liu J. The relationship between midday napping and neurocognitive function in early adolescents. Behav Sleep Med 2019;17(5): 537–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *[89].Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: a systematic review. Sleep Med Rev 2017;34:94–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Tkachenko O, Dinges DF. Interindividual variability in neurobehavioral response to sleep loss: a comprehensive review. Neurosci Biobehav Rev 2018;89:29–48. [DOI] [PubMed] [Google Scholar]
- [91].Ronnlund H, Elovainio M, Virtanen I, Matomaki J, Lapinleimu H. Poor parental sleep and the reported sleep quality of their children. Pediatrics 2016;137(4). [DOI] [PubMed] [Google Scholar]
- [92].Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: sleep, development, and beyond. Sleep Med Rev 2018;40:93–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep 2015;38(5):717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med 2010;11(4):393–9. [DOI] [PubMed] [Google Scholar]
- [95].Palmer CA, Clementi MA, Meers JM, Alfano CA. Co-sleeping among school-aged anxious and non-anxious children: associations with sleep variability and timing. J Abnorm Child Psychol 2018;46(6):1321–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Yau S, Pickering RM, Gringras P, Elphick H, Evans HJ, Farquhar M, et al. Sleep in infants and toddlers with Down syndrome compared to typically developing peers: looking beyond snoring. Sleep Med 2019;63:88–97. [DOI] [PubMed] [Google Scholar]
- [97].Sadeh A, Hen-Gal S, Tikotzky L. Young children’s reactions to war-related stress: a survey and assessment of an innovative intervention. Pediatrics 2008;121(1):46–53. [DOI] [PubMed] [Google Scholar]
- [98].Kushnir J, Sadeh A. Assessment of brief interventions for nighttime fears in preschool children. Eur J Pediatr 2012;171(1):67–75. [DOI] [PubMed] [Google Scholar]
- [99].Fitness CoNatCoSMa. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics 2011;127(6):1182–9. [DOI] [PubMed] [Google Scholar]
- [100].Ahluwalia N, Herrick K. Caffeine intake from food and beverage sources and trends among children and adolescents in the United States: review of national quantitative studies from 1999 to 2011. Adv Nutr 2015;6(1): 102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Ahluwalia N, Herrick K, Moshfegh A, Rybak M. Caffeine intake in children in the United States and 10-y trends: 2001–2010. Am J Clin Nutr 2014;100(4):1124–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Temple JL. Review: trends, safety, and recommendations for caffeine use in children and adolescents. J Am Acad Child Adolesc Psychiatry 2019;58(1):36–45. [DOI] [PubMed] [Google Scholar]
- [103].Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health 2015;1(1):15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Brambilla P, Giussani M, Pasinato A, Venturelli L, Privitera F, Miraglia Del GE, et al. Sleep habits and pattern in 1–14 years old children and relationship with video devices use and evening and night child activities. Ital J Pediatr 2017;43(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Gamble AL,, D’Rozario AL, Bartlett DJ, Williams S, Bin YS, Grunstein RR, et al. Adolescent sleep patterns and night-time technology use: results of the Australian Broadcasting Corporation’s Big Sleep Survey. PloS One 2014;9(11):e111700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Dube N, Khan K, Loehr S, Chu Y, Veugelers P. The use of entertainment and communication technologies before sleep could affect sleep and weight status: a population-based study among children. Int J Behav Nutr Phys Activ 2017;14(1):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015;135(2):e367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Power S, Taylor C, Horton K. Sleepless in school? The social dimensions of young people’s bedtime rest and routines. J Youth Stud 2017;20(8): 945–58. [Google Scholar]
- [109].Cespedes EM, Gillman MW, Kleinman K, Rifas-Shiman SL, Redline S, Taveras EM. Television viewing, bedroom television, and sleep duration from infancy to mid-childhood. Pediatrics 2014;133(5): e1163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Browne D, Thompson DA, Madigan S. Digital media use in children: clinical vs scientific responsibilities. JAMA Pediatr 2020;174(2):111–2. [DOI] [PubMed] [Google Scholar]
- [111].Williamson AA, Meltzer LJ, Fiks AG. A stimulus package to address the pediatric sleep debt crisis in the united states. JAMA Pediatr 2020;174(2): 115–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012;130(3):576–84. [DOI] [PubMed] [Google Scholar]
- [113].Owens JA, Dalzell V. Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: a pilot study. Sleep Med 2005;6:63–9. [DOI] [PubMed] [Google Scholar]
- [114].Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, et al. The Sleep Disturbance Scale for Children (SDSC) Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res 1996;5(4):251–61. [DOI] [PubMed] [Google Scholar]
- [115].Lewandowski AS, Toliver-Sokol M, Palermo TM. Evidence-based review of subjective pediatric sleep measures. J Pediatr Psychol 2011;36(7): 780–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev 2011;15(1):19–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Meltzer LJ. Assessment of sleep problems. In: Youngstrom EA, Prinstein MJ, Mash EJ, Barkley RA, editors. Assessment of childhood disorders. 5th ed. New York: Guilford Press; 2020. [Google Scholar]
- [118].Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 2000;23(8):1043–51. [PubMed] [Google Scholar]
- [119].Meltzer LJ, Avis KT, Biggs S, Reynolds AC, Crabtree VM, Bevans KB. The Children’s Report of Sleep Patterns (CRSP): a self-report measure of sleep for school-aged children. J Clin Sleep Med 2013;9(3):235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Meltzer LJ, Biggs S, Reynolds A, Avis KT, Crabtree VM, Bevans KB. The children’s report of sleep patterns - sleepiness scale: a self-report measure for school-aged children. Sleep Med 2012;13(4):385–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Meltzer LJ, Brimeyer C, Russell K, Avis KT, Biggs S, Reynolds AC, et al. The children’s report of sleep patterns: validity and reliability of the sleep hygiene index and sleep disturbance scale in adolescents. Sleep Med 2014;15(12):1500–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003;26(2):213–6. [DOI] [PubMed] [Google Scholar]
- [123].Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics 2004;113(6): e570–7. [DOI] [PubMed] [Google Scholar]
- [124].Mindell JA, Gould RA, Tikotzy L, Leichman ES, Walters RM. Norm-referenced scoring system for the Brief Infant Sleep Questionnaire - Revised (BISQ-R). Sleep Med 2019;63:106–14. [DOI] [PubMed] [Google Scholar]
- [125].Meltzer LJ, Moore M, Mindell JA. The need for interdisciplinary pediatric sleep clinics. Behav Sleep Med 2008;6(4):268–82. [DOI] [PubMed] [Google Scholar]
- [126].Moore KA, Mbwana K, Theokas C, Lippman L, Bloch M, Vandivere S, et al. Child well being: an index based on data of individual children. Washington, DC. 2011 2011. Report No.: 2011–10. [Google Scholar]
- *[127].Matricciani L, Paquet C, Galland B, Short M, Olds T. Children’s sleep and health: a meta-review. Sleep Med Rev 2019;46:136–50. [DOI] [PubMed] [Google Scholar]
- [128].Uong EC, Jeffe DB, Gozal D, Arens R, Holbrook CR, Palmer J, et al. Development of a measure of knowledge and attitudes about obstructive sleep apnea in children (OSAKA-KIDS). Arch Pediatr Adolesc Med 2005;159(2): 181–6. [DOI] [PubMed] [Google Scholar]
- [129].Papp KK, Penrod CE, Strohl KP. Knowledge and attitudes of primary care physicians toward sleep and sleep disorders. Sleep Breath 2002;6(3): 103–9. [DOI] [PubMed] [Google Scholar]
- [130].Mindell JA, Bartle A, Wahab NA, Ahn Y, Ramamurthy MB, Huong HT, et al. Sleep education in medical school curriculum: a glimpse across countries. Sleep Med 2011;12(9):928–31. [DOI] [PubMed] [Google Scholar]
- [131].Gamaldo CE, Salas RE. Sleep medicine education: are medical schools and residency programs napping on the job? Nat Clin Pract Neurol 2008;4(6): 344–5. [DOI] [PubMed] [Google Scholar]
- [132].Mindell JA, Bartle A, Ahn Y, Ramamurthy MB, Huong HT, Kohyama J, et al. Sleep education in pediatric residency programs: a cross-cultural look. BMC Res Notes 2013;6:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Faruqui F, Khubchandani J, Price JH, Bolyard D, Reddy R. Sleep disorders in children: a national assessment of primary care pediatrician practices and perceptions. Pediatrics 2011;128(3):539–46. [DOI] [PubMed] [Google Scholar]
- [134].Meltzer LJ, Phillips C, Mindell JA. Clinical psychology training in sleep and sleep disorders. J Clin Psychol 2009;65(3):305–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Mindell JA, Owens JA. Sleep problems in pediatric practice: clinical issues for the pediatric nurse practitioner. J Pediatr Health Care 2003;17(6): 324–31. [DOI] [PubMed] [Google Scholar]
- [136].Bonuck KA, Schwartz B, Schechter C. Sleep health literacy in head start families and staff: exploratory study of knowledge, motivation, and competencies to promote healthy sleep. Sleep Health 2016;2(1):19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Buckhalt JA, Wolfson AR, El-Sheik M. Children’s sleep and school psychology practice. Sch Psychol Q 2009;24(1):60–9. [Google Scholar]
- [138].Chung KF, Chan MS, Lam YY, Lai CS, Yeung WF. School-based sleep education programs for short sleep duration in adolescents: a systematic review and meta-analysis. J Sch Health 2017;87(6):401–8. [DOI] [PubMed] [Google Scholar]
- [139].Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med Rev 2012;16:355–70. [DOI] [PubMed] [Google Scholar]
- [140].Meltzer LJ, Wainer A, Engstrom E, Pepa L, Mindell JA. Seeing the whole elephant: a scoping review of behavioral treatments for pediatric insomnia. Sleep Med Rev. 2021;56:101410. [DOI] [PubMed] [Google Scholar]
- [141].Malow BA, MacDonald LL, Fawkes DB, Alder ML, Katz T. Teaching children with autism spectrum disorder how to sleep better: a pilot educational program for parents. Clinical Practice in Pediatric Psychology 2016;4(2): 125–36. [Google Scholar]
- [142].Malow BA, Adkins KW, Reynolds A, Weiss SK, Loh A, Fawkes D, et al. Parent-based sleep education for children with autism spectrum disorders. J Autism Dev Disord 2014;44(1):216–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Bonuck KA, Blank A, True-Felt B, Chervin R. Promoting sleep health among families of young children in Head Start: protocol for a social-ecological approach. Prev Chronic Dis 2016;13:E121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a sleep education program for low-income preschool children and their families. Sleep 2014;37(6):1117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Mindell JA, Leichman ES, Walters R, Bhullar B. Development and dissemination of a consumer health information website on infant and toddler sleep. under review. [DOI] [PubMed] [Google Scholar]
- [146].Meltzer LJ, Wainer A, Engstrom E, Pepa L, Mindell JA. Seeing the whole elephant: a scoping review of behavioral treatments for pediatric insomnia. Sleep Med Rev 2020;56:101410. [DOI] [PubMed] [Google Scholar]
- [147].Jackson CL, Walker JR, Brown MK, Das R, Jones NL. A workshop report on the causes and consequences of sleep health disparities. Sleep 2020;43(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Kelly RJ, El-Sheik M. Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol 2014;50(4):1137–47. [DOI] [PubMed] [Google Scholar]
- [149].Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev 2014;18(6):521–9. [DOI] [PubMed] [Google Scholar]
- [150].Bub KL, Buckhalt JA, El-Sheikh M. Children’s sleep and cognitive performance: a cross-domain analysis of change over time. Dev Psychol 2011;47(6):1504–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Friedman NP, Corley RP, Hewitt JK, Wright KP Jr. Individual differences in childhood sleep problems predict later cognitive executive control. Sleep 2009;32(3):323–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Dutil C, Chaput JP. Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutr Diabetes 2017;7(5):e266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].El-Sheikh M, Bub KL, Kelly RJ, Buckhalt JA. Children’s sleep and adjustment: a residualized change analysis. Dev Psychol 2013;49(8):1591–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Hash JB, Oxford ML, Fleming CB, Ward TM, Spieker SJ. Sleep problems, daily napping behavior, and social-emotional functioning among young children from families referred to child protective services. Behav Sleep Med 2019:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Cremone A, McDermott JM, Spencer RMC. Naps enhance executive attention in preschool-aged children. J Pediatr Psychol 2017;42(8): 837–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Miller AL, Seifer R, Crossin R, LeBourgeois MK. Toddler’s self-regulation strategies in a challenge context are nap-dependent. J Sleep Res 2015;24(3):279–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Hoyniak CP, Bates JE, Staples AD, Rudasill KM, Molfese DL, Molfese VJ. Child sleep and socioeconomic context in the development of cognitive abilities in early childhood. Child Dev 2019;90(5):1718–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin 2011;58(3):715–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *[159].Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metabol 2016;41(6 Suppl 3):S266–82. [DOI] [PubMed] [Google Scholar]
- *[160].Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Birken CS, et al. Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years). BMC Publ Health 2017;17(Suppl 5):855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *[161].Short MA, Blunden S, Rigney G, Matricciani L, Coussens S, Reynolds M, et al. Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep Health 2018;4(3):292–300. [DOI] [PubMed] [Google Scholar]
- *[162].Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev 2012;16(3): 231–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Quist JS, Sjodin A, Chaput JP, Hjorth MF. Sleep and cardiometabolic risk in children and adolescents. Sleep Med Rev 2016;29:76–100. [DOI] [PubMed] [Google Scholar]
- [164].Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc 2015; 44(2):405–18. [DOI] [PubMed] [Google Scholar]
- [165].Mindell JA, Lee C, Sadeh A. Young child and maternal sleep in the Middle East. Sleep Med 2017;32:75–82. [DOI] [PubMed] [Google Scholar]
- [166].Lee S, Hale L, Chang AM, Nahmod NG, Master L, Berger LM, et al. Longitudinal associations of childhood bedtime and sleep routines with adolescent body mass index. Sleep 2019;42(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Seifert SM, Schaechter JL, Hershorin ER, Lipshultz SE. Health effects of energy drinks on children, adolescents, and young adults. Pediatrics 2011;127(3):511–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Forrest CB, Meltzer LJ, Marcus CL, de la Motte A, Kratchman A, Buysse DJ, et al. Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep 2018;41(6). [DOI] [PubMed] [Google Scholar]
- [169].Melendres MCS, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics 2004;114(3):768–75. [DOI] [PubMed] [Google Scholar]
- [170].Janssen KC, Phillipson S, O’Connor J, Johns MW. Validation of the epworth sleepiness scale for children and adolescents using rasch analysis. Sleep Med 2017;33:30–5. [DOI] [PubMed] [Google Scholar]
- [171].Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med 2000;1(1):21–32. [DOI] [PubMed] [Google Scholar]
- [172].Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep 2003;26(4):455–8. [PubMed] [Google Scholar]
- [173].Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep 1993;16(3):258–62. [DOI] [PubMed] [Google Scholar]


