Abstract
Aims
None of the conventional echocardiographic parameters alone predict increased NTproBNP level and symptoms, making diagnosis of heart failure with preserved ejection fraction (HFpEF) very difficult in some cases, in resting condition. We evaluated LA functions by 2D speckle tracking echocardiography (STE) on top of conventional parameters in HFpEF and preHF patients with diastolic dysfunction (DD), in order to establish the added value of the LA deformation parameters in the diagnosis of HFpEF.
Methods
We prospectively enrolled 125 patients, 88 with HFpEF (68±9 yrs), and 37 asymptomatic with similar risk factors with DD (preHF) (61±8 yrs). We evaluated them by NTproBNP, conventional DD parameters, and STE. Global longitudinal strain (GS) was added. LA reservoir (R), conduit (C), and pump function (CT) were assessed both by volumetric and STE. 2 reservoir strain (S) derived indices were also measured, stiffness (SI) and distensibility index (DI).
Results
LA R and CT functions were significantly reduced in HFpEF compared to preHF group (all p<0.001), whereas conduit was similarly in both groups. SI was increased, whereas DI was reduced in HFpEF group (p<0.001). By adding LA strain analysis, from all echocardiographic parameters, SR_CT<-1.66/s and DI<0.57 (AUC = 0.76, p<0.001) demonstrated the highest accuracy to identify HFpEF diagnosis. However, by multivariate logistic regression, the model that best identifies HFpEF included only SR_CT, GS and sPAP (R2 = 0.506, p<0.001). Moreover, SR_CT, DI, and sPAP registered significant correlation with NTproBNP level.
Conclusions
By adding LA functional analysis, we might improve the HFpEF diagnosis accuracy, compared to present guidelines. LA pump function is the only one able to differentiates preHF from HFpEF patients at rest. A value of SR_CT < -1.66/s outperformed conventional parameters from the scoring system, reservoir strain, and LA overload indices in HFpEF diagnosis. We suggest that LA function by STE could be incorporated in the current protocol for HFpEF diagnosis at rest as a major functional criterion, in order to improve diagnostic algorithm, and also in the follow-up of patients with risk factors and DD, as a prognostic marker. Future studies are needed to validate our findings.
Introduction
Heart failure (HF) with preserved ejection fraction (HFpEF) has a growing prevalence, accounting for approximately 50% of patients with clinical HF syndrome [1–3]. However, despite preserved left ventricular ejection fraction (LVEF), HFpEF patients have high morbidity and mortality, almost similar to patients with reduced EF (HFrEF) [4]. Because the pathophysiological mechanisms underlying HFpEF remain incompletely understood, there is no standard diagnostic algorithm [3–8], and little therapeutic progress has been achieved [9]. Although the newly proposed algorithms H2FPEF [5] and HFA-PEFF [6] tried to identify better HFpEF patients, a significant fraction of patients are still classified discordantly or are classified in the intermediate-likelihood category, where additional testing are needed [3, 6–8]. The current definitions have some limitations: the subjectivity of the symptoms, and the unfeasibility of measurements of cardiac output or filling pressure (invasive), being the most important [10]. Moreover, in real world scenario, not all patients are able to perform echocardiographic exercise stress tests, proposed by the HFpEF consensus. Elevated NTproBNP support, but normal levels do not exclude diagnosis of HFpEF, especially in treated and obese patients [6, 10].
Since 2D echocardiography (2DE) in resting conditions is the most important piece in the diagnosis of HFpEF, we need to better understand and define the transition from asymptomatic DD stage (pre-HFpEF) to symptomatic stage (HFpEF), in terms of echocardiographic parameters [1, 5, 6, 10, 11]. However, none of the conventional parameters alone predict increased NTproBNP level: E/A ratio, E’ velocities, E/E’ ratio, systolic pulmonary arterial pressure (sPAP), and left atrial maximal volume indexed (LAVi max) [12]. The present diagnosis of HFpEF depends on the level of NTproBNP and echocardiographic data, but the sensitivities of both are quite low [10, 13, 14]. In summary, we need an easy-to-do echocardiographic marker, or a sum of markers, able to predict HFpEF, regardless of NTproBNP level. These markers should be thought as a stamp of myocardial dysfunctionality that can be revealed by changing hemodynamic conditions.
In the earlier stage, LV filling pressure (LVFP) is normal at rest, but markedly increases during exercise, while in an advanced stage it increases continuously even at rest [15]. Consequently, prolonged increased LVFP generates structural and functional remodelling of the LA [14]. LAVi assessed by 2DE is already incorporated in new HFpEF scoring system [6], using well established cut-off values for grading severity. These values have strong evidence for prognosis in HF [16]. However, LAVi has no evidence in prediction of HFpEF diagnosis alone, and it is insufficient to identify LA dysfunction. LA deformation analysis, particularly LA reservoir strain, by STE appears to be robust to detect LA dysfunction, and has been shown to carry prognostic value in patients with HFpEF [17, 18].
Previous studies reported preclinical atrial dysfunction, characterized by reduced reservoir and conduit function, with preserved contractile function in stage A of American College of Cardiology/American Heart Association (ACC/AHA) HF stages, prior to overt LA enlargement [19, 20]. Progressive subclinical dysfunction from stage B ACC/AHA leads to a consistently reduction in reservoir and conduit function, with compensatory increase of pump function [20]. Clinical HF, stages C and D, occur when contractile function fails to compensate for reservoir and conduit dysfunction, advanced symptomatic HFpEF being characterized by a significant decrease in all 3 atrial functions [19, 21–23]. At present, there are no clear data regarding parameters that are able to diagnose HFpEF in patients with risk factors and symptoms. This is very important, since the essence of HF treatment is to prevent development of HF in patient with risk factors.
Therefore, we conducted this study to evaluate the added value of the LA functions by STE in diagnosis of HFpEF, on top of conventional parameters used in HFpEF diagnosis.
Materials and methods
Study population
We prospectively enrolled consecutive ambulatory patients with cardiovascular risk factors, signs and symptoms of HF, from January 2018 to January 2020. All patients were referred to our dedicated excellence HF centre to establish if they have HFpEF, according to guidelines [4]. In order to evaluate the prediction power of each echocardiographic parameter for HFpEF diagnosis, patients with HFpEF were compared to a group of patients with similar risk factor profile and DD, but without HF signs and symptoms, and normal NTproBNP level (preHF group), also prospectively enrolled on a 2:1 ratio model (HFpEF:preHF). The study protocol conforms to the ethical guidelines as reflected in a priori approval by the Institution’s Human Research Committee of the Carol Davila University of Medicine and Pharmacy. Informed consent was obtained in all subjects prior to enrolment.
Inclusion criteria for HFpEF group were: age > 18 years, sinus rhythm, stable patient with clinical, biological, and echocardiographic criteria suggestive for HFpEF, according to 2016 guidelines [4], informed consent signed. Exclusion criteria were recent hospitalization for acute HF (< 4weeks), sustained atrial/ventricular arrhythmia, significant valvular heart disease, hypertrophic cardiomyopathy, pericardial disease, previous history of myocarditis, any systemic inflammatory disease or vasculitis, active cancer in the last year, renal failure with haemodialysis, pulmonary causes of dyspnoea, moderate to severe anaemia, inappropriate quality of echocardiographic images for STE analysis. preHF group was selected from the asymptomatic patients with risk factors, without clinical and biological criteria for HFpEF. All patients had clinical examination, 12-lead electrocardiogram, screening laboratory tests, NTproBNP, and a comprehensive 2DE.
Demographic and clinical data were collected before echo protocol (age, gender, BMI, heart rate, systolic and diastolic blood pressure, HF symptoms and NYHA class, if any, HF aetiology, risk factors (hypertension, diabetes mellitus, smoker status, pulmonary diseases, sleep apnea, obesity, dyslipidaemia, ischemic disease documented by ECG, coronarography or other imaging technique). Treatment with all potentially cardiovascular active drugs was recorded on enrolment. After complete evaluation of the patients, the HFA-PEFF score was calculated, according to the current consensus [6].
Echocardiographic protocol
Conventional echocardiography was performed using a Vivid E9 echocardiographic ultrasound system (GE Healthcare, Horten, Norway) with a 3.5 MHz transducer. The electrocardiographic tracing was adjusted to show a well-defined P wave. Standard images were acquired and digitally stored for offline analysis using a vendor specific software Echo PAC PC, version BT12. Echocardiographic protocol included three apical views (four-chamber, two-chamber, and long-axis) optimized for LV, followed by dedicated apical four-chamber and two-chamber views for LA, avoiding foreshortening of the LV and LA, during acquisition. For each view, three consecutive heart cycles were recorded with a frame rate ranging between 50 and 80 frames/sec. A good quality electrocardiogram (ECG) trace with well visible P was recorded. All images were digitally stored and exported to a separate workstation for offline analysis. The operators performing the echocardiographic analysis were blinded to the patient’s clinical and lab details. The quantification of the cardiac chamber size and function was performed in agreement with the current guidelines [16, 24]. LV mass indexed (LVMI) was calculated using the linear method from the parasternal long axis view (Cube formula) and indexed to the body surface area (BSA) [16].
LAVi max was calculated using the biplane disk summation technique and indexed to BSA, as a mean from the apical 4- and 2-chamber views [16]. Transmitral pulsed-wave Doppler velocities (E, A) and tissue Doppler velocities of the septal and lateral mitral annulus were recorded and mean of both velocities was calculated (E’). Tricuspid regurgitant jet velocity and inferior vena cava diameter were measured for the estimation of the sPAP. DD was assessed in a step-by-step algorithm, based on the 2016 American Society of Echocardiography recommendations [24].
LV global longitudinal strain (GS) was measured from apical 2D views (four-, two-, and three-chamber views), by manually tracing the endocardial border of the LV at the end of systole, at the smallest LV chamber size. GS was calculated as the average strain values of all 18 LV segments, according to the guidelines [16].
LA volumetric and functional assessment by 2DE
LA analysis was performed by two experienced operators, experts in STE analysis (RCR and SMB). LA volumetric assessment was done from 4C and 2C dedicated views, and reported as a mean value and indexed by BSA [25], as follows:
LA maximal volume (LAVi max)—volume at the LV end-systole, before the mitral valve opening.
LA pre-A volume (LAVi pre-A)—volume before the onset of the P-wave on the ECG tracing.
LA minimal volume (LAVi min)—volume at the LV end-diastole, after mitral valve closure.
LA phasic functions were generated by using published formulas, based on LA volumes [25]:
- Reservoir function:
Conduit function: LA passive EF = (LAV max—LAV preA)/LAV max x 100
Pump function: LA active EF = (LAV preA–LAV min)/LAV preA x100
LA longitudinal deformation analysis by STE
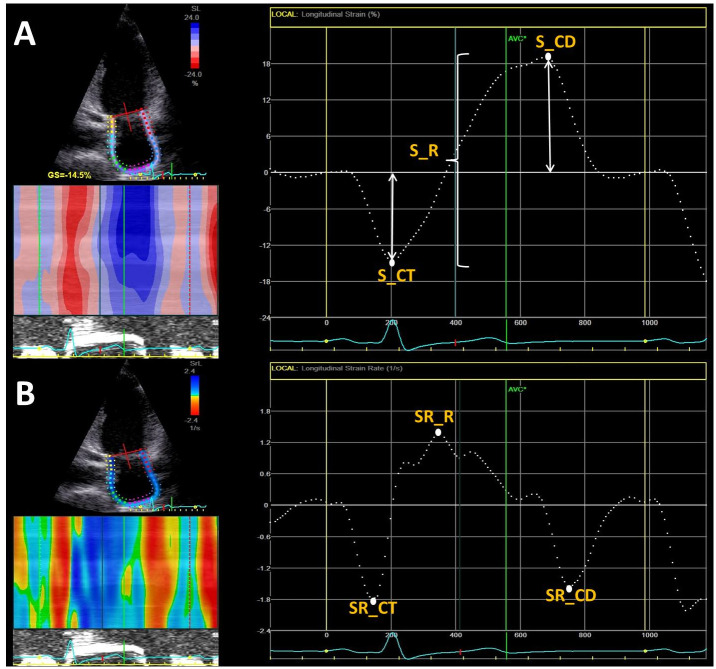
A detailed LA longitudinal deformation evaluation by 2DSTE was published previously by our echocardiography lab [26, 27]. In summary, the LA strain curves were generated by manually tracing the endocardial border in the apical four- and two-chamber views (P-P gating) [27, 28]. The average deformation values from the apical four- and two-chamber views were used for analysis. LA phasic functions were defined as follows:
LA reservoir function: LA reservoir strain (S_R) deformation between MVC to MVO (calculated as the sum between the peak negative longitudinal strain (absolute value), and LA reservoir strain rate (SR_R) during systole, defined as peak positive strain rate from de strain rate curve (Fig 1).
LA conduit function: LA conduit strain (S_CD) as peak positive strain (Fig 1A), and LA conduit strain rate (SR_CD) as peak negative strain rate during early LV diastole.
LA booster pump function: LA contractile strain (S_CT) as peak negative strain (Fig 1A) and strain rate during late diastole, corresponding to atrial contraction, defined as and strain rate (SR_CT) (Fig 1B).
- LA overload indices. We defined two non-invasive indices as markers of LA overload:
- stiffness index (SI), estimated by the ratio between E/E’ ratio and S_R [29], as a marker of pressure overload, representing the amount of pressure required to induce a change in LA deformation during the reservoir phase.
- distensibility index (DI), estimated by the ratio between S_R and LAVi max, as a marker of volume overload, representing the amount of deformation for any volume change of LA, knowing that the excursion is lower for an already dilated LA [30]. We also evaluated the time added for measurement of all LA parameters, in order to estimate how much time adds a functional assessment of the LA at the conventional echocardiographic evaluation proposed by the guidelines.
Fig 1. LA strain by speckle tracking echocardiography.
Example of left atrial strain (panel A) and strain rate (panel B) from four-chamber apical view, using speckle tracking echocardiography, illustrating reservoir, conduit and pump deformation in a diastolic dysfunction patient. S_R, reservoir strain; SR_R, reservoir strain rate; S_CD, conduit strain; SR_CD, conduit strain rate; S_CT, contractile strain, SR_CT, contractile strain rate.
Reproducibility
Intra- and inter-observer variability from our echo lab for all conventional echocardiographic and TDI parameters, and also for STE parameters were already reported elsewhere [27, 31–33]. We also assessed intra- and inter-observer variability for all LA strain and strain rate parameters, on 10 patients that were randomly selected, using an online random selection generator. The intra-observer assessment was performed at 2 weeks apart (RRC). For inter-observer variability assessment, the same patients were analysed by a second blinded observer (SMB).
Statistical analysis
All continuous variables were assessed for the normal distribution by Kolmogorov–Smirnov test. Normally distributed continuous variables were reported as mean ± SD and compared for statistical significance with Independent Samples T Test. Non-normally distributed continuous variables were presented as the median and interquartile range (IQR) and compared using the Mann Whitney U Test. A p value of <0.05 was considered significant. Categorical variables were expressed as percentages and compared with Chi-square test. Correlation between continuous variables was performed using Pearson’s or Spearman’s correlation coefficient as appropriate. Multivariate logistic regression was used to identify predictors of HFpEF and to calculate the corresponding odds ratios. The receiver operating characteristic (ROC) curve was used to identify prediction of HFpEF diagnosis for each echocardiographic parameter and to determine cut-off values. Sensitivity (Se) and specificity (Sp) were calculated. ICCs and their 95% confident intervals were calculated usingSPSS statistical package, based on an absolute-agreement, 2-way mixed-effects model. Statistical analysis was performed using SPSS version 21 (SPSS Inc., Chicago, IL, USA).
Results
Demographics and clinical data
We screened 100 symptomatic patients potentially having HFpEF, and 50 asymptomatic patients with cardiovascular risk factors and DD (preHF). We enrolled prospectively 125 patients, 88 patients with stable HFpEF (HFpEF group), and 37 asymptomatic patients, with cardiovascular risk factors and LVDD (preHF group). 12 patients were excluded from HFpEF group (2 with severe pulmonary diseases, 2 hypertrophic cardiomyopathy, 3 severe anaemia, 5 with images unsuitable for STE analysis). Patients excluded based on the echocardiographic evaluation were because of the inability to obtain optimal images, either for LV or for LA analysis, an essential part of the STE evaluation.
We excluded 13 patients from asymptomatic patients with RF because they do not have DD, according to 2016 guideline. Patients’ characteristics are summarized in Table 1. The two groups are almost similar in terms of demographic and clinical data, except that the HFpEF patients are older (Table 1). As expected, NT-proBNP level was significantly higher in HFpEF group, median 197 pg/ml, IQR (143, 318) vs preHF group, median 42 pg/ml, IQR (24, 68) (P<0.001).
Table 1. Demographic and clinical characteristics of all patients.
| Parameter | preHFpEF | HFpEF | P value |
|---|---|---|---|
| (n = 37) | (n = 88) | ||
| Age (yrs) | 61.4±8.3 | 67.5±9.1 | 0.001 |
| Female (%) | 62 | 75 | 0.15 |
| BMI (kg/m2) | 30.9±4.5 | 29.7±4.9 | 0.2 |
| SBP (mmHg) | 142±17 | 141±22 | 0.91 |
| DBP (mmHg) | 85±9 | 80±11 | 0.03 |
| HR (bpm) | 69±9 | 69±10 | 0.9 |
| Smoker (%) | 24 | 14.8 | 0.1 |
| Arterial hypertension (%) | 97. | 93. | 0.3 |
| Dyslipidaemia (%) | 89 | 89 | 0.8 |
| Diabetes mellitus (%) | 46 | 31 | 0.12 |
| AFib (n, %) | 0 | 17 (19%) | <0.001 |
| BMI >25kg/m2 (%) | 54 | 49 | 0.5 |
| HFA-PEFF score | - | 5.8±0.6 | |
| NYHA class | |||
| Class II (%) | - | 96.4 | |
| Class III (%) | - | 3.6 |
AFib, atrial fibrillation in the medical history. BMI-body mass index, SBP-systolic blood pressure, DBP-diastolic blood pressure, HR-heart rate.
LV structure and functions
LV dimensions, volumes, LVMI, and LVEF were similar in HFpEF and DD groups, but GS was impaired in HFpEF as we expected (Table 2). HFpEF group displayed lower mean E’ velocity, higher E/E’ ratio and sPAP. Regarding the severity of DD, grade 1 predominated in preHF group, whereas grade 2 in HFpEF group (Table 2).
Table 2. Comparison between groups in terms of systolic and diastolic parameters.
| Parameter | preHFpEF | HFpEF | P value |
|---|---|---|---|
| (n = 37) | (n = 88) | ||
| LV structure and systolic function | |||
| IVS (mm) | 12.4±1.9 | 12.0±2.0 | 0.43 |
| PW (mm) | 11±1.8 | 10.9±1.7 | 0.95 |
| LVEDD (mm) | 43.6±4.6 | 45.3±5.3 | 0.09 |
| LVEDVi (ml/m2) | 47.5±9.9 | 46.0±9.8 | 0.45 |
| LVESVi (ml/m2) | 19.97±6.9 | 18.74±5.5 | 0.29 |
| LVEF (%) | 58.8±6.9 | 60.3±5.7 | 0.22 |
| LVMI (kg/ m2) | 94.6±19.6 | 103.2±26.3 | 0.08 |
| GS (%) | -20±3 | -18±3 | <0.001 |
| Diastolic dysfunction | |||
| E (cm/s) | 74.±16. | 81.±22 | 0.07 |
| A (cm/s) | 88.±17.8 | 90.±22 | 0.48 |
| E/A median (IQ) | 0.82 (0.73, 099) | 0.86 (0.71, 1.1) | 0.37 |
| E’ mean (cm/s) | 8.3±1.6 | 7.5±1.7 | 0.014 |
| E/E’ median (IQ) | 9 (7.6, 10.6)) | 10.4 (8.8, 13)- | 0.03 |
| sPAP (mmHg) | 27.9±7.6 | 34.6±8.5 | <0.001 |
| Grade I % (n) | 81(30) | 46 (40) | <0.001 |
| Grade II % (n) | 19 (7) | 53 (48) | <0.001 |
| Grade III % (n) | 0 (0) | 1(1) | 0.52 |
E/A, ratio between peak early to late diastolic mitral inflow peak velocities; E/E’, ratio between early diastolic mitral inflow to mitral annular early diastolic tissue velocities; GS, global strain; IVS, interventricular septum; LVEDD, left ventricular end-diastolic diameter; LVEDVi, left ventricular end-diastolic volume indexed; LVESVi, left ventricular end-systolic volume indexed; LVEF, left ventricular ejection fraction; LVMI, left ventricular mass indexed, PW, posterior wall; sPAP, systolic pulmonary artery pressure.
LA volumes and phasic functions
LAVi max, preA, and min were significantly higher in HFpEF by comparison to preHF group (p<0.001). Reservoir function was significantly impaired in HFpEF compared to preHF (Table 3). LA conduit function was similar in both groups. By contrast, LA pump function was significantly reduced in HFpEF, with lower values of the S_CT, and SR_CT (Table 3). SI was significantly higher, whereas DI was significantly lower in HFpEF compared to preHF group (p<0.001) (Table 3). Time added for all LA strain derived parameters analysis was 148±14 sec (138–159).
Table 3. Left atrial volumes and functions.
| Parameter | preHFpEF | HFpEF | P value |
|---|---|---|---|
| (n = 37) | (n = 88) | ||
| LA volumes | |||
| LAVi max (ml/m2) | 40.3±9.2 | 48.6±11 | <0.001 |
| LAVi pre A(ml/m2) | 27.8±6.9 | 34.3±10.2 | <0.001 |
| LAVi min (ml/m2) | 16.7±5.2 | 22.5±8.8 | <0.001 |
| LA functions | |||
| Reservoir | |||
| Total EF (%) | 58.7±8.0 | 54.6±9.1 | 0.018 |
| Expansion index | 151.6±51.4 | 128.6±43.2 | 0.011 |
| S_R (%) | 25.4±3.8 | 23.3±4.5 | 0.014 |
| SR_R (1/s) | 1.2±0.2 | 1.1±0.3 | 0.383 |
| Conduit | |||
| Passive EF (%) | 31.0±8.9 | 30.0±7.1 | 0.508 |
| S_CD (%) | 10.9±3.2 | 10.1±3.3 | 0.172 |
| SR_CD (1/s) | -1.15±0.4 | -1.14±0.6 | 0.896 |
| Pump | |||
| Active EF (%) | 40.1±8.5 | 35.1±9.7 | 0.009 |
| S_CT (%) | -14.5±2.4 | -13.2±3.1 | 0.030 |
| SR_CT (1/s) | -1.8±0.4 | -1.4±0.5 | <0.001 |
| LA overload indexes | |||
| Stiffness index | 0.4±0.1 | 0.5±0.2 | <0.001 |
| Distensibility index | 0.7±0.2 | 0.5±0.2 | <0.001 |
EF, emptying fraction; LA, left atrium, LAVi, left atrium volume indexed, S_R, reservoir strain. SR_R, reservoir strain rate; S_CD, conduit strain; SR_CD, conduit strain rate; S_CT, strain contraction; SR_CT, strain rate contraction.
Correlations between NT-proBNP level and echocardiographic parameters
All parameters correlated to NT-proBNP are reported in Table 4. NTproBNP best correlated with sPAP, DI, and SR_CT (all p<0.001) (Table 4).
Table 4. Correlations between NT-proBNP and echo parameters.
| Parameter | R correlation | P value |
|---|---|---|
| sPAP (mmHg) | 0.422 | <0.001 |
| Distensibility index | -0.410 | <0.001 |
| SR_CT (1/s) | 0.406 | <0.001 |
| LAVi min (ml/m2) | 0.375 | <0.001 |
| LAVi max (ml/m2) | 0.358 | <0.001 |
| Stiffness index | 0.269 | 0.003 |
| GS (%) | -0.262 | 0.002 |
| E/E’ | 0.230 | 0.010 |
| S_R (%) | -0.178 | 0.047 |
E/E’, ratio between early diastolic mitral inflow to mitral annular early diastolic tissue velocities; GS, global strain; LAVi, left atrium volume indexed; sPAP, systolic pulmonary artery pressure; S_R, reservoir strain; SR_CT, contractile strain rate.
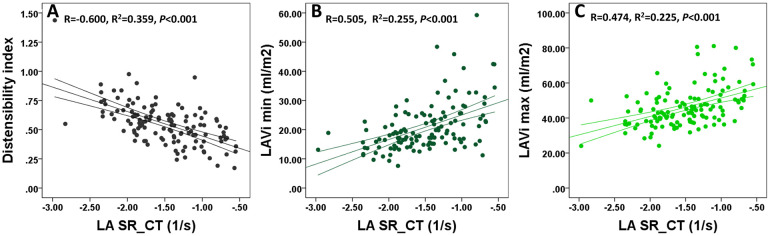
LA pump function correlations
Since from all LA deformation parameters the higher correlation of NT-proBNP was with SR_CT, we evaluated separately the additional correlations of this parameter. The best correlations were with DI, LAVi min and max, and S_CT (Fig 2). LAVi min correlated with SR_CT better then LAVi max. E/E’ ratio registered a weak correlation with SR_CT (Table 5).
Fig 2. Correlations between LA pump function and other parameters.
Correlations between LA pump function and distensibility index (Panel A), LAVi min (Panel B) and LAVi max (Panel C). LAVi, left atrium volume indexed; SR_CT, contractile strain rate.
Table 5. Correlations between LA pump function and other echo parameters.
| Parameter | R correlation | P value |
|---|---|---|
| Distensibility index | -0.60 | <0.001 |
| LAVi min | 0.51 | <0.001 |
| LAVi max | 0.47 | <0.001 |
| S_R | -0.41 | <0.001 |
| Stiffness index | 0.32 | <0.001 |
| GS | 0.27 | 0.002 |
| E/E’ | 0.18 | 0.048 |
E/E’, ratio between early diastolic mitral inflow to mitral annular early diastolic tissue velocities; GS, global strain; LAVi, left atrium volume indexed, S_R, reservoir strain.
Diagnostic performance of the conventional and STE parameters for HFpEF diagnosis
From all parameters included in the current HFpEF algorithm (6), with their cut-off values specified in the guidelines, sPAP >35 mmHg demonstrated the highest accuracy for HFpEF diagnosis, although with limited sensibility and specificity (Table 6, Fig 3). Parameters such as E/E’, E’ velocities, GS, LAVi max, LVMi, LVWT had low accuracy in detection of HFpEF (Table 6, Fig 3).
Table 6. Diagnostic accuracy for HFpEF diagnosis of the guideline and new suggested echocardiographic parameters.
| Cut-off values | AUC | p value | Sensitivity | Specificity | |
|---|---|---|---|---|---|
| LAVi max (ml/m 2 ) | >34 | 0.56 [0.45–0.679] | 0.26 | 96.7% | 16.2% |
| > 43 | 0.71 [0.6091–0.807] | <0.001 | 65.9% | 75.7% | |
| sPAP (mmHg) | >33.5 | 0.678 [0.575–0.782] | 0.002 | 61% | 74.3% |
| >35 | 0.670 [0.567–0.773] | 0.003 | 56.8% | 77.1 | |
| E/E’ | >12 | 0.633 [0.531–0.734] | 0.02 | 34.9% | 91.7% |
| 9–14 | 0.616 [0.504–0.728] | 0.04 | 73% | 50% | |
| >15 | 0.576 [0.47–0.68] | 0.19 | 15% | 100% | |
| E’ medial/lateral (cm/s) | >7/10 | 0.611 [0.501–0.68] | 0.05 | 68.2% | 54.1% |
| LVWT (mm) | >12 | 0.406 [0.299–0.51] | 0.10 | 56.8% | 24.3% |
| LVMi (g/m 2 ) (m/w) | 149/122 | 0.55 [0.443–0.65] | 0.39 | 12% | 97.3% |
| 115/95 | 0.56 [0.446–0.67] | 0.33 | 52% | 60% | |
| GS (%) | < -20 | 0.701 [0.611–0.810] | <0.001 | 72.7% | 67.6% |
| < -16 | 0.616 [0.611–0.810] | 0.04 | 66% | 90% | |
| S_R (%) | < 25 | 0.635 [0.521–0.739] | 0.017 | 69.3% | 56.8% |
| S_CT (%) | > -14.7 | 0.627 [0.523–0.732] | 0.025 | 71.6% | 51.4% |
| SR_CT (1/s) | < -1.66 | 0.760 [0.608–0.811] | <0.001 | 71.6% | 70.3% |
| Stiffness index | > 0.51 | 0.700 [0.609–0.792] | <0.001 | 37.5% | 97.2% |
| Distensibility index | < 0.57 | 0.766 [0.685–0.866] | <0.001 | 69.3% | 83.8% |
E’, diastolic tissue Doppler velocities; E/E’, ratio between early diastolic mitral inflow to mitral annular early diastolic tissue velocities; GS, global strain; LAVi, left atrium volume indexed; LVMi, left ventricle mass indexed; LVWT, left ventricle wall thickness, sPAP, systolic pulmonary artery pressure; S_R, reservoir strain; S_CT, contractile strain; SR_CT, contractile strain rate.
Fig 3. Comparative receiver-operating curves of the conventional echocardiographic parameters for HFpEF diagnosis, between new-proposed and old cut-off values.
Panel A. E/E’ ratio >12 registered a higher accuracy (AUC = 0.633), compared to the old values 9–14 (AUC = 0.616) and >15 (AUC = 0.576); Panel B. Systolic pulmonary artery pressure (sPAP) > 33.5 mmHg (AUC = 0.678) showed a slightly higher accuracy compared to the guidelines value > 35 mmHg (AUC = 0.670). Panel C. Global strain (GS) < -20% demonstrated a significantly higher AUC = 0.727, compared to the consensus proposed value of < -16%; Panel D. Left atrial maximal volume indexed (LAVimax) > 43 ml/m2 predicts better patients with HFpEF, by comparison to the conventional cut-off value >34 ml/m2.
However, we identified a new cut-off value for LAVi max > 43 ml/m2, able to detect HFpEF diagnosis with higher specificity by comparison to the conventional cut-off value (>34 ml/m2) (Sp = 75.7% vs 16.2%) (p<0.001) (Table 6, Fig 3). Moreover, LAVi min > 19.8 ml/m2 had a higher specificity for HFpEF diagnosis than LAVi max. Although E/E’ >12 had very good Sp = 91.7%, the sensitivity for HFpEF diagnosis was extremely low (Table 6). However, by comparison with the cut-off values from the HF consensus, the accuracy was higher (Table 6). GS <-20%, was identified as having a higher AUC than GS < -16%, considered as minor functional criteria in the consensus (Table 6, Fig 3).
From all strain derived parameters, DI and SR_CT were the best parameters able to identify HFpEF, with a cut-off value of <0.57 and < -1.66 /s, respectively (p<0.001). S_R<25% demonstrated lower accuracy for HFpEF diagnosis, by comparison with these two parameters (Fig 4, Table 6).
Fig 4. Comparative receiver-operating curves of guideline and new echocardiographic parameters for HFpEF diagnosis.
The new echocardiographic parameters (Panel B) showed higher AUC compared to all current guideline parameters (Panel A). A combined index of 3 from 5 parameters with the highest AUC (SR_CT, sPAP, GS, DI, LAVi min) identified HFpEF better than the actual guideline index and all parameters alone, including the new ones. LAVi, left atrium volume indexed; E/E’, ratio between early diastolic mitral inflow to mitral annular early diastolic tissue velocities; LVMi, left ventricle mass indexed; sPAP, systolic pulmonary arterial pressure; GS, global strain; SR_CT, LA contractile strain rate; DI, distensibility index; S_R, LA reservoir strain.
When compared the AUC for all newly defined cut-off values, DI and SR_CT were superior to all echocardiographic parameters used for diagnosing HFpEF in scoring system (Fig 4).
According to multivariate logistic regression, using all parameters defined in Table 6, the model that best identified HFpEF included only SR_CT < -1.66 1/s, sPAP >33.5 mmHg, and GS< - 20% (R2 = 0.506, p<0,001) (Table 7). Neither LAVi max/min, nor DI or SI were independent predictors. SR_CT < -1.66 1/s was an independent predictor of HFpEF, and had the most important role in this model, having the highest OR (Table 7).
Table 7. Predictors of HFpEF in multivariate logistic regression.
| Parameter | OR [95% CI] | P value |
|---|---|---|
| SR_CT | 5.829 [1.389–24.451] | 0.016 |
| GS | 1.303 [1.066–1.592] | 0.010 |
| sPAP | 1.129 [1.055–1.209] | 0.001 |
GS, global strain; sPAP, systolic pulmonary arterial pressure; SR_CT, contractile strain rate.
Using parameters with the highest AUC, such as SR_CT, sPAP, GS, DI, LAVi min, with their cutt-off values, we create a combined model (1point for each parameters), in order to see if a combination of parameters might identify HFpEF better than conventional and new parameters alone. A combined index of 3 from 5 parameters identified better HFpEF than SR_CT, DI, sPAP, GS, and than guidelines combined index (AUC = 0.775, Se = 70, Sp = 86%, p<0.001) (Fig 4). By using 4 or 5 parameters of 5, the AUC (0.73 vs 0.62) and Se (52 vs 24%) decrease, whereas Sp increases (95% vs 100%), respectively.
Intra- and inter-observer reproducibility were good to excelent for all LA strain and strain rate parameters (Table 8).
Table 8. Reproducibility of the LA strain parameters by STE.
| Intraobserver | Interobserver | |||||
|---|---|---|---|---|---|---|
| Parameters | MN±SD | ICC | 95% CI | MN±SD | ICC | 95% CI |
| S_R | 22.12±0.56 | 0.984 | 0.845–0.997 | 22.32±0.15 | 0.934 | 0.760–0.983 |
| SR_R | 1.09±0.03 | 0.976 | 0.891–0.994 | 1.09±0.03 | 0.800 | 0.391–0.946 |
| S_CD (%) | 9.38±0.29 | 0.981 | 0.924–0.995 | 9.60±0.14 | 0.937 | 0.771–0.984 |
| SR_CD (1/s) | -0.9±0.02 | 0.974 | 0.902–0.993 | -0.92±0.02 | 0.883 | 0.525–0.971 |
| S_CT (%) | -12.73±0.27 | 0.987 | 0.885–0.997 | -12,72±0.29 | 0.961 | 0.857–0.99 |
| SR_CT (1/s) | -1.59±0.03 | 0.980 | 0.927–0.995 | -1.612±0.02 | 0.970 | 0.891–0.992 |
MN, mean; SD, standard deviation; ICC, intraclass correlation coeficient; CI, confidence interval; S_R, reservoir strain; SR_R, reservoir strain rate; S_CD, conduit strain; SR_CD, conduit strain rate; S_CT, strain contraction; SR_CT, strain rate contraction.
Discussions
In our prospective study we enrolled 125 patients, 88 with stable HFpEF, and 37 asymptomatic LVDD patients without HF, analysed by conventional 2DE and STE, to establish the added value of the LA function in the diagnosis of HFpEF, on top of conventional parameters from the scoring system.
LA functional analysis
To the best of our knowledge, this is the first study that showed that LA pump function and distensibility index, evaluated by STE, are able to detect better HFpEF than any other structural or functional parameter from the 2019 scoring system. A value of SR_CT < -1.66/s and DI <0.57 outperformed conventional parameters, reservoir strain, and GS in HFpEF diagnosis. However, when clinical parameters, standard echocardiographic parameters, LA strain parameters, and GS were included in a multivariate logistic regression, the model that best predicted HFpEF, included only SR_CT, GS, and sPAP, SR_CT having the highest OR in this model. Our study also confirms significant impairment of the reservoir function, with similar conduit function in HFpEF compared to preHF group. Of note all LA strain and strain rate parameters had very good reproducibility in our study, similar to the most recent publications [33, 34].
By comparison to our study, previous studies have shown contradictory data on potential predictors of HFpEF. However, they compared patients with cardiac vs. non-cardiac dyspnoea, regardless of the presence or absence of DD, with other possible confounding factors in the control group [35–37]. Sanchis et al. [35] showed that DI is the best predictor for HF diagnosis. These results could be explained by different patients’ profile (older patients, severely dilated LA, mixed HFpEF and HFrEF patients). It worth mention that we found an almost similar cut-off value for SR_CT as Sanchis et al. (< -1.69/s), however with slightly lower sensitivity and specificity in our case. This might be explained by the differences in patient’s selection. Sanchis et al., in another paper, found that SR_CT< -1.40/s was the best parameter to evaluate prognosis in HF [38].
On the contrary, Reddy et al. [36], found that S_R outperformed the conventional used DD parameters. They found that S_R<24.5% can identify HFpEF (Se = 56%, Sp = 94%) very close to that identified by us, S_R < 25%. Moreover, they found that LA stiffness index was superior to S_R alone in diagnosis of HFpEF. Similarly, we found that SI was superior to S_R, when analysed alone, but both were inferior to SR_CT. The lack of discriminatory power of SR_CT in Reddy’s study might be related to the inclusion of patients with atrial fibrillation.
Compared to these two studies, in which in the control group GS was reduced, in our study, preHF patients had preserved GS, despite increased LAVi max and impaired LA phasic function. In this light, our findings confirm the hypothesis of an earlier LA failure in preHF patients [19].
Telles et al. demonstrated that HFpEF patients compared to patients with non-cardiac dyspnea (NCD), have decreased S_R (24.3±9.6 vs. 36.7±8.4%), SR_R (0.9±0.3 vs. 1.2±0.3/s), S_CT (-11.5±3.2 vs.-17.0±3.4%) and SR_CT (-1.1±0.5 vs. -1.6±0.4/s, p<0.001), with similar conduit function [37]. Our data confirm similar values for reservoir and pump strain in HFpEF patients, but different values for preHF group. Differences can be explained by the enrolment of patients with NCD as control group, without DD. Moreover, they also showed that S_CT identified HFpEF (Se = 94%, Sp = 80%, AUC = 0.88), while S_R (Se = 83%, Sp = 80%, AUC = 0.83) (P<0.001). Both reservoir and pump strain far exceeded the predictive ability of E/E’. By contrast, we found that SR_CT was superior to S_CT in prediction of HFpEF, because our HFpEF group had less severe symptoms (NYHA II class) and less severe dilated LA. The non-invasive SI was also higher in HFpEF patients, as in our study.
In another study, LVH magnitude and atrial dilation/failure provided the best separation between preHF and HFpEF group in hypertensive patients. Their results suggested that atrial function may be a key compensatory mechanism countering evolution of HFpEF, and they highlight the diagnostic utility of atrial failure as a marker of the disease, too [39].
LA morphological analysis
In our study, all LA volumes were significantly increased in HFpEF patients compared to preHF patients. LAVimax >43 ml/m2 can predict HFpEF with significant increased specificity when compared to the guideline value (>34 ml/m2). However, when LAVimax was included in the regression analysis, it did not predict HFpEF. Moreover, we found a better correlation of LAVi min, with SR_CT compared to LAVimax. Previous studies suggested that LAVimin, is a marker of atrial afterload and is more closely related to LVFP, being strongly associated with NT-proBNP than LAVimax [40–42]. Russo et al. [40] found that LAVimin had a strong association with E/E’ ratio, whereas LAVimax had not. Recently, Thadani et al. [42] demonstrated a better predictive power for LAVimin compared to LAVimax for HF hospitalization and cardiovascular outcomes.
Filling pressures analysis
In our study, sPAP and E/E`ratio, considered old surrogates for increased LVFP, demonstrated reduced diagnostic performance for HFpEF diagnosis, when compared to SR_CT and LAVimax. However, when included in a multivariate logistic regression, together with all the classical diastolic and strain parameters, only sPAP was incorporated in the model that best identified HFpEF, with p<0.001. Furthermore, we suggested new cut-off values to increase sensitivity for HFpEF diagnosis, for both sPAP (>33.5 mmHg) and E/E`ratio (>12), by comparison with values suggested by the scoring system.
E/E′ has been the main non-invasive surrogate parameter to predict LVFP. However, many studies demonstrated that E/E′ ratio has a weak correlation with pulmonary capillary wedge pressure (PCWP) in patients with HFpEF [43–48]. Overall, there is a lack of strong evidence in HFpEF patients supporting the utility of E/E′ as an accurate marker of LVFP. Even if the current guidelines [6, 10] use E/E’>15 as a parameter useful for HF diagnosis, this parameter demonstrated very low sensitivity in our study, in line with other studies. Horiuchi et al. found that only sPAP had a strong correlation with PCWP (R = 0.738, p<0.001), E/E`ratio having a weak correlation [49]. Another study demonstrated that tricuspid regurgitation velocity, used to non-invasively estimate sPAP, had the highest predictive value in identifying PCWP>15 mmHg (AUC = 0.89), compared to E/E’ and LAVimax [50]. The poor correlation of E/E’ ratio with LVFP in all studies might be explained by the fact that at least one third of patients with HFpEF may exhibit normal LVFP at rest, with elevated FP only on exertion [51]. In line with these findings, we also found a high performance for sPAP to identify HFpEF, when compared to E/E`ratio.
Lindqvist et al. [34], in a recent publication, demonstrated using invasive evaluation of the LA pressure, that SR_CT was the best accurate component of LA deformation measurements that correlated with PCWP. This parameter had superior accuracy in predicting elevated PCWP compared to recently proposed uni- and multivariable-based algorithms (r2 = 0.60, p < 0.001). Relationship was even stronger in patients with enlarged LA [34].
As 2019 scoring system suggested a multiparametric approach for HFpEF diagnosis, we also evaluated a combined parameter, composed by SR_CT, DI, sPAP, GS, LAVi min, these parameters exceeding the accuracy of conventional parameters. A combination of three from five parameters, was able to predict with the highest accuracy HFpEF diagnosis, by comparison with each parameter alone and by comparison with combined index from the scoring system. In these light, we suggest that these parameters should be validated in larger studies, in order to incorporate them in the scoring system, as functional and structural criteria. We also suggest that functional criteria might have higher contribution than structural ones, in a future alghorithm for HFpEF diagnosis, since than all functional parameters registered a higher accuracy than structural parameters. These parameters could be of particular interest to follow-up the preHFpEF patients to determine whether they progress to HFpEF.
Limitations
Several limitations of our study should be acknowledged. The main limitation was the lack of invasive hemodynamic data. However, invasive assessment in our patients was not clinically indicated. Also, exercise stress echo was not performed in our study because we selected patients with a clear diagnosis of HFpEF. Another limitation was that it was a single centre and single vendor experience (GE). However, our subjects were rigorously selected, representing a reasonable sample. Finally, in terms ofapplicability in clinical practice, it is hard to be confident with strain rate values, since changes in the range of subunit are hard to manage. Most of HFpEF patients were in NYHA functional class II, with grade I and II of LVDD. Hence, further studies, with larger numbers of patients in NYHA functional class III or IV and grade III of LVDD are needed to validate the findings from our study.
Conclusions
Our study demonstrated that by adding LA functional analysis, we might improve the HFpEF diagnosis accuracy, compared to present scoring system. Booster pump function is the only function that differentiates preHF from HFpEF patients. A value of SR_CT < -1.66/s outperformed conventional parameters from the scoring system, reservoir strain, and LA overload indices in HFpEF prediction. We also confirmed that none of the conventional parameters predict alone HFpEF diagnosis, making differentiation between HFpEF and preHF by echocardiography in resting condition impossible. The value of diagnosing HFpEF without the need for stress echo and invasive hemodynamic data is important, since not all patients are able to perform it in real world scenario. We suggest that functional LA analysis by STE could be used to improve diagnostic algorithms of HFpEF, and in the follow-up of HFpEF patients. Further studies are needed to validate our findings in a large population evaluated for HFpEF diagnosis.
Supporting information
(DOCX)
Acknowledgments
Professor Vinereanu Dragos is the head of our group (vinereanu@gmail.com).
Data Availability
All relevant data were placed in a repository. We have made available statistic data on protocols.io. Link:(https://www.protocols.io/joinworkspace/heartpreserved/KOURN;dx.doi.org/10.17504/protocols.io.bzffp3jn) DOI: 10.17504/protocols.io.bzffp3jn.
Funding Statement
This work was supported by 2 National grants of Romanian Ministry of Research and Innovation - UEFISCDI (PN-III-P1-1-TE-2016-0669 (RCR), acronym Heart-Preserved and PN-III-P1-1.2-PCCDI2017-0527, acronym BIOVEA (DV).
References
- 1.Thomas L, Marwick TH, Popescu BA, Donal E, Badano LP. Left Atrial Structure and Function, and Left Ventricular Diastolic Dysfunction: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:1961–77. doi: 10.1016/j.jacc.2019.01.059 [DOI] [PubMed] [Google Scholar]
- 2.Pfeffer MA, Shah AM, Borlaug BA. Heart Failure with Preserved Ejection Fraction in Perspective. Circ Res. 2019;124:1598–617. doi: 10.1161/CIRCRESAHA.119.313572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selvaraj S, Myhre PL, Vaduganathan M, Claggett BL, Matsushita K, Kitzman DW, et al. Application of Diagnostic Algorithms for Heart Failure With Preserved Ejection Fraction to the Community. JACC Hear Fail. 2020;8:640–53. doi: 10.1016/j.jchf.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–2200m. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 5.Reddy YNV, Carter RE, Obokata M, Redfield MM, Borlaug BA. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation. 2018;138:861–70. doi: 10.1161/CIRCULATIONAHA.118.034646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pieske B, Tschöpe C, De Boer RA, Fraser AG, Anker SD, Donal E, et al. How to diagnose heart failure with preserved ejection fraction: The HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40:3297–317. doi: 10.1093/eurheartj/ehz641 [DOI] [PubMed] [Google Scholar]
- 7.Barandiarán Aizpurua A, Sanders-van Wijk S, Brunner-La Rocca HP, Henkens M, Heymans S, Beussink-Nelson L, et al. Validation of the HFA-PEFF score for the diagnosis of heart failure with preserved ejection fraction. Eur J Heart Fail. 2020;22:413–21. doi: 10.1002/ejhf.1614 [DOI] [PubMed] [Google Scholar]
- 8.Sepehrvand N, Alemayehu W, Dyck GJB, Dyck JRB, Anderson T, Howlett J, et al. External Validation of the H2F-PEF Model in Diagnosing Patients with Heart Failure and Preserved Ejection Fraction. Circulation. 2019;139:2377–9. doi: 10.1161/CIRCULATIONAHA.118.038594 [DOI] [PubMed] [Google Scholar]
- 9.Henning RJ. Diagnosis and treatment of heart failure with preserved left ventricular ejection fraction. World J Cardiol. 2020;12:7–25. doi: 10.4330/wjc.v12.i1.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition o. Eur J Heart Fail. 2021;23:352–80. doi: 10.1002/ejhf.2115 [DOI] [PubMed] [Google Scholar]
- 11.Bayes-Genis A, Bisbal F, Núñez J, Santas E, Lupón J, Rossignol P, et al. Transitioning from Preclinical to Clinical Heart Failure with Preserved Ejection Fraction: A Mechanistic Approach. J Clin Med. 2020;9:1110. doi: 10.3390/jcm9041110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galderisi M, Lancellotti P, Donal E, Cardim N, Edvardsen T, Habib G, et al. European multicentre validation study of the accuracy of E/e’ ratio in estimating invasive left ventricular filling pressure: EURO-FILLING study. Eur Heart J Cardiovasc Imaging. 2014;15:810–6. doi: 10.1093/ehjci/jeu022 [DOI] [PubMed] [Google Scholar]
- 13.Michaud M, Maurin V, Simon M, Chauvel C, Bogino E, Abergel E. Patients with high left ventricular filling pressure may be missed applying 2016 echo guidelines: a pilot study. Int J Cardiovasc Imaging. 2019;35:2157–66. doi: 10.1007/s10554-019-01667-w [DOI] [PubMed] [Google Scholar]
- 14.Abergel E, Lafitte S, Mansencal N. Evaluation of left ventricular filling pressure: Updated recommendations lack new evidence and have severe interpretation issues. Arch Cardiovasc Dis. 2018;111:707–11. doi: 10.1016/j.acvd.2018.09.002 [DOI] [PubMed] [Google Scholar]
- 15.Fang NN, Sui DX, Yu JG, Gong HP, Zhong M, Zhang Y, et al. Strain/strain rate imaging of impaired left atrial function in patients with metabolic syndrome. Hypertens Res. Nature Publishing Group; 2015;38:758–64. doi: 10.1038/hr.2015.76 [DOI] [PubMed] [Google Scholar]
- 16.Lang RM, Badano LP, Victor MA, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 17.Obokata M, Negishi K, Kurosawa K, Arima H, Tateno R, Ui G, et al. Incremental diagnostic value of la strain with leg lifts in heart failure with preserved ejection fraction. JACC Cardiovasc Imaging. 2013;6:749–58. doi: 10.1016/j.jcmg.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 18.Santos ABS, Roca GQ, Claggett B, Sweitzer NK, Shah SJ, Anand IS, et al. Prognostic relevance of left atrial dysfunction in heart failure with preserved ejection fraction. Circ Hear Fail. 2016;9:1–12. doi: 10.1161/CIRCHEARTFAILURE.115.002763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bianco CM, Farjo PD, Ghaffar YA, Sengupta PP. Myocardial Mechanics in Patients With Normal LVEF and Diastolic Dysfunction. JACC Cardiovasc Imaging. 2020;13:258–71. doi: 10.1016/j.jcmg.2018.12.035 [DOI] [PubMed] [Google Scholar]
- 20.Brecht A, Oertelt-Prigione S, Seeland U, Rücke M, Hättasch R, Wagelöhner T, et al. Left Atrial Function in Preclinical Diastolic Dysfunction: Two-Dimensional Speckle-Tracking Echocardiography–Derived Results from the BEFRI Trial. J Am Soc Echocardiogr. 2016;29:750–8. doi: 10.1016/j.echo.2016.03.013 [DOI] [PubMed] [Google Scholar]
- 21.Santos ABS, Kraigher-Krainer E, Gupta DK, Claggett B, Zile MR, Pieske B, et al. Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014;16:1096–103. doi: 10.1002/ejhf.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morris DA, Gailani M, Vaz Pérez A, Blaschke F, Dietz R, Haverkamp W, et al. Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr. 2011;24:651–62. doi: 10.1016/j.echo.2011.02.004 [DOI] [PubMed] [Google Scholar]
- 23.Khan MS, Memon MM, Murad MH, Vaduganathan M, Greene SJ, Hall M, et al. Left atrial function in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2020;22:472–85. doi: 10.1002/ejhf.1643 [DOI] [PubMed] [Google Scholar]
- 24.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011 [DOI] [PubMed] [Google Scholar]
- 25.Thomas L, Muraru D, Popescu BA, Sitges M, Rosca M, Pedrizzetti G, et al. Evaluation of Left Atrial Size and Function: Relevance for Clinical Practice. J Am Soc Echocardiogr. 2020;33:934–52. doi: 10.1016/j.echo.2020.03.021 [DOI] [PubMed] [Google Scholar]
- 26.Rimbaş RC, Dulgheru RE, Vinereanu D. Methodological gaps in left atrial function assessment by 2D speckle tracking echocardiography. Arq Bras Cardiol. 2015;105:625–36. doi: 10.5935/abc.20150144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rimbaş RC, Mihăilă S, Vinereanu D. Sources of variation in assessing left atrial functions by 2D speckle-tracking echocardiography. Heart Vessels. 2016;31:370–81. doi: 10.1007/s00380-014-0602-8 [DOI] [PubMed] [Google Scholar]
- 28.Pathan F, D’Elia N, Nolan MT, Marwick TH, Negishi K. Normal Ranges of Left Atrial Strain by Speckle-Tracking Echocardiography: A Systematic Review and Meta-Analysis. J Am Soc Echocardiogr. 2017;30:59–70.e8. doi: 10.1016/j.echo.2016.09.007 [DOI] [PubMed] [Google Scholar]
- 29.Kurt M, Wang J, Torre-Amione G, Nagueh SF. Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging. 2009;2:10–5. doi: 10.1161/CIRCIMAGING.108.813071 [DOI] [PubMed] [Google Scholar]
- 30.Solomon SD, Biering-Sørensen T. LA Strain When Ejection Fraction Is Preserved: A New Measure of Diastolic Function? JACC Cardiovasc Imaging. 2017;10:744–6. doi: 10.1016/j.jcmg.2016.09.018 [DOI] [PubMed] [Google Scholar]
- 31.Rimbaş RC, Mihăilă S, Enescu OA, Vinereanu D. A new comprehensive 12-segment approach to right ventricular systolic and diastolic functions by 2D speckle tracking echocardiography in healthy individuals. Echocardiography. 2016;33:1866–73. doi: 10.1111/echo.13362 [DOI] [PubMed] [Google Scholar]
- 32.Florescu M, Benea DCCM, Rimbas RC, Cerin G, Diena M, Lanzzillo G, et al. Myocardial systolic velocities and deformation assessed by speckle tracking for early detection of left ventricular dysfunction in asymptomatic patients with severe primary mitral regurgitation. Echocardiography. 2012;29:326–33. doi: 10.1111/j.1540-8175.2011.01563.x [DOI] [PubMed] [Google Scholar]
- 33.Cameli M, Miglioranza MH, Magne J, Mandoli GE, Benfari G, Ancona R, et al. Multicentric Atrial Strain COmparison between Two Di ff erent Modalities: MASCOT HIT Study. Diagnostics. 2020;10:946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lindqvist P, Henein M. Left atrial strain rate during atrial contraction predicts raised pulmonary capillary wedge pressure: evidence for left atrio-ventricular interaction. Int J Cardiovasc Imaging. 2021;37:1529–38. doi: 10.1007/s10554-020-02126-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanchis L, Gabrielli L, Andrea R, Falces C, Duchateau N, Perez-Villa F, et al. Left atrial dysfunction relates to symptom onset in patients with heart failure and preserved left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging. 2015;16:62–7. doi: 10.1093/ehjci/jeu165 [DOI] [PubMed] [Google Scholar]
- 36.Reddy YNV, Obokata M, Egbe A, Yang JH, Pislaru S, Lin G, et al. Left atrial strain and compliance in the diagnostic evaluation of heart failure with preserved ejection fraction. Eur J Heart Fail. 2019;21:891–900. doi: 10.1002/ejhf.1464 [DOI] [PubMed] [Google Scholar]
- 37.Telles F, Nanayakkara S, Evans S, Patel HC, Mariani JA, Vizi D, et al. Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur J Heart Fail. 2019;21:495–505. doi: 10.1002/ejhf.1399 [DOI] [PubMed] [Google Scholar]
- 38.Sanchis L, Andrea R, Falces C, Lopez-Sobrino T, Montserrat S, Perez-Villa F, et al. Prognostic Value of Left Atrial Strain in Outpatients with De Novo Heart Failure. J Am Soc Echocardiogr. 2016;29:1035–1042.e1. doi: 10.1016/j.echo.2016.07.012 [DOI] [PubMed] [Google Scholar]
- 39.Melenovsky V, Borlaug BA, Rosen B, Hay I, Ferruci L, Morell CH, et al. Cardiovascular Features of Heart Failure With Preserved Ejection Fraction Versus Nonfailing Hypertensive Left Ventricular Hypertrophy in the Urban Baltimore Community. The Role of Atrial Remodeling/Dysfunction. J Am Coll Cardiol. 2007;49:198–207. doi: 10.1016/j.jacc.2006.08.050 [DOI] [PubMed] [Google Scholar]
- 40.Russo C, Jin Z, Homma S, Rundek T, Elkind MSV, Sacco RL, et al. Left atrial minimum volume and reservoir function as correlates of left ventricular diastolic function: Impact of left ventricular systolic function. Heart. 2012;98:813–20. doi: 10.1136/heartjnl-2011-301388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hedberg P, Selmeryd J, Leppert J, Henriksen E. Left atrial minimum volume is more strongly associated with N-terminal pro-B-type natriuretic peptide than the left atrial maximum volume in a community-based sample. Int J Cardiovasc Imaging. 2016;32:417–25. doi: 10.1007/s10554-015-0800-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thadani SR, Shaw RE, Fang Q, Whooley MA, Schiller NB. Left Atrial End-Diastolic Volume Index as a Predictor of Cardiovascular Outcomes: The Heart and Soul Study. Circ Cardiovasc Imaging. 2020;I:1–9. doi: 10.1161/CIRCIMAGING.119.009746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94. doi: 10.1161/01.cir.102.15.1788 [DOI] [PubMed] [Google Scholar]
- 44.Maeder MT, Karapanagiotidis S, Dewar EM, Gamboni SE, Htun N, Kaye DM. Accuracy of doppler echocardiography to estimate key hemodynamic variables in subjects with normal left ventricular ejection fraction. J Card Fail. 2011;17:405–12. doi: 10.1016/j.cardfail.2010.12.003 [DOI] [PubMed] [Google Scholar]
- 45.Sharifov OF, Schiros CG, Aban I, Denney TS, Gupta H. Diagnostic accuracy of tissue Doppler index E/e’ for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: A systematic review and meta-analysis. J Am Heart Assoc. 2016;5:1–19. doi: 10.1161/JAHA.115.002530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hummel YM, Liu LCY, Lam CSP, Fonseca-Munoz DF, Damman K, Rienstra M, et al. Echocardiographic estimation of left ventricular and pulmonary pressures in patients with heart failure and preserved ejection fraction: a study utilizing simultaneous echocardiography and invasive measurements. Eur J Heart Fail. 2017;19:1651–60. doi: 10.1002/ejhf.957 [DOI] [PubMed] [Google Scholar]
- 47.Nauta JF, Hummel YM, van der Meer P, Lam CSP, Voors AA, van Melle JP. Correlation with invasive left ventricular filling pressures and prognostic relevance of the echocardiographic diastolic parameters used in the 2016 ESC heart failure guidelines and in the 2016 ASE/EACVI recommendations: a systematic review in patients wi. Eur J Heart Fail. 2018;20:1303–11. doi: 10.1002/ejhf.1220 [DOI] [PubMed] [Google Scholar]
- 48.Jones R, Varian F, Alabed S, Morris P, Rothman A, Swift AJ, et al. Meta-analysis of echocardiographic quantification of left ventricular filling pressure. ESC Hear Fail. 2020; doi: 10.1002/ehf2.13119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Horiuchi Y, Tanimoto S, Aoki J, Fuse N, Yahagi K, Koseki K, et al. Mismatch between right- and left-sided filling pressures in heart failure patients with preserved ejection fraction. Int J Cardiol. 2018;257:143–9. doi: 10.1016/j.ijcard.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 50.Romano G, Magro S, Agnese V, Mina C, Di Gesaro G, Falletta C, et al. Echocardiography to estimate high filling pressure in patients with heart failure and reduced ejection fraction. ESC Hear Fail. 2020;7:2268–77. doi: 10.1002/ehf2.12748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Obokata M, Kane GC, Reddy YNV, Olson TP, Melenovsky V, Borlaug BA. Role of Diastolic Stress Testing in the Evaluation for Heart Failure with Preserved Ejection Fraction: A Simultaneous Invasive-Echocardiographic Study. Circulation. 2017;135:825–38. doi: 10.1161/CIRCULATIONAHA.116.024822 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data were placed in a repository. We have made available statistic data on protocols.io. Link:(https://www.protocols.io/joinworkspace/heartpreserved/KOURN;dx.doi.org/10.17504/protocols.io.bzffp3jn) DOI: 10.17504/protocols.io.bzffp3jn.