PURPOSE
The COVID-19 pandemic created an imperative to re-examine the role of telehealth in oncology. We studied trends and disparities in utilization of telehealth (video and telephone visits) and secure messaging (SM; ie, e-mail via portal/app), before and during the pandemic.
METHODS
Retrospective cohort study of hematology/oncology patient visits (telephone/video/office) and SM between January 1, 2019, and September 30, 2020, at Kaiser Permanente Northern California.
RESULTS
Among 334,666 visits and 1,161,239 SM, monthly average office visits decreased from 10,562 prepandemic to 1,769 during pandemic, telephone visits increased from 5,114 to 8,663, and video visits increased from 40 to 4,666. Monthly average SM increased from 50,788 to 64,315 since the pandemic began. Video visits were a significantly higher fraction of all visits (P < .01) in (1) younger patients (Generation Z 48%, Millennials 46%; Generation X 40%; Baby Boomers 34.4%; Silent Generation 24.5%); (2) patients with commercial insurance (39%) compared with Medicaid (32.7%) or Medicare (28.1%); (3) English speakers (33.7%) compared with those requiring an interpreter (24.5%); (4) patients who are Asian (35%) and non-Hispanic White (33.7%) compared with Black (30.1%) and Hispanic White (27.5%); (5) married/domestic partner patients (35%) compared with single/divorced/widowed (29.9%); (6) Charlson comorbidity index ≤ 3 (36.2%) compared with > 3 (31.3%); and (7) males (34.6%) compared with females (32.3%). Similar statistically significant SM utilization patterns were also seen.
CONCLUSION
In the pandemic era, hematology/oncology telehealth and SM use rapidly increased in a manner that is feasible and sustained. Possible disparities existed in video visit and SM use by age, insurance plan, language, race, ethnicity, marital status, comorbidities, and sex.
INTRODUCTION
With the onset of the COVID-19 pandemic, many health systems worldwide initiated or expanded telehealth programs1 to reduce infectious exposures, and government regulation was introduced to relax restrictions on reimbursement for telehealth.2 ASCO has and continues to advocate for telehealth services as a safer alternative for immunocompromised cancer patients and to facilitate access to health care for patients in historically underserved and rural areas.3 Accordingly, in the United States, since the pandemic began, utilization of telehealth services rapidly increased from a baseline of < 5%4 to about 30% of all patient-provider interactions outside of oncology,5 and about 50% of all community oncology visits.1 Secure messages, which are encrypted asynchronous e-mail–like communications between patients and their providers via a patient portal, have also been increasingly used in medical practices even before the pandemic,6 but it remains unknown to what extent this method of communication has been used more recently in oncology.
CONTEXT
Key Objective
The COVID-19 pandemic, which disproportionately affected historically underserved populations, has accelerated the adoption and use of telehealth (telephone and video visits) and secure messages (e-mails via electronic portal/app) in oncology. This large retrospective study examines the dynamics of telehealth and secure message use, in a large integrated health care system, before and since the pandemic and describes how frequently patients of various demographic groups use these technologies.
Knowledge Generated
Since the COVID-19 pandemic, in our health care system, there has been a sudden shift from office visits toward telehealth, and a continuous gradual increase in use of secure messages. However, we have found that certain historically disadvantaged demographic groups used video visits and secure messages less commonly than others.
Relevance
Recognizing these disparities in telehealth and secure message utilizations, which may have detrimental health effects, is the first necessary step toward improving equity and inclusion in these realms of care.
The COVID-19 pandemic, which disproportionately affected historically underserved populations such as people of color, patients with lower income, and the elderly,7 has brought to the forefront the national discussion on equity in health care. Although telehealth has long been viewed as one way to improve access to care,8 early pandemic era studies show that underserved populations and historically marginalized groups use telehealth less frequently in primary care,9 as well as in cancer care specialties including medical oncology,9,10 gynecologic oncology,11 and psychosocial oncology.12 Secure message utilization for cancer care, even before the pandemic, lagged among older patients, African Americans, and those with lower education, lower earnings, or weak English proficiency.6,13,14
Thus, our study aimed to (1) explore trends and shifts in utilization of office and telehealth visits, as well as secure messages, before and since the COVID-19 pandemic began; and (2) explore disparities in utilization of telehealth and secure messaging (SM) since the pandemic has started among various demographic groups, within a large integrated health care system in Northern California, USA.
METHODS
This study was reviewed by the Institutional Review Board of the Kaiser Permanente Northern California (KPNC) region and was exempt from ethics review or patient consent in accordance with US federal regulations.
Study Setting
We conducted a retrospective cohort study among all patients seen by any of the hematology-oncology practices within the KPNC region. KPNC is an integrated health care system serving more than 4.5 million members, with 262 medical offices, 21 hospitals, and 21 community cancer centers across the region. KPNC encompasses urban, suburban, and semirural areas, and its membership constitutes more than 30% of the population in the counties in which it has a physical presence, and reflects the diversity of the communities it serves.15 When the first community-spread cases of COVID-19 were reported in California in March 2020, KPNC decided to promote outpatient video (or, when not possible, telephone) telehealth visits in lieu of in-person office visits whenever safe and feasible. Since KPNC had an established, although not consistently used,16 telehealth program and secure message technology years before the pandemic,17 mechanisms for telehealth implementation were in place and the practice expanded rapidly.16,18,19 Live interpreter support is available to all patients and providers using KPNC's telehealth services (both phone and video visits). Throughout the study period, no new oncology clinics or hospitals were opened, acquired, or closed by KPNC, the total number of oncology providers was stable around 12820 and did not significantly change, and the number of adult KPNC members has changed by < 2% (internal unpublished data).
Participants and Data Collection
Starting in 2008, KPNC has used an Epic-based electronic health record (EHR) for membership records, as well as demographic and health care information such as utilization, diagnosis, and treatments provided. All data for this study were extracted from the EHR, organizational operational databases, or the 2010 US Census data. All outpatient encounters, including office, video, or telephone visits, as well as secure messages, between a patient and a hematology and/or medical oncology provider (physician or advance practice provider) between January 1, 2019, and September 30, 2020, were collected. Visits for procedures or infusions, as well as inpatient encounters, were excluded. Demographic and other variables were also collected from the EHR, including race and ethnicity (which in our system is self-reported), age, sex, marital status, language/need for interpreter for health care, patient's primary address on the index date (which is defined below), and insurance type (Medicare, Medicaid, commercial, multiple, or other/unknown) on the index date.
Definitions
Since this study focused on patients from Northern California, we chose March 19, 2020—the date of the COVID-19 California shelter-in-place (stay-at-home) order—as the cutoff date for distinguishing the time periods before and during the pandemic. Given the major shifts in patient and provider use of telehealth once the pandemic began, the analyses exploring possible disparities in utilization of telehealth and secure messages were limited to the pandemic era (March 19, 2020, to September 30, 2020).
In our study, we only included visits that were completed, and excluded canceled visits or when a patient did not show. The type of visit was determined on the basis of its classification in the EHR. A video visit was considered completed only if a successful connection was made and both provider and patient were present on the video at the same time, as is documented in databases of our proprietary system for video visits. There may have been instances when a video connection was initially successful but was then switched to a telephone visit because of technical or other reasons, and those visits were classified as video visits in our study.
The index date is the date of the patient's first visit with hematology/oncology in the study period. For analyses related to patients' age at index date, we defined five groups: Generation Z was born in 1997 or later, Generation Y/Millennials between 1981 and 1996, Generation X between 1965 and 1980, Baby Boomers between 1946 and 1964, and the Silent Generation before 1946.21 There were no missing values for age as the date of birth is a mandatory field in our EHR. We chose to categorize patients on the basis of their generation, since it is a static variable that does not change over time, unlike their current age bucket, which is a dynamic variable. In addition, prior research has shown distinct generational differences regarding the use of mobile technologies and attitudes toward the internet.22 The following variables were based on patients' self-report as was documented in the EHR on April 1, 2021: race and ethnicity (categorized as: Asian/Pacific Islander, Black/African American, Hispanic White, non-Hispanic White, or multiple/others/unknown), marital status (single, widowed, divorced, or unknown were grouped together v married/domestic partner), sex (male or female; very few had other listed as sex and were excluded from sex-related comparisons), as well as language/need for interpreter (categorized as English speakers if no interpreter needed was selected in the EHR; if English was not the listed primary language and interpreter required was marked in the EHR, then the patient was categorized as require interpreter). There were no missing data regarding need for interpreter (if this was not marked yes in the EHR, it was considered to be no).
Driving distance to the oncology clinic was calculated by the Graphical Information Systems team at Kaiser Permanente, using the charted primary address for each patient on their index date and the location of their hematology/oncology clinic. Population density was calculated for each of the participating 21 community cancer centers on the basis of data from the American Community Survey,23 and classified as long (top 25%) or short (bottom 75%). Since the patient's address is a mandatory field in their EHR, and since the location of their KPNC oncology clinic is always known, there were no missing values for these variables. Charlson Comorbidity Index24 was calculated by looking at International Classification of Diseases (9th revision) and procedure codes documented in the EHR in the 5 years before the index date, and categorized as < 4 versus ≥ 4. As this index is based on charted EHR information, it had no missing values; however, it may underestimate patients' comorbidities that are not documented appropriately.25 In our health care system, documentation of patient's comorbidities in the EHR is regularly confirmed, and problem lists are carefully maintained by providers and coding experts.
Missing or unknown data were classified as such and included in the analysis. In some cases, missing or unknown data were collapsed with other categories for brevity, and in those cases, this is shown in Figures 1 and 2.
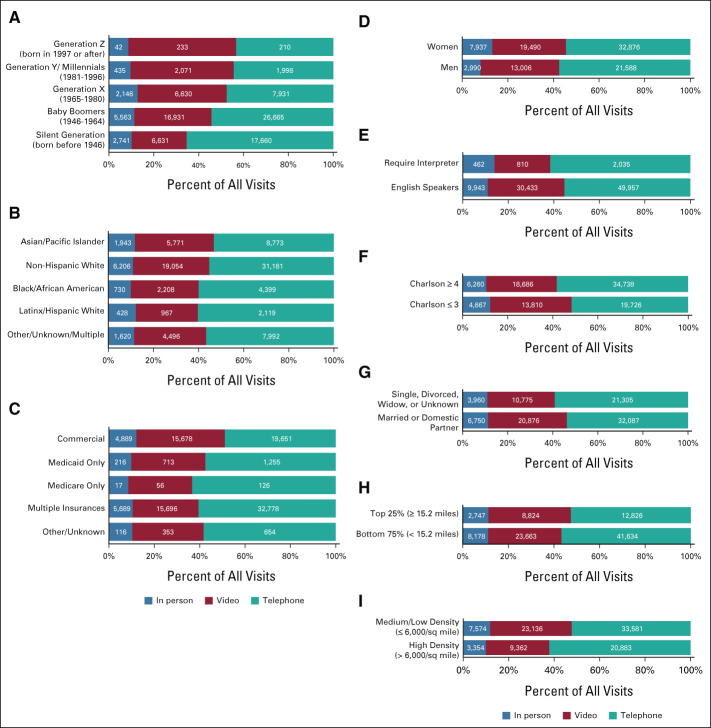
FIG 1.
Proportions and absolute numbers of office, telephone, and video visits between March 19, 2021, and September 30, 2021, by (A) age group, (B) race and ethnicity, (C) insurance type, (D) sex, (E) language/require interpreter, (F) Charlson comorbidity index, (G) marital status, (H) driving distance to clinic, and (I) clinic city population density. Missing/unknown values, when present, were grouped with other categories as described in the figure. Comparisons were made using Pearson's χ2 statistic. P < .01 for all comparisons.
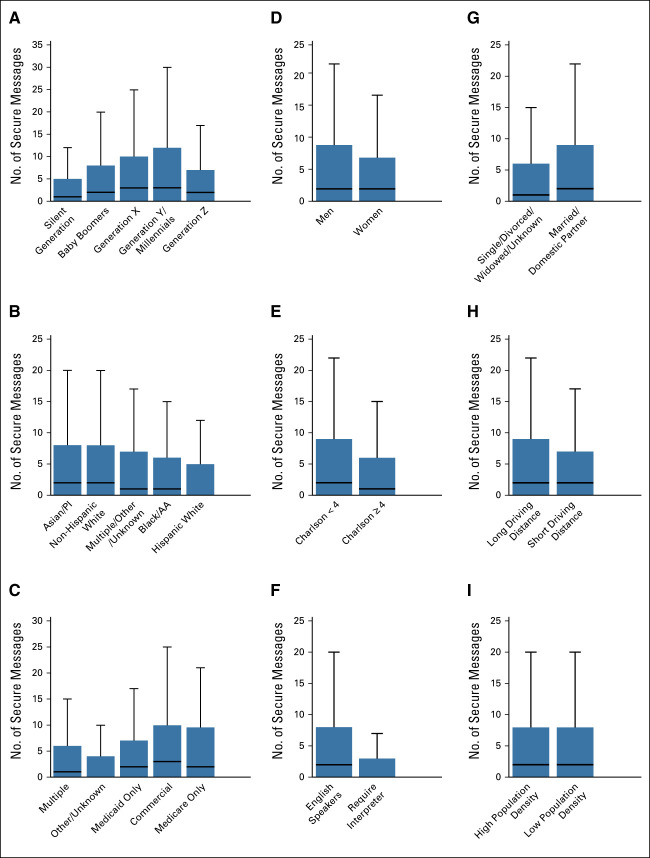
FIG 2.
Total number of secure messages per patient between March 19, 2021, and September 30, 2021, by (A) age group, (B) race and ethnicity, (C) insurance type, (D) sex, (E) Charlson comorbidity index, (F) language/require interpreter, (G) marital status, (H) driving distance to clinic, and (I) clinic city population density. Missing/unknown values, when present, were grouped with other categories as described in the figure. All comparisons were made using Mann-Whitney U test. P < .01 for all comparisons. AA, African American; PI, Pacific Islander.
Analysis
Descriptive statistics (means, medians, and proportions) were used to report distributions of the variables. When reporting fractions of visit types, all percentages are rounded to the nearest tenth. Because of the highly skewed distribution (few patients sent and received numerous times more messages than most other patients), we report medians and interquartile ranges (IQR) for secure message frequencies.
Bivariate comparisons of categorial were calculated using Pearson's χ2 statistic, and the Mann-Whitney U test was used for nonparametric comparisons of continuous data. Interrupted time series models were used to explore the trajectory of the shift away from in-person to telehealth visit. Specifically, we allowed for both a sudden shift toward telehealth (as opposed to in-person) visits and a change in the rate at which telehealth was substituted for in-person visits during the pandemic period compared with the prepandemic period, while controlling for autoregression.26
All analyses were performed with SAS 9.4 (SAS Institute, Carey, NC) and reported P-values < .05 as significant.
RESULTS
Utilization Trends of Office and Telehealth Visits
During the study period, there were 334,666 eligible visits (including telephone, video, or office), 11.7% involved consultations, and the rest were return visits. New consultations, which constituted 12.4% of all visits before the pandemic, decreased to a nadir of 8.6% in May 2020, before returning to 11.7% as of September 2020. Average monthly visits peaked in March 2020 at 15,794 and dropped to a low of 13,692 by May 2020. In total, since the pandemic, the average monthly visits declined by 4.1% from 16,155 to 15,499 (Fig 3A). Looking at specific types of visits (Figs 3B), monthly office visits decreased by 83% from a mean of 10,562 to 1,769, telephone visits increased by 69% from a monthly average of 5,114 to 8,663, and average monthly video visits increased substantially from 40 to 4,666. Interrupted time series analysis showed a statistically significant trend of increase in the fraction of telehealth out of all visits within the prepandemic period (P < .01), a statistically significant sudden shift to telehealth between prepandemic and pandemic periods (P < .01), as well as a statistically significant trend of reduction in telehealth use after the pandemic-related shift (P < .01).
FIG 3.
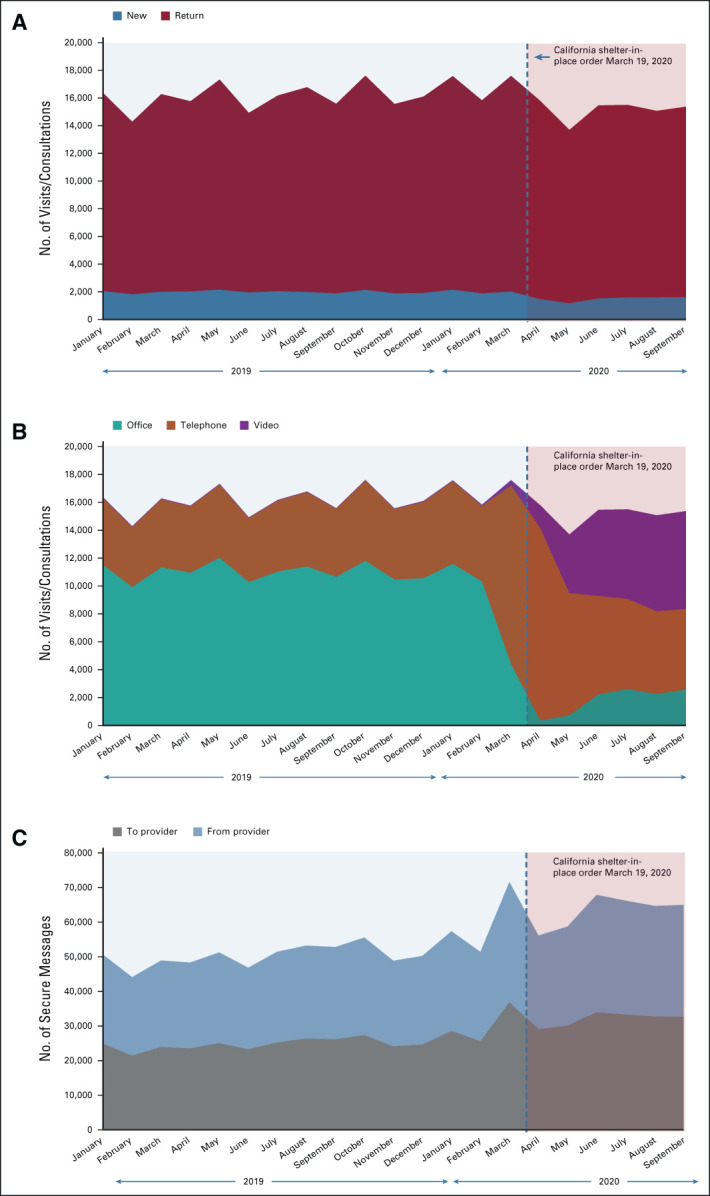
Trends in (A) overall visits, new consultations, (B) utilization of office and telehealth visits, as well as (C) secure messages from January 2019 to September 2020, before and since the COVID-19 pandemic.
Regarding secure messages, 1,161,239 were sent, evenly balanced between communications from patients to providers and from providers to patients. The monthly average gradually increased throughout the entire study period (Fig 3C). The number increased dramatically (41%) during the first month of the pandemic (March 2020) and remained high (26% greater than before the pandemic) throughout the pandemic.
Disparities in Utilization of Telehealth
Since the pandemic and until the end of the study period, a total of 97,887 visits were held with 46,052 patients. Of these visits, 10,927 (11.2%) were in office, 32,496 (33.2%) were by video, and 54,464 (55.6%) were by phone. Visit utilization patterns differed among demographic groups (see Fig 1; P < .01 for all comparisons). The fraction of video visits among all telehealth visits was higher for (1) younger patients compared with older patients (48% for Generation Z, 46% for Millennials/Generation Y, 39.6% for Generation X, 34.4% for Baby Boomers, and 24.5% for Silent Generation); (2) patients who are Asian/Pacific Islander (35%) or non-Hispanic White (33.8%) compared with patients who are Black/African American (30%) or LatinX/Hispanic White (27.5%); (3) patients who have a commercial insurance (39%), compared with those who have only Medicaid insurance (32.6%) or only Medicare (28%); (4) male patients (34.6%) compared with females (32.3%); (5) those who speak English (33.7%) compared with those who need an interpreter (24.5%); (6) those who have a Charlson comorbidity index of three or less (36.2%) versus a (worse) Charlson comorbidity score of four or more (31.3%); (7) those who are married or have a domestic partner (35%) compared with those who are single/divorced/widowed/unknown (29.9%); (8) those who have a longer driving distance to clinic (36.2%) compared with shorter driving distance (32.2%); and (9) those who belong to clinics in less dense cities (36%) compared with more dense cities (27.9%; see Fig 1).
Disparities in Utilization of Secure Messages
Since the pandemic and until the end of the study period, a total of 328,293 secure messages were sent and received by 46,052 patients. The median time interval between the first message in a thread sent by a patient until the first response from a physician was 220 minutes (IQR 34-1,277 minutes), and the median interval between the first message in a thread sent by a physician until the first response from a patient was 153 minutes (IQR 34-1,223 minutes). In the study period, statistically significant differences were noted between demographic groups in the total number of secure messages (Fig 2; P < .01 for all comparisons). Similar to the findings above relating to video visits, the total number of sent and received secure messages was higher, per patient, in (1) younger patients compared with older patients (Millennials/Generation Y: median = 3 and IQR [0-12]; Generation X: 3[0-10]; Baby Boomers: 2[0-8], and Silent Generation: 1[0-5]), except for Generation Z patients who had used less secure messages than expected (median = 2 and IQR [0-8]); (2) patients who are Asian/Pacific Islanders or non-Hispanic Whites (median = 2, IQR [0-8] for both), compared with patients who are Black/African American (1[0-6]) or LatinX/Hispanic White (0[0-5]); (3) patients who have a commercial insurance (3[0-10]), compared with those who have only Medicare insurance (2[0-9]) or only Medicaid (2[0-7]); (4) male patients (2[0-9]) compared with females (2[0-7]); (5) those who speak native English (2[0-8]) compared with those who need an interpreter (0[0-3); (6) those who have a lower Charlson comorbidity index (2[0-9]) versus a higher Charlson comorbidity score (1[0-6]); (7) those who are married or have a domestic partner (2[0-9]) compared with those who are single/divorced/widowed/unknown (1[0-6]); and (8) those who have a longer driving distance to clinic (2[0-9]) compared with shorter driving distance (2[0-7]). There was no difference in the total numbers of secure messages between those who belong to clinics in less dense cities and those in denser cities (2[0-8] for both).
DISCUSSION
Overall, the results of our study exhibited two main themes. First, in our health care system, the COVID-19 pandemic was associated with a rapid shift toward telehealth and away-from-office visits, while the patient and oncology provider populations remained steady. Similar reports were previously published by others27 and us,16,18,19 further supporting the feasibility and ubiquity of these changes.
Second, and more importantly, our study showed that secure messages and video visits were used less often by historically underserved populations such as the elderly, disadvantaged or historically marginalized groups, those without commercial insurance, non-English speakers, and others. Although all the comparisons included in this study are statistically significant (partly because of the large sample size), some of them are more clinically and/or operationally meaningful. For example, the small difference in video visit use between women and men (32.3% v 34.6%, respectively) is not deemed as meaningful as the much larger differences in video visit utilization of the various age groups. To the best of our knowledge, this is the first large study to describe disparities in use of telehealth and secure messages in medical hematology/oncology, across all types of cancers. Our findings were consistent with smaller prior studies that reported telehealth, secure-message, and EHR-portal enrollment-related disparities in various cancer-related disciplines,9-12,28 and they demonstrate that such disparities persisted despite the major shifts toward telehealth since COVID-19 emerged. Our study focused on patients in California, one of the most racially and ethnically diverse state in the United States (by US Census measures29), which outperforms most other states in government benchmarks of equity in health care.30 Kaiser Permanente has promoted equity, inclusion, and diversity throughout its history, and regularly embeds mechanisms to identify and eliminate inequities in its operations,31 and its patient population reflects the racial and ethnic diversity of the population it serves.15 Thus, it is possible that our findings may in fact under-represent the severity of disparities in utilization of telehealth and secure message by patients with cancer across the nation.
Surprisingly, among the various demographic groups, there were only subtle differences in the fraction of office visits out of all visits, and much more pronounced differences in the fraction of video versus telephone visits. This is in contrast to others' findings9 that also showed demographic disparities in use of office versus telehealth visit (video and telephone combined). In our health care system, medical assistants or navigators are in charge of booking patients for visits with hematology/oncology, and patients are not able to independently schedule their own appointments. Although our study was not designed to answer this question, it is hypothesized that in our health care system, it is the provider or the system that commonly decides between office or telehealth visit, but it is the patient or patient characteristics that influence the choice between telephone and video visits.
Our study was also one of the first to describe the volume of SM in oncology, showing that within our health care system, secure message utilization has been rising consistently before and even more so since the pandemic, and suggesting that use of secure messages is becoming a more prevalent method of care delivery in oncology. This study is somewhat limited in that we could not explore the content or themes of the included > 300,000 secure messages; however, we intend to report on this issue in future publications. SM technology is well received by patients32 and may reduce the need for more costly in-person or telehealth visits.14,33 However, the use of SM can have negative potential effects on provider well-being and work-life balance.34,35 Despite the above, secure messages are currently either not billed for or are compensated at a much lower rate compared with office or telehealth visits.36
Regulation on reimbursement for telephone and video visits, by contrast, continues to evolve since the COVID-19 pandemic started, but in certain practice settings, these types of visits are reimbursed at a considerably lower rate than office visits.2,18 The exemptions regarding payment for telehealth by the Centers for Medicare and Medicaid are still considered temporary, and coverage and compensation rates for telehealth services by private insurers are governed by individual state regulations.37 This lack of payment parity between methods of care delivery may affect provider choices in how frequently to see each patient and by which method(s), and/or discourage providers from attending to secure messages in a timely and thoughtful manner, thus potentially leading to insufficient medical supervision with less use of telehealth and secure messages, or increased exposures to COVID-19 and other pathogens with office visits. Additionally, since telephone visits are reimbursed at a much lower rate than video visits in most settings, some providers may not offer telephone visits to their patients and, as such, inadvertently exclude access to telehealth for those who cannot use video. Thus, it is concerning that this lack of payment parity combined with the disparities in use of video visits and secure messages reported herein may disproportionately negatively affect clinical outcomes and quality of life for disadvantaged populations.
There were several limitations to our study. First, it was conducted relatively early during the COVID-19 pandemic and thus may not fully represent the more recent or future evolutions in practice stemming from this pandemic. Second, our study was performed solely in Northern California, an area with one of the highest percentages of broadband internet access,38 and thus, our findings may be less relevant to rural and other areas with less pervasive access to broadband infrastructure. Third, the telehealth-related disparities noted in our study were based on the fraction of telehealth visits out of all visits but not on absolute numbers visits at the individual patient level. This may introduce a bias, as some patient groups may receive a similar fraction of video visits, but have higher or lower absolute number of video visits per patient compared with other groups of patients. However, the concordant disparities seen with absolute numbers of secure messages per patient make that concern less likely. Fourth, some of the demographic variables included herein (ie, race and ethnicity, and sex) were self-reported. There are many ways to describe these intricate social constructs; however, given the complex historical and societal connotations of sex, race, and ethnicity, we believe that self-report is the most appropriate way to describe/determine this information39. Finally, additional research is needed to measure the actual clinical impact of the disparities reported herein.
The future role of telehealth and secure messages in cancer care after the COVID-19 pandemic remains to be determined. However, several indications increasingly suggest that these technologies will continue to take a significant role in an emerging hybrid cancer care delivery model. These include the rapid and sustained uptake of telehealth and secure messages as shown herein, high patient40-42 and provider16 satisfaction with telehealth, the lower-than-desired COVID-19 vaccination rates and ongoing infection waves,43 dispersion of broadband internet technology over time, and the recent recommendations for policymakers to extend current telehealth-related regulatory expansions.44 Indeed, ASCO has advocated for telemedicine policies to remain in place after the public health emergency ends.3
As such, recognizing these disparities in telehealth and secure message utilizations is the first necessary step toward improving equity and inclusion in these realms of care. Specific improvement measures have been suggested by others, including live interpreter services, education and tech support for patients and caregivers, working with local communities to identify public facilities with broadband access for patients to use, and teaching clinicians communication skills specific to telehealth.45 The inherent characteristics of telehealth and SM technologies could be helpful in countering long-standing injustices and discrimination in health care by improving access to care and reducing logistic and financial burdens for caregivers and patients.3,45 Thus, overcoming the disparities in telehealth and secure messaging is a uniquely important and timely issue. Future research should focus on establishing the barriers to effective use of telehealth and secure messaging in various underserved populations, understanding preferences of patients and caregivers from various demographic groups regarding the use of these technologies, and testing interventions to improve access and equity in telehealth and secure messages. In our own health care system, improving equity in telehealth was chosen as the main patient-care equity goal for the department of Hematology and Oncology in 2021, and an extensive patient survey of patients' preferences and barriers relating to telehealth and secure messaging is underway.
Deepika Kumar
Employment: Televital (I)
Tatjana Kolevska
Employment: The Permanente Medical Group
Raymond Liu
Research Funding: Genentech
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented in part at the ASCO annual meeting, virtual, June 4-8, 2021.
SUPPORT
Supported by the Kaiser Permanente Northern California Graduate Medical Education, Kaiser Foundation Hospitals.
AUTHOR CONTRIBUTIONS
Conception and design: Elad Neeman, Hongxin Sun, Deepika Kumar, Tatjana Kolevska, Dinesh Kotak, Raymond Liu
Administrative support: Raymond Liu
Collection and assembly of data: Elad Neeman, Liisa Lyon, Hongxin Sun
Data analysis and interpretation: Elad Neeman, Liisa Lyon, Hongxin Sun, Carol Conell, Mary Reed, Tatjana Kolevska, Tilak Sundaresan, Raymond Liu
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Deepika Kumar
Employment: Televital (I)
Tatjana Kolevska
Employment: The Permanente Medical Group
Raymond Liu
Research Funding: Genentech
No other potential conflicts of interest were reported.
REFERENCES
- 1.2020 Trends in Cancer Care Delivery, Association of Community Cancer Centers,2021. https://www.accc-cancer.org/docs/documents/surveys/2020-trends/2020-trends-fast-facts-two-pdfs.pdf?sfvrsn=9dbbd2ef_2 [Google Scholar]
- 2.GovTrack : Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, HR 6074, 116th Congress, 2020. https://www.govtrack.us/congress/bills/116/hr6074 [Google Scholar]
- 3.Sternberg A: ASCO Submits Comments to Congress Supporting Advanced Measures to Facilitate Telehealth Access, 2021. https://www.cancernetwork.com/view/asco-submits-comments-to-congress-supporting-advanced-measures-to-facilitate-telehealth-access [Google Scholar]
- 4.Claxton G, Rae M, Cox C: Coverage and Utilization of Telemedicine Services by Enrollees in Large Employer Plans.Kaiser Family Foundation and The Peterson Center on Healthcare, 2020. https://www.healthsystemtracker.org/brief/coverage-and-utilization-of-telemedicine-services-by-enrollees-in-large-employer-plans/ [Google Scholar]
- 5.Demeke HB, Merali S, Marks S, et al. : Trends in Use of Telehealth Among Health Centers During the COVID-19 Pandemic—United States, June 26–November 6, 2020, Centers for Disease Control and Prevention, 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7007a3.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heisey-Grove DM, Carretta HJ: Disparities in secure messaging uptake between patients and physicians: Longitudinal analysis of two national cross-sectional surveys. J Med Internet Res 22:e12611, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao YD, Ding M, Dong X, et al. : Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 76:428-455, 2021 [DOI] [PubMed] [Google Scholar]
- 8.Kitamura C, Zurawel-Balaura L, Wong RK: How effective is video consultation in clinical oncology? A systematic review. Curr Oncol 17:17-27, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eberly LA, Kallan MJ, Julien HM, et al. : Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open 3:e2031640, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt AL, Bakouny Z, Bhalla S, et al. : Cancer care disparities during the COVID-19 pandemic: COVID-19 and cancer outcomes study. Cancer Cell 38:769-770, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAlarnen LA, Tsaih SW, Aliani R, et al. : Virtual visits among gynecologic oncology patients during the COVID-19 pandemic are accessible across the social vulnerability spectrum. Gynecol Oncol 162:4-11, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myers Virtue S, Howrey HL, Duffy NM, et al. : Shifting psychosocial oncology care to telepsychology during the COVID-19 pandemic. J Psychosoc Oncol 39:416-427, 2021 [DOI] [PubMed] [Google Scholar]
- 13.Abdel-Rahman O: Patient-related barriers to some virtual healthcare services among cancer patients in the USA: A population-based study. J Comp Eff Res 10:119-126, 2021 [DOI] [PubMed] [Google Scholar]
- 14.Yakushi J, Wintner M, Yau N, et al. : Utilization of secure messaging to primary care departments. Perm J 24, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon N, Lin T: The Kaiser Permanente Northern California adult member health survey. Perm J 20:15-225, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elad N, Tatjana K, Mary R, et al. : Cancer care telehealth utilization rates and provider attitudes in the wake of the novel coronavirus pandemic: The Kaiser Permanente Northern California Experience. Presented at the AACR Virtual Meeting: COVID-19 and Cancer, July 20-22, 2020 (abstr S06-03). Philadelphia, PA, AACR
- 17.Reed ME, Parikh R, Huang J, et al. : Real-time patient-provider video telemedicine integrated with clinical care. N Engl J Med 379:1478-1479, 2018 [DOI] [PubMed] [Google Scholar]
- 18.Tang A, Neeman E, Kuehner G, et al. : The emerging role of telehealth in preoperative evaluation of patients with breast cancer during the COVID-19 pandemic. Presented at the American Society of Breast Surgeons, Virtual, April 29, 2021
- 19.Liu R, Sundaresan T, Reed ME, et al. : Telehealth in oncology during the COVID-19 outbreak: Bringing the house call back virtually. JCO Oncol Pract 16:289-293, 2020 [DOI] [PubMed] [Google Scholar]
- 20.Neeman E, Kumar D, Lyon L, et al. : Attitudes and perceptions of multidisciplinary cancer care clinicians toward telehealth and secure messages. JAMA Netw Open 4:e2133877, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimock M: The Generations Defined. Washington, DC, Pew Research Center, 2019 [Google Scholar]
- 22.Millennials Stand Out for Their Technology Use, but Older Generations Also Embrace Digital Life, Washington, DC, Pew Research Center, 2019. https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/ [Google Scholar]
- 23.American Community Survey (ACS): Population Density Per Square Mile, 2013. https://www.sciencebase.gov/catalog/item/57068007e4b032f77a8a4395 [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, et al. : A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40:373-383, 1987 [DOI] [PubMed] [Google Scholar]
- 25.Savitz ST, Savitz LA, Fleming NS, et al. : How much can we trust electronic health record data? Healthc (Amst) 8:100444, 2020 [DOI] [PubMed] [Google Scholar]
- 26.Penfold RB, Zhang F: Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 13:S38-S44, 2013 [DOI] [PubMed] [Google Scholar]
- 27.Saulet D: How 55 Cancer Programs Are Treating Patients (and Keeping Them Safe) Amid COVID-19, Washington, DC, Advisory Board, 2020 [Google Scholar]
- 28.Sinha S, Garriga M, Naik N, et al. : Disparities in electronic health record patient portal enrollment among oncology patients. JAMA Oncol 7:935-937, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.2020 Census: Racial and Ethnic Diversity Index by State, United States Census Bureau, 2021. https://www.census.gov/library/visualizations/2021/dec/racial-and-ethnic-diversity-index.html [Google Scholar]
- 30.2019 National Healthcare Quality and Disparities Report, Agency for Healthcare Research and Quality, 2019. https://nhqrnet.ahrq.gov/inhqrdr/California/benchmark/summary/All_Measures/All_Topics [PubMed] [Google Scholar]
- 31.Equity, Inclusion, and Diversity, Kaiser Permanente, 2021. https://about.kaiserpermanente.org/our-story/news/equity-inclusion-and-diversity [Google Scholar]
- 32.Baer D: Patient-physician e-mail communication: The Kaiser Permanente experience. J Oncol Pract 7:230-233, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garrido T, Meng D, Wang JJ, et al. : Secure e-mailing between physicians and patients: Transformational change in ambulatory care. J Ambul Care Manage 37:211-218, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lieu TA, Altschuler A, Weiner JZ, et al. : Primary care physicians' experiences with and strategies for managing electronic messages. JAMA Netw Open 2:e1918287, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Akbar F, Mark G, Prausnitz S, et al. : Physician stress during electronic health record inbox work: In situ measurement with wearable sensors. JMIR Med Inform 9:e24014, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moore K, Mullins A, Solis E, et al. : The 2020 Medicare Documentation, Coding, and Payment Update, AAFP, 2020. https://www.aafp.org/fpm/2020/0100/p8.html [PubMed] [Google Scholar]
- 37.Centers for Medicare and Medicaid Services : Telehealth for Providers: What You Need To Know, 2021. https://www.cms.gov/files/document/telehealth-toolkit-providers.pdf [Google Scholar]
- 38.Federal Communications Commission : Fixed Broadband Deployment, 2021. https://broadbandmap.fcc.gov/#/ [Google Scholar]
- 39.Flanagin A, Frey T, Christiansen SL, et al. : Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 326:621-627, 2021 [DOI] [PubMed] [Google Scholar]
- 40.Zimmerman BS, Seidman D, Berger N, et al. : Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: A single center survey-based study. J Breast Cancer 23:542-552, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaverdian N, Gillespie EF, Cha E, et al. : Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J Natl Compr Canc Netw 19:1174-1180, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Darcourt JG, Aparicio K, Dorsey PM, et al. : Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the COVID-19 pandemic. JCO Oncol Pract 17:e36-e43, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.COVID Data Tracker, Centers for Disease Control and Prevention, 2021. https://covid.cdc.gov/covid-data-tracker/ [Google Scholar]
- 44.March 2021 Report to the Congress: Medicare Payment Policy, Medicare Payment Advisory Commission, 2021. http://www.medpac.gov/docs/default-source/reports/mar21_medpac_report_executivesummary_sec.pdf [Google Scholar]
- 45.Lafata JE, Smith AB, Wood WA, et al. : Virtual visits in oncology: Enhancing care quality while designing for equity. JCO Oncol Pract 17:220-223, 2021 [DOI] [PubMed] [Google Scholar]