Abstract
Objective:
Post-traumatic stress disorder (PTSD) has been associated with heightened impulsivity and risk-taking behaviours, including higher rates of substance use than individuals without PTSD. While a number of studies suggest that impulsivity is associated with substance use in PTSD, the specific role of impulsivity in this common pattern of comorbidity remains unclear. The current study investigated associations between PTSD symptoms, substance use patterns, and impulsivity in a sample of adults.
Method:
A total of 2967 participants were recruited online through Amazon’s Mechanical Turk. Participants who did not report at least one Criterion A traumatic event on the Brief Trauma Questionnaire were excluded. The remaining 1609 trauma-exposed individuals were placed into either the probable PTSD group (n=406) or the trauma-exposed non-PTSD group (n=1203) based on their PTSD Checklist for DSM-5 (PCL-5) score. Impulsivity was assessed via a delay discounting measure and the brief UPPS-P impulsiveness questionnaire. Alcohol and cannabis were assessed using the AUDIT and CUDIT-R scales, respectively.
Results:
Probable PTSD participants exhibited steeper (more impulsive) delay discounting and endorsed more impulsive traits than participants in the trauma-exposed non-PTSD group. Moreover, the PTSD group reported significantly higher scores on both the AUDIT and CUDIT-R. Lastly, impulsive personality traits on the UPPS-P partially mediated the association between PTSD and both cannabis and alcohol use.
Conclusions:
These findings suggest that trauma-exposed individuals who exhibit elevated PTSD symptoms show heightened impulsivity. It also appears that lower levels of impulsivity may serve as a protective factor among trauma-exposed individuals resilient to the development of PTSD.
Keywords: alcohol, cannabis, delay discounting, impulsivity, post-traumatic stress disorder
Introduction
Exposure to a traumatic event can lead to post-traumatic stress disorder (PTSD)—a chronic condition with debilitating effects on an individual’s social, emotional, physical, occupational, and cognitive functioning (American Psychiatric Association, 2013; Nemeroff et al., 2006). PTSD is associated with heightened impulsivity and risk-taking behaviours (Tull, Weiss, & Mcdermott, 2016) and according to the latest version of the Diagnostic and Statistical Manual for Mental Disorders involves increased recklessness and self-destructive behaviors (DSM-5; American Psychiatric Association, 2013). One common form of risk-taking behaviour often associated with PTSD is the problematic use of substances. Although prevalence estimates vary, rates of substance use disorders (SUDs) among individuals with PTSD are consistently found to be higher than in individuals without the disorder (Jacobsen, Southwick, & Kosten, 2001; Kachadourian, Mccarthy, & Petrakis, 2016; Van Ameringen, Mancini, Patterson, & Boyle, 2008), and reports of previous trauma exposure in individuals with SUDs are strikingly common (e.g., Back et al., 2000; Brown, Stout, & Mueller, 1996; Gielen, Havermans, Tekelenburg, & Jansen, 2012). Indeed, one nationally-representative U.S. sample found that 46% of individuals with PTSD also had a SUD (Pietrzak, Goldstein, Southwick, & Grant, 2011). Moreover, among patients seeking treatment for SUD, lifetime PTSD rates have been found to range from 30 to 60% (Back et al., 2000; Brady, Sudie E. Back, & Coffey, 2004; Jacobsen et al., 2001; McCauley, Killeen, Gros, Brady, & Back, 2012). Critically, individuals with comorbid PTSD and SUD appear to suffer a higher illness burden, with more acute psychiatric symptoms, worse physical health, and higher rates of other psychiatric comorbidities than those with either condition alone (Kachadourian et al., 2016; Schäfer & Najavits, 2007; Weiss, Tull, Anestis, & Gratz, 2013).
Substance use in individuals with PTSD might serve as a coping mechanism, arising in response to the negative alterations in mood, hyperarousal, and intrusive memories that characterize the disorder (Contractor, Weiss, Dranger, Ruggero, & Armour, 2017; Kachadourian et al., 2016). Indeed, increases in craving severity and substance use are often associated with increases in PTSD symptoms in individuals with comorbid PTSD and SUD (Schäfer & Najavits, 2007). Although this ‘self-medication’ explanation for the comorbidity of PTSD and SUDs is supported by extant research (e.g., Haller & Chassin, 2014; James, Strom, & Leskela, 2014), it does not explain why some individuals with PTSD develop problematic substance use, while others do not. From a clinical intervention perspective, the failure to identify differentiating factors between individuals with PTSD who use substances problematically and those who do not impedes clinicians’ ability to provide necessary supports and intervention strategies for those most in need. In the wider addiction literature, substance use and other addictive disorders have been associated with heightened impulsivity (Amlung, Vedelago, Acker, Balodis, & MacKillop, 2017; Perry & Carroll, 2008; VanderBroek-Stice, Stojek, Beach, & MacKillop, 2017). Moreover, impulsivity is thought to play an important role in both the development and maintenance of SUDs (Perry & Carroll, 2008). Since PTSD is also associated with higher levels of impulsivity (e.g., James et al., 2014), there is a growing interest in how PTSD, SUD, and impulsivity are related with each other (Tull et al., 2016) and how their associations may be fruitful in developing more effective evidence-based prevention and intervention strategies.
Impulsivity has been described as a ‘multidimensional construct’ that can be defined and measured in various ways (Grant & Chamberlain, 2014; MacKillop et al., 2016; Perry & Carroll, 2008). One form of impulsivity, impulsive choice, refers to the tendency to choose smaller immediate rewards over larger but non-immediate rewards. It is typically assessed using delayed reward discounting tasks, which measure the extent to which future rewards are devalued based on when they will be received (e.g., Amlung et al., 2017; MacKillop et al., 2011). Steeper discounting (i.e., the tendency to devalue the larger-delayed rewards to a greater extent in favor of immediate gratification of smaller-sooner rewards) has been consistently observed across addictive disorders, and appears to be related to symptom severity (Amlung et al., 2017; MacKillop et al., 2011). There is also evidence of significantly steeper discounting of delayed monetary gains among trauma-exposed individuals relative to controls (Li, Li, & Liu, 2011; Simmen-Janevska, Forstmeier, Krammer, & Maercker, 2015; Van Den Berk-Clark, Myerson, Green, & Grucza, 2018), and significantly altered delay discounting preferences in individuals with comorbid PTSD and major depressive disorder compared to controls (Engelmann, Maciuba, Vaughan, Paulus, & Dunlop, 2013). Despite these promising initial findings, research on the association between delay discounting and PTSD symptoms remains limited.
Another form of impulsivity is trait impulsivity, which is assessed using self-report measures such as the UPPS-P Impulsive Behavior Scale (Cyders, Littlefield, Coffey, & Karyadi, 2014; Whiteside & Lynam, 2001). The UPPS-P assesses five subtypes of impulsive behaviour: responding to immediate cues under conditions of positive or negative affect (positive and negative urgency), acting without thinking (lack of premeditation), failing to persist with or complete tasks (lack of perseveration), and engaging in highly stimulating activities (sensation seeking). Although all subtypes have been associated with substance use, positive urgency, negative urgency, and lack of premeditation are thought to be particularly important in problematic use of a wide range of substances (Oshri et al., 2017). Several studies have found higher levels of negative urgency in association with PTSD and trauma exposure (Contractor, Armour, Forbes, & Elhai, 2016; James et al., 2014; Mirhashem et al., 2017; Roley, Contractor, Weiss, Armour, & Elhai, 2013, 2017; Weiss et al., 2013). Furthermore, among individuals with a current or past SUD, those with comorbid PTSD have higher negative urgency than those with SUD alone (Mirhashem et al., 2017; Weiss et al., 2013). In one recent study, PTSD symptom severity was found to be positively associated with levels of positive and negative urgency, as well as substance-related problems (Mirhashem et al., 2017).
While a number of studies suggest that problematic substance use in PTSD is associated with heightened impulsivity, the role of impulsivity in this common pattern of comorbidity is unclear. In a recent study, Oshri and colleagues (2017) found mediating roles for impulsive choice (delay discounting) and trait impulsivity in the association between child abuse or neglect and substance use. Exposure to chronic early life adversity may influence later substance use through effects on impulsivity, but it is not clear whether impulsivity plays a similar role in the association between PTSD and substance use. The aim of the current study was, therefore, to investigate the association between PTSD, alcohol and cannabis use patterns, and impulsivity in a large sample of adults who reported exposure to at least one DSM-5 Criterion A traumatic event. As indicated above, prior studies have largely utilized two analytic approaches—either comparing a PTSD and control group or examining PTSD symptom severity as a continuous variable. Therefore, to be comprehensive and consistent with the literature, we examined both approaches by exploring between-group differences in impulsivity and using a structural equation modelling approach to examine continuous associations.
Based on previous findings (e.g., Mirhashem et al., 2017), we hypothesized that there would be a positive association between self-reported PTSD symptom severity and alcohol and cannabis use. In addition, we hypothesized that individuals reporting symptoms above the cutoff for probable PTSD would demonstrate higher levels of impulsivity on the UPPS-P, as well as steeper discounting on the delay discounting task. Lastly, based on Oshri et al. (2017), we expect that the association between PTSD symptoms and substance use would be partially mediated by increased trait impulsivity and impulsive delay discounting
Methods
Participants
Participants for the current study were recruited online through Amazon’s Mechanical Turk (MTurk; www.mturk.com). The survey visible to participants was titled “Investigating Decision Making and Personality Correlates of Behaviour” and provided a brief description stating that this was“… a research study on the relationships between personality traits and decision-making preferences and various lifestyle behaviors such as substance use, driving behaviors, stress.” Participants were not directly told that we would be examining a history of trauma and would therefore not be incentivized to report any past trauma. The survey was posted in September 2017 and made available until December 2017. The study was approved by the Hamilton Integrated Research Ethics Board, and all participants provided informed consent electronically. Participants received $2 USD upon successful completion of the survey. Eligible participants had to be at least 18 years of age, be geographically located in the United States, have previously completed at least 100 MTurk surveys with a minimum of 95% approval rating on prior surveys, and be responding from a unique IP address (to minimize the chance of duplication in responding). The initial recruited sample consisted of 3024 adults. After excluding participants with incomplete data (n=57), the sample consisted of 2967 participants.
Of the 2967 eligible participants, we excluded participants who did not report at least one Criterion A traumatic event on the Brief Trauma Questionnaire (BTQ). This resulted in a sample of 1609 trauma-exposed individuals. Individuals with a score of 33 or above on the PTSD Checklist for DSM-5 (PCL-5) (Creamer, Bell, & Failla, 2003) were placed into the probable PTSD group (n=406), while those with a score lower than 33 were placed into the trauma-exposed non-PTSD group (n=1203)
Measures
Participants completed a variety of measures using Qualtrics Survey Software. For the current study we examined participants’ responses on eight measures that were part of a larger test battery.
Brief Trauma Questionnaire.
The Brief Trauma Questionnaire (BTQ) is a self-report measure consisting of 10 items that may be used to assess traumatic exposure via the DSM-IV criteria (Schnurr, Iii, Vielhauer, Findler, & Hamblen, 2002). Positively endorsed items are followed by two subsequent questions that assess whether the event meets the definition of a Criterion A traumatic event (an event resulting in serious injury, or where risk of serious injury or death was perceived). A breakdown of the BTQ items endorsed and number of Criterion A traumatic events, is included in Tables S2–S3 in supplemental material.
PTSD Checklist for DSM-5.
The PCL-5 is a self-report measure consisting of 20 items reflecting the DSM-5’s symptoms of PTSD, each rated on a 5-point scale from not at all (0) to extremely (4). The total score on the PCL-5 (range 0–80) was used, with a cut-off score of 33 used to indicate a provisional diagnosis of having PTSD (Creamer, Bell, & Failla, 2003). Cronbach’s α for the current sample was 0.99.
Alcohol Use Disorders Identification Test.
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening tool used to assess alcohol consumption and alcohol-related problems over the past 12 months (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). A total score of 8 or above is typically considered an indication of hazardous alcohol use. Cronbach’s α for the current sample was 0.95.
Cannabis Use Disorders Identification Test-Revised.
The Cannabis Use Disorders Identification Test-Revised (CUDIT-R) is an 8-item screening tool adapted from the AUDIT to assess cannabis consumption and cannabis-related problems over the past 6 months (Adamson et al., 2010). A total score of 8 or above is typically considered an indication of hazardous cannabis use (Adamson et al., 2010). Cronbach’s α for the current sample was 0.90.
Generalized Anxiety Disorder 7-item Scale.
The Generalized Anxiety Disorder 7-item Scale (GAD-7) is a 7-item self-report questionnaire used for measuring generalized anxiety disorder symptoms over the past two weeks (Spitzer, Kroenke, Williams, & Löwe, 2006). Cronbach’s α for the current sample was 0.93.
Patient Health Questionnaire.
The Patient Health Questionnaire (PHQ-9) is a 9-item, self-report screening tool used to measure a participant’s severity of depression over the past two weeks (Kroenke, Spitzer, & Williams, 2001). Cronbach’s α for the current sample was 0.90.
Delay Discounting Task.
Participants completed two versions of a hypothetical five-choice monetary delay discounting paradigm for hypothetical monetary rewards (Koffarnus & Bickel, 2014). On each item, participants indicated whether they would rather receive a larger amount of money (either $10 or $100) at a specific point in the future (range: 1 hour to 25 years), or half the amount of money (either $5 or $50) immediately. Participant responses were used to calculate an Effective Delay 50% (ED50), and the inverse of this value is equivalent to the discounting rate (e.g., k = 1/ED50). Principal components analysis (PCA) was used to generate a single discounting index across the two magnitudes (e.g., Amlung & MacKillop, 2014).
Short UPPS-P.
The Short UPPS-P is a 20-item, self-report questionnaire that measures five dimensions of impulsive behaviour (negative urgency, lack of premeditation, lack of perseveration, sensation seeking, and positive urgency; Cyders et al., 2014). Each item is rated on a 4-point scale, from Agree strongly (1) to Disagree strongly (4). A mean score was calculated across the four items constituting each of the five subscales. The Cronbach’s alpha values for the UPPS-P in this sample are as follows: Negative Urgency (0.79), Positive Urgency (0.82), Sensation Seeking (0.73), Lack of Premeditation (0.80), Lack of Perseveration (0.72).
Data Analysis
Preliminary analyses compared demographic characteristics between participants in the PTSD and trauma-exposed non-PTSD groups using independent samples t-tests or chi-square tests. Next, we compared total scores on the AUDIT, CUDIT-R, PHQ-9, and GAD-7 between groups using independent samples t-tests. We compared delay discounting rate (composite log(k) across $10 and $100) between PTSD and non-PTSD groups using a univariate analysis of covariance (ANCOVA). A multivariate analysis of covariance (MANCOVA) was used to compare the five UPPS-P subscales between the two groups, with Bonferroni correction applied for pairwise comparisons by subscale. In both cases, we adjusted for age, sex, and education.
Mediation was tested using structural equation modeling (SEM) using maximum likelihood estimation as implemented in Mplus version 7.31 (Muthén & Muthén, 2011). We specified an indirect effect model using a latent impulsivity factor from the UPPS-P (described below), as well as a second model in which UPPS-P subscales were entered simultaneously as unique mediators.
Results
Sample Characteristics
Full sample characteristics are provided in Table 1. Compared to the non-PTSD group, participants in the PTSD group were younger, had fewer years of education, and had lower income. Groups did not differ with respect to sex or racial distribution. Scores on the PHQ-9 and GAD-7 indicated higher symptoms of depression and anxiety, respectively, in the PTSD group compared to the non-PTSD group. Finally, the PTSD group reported higher scores on both the AUDIT and CUDIT-R relative to the non-PTSD group. A greater percentage of participants in the PTSD group exceeded cutoffs for hazardous alcohol and cannabis use (see Table 1). Bivariate correlations among study variables are presented in Table S1.
Table 1.
Sample Characteristics
| Overall (n = 1609) |
PTSD (n = 406) |
Non-PTSD (n = 1203) |
||
|---|---|---|---|---|
| Mean (SD); %; Median | Mean (SD); %; Median | Mean (SD); %; Median | Sig. | |
| Sex | 59% Female | 63.1% Female | 58.6% Female | p = .11 |
| Age | 37.2 (11.9); Range 18–80 | 34.16 (12.3); Range 18–80 | 38.28 (10.2); Range 19–73 | p < .001 |
| Education | 15.2 (2.5) | 14.9 (2.8) | 15.4 (2.3) | p < .001 |
| Ethnicity | p = .58 | |||
| Caucasian | 72.8% | 70.9% | 73.4% | |
| Black | 6.3% | 7.6% | 5.8% | |
| Asian | 7.8% | 8.6% | 7.5% | |
| Native Hawaiian / Pacific Islander | 7.0% | 5.9% | 7.3% | |
| Hispanic / Latino | 0.5% | 0.5% | 0.5% | |
| Other | 5.6% | 6.5% | 5.5% | |
| Income | ||||
| < $15,000 | 10.6% | 17.7% | 8.1% | p < .001 |
| $15–30,000 | 19% | 20.4% | 18.5% | |
| $30–$45,000 | 17.8% | 18% | 17.8% | |
| $45–$60,000 | 15.5% | 16.5% | 15.2% | |
| $60–$75,000 | 11.2% | 11.8% | 11.1% | |
| $75–$90,000 | 10.1% | 7.6% | 10.9% | |
| > $90,000 | 15.8% | 8% | 18.4% | |
| Depression (PHQ-9) | 7.81 (6.27) | 14.02 (6.32) | 5.72 (4.67) | p < .001 |
| Anxiety (GAD-7) | 7.25 (5.80) | 13.03 (5.1) | 5.30 (4.57) | p < .001 |
| Alcohol Use (AUDIT) | 5.03 (5.77) | 6.89 (7.52) | 4.40 (4.89) | p < .001 |
| AUDIT 8+ | 22.4% | 33.3% | 18.8% | p < .001 |
| Cannabis Use (CUDIT-R) | 3.58 (5.89) | 5.73 (7.60) | 2.86 (4.98) | p < .001 |
| CUDIT-R 8+ | 20.8% | 32.8% | 16.9% | p < .001 |
Note. PHQ-9 = Patient Health Questionnaire; GAD-7 = Generalized Anxiety Disorder questionnaire; AUDIT = Alcohol Use Disorders Identification Test (Hazardous use defined as AUDIT score of 8 or higher); CUDIT-R = Cannabis Use Disorders Identification Test (Hazardous use defined as a CUDIT-R score of 8 or greater).
Differences in Impulsivity between PTSD Groups
Differences in delay discounting between the PTSD and non-PTSD groups were examined using ANCOVA models adjusting for age, sex, and education. The PTSD group exhibited steeper discounting of delayed rewards compared to the trauma-exposed non-PTSD group, F(1, 1600) = 25.26, p < .001, ηp2 = .02 (Table 2). A follow-up ANCOVA that also included income and depressive symptoms as covariates did not impact the significant differences in delay discounting between groups. With respect to impulsive personality traits, there was a significant omnibus effect of PTSD group, F(5, 1600) = 58.24, p < .001, Wilks’ Λ = .846, ηp2 = .02 (Table 2). Pairwise comparisons with Bonferroni correction indicated that the PTSD group reported higher scores on four of the UPPS-P subscales relative to the trauma-exposed non-PTSD group, including Negative Urgency (p < .001), Positive Urgency (p < .001), Lack of Premeditation (p < .001), and Lack of Perseveration (p < .001). Sensation seeking did not significantly differ between groups (p = .93).
Table 2.
Group Means for Delay Discounting and UPPS-P Subscales in PTSD and Non-PTSD Groups
| PTSD | Non-PTSD | |||
|---|---|---|---|---|
|
| ||||
| Mean | SD | Mean | SD | |
| Delay Discounting Log(k) | 0.27 | 0.93 | −0.05 | 0.95 |
| UPPS Negative Urgency | 2.70 | 0.73 | 2.03 | 0.68 |
| UPPS Positive Urgency | 2.12 | 0.79 | 1.62 | 0.60 |
| UPPS Premeditation | 1.95 | 0.65 | 1.64 | 0.52 |
| UPPS Perseverance | 1.86 | 0.61 | 1.71 | 0.52 |
| UPPS Sensation Seeking | 2.37 | 0.79 | 2.35 | 0.77 |
Note: Unadjusted means and SD presented in table.
Indirect Effects Model with Impulsivity Latent Factor
We specified an indirect effect model in which a latent impulsivity factor (comprised of Negative Urgency, Positive Urgency, Lack of Premeditation, and Lack of Perseveration; see below) mediated the influence of PTSD symptoms on alcohol and cannabis use. Full statistical results of the indirect effects model are presented in Supplementary Materials (Table S4–S5). Age, sex, and education were adjusted for by including them as covariates. We also specified an indirect effect model for delay discounting; however, model fit was unacceptable for this analysis and results are not included.
Factor loadings for Impulsivity (IMP) were significant and in the predicted direction; all indicators exceeded .45 except for Lack of Perseveration (Persev), which was kept in the model due to its theoretical foundations (see MacKillop et al., 2016). Sensation seeking was trimmed from the model because of low factor loading (λ < 0.2) and poor model fit. No offending estimates emerged (e.g., negative residual variances or correlations > 1.0). Measurement model is depicted in Figure S1 in Supplementary Materials
Next, we tested the pathway from PTSD symptoms to AUDIT and CUDIT-R via changes in impulsivity. Participants’ age, sex, and education were included as covariates. Among the control variables, male sex was associated with higher impulsivity (β = −.050, p < .040) and AUDIT (β = −.134, p < .000). Age was associated negatively with impulsivity (β = −.111, p < .001), AUDIT (β = −.114, p < .001), and CUDIT-R (β = −.110, p < .001). Years of education was associated negatively with CUDIT-R (β = −.083, p < .001). Non-significant covariates were trimmed from the model; therefore, education was trimmed as a covariate of impulsivity and AUDIT, and sex was trimmed as a covariate of CUDIT-R.
Modification indices suggested covarying the residuals of Lack of Premeditation (Premed) with Positive Urgency (PosUrg), Lack of Premeditation with Lack of Perseveration, and AUDIT with CUDIT-R. The final model and fit indices are presented in Figure 1a. PTSD symptoms were positively associated with impulsivity (β = .546, p < .001). Impulsivity in turn was positively associated with AUDIT (β = .231, p < .001) and CUDIT-R (β = .089, p < .010). PTSD symptoms were positively associated with CUDIT-R (β = .150, p < .001) but not AUDIT (β = .039, p = .204). A significant indirect association was found for both AUDIT (α x β = .126, p < .001) and CUDIT-R (α x β = .049, p < .010).
Figure 1. Mediation Model with PTSD and Impulsivity Latent Factor.
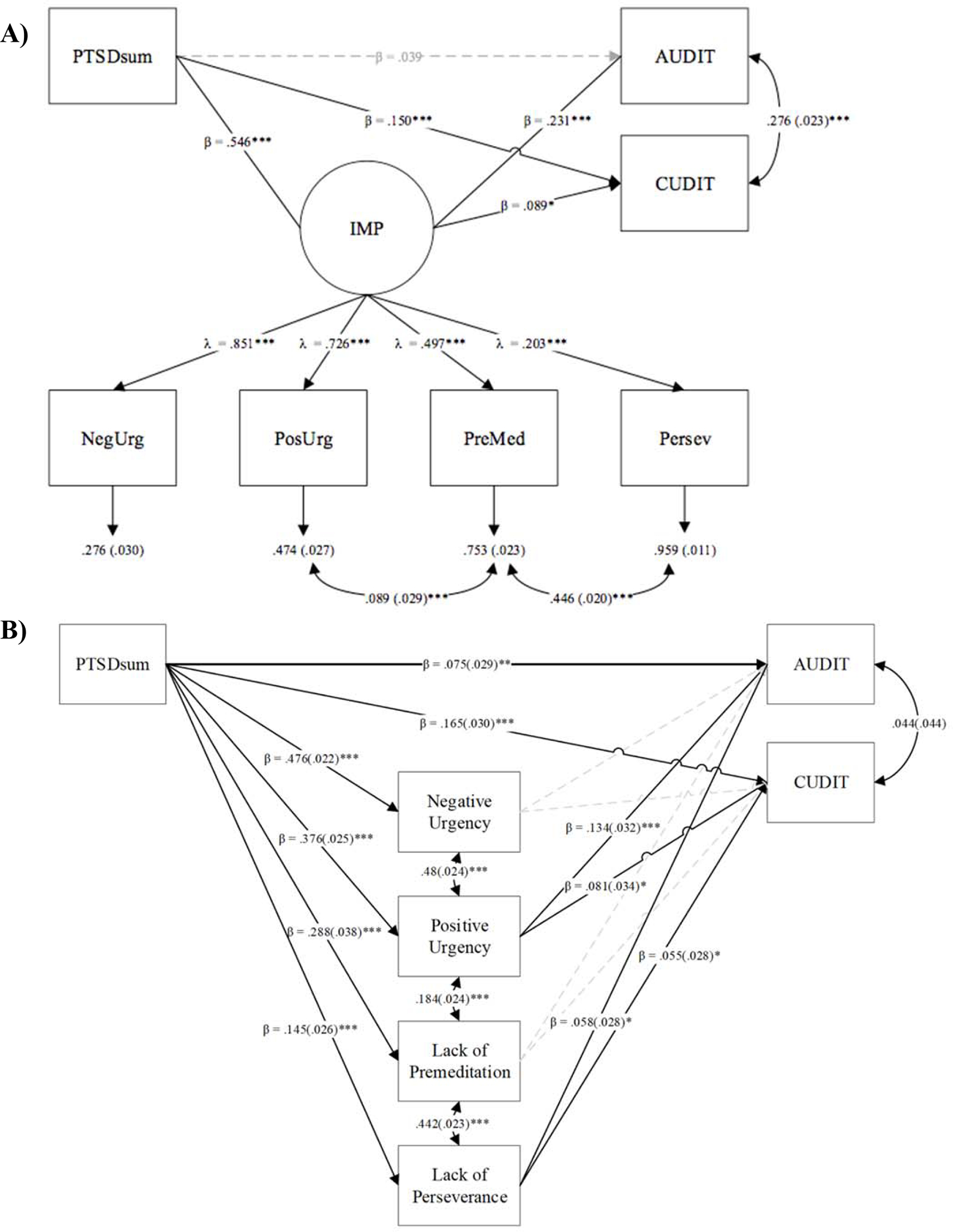
Note. Panel A depicts model with latent impulsivity factor. Panel B depicts model with individual UPPS-P subscales modeled concurrently. All values are standardized. Standard errors for residuals and covariances in parentheses. PTSDsum = PCL-5 sum score; IMP = Impulsivity factor; AUDIT = Alcohol use; CUDIT = Cannabis use; NegUrg = Negative Urgency, PosUrg = Positive Urgency, PreMed = Lack of Premeditation. Persev = Lack of Perseverence. Model fit was acceptable: Panel A: χ2(30) = 88.725, p < .001; CFI = .974; RMSEA = .045; SRMR = .022. *p < .05; **p < .01; *** p < .001.
A second indirect effects model examined each of the UPPS-P subscales (except Sensation Seeking) as unique mediators (see Figure 1b). Full statistical results of this model are provided in supplementary materials (Table S5). Briefly, this model had similar model fit as the latent factor model. In this model, the only statistically significant indirect effects were observed for Positive Urgency as a mediator of the association between PTSD symptoms and AUDIT (α x β = .05, p < .001) and CUDIT-R (α x β = .03, p < .001).
Discussion
The current study examined the associations between PTSD symptoms, impulsivity, and problematic substance use in a sample of trauma-exposed U.S. adults. Consistent with previous research, individuals who met probable diagnostic criteria for PTSD reported more symptoms of problematic substance use and displayed higher levels of trait and choice-based impulsivity as compared to trauma-exposed participants who did not meet criteria for current PTSD. To our knowledge, this is the first study to examine multiple forms of impulsivity as potential mediators between PTSD symptoms and substance use. Our results indicated that impulsive personality traits on the UPPS-P measure partially mediated the association between PTSD and alcohol and cannabis use. This may indicate that among individuals exposed to traumatic events, lower levels of impulsivity may buffer against engagement in substance use, although a number of important considerations discussed below must be taken into account when interpreting our results.
Findings from the current study are well-aligned with those of previous work. Greater impulsive personality traits in the probably PTSD group is in line with the findings of Roley et al. (2017) who found that trait impulsivity accounted for PTSD’s arousal symptoms, and of Tull et al. (2016) who found that individuals with PTSD were more likely to engage in impulsive and risky behaviours such as substance misuse, non-suicidal self-injury, and risky sexual behaviour. Moreover, the PTSD group in the current study reported significantly higher scores on both the AUDIT and CUDIT-R relative to the trauma-exposed non-PTSD group, indicating greater use of and associated problems with alcohol and cannabis. Several prior studies have reported that persons with SUD have co-occurring PTSD in 30–60% of cases (Back et al., 2000; Brady et al., 2004; McCauley et al., 2012; Triffleman, Marmar, Delucchi, & Ronfeldt, 1995). Moreover, a national study by Pietrzak et al. (2011) found that 46% of respondents who met criteria for PTSD also met criteria for a SUD (Pietrzak et al., 2011).
A unique contribution of the current study is the use of a indirect effects model examining whether impulsivity mediates the association between PTSD symptoms and substance use. Although impulsivity, PTSD, and substance use have been recognized as interrelated (Mills et al., 2006; Pietrzak et al., 2011), the use of indirect effects models to examine the association between these three variables has been relatively scarce. Contractor et al. (2016) found that anger mediated the association between PTSD and impulsivity, and Weiss et al. (2013) found that emotion dysregulation mediated the association between PTSD and impulsive behaviors. However, neither of these studies examined substance use as an outcome. Our results indicated that impulsive personality traits on the UPPS-P partially mediated the association between PTSD and both cannabis and alcohol use. The follow-up model indicated that this result was largely driven by mediation by Positive Urgency. Importantly, due to the cross-sectional nature of these data, we cannot definitively infer directionality of the association. Therefore, we are unable to make the causal conslusion that PTSD symptoms lead to greater impulsivity, which in turn leads to engagement in alcohol and cannabis use. Moreover, we acknowledge that this sample reported relatively low levels of alcohol and cannabis use, given that the study did not specifically recruit substance users, thus we cannot say for certain whether or not these results would have been different had the sample been selected based on substance use. Nonetheless, the present findings suggest that impulsive traits are an important mediating factor in the association between PTSD and problematic alcohol and cannabis use.
Another notable finding from the current study was that the PTSD group exhibited significantly steeper delay discounting of monetary rewards compared to the trauma-exposed non-PTSD group. This significant difference is important given the relatively limited research on delay discounting among people with PTSD. In a recent meta-analysis of delay discounting in psychiatric disorders, Amlung et al. (2019) were unable to identify a sufficient number of studies to include PTSD as a disorder category and emphasized this as a priority area for research. The limited studies that have been conducted suggest that individuals who have experienced trauma prefer immediate smaller rewards to larger delayed rewards (Simmen-Janevska et al., 2015; Van Den Berk-Clark et al., 2018), and that history of abuse and lower self-efficacy significantly predict steeper delay discounting (Simmen-Janevska et al., 2015). Together with the current findings, this growing body of research suggests that only trauma-exposed individuals who go on to develop probable PTSD may be the ones who exhibit an increased immediate reward bias as evidenced by a decreased willingness to wait for delayed rewards. Nonetheless, the indirect effect model with delay discounting as the mediator had poor model fit and we were not able to examine indirect effects involving delay discounting.
Taken together, the present findings suggest that some aspects of impulsivity are a salient mechanistic variable linking PTSD and substance use. This finding is consistent with work by Oshri et al., (2017) who examined the role of impulsivity, child abuse, and adult substance use in a longitudinal sample of youth and a cross-sectional sample of adults. Self-reported impulsivity traits among adolescents mediated the association between adverse childhood experiences and smoking and cannabis use during young adulthood. In the adult sample, they reported indirect links between child abuse and substance use via delay discounting and impulsivity traits. Although these results appear generally consistent with our results (with the exception of delay discounting), there are a variety of notable differences to note between the two studies. First, the Oshri et al. study specifically examined childhood abuse and neglect, whereas the current study examined participants who reported lifetime traumatic exposures that may not be specific to childhood and PTSD symptoms in adulthood. Second, the measures used to assess participants’ substance use differed across studies (focusing on frequency only vs frequency and associated problems). Lastly, the measure of delay discounting differed, with Oshri et al. (2017) using the Monetary Choice Questionnaire (MCQ; Kirby, Petry, & Bickel, 1999) and the current study using the 5-Choice Delay Discounting Measure (Koffarnus & Bickel, 2014). Differences in reward magnitudes and delays between measures may have contributed to differing results.
Findings from the current study should be considered alongside several important limitations. First, these data were collected online using Amazon MTurk. Although we included a number of data quality measures in order to ensure our data were as valid as possible (e.g., prior approval ratings, IP address tracking), we acknowledge that MTurk samples may be prone to low effort or computerized “bot” responses. Unfortunately, we did not administer attention checks used in many MTurk studies, but the high internal consistency of responses on the clinical scales (αs > .90) increases our confidence in the data. Second, MTurk workers tend to be older, more educated, less religious, and more likely to be unemployed (Buhrmester, Kwang, & Gosling, 2011; Goodman, Cryder, & Amar, 2013). Moreover, although evenly our sample was balanced between sex and income, the participants were mostly Caucasian, so our results may not generalize to the general population. Third, trauma exposure and PTSD symptoms were determined via self-report scales, and we acknowledge that these measures need to be assessed in conjunction with a clinical interview to provide a diagnosis of PTSD. Although a cutoff of 33 on the PCL-5 is well-established, clinical levels of PTSD may be more consistent with a higher cutoff (e.g., 50+). Although our study sample was not designed to examine a clinical 50+ cutoff (i.e., only 144 participants exceeded this level), exploratory analysis did reveal similar results when this cutoff was used. Finally, the different assessment time windows for the BTQ and the PCL-5 are a notable limitation in the current study. Given that the BTQ assesses lifetime history and the PCL-5 assesses PTSD symptoms over the past month, there is a chance that participants may have reported fewer symptoms on the PCL-5 due to the narrow timeframe of the scale. We are also not able to confirm that the symptoms reported on the PCL-5 were related to specific traumatic events on the BTQ. Thus, it is important to recognize that our assessment of PTSD symptoms considered current (or very recent) symptoms only, and that there might have been participants in the ‘non-PTSD’ group who had a history of PTSD symptoms.
In conclusion, the novel finding that impulsivity mediates the association between PTSD and substance use lays a foundation for further work using longitudinal designs to examine the temporal association between these three factors. The use of advanced statistical methods in order to distinguish directionality amongst various constructs, including impulsivity, is of particular importance based on the need to address and target impulsivity in prevention and treatment efforts (Chamorroa et al., 2012). If replicated in a more diverse, clinical sample, these results could also have important clinical implications. First, a growing body of literature suggests that impulsivity is a transdiagnostic and multifaceted construct responsible for numerous adverse outcomes, risky behaviours, and psychiatric disorders (Amlung et al., 2019; Chamorroa et al., 2012; Griffin, Lynam, & Douglas, 2018). Utilizing brief assessments of delay discounting or impulsivity at intake may identify clients with PTSD who are more prone to engaging in problematic levels substance use. Conversely, the findings are generally consistent with the idea that lower levels of impulsivity in people with PTSD may be a protective factor for substance-related problems, although prospective studies are necessary to test this hypothesis. From a case-conceptualization intervention perspective, a thorough examination of impulsive urges and behaviours at the outset of treatment may inform specific targets in the course of PTSD treatment. Among those with heightened impulsivity, psychoeducation at the beginning of PTSD treatment and ongoing querying around potential use of substances throughout therapy may be indicated. Second, this study also suggests that impulsive behaviours in the context of heightened positive emotions (i.e., positive urgency) appear to be a particularly salient factor, and finding ways for clients to be more aware of and regulate their emotional and behavioural responses in these situations may reduce negative outcomes from substance use. Inclusion of tools that target motivation, awareness of urges and emotions, and problem solving of heightened emotionality from existing treatment modalities such as Acceptance and Commitment Therapy and Dialectical Behaviour Therapy has been shown to be useful among individuals with substance use (e.g., Stotts & Northrup, 2015), and clinicians may consider using these strategies to better support their patients. Finally, developing strategies to decrease impulsivity—such as episodic future thinking or executive function training (e.g., Koffarnus, Jarmolowicz, Mueller, & Bickel, 2013)—may prove to be a critical treatment target to offset the risks of problematic substance use among individuals with PTSD.
Supplementary Material
Clinical Impact Statement:
This study found that participants with higher PTSD symptoms made more impulsive decisions (delay discounting) and reported more impulsive traits than participants in the trauma-exposed non-PTSD group. Moreover, the PTSD group also reported significantly higher scores on both the alcohol and cannabis use measures. Lastly, impulsive personality traits were found to partially account for the association between PTSD symptoms and both cannabis and alcohol use. These results highlight 1) the need to address impulsivity in patients with comorbid substance use disorders and histories of trauma, and 2) impulsivity as a possible protective factor in the progression of trauma to PTSD.
Funding Support and Acknowledgements:
This research was supported by the Peter Boris Centre for Addictions Research and the Michael G. DeGroote Centre for Medicinal Cannabis Research at McMaster University and St. Joseph’s Healthcare Hamilton. The authors recognize and acknowledge that the land on which this work was completed is the traditional territory of the Mississauga and Haudenosaunee nations, and within the lands protected by the “Dish With One Spoon” wampum agreement. Dr. McKinnon is supported by the Homewood Chair in Mental Health and Trauma. Her research program is supported by the Canadian Institutes of Health Research, Department of National Defence, Canadian Institute for Military and Veteran Health Research, the Military Casualty Support Foundation, the Cowan Foundation, and the Homewood Research Institute. Dr. Oshri was partially supported by NIDA (5K01DA045219–02). Dr. Holshausen’s research program is supported by the Canadian Institutes of Health Research and the Research Institute of St. Joe’s.
References
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, & Sellman JD (2010). An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and Alcohol Dependence, 110(1–2), 137–143. 10.1016/j.drugalcdep.2010.02.017 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Amlung M, & MacKillop J (2014). Clarifying the relationship between impulsive delay discounting and nicotine dependence. Psychology of Addictive Behaviors, 28(3), 761–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, Marsden E, Holshausen K, Morris V, Patel H, Vedelago L, … McCabe R (2019). Delay Discounting as a Transdiagnostic Process in Psychiatric Disorders: A Meta-analysis. JAMA Psychiatry. 10.1001/jamapsychiatry.2019.2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung Michael, Vedelago L, Acker J, Balodis I, & MacKillop J (2017). Steep delay discounting and addictive behavior: a meta-analysis of continuous associations. Addiction, 112(1), 51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, & Brady KT (2000). Cocaine Dependence with and without Post-traumatic Stress Disorder: A Comparison of Substance Use, Trauma History and Psychiatric Comorbidity. American Journal on Addictions, 9(1), 51–62. 10.1080/10550490050172227 [DOI] [PubMed] [Google Scholar]
- Brady KT, Back Sudie E., & Coffey S (2004). Substance Abuse and Posttraumatic Stress Disorder. Current Directions in Psychological Science, 13(5), 206–209. 10.1111/j.0963-7214.2004.00309.x [DOI] [Google Scholar]
- Brown PJ, Stout RL, & Mueller T (1996). Posttraumatic Stress Disorder and Substance Abuse Relapse Among Women: A Pilot Study. Psychology of Addictive Behaviors, 10(2), 124–128. [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspectives on Psychological Science, 6(1), 3–5. [DOI] [PubMed] [Google Scholar]
- Chamorroa J, Bernardia S, Potenzab MN, Grante JE, Marsha R, Wanga S, & Carlos B (2012). Impulsivity in the general population: A national study, 46(8), 994–1001. 10.1016/j.jpsychires.2012.04.023.Impulsivity [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Armour C, Forbes D, & Elhai JD (2016). Posttraumatic stress disorder’s underlying dimensions and their relation with impulsivity facets. Journal of Nervous and Mental Disease, 204(1), 20–25. 10.1097/NMD.0000000000000417 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Dranger P, Ruggero C, & Armour C (2017). PTSD’s risky behavior criterion: Relation with DSM-5 PTSD symptom clusters and psychopathology. Psychiatry Research, 252, 215–222. 10.1016/j.psychres.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors, 39(9), 1372–1376. 10.1016/j.addbeh.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelmann JB, Maciuba B, Vaughan C, Paulus MP, & Dunlop BW (2013). Posttraumatic Stress Disorder Increases Sensitivity to Long Term Losses among Patients with Major Depressive Disorder. PLoS ONE, 8(10), 1–13. 10.1371/journal.pone.0078292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen N, Havermans R, Tekelenburg M, & Jansen A (2012). Prevalence of post-traumatic stress disorder among patients with substance use disorder: it is higher than clinicians think it is. European Journal of Psychotraumatology, 3(1), 17734. 10.3402/ejpt.v3i0.17734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman J, Cryder C, & Amar C (2013). Data Collection in a Flat World : The Strengths and Weaknesses of Mechanical Data Collection in a Flat World : The Strengths and Weaknesses of Mechanical. Journal of Behavioral Decision Making, 26, 213–224. 10.1002/bdm.1753 [DOI] [Google Scholar]
- Grant JE, & Chamberlain SR (2014). Impulsive action and impulsive choice across substance and behavioral addictions: Cause or consequence? Addictive Behaviors, 39(11), 1632–1639. 10.1016/j.addbeh.2014.04.022 [DOI] [PubMed] [Google Scholar]
- Griffin S, Lynam DR, & Douglas S (2018). Dimensional conceptualizations of impulsivity. Personality Disorders: Theory, Research, and Treatment, 9(4), 333–345. [DOI] [PubMed] [Google Scholar]
- Haller M, & Chassin L (2014). Risk Pathways Among Traumatic Stress, Posttraumatic Stress Disorder Symptoms, and Alcohol and Drug Problems: A Test of Four Hypotheses. Psychology of Addictive Behaviors, 28(3), 841–851. 10.1037/a0035878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen L, Southwick S, & Kosten T (2001). Substance Use Disorders in Patients With Posttraumatic Stress Disorder: A Review of the Literature. American Journal of Psychiatry, 158(8), 1184–1190. 10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- James LM, Strom TQ, & Leskela J (2014). Risk-Taking Behaviors and Impulsivity Among Veterans With and Without PTSD and Mild TBI. Military Medicine, 179(4), 357–363. 10.7205/MILMED-D-13-00241 [DOI] [PubMed] [Google Scholar]
- Kachadourian LK, Mccarthy E, & Petrakis IL (2016). Alcohol Use Disorders and Comorbid Post-Traumatic Stress Disorder in US Military Veterans: Etiology and Current Treatment Approaches. In Martin CR, Preedy VR, & Patel VB (Eds.), Comprehensive Guide to Post-Traumatic Stress Disorders (pp. 627–642). Cham: Springer. 10.1007/978-3-319-08359-9_108 [DOI] [Google Scholar]
- Kirby KN, Petry NM, & Bickel WK (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128(1), 78–87. Journal Article. 10.1037/0096-3445.128.1.78 [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, & Bickel WK (2014). A 5-trial adjusting delay discounting task: Accurate discount rates in less than one minute. Experimental and Clinical Psychopharmacology, 22(3), 222–228. 10.1037/a0035973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Jarmolowicz DP, Mueller ET, & Bickel WK (2013). Changing delay discounting in the light of the competing neurobehavioral decision systems theory: a review. Journal of the Experimental Analysis of Behavior, 99(1), 32–57. 10.1002/jeab.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The Patient Health Questionnaire-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. 10.1097/01.mlr.0000093487.78664.3c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JZ, Li S, & Liu H (2011). How has the Wenchuan earthquake influenced people’s intertemporal choices? Journal of Applied Social Psychology, 41(11), 2739–2752. 10.1111/j.1559-1816.2011.00847.x [DOI] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, & Munafò MR (2011). Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology, 216(3), 305–321. 10.1007/s00213-011-2229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Weafer J, Gray J, Oshri A, Palmer A, & de Wit H (2016). The Latent Structure of Impulsivity: Impulsive Choice, Impulsive Action, and Impulsive Personality Traits. Psychopharmacology, 233(18), 3361–3370. 10.1183/09031936.00063810.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley J, Killeen T, Gros D, Brady K, & Back S (2012). Posttraumatic Stress Disorder and Co-Occurring Substance Use Disorders: Advances in Assessment and Treatment. Clin Psychol (New York), 19(3). 10.1111/cpsp.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills KL, Sc BH, Teesson M, Ph D, Ross J, Ph D, … Ph D (2006). Trauma, PTSD, and Substance Use Disorders : Findings, (April), 652–658. [DOI] [PubMed] [Google Scholar]
- Mirhashem R, Allen HC, Adams ZW, van Stolk-Cooke K, Legrand A, & Price M (2017). The intervening role of urgency on the association between childhood maltreatment, PTSD, and substance-related problems. Addictive Behaviors, 69, 98–103. 10.1016/j.addbeh.2017.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2011). Mplus user’s guide, sixth edition. Los Angeles, CA: Authors. [Google Scholar]
- Nemeroff CB, Bremner JD, Foa EB, Mayberg HS, North CS, & Stein MB (2006). Posttraumatic stress disorder: A state-of-the-science review. Journal of Psychiatric Research, 40(1), 1–21. 10.1016/j.jpsychires.2005.07.005 [DOI] [PubMed] [Google Scholar]
- Oshri A, Kogan SM, Kwon JA, Wickrama KAS, Vanderbroek L, Palmer AA, & MacKillop J (2017). Impulsivity as a mechanism linking child abuse and neglect with substance use in adolescence and adulthood. Development and Psychopathology, 30(2), 417–435. 10.1017/S0954579417000943 [DOI] [PubMed] [Google Scholar]
- Perry JL, & Carroll ME (2008). The role of impulsive behavior in drug abuse. Psychopharmacology, 200, 1–26. 10.1007/s00213-008-1173-0 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I Comorbidity of Full and Partial Posttraumatic Stress Disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roley ME, Contractor AA, Weiss NH, Armour C, & Elhai JD (2013). Impulsivity facets’ predictive relations with DSM-5 PTSD symptom clusters. Journal of Thoracic Oncology, 8(1), S89. 10.1097/01.JTO.0000438438.14562.c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roley ME, Contractor AA, Weiss NH, Armour C, & Elhai JD (2017). Impulsivity facets’ predictive relations with DSM-5 PTSD symptom clusters., 9(1), 76–79. 10.1037/tra0000146.Impulsivity [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. II. Addiction, 88, 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schäfer I, & Najavits LM (2007). Clinical Challenges in the Treatment of Patients with PTSD and Substance Abuse. Current Opinion in Psychiatry, 20(6), 614–618. [DOI] [PubMed] [Google Scholar]
- Simmen-Janevska K, Forstmeier S, Krammer S, & Maercker A (2015). Does Trauma Impair Self-Control? Differences in Delaying Gratification Between Former Indentured Child Laborers and Nontraumatized Controls. Violence and Victims, 30(6), 1068–1081. 10.1891/0886-6708.vv-d-13-00174 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A Brief Measure for Assessing Generalized Anxiety Disorder. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Stotts A, & Northrup T (2015). The Promise of Third-Wave Behavioral Therapies in the Treatment of Substance Use Disorders. Current Opin Psychol, 176(3), 75–81. 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triffleman EG, Marmar CR, Delucchi KL, & Ronfeldt H (1995). Childhood trauma and posttraumatic stress disorder in substance abuse inpatients. Journal of Nervous and Mental Disease, 183(3), 172–176. [DOI] [PubMed] [Google Scholar]
- Tull MT, Weiss NH, & Mcdermott MJ (2016). Post-Traumatic Stress Disorder and Impulsive and Risky Behavior: Overview and Discussion of Potential Mechanisms. In Martin CR, Preedy VR, & Patel VB (Eds.), Comprehensive Guide to Post-Traumatic Stress Disorders (pp. 803–816). Cham: Springer. 10.1007/978-3-319-08359-9_16 [DOI] [Google Scholar]
- Van Ameringen M, Mancini C, Patterson B, & Boyle MH (2008). Post-Traumatic Stress Disorder in Canada. CNS Neuroscience & Therapeutics, 14(5), 171–181. 10.1016/j.optm.2009.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Berk-Clark C, Myerson J, Green L, & Grucza RA (2018). Past trauma and future choices: Differences in discounting in low-income, urban African Americans. Psychological Medicine, 48(16), 2702–2709. 10.1017/S0033291718000326 [DOI] [PubMed] [Google Scholar]
- VanderBroek-Stice L, Stojek MK, Beach SRH, & MacKillop J (2017). Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite, 112, 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128(1–2), 45–51. 10.1016/j.drugalcdep.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. 10.1016/S0191-8869(00)00064-7 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


