Abstract
IMPORTANCE
Orphans and vulnerable children (OVC) are at high risk for experiencing trauma and related psychosocial problems. Despite this, no randomized clinical trials have studied evidence-based treatments for OVC in low-resource settings.
OBJECTIVE
To evaluate the effectiveness of lay counselor–provided trauma-focused cognitive behavioral therapy (TF-CBT) to address trauma and stress-related symptoms among OVC in Lusaka, Zambia.
DESIGN, SETTING, AND PARTICIPANTS
This randomized clinical trial compared TF-CBT and treatment as usual (TAU) (varying by site) for children recruited from August 1, 2012, through July 31, 2013, and treated until December 31, 2013, for trauma-related symptoms from 5 community sites within Lusaka, Zambia. Children were aged 5 through 18 years and had experienced at least one traumatic event and reported significant trauma-related symptoms. Analysis was with intent to treat.
INTERVENTIONS
The intervention group received 10 to 16 sessions of TF-CBT (n = 131). The TAU group (n = 126) received usual community services offered to OVC.
MAIN OUTCOMES AND MEASURES
The primary outcome was mean item change in trauma and stress-related symptoms using a locally validated version of the UCLA Posttraumatic Stress Disorder Reaction Index (range, 0–4) and functional impairment using a locally developed measure (range, 0–4). Outcomes were measured at baseline and within 1 month after treatment completion or after a waiting period of approximately 4.5 months after baseline for TAU.
RESULTS
At follow-up, the mean item change in trauma symptom score was −1.54 (95% CI, −1.81 to −1.27), a reduction of 81.9%, for the TF-CBT group and −0.37 (95% CI, −0.57 to −0.17), a reduction of 21.1%, for the TAU group. The mean item change for functioning was −0.76 (95% CI, −0.98 to −0.54), a reduction of 89.4%, and −0.54 (95% CI, −0.80 to −0.29), a reduction of 68.3%, for the TF-CBT and TAU groups, respectively. The difference in change between groups was statistically significant for both outcomes (P < .001). The effect size (Cohen d) was 2.39 for trauma symptoms and 0.34 for functioning. Lay counselors participated in supervision and assessed whether the intervention was provided with fidelity in all 5 community settings.
CONCLUSIONS AND RELEVANCE
The TF-CBT adapted for Zambia substantially decreased trauma and stress-related symptoms and produced a smaller improvement in functional impairment among OVC having experienced high levels of trauma.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT01624298
There are 15.1 million youth orphaned by AIDS in sub-Saharan Africa, with numbers predicted to increase.1,2 Orphans and vulnerable children (OVC) (groups of children that experience negative outcomes, such as the loss of their education, morbidity, and malnutrition, at higher rates than do their peers) experience multiple traumatic experiences, including abuse and exploitation, premature parental death, human immunodeficiency virus (HIV) infection and stigma, poor health care, poverty, reduced social support, and abbreviated childhood and education.3–5 Given the association of childhood trauma with skill deficits and unhealthy decision making,6–8 as well as with long-term negative health outcomes,9 early and effective mental health intervention is critical to the care of OVC. However, little evidence exists about what types of programs enhance the well-being of OVC.10
We have conducted studies in Zambia to understand local mental and behavioral health problems, validate mental and behavioral assessment instruments, and examine the cross-cultural feasibility of evidence-based treatment.11–15 These studies culminated in the randomized clinical trial reported in this article, which tests the effectiveness of trauma-focused cognitive behavioral therapy (TF-CBT; http://tfcbt.musc.edu/)16 for OVC compared with treatment as usual (TAU) provided by lay counselors without previous mental health care training. This trial was a collaboration with Serenity Harm Reduction Programme Zambia, a local nongovernmental organization.
Methods
Participants
This study included children recruited from August 1, 2012, through July 31, 2013, and treated until December 31, 2013, for trauma-related symptoms. The 5 study sites included a home-based care program, program for street children, government health clinic, public school, and school or residential program. Inclusion criteria were age of 5 through 18 years, living within a site catchment area, history of at least one traumatic event, and significant trauma-related symptoms (mean item score of ≥1.0 on the locally validated UCLA Posttraumatic Stress Disorder Reaction Index [PTSD-RI]).12 Exclusion criteria were child or legal caregivers not mentally competent to give consent or currently receiving psychiatric treatment. Assessors were trained in signs of psychosis and called a supervisor for further assessment if any signs were present.
Recruitment and Consent
Participants were recruited from existing clients at the study sites. Site staff members were familiar with the clientele and referred potentially eligible children to a study assessor. Eleven trained study assessors, selected by the sites based on set requirements, obtained oral informed consent from the caretaker and child for screening and, if eligible, the full study. All interviews were conducted in a confidential location at the 5 study sites in the participant’s preferred language via interview format.
Study Protocol
Each trial consent form contained a participant identification number. Once an eligible child consented, the child was assigned that number and completed a baseline assessment. The assessor then opened a sealed envelope stapled to the consent form, which indicated random assignment (TF-CBT vs TAU). Random assignment was performed offsite by a Johns Hopkins University investigator (J.C.K.) who kept a master list of identification numbers to enable checks of fidelity. All participants were informed that they could continue receiving community services as they wished, including counseling services. The study protocol can be found in the trial protocol in Supplement 1.
Postassessments were completed within 1 month after TF-CBT completion (for the TAU participants, approximately 4 months after baseline). To ensure masked assessment, assessors from a site other than where the participant received services completed the postassessment. At postassessment, all TAU participants were offered TF-CBT.
Safety Protocol
A safety protocol was developed as part of the standard assessment procedures for both conditions.17 The protocol specified steps for assessing risk, a notification tree, and possible referrals. The Institutional Review Board of Johns Hopkins Bloomberg School of Public Health and the local Zambian institutional review board, ERES Converge, approved the study protocol.
Intervention
The TF-CBT is typically conducted in weekly 60- to 90-minute sessions with the child and caregiver (if available) and involves provision of 9 components16 (Box). Twenty adult counselors (11 from the sites and 12 external) were trained in TF-CBT via the apprenticeship model: a 10-day on-site training of counselors and supervisors, followed by weekly meetings of local supervisors with groups of counselors and weekly supervisor consultation with TF-CBT experts.18 Backgrounds varied, but all counselors had at least a high school education and basic communication and social skills. One supervisor had been a TF-CBT counselor in a previous study, and another supervisor was selected from the counselor group given her strong understanding of the model and clinical skills.
Box. Description of TF-CBT Components and TAU Services.
| TF-CBT a | Enhancing safety skills |
| Component | Developing a safety plan linked to the trauma experience and possible future challenges |
| Brief description | TAU |
| Psychoeducation (introduction) | Site |
| Program information (duration, content, and expectations) | Services offeredb |
| Normalization of symptoms and problems | Barefeet (community outreach) |
| Parenting skills | Psychosocial counseling |
| Praise | Peer education |
| Rewards | Prevention of HIV and AIDS |
| One-on-one time | City of Hope (community school or residence) |
| Relaxation | Education and assistance (school fees) |
| Strategies to reduce physiological tension and stress | Nutrition |
| Affective modulation | Room and board for adolescent girls |
| Identifying feelings, linking them to situations, and rating intensity of emotions | Kaunda Square Ministry of Health Clinic |
| Cognitive coping | Primary health care services |
| Distinguish and connect thoughts, feelings, and behaviors | St Paul’s School |
| Evaluate and restructure thoughts to be more accurate and/or helpful | Education |
| Trauma narrative (imaginal gradual exposure) | Psychosocial and guidance counseling |
| Facing feared and/or avoided traumatic memories through writing or drawing | Ngombe home-based care |
| Identifying related thoughts and feelings | Medical support and referrals |
| Restructuring unhelpful thoughts from the trauma narrative | Support groups |
| In vivo exposure (live exposure) | Community outreach |
| Facing innocuous triggers or reminders in the client’s environment | |
| Conjoint session | |
| Sharing of the trauma narrative and restructured thoughts between child and supportive caregiver (if available) |
Abbreviations: HIV, human immunodeficiency virus; TAU, treatment as usual; TF-CBT, trauma-focused cognitive behavioral therapy.
See Cohen et al16 for a more detailed description.
In addition to site-specific services received, additional services included spiritual care, medical, HIV and AIDS treatment, and/or voluntary counseling and testing.
Studies in the United States have found TF-CBT to be highly effective in treating the sequelae of child trauma19,20 with sustained benefit at 6 to 24 months after treatment.21–23 Research suggests broad applicability across a wide range of trauma types and acceptability among ethnically diverse therapists, children, and parents.24 We previously modified TF-CBT for Zambia13 and documented its feasibility in an open trial.15
At the time of this study, there were no other evidence-based programs for trauma-related symptoms among OVC against which to compare TF-CBT. However, OVC commonly receive various forms and amounts of psychosocial programming in Zambia, including counseling (eg, support groups and nonspecific counseling), education, nutrition, and HIV-related services,10 which could affect mental health. Participants randomized to the TAU group continued to receive these types of regular services specific to each site (Box). Participants in the TAU group were telephoned weekly and visited once a month by a study assessor to evaluate safety (eg, suicidal ideation) and need for referral to other critical services (eg, medical assistance). For participants without a telephone, assessors attempted to provide in-person visits.
Intervention Fidelity
Counselors documented how they provided each component according to specific steps detailed in the manual. Supervisors elicited (from counselors) and recorded session details (techniques used and homework assigned) during weekly supervision meetings. If a component (eg, relaxation) or component step was missed (eg, assigning homework), the supervisor requested completion in the next session. The local supervisor and counselor discussed and/or role-played the component and planning for the next session. A TF-CBT expert (L.K.M., S.S., or S.D.) recorded detailed notes from the supervisors’ weekly verbal reports, checking that all TF-CBT components were provided with proper technique or, if not, asked for those components to be provided again.
Outcome Measurements
The PTSD-RI was used to identify traumatic events a child had experienced or witnessed and the associated PTSD symptoms.25 The PTSD-RI was translated into 3 Zambian languages, validated, and adapted for local use, including the addition of 18 local symptoms to the original 20 items (eTable 1 in Supplement 2).12 Participants reported whether they had ever experienced 13 events. Responses were summed to create a total traumatic event score (range, 0–13). Response options for the 38 symptoms ranged from 0 (never) to 4 (most of the time) and were used to calculate a mean trauma symptom score for each respondent (the primary outcome). Internal consistency for the PTSD-RI 38-item trauma symptom scale at baseline was very good (α = .83), with similar results for children (aged 5–12 years) (α = .79) and adolescents (aged 13–18 years) (α = .84). Given no clear cutoff recommendation from our validation study, but taking into account the receiver operating characteristic curves, we decided to maximize sensitivity so that a response of 1 or more per item would be indicative of symptoms appropriate for TF-CBT.
Functional impairment was measured using locally developed scales and developed using methods described elsewhere.26 Items included tasks and/or activities that respondents frequently reported as regular aspects of caring for self, family, and/or community. Respondents reported current difficulty doing each activity compared with other children (0 for no difficulty to 4 for often cannot do). A mean item score (range, 0–4) was calculated for each participant. Internal consistency for the functional impairment scale was excellent (α = .90), with similar results for children (aged 5–12 years) (α = .92) and adolescents (aged 13–18 years) (α = .89).
Caretakers of child participants were asked to complete the Child Behavior Checklist.27 Adolescent respondents (aged 12–18 years) who reported sexual activity were asked about HIV risk behavior using the World AIDS Foundation measure,28 and those reporting alcohol or other substance use were assessed with the Alcohol, Smoking, and Substance Involvement Screening Test.29
Statistical Analysis
Analysis was with intent to treat. Baseline sample characteristics for the intervention and TAU conditions were compared to indicate whether randomization resulted in balanced groups. Multiple imputation (11 imputations) with chained equations was used to account for participant loss to follow-up and item-level missing data.30 Factors associated with dropout included sex (males more likely to drop out), age (older age associated with dropout), school status (those not currently in school more likely to drop out), trauma history (those with greater number of traumatic events more likely to drop out), and site (children in St Paul’s school more likely to drop out).
We used mixed-effects regression modeling to evaluate TF-CBT effectiveness for trauma symptoms and functional impairment outcomes. The trauma symptom outcome was a linear mixed-effects model; the functioning outcome model was a generalized linear mixed-effects model with a Poisson distribution and log link to account for right skewed data. Random effects for both models included the participant, site, and counselor. Fixed effects included intervention group, time, and an interaction term of intervention group × time. For the trauma symptom outcome, we estimated this model for the full 38-item modified PTSD-RI and also separately for the original 20 items and the local 18 items. We also estimated a version of these models adjusting for possible confounders; covariates were included in the adjusted model if they differed meaningfully between intervention and TAU groups at baseline or if they were significantly associated with change in the mean trauma symptom score or functional impairment score from baseline to postassessment (significance threshold of P < .05).
Estimates of effect size using the Cohen d statistic were calculated for each outcome by dividing the difference in mean change between treatment groups by the pooled baseline SD.31 All analyses were conducted using STATA software, version 13 (Stata Corp).
Sample size calculations were based on the comparison of difference between mean baseline and follow-up trauma symptom scores between the 2 study groups. We decided that the ability to detect a 25% difference in mean change would be substantial and worth finding. Using a t test assuming unknown but equal SDs, 80% power, and an α level of .05, we calculated that 100 children would be required in each study group. This was increased to 120 per group assuming a 20% loss to follow-up based on previous experience.
Results
Of 298 children screened, 257 (86.2%) were eligible and agreed to participate. These children were randomized to TF-CBT (n = 131) or TAU (n = 126) (Figure 1).
Figure 1.
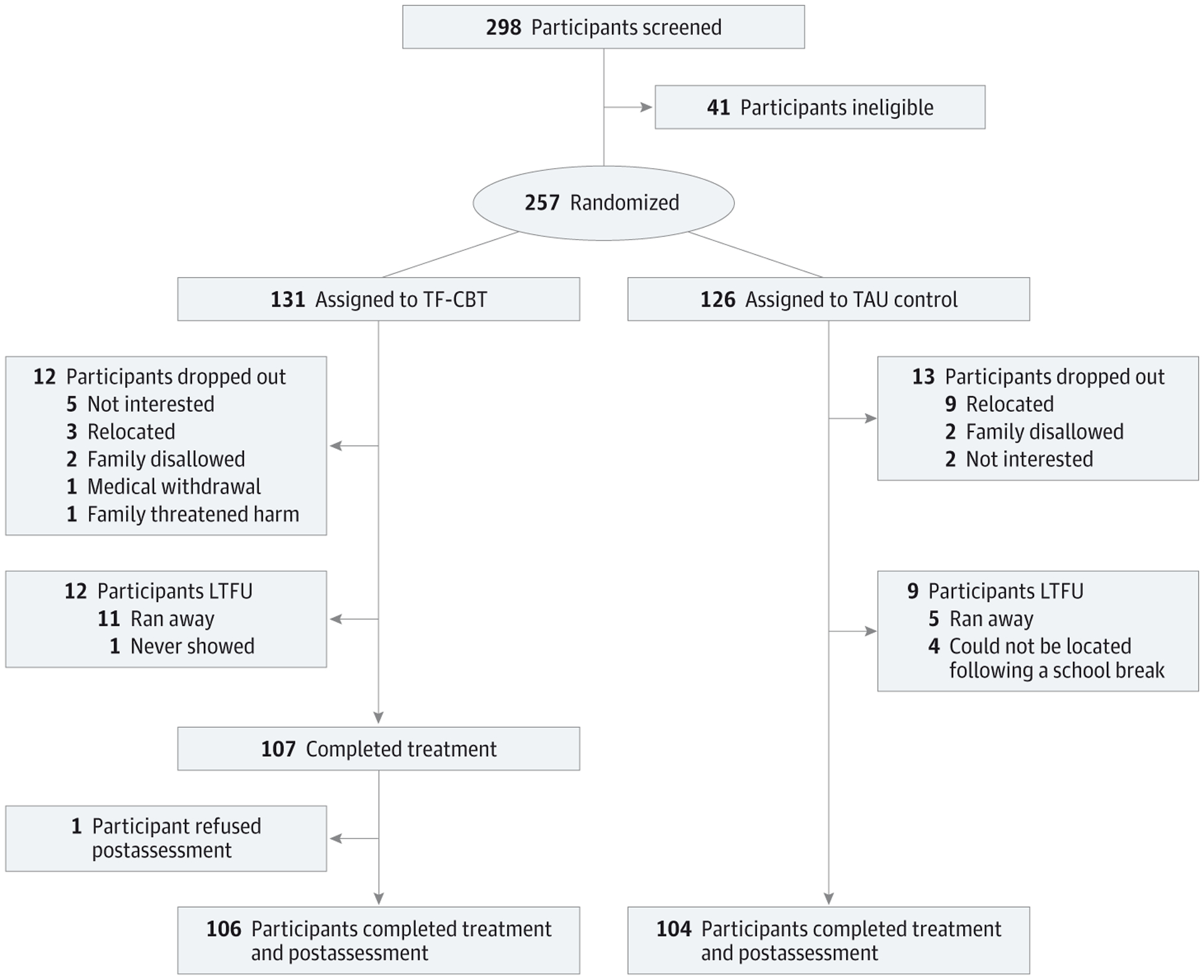
Flowchart of Study Participants Siblings were randomized together to the same treatment group. LTFU indicates lost to follow-up; TAU, treatment as usual; TF-CBT, trauma-focused cognitive behavioral therapy.
Baseline Characteristics
The only variable that appeared different between the groups was the length of time between baseline and postassessments, which was longer on average for the TF-CBT group (150.83 days) compared with the TAU group (116.03 days). Otherwise, baseline characteristics were similar between the groups (Table 1). Mean baseline trauma symptom scores (1.88 in the TF-CBT group and 1.75 in the TAU group) and functional impairment scores (0.85 in the TF-CBT group and 0.79 in the TAU group) were comparable between groups. The mean number of trauma events reported was 5.07, and Figure 2 summarizes the types.
Table 1.
Baseline Sociodemographic and Clinical Characteristics of the 257 Study Childrena
| Characteristic | TF-CBT Group (n = 131) | TAU Group (n = 126) |
|---|---|---|
| Male sex | 68 (51.9) | 61 (48.4) |
| Age, mean (SD) [range], y | 14.02 (2.77) [5–18] | 13.29 (2.99) [5–18] |
| Currently in school | 111 (84.7) | 112 (88.9) |
| Highest grade of school achieved | ||
| 1–3 | 41 (31.3) | 40 (31.8) |
| 4–5 | 21 (16.0) | 33 (26.2) |
| 6–7 | 42 (32.0) | 36 (28.6) |
| 8–9 | 26 (19.9) | 15 (11.9) |
| Ethnicity | ||
| Ngoni | 29 (22.1) | 26 (20.6) |
| Bemba | 42 (32.1) | 39 (31.0) |
| Other | 60 (45.8) | 59 (46.8) |
| Primary caretaker | ||
| Mother or father | 54 (41.2) | 37 (29.4) |
| Someone else | 75 (57.3) | 86 (68.3) |
| No one | 2 (1.5) | 3 (2.4) |
| Mother alive | 85 (64.9) | 70 (55.6) |
| Father alive | 70 (53.4) | 61 (48.4) |
| Score, mean (SD) [range] | ||
| Trauma symptoms | 1.88 (0.52) [1.0–3.24] | 1.75 (0.45) [1.0–3.03] |
| Functional impairment | 0.85 (0.67) [0–2.94] | 0.79 (0.64) [0–2.41] |
| No. of trauma types experienced, mean (SD) [range] | 4.96 (2.35) [0–11] | 5.18 (2.08) [0–10] |
| Time between assessments, mean (SD) [range], d | 150.83 (67.51) [47–384] | 116.03 (56.43) [31–328] |
Abbreviations: TAU, treatment as usual; TF-CBT, trauma-focused cognitive behavioral therapy.
Table includes all available data at baseline. Multiple imputation not conducted for data included in this table. Data are presented as number (percentage) of children unless otherwise indicated.
Figure 2.
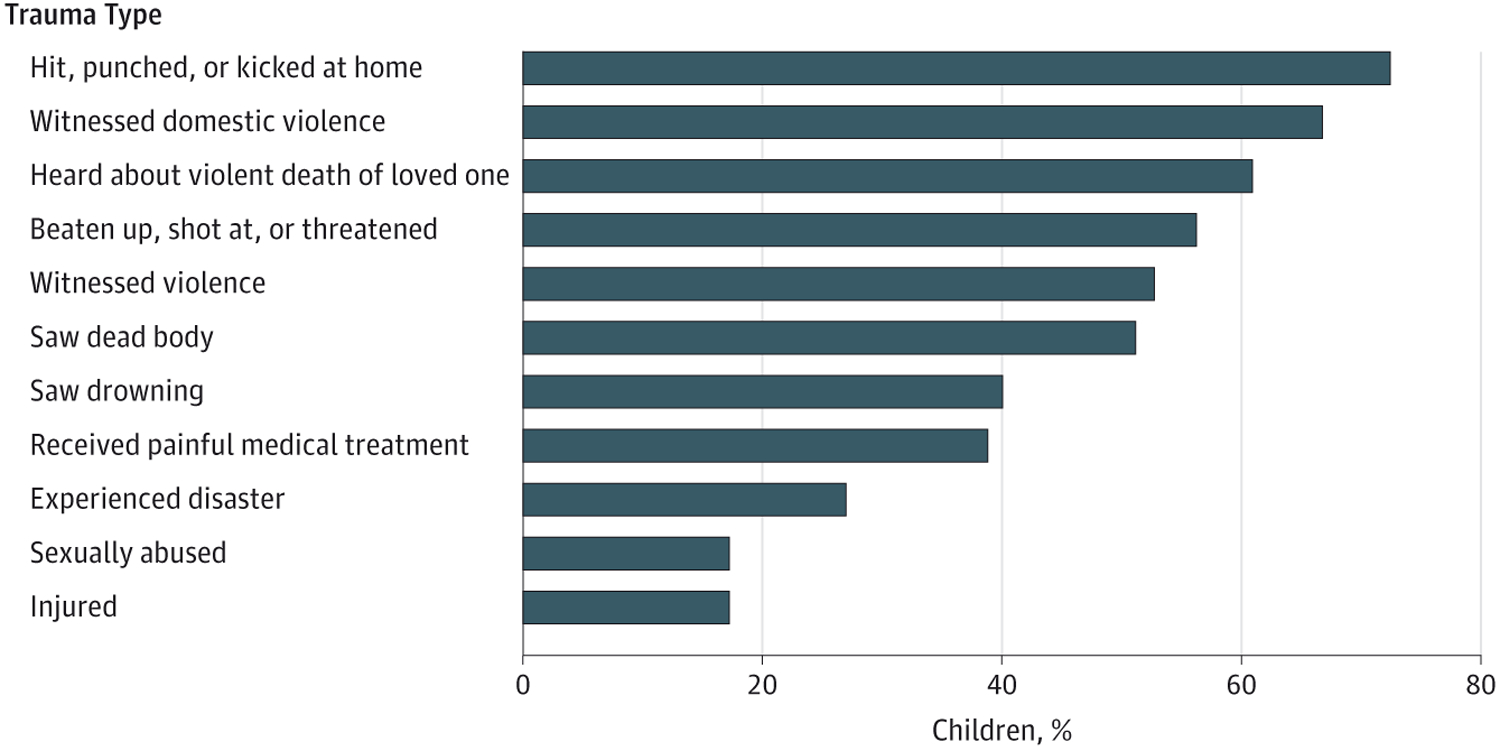
Proportion of the 257 Children Reporting Lifetime Experience for Each Trauma Type at Baseline
Outcomes of the TF-CBT vs TAU Groups
Mean trauma symptom score change from baseline to postassessment was −1.54 (95% CI, −1.81 to −1.27) for the TF-CBT group and −0.37 (95% CI, −0.57 to −0.17) for the TAU group. The larger reduction in the TF-CBT group compared with the TAU group was significant (P < .001), rendering an effect size of 2.39 (Table 2). We also conducted this analysis separately for the 20-item original PTSD-RI scale (effect size, 2.57) and the 18 item local symptom scale (effect size, 1.68) (eTable 2 in Supplement 2).
Table 2.
Predicted Mean Outcome Scores, Mean Change Scores, and Between-Treatment Group Effect Sizes, Adjusted for Clustering by Counselor, Site, and Participant
| Outcome | TF-CBT Group (n = 131)a | TAU Group (n = 126)a | Mean Change Difference (95% CI)b | P Valuec | Effect Sized | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI)b | Change, % | Mean Change (95% CI)b | Mean (95% CI)b | Change, % | Mean Change (95% CI)b | ||||||
| Baseline | Postassessment | Baseline | Postassessment | ||||||||
| Trauma symptomse | 1.88 (1.73 to 2.03) | 0.34 (0.20 to 0.48) | −81.9 | −1.54 (−1.81 to −1.27) | 1.75 (1.58 to 1.93) | 1.38 (1.20 to 1.57) | −21.1 | −0.37 (−0.57 to −0.17) | −1.17 (−1.45 to −0.89) | <.001 | 2.39 |
| Functional impairmente | 0.85 (0.65 to 1.12) | 0.09 (0.08 to 0.12) | −89.4 | −0.76 (−0.98 to −0.54) | 0.79 (0.58 to 1.06) | 0.25 (0.22 to 0.27) | −68.3 | −0.54 (−0.80 to −0.29) | −0.22 (−0.32 to −0.11) | <.001 | 0.34 |
Abbreviations: TF-CBT, trauma-focused cognitive behavioral therapy; TAU, treatment as usual.
All 257 participants were included in the analysis after multiple imputation procedures for loss to follow-up and item-level missing data.
The range for the trauma symptom and functional impairment outcomes was 0 to 4, with higher scores reflecting greater symptom severity and greater functional impairment, respectively. Estimates for mean, change, mean change, and mean change difference were calculated from the coefficients of the mixed-effects models accounting for clustering by participant, site, and counselor as described above after multiple imputation. The coefficients for the functioning model were back-transformed from the log scale by exponentiation.
P is the significance level of the mean change difference from the mixed-effects model indicating statistical significance of the difference in change of outcome score between the treatment and control groups from baseline to postassessment.
The Cohen d effect size was calculated by dividing mean change difference predicted from the unadjusted models (trauma symptom score, −1.17; functional impairment score, −0.22) by the pooled baseline SD (posttraumatic stress disorder score, 0.49; functional impairment score, 0.65). The absolute value of the effect size is presented.
The trauma symptoms model was a linear mixed-effects model, and the functional impairment model was a generalized linear mixed-effects model with a log link. Both models included random effects of participant, site, and counselor. The fixed effects included treatment group, time, and an interaction term of treatment group × time. Adjusted models that included additional fixed effects to control for potential confounding were also estimated and are included in eTable 2 in Supplement 2. There was no substantial difference in statistical significance or effect sizes between the adjusted and unadjusted models for either outcome; therefore, we present the more parsimonious unadjusted models.
Mean functional impairment score change from baseline to postassessment was −0.76 (95% CI, −0.98 to −0.54) for the TF-CBT group and −0.54 (95% CI, −0.80 to −0.29) for the TAU group. The larger reduction in the TF-CBT group compared with the TAU group was significant (P < .001), giving an effect size of 0.34 (Table 2).
These results were comparable to models adjusted for potential confounders (eTable 3 in Supplement 2) in which effect sizes were 2.41 and 0.26 for trauma symptoms and functioning, respectively. Therefore, only the unadjusted models are presented in the main article. In the adjusted models, covariates included length of time between assessments and primary caretaker (trauma and functioning models) and school status (functioning model).
Secondary outcomes of the trial are not reported. Only 58 participants (22.6%) reported ever having had sex at baseline, and only those respondents were eligible to respond to the HIV risk behavior questions. A total of 16 (47.1%) of those who responded that they ever had sex subsequently changed their answer and reported never having had sex at follow-up. Similarly, 14 (73.7%) of the participants who reported using tobacco, 38 (79.2%) who reported drinking alcohol, and 8 (61.5%) who reported using inhalants changed their responses at postassessment to never having used these substances.Because of the small sample size and inconsistent responses, no additional analyses were performed. We did not analyze the caretaker Child Behavior Checklist32 because of a very low response rate(33.9% at baseline and 6.2% at follow-up) due to competing demands (eg, other children and selling at the market).
Implementation Results
Counselors completed a mean of 7 sessions during the year (range, 2–12). Those who completed treatment (n = 107) received a mean (SD) of 11.77 (2.80) sessions (range, 6–21). Within the TAU group (n = 104), 82 expressed interest in TF-CBT and were assigned a counselor, suggesting treatment acceptability within the community. Eighteen high-risk cases were identified: child sexual abuse (n = 5), physical abuse (n = 2), severe neglect and verbal abuse (n = 1), suicidal ideation or plan (n = 8), and homicidal ideation (n = 2). All were successfully managed with the safety protocol.17 The Child Protection Unit was informed, and investigations took place for child abuse and neglect cases; only one case resulted in outside placement.
Discussion
Summary and Interpretation of Results
We evaluated the effectiveness of an individually provided, evidence-based mental health treatment (TF-CBT) for OVC with histories of experiencing traumatic events. The TF-CBT was significantly superior to TAU in reducing trauma and stress-related symptoms when provided by lay counselors.
This study adds to a small body of literature examining evidence-based treatments for youth in low- and middle income countries (LMICs), mostly among war-affected populations.33–36 Together, these studies indicate that it is feasible to implement evidence-based practices in lower-resource settings. Trauma-focused interventions (narrative exposure therapy and TF-CBT) revealed strong effect sizes (effect sizes, 0.5–1.80) on trauma symptoms in previous studies,33–35 with maintenance at longer-term follow-up. Our study adds to the literature by revealing that TF-CBT is also effective for other types of wide-ranging trauma and stressors as reported by the OVC in our sample. Studies examining a newly developed stabilization and skill-focused group intervention,36 art therapy,37 and school-based interventions,38 however, have found nonsignificant effects in reducing trauma-related symptoms in youth. Trauma-affected populations therefore may be better served by trauma-focused interventions as opposed to other psychosocial programs.
The effect size for TF-CBT on trauma symptoms was large compared with other trials of TF-CBT in the United States (effect sizes, 0.4–0.7)19 and Norway (Cohen d = 0.5).39 In high-resource settings, TAU is likely to be effective because these conditions are treated by highly trained and licensed mental health care professionals. In our study, like most LMICs, TAU consisted of diverse services with no established effectiveness on trauma-related symptoms provided by lay counselors with limited or no mental health education. Our effect sizes are similar to trials comparing interventions to controls or similar TAU conditions in other LMICs.33,35,40 The results should be generalizable to other OVC populations because there were few exclusion criteria and participants were exposed to a wide range of traumatic events.
The trial had some important limitations. First, for financial and grant-life reasons, postassessments were completed only once, approximately 1 month after treatment completion. It is unknown whether the results were maintained over time and thus must be interpreted carefully. However, multiple trials in the United States have sustained superior out comes during follow-up periods of 1 to 2 years.21–23 An open trial in Tanzania using the TF-CBT also found improvements in psychological symptoms sustained at 3 and 12 months after treatment (all P < .001).41 Second, this was a single-blind study. At postassessment, assessors were masked; however, participants were aware of their own study status and could have divulged this or been biased based on expectations. Third, TF-CBT ideally includes regular caregiver participation. Most caregivers in our study were not involved because of livelihood activities, caring for other children, and/or lack of transport funds. Other trials have also found positive results with no caregiver involvement,42 suggesting that this may not be critical. Fourth, the sample of the PTSD-RI validity study differed from the study population in terms of sex and sexual abuse as a common experience; however, most participants also reported other types of traumatic experiences. Finally, our functioning measure had many items that would be considered critical or basic, such as playing and bathing, resulting in a floor effect that made demonstration of change more difficult. Despite this, we observed a significant, though small, effect size.
Our results agree with other studies in the LMICs that have found that lay counselors can provide psychotherapeutic interventions with fidelity and effectiveness.33,40,43–46 Our study found challenges with workload and availability of counselors, indicated by completion of only a mean of 7 sessions during a year. The literature is increasing on the challenges inherent in a task-sharing approach, including, among others, workload of the new tasks, lack of funding or infrastructure, and the incentives provided to ensure workforce retention.47 The field needs to better understand how to create a place for trained lay counselors in the workforce and ensure the time needed to implement mental health treatments.
Conclusions
Abuse, neglect, and violence among children present serious global health challenges. Evidence-based treatments, such as TF-CBT, are commonly conceptualized as specialized services only needed by a small percentage of the population,48 with less specific interventions provided to larger numbers of children. However, research reveals that high numbers of OVC present with psychological distress,8,49,50 which represents a highly prevalent need for specific services. Findings that nonspecific interventions are minimally effective for psychological problems in youth after conflicts33,36,38,45 in combination with the current trial raise important questions for OVC programming. Further studies are needed to evaluate the effectiveness of widely funded psychosocial support interventions within OVC programs relative to interventions such as the TF-CBT for addressing mental health problems.
This is the first trial we are aware of that tested an evidence-based intervention specifically for OVC—a major population of concern in LMICs. Rigorous intervention trials for youth in LMICs are few compared with adult populations, despite the fact that 90% of the world’s children and adolescents live in LMICs.51 Close collaboration by funders, programmers, and researchers is needed so that the progress in child mental health does not lag behind that of adults.
Supplementary Material
At a Glance.
Orphans and vulnerable children (OVC) are at high risk for experiencing trauma and related psychosocial problems, yet little is known about what interventions may be effective.
Purpose: To evaluate the effectiveness of lay counselor–provided trauma-focused cognitive behavioral therapy (TF-CBT) compared with treatment as usual to address trauma and stress-related symptoms among OVC in Lusaka, Zambia.
Results: Trauma symptom score decreased by 81.9% among those who received TF-CBT, a statistically significantly greater reduction than the 21.1% reduction in symptoms among the treatment as usual group, resulting in an effect size of 2.39 (large effect).
The TF-CBT adapted for Zambia substantially decreased trauma and stress-related symptoms and produced a smaller improvement in functional impairment among OVC.
Funding/Support:
This study was supported by grant GHS-A-00-09-00004 Mod 6 from the US Agency for International Development Displaced Children’s and Orphans Fund.
Role of the Funder/Sponsor:
The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Supplemental content at jamapediatrics.com
REFERENCES
- 1.UNICEF. Towards an AIDS-Free Generation – Children and AIDS: Sixth Stocktaking Report, 2013. http://www.avert.org/children-orphaned-hiv-and-aids.htm#sthash.UT2jNnZs.dpuf. Accessed July 24, 2014.
- 2.UNAIDS. Towards an AIDS Free Generation. UNAIDS Children and AIDS Sixth Stocktaking Report. 2013. http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/unaidspublication/2013/20131129_stocktaking_report_children_aids_en.pdf. Accessed July 24, 2014. [Google Scholar]
- 3.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–1525. [DOI] [PubMed] [Google Scholar]
- 4.Benjet C Childhood adversities of populations living in low-income countries: prevalence, characteristics, and mental health consequences. Curr Opin Psychiatry. 2010;23(4):356–362. [DOI] [PubMed] [Google Scholar]
- 5.Idele P, Gillespie A, Porth T, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr. 2014;66(suppl 2):S144–S153. [DOI] [PubMed] [Google Scholar]
- 6.Monasch R, Boerma JT. Orphanhood and childcare patterns in sub-Saharan Africa: an analysis of national surveys from 40 countries. AIDS. 2004; 18(suppl 2):S55–S65. [DOI] [PubMed] [Google Scholar]
- 7.Andrews G, Skinner D, Zuma K. Epidemiology of health and vulnerability among children orphaned and made vulnerable by HIV/AIDS in sub-Saharan Africa. AIDS Care. 2006;18(3):269–276. [DOI] [PubMed] [Google Scholar]
- 8.Cluver L, Gardner F. The mental health of children orphaned by AIDS: a review of international and southern African research. J Child Adolesc Ment Health. 2007;19(1):1–17. [DOI] [PubMed] [Google Scholar]
- 9.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 10.Schenk KD. Community interventions providing care and support to orphans and vulnerable children: a review of evaluation evidence. AIDS Care. 2009;21(7):918–942. [DOI] [PubMed] [Google Scholar]
- 11.Murray LK, Haworth A, Semrau K, et al. Violence and abuse among HIV-infected women and their children in Zambia: a qualitative study. J Nerv Ment Dis. 2006;194(8):610–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray LK, Bass J, Chomba E, et al. Validation of the UCLA Child Posttraumatic stress disorder-reaction index in Zambia. Int J Ment Health Syst. 2011;5(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray LK, Dorsey S, Skavenski S, et al. Identification, modification, and implementation of an evidence-based psychotherapy for children in a low-income country: the use of TF-CBT in Zambia. Int J Ment Health Syst. 2013;7(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray LK, Skavenski S, Michalopoulos LM, et al. Counselor and client perspectives of Trauma-focused Cognitive Behavioral Therapy for children in Zambia: a qualitative study. J Clin Child Adolesc Psychol. 2014;43(6):902–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray LK, Familiar I, Skavenski S, et al. An evaluation of trauma focused cognitive behavioral therapy for children in Zambia. Child Abuse Negl. 2013;37(12):1175–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen JA, Mannarino A, Deblinger E. Treating Trauma and Traumatic Grief in Children and Adolescents. New York, NY: Guilford Press; 2006. [Google Scholar]
- 17.Murray LK, Skavenski S, Bass J, et al. Implementing evidence-based mental health care in low-resource settings: a focus on safety planning procedures. J Cogn Psychother. 2014;28(3):168–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray LK, Dorsey S, Bolton P, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int J Ment Health Syst. 2011; 5(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2004;43(4):393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorsey S, Briggs EC, Woods BA. Cognitive-behavioral treatment for posttraumatic stress disorder in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20(2):255–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse Negl. 2005;29(90):135–145. [DOI] [PubMed] [Google Scholar]
- 22.Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1474–1484. [DOI] [PubMed] [Google Scholar]
- 23.Deblinger E, Steer RA, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse Negl. 1999;23(12): 1371–1378. [DOI] [PubMed] [Google Scholar]
- 24.Huey SJ Jr, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. J Clin Child Adolesc Psychol. 2008;37(1):262–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steinberg AM, Brymer MJ, Kim S, et al. Psychometric properties of the UCLA PTSD reaction index: part I. J Trauma Stress. 2013;26(1):1–9. [DOI] [PubMed] [Google Scholar]
- 26.Johns Hopkins Bloomberg School of Public Health. The DIME Program Research Model: design, implementation, monitoring, and evaluation. 2013. http://www.jhsph.edu/research/centers-and-institutes/center-for-refugee-and-disaster-response/response_service/AMHR/dime/index.html. Accessed August 9, 2014.
- 27.Achenbach T Manual for the Child Behavior Checklist. Burlington: University of Vermont; 1992. [Google Scholar]
- 28.Sikkema KJ, Anderson ES, Kelly JA, et al. Outcomes of a randomized, controlled community-level HIV prevention intervention for adolescents in low-income housing developments. AIDS. 2005;19(14):1509–1516. [DOI] [PubMed] [Google Scholar]
- 29.Humeniuk RE, Henry-Edwards S, Ali RL, Poznyak V, Monteiro M The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for Use in Primary Care. Geneva, Switzerland; World Health Organization; 2010. [Google Scholar]
- 30.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen J Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 32.Achenbach TM, Rescorla LA. The Achenbach System of Empirically Based Assessment (ASEBA) for Ages 1.5 to 18 Years. Vol 2. 3rd ed. Mahwah, NJ: Erlbaum: 2004:179–213. [Google Scholar]
- 33.Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F. Community-implemented trauma therapy for former child soldiers in Northern Uganda: a randomized controlled trial. JAMA. 2011;306(5): 503–512. [DOI] [PubMed] [Google Scholar]
- 34.McMullen J, O’Callaghan P, Shannon C, Black A, Eakin J. Group trauma-focused cognitive-behavioural therapy with former child soldiers and other war-affected boys in the DR Congo: a randomised controlled trial. J Child Psychol Psychiatry. 2013;54(11):1231–1241. [DOI] [PubMed] [Google Scholar]
- 35.O’Callaghan P, McMullen J, Shannon C, Rafferty H, Black A. A randomized controlled trial of trauma-focused cognitive behavioral therapy for sexually exploited, war-affected Congolese girls. J Am Acad Child Adolesc Psychiatry. 2013;52(4): 359–369. [DOI] [PubMed] [Google Scholar]
- 36.Betancourt TS, McBain R, Newnham EA, et al. A behavioral intervention for war-affected youth in Sierra Leone: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2014;53(12):1288–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mueller J, Alie C, Jonas B, Brown E, Sherr L. A quasi-experimental evaluation of a community-based art therapy intervention exploring the psychosocial health of children affected by HIV in South Africa. Trop Med Int Health. 2011;16(1):57–66. [DOI] [PubMed] [Google Scholar]
- 38.Tol WA, Komproe IH, Jordans MJD, et al. School-based mental health intervention for children in war-affected Burundi: a cluster randomized trial. BMC Med. 2014;12(56):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jensen TK, Holt T, Ormhaug SM, et al. A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. J Clin Child Adolesc Psychol. 2014;43(3):356–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bolton P, Lee C, Haroz EE, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Med. 2014;11(11):e1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O’Donnell K, Dorsey S, Gong W, et al. Treating maladaptive grief and posttraumatic stress symptoms in orphaned children in Tanzania: group-based trauma-focused cognitive-behavioral therapy. J Trauma Stress. 2014;27(6):664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: Initial treatment outcome findings. Child Maltreat. 1996;1:310–321. [Google Scholar]
- 43.Bass JK, Annan J, McIvor Murray S, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med. 2013; 368(23):2182–2191. [DOI] [PubMed] [Google Scholar]
- 44.Bolton P, Bass J, Neugebauer R, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003; 289(23):3117–3124. [DOI] [PubMed] [Google Scholar]
- 45.Bolton P, Bass J, Betancourt T, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA. 2007;298(5):519–527. [DOI] [PubMed] [Google Scholar]
- 46.Patel V, Weiss HA, Chowdhary N, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376 (9758):2086–2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med. 2013;97:82–86. [DOI] [PubMed] [Google Scholar]
- 48.Interagency Standing Committee, World Health Organization. IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 49.Cluver L, Gardner F, Operario D. Psychological distress amongst AIDS-orphaned children in urban South Africa. J Child Psychol Psychiatry. 2007;48 (8):755–763. [DOI] [PubMed] [Google Scholar]
- 50.Whetten K, Ostermann J, Whetten RA, et al. ; Positive Outcomes for Orphans (POFO) Research Team. A comparison of the wellbeing of orphans and abandoned children ages 6–12 in institutional and community-based care settings in 5 less wealthy nations. PLoS One. 2009;4(12):e8169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.UNICEF. Statistics and Monitoring. 2010. http://www.unicef.org/statistics. Accessed September 2, 2014.
- 52.Tol WA, Komproe IH, Susanty D, Jordans MJD, Macy RD, De Jong JT. School-based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA. 2008;300(6):655–662. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


