Abstract
Purpose
1) To investigate the effectiveness of school-based high-intensity interval training (HIIT) interventions in promoting health outcomes of children and adolescents compared with either a control group or other exercise modality; and 2) to explore the intervention characteristics and process outcomes of published school-based HIIT interventions.
Methods
We searched Medline, Embase, CINAHL, SPORTDiscus, and Web of Science from inception until 31 March 2021. Studies were eligible if 1) participants aged 5–17 years old; 2) a HIIT intervention within a school setting ≥ 2 weeks duration; 3) a control or comparative exercise group; 4) health-related, cognitive, physical activity, nutrition, or program evaluation outcomes; and 5) original research published in English. We conducted meta-analyses between HIIT and control groups for all outcomes with ≥ 4 studies and meta-regressions for all outcomes with ≥ 10 studies. We narratively synthesised results between HIIT and comparative exercise groups.
Results
Fifty-four papers met eligibility criteria, encompassing 42 unique studies (35 randomised controlled trials; 36 with a high risk of bias). Meta-analyses indicated significant improvements in waist circumference (mean difference (MD) = -2.5cm), body fat percentage (MD = -1.7%), body mass index (standardised mean difference (SMD) = -1.0), cardiorespiratory fitness (SMD = +1.0), resting heart rate (MD = -5bpm), homeostatic model assessment–insulin resistance (MD = -0.7), and low-density lipoprotein cholesterol (SMD = -0.9) for HIIT compared to the control group. Our narrative synthesis indicated mixed findings between HIIT and other comparative exercise groups.
Conclusion
School-based HIIT is effective for improving several health outcomes. Future research should address the paucity of information on physical activity and nutrition outcomes and focus on the integration and long-term effectiveness of HIIT interventions within school settings.
Trial registration number
PROSPERO CRD42018117567.
Introduction
Recent evidence suggests that vigorous physical activity, as opposed to moderate physical activity, could be driving health benefits, such as reduced cardiometabolic risk, in youth [1–3]. Consequently, there has been an interest in high-intensity interval training (HIIT), defined as short bouts of vigorous exercise followed by recovery periods [4], as a potential method to acquire vigorous physical activity. For example, recent physical activity guidelines have called for research evaluating the effectiveness of HIIT [5, 6]. Available reviews in this area have demonstrated that HIIT can promote favourable changes in cardiometabolic risk, cardiorespiratory fitness (CRF), cognition and wellbeing in youth [7–15]. However, these reviews are confounded by the inclusion of studies conducted within different paediatric groups (e.g., athletic, or clinical populations) and in various settings (e.g., laboratory, school, clinical, and sports settings), introducing heterogeneity [9, 10, 16].
HIIT interventions conducted in the school setting need to be evaluated independently. Schools are an ideal setting for physical activity promotion as they can help reach a large percentage of children and adolescents with their policies and practices, existing infrastructure, and personnel who are or can be trained to support physical actvity [17]. Additionally, school-based interventions have the potential to be scalable and tend to be low cost [18]. However, this setting presents unique challenges, including time constraints, curriculum demands, and teacher workload and training [19]. Previous school-based physical activity interventions have had limited success at increasing physical activity levels [20–23], suggesting that novel approaches and improved delivery are necessary. HIIT may be a promising approach to use in schools given it aligns to habitual physical activity patterns in youth and the intermittent style of most modern sports [24, 25]. It is also associated with greater post-exercise enjoyment than continuous exercise and does not elicit unpleasant feelings [26]. Two recent reviews focused on HIIT in schools [7, 27]; however, recommendations for informing policy advocate for a systematic review with a meta-analysis [28]. Delgado-Floody et al. did conduct a meta-analysis but only focused on HIIT delivered in physical education classes in a population classified as overweight or obese, leading to the inclusion of only six studies [27]. Further, both reviews focused solely on cardiometabolic and fitness outcomes and did not consider outcomes related to psychological wellbeing, learning, nutrition, or program feasibility and sustainability [7, 27]. It is important to assess these outcomes to understand the uptake and sustainability of HIIT programs within the school setting.
Therefore, the objectives of this systematic review were to: 1) investigate the effectiveness of school-based HIIT interventions in promoting physical health, cognitive health, and psychological wellbeing of children and adolescents (5–17 years old); and 2) explore the intervention characteristics and process outcomes of published school-based HIIT interventions.
Methods
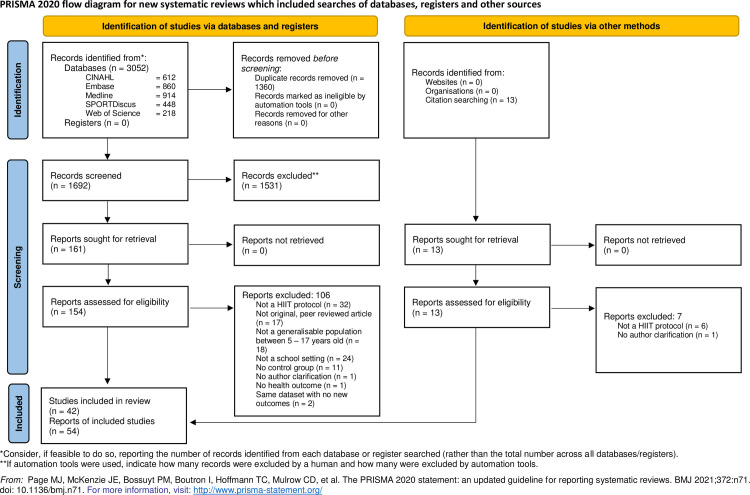
This review follows the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines and was registered with the International Prospective Registry of Systematic Reviews (registration number CRD42018117567).
Search strategy
We conducted a structured electronic search from inception until March 2021 via MEDLINE, EMBASE, CINAHL, SPORTDiscus, and Web of Science using subject headings and keywords related to “high intensity interval training”, “high intensity interval exercise”, “sprint interval training”, “children”, and “adolescents” (S1 File). These terms were selected based on relevant papers and a participant, intervention, comparison, and outcome (PICO) statement [29]. They were trialled and refined with the support of a librarian. Using forward citation chasing, we scanned reference lists of included full-text articles and systematic reviews for additional articles.
Study selection and inclusion and exclusion criteria
After duplicate removal through Endnote (Clarivate Analytics, Philadelphia, USA) and Covidence software (Veritas Health Innovation, Melbourne Australia), titles and abstracts and subsequently full-text articles were screened independently by two reviewers. Discrepancies were resolved with a third reviewer. Articles were considered eligible for inclusion if they: 1) included 5–17-year-olds; 2) examined a HIIT intervention that occurred within a school setting at any point in the school day or before or after school; 3) had a minimum duration of two weeks; 4) had a control or a comparative exercise group; 5) examined outcomes related to health, cognition, physical activity, nutrition, or program evaluation; and 6) were original research articles published in English in peer-reviewed journals. Both randomised control trials (RCTs) and quasi-experimental studies were included as randomisation is not always feasible in school-based studies and informative literature could have been missed if only RCTs were included. We excluded studies if they focused on a specific disease or condition, or the youth athlete. Articles on children classified as obese or overweight were included. We placed no restrictions on the type of activity, intervention frequency, or cut-off intensity for “high-intensity”, if an interval component was included. However, interventions had to be defined as “high-intensity” by the original authors. We attempted to contact authors when information was missing. If authors did not reply within two months, articles were excluded.
Data extraction
Data extraction was conducted by one reviewer and verified by another. We extracted: 1) key characteristics about the study (study design, country), participants (inclusion/exclusion criteria, age, sex), and intervention (HIIT protocol and modality, adherence, attendance, location and time within the school, individual leading the intervention); 2) outcomes examined as specified in our protocol; and 3) results. For study results, we extracted the mean and standard deviation pre- and post-intervention for each group. When reported, we also extracted the mean difference, effect size, group significance, time significance, and group x time significance.
Risk of bias and certainty of evidence
For our risk of bias assessment, we combined and adapted two tools recommended by the Cochrane Collaboration [29]. We used the Risk of Bias-2 (ROB-2) tool, which is designed for randomised studies, and for non-randomised quasi-experimental studies, we included a section of the Risk of Bias in Non-Randomised Studies (ROBINS-I) tool. For missing data, we used a cut-off of 15% based on quality assessments of other exercise interventions [30]. We modified the risk of bias due to deviations from the intended intervention section to appropriately reflect targeted interventions by evaluating adherence (attendance), adverse events, and program fidelity (meeting the desired exercise intensity). Each category received a bias score of “low”, “some concerns”, or “high”. Overall bias was determined using the ROB-2 algorithm. Each study was assessed independently by two reviewers and discrepancies were resolved with a third reviewer. The certainty of evidence for each outcome included in a meta-analysis was assessed using the approach proposed by the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) working group [31]. The evidence was classified into one of four levels of certainty: “high”, “moderate”, “low”, or “very low”. The certainty of the evidence was downgraded due to a high risk of bias, inconsistency within the results (unexplained heterogeneity), indirectness of the findings (lack of generalisability and/or external validity), imprecision (small sample sizes and/or wide confidence intervals) or detected publication bias. The certainty of evidence was upgraded for large effect sizes or if all plausible bias would reduce the determined effect size.
Data synthesis and meta-analyses
For comparisons between the HIIT and control groups, we conducted meta-analyses for outcomes included in four or more studies and narratively synthesised the results for remaining outcomes that were reported in more than one study. For comparisons between HIIT and other exercise groups, we narratively synthesised available results reported in more than one study due to the heterogeneity among comparative group protocols.
Meta-analyses were conducted in R (Version 3.6.2; The R Foundation for Statistical Computing, Vienna, Austria) using the “meta” package. As this review included both randomised and quasi-experimental studies, we used change scores to analyse the effect of HIIT compared with control groups. When change score standard deviations were not reported, they were calculated from standard errors or confidence intervals, or imputed from correlation coefficients derived from other studies [32]. Random effect models were used to allow for variations between studies. For variables with measurements reported on multiple scales, a standardised mean difference (SMD) with inverse proportion weighting was used. For all other variables, the mean difference (MD) was used. Alpha was set at 0.05. We calculated heterogeneity using the I2 statistic, with values between 0% to 40%, 30% to 60%, 50% to 90% and 75% to 100% representing trivial, moderate, substantial and considerable heterogeneity, respectively [29]. We used funnel plots to visually assess publication bias and Egger’s test to quantify asymmetry and determine significance [33, 34].
We conducted meta-regressions and sub-analyses on unadjusted data to determine if the effects of the intervention differed due to intervention characteristics, including: 1) HIIT volume (minutes), defined as the total time performing HIIT including recovery periods but excluding warmup and cooldown, and 2) study duration (weeks). Additionally, meta-regressions were conducted on several participant characteristics: 1) mean age (years); 2) weight status classification (overweight and obese); and 3) sex (percentage of females). We removed the six studies where this percentage was not reported. Lastly, meta-regressions were conducted to understand the effect of study design and bias as follows: 1) RCTs vs quasi-experimental studies; 2) high, some concerns, or low risk of overall bias; and 3) high, some concerns, or low bias due to deviations from the intended intervention. These sensitivity analyses were only completed for meta-analyses with an n > 10 to ensure there was adequate power and to limit false positives [35]. Alpha was set at 0.05 for moderator effects and only significant moderators are reported.
Results
Study characteristics
Fifty-four articles [32, 36–88] were eligible for inclusion in the review (Fig 1), consisting of 42 unique studies after combining the papers by Buchan et al. [46, 47], Costigan et al. [50–52], Cvetković et al. [53, 54], Arariza and Ruiz-Ariza et al. [39, 83], Van Biljon et al. [85, 86], Mucci et al. and Nourry et al. [76, 78], Lambrick et al. and McNarry et al. [63, 73], FIT-First study papers [56, 64] and Burn2Learn study papers [61, 65, 66, 68]. Thirty-nine of 42 studies included a control group, 13 contained an additional comparative group. The majority of the comparative groups included continuous exercise, but two studies used football and two used moderate intensity intervals. Four studies contained two different HIIT protocol groups, of which one combined HIIT and nutritional counselling. Three studies included only a HIIT group with a comparative exercise group. Studies used a variety of modalities within their protocols, including running, cycling, dance, resistance training, circuits, games, strength training, and sports drills. The most common modality was running, and interval lengths within the interventions spanned from 10 seconds to a 4-minute bout of HIIT games. Summary study and HIIT program characteristics are reported in Table 1, with additional details available in Table 2.
Fig 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
HIIT = high-intensity interval training; WoS = Web of Science.
Table 1. Summary of study and program characteristics.
| Characteristic | Category | N | % |
|---|---|---|---|
| Europe | 25 | 59.5 | |
| Africa | 6 | 14.3 | |
| Continent | Australia/New Zealand | 4 | 9.5 |
| Asia | 4 | 9.5 | |
| South America | 3 | 7.1 | |
| Study Design | Randomised | 35 | 83.3 |
| Non-randomised | 7 | 16.7 | |
| Sex | Male and Female | 22 | 52.3 |
| Males only | 7 | 16.7 | |
| Females only | 8 | 19.1 | |
| Not Reported | 5 | 11.9 | |
| Sample Size | <100 | 30 | 71.4 |
| > 100 | 12 | 28.6 | |
| Intervention Length | 2–7 weeks | 13 | 30.9 |
| 8–12 weeks | 23 | 54.8 | |
| > 12 weeks | 6 | 14.3 | |
| Intervention Timing | Before or after school | 4 | 9.5 |
| During school hours | 7 | 16.7 | |
| During PE | 24 | 57.1 | |
| Not reported | 7 | 16.7 | |
| Intervention Frequency | 1–2 times/week | 11 | 26.2 |
| 3 times/week | 28 | 66.7 | |
| 4–5 times/week | 3 | 7.1 | |
| Intervention Facilitator | External Trainers | 5 | 11.9 |
| Researchers | 6 | 14.3 | |
| PE teachers | 7 | 16.7 | |
| Researchers and PE teachers | 4 | 9.5 | |
| Not Reported | 20 | 47.6 | |
| Intensity Results Reported | Heart Rate | 20 | 47.6 |
| Rating of Perceived Exertion | 1 | 2.4 | |
| Percentage of one repetition maximum | 1 | 2.4 | |
| Not reported | 20 | 47.6 | |
| Adverse Events | Yes | 2 (2 students) | 4.8 |
| No | 16 (969 students) | 38.1 | |
| Not reported | 24 | 57.1 | |
| Attendance Reported | Yes | 15 | 35.7 |
| No | 27 | 64.3 |
N = number of studies; PE = physical education; % = the percentage of studies (N / 42) with rounding completed to the nearest 10th.
Table 2. Study characteristics.
| Author (Year) | Sample Size, Age, ˆSex Ratio (Girls/Boys) a | HIIT: | Comparative Exercise Group: | Control Group: | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Duration, Modality, Frequency, Total Volume of HIIT, b | Duration, Modality, Frequency, Total Volume of Exercise, b | Protocol Summary | ||||||||||
| Location, Study Design | ||||||||||||
| Bout Summary and Intensity | ||||||||||||
| Bout Summary and Intensity | ||||||||||||
| Abassi et al. (2020), [36] | 12 weeks, | 12 weeks, | Told to maintain daily living | |||||||||
| 24, | Running, | Running, | ||||||||||
| Tunisia, RCT | 16.5 ± 1.1, | 3 x week, | 3 x week, | |||||||||
| 100.0 / 0.0 | 900 minutes | 900 minutes | ||||||||||
| 6–8 x (30/30)) @ 100–100% MAV | 2 x (6 to 8 x (30/30)) @ 70–80% MAV | |||||||||||
| Adeniran et al. (1988), [37] | 8 weeks, | 8 weeks, | Not Recorded | |||||||||
| 76, | Running, | Continuous Running | ||||||||||
| Nigeria, RCT | 15.6 ± 1.4, | 3 x week, | 3 x week | |||||||||
| 100.0 / 0.0 | 768 minutes | 576 minutes | ||||||||||
| 4 x (240/240) @ > 90% HR Max | 3 miles (@ ≈ 8 min/mile) @ 80–85% HR Max | |||||||||||
| Alonso-Fernandez et al. (2019), [38] Spain, RCT | 7 weeks, | NA | Attended regular PE class | |||||||||
| 28, | Body Weight Exercises, | |||||||||||
| 15–16, | 2 x week, | |||||||||||
| 46.4 / 53.6 | 92 minutes | |||||||||||
| 8 x (20/10) @ NR | ||||||||||||
| Arariza (2018)/ Ruiz Arirza et al. (2019) [39, 83] Spain, RCT | 12 weeks, | NA | Static Stretching | |||||||||
| 184, | Circuit Exercises, | |||||||||||
| 13.7 ± 1.3, | 2 x week, | |||||||||||
| 46.7 / 53.3 | 408 minutes | |||||||||||
| 4 x (20/40) or (25/35) or (30/30) or (35/25) or (40/20) @ > 85% HR Max | ||||||||||||
| Baquet et al. (2001), [41] France, Non-RCT | 10 weeks, | NA | Attended regular PE class | |||||||||
| 551, | Running, | |||||||||||
| 13.0 ± 1.0, | 3 x week, | |||||||||||
| 47.4 / 52.6 | 306 minutes | |||||||||||
| 10 x (10/10) @ 100–120% MAV | ||||||||||||
| Baquet et al. (2002), [40] France, Non-RCT | 7 weeks, | NA | Attended regular PE class | |||||||||
| 53, | Running, | |||||||||||
| 9.9 ± 0.4, | 2 x week, | |||||||||||
| 56.6 / 43.4 | 420 minutes | |||||||||||
| 10 x (10/10) or 5 x (20/20) @ 100–130% MAV | ||||||||||||
| Baquet et al. (2004), [43] France, RCT | 7 weeks, | NA | Attended regular PE class | |||||||||
| 100, | Running, | |||||||||||
| 9.8 ± 0.6, | 2 x week, | |||||||||||
| 54.0 / 46.0 | 420 minutes | |||||||||||
| 10 x (10/10) or 5 x (20/20) @ 110–130% MAV | ||||||||||||
| Baquet et al. (2010), [42] France, RCT | 7 weeks, | 7 weeks, | Attended | |||||||||
| 72, | Running, | Continuous Running, | regular PE | |||||||||
| 9.8 ± 1.2, | 3 x week, | 3 x week, | class | |||||||||
| 47.2 / 52.8 | 492 minutes | 446 minutes | ||||||||||
| 10 x (10/10) or 5 x (20/20) or 5 x (15/15) or 10 x (15/10) or 5 x (30/30) @ 100–130% MAV | 6 to 20 minutes @ 80–85% MAV | |||||||||||
| Ben-Zeev et al. (2020), Israel, RCT | 12 weeks, | NA | Attended | |||||||||
| 40, | Running and resistance training, | regular PE | ||||||||||
| 12–13 | 3 x week, | class | ||||||||||
| 0.0 / 100.0 | 720 minutes, | |||||||||||
| 2 x (30s aerobic / 30s resistance) @ NR | ||||||||||||
| Boddy et al. (2010), [44] England, RCT | 3 weeks, | NA | Not Reported | |||||||||
| 72, | Dance, | |||||||||||
| 9.8 ± 1.2, | 4 x week, | |||||||||||
| 47.2 / 52.8 | 90 minutes | |||||||||||
| 6 x (30/45) @ NR | ||||||||||||
| Bogataj et al. (2020), [45] Serbia, RCT | 8 weeks, | Attended | ||||||||||
| 66 | Body weight exercises | regular PE | ||||||||||
| 15.7 ± 0.6 | 3 x week, + nutritionist 2 x week | class | ||||||||||
| 100.0 / 0.0 | 360 minutes, | |||||||||||
| 10 x (30s/15s) @ 80% Max HR | ||||||||||||
| Buchan et al. (2011), [46, 47] Scotland, Non-RCT | 7 weeks, | 7 weeks, | Attended regular PE class | |||||||||
| 47, | Running, | Continuous Running, | ||||||||||
| 16.3 ± 0.5, | 3 x week, | 3 x week, | ||||||||||
| 21.2 / 78.8 | 105 minutes | 700 minutes | ||||||||||
| 4/5/6 x (30/30) or 6 x (30/20) @ NR | 20 minutes @ 70% VO2 | |||||||||||
| Camacho-Cardenosa et al. (2016), [48] Spain, RCT | 8 weeks, | 8 weeks, | NA | |||||||||
| 47, | Running, | Continuous Running, | ||||||||||
| 16.3 ± 0.5, | 3 x week, | 3 x week, | ||||||||||
| 21.2 / 78.8 | 125 minutes | 125 minutes | ||||||||||
| 3/4/5/6 x (20/60) or 4/5/6 x (20/40) or 4 x (20/20) @ NR | Equivalent time to HIIT workout @ 65–75% HR Max | |||||||||||
| Cheunsiri et al. (2018), [49] Thailand, RCT | 12 weeks, | 12 weeks, | Told to maintain daily living | |||||||||
| 48, | Cycling, | Cycling, | ||||||||||
| 11.0 ± 0.3, | 3 x week | 3 x week, | ||||||||||
| 0.0 / 100.0 | 864 minutes | 144 minutes | ||||||||||
| 8 x (120/60) @ > 90% peak power output | 8 x (20/10) @ > 170% peak power output | |||||||||||
| Costigan et al. (2015/ 2016/2018), [50–52] Australia, RCT | 8 weeks, | 8 weeks, | Attended regular PE class | |||||||||
| 65, | Running, | HIIT Resistance Training, | ||||||||||
| 15.6 ± 0.6, | 3 x week (2 in PE, one at lunch), | 3 x week (2 in PE, one at lunch), | ||||||||||
| 30.8 / 69.2 | 213 minutes | 213 minutes | ||||||||||
| 8/9/10 x (30/30) @ > 85% HR Max | 8/9/10 x (30/30) @ 85% HR Max | |||||||||||
| Cvetkovic et al. (2018), [53, 54] Serbia, RCT | 12 weeks, | 12 weeks, | Not Reported | |||||||||
| 42, | Running, | Football, | ||||||||||
| 11–13, | 3 x week, | 3 x week, | ||||||||||
| 0.0 / 100.0 | 660 minutes | 1080 minutes | ||||||||||
| 5 x (10/10) or 8 x (15/15) or 10 x (20/20) @ 100% MAV | 4 x 8 minutes of playing @ NR | |||||||||||
| Delgado Floody et al. (2018), [55] Chile, Non-RCT | 28 weeks, | NA | Attended regular PE class | |||||||||
| 197, | Running, Jumps, Throws | |||||||||||
| 8.4 ± 1.2, | 2 x week, | |||||||||||
| 54.8 / 45.2 | NR (≈ 1512 minutes) | |||||||||||
| 2/3/4 x (30-60/30-60) @ 80–95% HR Max | ||||||||||||
| Elbe et al. (2016)/ Larsen et al. (2017), [56, 64] Denmark, RCT | 44 weeks, or | 44 weeks | 44 weeks, or | 44 weeks, | Attended regular PE class | |||||||
| 300, | Running, or | Strength and Games | Football, or | Football, | ||||||||
| 9.3 ± 0.4, | 5 x week, or | 3 x week, | 5 x week, | 3 x week, | ||||||||
| 52.6 / 47.4 | 2640 minutes | 5280 minutes | 2640 minutes | 5280 minutes | ||||||||
| 8 x (60/30) @ NR | 6–10 x (30/45) @ NR | Continuous play | Continuous play | |||||||||
| Espinoza-Silva et al. (2019), [57] Chile, Non-RCT | 28 weeks, | NA | Attended regular PE class | |||||||||
| 274, | Running, Jumps, Throws | |||||||||||
| 7–9, | 2 x week, | |||||||||||
| 56.2 / 43.8 | NR (≈ 1960 minutes) | |||||||||||
| NR x (30-60/60-120) and 3–4 x (240/60-120) | ||||||||||||
| @ 8–10 RPE | ||||||||||||
| Gamelin et al. (2009), [58] France, RCT | 7 weeks, | NA | Not Recorded | |||||||||
| 38, | Running, | |||||||||||
| 9.6 ± 1.2, | 3 x week, | |||||||||||
| 50.0 / 50.0 | 492 minutes | |||||||||||
| 10 x (10/10) or 5 x (20/20) or 5 x (15/15) or 10 x (15/10) or 5 x (30/30) or 2o x (5/15) | ||||||||||||
| @ 100–130% MAV | ||||||||||||
| Granacher et al. (2011), [59] Switzerland, RCT | 10 weeks, | NA | Attended regular PE class | |||||||||
| 34, | Strength Training, | |||||||||||
| 8.6 ± 0.5, | 2 x week, | |||||||||||
| 43.8 / 56.2 | 1400 minutes | |||||||||||
| 3 x (10–12 reps/180-240s) | ||||||||||||
| @ 70–80% 1 rep max | ||||||||||||
| Haghshenas et al. (2019) [60] Iran, RCT | 8 weeks, | NA | Active walks in the school yard | |||||||||
| 100, | Running, | |||||||||||
| 14.0 ± 1.0, | 3 x week, | |||||||||||
| 0.0 / 100.0 | 430.5 minutes | |||||||||||
| 2–4 (60-120/240/300) | ||||||||||||
| @ NR MAV | ||||||||||||
| Ketelhut et al. (2020), [62] Germany, RCT | 12 weeks, | NA | Attended regular PE class | |||||||||
| 46, | Games, Circuits, Choreographies | |||||||||||
| 10.8 ± 0.6, | 2 x week, | |||||||||||
| 45.7 / 54.3 | 480 minutes | |||||||||||
| 2–6 x (20-120/30-90) | ||||||||||||
| @NR HR Max | ||||||||||||
| Lambrick et al. (2016)/McNarry et al. (2015), [63, 73] England, RCT | 6 weeks, | NA | Attended regular PE class | |||||||||
| 55, | Games | |||||||||||
| 9.2 ± 0.8, | 2 x week, | |||||||||||
| 45.5 / 54.5 | 408 minutes | |||||||||||
| 6 x (360/120) games and 4 min circuit | ||||||||||||
| @> 85% HR Max | ||||||||||||
| Logan et al. (2016), [63] New Zealand, RCT | 8 weeks, | NA | ||||||||||
| 24, | Aerobic and Resistance | |||||||||||
| 16.0 ± 1.0, | 3 x week (2 HIIT, 1 resistance), | |||||||||||
| 0.0 / 100.0 | 173.3 minutes | 234.7 minutes | 296.0 minutes | 357.3 minutes | 418.7 minutes c | |||||||
| 1 x (4 x 20/10) | 2 x (4 x 20/10) | 3 x (4 x 20/10) | 4 x (4 x 20/10) | 5 x (4 x 20/10) | ||||||||
| Resistance = 3 x 8–12 of 3 compound movements | ||||||||||||
| @ 90–100% HR Max for HIIT and 70% 1RM for Resistance | ||||||||||||
| Lubans et al. (2020)/Kennedy et al. (2020)/Leahy et al. (2019)/ Leahy et al. (2020), [61, 65, 66, 68] Australia, RCT | 52 weeks, | NA | Attended regular PE class | |||||||||
| 670, | Aerobic, Resistance, Dance, Boxing | |||||||||||
| 16.0 ± 0.4, | 3 x week (½ year: 2 in PE, one own time, ½ year: all own time), | |||||||||||
| 44.6 / 55.4 | ≈ 1248 minutes (using 8 min average/session and 52 weeks) | |||||||||||
| 8–16 x (30/30) | ||||||||||||
| @> 85% HR Max | ||||||||||||
| Martin et al. (2015), [69] Scotland, RCT | 7 weeks, | NA | Attended regular PE class | |||||||||
| 49, | Running, | |||||||||||
| 16.9 ± 0.4 | 3 x week, | |||||||||||
| 24.5 / 75.5 | 108 minutes | |||||||||||
| 4–6 x (30/30) | ||||||||||||
| @ NR | ||||||||||||
| Martin-Smith et al. (2018), [70] Scotland, RCT | 4 weeks, | NA | Attended regular PE class | |||||||||
| 56, | Running, | |||||||||||
| 17 ± 0.3 | 3 x week, | |||||||||||
| 37.5 / 62.5 | 66 minutes | |||||||||||
| 5–6 x (30/30) | ||||||||||||
| @ NR (used a sprint pacer) | ||||||||||||
| McManus et al. (1997), [71] England, RCT | 8 weeks, | 8 weeks, | Not Reported | |||||||||
| 45, | Running, | Continuous Cycling, | ||||||||||
| 9.6 ± 0.5 | 3 x week, | 3 x week, | ||||||||||
| 100.0 / 0.0 | 304 minutes | 320 minutes | ||||||||||
| 3–6 x (10/30) and 3–6 x (30/90) | 20 minutes | |||||||||||
| @ NR (used a distance) | @ 80–85% HR Max | |||||||||||
| McManus et al. (2005), [72] Hong Kong, RCT | 8 weeks, | 8 weeks, | Not Reported | |||||||||
| 45, | Cycling, | Continuous Cycling, | ||||||||||
| 10.4 ± 0.5 | 3 x week, | 3 x week, | ||||||||||
| 0.0 / 100.0 | 320 minutes | 320 minutes | ||||||||||
| 7 x (30/165) | 20 minutes | |||||||||||
| @ Peak Power elicited during VO2 test | @ 70–85% HR Max | |||||||||||
| McNarry et al. d (2020), [74] Wales, RCT | 26 weeks, | NA | Not Reported | |||||||||
| 33, | Circuits and Games, | |||||||||||
| 13.5 ± 0.8 | 3 x week, | |||||||||||
| 45.4 / 55.6 | 1890 minutes | |||||||||||
| (10-30/10-30) | ||||||||||||
| @ > 90% HR Max | ||||||||||||
| Moreau et al. (2017), [75] New Zealand, RCT | 6 weeks, | NA | Board Games | |||||||||
| 305, | Video Workouts, | |||||||||||
| 9.9 ± 1.7 | 5 x week, | |||||||||||
| 61.3 / 38.7 | 150 minutes | |||||||||||
| 1 x (20/20) and 1 x (20/30) and 1 x (20/40) and 1 x (20/50) and 1 x (20/60) | ||||||||||||
| @ NR | ||||||||||||
| Mucci et al. (2013)/ Nourry et al. (2005), [76, 78] France, RCT | 8 weeks, | NA | Not Recorded | |||||||||
| 18, | Running, | |||||||||||
| 10.0 ± 0.7 | 2 x week, | |||||||||||
| 38.9 / 61.1 | 198 minutes | |||||||||||
| 10 x (10/10); 5 x (20/20); 5 x (15/15); 10 x (15/10); 5 x (30/30) | ||||||||||||
| @ 100–130% MAV | ||||||||||||
| Muntaner-Mas et al. (2017), [77] Spain, RCT | 16 weeks, | NA | Attended regular PE class | |||||||||
| 80, | Circuit, | |||||||||||
| 15.8 ± 0.5 | 2 x week, | |||||||||||
| NR | 320 minutes | |||||||||||
| 10 x (45/15) | ||||||||||||
| @ > 85% Max HR | ||||||||||||
| Racil et al. (2013), [79] Tunisia, RCT | 12 weeks, | 12 weeks, | Not Recorded | |||||||||
| 36, | Running, | Running | ||||||||||
| 15.9 ± 1.2 | 3 x week, | 3 x week, | ||||||||||
| 100.0 / 0.0 | 672 minutes | 672 minutes | ||||||||||
| 6–8 x (30/30) | 6–8 x (30/30) | |||||||||||
| @ 100–100% MAV and 50% MAV on rest | @ 70–80% MAV and 50% MAV on rest | |||||||||||
| Racil et al. (2016a), [80] Tunisia, RCT | 12 weeks, | 12 weeks, | Not Recorded | |||||||||
| 47, | Running, | Running | ||||||||||
| 14.2 ± 1.2 | 3 x week, | 3 x week, | ||||||||||
| 100.0 / 0.0 | 440 minutes | 440 minutes | ||||||||||
| 4–8 x (15/15) | 4–8 x (15/15) | |||||||||||
| @ 100 MAV and 50% MAV on rest | @ 80% MAV and 50% MAV on rest | |||||||||||
| Racil et al. (2016b), [81] Tunisia, RCT | 12 weeks, | 12 weeks, | Not Recorded | |||||||||
| 75, | Running, | Running and Plyometrics | ||||||||||
| 16.6 ± 0.9 | 3 x week, | 3 x week, | ||||||||||
| 100.0 / 0.0 | 672 minutes | 996 minutes | ||||||||||
| 6–8 x (30/30) | 4 x (15/15) for plyometrics | |||||||||||
| 6–8 x (30/30) for sprints | ||||||||||||
| @ 100% MAV and 50% MAV on rest | @ 100% MAV and 50% MAV on rest | |||||||||||
| Reyes Amigo et al. (2021), [82] Chile, RCT | 11 weeks, | 11 weeks, | NA | |||||||||
| HIIT Games, | Moderate Intensity Games, | |||||||||||
| 48, | 2 x week, | 2 x week, | ||||||||||
| 9.5 ± 0.5 | 510 minutes, | 510 minutes, | ||||||||||
| 66.7 / 33.3 | 4 x (6-minute intermittent game) | 4 x (6-minute continuous game) | ||||||||||
| @75–95% Max HR or 6–8 / 10 RPE | @60–74% Max HR or 4–5 / 10 RPE | |||||||||||
| Segovia et al. (2020), [84] Spain, RCT | 6 weeks, | NA | Played Ringo | |||||||||
| 154 | Games and Circuit, | In regular | ||||||||||
| 10.7 ± 0.8 | 2–3 x week, | PE class | ||||||||||
| 47.4 / 52.6 | 195 minutes | |||||||||||
| 1 x 300–420 for games | ||||||||||||
| 5–8 x (40/20) for circuit | ||||||||||||
| @85–90% | ||||||||||||
| Van Biljon et al. (2018), [85, 86] South Africa, Non-RCT | 5 weeks, | 5 weeks, | 5 weeks, | Not Recorded | ||||||||
| 120, | Running, | Walking, | Alt. Running and Walking | |||||||||
| 11.1 ± 0.8 | 3 x week, | 3 x week, | 3 x week, | |||||||||
| 61.4 / 38.6 | 337.5 minutes | 495 minutes | 400.5 minutes | |||||||||
| 10 x (60/75) @ > 80% Max HR | 33 minutes @ 65–70% Max HR | 3 weeks of sprints 2 weeks of walking | ||||||||||
| Weston et al. (2016), [87] England, Non-RCT | 10 weeks, | NA | Attended regular PE class | |||||||||
| 101, | Dance, Soccer, Boxing, Basketball | |||||||||||
| 14.1 ± 0.3 | 3 x week (2 in PE, 1 after school/at lunch), | |||||||||||
| 37.6 / 62.4 | 119.3 minutes | |||||||||||
| 4–7 x (45/90) @ >90% Max HR | ||||||||||||
| Williams et al. (2000), [88] England, RCT | 8 weeks, | 8 weeks, | Normal everyday activities | |||||||||
| 45, | Running, | Cycling | ||||||||||
| 10.0 ± 0.2 | 3 x week, | 3 x week, | ||||||||||
| 0.0 / 100.0 | 330 minutes | 420 minutes | ||||||||||
| 3–6 x (10/30) and 3–6 x (30/90) @ 100% MAV and 50% MAV on rest | 20 minutes @ 80–85% HR Max | |||||||||||
Study characteristics including participant characteristics (sample size, age, sex ratio), protocol characteristics for HIIT and the comparative exercise group (duration–in weeks, modality–style of exercise, frequency–number of times per week, total time, and a general description with intensity), and protocol characteristics for the control group; HIIT = high intensity interval training; Max HR = maximum heart rate; MAV = maximal aerobic velocity; NA = not applicable; NR = not recorded; PE = physical education; RCT = randomised control trial; 1RM = 1 repetition maximum.
ˆ reported as mean and standard deviation (x ± x), or where not provided as range (x–x).
a reported as frequency (%).
b time in intervention excluding warm up and cool down.
c This study compares 5 different HIIT protocols with different volumes of HIIT.
d Data extracted only for healthy children.
Process outcomes
Over half of the studies (24 of 42) were completed during physical education (PE) class but only 11 documented that PE teachers played a role in their delivery, while 20 studies did not provide information on the intervention facilitator. Attendance data was reported in only 35.7% of studies (Table 1). It varied across studies from 63% [65] to above 90% [32, 45, 59, 62, 63, 76, 79–82, 85]. Different intensity targets were set for participants in interventions. Four studies did not specify a target and instead used terminology such as “suitably high” and “sprint maximally” [32, 44, 47, 75]. For all other studies, a target threshold for heart rate, speed, power, or RPE was provided to participants. The lowest intensity target among any study was 75% of maximum heart rate during high intensity games with both work and rest included [82]. Assessment of whether these targets were achieved (fidelity) only occurred in 47.6% studies, with heart rate as the most commonly used tool. Session intensity was most often reported as an average heart rate across all participants and sessions. Five studies [48, 69, 70, 87, 88] used the average heart rate during only work intervals whereas other studies used an average that included both work and rest intervals or did not specify what was included. One study [64] reported the average time spent in different heart rate zones by participants and one study reported the number of students that achieved the desired heart rate during sessions in addition to the average and maximum heart rate [61]. Among the studies that reported session intensity, two studies did not use heart rate, with one using an RPE scale [55] and the other using a percentage of a one maximum repetition [59].
Risk of bias and certainty of evidence
Thirty-six of the 42 studies had a “high” risk of bias (Table 3), mostly related to deviation from the intended intervention and missing data. High bias related to randomisation was noted least often. Four studies were classified as having “some concerns”, and only two as having a “low” risk of bias. Using the GRADE approach, the certainty of the outcomes ranged between “very low” and “moderate” (S2 File). The most common reasons for downgrading the evidence were risk of bias and inconsistency within the findings. The certainty of evidence for body fat percentage, body mass index (BMI), low-density lipoprotein (LDL), and CRF was upgraded by one point due to large effect sizes within the findings.
Table 3. Risk of bias assessment based on ROB-2 and ROBINS.
| Randomised Control Trials | ||||||
| Randomisation and Selection Bias | Bias due to Missing Data | Measurement Bias | Bias due to Deviations from the Intended Intervention | Bias due to Analysis and Selection of Reported Results | Overall Risk of Bias | |
| Abassi et al. (2020) [36] | Some Concerns | High | Some Concerns | High | High | High |
| Adeniran et al. (1988) [37] | Low | Low | Some Concerns | High | Some Concerns | High |
| Arariza (2018)/Ruiz Arirza et al. (2019) [39, 83] | Low | Low | Low | Low | Some Concerns | Some Concerns |
| Alonso-Fernandez et al. (2019) [38] | Low | High | Some Concerns | High | Some Concerns | High |
| Baquet et al. (2004) [43] | Low | Some Concerns | Some Concerns | High | Some Concerns | High |
| Baquet et al. (2010) [42] | Low | Some Concerns | High | High | High | High |
| Boddy et al. (2010) [44] | Some Concerns | Some Concerns | Low | Some Concerns | High | High |
| Ben-Zeev et al. (2020) [32] | High | Low | Some Concerns | High | Some Concerns | High |
| Bogataj et al. (2020) [45] | Some Concerns | Low | Low | High | Some Concerns | High |
| Buchan et al. (2011) [46, 47] | High | Low | Some Concerns | Low | High | High |
| Camacho-Cardenosa et al. (2016) [48] | Low | Low | Some Concerns | Some Concerns | Some Concerns | Some Concerns |
| Cheunsiri et al. (2018) [49] | Some Concerns | High | Some Concerns | High | Some Concerns | High |
| Costigan et al. (2015/2016/2018) [50–52] | Low | Low | Low | Low | Low | Low |
| Cvetkovic et al. (2018) [53, 54] | Some Concerns | High | Some Concerns | Some Concerns | Some Concerns | High |
| Elbe et al. (2016)/Larsen et al. (2015) [56, 64] | Low | High | Some Concerns | High | Low | High |
| Gamelin et al. (2009) [58] | Low | Some Concerns | Some Concerns | High | Some Concerns | High |
| Granacher et al. (2011) [59] | Low | Low | Some Concerns | Low | Some Concerns | Some Concerns |
| Haghshenas et al. (2019) [60] | Low | Low | Some Concerns | High | Some Concerns | High |
| Lambrick et al. (2016)/McNarry et al. (2015) [63, 73] | Some Concerns | Some Concerns | Some Concerns | Low | Some Concerns | High |
| Ketelhut et al. (2020) [62] | Low | High | Some Concerns | High | Some Concerns | High |
| Lubans et al. (2020)/Leahy et al. (2018)/Leahy et al. (2020)/Kennedy et al. (2020) [62, 65, 66, 68] | Some Concerns | Low | Some Concerns | High | Low | High |
| Logan et al. (2016) [67] | High | Low | Some Concerns | Low | Some Concerns | High |
| Martin et al. (2015) [69] | Low | High | Some Concerns | High | Some Concerns | High |
| Martin-Smith et al. (2018) [70] | Low | Low | Some Concerns | High | Low | High |
| McManus et al. (1997) [71] | High | High | Some Concerns | High | Some Concerns | High |
| McManus et al. (2005) [72] | Some Concerns | High | Some Concerns | High | Some Concerns | High |
| McNarry et al. (2020) [74] | Low | High | Some Concerns | Some Concerns | Some Concerns | High |
| Moureau et al. (2017) [75] | Some Concerns | Low | Low | Low | Low | Low |
| Mucci et al. (2013)/Nourry et al. (2005) [76, 78] | Some Concerns | Some Concerns | Low | High | Some Concerns | High |
| Racil et al. (2013) [79] | Some Concerns | Low | Some Concerns | High | Some Concerns | High |
| Racil et al. (2016a) [80] | High | Low | Some Concerns | Some Concerns | Some Concerns | High |
| Racil et al. (2016b) [81] | Some Concerns | Low | Some Concerns | High | Some Concerns | High |
| Reyes Amigo et al. (2021) [82] | High | Low | Some Concerns | High | Some Concerns | High |
| Segovia et al. (2020) [84] | Low | High | Some Concerns | High | Some Concerns | High |
| Williams et al. (2000) [88] | Some Concerns | Low | Some Concerns | Low | High | High |
| Quasi-Experimental Studies | ||||||
| Bias due to Confounding | Bias due to Missing Data | Measurement Bias | Bias due to Deviations from the Intended Intervention | Bias due to Analysis and Selection of Reported Results | Overall Risk of Bias | |
| Baquet et al. (2001) [41] | Some Concerns | High | Some Concerns | High | Some Concerns | High |
| Baquet et al. (2002) [40] | Low | High | Some Concerns | Some Concerns | Some Concerns | High |
| Delgado Floody et al. (2018) [55] | High | High | Some Concerns | High | Some Concerns | High |
| Espinoza-Sliva et al. (2019) [57] | Low | High | Some Concerns | High | High | High |
| Muntaner-Mas et al. (2017) [77] | High | High | Some Concerns | High | High | High |
| Van Biljon et al. (2018) [85, 86] | High | Low | Some Concerns | Low | Some Concerns | High |
| Weston et al. (2016) [87] | Low | Low | Some Concerns | Some Concerns | Some Concerns | Some Concerns |
Risk of bias assessment for each study included in the review.; Bias due to missing data uses a 15% cut-off; Bias due to deviations from the intended intervention was modified to reflect an exercise intervention by assessing the fidelity of attaining high intensity, the attendance, the adverse events, and the qualifications of the person leading the intervention. ROB-2 = risk of bias; ROBINS = risk of bias in non-randomised studies; RCT = randomised control trial
Physical health outcomes
Table 4 reports results for all outcomes examined in two or more studies comparing HIIT to a control group. Forest plots for all meta-analyses are presented in S3 File. HIIT was favoured in meta-analyses for waist circumference, body fat percentage, BMI, CRF, resting heart rate, homeostatic model assessment–insulin resistance (HOMA-IR), and LDL. Publication bias was significant for body fat percentage (p = 0.049), BMI (p = 0.003) and CRF (p = 0.001). According to the meta-regression results, having an entire population classified as overweight or obese significantly moderated the results for waist circumference (n = 7, β = -0.56, p = 0.009), body fat percentage (n = 9, β = -2.11, p < 0.0001), and BMI (n = 9, β = -1.38, p < 0.0001), with a greater decrease noted in this population. Additionally, there was a greater increase in CRF in these studies (n = 5, β = 1.01, p = 0.007). Having an entire population classified as overweight or obese also explained some of the heterogeneity present in the model for waist circumference (Residual heterogeneity: I2 = 36%, p = 0.06). Studies with a higher volume of HIIT were associated with a greater decrease in body fat percentage (β = -0.002, p < 0.0001) and BMI (β = -0.001, p = 0.0014). Studies with a longer protocol duration had a greater decrease in body fat percentage (β = -0.12, p = 0.0004). Including a higher percentage of girls was also associated with a greater decrease in body fat percentage (β = -0.01, p = 0.0377) and BMI (β = -0.01, p = 0.0109). Studies with a high risk of bias due to deviations from the intended intervention had a significantly greater increase in CRF compared to studies with low bias (β = 1.03, p = 0.013). When only the 5 studies with low bias were included in the analysis, heterogeneity was not significant (I2 = 14%, p = 0.32) and the random effects model was still significant (SMD = 0.41, 95% CI = 0.12 to 0.70) [47, 52, 63, 86, 88]. The method used to assess CRF (20 m shuttle run, cycle ergometer, or treadmill ergometer) and body fat percentage (Dual X-ray absorptiometry, bioelectrical impedance, or skinfold estimation) did not significantly moderate the results.
Table 4. Summary of outcomes between HIIT and control groups for all outcomes reported in ≥ 2 studies.
| Outcome | Participants (Studies) | Analysis | Certainty of the Evidence (GRADE) | Key Finding | Heterogeneity | |
|---|---|---|---|---|---|---|
| Body Composition | Waist circumference | 1175 (14) | MA + MR | ⨁⨁⨁⊖ | Favoured HIIT, MD = -2.5 cm (-3.1 to -1.9) [36, 44, 52, 55, 57, 63, 70, 77, 79–81, 84, 85, 87] | I2 = 47%, p = 0.01 |
| Body fat percentage | 1893 (19) | MA + MR | ⨁⨁⊖⊖ | Favoured HIIT, MD = -1.7% (-2.3 to -1.1) [36, 38, 40, 41, 43–45, 47, 49, 54, 55, 57, 63, 77, 79–81, 84, 87] | I2 = 93%, p < 0.01 | |
| Body Mass Index | 2450 (22) | MA + MR | ⨁⨁⊖⊖ | Favoured HIIT, SMD = -0.9 (-1.3 to -0.6) [36, 38, 41, 42, 44, 45, 47, 49, 52, 54, 55, 57, 63, 68, 69, 74, 77, 79–81, 85, 87] | I2 = 92%, p < 0.01 | |
| Muscle mass | 264 (5) | MA | ⨁⨁⊖⊖ | Summary statistic NS [45, 49, 54, 63, 87] | I2 = 43%, p = 0.12 | |
| Lean mass | 297 (4) | MA | ⨁⊖⊖⊖ | Summary statistic NS [44, 54, 64, 80] | I2 = 90%, p < 0.01 | |
| Hip circumference | 126 (3) | Narrative | NS in 3 studies [44, 63, 70] | |||
| Bone density and content | 300 (2) | Narrative | NS in 2 studies [44, 64] | |||
| Cardiovascular Health | Systolic blood pressure | 872 (11) | MA | ⨁⨁⨁⊖ | Summary statistic NS [44, 47, 49, 54, 55, 57, 62, 70, 80, 85, 87] | I2 = 29%, p = 0.14 |
| Diastolic blood pressure | 872 (11) | MA | ⨁⨁⊖⊖ | Summary statistic NS [44, 47, 49, 54, 55, 57, 62, 70, 80, 85, 87] | I2 = 68%, p < 0.01 | |
| Resting heart rate | 381 (6) | MA | ⨁⨁⊖⊖ | Favoured HIIT, MD = -5 bpm (-7 to -2) [49, 54, 55, 58, 80, 85] | I2 = 52%, p = 0.03 | |
| Heart rate variability | 147 (2) | Narrative | Favoured HIIT in 1 study [86], NS in 1 study [58] | |||
| Aortic pulse wave velocity | 166 (2) | Narrative | Favoured HIIT in 1 study [62], NS in 1 study [85] | |||
| Blood Profile | Glucose | 447 (10) | MA | ⨁⨁⨁⊖ | Summary statistic NS [36, 47, 53, 69, 70, 79–81, 86, 87] | I2 = 0%, p = 0.81 |
| Insulin | 321 (8) | MA | ⨁⊖⊖⊖ | Summary statistic NS [36, 47, 69, 70, 79–81, 85] | I2 = 93%, p < 0.01 | |
| HOMA-IR | 211 (5) | MA | ⨁⨁⨁⊖ | Favoured HIIT, MD = -0.7 (-1.1 to -0.4) [69, 70, 79–81] | I2 = 95%, p < 0.01 | |
| Triglycerides | 279 (6) | MA | ⨁⊖⊖⊖ | Summary statistic NS [47, 49, 54, 70, 79, 87] | I2 = 84%, p < 0.01 | |
| Total cholesterol | 279 (6) | MA | ⨁⊖⊖⊖ | Summary statistic NS [47, 49, 54, 70, 79, 87] | I2 = 84%, p < 0.01 | |
| High-density lipoprotein | 254 (5) | MA | ⨁⨁⊖⊖ | Summary statistic NS [47, 49, 54, 70, 79, 87] | I2 = 36%, p = 0.18 | |
| Low-density lipoprotein | 153 (4) | MA | ⨁⨁⨁⊖ | Favoured HIIT, SMD = -0.9 (-1.2 to -0.5) [47, 49, 70, 79] | I2 = 0%, p = 0.53 | |
| Leptin | 152 (3) | Narrative | Favoured HIIT in 2 studies [80, 81], NS in 1 study [49] | |||
| Adiponectin | 206 (4) | Narrative | Favoured HIIT in 3 studies [47, 79, 81], NS in 1 study [49] | |||
| C-reactive Protein | 265 (3) | Narrative | Favoured HIIT in 1 study [85], NS in 2 studies [47, 87] | |||
| Aerobic & Muscular Fitness | Cardiorespiratory fitness (all methods)** | 2099 (25) | MA + MR | ⨁⊖⊖⊖ | Favoured HIIT, SMD = 1.0 (0.7 to 1.3) [36, 38, 40–42, 44, 45, 47, 49, 52, 58, 63, 68–72, 74, 78–81, 86–88] | I2 = 83%, p < 0.01 |
| Cardiorespiratory fitness (relative VO2) † | 403 (11) | MA | ⨁⨁⨁⊖ | Favoured HIIT, MD = 3.1 ml/min/kg (2.4 to 3.8) [40, 42, 44, 49, 58, 63, 72, 76, 79, 81, 88] | I2 = 50%, p = 0.03 | |
| Cardiorespiratory fitness (shuttles) ‡ | 299 (5) | MA | ⨁⊖⊖⊖ | Favourite HIIT, MD = 10.4 shuttles (1.9 to 18.9) [46, 52, 65, 69, 87] | I2 = 88%, p < 0.01 | |
| Standing long jump | 1428 (5) | MA | ⨁⨁⊖⊖ | Summary statistic NS [41, 43, 52, 68, 77] | I2 = 84%, p < 0.01 | |
| Countermovement jump | 212 (5) | MA | ⨁⨁⊖⊖ | Summary statistic NS [45, 46, 53, 59, 81] | I2 = 53%, p = 0.07 | |
| Push ups | 735 (2) | Narrative | Favoured HIIT in 1 study [68], NS in 1 study [52] | |||
| Handgrip Strength | 146 (2) | Narrative | NS in 2 studies [45, 77] | |||
| Sit ups | 624 (2) | Narrative | NS in 2 studies [41, 43] | |||
| Sprint time | 331 (3) | Narrative | Favoured HIIT in 2 studies [46, 64], NS in 1 study [53] | |||
| Flexibility | 693 (3) | Narrative | NS in 3 studies [41, 43, 53] | |||
| Balance | 334 (2) | Narrative | NS in 2 studies [59, 64] | |||
| Cognition and Wellbeing | Inhibition | 1199 (4) | Narrative | Favoured HIIT in 3 studies [32, 39, 75], NS in 1 study [68] | ||
| Memory | 1199 (4) | Narrative | Favoured HIIT in 2 studies [32, 75], NS in 2 studies [39, 68] | |||
| Wellbeing | 919 (3) | Narrative | Favoured HIIT in 1 study [83], NS in 2 studies [51, 68] | |||
| Motivation levels | 126 (2) | Narrative | NS in 2 studies [51, 68] | |||
| Physical activity and Nutrition | Vigorous Physical Activity | 791 (3) | Narrative | Favoured HIIT in 2 studies [50, 70], NS in 1 study [68] | ||
| Moderate Physical Activity | 791 (3) | Narrative | Favoured HIIT in 1 study [70] NS in 2 studies [50, 68] | |||
| Moderate-to-Vigorous Physical Activity | 843 (3) | Narrative | Favoured HIIT in 1 study [87] NS in 2 studies [44, 68] | |||
| Step Count | 790 (3) | Narrative | Favoured HIIT in 1 study [68], NS in 2 studies [44, 49] | |||
| Caloric intake | 71 (3) | Narrative | NS in 2 studies [69, 81] |
Participants (studies) = number of participants (number of studies) included. HOMA-IR–homeostatic model assessment–insulin resistance; MA–meta-analysis; MR–meta-regressions; HIIT–high intensity interval training; NS–not significant; MD–mean difference; SMD–standardised mean difference.
** cardiorespiratory fitness was examined using either 20 m shuttle runs, cycle ergometer, or treadmill ergometer and it was reported either as the number of shuttles completed, or as VO2, which was either measured by a metabolic cart or estimated using an equation. The type of measurement did not significantly moderate the results.
† Body mass relative maximum oxygen consumption directly assessed by metabolic cart.
‡ Number of shuttles completed in the 20 m shuttle run test using a mean difference.
Table 5 reports findings for all outcomes examined in two or more studies comparing HIIT and comparative exercise groups, with no significant differences reported between the two groups for most health outcomes. Across all health outcomes, only three studies had results that favoured HIIT [79, 80, 85], while one study had results that favoured continuous exercise [47].
Table 5. Summary of outcomes between HIIT and comparative exercise groups for all outcomes reported in ≥ 2 studies.
| Outcome | Participants (studies) | General Finding | |
|---|---|---|---|
| Body Composition | Waist circumference | 137 (4) | Favoured HIIT in 1 study [85], NS in 3 studies [36, 79, 80] |
| Body fat percentage | 168 (6) | Favoured HIIT in 1 study [79], Favoured comparator in 1 study [47], NS in 4 studies [36, 48, 54, 80] | |
| BMI | 235 (7) | NS in 7 studies [36, 42, 47, 54, 79, 80, 85] | |
| Cardiovascular Health | Systolic blood pressure | 145 (4) | Favoured HIIT in 1 study [86], NS in 3 studies [47, 54, 80] |
| Diastolic blood pressure | 145 (4) | NS in 4 studies [47, 54, 80, 86] | |
| Resting heart rate | 112 (2) | Favoured HIIT in 1 study [86], NS in 1 study [54] | |
| Blood Profile | Glucose | 191 (6) | NS in 6 studies [36, 47, 53, 79, 80, 85] |
| Insulin | 170 (5) | Favoured HIIT in 2 studies [79, 80], Favoured comparator in 1 study [47], NS in 2 study [36, 85] | |
| HOMA-IR | 79 (3) | NS in 3 studies [36, 79, 80] | |
| Triglycerides | 76 (3) | Favoured HIIT in 1 study [79], NS in 2 studies [47, 54] | |
| Total cholesterol | 76 (3) | NS in 3 studies [47, 54, 79] | |
| High-density lipoprotein | 55 (2) | NS in 2 studies [47, 79] | |
| Low-density lipoprotein | 55 (2) | NS in 2 studies [47, 79] | |
| Aerobic & Muscular Fitness | Cardiorespiratory fitness | 225 (7) | Favoured HIIT in 1 study [85], NS in 6 studies [36, 42, 71, 72, 79, 80, 88] |
| Countermovement jump | 220 (2) | NS in 2 studies [46, 53] |
Participants (studies) = number of participants (number of studies) included. HOMA-IR = homeostatic model assessment–insulin resistance; HIIT = high intensity interval training; NS = not significant.
Psychosocial and cognitive outcomes
As shown in Table 4, there were heterogeneous results for inhibition and memory when comparing HIIT and control groups in the four studies where these outcomes were examined. A variety of tests were used to investigate these two outcomes, with no two studies using the same battery of tests so no meta-analyses were performed. Two studies demonstrated no improvement to wellbeing after HIIT [51, 68], while one found an improvement in inactive children only [83]. No between-group difference was present for motivation levels towards completing the HIIT workouts [51, 68].
HIIT intervention enjoyment
Enjoyment of HIIT was examined in four studies [49, 52, 56, 61]. Two [49, 56] used the validated Physical Activity Enjoyment Scale (PACES) questionnaire and determined that team sports elicited significantly greater enjoyment than individual sports [56], that 20-second bouts were enjoyed more than 120-second bouts [49], and that enjoyment was significantly associated with improvement in running performance [56]. Two studies [52, 61] used Likert questions to examine enjoyment alongside motivation, fatigue, and satisfaction, and found that students and teachers were satisfied with the HIIT workouts, and the majority intended to continue using the workouts.
Physical activity levels and energy intake
Five studies used accelerometers to quantify physical activity outcomes for HIIT and control groups [44, 50, 68, 70, 87], one used a pedometer [49], and one used the Physical Activity Questionnaire for Children [49]. Physical activity outcomes were reported using different outcome variables (Table 4), with no more than three studies reporting the same variable, therefore meta-analyses were not performed. Heterogeneous findings were present for physical activity variables and no significant differences existed between the HIIT and control groups for caloric intake in the two studies examining the outcome (Table 4).
Comparing HIIT protocols
Four studies compared different HIIT protocols. Two compared aerobic training to aerobic training plus resistance or plyometric training [52, 81]. A third compared a shorter bout length of higher intensity to longer bouts of lower intensity [49], and the last looked at different doses of HIIT by changing the number of sets [67]. No clear effect of dose or bout length was found in these studies [49, 67] and heterogenous findings were reported when resistance training was added to aerobic training [52, 81].
Discussion
This systematic review advances the findings of previous reviews [9–11] by investigating a broader range of outcomes associated with school-based HIIT interventions through comprehensive statistical analysis. The results of this review demonstrate that school-based HIIT is an effective strategy for improving various health outcomes compared with control groups. However, there are heterogenous findings when HIIT is compared to other exercise modalities. Overall, most studies had a high risk of bias, therefore the results need to be interpreted cautiously. Although findings support HIIT can be a useful tool within schools to promote a range of health benefits, they also highlight that further research is needed to examine the meaningful integration of these interventions within schools.
Physical health outcomes: HIIT compared with control
Youths with obesity have an increased risk of developing cardiometabolic conditions [89–91], making it an important outcome to monitor. Improvements to body composition were documented across the included studies in this review with moderate (waist circumference, body fat percentage) or low (BMI) certainty according to GRADE when comparing HIIT with control groups. Our body fat percentage summary effect (1.7%) is similar to another meta-analysis on HIIT, where a 1.6% (95% CI: 0.5% to 2.9%) change was noted in favour of HIIT compared to a combination of non-training controls and moderate intensity groups [9]. While our summary effect for BMI differs to a systematic review on all school-based physical activity interventions that reported no significant change [20], it is equivalent to a previous meta-analysis (n = 8) that compared HIIT to both control groups and moderate intensity comparative groups across various settings [9]. Our findings also have the potential to be clinically meaningful. For example, while we do not have individual data points in this synthesis, a summary effect demonstrating a decrease in waist circumference of 2.5 cm (1.9 to 3.1 cm) is equitable to a decrease from the 90th to 85th percentile in 16-year-old boys or a decrease from the 90th to 80th percentile in 7-year-old girls [91], but this could be influenced by baseline values. In our review, studies that only included students classified as overweight or obese had significantly greater health benefits as a result of HIIT. As increased adiposity is associated with future disease related morbidity and mortality [92], decreasing adiposity, especially in populations classified as obese and overweight, is critical to prevent disease [93]. No significant differences were seen for lean mass, muscle mass, or hip circumference within our systematic review. However, this could be due to the smaller sample sizes for these outcomes.
We can say with moderate certainty that CRF is significantly improved as a result of HIIT interventions compared with a control group. The large effect size (d = 0.9) established in this study mirrors that of two previous meta-analyses on HIIT (d = 1.05 in adolescents and d = 1.11 in adolescents classified as obese or overweight) [9, 13]. Relevant literature shows a positive association between vigorous activity and CRF, corroborating this finding [94]. According to our findings, there was an increase of 3.1 ml/kg/min (2.4 to 3.8 ml/kg/min) in the HIIT group after the intervention compared with the control group in the 11 studies that directly determined peak O2, maximum oxygen consumption. This difference has the potential to be clinically meaningful as a lower CRF is associated with higher cardiometabolic risk in children, independent from physical activity and adiposity [95]. Further, children and adolescents in the lowest quartile for fitness have a greater risk for developing cardiovascular disease compared with those in the highest quartile for fitness [96]. Muscular fitness was examined in fewer studies than CRF, with no difference between the HIIT and control group noted for jumping, handgrip strength or sit-ups through meta-analyses and narrative synthesis. These will be important outcomes to study in more detail as HIIT protocols diversify and further involve different muscle groups. HIIT could have effects on muscular fitness with current research demonstrating a link between vigorous activity and a variety of muscular fitness test outcomes [97, 98].
The LDL and HOMA-IR blood biomarkers were significantly improved following HIIT compared with control groups in this review. However, the studies within these meta-analyses comprised of mainly populations classified as overweight or obese (50% and 60% of studies, respectively), which could be driving this change. The lack of change to other biomarkers for cardiometabolic health, including blood pressure, fasting glucose, triglycerides, and total cholesterol, could be reflective of the fact that baseline measures were within normal thresholds. We might expect to see changes for these variables in populations where the initial levels are elevated, such as in students who are classified as overweight or obese. This is consistent with findings from a recent review that demonstrated that while physical activity interventions in youths classified as obese are capable of producing favourable changes in biomarkers, the same dose is not effective for non-obese youths [99]. However, it is still important to encourage physical activity in all students regardless of their body composition as there is a strong positive association between total physical activity and blood biomarkers in youths [99] and puberty is a crucial period for the development of hypertension later in life [100].
HIIT protocols and comparative exercise
More research is needed to determine if differences exist between HIIT and comparative exercise protocols in the school setting. Our narratively synthesised results did not detect any differences between HIIT and moderate continuous exercise or other comparative exercise protocols, such as moderate intensity intervals or football. However, HIIT provides educators with another option for promoting physical activity and has several unique characteristics that may make it effective in this setting. It can be short and simple to conduct, enabling it to be performed in a classroom setting [65, 101], while partly alleviating concerns that it will compete for time with curricular demands, which is a common reason compromising the effectiveness of school-based interventions [19].
Process outcomes
Overall, process outcomes were documented poorly throughout these studies. The lack of fidelity and attendance data makes it difficult to assess if students received the intended HIIT intervention, which is critical as the intensity of exercise is likely to be important in driving physiological changes. Even for studies that stated that the desired intensity was achieved, this was most often based on an average heart rate across all participants and sessions, which does not allow provide readers with information on how many students successfully completed the intervention. Further, mean peak heart rate was occasionally reported as an outcome measure, which does not capture the variability within sessions. It will be important for future studies to appropriately document the attendance and fidelity of these interventions for proper evaluation [102]. This could help inform readers of HIIT protocols that are more likely to achieve high intensity in this setting. The intervention timing and facilitators varied between studies, and this could have implications on the reach, maintenance, and scalability of studies. However, the variation in the HIIT protocols across studies suggests that there are opportunities to tailor protocols to specific classes or students to appropriately engage and challenge them, and in turn optimise associated outcomes. There was no evidence of integration within the school curriculum in these studies, even though integration can mitigate the overloading teachers and provide staff with appropriate resources, which are shown to improve implementation [19] and should be a focus of future studies.
Future directions
High-quality studies are needed in this area to be able to reach more robust conclusions as significant limitations were identified in the studies included in this review. Specifically, the lack of power calculations and documentation whether the intervention took places as was intended, along with the high levels of missing data that were unaccounted for in the analyses lead to studies with high risk of bias. Future studies should focus on 1) providing justification for their sample size; 2) reporting adherence, fidelity, and whether blinding occurred to determine deviations from the intended intervention; 3) and performing statistical analyses that account for any missing data.
The body of work focusing on school-based HIIT would benefit from additional studies examining cognitive, physical activity and nutrition outcomes. Our findings for cognitive outcomes are similar to those of a systematic review focusing on the impact of HIIT in adolescents across all settings that determined that HIIT may improve cognitive function but highlighted the need for more relevant studies [103]. These outcomes are important to assess, especially within the school setting, as they are related to academic success and improvements in this domain are likely to encourage schools to engage with HIIT [104]. Our narrative synthesis included heterogenous findings for the few studies that examined physical activity levels. More studies investigating physical activity levels and nutritional intake will be useful to help understand the impact of HIIT on these outcomes and whether incorporating HIIT leads to any compensatory behaviours in these domains, as recommended by a recent expert statement [105]. This expert statement also calls for further research into the benefits that are specific to students classified as overweight or obese [105]. Our meta-regressions demonstrated that studies including only those classified as overweight or obese moderated the results for waist circumference, body fat, BMI, and CRF. Moving forward, this will be important to also assess for other variables. As the body of evidence grows, it will be important to investigate potential sex and pubertal differences. Future studies should ensure that they report participants’ pubertal stages in addition to their sex. Further, it will be important for future studies to report results stratified by sex and maturity status to enable the effects of these variables to be understood. Additionally, beyond sex and maturity, studies should aim to investigate these health outcomes are present across schools in different contexts with varying physical activity policies and practices as these vary greatly between countries, school systems, and individual schools.
While this review supports the effectiveness of HIIT interventions in schools, factors related to their feasibility and maintenance must also be considered to improve meaningful short-term and long-term outcomes. It will be important to further investigate enjoyment and affect among HIIT protocols in schools to understand the likelihood for future engagement in these programs [106]. Current research on HIIT has displayed favourable results on enjoyment during and after exercise compared to moderate-intensity continuous training [107]. One strategy to facilitate high levels of student enjoyment may be involving students in the design of HIIT protocols. Affording students ownership in the design of HIIT protocols has the additional potential to also enhance students’ accountability, participation, confidence and perceived competence in completing the workouts when the interventions reach the implementation phase [108]. This may be particularly useful for girls given they are less likely to enjoy school physical education and have on average a lower self-perceived physical ability [109]. Beyond students, studies should consider engaging other key stakeholders (e.g., teachers, parents, principals, local policy makers) in designing the intervention to increase the likelihood that interventions are maintained. Co-designing relevant interventions with teachers and integration of the interventions within the curriculum and with relevant educative outcomes could mitigate common reasons for implementation failure such as time constraints, competing curricular demands and overburdened teachers [19, 110].
Strengths and limitations
This is the first systematic review to comprehensively synthesise the effects of school-based HIIT interventions across a wide range of health and wellbeing outcomes. The review has conducted a rigorous assessment of the risk of bias of included studies and available evidence, which allows the results to be interpreted with the required caution. Further, the review includes several meta-analyses and subsequent meta-regressions, which provide novel insights into the impact of HIIT in this setting along with associated factors. A limitation of this review includes the potential publication bias from only using articles published in English and omitting literature that was not peer-reviewed. Additionally, the papers included within this systematic review were mainly studies with small sample sizes and were classified as having a high risk of bias. Therefore, the results may need to be interpreted with caution.
Conclusion
HIIT is an effective strategy for improving various health outcomes within the school setting, with our meta-analyses indicating meaningful improvements in markers of body size and composition, cardiovascular disease blood biomarkers, and CRF when compared to a non-exercise control group. However, our risk of bias results highlight that more high-quality studies are needed in this area. Currently, there is insufficient evidence to suggest that HIIT is superior to moderate continuous exercise or other types of comparative exercise. It is recommended that future research addresses the paucity of information on cognitive, physical activity, and nutrition outcomes associated with school-based HIIT interventions. It is also recommended that future research examines the effectiveness of these interventions over longer periods and how the interventions can be best developed and integrated within school practice to ensure engagement and maintenance.
Supporting information
(DOCX)
(DOCX)
(PDF)
(XLSX)
(DOCX)
Acknowledgments
The authors would like to thank Kate Sansum and Jenna Markey, University of Exeter students, and Tracy Bruce, University of Queensland academic librarian, for their assistance and contributions to this review through the search and data extraction phases.
Data Availability
All relevant data are within a Supporting Information file (S4).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Barker AR, Gracia-Marco L, Ruiz JR, Castillo MJ, Aparicio-Ugarriza R, González-Gross M, et al. Physical activity, sedentary time, TV viewing, physical fitness and cardiovascular disease risk in adolescents: The HELENA study. International Journal of Cardiology. 2018;254:303–9. doi: 10.1016/j.ijcard.2017.11.080 [DOI] [PubMed] [Google Scholar]
- 2.Carson V, Rinaldi RL, Torrance B, Maximova K, Ball GDC, Majumdar SR, et al. Vigorous physical activity and longitudinal associations with cardiometabolic risk factors in youth. International Journal of Obesity. 2014;38(1):16–21. doi: 10.1038/ijo.2013.135 [DOI] [PubMed] [Google Scholar]
- 3.Gralla MH, McDonald SM, Breneman C, Beets MW, Moore JB. Associations of Objectively Measured Vigorous Physical Activity With Body Composition, Cardiorespiratory Fitness, and Cardiometabolic Health in Youth: A Review. American Journal of Lifestyle Medicine. 2019;13(1):61–97. doi: 10.1177/1559827615624417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buchheit M, Laursen PB. High-Intensity Interval Training, Solutions to the Programming Puzzle. Sports Medicine. 2013;43(10):927–54. doi: 10.1007/s40279-013-0066-5 [DOI] [PubMed] [Google Scholar]
- 5.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health and Human Services, 2018.
- 6.Department of Health & Social Care. UK Chief Medical Officers’ Physical Activity Guidelines 2019. Available from: https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report.
- 7.Bond B, Weston K, Williams C, Barker A. Perspectives on high-intensity interval exercise for health promotion in children and adolescents. Open Access Journal of Sports Medicine. 2017;Volume 8:243–65. doi: 10.2147/OAJSM.S127395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper SB, Dring KJ, Nevill ME. High-Intensity Intermittent Exercise: Effect on Young People’s Cardiometabolic Health and Cognition. Current Sports Medicine Reports (Lippincott Williams & Wilkins). 2016;15(4):245–51. 1; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 9.Costigan SA, Eather N, Plotnikoff RC, Taaffe DR, Lubans DR. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1253–61. doi: 10.1136/bjsports-2014-094490 1; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 10.Eddolls WTB, McNarry MA, Stratton G, Winn CON, Mackintosh KA. High-Intensity Interval Training Interventions in Children and Adolescents: A Systematic Review. Sports Medicine. 2017;47(11):2363–74. doi: 10.1007/s40279-017-0753-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logan GRM, Harris N, Duncan S, Schofield G. A Review of Adolescent High-Intensity Interval Training. Sports Medicine. 2014;44(8):1071–85. doi: 10.1007/s40279-014-0187-5 [DOI] [PubMed] [Google Scholar]
- 12.Martin-Smith R, Cox A, Buchan DS, Baker JS, Grace F, Sculthorpe N. High Intensity Interval Training (HIIT) Improves Cardiorespiratory Fitness (CRF) in Healthy, Overweight and Obese Adolescents: A Systematic Review and Meta-Analysis of Controlled Studies. International Journal of Environmental Research and Public Health. 2020;17(8):2955. doi: 10.3390/ijerph17082955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thivel D, Masurier J, Baquet G, Timmons BW, Pereira B, Berthoin S, et al. High-intensity interval training in overweight and obese children and adolescents: systematic review and meta-analysis. J Sports Med Phys Fitness. 2018;27:27. 10.23736/S0022-4707.18.08075-1 . [DOI] [PubMed] [Google Scholar]
- 14.Hsieh S-S, Chueh T-Y, Huang C-J, Kao S-C, Hillman CH, Chang Y-K, et al. Systematic review of the acute and chronic effects of high-intensity interval training on executive function across the lifespan. Journal of Sports Sciences. 2020:1–13. doi: 10.1080/02640414.2020.1803630 [DOI] [PubMed] [Google Scholar]
- 15.Leahy AA, Mavilidi MF, Smith JJ, Hillman CH, Eather N, Barker D, et al. Review of High-Intensity Interval Training for Cognitive and Mental Health in Youth. Medicine & Science in Sports & Exercise. 2020;52:2224–34. doi: 10.1249/MSS.0000000000002359 [DOI] [PubMed] [Google Scholar]
- 16.Cao M, Quan M, Zhuang J. Effect of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Cardiorespiratory Fitness in Children and Adolescents: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2019;16(9):1533. doi: 10.3390/ijerph16091533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Booth M, Okely A. Promoting physical activity among children and adolescents: the strengths and limitations of school-based approaches. Health Promotion Journal of Australia. 2005;16(1):52–4. doi: 10.1071/he05052 [DOI] [PubMed] [Google Scholar]
- 18.Lonsdale C, Sanders T, Parker P, Noetel M, Hartwig T, Vasconcellos D, et al. Effect of a Scalable School-Based Intervention on Cardiorespiratory Fitness in Children: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2021;175(7):680–8. Epub 2021/05/04. doi: 10.1001/jamapediatrics.2021.0417 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naylor P-J, Nettlefold L, Race D, Hoy C, Ashe MC, Wharf Higgins J, et al. Implementation of school based physical activity interventions: A systematic review. Preventive Medicine. 2015;72:95–115. doi: 10.1016/j.ypmed.2014.12.034 [DOI] [PubMed] [Google Scholar]
- 20.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. Canadian Medical Association Journal. 2009;180(7):719–26. doi: 10.1503/cmaj.080966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Behavioral Interventions to Prevent Childhood Obesity: A Systematic Review and Metaanalyses of Randomized Trials. The Journal of Clinical Endocrinology & Metabolism. 2008;93(12):4606–15. doi: 10.1210/jc.2006-2411 [DOI] [PubMed] [Google Scholar]
- 22.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes. BMJ. 2012;345(7876):16. doi: 10.1136/bmj.e5888 [DOI] [PubMed] [Google Scholar]
- 23.Love R, Adams J, Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obesity Reviews. 2019;20(6):859–70. doi: 10.1111/obr.12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker L, Rollo I, Stein K, Jeukendrup A. Acute Effects of Carbohydrate Supplementation on Intermittent Sports Performance. Nutrients. 2015;7(7):5733–63. doi: 10.3390/nu7075249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanders T, Cliff DP, Lonsdale C. Measuring Adolescent Boys’ Physical Activity: Bout Length and the Influence of Accelerometer Epoch Length. PLoS One. 2014;9(3):e92040. doi: 10.1371/journal.pone.0092040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik AA, Williams CA, Weston KL, Barker AR. Perceptual Responses to High- and Moderate-Intensity Interval Exercise in Adolescents. Medicine & Science in Sports & Exercise. 2018;50(5):1021–30. doi: 10.1249/MSS.0000000000001508 [DOI] [PubMed] [Google Scholar]
- 27.Delgado-Floody P, Latorre-Román P, Jerez-Mayorga D, Caamaño-Navarrete F, García-Pinillos F. Feasibility of incorporating high-intensity interval training into physical education programs to improve body composition and cardiorespiratory capacity of overweight and obese children: A systematic review. Journal of Exercise Science & Fitness. 2019;17(2):35–40. doi: 10.1016/j.jesf.2018.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murad MH, Asi N, Alsawas M, Alahdab F. New evidence pyramid. Evidence Based Medicine. 2016;21(4):125–7. doi: 10.1136/ebmed-2016-110401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2 ed. Chichester (UK): John Wiley & Sons; 2019. [Google Scholar]
- 30.Smart NA, Waldron M, Ismail H, Giallauria F, Vigorito C, Cornelissen V, et al. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int J Evid Based Healthcare. 2015;13(1):9–18. doi: 10.1097/XEB.0000000000000020 [DOI] [PubMed] [Google Scholar]
- 31.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations.: The GRADE Working Group; 2013. [Google Scholar]
- 32.Ben-Zeev T, Hirsh T, Weiss I, Gornstein M, Okun E. The Effects of High-intensity Functional Training (HIFT) on Spatial Learning, Visual Pattern Separation and Attention Span in Adolescents. Front Behav Neurosci. 2020;14:577390. 10.3389/fnbeh.2020.577390 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis. Journal of Clinical Epidemiology. 2001;54(10):1046–55. doi: 10.1016/s0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- 35.Higgins JPT, Thompson SG. Controlling the risk of spurious findings from meta-regression. Statistics in Medicine. 2004;23(11):1663–82. doi: 10.1002/sim.1752 [DOI] [PubMed] [Google Scholar]
- 36.Abassi W, Ouerghi N, Ghouili H, Haouami S, Bouassida A. Greater effects of high- compared with moderate-intensity interval training on thyroid hormones in overweight/obese adolescent girls. Horm. 2020;41(4):25. 10.1515/hmbci-2020-0031 . [DOI] [PubMed] [Google Scholar]
- 37.Adeniran SA, Toriola AL. Effects of continuous and interval running programmes on aerobic and anaerobic capacities in schoolgirls aged 13 to 17 years. The Journal of Sports Medicine and Physical Fitness. 1988;28(3):260–6. [PubMed] [Google Scholar]
- 38.Alonso-Fernández D, Fernández-Rodríguez R, Taboada-Iglesias Y, Gutiérrez-Sánchez Á. Impact of a HIIT protocol on body composition and VO2max in adolescents. Science & Sports. 2019;34(5):341–7. doi: 10.1016/j.scispo.2019.04.001 [DOI] [Google Scholar]
- 39.Arariza A. 24 sessions of monitored cooperative high-intensity interval training improves attention-concentration and mathematical calculation in secondary school. Journal of Physical Education & Sport. 2018;18(3):1572–82. . [Google Scholar]
- 40.Baquet G, Berthoin S, Dupont G, Blondel N, Fabre C, van Praagh E. Effects of high intensity intermittent training on peak VO2 in prepubertal children. Int J Sports Med. 2002;23(6):439–44. doi: 10.1055/s-2002-33742 PubMed PMID: WOS:000177941300009; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 41.Baquet G, Berthoin S, Gerbeaux M, Van Praagh E. High-intensity aerobic training during a 10 week one-hour physical education cycle: Effects on physical fitness of adolescents aged 11 to 16. Int J Sports Med. 2001;22(4):295–300. doi: 10.1055/s-2001-14343 PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 42.Baquet G, Gamelin FX, Mucci P, Thevenet D, Van Praagh E, Berthoin S. Continuous vs. interval aerobic training in 8-to 11-year-old children. J Strength Cond Res. 2010;24(5):1381–8. doi: 10.1519/JSC.0b013e3181d1575a PubMed PMID: WOS:000277608000032; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 43.Baquet G, Guinhouya C, Dupont G, Nourry C, Berthoin S. Effects of a short-term interval training program on physical fitness in prepubertal children. J Strength Cond Res. 2004;18(4):708–13. PubMed PMID: WOS:000225444300004; PubMed Central PMCID: PMC. doi: 10.1519/13813.1 [DOI] [PubMed] [Google Scholar]
- 44.Boddy L, Stratton G, Hackett A, George K. The effectiveness of a ‘short, sharp, shock’ high intensity exercise intervention in 11- and 12-year-old Liverpool schoolgirls. Arch Exerc Health Dis. 2010;1(1):19–25. [Google Scholar]
- 45.Bogataj S, Trajkovic N, Cadenas-Sanchez C, Sember V. Effects of school-based exercise and nutrition intervention on body composition and physical fitness in overweight adolescent girls. Nutrients. 2021;13(1):1–12. 10.3390/nu13010238 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Buchan DS, Ollis S, Thomas NE, Buchanan N, Cooper SM, Malina RM, et al. Physical activity interventions: effects of duration and intensity. Scandinavian Journal of Medicine & Science in Sports. 2011;21(6):e341–e50. doi: 10.1111/j.1600-0838.2011.01303.x ; PubMed Central PMCID: PMC1. [DOI] [PubMed] [Google Scholar]
- 47.Buchan DS, Ollis S, Young JD, Thomas NE, Cooper SM, Tong TK, et al. The Effects of Time and Intensity of Exercise on Novel and Established Markers of CVD in Adolescent Youth. Am J Hum Biol. 2011;23(4):517–26. doi: 10.1002/ajhb.21166 PubMed PMID: WOS:000291898700009; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 48.Camacho-Cardenosa A, Brazo-Sayavera J, Camacho-Cardenosa M, Marcos-Serrano M, Timon R, Olcina G. Effects of High Intensity Interval Training on Fat Mass Parameters in Adolescents. Revista espanola de salud publica. 2016;90:e1–e9. [PubMed] [Google Scholar]
- 49.Chuensiri N, Suksom D, Tanaka H. Effects of High-Intensity Intermittent Training on Vascular Function in Obese Preadolescent Boys. Childhood Obesity. 2018;14(1):41–9. doi: 10.1089/chi.2017.0024 . Language: English. Entry Date: 20180121. Revision Date: 29099231. Publication Type: Article. [DOI] [PubMed] [Google Scholar]
- 50.Costigan S, Ridgers N, Eather N, Plotnikoff R, Harris N, Lubans D. Exploring the impact of high intensity interval training on adolescents’ objectively measured physical activity: Findings from a randomized controlled trial. Journal of Sports Sciences. 2018;36(10):1087–94. doi: 10.1080/02640414.2017.1356026 ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 51.Costigan SA, Eather N, Plotnikoff RC, Hillman CH, Lubans DR. High-Intensity Interval Training for Cognitive and Mental Health in Adolescents. Medicine & Science in Sports & Exercise. 2016;48(10):1985–93. doi: 10.1249/MSS.0000000000000993 ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 52.Costigan SA, Eather N, Plotnikoff RC, Taaffe DR, Pollock E, Kennedy SG, et al. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: A pilot randomized controlled trial. Preventive Medicine Reports. 2015;2:973–9. doi: 10.1016/j.pmedr.2015.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cvetković N, Stojanović E, Stojiljković N, Nikolić D, Milanović Z. Effects of a 12 week recreational football and high-intensity interval training on physical fitness in overweight children. Facta Universitatis: Series Physical Education & Sport. 2018;16(2):435–50. ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 54.Cvetković N, Stojanović E, Stojiljković N, Nikolić D, Scanlan AT, Milanović Z. Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scandinavian Journal of Medicine & Science in Sports. 2018;28:18–32. doi: 10.1111/sms.13241 ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 55.Delgado-Floody P, Espinoza-Silva M, García-Pinillos F, Latorre-Román P. Effects of 28 weeks of high-intensity interval training during physical education classes on cardiometabolic risk factors in Chilean schoolchildren: a pilot trial. European Journal of Pediatrics. 2018;177(7):1019–27. doi: 10.1007/s00431-018-3149-3 . Language: English. Entry Date: 20180811. Revision Date: 20181120. Publication Type: journal article. Journal Subset: Biomedical; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 56.Elbe A-M, Wikman JM, Zheng M, Larsen MN, Nielsen G, Krustrup P. The importance of cohesion and enjoyment for the fitness improvement of 8–10-year-old children participating in a team and individual sport school-based physical activity intervention. European Journal of Sport Science. 2017;17(3):343–50. doi: 10.1080/17461391.2016.1260641 ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 57.Espinoza-Silva M, Latorre-Roman PA, Parraga-Montilla J, Caamano-Navarrete F, Jerez-Mayorga D, Delgado-Floody P. Response of obese schoolchildren to high-intensity interval training applied in the school context. Endocrinologia Diabetes y Nutricion. 2019;66(10):611–9. doi: 10.1016/j.endinu.2019.05.005 . [DOI] [PubMed] [Google Scholar]
- 58.Gamelin F-X, Baquet G, Berthoin S, Thevenet D, Nourry C, Nottin S, et al. Effect of high intensity intermittent training on heart rate variability in prepubescent children. European Journal of Applied Physiology. 2009;105(5):731–8. doi: 10.1007/s00421-008-0955-8 ; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 59.Granacher U, Goesele A, Roggo K, Wischer T, Fischer S, Zuerny C, et al. Effects and Mechanisms of Strength Training in Children. Int J Sports Med. 2011;32(5):357–64. doi: 10.1055/s-0031-1271677 . [DOI] [PubMed] [Google Scholar]
- 60.Haghshenas R, Jamshidi Z, Doaei S, Gholamalizadeh M. The Effect of a High-intensity Interval Training on Plasma Vitamin D Level in Obese Male Adolescents. Indian Journal of Endocrinology and Metabolism. 2019;23(1):72–5. doi: 10.4103/ijem.IJEM_267_18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kennedy SG, Leahy AA, Smith JJ, Eather N, Hillman CH, Morgan PJ, et al. Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial. Children (Basel). 2020;7(12):16. 10.3390/children7120299 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ketelhut S, Kircher E, Ketelhut SR, Wehlan E, Ketelhut K. Effectiveness of Multi-activity, High-intensity Interval Training in School-aged Children. Int J Sports Med. 2020;14:14. doi: 10.1055/a-1068-9331 . [DOI] [PubMed] [Google Scholar]
- 63.Lambrick D, Westrupp N, Kaufmann S, Stoner L, Faulkner J. The effectiveness of a high-intensity games intervention on improving indices of health in young children. Journal of Sports Sciences. 2016;34(3):190–8. doi: 10.1080/02640414.2015.1048521 [DOI] [PubMed] [Google Scholar]
- 64.Larsen MN, Nielsen CM, Orntoft C, Randers MB, Helge EW, Madsen M, et al. Fitness Effects of 10-Month Frequent Low-Volume Ball Game Training or Interval Running for 8-10-Year-Old School Children. Biomed Res Int. 2017;2017:2719752. 10.1155/2017/2719752 ; PubMed Central PMCID: PMC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leahy AA, Eather N, Smith JJ, Hillman CH, Morgan PJ, Plotnikoff RC, et al. Feasibility and Preliminary Efficacy of a Teacher-Facilitated High-Intensity Interval Training Intervention for Older Adolescents. Pediatric Exercise Science. 2019;31(1):107–17. doi: 10.1123/pes.2018-0039 3. [DOI] [PubMed] [Google Scholar]
- 66.Leahy AA, Michels MFI, Eather N, Hillman CH, Shigeta TT, Lubans DR, et al. Feasibility of test administration and preliminary findings for cognitive control in the Burn 2 learn pilot randomised controlled trial. Journal of Sports Sciences. 2020;38(15):1708–16. 10.1080/02640414.2020.1756673 . [DOI] [PubMed] [Google Scholar]
- 67.Logan GRM, Harris N, Duncan S, Plank LD, Merien F, Schofield G. Low-Active Male Adolescents: A Dose Response to High-Intensity Interval Training. Medicine & Science in Sports & Exercise. 2016;48(3):481–90. doi: 10.1249/MSS.0000000000000799 . Language: English. Entry Date: 20170629. Revision Date: 20170629. Publication Type: Article. [DOI] [PubMed] [Google Scholar]
- 68.Lubans DR, Smith JJ, Eather N, Leahy AA, Morgan PJ, Lonsdale C, et al. Time-efficient intervention to improve older adolescents’ cardiorespiratory fitness: findings from the ’Burn 2 Learn’ cluster randomised controlled trial. Br J Sports Med. 2020;21:21. 10.1136/bjsports-2020-103277 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martin R, Buchan DS, Baker JS, Young J, Sculthorpe N, Grace FM. Sprint interval training (SIT) is an effective method to maintain cardiorespiratory fitness (CRF) and glucose homeostasis in Scottish adolescents. Biology of Sport. 2015;32(4):307–13. doi: 10.5604/20831862.1173644 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Martin-Smith R, Buchan DS, Baker JS, Macdonald MJ, Sculthorpe NF, Easton C, et al. Sprint Interval Training and the School Curriculum: Benefits Upon Cardiorespiratory Fitness, Physical Activity Profiles, and Cardiometabolic Risk Profiles of Healthy Adolescents. Pediatric Exercise Science. 2019;31(3):296–305. doi: 10.1123/pes.2018-0155 . [DOI] [PubMed] [Google Scholar]
- 71.McManus A, Armstrong N, Williams C. Effect of training on the aerobic power and anaerobic performance of prepubertal girls. Acta Paediatrica. 1997;86(5):456–9. doi: 10.1111/j.1651-2227.1997.tb08912.x [DOI] [PubMed] [Google Scholar]
- 72.McManus AM, Cheng CH, Leung MP, Yung TC, Macfarlane DJ. Improving Aerobic Power in Primary School Boys: A Comparison of Continuous and Interval Training. Int J Sports Med. 2005;26(9):781–6. PubMed PMID: SPHS-1008528; PubMed Central PMCID: PMC. doi: 10.1055/s-2005-837438 [DOI] [PubMed] [Google Scholar]
- 73.McNarry MA, Lambrick D, Westrupp N, Faulkner J. The influence of a six-week, high-intensity games intervention on the pulmonary oxygen uptake kinetics in prepubertal obese and normal-weight children. Applied Physiology, Nutrition & Metabolism. 2015;40(10):1012–8. doi: 10.1139/apnm-2015-0051 . [DOI] [PubMed] [Google Scholar]
- 74.McNarry MA, Winn CON, Davies GA, Eddolls WTB, Mackintosh KA. Effect of High-Intensity Training and Asthma on the V[Combining Dot Above]O2 Kinetics of Adolescents. Medicine & Science in Sports & Exercise. 2020;16:16. doi: 10.1249/MSS.0000000000002270 . [DOI] [PubMed] [Google Scholar]
- 75.Moreau D, Kirk IJ, Waldie KE. High-intensity training enhances executive function in children in a randomized, placebo-controlled trial. eLife. 2017;6 (no pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mucci P, Baquet G, Nourry C, Deruelle F, Berthoin S, Fabre C. Exercise Testing in Children: Comparison in Ventilatory Thresholds Changes with Interval-Training. Pediatr Pulmonol. 2013;48(8):809–16. doi: 10.1002/ppul.22646 PubMed PMID: WOS:000321977200010; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 77.Muntaner-Mas A P. P. EFFECTS OF HIGH INTENSITY INTERVAL TRAINING (HIIT) INTERVENTION AMONGST SCHOOL ADOLESCENTS. Journal of Physical Education & Health. 2017;6(10):19–25. [Google Scholar]
- 78.Nourry C, Deruelle F, Guinhouya C, Baquet G, Fabre C, Bart F, et al. High-intensity intermittent running training improves pulmonary function and alters exercise breathing pattern in children. European Journal of Applied Physiology. 2005;94(4):415–23. doi: 10.1007/s00421-005-1341-4 PubMed PMID: WOS:000230071900009; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 79.Racil G, Ben Ounis O, Hammouda O, Kallel A, Zouhal H, Chamari K, et al. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. European Journal of Applied Physiology. 2013;113(10):2531–40. doi: 10.1007/s00421-013-2689-5 PubMed PMID: WOS:000324379600011; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 80.Racil G, Coquart JB, Elmontassar W, Haddad M, Goebel R, Chaouachi A, et al. Greater effects of high- compared with moderate-intensity interval training on cardio-metabolic variables, blood leptin concentration and ratings of perceived exertion in obese adolescent females. Biology of Sport. 2016;33(2):145–52. doi: 10.5604/20831862.1198633 ; PubMed Central PMCID: PMC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Racil G, Zouhal H, Elmontassar W, Abderrahmane AB, De Sousa MV, Chamari K, et al. Plyometric exercise combined with high-intensity interval training improves metabolic abnormalities in young obese females more so than interval training alone. Applied Physiology, Nutrition & Metabolism. 2016;41(1):103–9. doi: 10.1139/apnm-2015-0384 . [DOI] [PubMed] [Google Scholar]
- 82.Reyes-Amigo T, Molina JS, Martinez Mera G, De Souza Lima J, Ibarra Mora J, Soto-SÁNchez J. Contribution of high and moderate-intensity physical education classes to the daily physical activity level in children. Journal of Physical Education & Sport. 2021;21(1):29–35. . [Google Scholar]
- 83.Ruiz-Ariza A, Suárez-Manzano S, López-Serrano S, Martínez-López EJ. The effect of cooperative high-intensity interval training on creativity and emotional intelligence in secondary school: A randomised controlled trial. European Physical Education Review. 2019;25(2):355–73. . [Google Scholar]
- 84.Segovia Y, GutiÉRrez D. Effect of a game-based high intensity interval training program on body composition in primary education: comparison of the Sport Education model and traditional methodology. Journal of Physical Education & Sport. 2020;20(2):791–9. . [Google Scholar]
- 85.van Biljon A, McKune AJ, DuBose KD, Kolanisi U, Semple SJ. Do Short-Term Exercise Interventions Improve Cardiometabolic Risk Factors in Children? Journal of Pediatrics. 2018;203:325–9. doi: 10.1016/j.jpeds.2018.07.067 . Language: English. Entry Date: In Process. Revision Date: 20181125. Publication Type: journal article. Journal Subset: Biomedical; PubMed Central PMCID: PMC. [DOI] [PubMed] [Google Scholar]
- 86.Van Biljon A, McKune AJ, Dubose KD, Kolanisi U, Semple SJ. Short-term high-intensity interval training is superior to moderate-intensity continuous training in improving cardiac autonomic function in children. Cardiology (Switzerland). 2018;141(1):1–8. doi: 10.1159/000492457 [DOI] [PubMed] [Google Scholar]
- 87.Weston KL, Azevedo LB, Bock S, Weston M, George KP, Batterham AM. Effect of Novel, School-Based High-Intensity Interval Training (HIT) on Cardiometabolic Health in Adolescents: Project FFAB (Fun Fast Activity Blasts)—An Exploratory Controlled Before-And-After Trial. PLoS ONE. 2016;11(8):e0159116. 10.1371/journal.pone.0159116 ; PubMed Central PMCID: PMC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Williams CA, Armstrong N, Powell J. Aerobic responses of prepubertal boys to two modes of training. Br J Sports Med. 2000;34(3):168–73. doi: 10.1136/bjsm.34.3.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bassali R, Waller JL, Gower B, Allison J, Davis CL. Utility of waist circumference percentile for risk evaluation in obese children. International Journal of Pediatric Obesity. 2010;5(1):97–101. doi: 10.3109/17477160903111722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kelishadi R, Mirmoghtadaee P, Najafi H, Keikha M. Systematic review on the association of abdominal obesity in children and adolescents with cardio-metabolic risk factors. J Res Med Sci. 2015;20(3):294–307. Epub 2015/06/26. ; PubMed Central PMCID: PMC4468236. [PMC free article] [PubMed] [Google Scholar]
- 91.Xi B, Zong XN, Kelishadi R, Litwin M, Hong YM, Poh BK, et al. International Waist Circumference Percentile Cutoffs for Central Obesity in Children and Adolescents Aged 6 to 18 Years. The Journal of Clinical Endocrinology & Metabolism. 2020;105(4):e1569–e83. doi: 10.1210/clinem/dgz195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. International Journal of Obesity. 2011;35(7):891–8. doi: 10.1038/ijo.2010.222 [DOI] [PubMed] [Google Scholar]
- 93.Ayer J, Charakida M, Deanfield JE, Celermajer DS. Lifetime risk: childhood obesity and cardiovascular risk. European Heart Journal. 2015;36(22):1371–6. doi: 10.1093/eurheartj/ehv089 [DOI] [PubMed] [Google Scholar]
- 94.Dencker M, Thorsson O, Karlsson MK, Lindén C, Wollmer P, Andersen LB. Daily physical activity related to aerobic fitness and body fat in an urban sample of children. Scandinavian Journal of Medicine & Science in Sports. 2008;18(6):728–35. doi: 10.1111/j.1600-0838.2007.00741.x [DOI] [PubMed] [Google Scholar]
- 95.Ekelund U, Anderssen SA, Froberg K, Sardinha LB, Andersen LB, Brage S. Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: the European youth heart study. Diabetologia. 2007;50(9):1832–40. doi: 10.1007/s00125-007-0762-5 [DOI] [PubMed] [Google Scholar]
- 96.Andersen LB, Hasselstrøm H, Grønfeldt V, Hansen S, Karsten F. The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish Youth and Sport Study. Int J Behav Nutr Phys Act. 2004;1(1):6. doi: 10.1186/1479-5868-1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Moliner-Urdiales D, Ortega FB, Vicente-Rodriguez G, Rey-Lopez JP, Gracia-Marco L, Widhalm K, et al. Association of physical activity with muscular strength and fat-free mass in adolescents: the HELENA study. European Journal of Applied Physiology. 2010;109(6):1119–27. doi: 10.1007/s00421-010-1457-z [DOI] [PubMed] [Google Scholar]
- 98.Martínez-Gómez D, Welk GJ, Puertollano MA, Del-Campo J, Moya JM, Marcos A, et al. Associations of physical activity with muscular fitness in adolescents. Scandinavian Journal of Medicine & Science in Sports. 2011;21(2):310–7. doi: 10.1111/j.1600-0838.2009.01036.x [DOI] [PubMed] [Google Scholar]
- 99.Gutin B, Owens S. The Influence of Physical Activity on Cardiometabolic Biomarkers in Youths: A Review. Pediatric Exercise Science. 2011;23(2):169–85. doi: 10.1123/pes.23.2.169 [DOI] [PubMed] [Google Scholar]
- 100.Shen W, Zhang T, Li S, Zhang H, Xi B, Shen H, et al. Race and Sex Differences of Long-Term Blood Pressure Profiles From Childhood and Adult Hypertension. Hypertension. 2017;70(1):66–74. doi: 10.1161/HYPERTENSIONAHA.117.09537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ma JK, Le Mare L, Gurd BJ. Classroom-based high-intensity interval activity improves off-task behaviour in primary school students. Applied Physiology, Nutrition, & Metabolism = Physiologie Appliquee, Nutrition et Metabolisme. 2014;39(12):1332–7. doi: 10.1139/apnm-2014-0125 . [DOI] [PubMed] [Google Scholar]
- 102.Taylor KL, Weston M, Batterham AM. Evaluating Intervention Fidelity: An Example from a High-Intensity Interval Training Study. PLoS ONE. 2015;10(4):e0125166. doi: 10.1371/journal.pone.0125166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Leahy AA, Mavilidi MF, Smith JJ, Hillman CH, Eather N, Barker D, et al. Review of High-Intensity Interval Training for Cognitive and Mental Health in Youth. Medicine & Science in Sports & Exercise. 2020;52:2224–34. doi: 10.1249/MSS.0000000000002359 [DOI] [PubMed] [Google Scholar]
- 104.De Greeff JW, Bosker RJ, Oosterlaan J, Visscher C, Hartman E. Effects of physical activity on executive functions, attention and academic performance in preadolescent children: a meta-analysis. Journal of Science and Medicine in Sport. 2018;21(5):501–7. doi: 10.1016/j.jsams.2017.09.595 [DOI] [PubMed] [Google Scholar]
- 105.Weston K, Barker AR, Bond B, Costigan SA, Ingul C, Williams C. The BASES Expert Statement on the Role of High-intensity Interval Exercise for Health and Fitness Promotion in Young People. The Sport and Exercise Scientist. 2020;(64). [Google Scholar]
- 106.Barnett EY, Ridker PM, Okechukwu CA, Gortmaker SL. Integrating children’s physical activity enjoyment into public health dialogue (United States). Health Promotion International. 2019;34(1):144–53. doi: 10.1093/heapro/dax068 [DOI] [PubMed] [Google Scholar]
- 107.Oliveira BRR, Santos TM, Kilpatrick M, Pires FO, Deslandes AC. Affective and enjoyment responses in high intensity interval training and continuous training: A systematic review and meta-analysis. PLoS ONE. 2018;13(6):e0197124. doi: 10.1371/journal.pone.0197124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Enright E, O’Sullivan M. ‘Can I do it in my pyjamas?’ Negotiating a physical education curriculum with teenage girls. European Physical Education Review. 2010;16(3):203–22. doi: 10.1177/1356336x10382967 [DOI] [Google Scholar]
- 109.Cairney J, Kwan MY, Velduizen S, Hay J, Bray SR, Faught BE. Gender, perceived competence and the enjoyment of physical education in children: a longitudinal examination. Int J Behav Nutr Phys Act. 2012;9(1):26. doi: 10.1186/1479-5868-9-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Stylianou M. Health Benefits of Physical Activity: Cognitive Performance and School Engagement. Active and Healthy Journal. 2018;25(2/3):32–8. [Google Scholar]