Abstract
The failure to reduce maternal mortality rates in high-burden countries has led to calls for a greater understanding of structural determinants of inequities in access to maternal health services. Caste is a socially constructed identity that imposes structural disadvantages on subordinate groups. Although a South Asian construct, the existence of caste as a structural social stratifier is actively rejected in Muslim Pakistan as a regressive symbol of Hinduism. In this inimical context, the possibility of caste as a driver of maternal health care inequities is not acknowledged and has, therefore, remained unexplored in Pakistan. The objective of the present study is to quantitatively assess the variation in the use of maternity services across different caste groups in Pakistan. The research also contributes to methodological innovation in modelling relationships between caste, mediating and/or confounding socio-economic factors and maternal health service indicators. A clustered, stratified survey sampled 1457 mothers in districts Jhelum and Layyah. Multivariable, multi-level (confounder-adjusted) logistic regression analysis showed “Low” caste mothers had higher odds of landlessness, no education, working in unskilled occupations, asset poverty, no antenatal care and a home-based birth with an unskilled attendant compared to “High” or “Middling” caste individuals. Despite the important role of caste in patterning socio-economic disadvantage, its indirect causal effect on maternal health care was predominantly mediated through mothers’ education and household assets. Our findings suggest a need for group-specific policies, including constructing schools in low-caste dominant settlements, affirmative action with job quotas, redistributing agricultural lands and promoting industrial development in the poorer districts.
Keywords: caste in Pakistan, maternal health services, inequities, structural determinants of inequities, Pakistan, caste and Islam
Résumé
L’incapacité à réduire les taux de mortalité maternelle dans les pays à forte charge a entraîné des appels à une meilleure compréhension des déterminants structurels des inégalités dans l’accès aux services de santé maternelle. La caste est une identité construite socialement qui impose un handicap structurel à des groupes subordonnés. Même si les castes sont un phénomène d’Asie du Sud, leur existence comme facteur de stratification sociale structurelle est activement rejetée dans le Pakistan musulman comme un symbole régressif de l’hindouisme. Dans ce contexte inamical, la possibilité que les castes soient un facteur d’inégalités dans les soins de santé maternelle n’est pas prise en compte et elle est donc restée inexplorée au Pakistan. L’objectif de la présente étude est d’évaluer quantitativement la variation dans l’emploi des services de maternité entre différents groupes de castes au Pakistan. La recherche contribue également à l’innovation méthodologique en modélisant les relations entre les castes, les facteurs socioéconomiques de médiation et/ou de confusion et les indicateurs des services de santé maternelle. Une enquête stratifiée en grappes a sélectionné un échantillon de 1457 mères dans les districts de Jhelum et Layyah. Une analyse de régression logistique multivariables et à plusieurs niveaux (ajustée selon les facteurs confondants) a montré que les mères de « basses » castes avaient de plus fortes probabilités de ne pas posséder de terres, de ne pas être instruites, d’occuper des postes non qualifiés, d’être pauvres, de ne pas bénéficier de soins prénatals et d’accoucher à domicile avec l’aide d’une accoucheuse non qualifiée que les femmes de castes « élevées » ou « moyennes ». En dépit du rôle important de la caste dans la structuration du handicap socioéconomique, son effet causal indirect sur les soins de santé maternelle était véhiculé en prédominance par l’instruction de la mère et les biens du ménage. Nos conclusions suggèrent la nécessité de politiques spécifiques pour les différents groupes, y compris la construction d’écoles dans les zones d’établissement où dominent les bases castes, des mesures palliatives avec des quotas de postes de travail réservés aux groupes défavorisés, la redistribution des terres agricoles et la promotion du développement industriel dans les districts les plus démunis.
Resumen
En respuesta al incumplimiento de reducir las tasas de mortalidad materna en países con altas tasas, se les ha instado a adquirir mayor comprensión de los determinantes estructurales de las desigualdades en el acceso a los servicios de salud materna. Casta es una identidad construida por la sociedad que impone una desventaja estructural en grupos subordinados. A pesar de ser constructo de Asia meridional, la existencia de casta como estratificador social estructural es rechazada activamente por la población musulmana de Pakistán como símbolo retrógrado del hinduismo. En este contexto hostil, no se reconoce la posibilidad de casta como impulsor de las desigualdades en salud materna, por lo cual continúa sin explorarse en Pakistán. El objetivo del presente estudio es evaluar cuantitativamente la variación en el uso de servicios de maternidad en diferentes grupos de castas en Pakistán. Además, la investigación contribuye a la innovación metodológica en modelar relaciones entre castas, factores socioeconómicos de mediación y/o confusión e indicadores de servicios de salud materna. Una encuesta estratificada por conglomerados muestreó a 1457 madres en los distritos de Jhelum y Layyah. El análisis de regresión logística multivariable y multinivel (ajustado por factores de confusión) mostró que las madres de castas “Bajas” tenían mayor probabilidad de carecer de tierras, carecer de formación, trabajar en ocupaciones sin calificación, sufrir pobreza de bienes, no recibir atención prenatal y tener partos domiciliarios con asistentes no calificados, en comparación con las madres de castas “Altas”/“Medias”. A pesar de la importante función de la casta en establecer el patrón de la desventaja socioeconómica, su efecto causal indirecto en los servicios de salud materna fue mediado predominantemente por la formación y los bienes domésticos de las madres. Nuestros hallazgos indican la necesidad de formular políticas específicas para cada grupo, tales como construir escuelas en asentamientos donde dominen las castas bajas, acción afirmativa con cuotas de trabajo, redistribución de tierras agrícolas y promoción del desarrollo industrial en los distritos más pobres.
Introduction
It is increasingly acknowledged that inequities in health are products of embedded societal structures.1 Processes of exclusion and exploitation of particular sub-groups result in an inequitable distribution of the social determinants of health, such as education and income/wealth, thereby establishing numerous barriers to the fulfilment of marginalised groups’ basic right to health. The Sustainable Development Goal 10 and the WHO Commission on the Social Determinants of Health have given a powerful impetus to research and action on these structures and processes.2,3
The failure of 69 out of the 75 high-burden countries to achieve their Millennium Development Goal’s maternal health targets is increasingly being analysed in terms of inequities.4 In particular, there have been calls for a greater understanding of the patterns and processes of inequity in access to maternal health services within countries.5 Traditionally, inequities have been described in terms of individual socio-economic factors, such as women’s and men’s education and occupation, income/wealth, rural/urban residence and measures of women’s experiences of gendered inequality.6 The WHO Social Determinants of Health Framework, however, suggests there is a need to go beyond single variable analyses to illuminate the inter-relationships between individual-level and structural determinants of inequities and how they mutually reinforce each other to perpetuate poor outcomes for marginalised sub-groups.3 This approach argues that the marginalised sub-groups are “structurally vulnerable”, for not only do they experience multi-dimensional poverty, but their ability to overcome it is limited by larger social, cultural and market-related economic forces that discriminate against them.7 These disadvantages are sustained by social hierarchies, cultural norms and practices, which disparage, stereotype and exclude certain social groups, denying them full personhood. Importantly, these collective understandings are accompanied by a material reality in which the dominant groups have a proprietary claim, and in some cases exclusive rights, to participate in the economic, social and political lives of their society.7 Fear that the subordinate group might contest the dominant group’s privileges further feeds the antipathy.8
Caste is one such socially constructed identity that imposes structural disadvantages on those at the bottom of the hierarchy. A hereditary, immutable, multi-dimensional construct, the Indian caste system is the best known, although other cultures, including Yemenis, Japanese and Koreans, have similar structures.9–11 A common attribute of the caste system is the existence of the “low-caste” group. All classified in this way, whether they be Dalit in India, Burakumin in Japan or Baekjeong in Korea, experience chronic intergenerational poverty, barriers in access to resources and opportunities, habitation of physically deprived spaces and systematic exclusion from economic and political processes.12 Evidence from India and Nepal indicates caste is a determinant of overall health status 13,14 and use of health services, including maternal health care.15 Low-caste women in India have lower uptake of antenatal care (ANC), skilled birth attendance and facility deliveries.15,16
Caste in Pakistan
The Indian caste system is an integral and openly acknowledged element of Hinduism.17 Islam, in contrast, represents itself as an egalitarian religion which does not advocate for any form of stratification. However, academic analyses of the social stratification of Muslim communities in the Indian sub-continent show that the adoption of Islam did not transform the deeply embedded, caste-based social order of this society. According to Sikhand,18 the caste system has continued as a fundamental component of social identity for Muslims in South Asia for the converts “remained within a predominantly Hindu cultural universe and retained many of its associated beliefs and practices”.18
Nonetheless, following the partition of the sub-continent in 1947, discussion of caste virtually disappeared from academic and policy discourse in Pakistan.19 Interest in the study of caste has revived recently in response to a need to understand poverty and social exclusion in ostensibly ethnically homogenous villages.20–22 These researchers describe caste in Pakistan as the elephant in the room, “everyone knows it’s there, but no one wants to talk about it”.23 There is little tolerance of discussing caste and caste-based oppression and social hierarchies in the public domain in the country.23,24 Attempts to highlight the existence of the caste system or its role in the creation of structural inequities are silenced by comments that “we are Muslims” and that such conversations besmirch the image of Islam and Pakistan.24
In such an inimical context, the role of caste in creating and perpetuating maternal health inequities in Pakistan has not been considered a relevant dimension worth studying.20,24 Only recently has a small body of mostly ethnographic research started to document the lived realities of low-caste women in rural Pakistan and to trace the effects of their social and economic marginalisation on maternal health service use and outcomes.19,25,26 This literature shows that not only is the caste system prevalent, it continues to underpin the contemporary societal structure in Pakistan.20 Known as zaat or qaum, the Pakistani caste structure is, as in the rest of South Asia, based on hereditary occupational and social hierarchies. It is “historically arrived at, sociologically presented and discursively constituted”.27 Caste categories are also, according to Hussein,5 emically instituted and depend on the local social, religious, economic and political context. A graded hierarchy is the bedrock of the caste system in Pakistan with the lower castes accepting their position and revering the higher castes.20,26 Sanctified caste endogamy ensures caste purity.28 A village ethnography in district Chakwal, for example, demonstrated the existence of five main castes or zaats that were emically understood on a graded hierarchy that loosely followed the four Hindu Vernas (classes of people): the Chaudhry’s and Raja’s at the top, followed by Mirza’s and Miannei as “Middling” castes and the Kammi’s at the bottom.26 Each caste was further sub-divided into finely graded sub-castes. The low-caste Kammi included the sub-castes tharkan (iron-mongers), mochis (shoemakers) and kasai (butchers) amongst others. The subcaste tharkan were located higher on the hierarchy, while the Mussalis, who were designated to perform the most menial tasks, held a social status similar to the Dalits (untouchables). Caste boundaries in this village were largely rigid and caste identities resilient despite some individual aspirations and attempts to change their labelling and names when they moved away from villages to anonymous urban spaces.26,27 Despite this potential flexibility, the wider social structures ensured that low-caste members did not rise to higher positions in the hierarchy. Even in cases where low-caste individuals managed to change their occupations, it did not lead to a change in social status, with such individuals continuing to experience discrimination and exclusion.20,29
The occupational and social hierarchies mirror and reinforce economic hierarchies. The lowest caste groups, the Kammis, in Pakistan remain largely landless, are systematically denied access to education, remain confined to occupations characterised by poor remuneration and are often dependent upon informal entitlements.30 The land-owning, higher castes in Pakistan continue to draw upon societal beliefs regarding the inferiority of lower castes to disparage and demean them. Hussain,20 Mumtaz et al.29 and Aziz et al.31 also map how the ultra-poor, socially excluded low-caste women are invisible to programme developers and implementers and health care providers and how they are overlooked in the design and delivery of community health programmes. Community engagement activities of the government’s maternal and child health program, including the much-touted women’s groups, are structured in ways that systemically exclude low-caste women.31 Even where maternal health facilities are available, low-caste women avoid seeking care for fear of poor treatment by health care providers.26
Acknowledging that the caste system exists and forms a core part of structural differences and disadvantages within Pakistani society is a vital first step for any policy action aimed at ensuring equity in access to maternal health care and outcomes. Notwithstanding a school of thought that policies applicable to all poor people are good enough to address issues of inequity,32 evidence suggests that supplementing general policies with group-specific policies ensures a more fair and non-discriminatory support for those groups that suffer prejudice.33 A first step, therefore, is to gather evidence of how the caste system might determine access to maternal health care in Pakistan. While there is some ethnographic evidence documenting caste as a structural driver of poor women's limited access to maternal health services, there is, to our knowledge, no quantitative documentation of the relationship between caste and use of maternal health services.26 Given policymakers’ partiality to quantitative data, the present study aims to quantitatively assess variation in the use of ANC, skilled birth attendants, facility/home delivery and costs of such care across different caste groups in Muslim Pakistan.
This paper also contributes to the existing literature on how to appropriately model the relationships between caste and maternal health outcomes. Assessing the role of caste is complex for it encompasses material interests as well as the intangible, psychic elements of status. Moreover, both forces operate at the individual and group level.8 A large body of literature, mostly from India, documents how caste membership determines access to educational opportunities, type of employment, income/wealth and political capital, with low castes experiencing the least access. Similarly, a voluminous body of research has documented the association between education, employment and income/wealth with maternal health service use. However, despite these two bodies of evidence, most studies exploring the role of caste have simply added the variable as one additional socio-demographic characteristic in the models. In other words, the literature has failed to explore whether caste acts as a proximate determinant of variable access to maternal health care that mediates via differential access to education, employment and income/wealth or directly impacts via discrimination of a group, or both. The present research explores this question in Pakistan.
Methods
Study context
Two districts in Punjab which displayed ostensibly contrasting levels of socio-economic status and health service provision were selected. The first, Jhelum, is a relatively well-developed district while the second, Layyah, is one of the least developed in Punjab. Agriculture and livestock rearing are the principal economic activities in both districts. However, rain-dependent agricultural practices in Jhelum are likely to limit the capacity of agriculture to sustain livelihoods, while an established aqueduct irrigation system in Layyah means that agriculture alone is generally sufficient to support the communities living there (the majority of whom are refugees from India and from recent natural disasters). Livelihoods in both districts are also supported by remittances from male migrants working in urban areas of Pakistan and overseas. These remittances and the accompanying exposure to urban lifestyles have helped to promote development in a number of sectors, including health and education.34 Both districts have the standard government health facilities including a district hospital and one basic health unit in each union council, the smallest administrative unit. There are 107 facilities for 1.82 million population in Layyah and 88 facilities for 1.2 million population in Jhelum.35 Both districts also have a large, but undocumented private health care sector.
Sampling
To ensure that the present study collected sufficient data to generate reliable and precise estimates of caste-related variation in maternal health service use, the target sample size was based on findings from the most recent Demographic and Health Survey.36 This survey provided data for the province of Punjab on: the coverage of ANC (61.0%); the percentage of births occurring in healthcare facilities (34.5%) and the percentage of births attended by a qualified physician (31.2%). Using these data, it was calculated that in order to detect a 10% difference in all three of these indicators of maternal health care uptake (at 90% power and with α = 0.05), the present study would require a sample size of between n = 988 (i.e. for a 10% disparity in ANC coverage; from 56.0% to 66.0%) and n = 890 (i.e. for a 10% disparity in physician-attended births; from 26.2% to 36.2%).
A stratified random sampling frame was developed to recruit women from each of the two districts (Jhelum and Layyah) who had given birth in the two years preceding the study. This sampling frame drew on lists of all births compiled by “Lady Health Workers” (LHWs), a cadre of community health workers who provide door-to-door primary health care services throughout Pakistan.37 We aimed to generate a representative sample comprising equal numbers of households with “High”/“Middling” and “Low” caste mothers to ensure sufficient numbers of respondents from both castes (and particularly those from “Low” castes, since socially disadvantaged groups are routinely under-represented in health research).38 Random sampling was undertaken with stratification at five different levels: district, tehsil, union council (the second lowest and lowest tier of local government respectively); village and household. This involved randomly selecting: six of the seven tehsils (i.e. three of the four tehsils in Jhelum; and all three tehsils in Layyah); five of the union councils within each tehsil (from a total of 97 union councils); two villages within each union council; and 22 households (11 with “High”/“Middling” caste mothers; and 11 with “Low” caste mothers) within each village. LHWs familiar with these villages assisted the research team to identify each of the households selected from their lists. LHWs also introduced trained fieldworkers to the women concerned – a step considered necessary and appropriate given the context of insecurity that characterises contemporary Pakistan.39 An introduction by the LHW reassured women of the research team’s identity and ensured that women felt safe to share personal information with the team’s fieldworkers.
Given the focus of the present study on the role of caste in access, uptake and expenditure on maternal health services, it was critical to generate an early assessment of caste identity during the sampling phase. For this reason, and because data on caste are not currently routinely collected in Pakistan, we started by requesting the LHWs to label each mother’s caste. LHWs were well-placed to make such assessments since they are members of their local communities where an individual’s caste membership, based on ancestry, is common knowledge. The villagers are often also members of their biradaris, a kinship unit consisting of an endogamous group of households related by blood. They are neighbours who have shared common space over generations. Moreover, each LHW is responsible for only about 150 households situated within a one-hour walking distance. She, therefore, often has first-hand, deep knowledge of the socio-demographic characteristics of her target population. The researchers used the LHWs identification of mother’s caste to categorise them into “High”, “Middling” or “Low” based on a glossary of castes in Punjab40 (see Table 1). We used Rose’s glossary to categorise potential respondents’ caste since this digital source is, to the best of our knowledge, the most comprehensive ethnological study of the castes in the present-day Pakistani Punjab. In this way, in those instances where stratified random sampling generated insufficient numbers of households (i.e. <n = 11) with “High”/“Middling” and/or “Low” caste mothers eligible for inclusion in the study, additional households from a neighbouring village within the same union council were included in that sample. For the most part, this involved additional effort to include “Low” caste respondents, since this population was numerically small in most villages.31
Table 1.
Hierarchical classification of castes in Pakistan (after Rose, 1911)40
| Level of hierarchy | Castes included |
|---|---|
| Level 1 – “High” castes | Jatt; Rajput; Mughal; Arain; Baloch; Butt; Mirza; and Oray |
| Level 2 – “Middling” castes | Awan; Qureshi; Gujjar; Sheikh; and Dund |
| Level 3 – “Low’”castes | Kammi (including the following sub-castes: Mistri; Mussali; Marasi; Nai; Mochi; Kumhar; Lohar; Tarkhan; and Bazigar) |
Data collection
A bespoke questionnaire was developed to collect additional self-reported data from study participants. The tool was piloted initially with 20 women, leading to the revision and restructuring of some questions. The revised draft was then again piloted with a smaller sample to test the restructured questions and develop the final version. In addition to caste, the principal exposure of interest, the questionnaire collected data on each of the four outcomes of maternal health care: uptake of ANC; place of birth; type of birth attendant; and expenditure on the birth. Additional items in the questionnaire sought information on individual- and household-level demographic and economic variables considered likely to play important roles as mediators in any causal relationship between caste and each of the maternal healthcare outcomes of interest. These included individual-level data on each mother's age; the educational attainment and current employment status of each mother and her husband; and the number of children in the household who were under the age of 14 years and currently employed. Household-level data were generated from items on the ownership of agricultural land; household assets (comprising separate items on housing tenure; dwelling construction; source[s] of water; access to electricity; type[s] of fuel used for cooking; and ownership of livestock, a television, a motor vehicle and/or a telephone); and money set aside in case of emergency during delivery. All the questions were based on validated Demographic Health Survey questions and those used by the Pakistan Poverty Scorecard.41 The latter scale’s scoring technique was adapted to generate a “Household Assets Index” capable of distinguishing between the better- and worse-off households included in the present study. Self-reported caste was classified into “High”, “Middling” and “Low” (using Rose’s40 glossary) because graded inequality is the bedrock of the caste system. It also reflects the hierarchy of the castes as understood by our respondents in an earlier village ethnography that framed the quantitative study26 (see online supplementary materials). Following informed consent, the data were collected from October 2012 to June 2013.
Statistical analyses
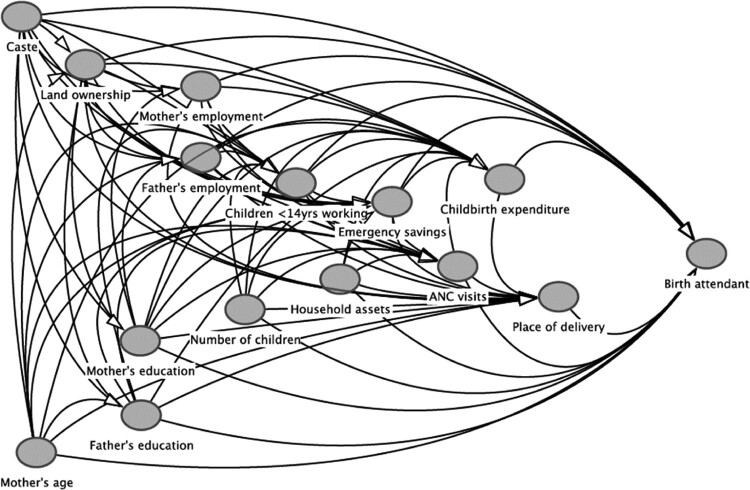
Data analysis was informed by a causal path diagram generated in the form of a Directed Acyclic Graph (DAG; see Figure 1), interpreted using the freeware program DAGitty.42,43 Based on in-depth, context-specific knowledge, this diagram constitutes a non-parametric, theoretical representation of the temporal and functional relationships between each of the variables collected in the present study. The guiding principles underpinning the construction of this diagram were that: (i) only variables that precede others can act as potential causes thereof; and (ii) preceding variables should be assumed to act as probabilistic causes of all subsequent variables unless there is definitive evidence to the contrary.44 Figure 1, therefore, provides a summary of these theoretical considerations and their relevance to the role that socio-demographic, material and structural factors might play in differential access to, uptake of, and expenditure on antenatal and maternity services amongst “High”/“Middling” and “Low” caste mothers in Jhelum and Layyah.
Figure 1.
Hypothesised relationship between socio-demographic, economic and maternal health service variables available for examination in the present study, drawn in the form of a Directed Acyclic Graph (DAG) using the freeware programme www.dagitty.net42
Univariable descriptive analyses were used to summarise the distribution of individual- and household-level socio-economic and maternal health service variables, disaggregated by district, by caste, and by caste-within-district.45 These summaries were presented as frequencies with percentages (%) in parentheses; and the statistical significance of any differences observed were assessed using Chi-squared tests. Multi-level logistic regression models were then used to assess the relationship between individual- and household-level socio-demographic and economic characteristics and each of the four maternal health care indicators, both before and after adjustment for potential confounders. The designs of these models were informed by the DAG (Figure 1), from which it was possible to identify which of the measured variables were likely to act as: potential confounders (which are preceding probabilistic causes of both the specified exposure and specified outcome, and should therefore be included in the covariate adjustment sets used to mitigate confounder bias); and potential mediators (which fall on the causal path between the specified exposure and specified outcome, and should not be included in covariate adjustment sets to avoid inferential mediator adjustment bias).46,47 The results of the logistic regression models were presented as odds ratios (OR) with 95% confidence intervals (95% CI) in parentheses.
In this way, by comparing the univariable models of caste-related variation in socio-demographic, economic and health care variables with multivariable models of (confounder-adjusted) variation in health care variables associated with each of the socio-economic variables, these analyses aimed to assess the extent to which differential access to, uptake of and expenditure on maternal health care was associated with caste (mediated by all subsequent socio-economic characteristics); and the extent to which these differences were independently associated with each of the subsequent socio-demographic and economic factors (acting as mediators between caste and maternal health care). As such, the multi-level multivariable logistic regression models were designed to evaluate the potential role of each of the measured socio-economic factors that flow from membership of “High”/“Middling” vs. “Low” castes in the (re)production of inequalities in maternal health care. All statistical analyses were conducted using STATA version 15.48
Ethical approval
Ethical approval was obtained from the University of Alberta Health Research Ethics Board (Approval number: Pro00019042, dated April 8, 2011), and from the National Bioethics Committee in Pakistan (Approval number: 4-87/11/NBC/RDC/32/7, dated January 26, 2011).
Results
Sample size and response rate
The study recruited a total of 1457 mothers from 747 households in Jhelum and 710 in Layyah – a sample that exceeded the n = 890–988 that had been calculated as necessary to detect a 10% difference in the three key indicators of maternal health service use (i.e. ANC; births occurring in healthcare facilities; and those attended by a qualified physician) with 90% power and α = 0.05.36 The vast majority of households recruited into the present study (702/747 – 94.0% in Jhelum and 683/710 – 96.2% in Layyah) provided complete data for all of the items included in the study’s questionnaire – an overall response rate of 95.1% that was very similar in each of the two districts examined (χ2 = 0.79; d.f. = 1; p = 0.37); and is unlikely to pose a substantial risk of endogenous/collider selection bias in the analyses that follow.49
Overall, 49% of respondents self-identified as members of “High”/“Middling” castes and 51% as members of “Low” castes (see Table 2), a distribution that reflects our sampling strategy. Seventy percent of respondents reported having received no education or only a primary or less; 90% classified themselves as homemakers (as opposed to professional, skilled or unskilled workers); and 56% lived in households that did not own agricultural land. While ANC use was common, with 95% reporting at least one visit, nearly half (45.5%) had delivered their last child at home, and over a third of all deliveries (34.5%) had been attended by an unskilled birth attendant (known locally as a Dai) (see Table 2).
Table 2.
The distribution of caste, age and socio-economic characteristics; and of maternal health care indicators amongst the 1385 households providing complete data on all variables, before and after disaggregation by district
| All respondents n = 1385 n (%) |
Comparison by district | |||
|---|---|---|---|---|
| Variables | Jhelum n = 702 n (%) |
Layyah n = 683 n (%) |
p | |
| Caste | 0.889 | |||
| High/Middling | 699 (50.5%) | 353 (50.3%) | 346 (50.7%) | |
| Low | 686 (49.5%) | 349 (49.7%) | 337 (49.3%) | |
| Mother’s age | 0.031 | |||
| 15–19 | 46 (3.3%) | 29 (4.1%) | 17 (2.5%) | |
| 20–29 | 773 (55.8%) | 404 (57.6%) | 369 (54.0%) | |
| 30–39 | 511 (36.9%) | 249 (35.5%) | 262 (38.4%) | |
| 40–49 | 55 (4.0%) | 20 (2.8%) | 35 (5.1%) | |
| Socio-economic characteristics | ||||
| Land ownership | <0.001 | |||
| None | 775 (56.0%) | 423 (60.3%) | 352 (51.5%) | |
| Agricultural land owned | 610 (44.0%) | 279 (39.7%) | 346 (48.5%) | |
| Mother’s education | <0.001 | |||
| No Education | 607 (43.8%) | 202 (28.9%) | 405 (59.3%) | |
| Primary or less | 367 (26.5%) | 214 (30.5%) | 153 (22.4%) | |
| High School or less | 335 (24.2%) | 234 (33.3%) | 101 (14.8%) | |
| More than High School | 76 (5.5%) | 52 (7.4%) | 24 (3.8%) | |
| Father’s education | <0.001 | |||
| No Education | 337 (24.3%) | 113 (16.1%) | 224 (32.8%) | |
| Primary or less | 235 (17.0%) | 93 (13.3%) | 142 (20.8%) | |
| High School or less | 665 (48.0%) | 425 (60.5%) | 240 (35.1%) | |
| More than High School | 148 (10.7%) | 71 (10.1%) | 77 (11.3%) | |
| Mother’s employment | <0.001 | |||
| Homemaker | 1219 (88.0%) | 668 (95.2%) | 551 (80.7%) | |
| Professional | 22 (1.6%) | 9 (1.3%) | 13 (1.9%) | |
| Skilled workers | 107 (7.7%) | 17 (2.4%) | 90 (13.2%) | |
| Unskilled workers | 37 (2.7%) | 8 (1.1%) | 29 (4.2%) | |
| Father’s employment | <0.001 | |||
| Professional/landowner | 335 (24.2%) | 195 (27.8%) | 140 (20.5%) | |
| Skilled worker | 431 (31.1%) | 258 (36.8%) | 173 (25.3%) | |
| Unskilled worker | 443 (32.0%) | 182 (25.9%) | 261 (38.2%) | |
| Not working/unemployed | 176 (12.7%) | 67 (9.5%) | 109 (16.0%) | |
| Number of children | <0.001 | |||
| 1–2 | 668 (48.2%) | 365 (52.0%) | 303 (44.4%) | |
| 3–4 | 475 (34.3%) | 241 (34.3%) | 234 (34.3%) | |
| 5+ | 242 (17.5%) | 96 (13.7%) | 146 (21.4%) | |
| Children <14 years working | <0.001 | |||
| None | 1329 (96.0%) | 700 (99.7%) | 629 (92.1%) | |
| ≥1 | 56 (4.0%) | 2 (0.3%) | 54 (7.9%) | |
| Household Asset Index | <0.001 | |||
| First quartile (poorest) | 479 (34.6%) | 189 (26.9%) | 290 (42.5%) | |
| Second quartile | 345 (24.9%) | 168 (23.9%) | 177 (25.9%) | |
| Third quartile | 303 (21.9%) | 184 (26.2%) | 119 (17.4%) | |
| Fourth quartile (richest) | 258 (18.6%) | 161 (22.9%) | 97 (14.2%) | |
| Emergency savings for maternal health | 0.034 | |||
| None | 547 (39.5%) | 258 (36.8%) | 289 (42.3%) | |
| Yes | 838 (60.5%) | 444 (63.2%) | 394 (57.7%) | |
| Maternal health care indicators | ||||
| Antenatal care (ANC%) | <0.001 | |||
| No ANC visits | 57 (4.1%) | 16 (2.3%) | 41 (6.0%) | |
| ≥1 ANC visit | 1328 (95.9%) | 686 (97.7%) | 642 (94.0%) | |
| Amount of money spent on last childbirth delivery | <0.001 | |||
| >PKR 3000 | 605 (43.7%) | 373 (53.1%) | 232 (34.0%) | |
| ≤PKR 3000 | 780 (56.3%) | 329 (46.9%) | 451 (66.0%) | |
| Place of delivery | <0.001 | |||
| Home | 630 (45.5%) | 226 (32.2%) | 404 (59.2%) | |
| Government healthcare facility | 273 (19.7%) | 182 (25.9%) | 91 (13.3%) | |
| Private healthcare facility | 482 (34.8%) | 294 (41.9%) | 188 (27.5%) | |
| Type of birth attendant | <0.001 | |||
| Skilled birth attendant | 907 (65.5%) | 589 (83.9%) | 318 (46.6%) | |
| Physician | 435 (31.4%) | 291 (41.5%) | 144 (21.1%) | |
| Non-Physician | 472 (34.1%) | 298 (42.4%) | 174 (25.5%) | |
| Unskilled birth attendant | ||||
| Dai | 478 (34.5%) | 113 (16.1%) | 365 (3.4%) | |
All results are presented as frequencies with percentages in parentheses (%); with p-values relating to district-wise statistical comparisons involving χ2 tests.
There was considerable variation in socio-economic and maternal health care indicators by the district. Mothers in Jhelum tended to be better educated; had better-educated husbands; had, on average, fewer children; and were less likely to be employed outside the home than those in Layyah. Moreover, a comparison of the composite Household Asset Index confirmed that only a quarter of households in Jhelum (26.9%) were in the least wealthy quartile overall compared to 42.5% of the households in Layyah. This finding is counterintuitive given that the percentage of households owning land was substantially lower in Jhelum (39.7%) than in Layyah (48.5%). The lower percentage of Jhelum’s (wealthier) households owning land than the (poorer) households in Layyah reflects the different geographies and opportunities that led to higher levels of non-agriculture economic development in Jhelum described above.
Despite the individual- and household-level disparities in education, employment and wealth between Jhelum and Layyah, there were only modest differences in the percentage of mothers who had received at least one ANC visit during their most recent pregnancy. It is possible that disparities in the total number of ANC visits might have been revealed had this information been collected. There were nevertheless substantial district-related disparities in the proportion of women who had given birth at a (government or private) healthcare facility attended by a skilled birth attendant, and related disparities in delivery-related expenditure (see Table 2). Most of the mothers in Jhelum had given birth to their most recent child in a government or private healthcare facility (67.8%), with a skilled birth attendant (83.9%) at a cost that was greater than PKR 3000 (53.1%). In contrast, over half of the mothers in Layyah had given birth to their most recent child at home (59.2%), with an unskilled birth attendant/Dai (53.4%), at a cost of less than PKR 3000 (see Table 2).
Caste-related variation in socio-economic and maternal health care indicators
In Table 3, we explore the relationships between caste and each of the individual- and household-level socio-economic and maternal health care indicators separately within each district and across both districts sampled. These comparisons show that all but two of the socio-economic and maternal health care variables displayed consistent differences between “High”/“Middling” and “Low” caste, with “Low” caste mothers displaying less favourable indicators than those who self-reported as “High”/“Middling” caste. In both districts, “Low” caste mothers were less likely to report having received an education and were less likely to report that their husbands had received an education. They were also less likely to live in households that owned land and were more likely to be asset-poor as measured by the Household Asset Index. These trends in structural inequality were also evident in access to, uptake of and expenditure on maternal healthcare services. “Low” caste mothers were far less likely than “High”/“Middling” caste mothers to have given birth to their last child in a government or private healthcare facility, with a skilled birth attendant, at a cost of more than PKR 3000. These patterns also varied between the two districts examined in the present study. On the whole, access to, uptake of and expenditure on maternal care services were lower in Layyah than in Jhelum (the more socio-economically developed of the two districts) amongst both “Low” and “High”/“Middling” caste respondents (see Table 3).
Table 3.
The distribution of age and socio-economic characteristics; and of maternal health care indicators, disaggregated by caste across all respondents and within each district separately
| Comparison by caste | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All respondents n = 1385 |
Jhelum district n = 702 |
Layyah district n = 683 |
|||||||
| Variables | High/Middling n = 699 n (%) |
Low n = 686 n (%) |
p | High/Middling n = 353 n (%) |
Low n = 349 n (%) |
p | High/Middling n = 346 n (%) |
Low n = 337 n (%) |
p |
| Mother’s age | 0.123 | 0.206 | 0.157 | ||||||
| 15–19 | 17 (2.4) | 29 (4.2) | 12 (3.4) | 17 (4.9) | 5 (1.4) | 12 (3.6) | |||
| 20–29 | 387 (55.4) | 386 (56.3) | 193 (54.7) | 211 (60.5) | 194 (56.1) | 175 (51.9) | |||
| 30–39 | 271 (38.8) | 240 (35.0) | 138 (39.1) | 111 (31.8) | 133 (38.4) | 129 (38.3) | |||
| 40–49 | 24 (3.4) | 31 (4.5) | 10 (2.8) | 10 (2.9) | 14 (4.1) | 21 (6.2) | |||
| Socio-economic characteristics | |||||||||
| Land ownership | <0.001 | <0.001 | <0.001 | ||||||
| None | 231 (33.0) | 544 (79.3) | 111 (31.4) | 312 (89.4) | 120 (34.7) | 232 (68.8) | |||
| Agricultural land owned | 468 (67.0) | 142 (20.7) | 242 (68.6) | 37 (10.6) | 226 (65.3) | 105 (31.2) | |||
| Mother’s education | <0.001 | <0.001 | <0.001 | ||||||
| No Education | 228 (32.6) | 379 (55.2) | 69 (19.5) | 133 (38.1) | 159 (45.9) | 246 (73.0) | |||
| Primary or less | 191 (27.3) | 176 (25.7) | 105 (29.8) | 109 (31.2) | 86 (24.9) | 67 (19.9) | |||
| High School or less | 222 (31.8) | 113 (16.5) | 143 (40.5) | 91 (26.1) | 79 (22.8) | 22 (6.5) | |||
| More than High School | 58 (8.3) | 18 (2.6) | 36 (10.2) | 16 (4.6) | 22 (6.4) | 2 (0.6) | |||
| Father’s education | <0.001 | <0.001 | <0.001 | ||||||
| No Education | 116 (16.6) | 221 (32.2) | 42 (11.9) | 71 (20.3) | 74 (21.4) | 150 (44.5) | |||
| Primary or less | 92 (13.2) | 143 (20.9) | 33 (9.4) | 60 (17.2) | 59 (17.0) | 83 (24.6) | |||
| High School or less | 374 (53.5) | 291 (42.4) | 225 (63.7) | 200 (57.3) | 149 (43.1) | 91 (27.0) | |||
| More than High School | 117 (16.7) | 31 (4.5) | 53 (15.0) | 18 (5.2) | 64 (18.5) | 13 (3.9) | |||
| Mother’s employment | <0.001 | 0.014 | <0.001 | ||||||
| Housewife | 637 (91.1) | 582 (84.8) | 342 (96.9) | 326 (93.4) | 295 (85.3) | 256 (76.0) | |||
| Professional | 16 (2.3) | 6 (0.9) | 6 (1.7) | 3 (0.9) | 10 (2.9) | 3 (0.9) | |||
| Skilled workers | 38 (5.4) | 69 (10.1) | 4 (1.1) | 13 (3.7) | 34 (9.8) | 56 (16.6) | |||
| Unskilled workers | 8 (1.1) | 29 (4.2) | 1 (0.3) | 7 (2.0) | 7 (2.0) | 22 (6.5) | |||
| Father’s employment | <0.001 | <0.001 | <0.001 | ||||||
| Professional/landowner | 233 (33.3) | 102 (14.9) | 131 (37.1) | 64 (18.3) | 102 (29.5) | 38 (11.3) | |||
| Skilled worker | 196 (28.0) | 235 (34.3) | 120 (34.0) | 138 (39.5) | 76 (22.0) | 97 (28.8) | |||
| Unskilled worker | 131 (18.7) | 312 (45.5) | 48 (13.6) | 134 (38.4) | 83 (24.0) | 178 (52.8) | |||
| Not working/unemployed | 139 (19.9) | 37 (5.4) | 54 (15.3) | 13 (3.7) | 85 (24.6) | 24 (7.1) | |||
| Number of children | 0.283 | 0.280 | 0.027 | ||||||
| 1–2 | 351 (50.2) | 317 (46.2) | 186 (52.7) | 179 (51.3) | 165 (47.7) | 138 (41.0) | |||
| 3–4 | 234 (33.5) | 241 (35.1) | 113 (32.0) | 128 (36.7) | 121 (35.0) | 113 (33.5) | |||
| 5+ | 114 (16.3) | 128 (18.7) | 54 (15.3) | 42 (12.0) | 60 (17.3) | 86 (25.5) | |||
| Children <14yrs working | 0.002 | 0.154 | 0.003 | ||||||
| None | 682 (97.6) | 647 (94.3) | 353 (100) | 347 (99.4) | 329 (95.1) | 300 (89.0) | |||
| ≥1 | 17 (2.4) | 39 (5.7) | – | 2 (0.6) | 17 (4.9) | 37 (11.0) | |||
| Household Asset Index | <0.001 | <0.001 | <0.001 | ||||||
| First quartile (poorest) | 116 (16.6) | 363 (52.9) | 34 (9.6) | 155 (44.4) | 82 (23.7) | 208 (61.7) | |||
| Second quartile | 177 (25.3) | 168 (24.5) | 86 (24.4) | 82 (23.5) | 91 (26.3) | 86 (25.5) | |||
| Third quartile | 185 (26.5) | 118 (17.2) | 104 (29.5) | 80 (22.9) | 81 (23.4) | 38 (11.3) | |||
| Fourth quartile (richest) | 221 (31.6) | 37 (5.4) | 129 (36.5) | 32 (9.2) | 92 (26.6) | 5 (1.5) | |||
| Emergency savings for maternal health | <0.001 | <0.001 | 0.107 | ||||||
| None | 235 (33.6) | 312 (45.5) | 99 (28.0) | 159 (45.6) | 136 (39.3) | 153 (45.4) | |||
| Yes | 464 (66.4) | 374 (54.5) | 254 (72.0) | 190 (54.4) | 210 (60.7) | 184 (54.6) | |||
| Maternal health care indicators | |||||||||
| Antenatal care (ANC) | <0.001 | 0.301 | 0.007 | ||||||
| No ANC visits | 17 (2.4) | 40 (5.8) | 6 (1.7) | 10 (2.9) | 11 (3.2) | 30 (8.9) | |||
| ≥1 ANC visit | 682 (97.6) | 646 (94.2) | 347 (98.3) | 339 (97.1) | 335 (96.8) | 307 (91.1) | |||
| Amount of money spent on last childbirth delivery | <0.001 | <0.001 | <0.001 | ||||||
| >PKR 3000 | 379 (54.2) | 226 (32.9) | 226 (64.0) | 147 (42.1) | 153 (44.2) | 79 (23.4) | |||
| ≤PKR 3000 | 320 (45.8) | 460 (67.1) | 127 (36.0) | 202 (57.9) | 193 (55.8) | 258 (76.6) | |||
| Place of delivery | <0.001 | <0.001 | <0.001 | ||||||
| Home | 262 (41.6) | 368 (53.6) | 92 (26.1) | 134 (38.4) | 170 (49.1) | 234 (69.4) | |||
| Government healthcare facility | 146 (20.9) | 127 (18.5) | 88 (24.9) | 94 (26.9) | 58 (16.8) | 33 (9.8) | |||
| Private healthcare facility | 291 (41.6) | 191 (27.8) | 173 (49.0) | 121 (34.7) | 118 (34.1) | 70 (20.8) | |||
| Type of birth attendant | <0.001 | <0.001 | <0.001 | ||||||
| Skilled birth attendant | 515 (73.4) | 392 (57.1) | 319 (90.4) | 270 (77.4) | 196 (56.6) | 122 (36.2) | |||
| Physician | 285 (40.8) | 150 (21.9) | 188 (53.3) | 103 (29.5) | 97 (28.0) | 47 (13.9) | |||
| Non-Physician | 230 (32.9) | 242 (35.3) | 131 (37.1) | 167 (47.9) | 99 (28.6) | 75 (22.3) | |||
| Unskilled birth attendant | |||||||||
| Dai | 184 (26.3) | 294 (42.9) | 34 (9.6) | 79 (22.6) | 150 (43.4) | 215 (63.8) | |||
All results are presented as frequencies with percentages in parentheses (%); with p-values relating to caste-wise statistical comparisons involving χ2 tests.
Direct and indirect effects of caste on maternal health care indicators
The above patterns of caste-related variation were also evident in the multi-level, unadjusted logistic regression analyses presented in Table 4. Interpreting these estimates as the total causal effect of caste on each of the socio-economic characteristics and maternal health care indicators examined (as theorised in Figure 1), it is clear that “Low” caste was strongly associated with many of the least favourable socio-economic characteristics, displaying a higher odds of mothers and fathers who were: uneducated (mothers – OR: 7.53; 95% CI: 3.91, 14.53; fathers – OR: 10.9; 95% CI: 5.99, 19.7); unskilled workers (mothers – OR: 3.63; 95%CI: 1.55, 8.50; fathers – OR: 6.61; 95% CI 4.63, 9.45); categorised in the poorest quartile for household assets (OR: 76.4; 95% CI: 36.5, 160.8); and possessed neither agricultural land (OR: 9.55; 95% CI:7.26, 12.57) nor emergency health savings (OR:1.66; 95% CI:1.32, 2.08) when compared to “High”/“Middling” caste. These patterns are replicated in maternal health care use. “Low” caste respondents had 2–2½ times the odds of: no ANC visits (OR: 2.78; 95%CI: 1.48, 5.22); a home-based birth (OR: 2.32; 95% CI:1.76, 3.07) with an unskilled attendant (OR: 3.76; 95% CI:2.68, 5.28), spending less than PKR3000 on their most recent birth (OR: 2.6; 95% CI:2.11, 3.37) when compared to “High”/“Middling” caste individuals.
Table 4.
Estimates of the total (probabilistic, unadjusted) effect of caste on each of the subsequent socio-demographic and economic characteristics; and maternal health care indicators, expressed as odds ratios (OR) with 95% confidence intervals (CIs) in parentheses
| Specified outcome (referent) | Caste (“High/Middling”) | Specified outcome (referent) | Caste (“High/Middling”) | Specified outcome (referent) | Caste (“High/Middling”) |
|---|---|---|---|---|---|
| “Low” OR (95%CI) | “Low” OR (95%CI) | “Low” OR (95%CI) | |||
|
Mother's age (20–29 years) |
Mother’s education (More than High School) | Father’s education (More than High School) | |||
| 15–19 years | 1.72 (0.92, 3.22) | High School or less | 1.64 (0.92, 2.92) | High School or less | 2.81 (1.80, 4.36) |
| 30–39 years | 0.89 (0.71, 1.11) | Primary or less | 3.14 (1.72, 5.71) | Primary or less | 8.29 (4.51, 15.2) |
| 40–49 years | 1.30 (0.74, 2.28) | None | 7.53 (3.91, 14.51) | None | 10.9 (5.99, 19.7) |
|
Household Asset Index (Fourth quartile - richest) |
Mother’s employment (Housewife) | Father’s employment (Professional/landowner) | |||
| Third quartile | 4.16 (2.65, 6.56) | Professional | 0.41 (0.16, 1.06) | Skilled worker | 2.75 (2.03, 3.74) |
| Second quartile | 6.99 (4.41, 11.11) | Skilled worker | 2.22 (1.41, 3.49) | Unskilled labour | 6.61 (4.63, 9.45) |
| First quintile – poorest | 76.4 (36.5, 160.8) | Unskilled worker | 3.63 (1.55, 8.50) | Not working | 0.44 (0.26, 0.74) |
| Land ownership (Agricultural land owned) | Children <14 years working (None) |
Emergency health savings (Yes) |
|||
| None | 9.55 (7.26, 12.57) | Yes | 2.53 (1.40, 4.58) | None | 1.66 (1.32, 2.08) |
|
Number of Children (1–2) |
Place of delivery (Private healthcare facility) | Type of birth attendant (Physician) | |||
| 3–4 | 1.14 (0.90, 1.44) | Govt healthcare facility | 1.35 (0.96, 1.91) | Non-physician | 2.17 (1.59, 2.95) |
| 5+ | 1.23 (0.91, 1.66) | Mother’s or Dai’s home | 2.32 (1.76, 3.07) | Dai | 3.76 (2.68, 5.28) |
|
ANC visits (≥1 ANC visit) |
Money spent on last delivery (>PKR 3000) | ||||
| No ANC visits | 2.78 (1.48, 5.22) | 0–3000 PKR | 2.66 (2.11, 3.37) |
Each estimate was generated using a separate univariable logistic regression model in which no adjustment was made for any other variable (since none of these were considered to have acted as potential confounders in any of these relationships; see Figure 1).
Table 5 presents the estimates generated by the multi-level, multivariable logistic regression models adjusted for all preceding socio-economic and maternal health care variables (which were assumed to act as potential confounders as theorised in Figure 1). These analyses show that mother’s education, father’s occupation, Household Asset Index and land ownership exhibited total, confounder-adjusted, probabilistic causal effects with one or more of the four maternal health care indicators. A key finding is the particularly strong association between mother’s education and Household Asset Index and the maternal health care indicators. Mothers with no education had 16 times the odds of reporting their last birth at home, attended by an unskilled Dai compared to mothers with more than high-school education. Mothers living in the poorest households had two to three times higher odds of reporting a home-birth, attended by an unskilled Dai and spent less than PKR 3000 compared to those living in the richest households. It is also worth noting the finding that the variable “number of children” in the household – which demonstrated no association with caste – displayed a strong association with all four maternal health care indicators, such that families with >5 children had higher odds of having no ANC visits (OR:3.36; 95% CI:1.24;9.13) and a home-birth (OR:2.38; 95% CI:1.43, 3.97) with an unskilled birth attendant (OR:2.26; 95% CI:1.19, 4.29), spending less than PKR3000 on their most recent birth (OR:2.43; 95% CI:1.59, 3.73) compared to those with one or two children.
Table 5.
Estimates of the total (confounder-adjusted, probabilistic) effect of each of the sociodemographic and economic characteristics on subsequent maternal health care indicators, expressed as odds ratios (OR) with 95% confidence intervals (CIs) in parentheses
| Specified outcome (referent) | |||||||
|---|---|---|---|---|---|---|---|
| ANC visits (≥1 ANC visit) | Birth cost for last childbirth delivery (>PKR 3000) | Place of delivery (Private healthcare facility) | Type of birth attendant (Physician) | ||||
| Specified exposure (referent) | No ANC visits OR (95%CI) | 0–3000 PKR OR (95%CI) |
Government healthcare facility OR (95%CI) |
Mother’s home or Dai’s home OR (95%CI) |
Non-physician skilled attendant OR (95%CI) |
Dai OR (95%CI) |
|
| Model 1 |
Caste (“High/Middling”) |
||||||
| “Low” | 2.78 (1.48, 5.22) | 2.67 (2.11, 3.37) | 1.35 (0.96, 1.91) | 2.32 (1.76, 3.07) | 2.17 (1.59, 2.95) | 3.76 (2.68, 5.28) | |
| Model 2 |
Mother's age (20–29 years) |
||||||
| 15–19 years | 0.53 (0.06, 4.59) | 1.54 (0.79, 3.01) | 2.13 (0.85, 5.35) | 1.26 (0.54, 2.95) | 1.57 (0.71, 3.44) | 0.49 (0.18, 1.36) | |
| 30–39 years | 1.70 (0.93, 3.11) | 1.22 (0.95, 1.56) | 0.78 (0.55, 1.12) | 1.17 (0.87, 1.57) | 0.94 (0.69, 1.30) | 1.29 (0.91, 1.84) | |
| 40–49 years | 1.82 (0.60, 5.52) | 1.74 (0.91, 3.33) | 0.73 (0.27, 2.00) | 1.17 (0.57, 2.39) | 1.25 (0.54, 2.93) | 1.17 (0.50, 2.76) | |
| Model 3 | Land ownership (Agricultural land owned) | ||||||
| None | 0.66 (0.33, 1.31) | 1.32 (1.01, 1.74) | 1.28 (0.85, 1.92) | 1.00 (0.72, 1.39) | 1.19 (0.83, 1.70) | 1.09 (0.74, 1.61) | |
| Model 4 | Mother’s education (More than High School) | ||||||
| High School or less | Small n | 3.50 (1.77, 6.93) | 1.00 (0.53, 1.90) | 4.44 (1.66, 11.9) | 2.18 (1.12, 4.23) | 4.03 (1.25, 13.0) | |
| Primary or less | 4.98 (2.49, 9.98) | 1.10 (0.56, 2.19) | 10.0 (3.69, 27.1) | 3.72 (1.86, 7.47) | 11.5 (3.69, 37.2) | ||
| None | 7.94 (3.92, 16.1) | 1.06 (0.52, 2.17) | 16.0 (5.87, 43.8) | 4.62 (2.25, 9.50) | 16.3 (5.04, 52.9) | ||
| Model 5 | Father’s education (More than High School) | ||||||
| High School or less | 0.26 (0.08, 0.89) | 1.01 (0.66, 1.55) | 1.21 (0.70, 2.11) | 1.01 (0.60, 1.72) | 1.04 (0.62, 1.73) | 1.22 (0.66, 2.26) | |
| Primary or less | 0.27 (0.07, 1.06) | 1.59 (0.96, 2.65) | 1.21 (0.60, 2.44) | 1.32 (0.71, 2.43) | 1.49 (0.79, 2.82) | 1.60 (0.78, 3.26) | |
| None | 0.54 (0.16, 1.82) | 1.17 (0.71, 1.93) | 0.81 (0.40, 1.65) | 1.08 (0.59, 1.95) | 1.09 (0.58, 2.07) | 1.52 (0.76, 3.04) | |
| Model 6 | Mother’s employment (Housewife) | ||||||
| Professional | n = 0 | 1.42 (0.50, 4.04) | 0.69 (0.21, 2.35) | 0.90 (0.44, 3.28) | 1.81 (0.57, 5.83) | 2.99 (0.49, 18.1) | |
| Skilled worker | 1.21 (0.44, 3.32) | 1.50 (0.91, 2.48) | 1.53 (0.72, 3.28) | 1.44 (0.81, 2.60) | 0.69 (0.33, 1.42) | 1.01 (0.54, 1.88) | |
| Unskilled worker | 0.19 (0.02, 1.66) | 1.24 (0.53, 2.90) | 1.08 (0.27, 4.36) | 0.90 (0.36, 2.27) | 1.25 (0.31, 5.02) | 2.01 (0.57, 7.04) | |
| Model 7 | Father’s employment (Professional/landowner) | ||||||
| Skilled worker | 0.75 (0.24, 2.36) | 1.12 (0.79, 1.58) | 0.67 (0.42, 1.07) | 1.58 (1.02, 2.43) | 1.11 (0.73, 1.67) | 1.83 (1.09, 3.12) | |
| Unskilled labour | 1.47 (0.51, 4.22) | 1.19 (0.82, 1.74) | 0.68 (0.40, 1.15) | 1.48 (0.93, 2.34) | 0.78 (0.49, 1.27) | 1.49 (0.86, 2.57) | |
| Not working | 1.49 (0.47, 4.74) | 0.98 (0.63, 1.52) | 0.80 (0.43, 1.50) | 1.20 (0.70, 2.06) | 1.02 (0.59, 1.78) | 1.16 (0.62, 2.17) | |
| Model 8 |
Number of Children (1–2) |
||||||
| 3–4 | 3.02 (1.34, 6.83) | 1.53 (1.15, 2.05) | 1.31 (0.88, 1.97) | 1.50 (1.06, 2.12) | 1.72 (1.19, 2.49) | 1.46 (0.95, 2.23) | |
| 5+ | 3.36 (1.24, 9.13) | 2.43 (1.59, 3.73) | 1.93 (1.01, 3.68) | 2.38 (1.43, 3.97) | 2.06 (1.18, 3.40) | 2.26 (1.19, 4.29) | |
| Model 9 |
Children <14 years working (None) |
||||||
| Yes | 1.37 (0.42, 4.55) | 1.03 (0.51, 2.07) | 0.65 (0.19, 2.29) | 1.11 (0.51, 2.38) | 0.66 (0.20, 2.14) | 1.27 (0.52, 3.13) | |
| Model 10 | Household Asset Index (Fourth quartile – richest) | ||||||
| Third quartile | 1.14 (0.17, 7.40) | 1.32 (0.88, 1.98) | 1.53 (0.91, 2.61) | 1.59 (0.96, 2.64) | 1.48 (0.91, 2.41) | 2.20 (1.19, 4.08) | |
| Second quartile | 2.74 (0.50, 15.2) | 1.67 (1.09, 2.55) | 1.48 (0.83, 2.66) | 1.68 (0.99, 2.83) | 1.72 (1.02, 2.90) | 2.27 (1.22, 4.22) | |
| First quintile – poorest | 2.86 (0.47, 17.5) | 2.06 (1.27, 3.35) | 2.19 (1.11, 4.30) | 2.80 (1.54, 5.10) | 2.51 (1.36, 4.63) | 2.93 (1.45, 5.92) | |
| Model 11 |
Emergency savings for maternal health (Yes) |
||||||
| None | 1.92 (0.99, 3.71) | 0.84 (0.65, 1.09) | 0.72 (0.49, 1.06) | 0.79 (0.58, 1.08) | 0.92 (0.66, 1.29) | 0.80 (0.55, 1.16) | |
| Model 12 |
ANC visits (≥1 ANC visit) |
||||||
| No ANC visits | – | 2.65 (1.17, 5.98) | 2.51 (0.46, 13.8) | 5.81 (1.67, 20.2) | 4.57 (0.78, 26.7) | 7.02 (1.56, 31.6) | |
| Model 13 | Amount of money spent on last childbirth delivery (>PKR 3000) | ||||||
| 0–3000 PKR | – | – | 10.7 (6.92, 16.5) | 22.2 (14.4, 34.1) | 4.68 (3.29, 6.66) | 17.4 (10.8, 27.9) | |
| Model 14 | Place of delivery (Private healthcare facility) | ||||||
| Government health facility | – | – | – | – | 0.76 (0.50, 1.17) | ||
| Mother’s or Dai’s home | – | – | – | – | 38.5 (13.9, 106) | Small n | |
Each estimate was generated using a separate multi-level multivariable logistic regression model involving adjustment for all preceding variables (which were assumed to act as potential confounders, as theorised in Figure 1).
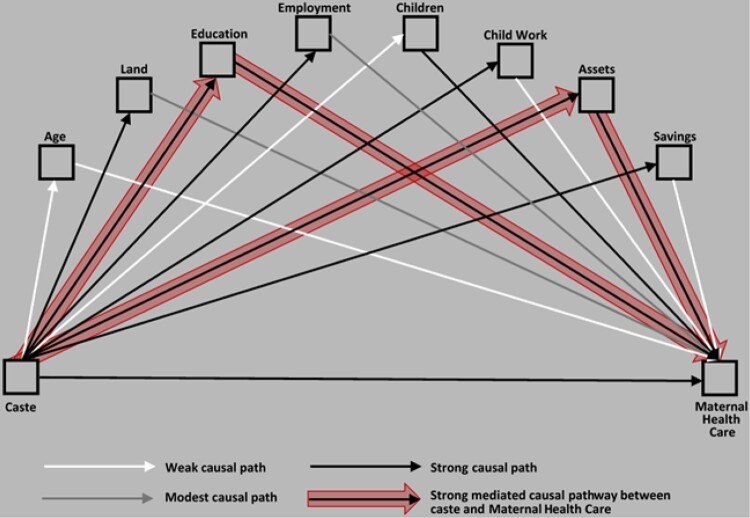
Figure 2 is a diagrammatic presentation of these findings. In it, we explicate the hypothesised, non-parametric representation of the likely temporal sequence of events described in Figure 1 with the evidence presented in Tables 4 and 5. Figure 2 simplifies each of the indirect causal pathways between caste and maternal health care as mediated through each of the individual- and/or household-level socio-economic characteristics examined in the present study. Mother’s and father’s education and occupation are also merged into “parental” variables. Overall, Figure 2 shows that caste had a strong confounder-adjusted, probabilistic causal effect on parental education and household assets and a modest one on land-ownership, employment, child-work and savings. At the same time, parental education (predominantly mother’s education) and household assets had strong confounder-adjusted, probabilistic causal effects on maternal health care use, while the number of children also had a strong effect.
Figure 2.
Simplified causal path diagram summarising the estimated strength of: (i) the total (probabilistic) causal effects of caste on each successive socio-demographic and economic characteristic, and the four maternal health care indicators (treated as a composite outcome); and (ii) the total (adjusted, probabilistic) causal effects of each successive socio-demographic and economic characteristic on the composite maternal health care indicators
Viewed together, the parametric analyses suggest that, despite the important role that caste plays in the socio-economic patterning of disadvantage across a wide range of individual- and household-level characteristics, its indirect causal effect on access to, uptake of, and expenditure on maternal health care is predominantly mediated through mother’s education and the availability of household assets. However, it is entirely plausible that caste also plays a direct role in determining uptake of maternal health care. Indeed, notwithstanding the risk of bias involved in naive mediation analyses (which interpret the path coefficient between exposures and outcomes after adjustment for one or more potential mediators),50 it is worth noting that there remained a strong direct causal effect between caste and all the four maternal health care indicators. See Table S1, online supplementary material.
Discussion
The present study is, to the best of our knowledge, the first systematic attempt to quantitatively evaluate the extent to which caste and associated socio-economic disadvantage might affect patterns of maternal health care use in Pakistan. The results of our survey provide compelling evidence that caste remains an important dimension of social stratification shaping structural disadvantage in contemporary Muslim Punjab, Pakistan. Caste emerged as an important correlate of inequitable distribution of education, occupation, land ownership and household assets. These findings align with both the small body of largely qualitative literature from Pakistan, and the vast literature from India, describing how the lowest caste groups remain largely landless, are systematically denied access to education, and remain confined to occupations characterised by poor remuneration and household asset accumulation.12,19,51
However, only two socio-economic variables – mother’s education and Household Asset Index – demonstrated strong, confounder-adjusted, probabilistic causal relationships with caste on the one hand and with maternal health services on the other. If we assume, at the minimum, that mother’s education is a proxy indicator of a woman’s knowledge of the importance of seeking biomedical care during pregnancy and birth, and the Household Asset Index is an indicator of the “financial ability” of seeking such care, it is reasonable to conclude that “Low” caste women are systematically disadvantaged. Their limited access to education opportunities potentially translates into a lack of knowledge of the importance of seeking care, and their poverty prevents them from seeking such care. Caste as a structural driver of schooling opportunities is well documented in Pakistan. Jacoby and Mansuri’s52 analysis of Pakistan Rural Household Survey data and an associated school census showed that caste and gendered norms of female seclusion constitute the two key social barriers “Low” caste girls face in accessing schools. Qualitative evidence showed that caste-based stigma also played a role in either excluding “Low” caste children or making them unwelcome.52 “Our daughters cannot attend classes together with the [high-caste] girls” and “The children of rich [high castes] are taught seriously but our children are paid no attention to” were some of the reasons low-caste mothers provided for not sending their daughters to school.52, p. 8
Nonetheless, a number of findings in the present study suggest caste alone may not be the only distal force underlying patterns of maternal health services use. Agricultural land ownership and father’s employment had a strong confounder-adjusted probabilistic causal relationship with caste, but only a modest relationship with maternal health care use. Similarly, father’s education had no relationship with any of the maternal health care indicators. In contrast, the number of children was not associated with caste but had a strong relationship with all four maternal health care indicators. We postulate the Household Asset Index might perhaps be a better indicator of the financial resources available to households for health care than land ownership, father’s employment or self-reported emergency health savings. This may be explained in terms of the Pakistani (and South Asian) cultural norm of joint families in which adult brothers not only live together but contribute to a common financial pot.53 The lack of importance of father’s education may be explained in terms of operationalisation of gender norms which exclude men from the decision-making processes around women’s reproductive health matters.54 Men who indicate an interest in their wives’ pregnancies are derogatively labelled de-masculinising terms such as a “zanankhuna”.54 Ethnographic research from Pakistan shows household “elders” – often the parental grandmother and father’s elder brother – make maternal health care seeking and associated financial decisions.53 Finally, large families are the norm in the highly pro-natalist Pakistani society.55 We postulate pronatalism is a value common to all caste groups in the country.
There also appear to be other causal pathways linking caste to poorer maternal health service use that were outside the scope of the present study. The literature indicates prejudice and discrimination are operative, mobilising instruments for preserving the advantages of the dominant groups, be it race, caste or other axis of inequity.8 A small body of ethnographic research from Pakistan has shown that prejudice and discrimination are instrumentally used by higher castes to protect their privileges in the ownership of material assets and access to social and political capital.29 In health care, disproportionately greater access of the higher castes to maternal health services is possibly a part of this proprietary claim to resources. There is, therefore, a need for further research to directly and quantitatively measure how the higher castes (and other dominant groups) determine and shape prejudice in maternal health care services.
Policy implications
Our findings have a number of policy implications for attenuating the impact of caste on maternal health care, even though caste is a millennia old, foundational structure of South Asian societies that is almost immutable.51 The first is that mothers’ education can improve uptake of maternal health care services. The value of educating the girl-child is self-evident, yet large numbers of low-caste girls remain out of school. There is some evidence that educational access for low-caste girls improves only when the school is caste-concordant, that is, the school is located in a settlement (even within a village) where low-caste groups are dominant.52 Since it is usually not economical to provide a school to each settlement, let alone cater separately to caste groups within a settlement, the authors recommend that a policy of constructing schools in low-caste dominant settlements would increase overall enrolment by almost twice as much as a policy of placing a school in every unserved village, and would do so at one-sixth of the cost.52
Another finding that can provide direction for policy development is the strong association between the Household Asset Index with both caste and maternal health care use. The existence of the minute proportion of “Low” caste wealthy groups is often cited as evidence that caste is not a relevant structural driver of inequity in Pakistan.24,26 On a more positive note, it shows that there is some room for manoeuvre and that “Low” caste groups can improve their material asset base if they are given the necessary opportunities. The first issue for policy purpose, therefore, is to improve access to opportunities for education and occupations with higher remuneration. It calls for a policy of redistribution of land, agricultural land in particular, for land ownership is highly skewed towards high-caste groups. The populist Pakistan People’s Party did try to give land to the rural landless in the Punjab Five Marla Scheme in the 1970s, but the intervention was short-lived.19 The current government’s stated aim is to provide housing for the poor, but there is no acknowledgment of the role of caste as a marker of poverty in Pakistan.
Finally, our results reveal the critical interaction between caste and district context in the production of structural inequalities in education, employment, income/wealth and health care. Caste inequity appears to be accentuated by the structural economic disparities between the two districts examined. Overall, Jhelum is the more socio-economically developed district. For example, only a quarter of households in Jhelum were in the least wealthy quartile, compared to nearly half in Layyah. This differential exists even though the percentage of households owning land was substantially lower in Jhelum than in Layyah. Clearly policies promoting broad socio-economic development have the potential to impact the broader opportunity structures and mitigate the effects of caste.
Limitations
The study has a number of limitations. The first is the possibility of potential bias introduced by our sampling methodology in which we used the Lady Health Workers’ (LHWs) database to identify women who had recently given birth. Although most “Low” caste people live amongst the “High”/“Middling” caste populations in the main settlements, some tend to live in spaces that may not be part of LHW-catchment areas.26 This commonly happens in bhattas (brick kilns) that often operate with bonded labour.56 Our sampling approach may have under-represented the most disadvantaged of the lower caste groups. Second, and closely associated, is the role of geography. It is possible some of the low-caste groups might be living in geographically clustered areas on the outskirts of the village settlement, which might add distance as an additional barrier to seeking services of all kinds (roads, schools, clinics). This is an important limitation for we did not collect data on geography and distance. A third limitation is a possibility of respondents self-reporting their caste as higher than that recognised by their wider society. As discussed above, caste is a socially presented and discursively constituted identity and depends on local social, religious, economic and political contexts.20,27 Low-caste groups constantly aspire to change their identity, most commonly by reporting their caste as a higher one.30 This possible “misclassification” will bias the estimates towards the null and reduce the effect of caste inequities on maternal health care use. Another limitation is that the hypothesised causal pathways summarised in Figure 1 might incorrectly distinguish between variables acting as confounders vs. mediators for each of the exposures examined in Table 5’s 14 discrete models. Our novel analytical approach strove to reduce the risk of confounder bias while avoiding biases associated with the inappropriate adjustment for mediators.46,47 There is also a possibility some variables – specifically women’s employment and number of children – may be endogamous to outcomes of interest. In that case, the variables may be neither confounding nor mediating. However, this possibility might only be true for a small number of respondents, as a large body of literature shows that women’s labour force participation in Pakistan is low, largely due to gender norms that prize women’s seclusion and economic dependency54,57; It is possible that there exist additional, possibly latent variables that are likely to be involved in the causal pathways between caste and maternal health care outcomes but that remained unmeasured in the present survey. These unexplored factors might include the well-documented prejudice and discrimination towards the low-caste Kammi women reported from Pakistan and India.23,58 They might also include other gender-based values that cut across all caste groups. Some of these unmeasured variables may be capable of contributing confounding bias to each of the adjusted estimates summarised in Table 5 (see Figure 2). It is also inevitable that imprecision and error in the measurement (and categorisation) of the variables collected during the study’s survey is likely to mean that some residual confounding will be present and may affect the adjusted estimates generated by each of the multivariable statistical models in Table 5. Finally, our study was limited to two districts in one province of Punjab. The study would have been more meaningful politically if we had a larger sample representing all marginalised groups in Pakistan, including the Dalit Christians living in urban ghettos and Hindus living in Sindh.20
To conclude, our study provides strong empirical evidence of the existence and operationalisation of the caste system as a structural driver of socio-economic and maternal health care inequities in contemporary Pakistan. The study adds to the small, but emerging body of literature mapping how this Muslim society continues to actively draw on notions of caste to maintain class and material hierarchy. The findings provide a pivot for policy re-engagement with caste as a valid category addressing class and health care inequities in Pakistan. They are particularly useful for convincing sceptical Pakistani policymakers who tend to reject evidence that caste is a societal cause of deprivation and marginalisation in Pakistan.24
Supplementary Material
Funding Statement
This work was supported by Research and Advocacy Fund, Pakistan.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed at http://dx.doi.org/10.1080/26410397.2022.2035516.
References
- 1.Porroche-Escudero A, Popay J, Ward F.. From fringe to centre-stage: experiences of mainstreaming health equity in a health research collaboration. Health Res Policy Syst. 2021;19(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.General Assembly . Sustainable development goals: transform our world, 2030. Geneva: United Nations; 2015. [Google Scholar]
- 3.Commission on Social Determinants of Health . Closing the gap in a generation: health equity. Geneva: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 4.Sanneving L, Trygg N, Saxen D, et al. Inequity in India: the case of maternal and reproductive health. Glob Health Action. 2013;6:19145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussein J. Exploring inequities, inspiring new knowledge and action. Glob Health Action. 2018;26(54):1–4. [DOI] [PubMed] [Google Scholar]
- 6.Khatri R, Karkee R.. Social determinants of health affecting utilisation of routine maternity services in Nepal: a narrative review of the evidence. Reprod Health Matters. 2018;26(54):32–46. [DOI] [PubMed] [Google Scholar]
- 7.Kabeer N. Social exclusion and the MDGs: challenge of ‘durable inequalities’ in the Asian context. Inst Develop Stud Bull. 2006;37:64–78. [Google Scholar]
- 8.Darity W. The economics of the dispossessed. J Soc Inclusion Stud. 2014;1(1):7–15. [Google Scholar]
- 9.Amos T. Portrait of a Tokugawa outcaste community. East Asian Hist (Canberra). 2006;32(33):83–108. [Google Scholar]
- 10.Seif H. The accursed minority: The ethno-cultural persecution of Al-Akhdam in the Republic of Yemen. Muslim World J Hum Right. 2005;2(1):10–29. [Google Scholar]
- 11.Rhim SM. The Paechong: “Untouchables” of Korea. J Orient Stud. 1974;12:30–40. [Google Scholar]
- 12.Borooah VK, Sabharwal NS, Diwakar DG, et al. Caste, discrimination and exclusion in modern India. New Dehli: SAGE; 2015. [Google Scholar]
- 13.Mojumdar S. Determinants of Health service utilization by urban households in India: a multivariate analysis of NSS case-level data. J Health Manag. 2018;20:105–121. [Google Scholar]
- 14.Ghimire U. Inequalities in health outcomes and access to services by caste/ethnicity, province, and wealth quintile. Rockville, MD, USA: ICF: DHS Further Analysis Reports No. 117. 2019.
- 15.Pathak P, Singh A, Subramanian S.. Economic inequalities in maternal health care: prenatal care and skilled birth attendance in India. PLoS One. 2010;5(10):e13593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yadav A, Jena P.. Maternal health outcomes of socially marginalized groups in India. Int J Health Care Qual Assur. 2020;3(2):172–188. [DOI] [PubMed] [Google Scholar]
- 17.Ambedkar B. The Hindu social order: Its essential features. Mumbai: Higher Education Department, Government of Maharashtra; 1987. [Google Scholar]
- 18.Sikand Y. Islam, caste and Dalit-Muslim relations in India. 1st ed. New Delhi: Global Media Publications; 2004. [Google Scholar]
- 19.Gazdar H, Mallah H.. Class, caste and housing in rural Pakistani Punjab: The untold story. Ind Sociol. 2012;4(3):311–336. [Google Scholar]
- 20.Hussain G. ‘Dalits are in India, not in Pakistan’: Exploring the Discursive Bases of the Denial of Dalitness under the Ashrafia Hegemony. J Asian Afr Stud. 2020;55(1):17-43. [Google Scholar]
- 21.Gazdar H. Rural economy and livelihoods in Pakistan. TA 4319-PAK determinants and drivers of poverty reduction and ADB’s contribution in rural Pakistan. Islamabad: Asian Development Bank; 2007b.
- 22.Mumtaz Z, Salway S, Shanner L, et al. Addressing disparities in maternal health care in Pakistan: gender, class and social exclusion. BMC Pregnancy Childbirth. 2012;12:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aliani S. Caste in Pakistan: The elephant in the room. [Online]. 2009 [cited 24 Feb 2021]. Available at: https://reddiarypk.wordpress.com/2009/08/25/caste-in-pakistan/.
- 24.Gazdar H. Class, caste or race: veils over social oppression in Pakistan. Econ Polit Wkly. 2007a;42(2):86–88. [Google Scholar]
- 25.Martin N. The political Economy of bonded labour in the Pakistani Punjab. Contrib Ind Sociol. 2009;43(1):35–59. [Google Scholar]
- 26.Mumtaz Z, Salway S, Bhatti A, et al. Improving maternal health in Pakistan: towards a deeper understanding of the social determinants of poor women's access to maternal health services. Am J Public Health. 2014a;104:S1: S17–S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guru G Politics of Naming. Seminar. 1998. [October] http://www.india-seminar.com/2018/710/710_gopal_guru.htm (accessed 28 March 2020).
- 28.Bidner C, Eswaran M.. A gender-based theory of the origin of the caste system of India. J Dev Econ. 2015;114:142-58. [Google Scholar]
- 29.Mumtaz Z, Salway S, Bhatti A, et al. Addressing invisibility, inferiority and powerlessness to achieve gains in maternal health for the ultra-poor. Lancet. 2014b;383(9922):1095–1097. [DOI] [PubMed] [Google Scholar]
- 30.Butt WH. Waste intimacies: Caste and the unevenness of life in urban Pakistan. Am Ethnol. 2020;47(3):234-48. [Google Scholar]
- 31.Aziz A, Khan F, Wood G.. Who is excluded and how? An analysis of community spaces for maternal and child health in Pakistan. Health Res Policy Syst. 2015;13:65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thorat S, Newman K.. Blocked By caste: economic discrimination in modern India. New Dehli: Oxford Press; 2010. [Google Scholar]
- 33.Marmot M. Just societies, health equity, and dignified lives: the PAHO equity. Lancet. 2018;392(10161):2247–2250. [DOI] [PubMed] [Google Scholar]
- 34.Jamal H. Spatial disparities in socioeconomic development: the case of Pakistan. Pak Develop Rev. 2016;55(4):421–435. [Google Scholar]
- 35.Punjab Health Statistics 2020 [Internet] . Lahore: Bureau of Statistics, Government of Punjab. 2020. Jan 1 [cited 2022 Feb 4]. Available from: http://bos.gop.pk/system/files/Punjab%20Health%20Statistics%202019-2020.pdf.
- 36.National Institute of Population Studies . Demographic and health survey 2006-07. Islamabad, Pakistan, Calverton, MD, USA: Macro International Inc. 2008.
- 37.Wazir M, Shaikh B, Ahmed A.. National program for family planning and primary health care Pakistan: a SWOT analysis. Reprod Health. 2013;10:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonevski B, Randell M, Paul C, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014;14:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Felbab-Brown V. Security considerations for conducting fieldwork in highly dangerous places or on highly dangerous subjects. Soc Sci Res Counc Work Papers. 2014;3:1–27. [Google Scholar]
- 40.Rose H. A glossary of the tribes and castes of the Punjab and North-West Frontier Province [Internet]. Lahore: Open Library; 1911. - [cited 2017 Jun 5]. Available from: https://archive.org/details/glossaryoftribes03rose/page/n5/mode/2up?view=theater. [Google Scholar]
- 41.Schreiner M. A simple poverty scorecard for Pakistan. J Asian Afr Stud. 2010;45(3):1–11. [Google Scholar]
- 42.Textor J, Hardt J, Knüppel S.. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745. [DOI] [PubMed] [Google Scholar]
- 43. www.dagitty.net . DAGitty – draw and analyze causal diagrams. [Internet]. 2021 - [cited 24 Mar 2021]. Available from: http://www.dagitty.net/.
- 44.Tennant PW, Murray EJ, Arnold KF, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peters T. Multifarious terminology: multivariable or multivariate? Univariable or univariate?. Paediatr Perinat Epidemiol. 2008;22(6):506. [DOI] [PubMed] [Google Scholar]
- 46.Schisterman E, Cole S, Platt R.. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richiardi L, Bellocco R, Zugna D.. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42:1511–1519. [DOI] [PubMed] [Google Scholar]
- 48.StataCorp . Stata statistical software: release 15. College Station (TX: ): StataCorp LP; 2017. [Google Scholar]
- 49.Munafò MTK, Taylor A, Evans D, et al. Collider scope: when selection bias can substantially influence observed associations. Int J Epidemiol. 2018;47:226–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hudgens M, Halloran M.. Toward causal inference with interference. J Am Stat Assoc. 2008;103:832–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Desai S, Dubey A.. Caste in 21st century India: competing narratives. Econ Polit Wkly. 2011;46(11):40–49. [PMC free article] [PubMed] [Google Scholar]
- 52.Jacoby H, Mansuri G. Crossing boundaries: gender, caste and schooling in rural Pakistan. Washington (DC): World Bank Policy Research Working Paper 5710; 2021.
- 53.Mumtaz Z. Gender and reproductive health: a need for reconceptualization. London: University of London; 2003. [Google Scholar]
- 54.Mumtaz Z, Salway S.. Understanding the gendered influences on women’s reproductive health in Pakistan: moving beyond the autonomy paradigm. Soc Sci Med. 2009;68(7):1349–1356. [DOI] [PubMed] [Google Scholar]
- 55.Ataullahjan A, Vallianatos H, Mumtaz Z.. Violence and precarity: a neglected cause of large family sizes in Pakistan. Glob Public Health. 2021;10:1–0. [DOI] [PubMed] [Google Scholar]
- 56.Ercelawn A, Nauman M.. Bonded labour in Pakistan [Internet]. Geneva: International Labor Organization; 2001. Jun 1 [cited 2020 Feb 10]. Available from: http://ilo.org/wcmsp5/groups/public/---ed_norm/---declaration/documents/publication/wcms_096991.pdf. Accessed on Feb 10, 2020. [Google Scholar]
- 57.National Institute of Population Studies (NIPS) [Pakistan] and ICF . 2020. Pakistan Demographic and Health Survey 2017-18. Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF. [Google Scholar]
- 58.Mumtaz Z, Levay A, Salway S, et al. Disparities, status and signalling in maternal health care use in Punjab, Pakistan. Soc Sci Med. 2013;94:98–105. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.