Highlights
-
•
Compared to sedentary virtual reality (SVR), active virtual reality (AVR) induces higher heart rate and more moderate-to-vigorous physical activity.
-
•
Compared to SVR, AVR elicits greater sensory and imaginative immersion, challenge, and positive affect.
-
•
AVR elicits a marginally higher recognition score in a recognition memory test than does SVR.
-
•
Motion sickness is low in both SVR and AVR.
-
•
Virtual reality has the potential to improve both moderate-to-vigorous physical activity and cognitive health.
Keywords: Active video game, Cognitive performance, Mnemonic similarity test, MVPA, Virtual reality
Abstract
Background
Active video games are a new method for increasing physical activity (PA). Fully immersive virtual reality (VR) is a hardware device on which an active video game can run. Active (video games in) VR (AVR), might increase immersion, game engagement, and moderate-to-vigorous PA (MVPA), thereby yielding greater exercise-related benefits, e.g., cognitive performance.
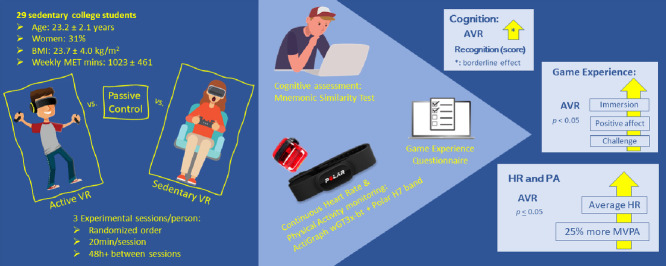
Methods
We examined the induction of MVPA via an AVR and a sedentary VR (SVR) as well as the effects of VR play on cognitive performance, which was monitored using 2 different methods. Each of 29 sedentary college students attended three 20-min laboratory sessions (AVR, SVR, or control) in a randomized order; during the control session, they sat quietly doing nothing. A fully immersive headset was used for the 2 video game sessions. We monitored and computed participants’ PA using hip-worn accelerometers (wGT3x-bt; ActiGraph, Pensacola, FL, USA) and a heart rate band (Polar H7; Polar, Kempele, Finland). After each session, the participants completed a mnemonic similarity test (MST) to measure recognition memory. They also filled out a motion sickness questionnaire and an abbreviated game experience questionnaire.
Results
The AVR session induced a significantly greater heart rate and more time spent in MVPA than did either of the other 2 sessions regardless of the PA monitoring method. AVR elicited greater game experience questionnaire-assessed sensory and imaginative immersion, challenge, and positive affect than did SVR. The mnemonic similarity test recognition score was marginally higher post-AVR session than it was post-SVR session.
Conclusion
AVR elicited MVPA without a significant increase in motion sickness and induced a better game experience and better borderline cognitive performance than did SVR.
Graphical abstract
1. Introduction
An insufficient level of physical activity (PA) is a major contributor to multiple non-communicable diseases, including type 2 diabetes, obesity, and cardiovascular disease.1 Researches have shown that active video games (AVGs) may induce moderate-to-vigorous PA (MVPA) in adults and children.2 Current U.S. PA guidelines recommend at least 150–300 min/week of moderate-intensity or 75–150 min/week of vigorous-intensity aerobic PA,3 yet few individuals meet this guideline.4 Sedentary behavior and low levels of PA are prevalent in college students due to class attendance and study sessions at the library as well as screen media engagement (i.e., smartphones, video games, or computers).5,6 Low PA and high sedentary behavior earlier in adulthood are strong determinants of the same behaviors in later life, along with an increased likelihood of cardiovascular disease.7 Therefore, identification of strategies to increase MVPA in the young adult population is crucial.
AVG constitutes an important option in terms of exercise and eliciting MVPA. This is especially true in times of social isolation, such as the current coronavirus disease 2019 pandemic, during which more traditional methods for increasing PA (i.e., outdoor running, resistance exercise in the gym, in-person yoga classes, and indoor cycling) are unavailable or represent an additional risk of infection. Additionally, compared to conventional methods of inducing PA, AVG elicits higher levels of motivation and engagement.8 For instance, well-designed video games can create a sense of flow and immersion by incorporating important parts of game engagement, such as discovery, role playing, mastery, and control.9,10 These aspects, along with AVG-elicited feelings of competence, autonomy, and immersion, are key contributors to a greater motivation to play video games.8,10 During the last 2 decades, AVGs have evolved rapidly, and the recent development of virtual reality (VR) provides a novel platform for active gaming.11 An immersive VR headset with image and sound input entirely cocoons the user within a computer-generated world.12 VR can be AVR, which requires lower-, upper-, or whole-body movements, or sedentary VR (SVR), which requires only finger movements. These are likely to result in different levels of PA. Also, a VR setting may yield a better player game experience than the non-VR setting,13 i.e., its use has been found to elicit greater immersion, flow, positive affect, and empathy while lowering negative affect.13 These aspects could help increase game engagement and, for players using AVR, time spent in MVPA.
A fully immersive VR (3-dimensional VR) is an immersive display device for individual immersion.14 When immersed in a VR environment, the player can interact in real-time with objects and avatars.14 With AVR, this complete immersion might produce motion sickness because of the mismatch between an individual's visual and vestibular systems.15 Research found that adults using fully immersive VR are at increased risk of experiencing motion sickness due to increased postural instability.16 In such cases, the motion required to play the AVG in VR may lead to decreased game engagement.17
Hip-worn accelerometers,18, 19, 20 the recommended method for assessing PA in free-living conditions,21 are frequently employed in studies of AVG-induced MVPA.22 Due to the lack of uniform AVG requirements for body movements and player body-movement types, additional physiological measurement methods (e.g., heart rate) should be considered when evaluating activity elicited by AVG play. Using multiple sensing measurement methodologies may improve the validity of MVPA measurement during AVG play,23 especially in a VR environment.
Researchers have demonstrated that a single AVG play session elicited cognitive benefits in healthy adults24 and children.25 Cognition is defined as the actions of the brain involved in understanding and functioning in an external environment.26 While cognitive performance has been shown to predict real-world functionality and occupational performance,27 it naturally decreases across the lifespan of an individual and is associated with several age-related co-morbidities.28 Thus, activities that acutely boost cognition, such as AVG play, may attenuate the natural age-related cognitive decline in children and young adults, thereby preventing it in older adults.29 Reports of comparisons of the effects of AVG, sedentary games, and treadmill exercise indicate that AVG elicits benefits for focus and concentration that are similar to those of treadmill exercise but with lower exertion levels and a higher perception of fun.24 A substantial body of literature indicates that exercise can elicit cognitive improvement, possibly due to an increased heart rate as well as an increase in circulating catecholamines and brain-derived neurotrophic factor.30 Additionally, a comparison of the effects of a desktop game vs. immersive SVR indicated that only the latter elicited a greater amount of working memory.31 Thus, immersive VR coupled with exercise could result in a boost in cognitive performance.
We investigated the use of AVR as an MVPA inducer for sedentary college students and validated the outcomes using 2 methods of PA assessment. We also compared the cognitive performance effects of AVR vs. SVR in college students. We hypothesized that AVR would yield greater MVPA, regardless of the PA monitoring method, and greater cognitive benefits than either SVR or control. We examined the difference in motion sickness and game engagement as part of an exploratory analysis.
2. Methods
2.1. Ethical concerns
The Institutional Review Board at the Northeastern University approved our study.
2.2. Sample
We invited participants via web advertisements and posters displayed in common areas on campus and nearby areas. Inclusion criteria were: low levels of PA (weekly reported total PA metabolic equivalent of task (MET) minutes ≤ 1500 min as calculated using the International Physical Activity Questionnaire-Short Version);32 aged between 20 and 29 years; no cardiovascular, cerebrovascular, or neurological diseases, no attention disorders or physical disability; never used tobacco (as both its usage and deprivation impact cognitive function);33,34 English speaking; and never previously played the video games we used.
We recruited 306 students who indicated their interest by completing an online pre-screening questionnaire, including the International Physical Activity Questionnaire-Short Version.32 Most of these students were excluded due to reported high PA levels (weekly reported total PA MET minutes > 1500 min), leaving 66 who met our inclusion criteria and were invited to the initial screening and first visit. We sent ineligible responders a “thank-you” e-mail for their interest. Of the 66 students, 34 completed all 3 visits, of whom 5 were excluded due to invalid heart rate data (due to device misplacement or malfunction). Thus, our final sample size was 29 participants.
2.3. General procedures
During the first visit, participants signed a written informed consent and provided their demographic information via an online questionnaire. The research assistants measured their height and weight using a stadiometer (ShorrBoard, Weigh and Measure, LLC, Olney, MD, USA) and a calibrated scale (Seca GmbH, Hamburg, Germany). Three visits (AVR, SVR, and control session (CS)) were required of each participant and administered in random order based on Microsoft Excel's (Microsoft, Redmond, WA, USA) random list function. Each visit was scheduled, on average, between 96 h and 120 h apart.
During each session (AVR, SVR, and CS), participants were not allowed to use their mobile devices (smartphones, tablets, or laptops), perform any other activity, or fall asleep. We attached an accelerometer to their non-dominant hip (wGT3x-bt; ActiGraph, Pensacola, FL, USA) and an heart rate (HR) band (Polar H7; Polar, Kempele, Finland) to their chest. For AVR and SVR, participants first obtained instructions on how to play the game via a tutorial. They then performed one of the three 20-min session assignments by playing the AVR or SVR or by sitting quietly (CS). Next, participants completed an abbreviated version of the game experience questionnaire (GEQ).35 We then cognitively assessed them using the mnemonic similarity test (MST).36 Participants completing all 3 visits received a USD45.00 “thank-you” gift card.
2.4. AVR and SVR
For both AVR and SVR sessions, we used the Vive Pro system (HTC, New Taipei, Taiwan, China). The Vive Pro headset features high-resolution displays at 1440 × 1600 resolution per eye, along with a second outward-facing camera, attachable headphones, a microphone for noise cancellation analysis, and a wireless adapter for untethered play. They are lightweight (803 g) and have a sizing dial.
In the AVR session, participants played Beat Saber,37 a rhythm-based AVG in which the participant uses virtual lightsabers (laser swords) to cut through blocks (upper-body movement) or to evade large blocks by moving to either side or crouching (whole-body movement). The blocks move in the player's direction according to the rhythm of the song being played in the background. Since all participants played Beat Saber for the first time in our study, we created a song list that began with an easier song to ensure the participants could better understand the game flow as well as the game instructions. The difficulty gradually increased with each subsequent song. The playlist was as follows: USD100; Country Roads; Escape; Beat Saber; Level Insane; Turn Me On; Elixia; Commercial Pumping; Unlimited Power; and Balearic Pumping.
In the SVR session, participants played Thumper,38 another rhythmic game in which players guide their character and hit “notes” in synchrony with background music. In this game, players use an Xbox One controller (Microsoft, Redmond, WA, USA) while seated and are only required to move their fingers.
Although Beat Saber and Thumper are both rhythm games and share similar visual characteristics and audio styles, they differ significantly in the amount of PA required to play them.
During the CS, the participant remained seated without any task.
2.5. PA assessment
ActiGraph accelerometer devices are widely used to assess individual levels of PA in children and young adults.39, 40, 41 In this study, we attached an ActiGraph GT3x-bt (ActiGraph) to each participant's non-dominant hip and initialized the device at a 30-Hz sampling rate. The ActiGraph triaxial accelerometers (ActiGraph) assessed PA by providing measures of acceleration from the subject's movement in 3 individual axes (anterior–posterior, vertical, and medial–lateral). With these measures we were able to obtain the frequency, duration, and intensity of their physical movement.23
We also attached a Polar HR band (Polar) to each participant's chest behind a privacy curtain. We used heart rate measurements only as a measure of the intensity of PA,23 including the linear and proportionate increase corresponding to more intense movement.42
We downloaded the activity monitor data via ActiLife software (Version 6.13.2; ActiGraph, Pensacola, FL, USA) and converted it into a triaxial form for activity counts in order to quantify the amplitude and frequency of detected accelerations at a 1-s epoch. A 1-s epoch is the most appropriate epoch length to detect short bursts of intense PA and may be the best choice for examinations of intermittent PA.40 We also used the ActiLife software (Version 6.13.3; ActiGraph) to download the HR measurement data, which we analyzed at 1-min intervals.
We used the following cut-off points to estimate the time spent in light, moderate, and vigorous PA according to the hip accelerometers: light, <760 counts/min; moderate, = 760–5724 counts/min; and vigorous, >5724 counts/min.43 We estimated HR-based MVPA using the maximum HR (HRmax) together with the relative HR intensity cut-offs set by the American College of Sports Medicine: light PA <64% HRmax; moderate PA = 64%–76% HRmax; and vigorous PA >76% HRmax.44
2.6. Motion sickness and GEQ
In the AVR and SVR sessions, we asked participants to complete an abbreviated version of the GEQ, in-game GEQ,35 and a motion sickness questionnaire.45 The motion sickness questionnaire is a 15-item, 10-point Likert-style scale (0 = not at all; 9 = severely). Sample items included “I felt sick to my stomach”, “I felt queasy”, and “I felt dizzy”.
We used the in-game GEQ35 to minimize participant burden while obtaining as much information as we could. The original GEQ contained 33 items, measuring 7 components of the game experience, including immersion and flow; more specifically, immersion was measured with 6 items and flow was measured with 5 items in this version of the GEQ. The in-game GEQ, however, only contained 14 items, with 2 items measuring each of the 7 components. Since immersion and flow are highly relevant to our project's scope and also represent the core definition of VR,14 we decided to use the full measure of these 2 components from the original GEQ Module by including the 4 items for immersion and 3 items for flow that had been omitted from the in-game GEQ. To report their gaming experience, participants responded to our 21-item questionnaire; each item had a 5-point Likert-style scale response (0 = not at all; 4 = extremely). This information was used to assess competence, sensory and imaginative immersion, flow, tension, challenge, and positive and negative affect.
Sample items for immersion included “It was aesthetically pleasing”, “I felt imaginative”, “I felt that I could explore things”, and “It felt like a rich experience”. Sample items for flow included “I lost track of time”, “I was deeply concentrated in the game”, and “I lost connection with the outside world”.
2.7. MST
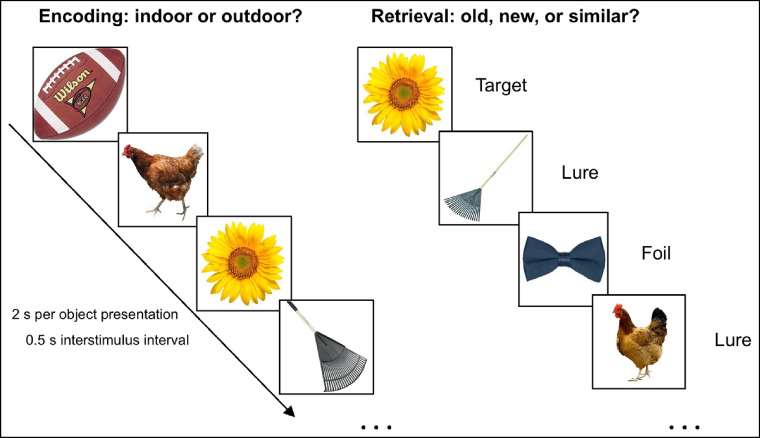
The MST is a robust behavioral measure of recognition (REC) memory with strong demands on pattern separation processes; it has been used in various populations across the lifespan.46, 47, 48, 49 The MST task assesses REC memory performance for objects using the traditional targets and unrelated foils plus similar lures varied along several dimensions.50 PA, especially MVPA, has been found to improve respondents’ MST performance.51
Each MST testing session took about 15 min to complete in 2 phases during each of the 3 visits: encoding and retrieval (Fig. 1). In the encoding phase, the participants classified each item in a sequence of 128 objects to be indoor or outdoor (2 s per object presentation with 0.5 s interstimulus interval). There was no right or wrong answer in this phase. In the retrieval phase, the participants classified each item in a sequence of 192 objects to be old, new, or similar. Of the 192 objects, 64 were items seen in the encoding phase (target), 64 were similar to items seen in the encoding phase (lure), and 64 were new objects (foil). All object images were randomly selected from the MST Image Set F (https://faculty.sites.uci.edu/starklab/mnemonic-similarity-task-mst/), which was a recent expansion of the original sets with better graphic quality and ease of application.50
Fig. 1.
Mnemonic similarity test.
The raw data from each of the sessions are present in Table 1. From the raw MST data, we derived the Lure Discrimination Index as the difference between the rate of “similar” responses for the lure items minus “similar” responses for the foils (to correct for any response biases). We calculated the REC for repeat items as the difference between the rate of “old” responses for target items minus “old” responses for the foils.36
Table. 1.
Raw data of MST after each session (n = 29) (mean ± SD).
| MST object |
||||
|---|---|---|---|---|
| Session | Target | Lure | Foil | |
| AVR | Old | 0.81 ± 0.18 | 0.33 ± 0.14 | 0.09 ± 0.16 |
| Similar | 0.13 ± 0.10 | 0.56 ± 0.18 | 0.27 ± 0.17 | |
| New | 0.06 ± 0.12 | 0.09 ± 0.09 | 0.65 ± 0.19 | |
| SVR | Old | 0.67 ± 0.28 | 0.27 ± 0.16 | 0.07 ± 0.14 |
| Similar | 0.16 ± 0.10 | 0.53 ± 0.21 | 0.20 ± 0.14 | |
| New | 0.15 ± 0.23 | 0.18 ± 0.20 | 0.66 ± 0.22 | |
| Control | Old | 0.78 ± 0.21 | 0.31 ± 0.17 | 0.09 ± 0.19 |
| Similar | 0.14 ± 0.10 | 0.55 ± 0.21 | 0.22 ± 0.16 | |
| New | 0.07 ± 0.16 | 0.12 ± 0.14 | 0.64 ± 0.23 | |
Abbreviations: AVR = active virtual reality; MST = mnemonic similarity test; SVR = sedentary virtual reality.
2.8. Statistical analysis
All data are expressed as mean ± SD. All GEQ-derived variables were scored and analyzed per the developer's recommendation.35 Immersion (Cronbach's α > 0.79), flow (Cronbach's α > 0.85), and motion sickness (Cronbach's α > 0.95) were calculated by averaging their respective items (immersion: 6 items; flow: 5 items; motion sickness: 15 items). All other constructs (e.g., challenge, competence) were measured by 2 items each and averaged as suggested.35
We used a general linear model (GLM: two-way analysis of variance) with sessions (CS, SVR, and AVR) and methods (hip, HR) as random factors to analyze MVPA. We used repeated-measures analysis of variance to determine whether there was a session effect on HR and MST scores. Bonferroni's post hoc was used to identify specific differences among the sessions.
Power calculations were conducted post hoc using G* Power (G*Power; Brunsbüttel, Germany),52 and all other statistical procedures were performed using SPSS (Version 26.0; IBM Corp., Armonk, NY, USA). Power calculations were then conducted using the actual sample size (n = 29) for the primary analysis (GLM with 2 random independent factors). Our estimates indicated sufficient power to detect an effect size of η2p = 0.5 (critical F = 2.24), and our analysis was assured of having a power of 90.3%. The significance level was set at p < 0.05.
3. Results
The average body mass index of the participants falls within the normal weight category (<25 kg/m2). All reported insufficient weekly MET to be considered physically active (Table 2).
Table 2.
Demographic and anthropometric characteristics of the sample (n = 29).
| Characteristic | % or mean ± SD |
|---|---|
| Gender | |
| Female | 31.0 |
| Male | 69.0 |
| Ethnicity | |
| Caucasian | 24.1 |
| Far East Asian | 13.8 |
| Hispanic or Latino | 6.9 |
| South Asian | 55.2 |
| Age (year) | 23.2 ± 2.1 |
| Height (cm) | 172.5 ± 8.7 |
| Weight (kg) | 70.4 ± 13.1 |
| BMI (kg/m2) | 23.7 ± 4.0 |
| Weekly MET (min) | 1023.3 ± 461.0 |
Abbreviations: BMI = body mass index; MET = metabolic equivalent of task.
The GLM for MVPA showed a significant method-effect (F = 48.9; p < 0.001), session-effect (F = 168.9; p < 0.001); and interaction effect of method × session (F = 37.7; p < 0.001). Post hoc analysis identified the AVR session as inducing higher MVPA than CS or SVR across the 2 PA assessment methods (Table 3). HR showed a significant session-effect (F = 29.1; p < 0.001) with higher values in the AVR session after a post hoc analysis (Table 3).
Table 3.
Time spent in MVPA and average HR assessed through hip-worn accelerometers and HR band (mean ± SD).
| Method | Session |
||
|---|---|---|---|
| Control session | Sedentary VR | Active VR | |
| MVPA-hip (min) | 0.00 ± 0.01 | 0.02 ± 0.08 | 4.10 ± 4.93** |
| MVPA-HR (min) | 0.09 ± 0.43 | 0.25 ± 1.30 | 5.67 ± 7.91** |
| HR (bpm) | 75.0 ± 11.3 | 77.4 ± 13.8 | 110.2 ± 21.5** |
** p < 0.001, different from the other 2 sessions.
Abbreviations: bpm = beats per minute; HR = heart rate; MVPA = moderate-to-vigorous physical activity; VR = virtual reality.
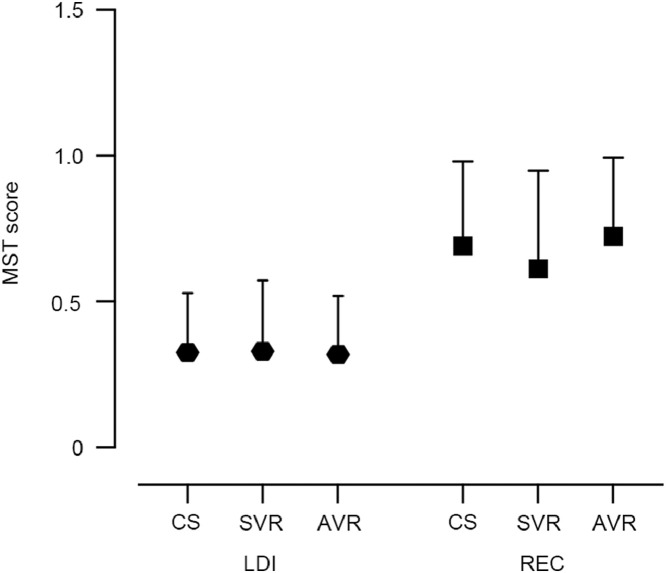
The GLM for the MST identified no significant session-effect for Lure Discrimination Index (F = 0.06; p = 0.909), and a trend session-effect for REC (F = 3.69; p = 0.057). A post hoc analysis for the REC showed a trend of higher scores following AVR than SVR (p = 0.084) (Fig. 2).
Fig. 2.
LDI and REC from the MST after CS, SVR, and AVR. Borderline session-effect for REC (p = 0.084). AVR = active virtual reality; CS = control session; LDI = Lure Discrimination Index; MST = mnemonic similarity test; REC = recognition; SVR = sedentary virtual reality.
The motion sickness scores were relatively low and not different between the AVR and SVR conditions. The GEQ scores showed significantly higher immersion (p < 0.05), challenge (p < 0.05), and positive affection for AVR than SVR (p < 0.01), with moderate-large effect sizes (Table 4).
Table 4.
Motion sickness, competence, sensory and imaginative immersion, flow, tension, challenge, positive affect, and negative affect after active and sedentary VR (mean ± SD).
| Questionnaire score | AVR | SVR | t | p | d |
|---|---|---|---|---|---|
| Motion sickness | 0.89 ± 1.29 | 0.81 ± 1.21 | 0.22 | 0.83 | 0.06 |
| Competence | 2.84 ± 0.79 | 2.75 ± 1.00 | 0.39 | 0.61 | 0.10 |
| Sensory and imaginative immersion | 3.26 ± 0.81 | 2.80 ± 0.95 | 2.62 | 0.01* | 0.52 |
| Flow | 3.58 ± 0.79 | 3.32 ± 0.99 | 1.31 | 0.20 | 0.29 |
| Tension | 1.36 ± 0.59 | 1.38 ± 0.72 | 0.13 | 0.90 | 0.03 |
| Challenge | 3.63 ± 0.66 | 3.04 ± 1.03 | 2.86 | 0.01* | 0.68 |
| Positive affect | 3.71 ± 0.70 | 2.86 ± 1.02 | 3.78 | <0.01** | 0.97 |
| Negative affect | 1.46 ± 0.68 | 1.59 ± 0.81 | 0.86 | 0.40 | 0.17 |
* p < 0.05; ** p < 0.01, compared with AVR and SVR groups.
Abbreviations: AVR = active virtual reality; SVR = sedentary virtual reality.
4. Discussion
We elicited MVPA via AVR among sedentary young adults without significantly increasing motion sickness. The within-subject design and inclusion of a control condition add to the robustness of the findings. AVR could thus be an alternative to traditional exercise methods intended to increase PA in young adults. AVR resulted in higher immersion, challenge, and positive affect than did SVR, although the game experiences did not seem to mediate the relationship between VR type and MVPA. AVR marginally increased the REC score from MST, whereas SVR did not.
Researchers have demonstrated that fully immersive VR can reduce pain scores as a distraction,53 increase knowledge retention as an educational method,54 and improve cardiovascular parameters as a method of exercise.55 We are among the first to demonstrate that a fully immersive AVR game can elicit MVPA in young adults with better game engagement in several dimensions and without significantly increasing motion sickness. Our results indicate that the time spent in MVPA represents around 40% of the total play time, a considerable portion (5–8 min out of 20-min play time). To induce health-related outcomes, it is recommended that an adult should engage in a minimum of 200 min of MVPA every week.56 Additional physical exercise activities might be needed to achieve weekly MVPA goals.
Although researchers have investigated AVG-induced MVPA in college students,57 research on PA via AVR is scarce. An investigation of the effect of a 15-min session of AVR exergame indicated that, regardless of age, gender, and PA level, AVR elicited high levels of perceived exertion and HR.19 An examination of HR during 2 types of AVR using an omni treadmill vs. a flight simulator indicated that the omni treadmill produced 80.6% of HRmax at the recommended PA guidelines.58 It is likely that VR with an enhanced technological interface could induce more intense PA via a more immersive experience.
Similar to previous researchers who found that a VR setting improves the player's experience more than a non-VR setting does,13 we found that an AVR elicits greater immersion, challenge, and positive affect than an SVR does. Immersive hardware with well-developed software may result in a better game experience.59,60 For AVR, this experience might yield increased play with more MVPA. AVR games eliciting a better game experience could benefit the users with PA-derived positive health outcomes beyond entertainment. While both VR sessions elicited some levels of challenge and immersion, the physical exercise component in the AVR may create another level of role playing and game goals, further increasing perceived immersion and challenge. The challenge construct in video games contains “goals” and “feedback”.61 Although the goal-setting can be utilized for behavioral change, its role in motivating exergame play remains unclear.62 The motion sickness measure produced relatively low scores across both game conditions. This could potentially alleviate some VR by-standers’ concerns.
Studies of time spent in MVPA during AVG play using multiple sensors are scarce. To our knowledge, no one has studied immersive VR. In one study, hip-worn accelerometers used to assess time spent in MVPA during two 20-min Xbox 360 AVG play sessions indicated an average of 10.7 min of MVPA—approximately 50% of playing time.57 MVPA, measured through hip-worn accelerometer and HR band, was estimated in 40%–50% of the play session, corroborating our findings.57 Another investigation of time spent in MVPA used wrist and hip accelerometers in a 30-min AVG play session on Xbox Kinect and reported 29.9 min vs. 30.0 min of MVPA, respectively.19 As the wrist accelerometer records accelerations of the forearm, indicating a large number of upper-body movements,63 this could lead to overestimated PA measures. That is, while hip-worn accelerometers may not record the upper-movements used in many AVGs, wrist-worn accelerometers may overestimate PA during AVG play. Thus, in addition to PA monitoring, physiological measures (e.g., HR, oxygen uptake) should be monitored during AVG sessions to better assess exercise intensity.
The effects of AVG on cognitive function are evident in older adults64 and children.25 The use of active games in AVR is scarce, and no one has investigated the use of immersive AVR to induce MVPA among young adults. Research indicates that immersive VR alone has the ability to boost cognitive performance in people with cognitive impairment.65,66 This is not reflected by our findings, which showed no difference between SVR and control. However, most studies that used non-exercising VR applications to improve cognition used a software package or specialized game developed for cognitive improvement in populations with cognitive deficit.65, 66, 67 Our study was conducted among young adults using a commercially available entertainment VR game that does not target cognitive improvement. Specifically, with regard to MST, researchers have demonstrated an age-related deficit in cognitive performance.36 This means that our young adults should have performed excellently on MST and, thus, created a ceiling effect from the beginning.
Nevertheless, AVR still elicited a borderline better REC score than CS or SVR. Physical fitness is associated with better baseline MST scores in young adults,68 though whether long-term AVR play can improve baseline MST scores remains to be studied. Additionally, our results show that the exercise component in AVR might contribute to its ability to elicit more significant cognitive improvement than SVR. These findings are in line with previous research indicating that an acute session of moderate exercise can improve cognitive performance.30 However, specifically regarding memory, the literature is not consistent with respect to positive exercise-induced effects.69,70
AVR and SVR games may elicit MVPA and cognitive benefits differently, but our evaluations were limited to one game of each type. Our study was conducted in a laboratory setting with a preset time limit and preselected games. Investigating VR gameplay in a free-living environment for players across the developmental span would afford better generalizability of similar evaluations along with clinically relevant outcomes. Future comparisons of the ability of different AVR games to affect MVPA and cognitive performance, and their potential long-term effects on players, should be conducted. Additionally, the fact that participants played different games in AVR and SVR sessions does not rule out the possibility that some of the game design characteristics, rather than PA, elicited the differing physiological and cognitive responses. Nevertheless, both are rhythm games with similar visual and audio style characteristics, leaving the active capacity as the key difference.
5. Conclusion
AVR feasibly elicits MVPA, which we validated through hip-worn accelerometers and HR monitors, without a significant increase in motion sickness. AVR also induced a better game experience and better borderline cognitive performance than did SVR in young adults. We hope our results may inform future fully powered explorations and well-developed interventions to maximize the potential physical and cognitive health benefits of fully immersive VR.
Acknowledgments
Acknowledgments
The authors thank the Health Technology Laboratory members, including Dar Alon for her help and effort with data collection and data preparation. This study was supported in part by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK109316, principle investigator: ASL), and by the College of Arts, Media, and Design, Bouvé College of Health Sciences at Northeastern University, Boston, MA, USA.
Authors’ contributions
CVS contributed to data collection, data analysis, interpretation of results, and wrote the first draft of the manuscript; JH participated in the design of the study and manuscript preparation; RCP, AF, AM, and KN participated in data collection and contributed to data preparation; ASL participated in the design of the study, supervised the study data collection, and contributed to data analysis, results interpretation, and manuscript preparation. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials
References
- 1.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. The Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peng W, Crouse JC, Lin JH. Using active video games for physical activity promotion: A systematic review of the current state of research. Health Educ Behav. 2013;40:171–192. doi: 10.1177/1090198112444956. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Available at: https://health.gov/our-work/physical-activity/current-guidelines. [accessed 18.03.2020]
- 4.Tucker JM, Welk GJ, Beyler NK. Physical activity in US adults: Compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40:454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Castro O, Bennie J, Vergeer I, Bosselut G, Biddle SJH. Correlates of sedentary behaviour in university students: A systematic review. Prev Med. 2018;116:194–202. doi: 10.1016/j.ypmed.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Vainshelboim B, Brennan GM, LoRusso S, Fitzgerald P, Wisniewski KS. Sedentary behavior and physiological health determinants in male and female college students. Physiol Behav. 2019;204:277–282. doi: 10.1016/j.physbeh.2019.02.041. [DOI] [PubMed] [Google Scholar]
- 7.Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior determinants and interventions. Am J Prev Med. 2011;41:189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 8.Staiano AE, Adams MA, Norman GJ. Motivation for exergame play inventory: Construct validity and relationship to game play. Cyberpsychology. 2019;13 doi: 10.5817/CP2019-3-7. [DOI] [Google Scholar]
- 9.Yee N. Motivations for play in online games. Cyberpsychol Behav. 2006;9:772–775. doi: 10.1089/cpb.2006.9.772. [DOI] [PubMed] [Google Scholar]
- 10.Ryan RM, Rigby CS, Przybylski A. The motivational pull of video games: A self-determination theory approach. Motiv Emot. 2006;30:344–360. [Google Scholar]
- 11.Costa MTS, Vieira LP, Barbosa EO, et al. Virtual reality-based exercise with exergames as medicine in different contexts: A short review. Clin Pract Epidemiol Ment Health. 2019;15:74. doi: 10.2174/1745017901915010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Furht B. Springer; New York, NY: 2008. Encyclopedia of multimedia. [Google Scholar]
- 13.Christensen JV, Mathiesen M, Poulsen JH, Ustrup EE, Kraus M. Player experience in a VR and non-VR multiplayer game. Paper presented at: Proceedings of the Virtual Reality International Conference-Laval Virtual. Laval, France. April 4–6, 2018.
- 14.Pasco D. The potential of using virtual reality technology in physical activity settings. Quest. 2013;65:429–441. [Google Scholar]
- 15.Yates BJ, Miller AD, Lucot JB. Physiological basis and pharmacology of motion sickness: An update. Brain Res Bull. 1998;47:395–406. doi: 10.1016/s0361-9230(98)00092-6. [DOI] [PubMed] [Google Scholar]
- 16.Munafo J, Diedrick M, Stoffregen TA. The virtual reality head-mounted display Oculus Rift induces motion sickness and is sexist in its effects. Exp Brain Res. 2017;235:889–901. doi: 10.1007/s00221-016-4846-7. [DOI] [PubMed] [Google Scholar]
- 17.Faric N, Potts HWW, Hon A, et al. What players of virtual reality exercise games want: Thematic analysis of web-based reviews. J Med Internet Res. 2019;21:e13833. doi: 10.2196/13833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasco D, Roure C, Kermarrec G, Pope Z, Gao Z. The effects of a bike active video game on players’ physical activity and motivation. J Sport Health Sci. 2017;6:25–32. doi: 10.1016/j.jshs.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang C, Wickert Z, Roedel S, et al. Time spent in MVPA during exergaming with Xbox Kinect in sedentary college students. Int J Exerc Sci. 2014;7:286–294. [Google Scholar]
- 20.McDougall J, Duncan MJ. Children, video games and physical activity: An exploratory study. Int J Disabil Hum Dev. 2008;7:89–94. [Google Scholar]
- 21.Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48:1019–1023. doi: 10.1136/bjsports-2014-093546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hwang J, Lee IM, Fernandez AM, Hillman CH, Lu AS. Exploring energy expenditure and body movement of exergaming in children of different weight status. Pediatr Exerc Sci. 2019;31:438–447. doi: 10.1123/pes.2019-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strath SJ, Kaminsky LA, Ainsworth BE, et al. Guide to the assessment of physical activity: Clinical and research applications. Circulation. 2013;128:2259–2279. doi: 10.1161/01.cir.0000435708.67487.da. [DOI] [PubMed] [Google Scholar]
- 24.Gao Y, Mandryk R. The acute cognitive benefits of casual exergame play. Paper presented at: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. Austin, TX, USA. May 5–10, 2012.
- 25.Best JR. Exergaming immediately enhances children's executive function. Dev Psychol. 2012;48:1501–1510. doi: 10.1037/a0026648. [DOI] [PubMed] [Google Scholar]
- 26.Hirschfeld LA, Gelman SA. Cambridge University Press; Cambridge: 1994. Mapping the mind: Domain specificity in cognition and culture. [Google Scholar]
- 27.Chaytor N, Schmitter-Edgecombe M. The ecological validity of neuropsychological tests: A review of the literature on everyday cognitive skills. Neuropsychol Rev. 2003;13:181–197. doi: 10.1023/b:nerv.0000009483.91468.fb. [DOI] [PubMed] [Google Scholar]
- 28.van Hooren SA, Valentijn AM, Bosma H, Ponds RW, van Boxtel MP, Jolles J. Cognitive functioning in healthy older adults aged 64–81: A cohort study into the effects of age, sex, and education. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2007;14:40–54. doi: 10.1080/138255890969483. [DOI] [PubMed] [Google Scholar]
- 29.Stanmore E, Stubbs B, Vancampfort D, de Bruin ED, Firth J. The effect of active video games on cognitive functioning in clinical and non-clinical populations: A meta-analysis of randomized controlled trials. Neurosci Biobehav Rev. 2017;78:34–43. doi: 10.1016/j.neubiorev.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Chang YK, Labban JD, Gapin JI, Etnier JL. The effects of acute exercise on cognitive performance: A meta-analysis. Brain Res. 2012;1453:87–101. doi: 10.1016/j.brainres.2012.02.068. [DOI] [PubMed] [Google Scholar]
- 31.Gabana D, Tokarchuk L, Hannon E, Gunes H. Effects of valence and arousal on working memory performance in virtual reality gaming. Paper presented at: 2017 Seventh International Conference on Affective Computing and Intelligent Interaction (ACII). San Antonio, TX, USA. October 23–26, 2017.
- 32.Booth M. Assessment of physical activity: An international perspective. Res Q Exerc Sport. 2000;71(Suppl. 2):S114–S120. [PubMed] [Google Scholar]
- 33.Snyder FR, Davis FC, Henningfield JE. The tobacco withdrawal syndrome: Performance decrements assessed on a computerized test battery. Drug Alcohol Depend. 1989;23:259–266. doi: 10.1016/0376-8716(89)90090-2. [DOI] [PubMed] [Google Scholar]
- 34.Olds D. Tobacco exposure and impaired development: A review of the evidence. Ment Retard Dev Disabil Res Rev. 1997;3:257–269. [Google Scholar]
- 35.IJsselsteijn WA, de Kort YA, Poels K. Technische Universiteit Eindhoven; Eindhoven, the Netherland: 2013. The game experience questionnaire. [Google Scholar]
- 36.Stark SM, Stark CEL. Age-related deficits in the mnemonic similarity task for objects and scenes. Behav Brain Res. 2017;333:109–117. doi: 10.1016/j.bbr.2017.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beat Games. Beat Saber. Available at: https://beatsaber.com. [accessed 10.06.2020] 2021.
- 38.Drool LLC.Thumper, a rhythm violence game. Available at: https://thumpergame.com/. [accessed 10.06.2020].
- 39.Hwang J, Lee IM, Fernandez AM, Hillman CH, Lu AS. Exploring energy expenditure and body movement of exergaming in children of different weight status. Pediatr Exerc Sci. 2019;31:438–447. doi: 10.1123/pes.2019-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hwang J, Fernandez AM, Lu AS. Application and validation of activity monitors’ epoch lengths and placement sites for physical activity assessment in exergaming. J Clin Med. 2018;7:268. doi: 10.3390/jcm7090268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwon S, Janz KF. International Children's Accelerometry Database (ICAD) Collaborators. Tracking of accelerometry-measured physical activity during childhood: ICAD pooled analysis. Int J Behav Nutr Phys Act. 2012;9:68. doi: 10.1186/1479-5868-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Strath SJ, Swartz AM, Bassett DR, Jr, O'Brien WL, King GA, Ainsworth BE. Evaluation of heart rate as a method for assessing moderate intensity physical activity. Med Sci Sports Exerc. 2000;32(Suppl. 9):S465–S470. doi: 10.1097/00005768-200009001-00005. [DOI] [PubMed] [Google Scholar]
- 43.Matthew CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(Suppl. 11):S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 44.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 45.Liang B, Lin Y. Using physiological and behavioral measurements in a picture-based road hazard perception experiment to classify risky and safe drivers. Transp Res Part F Traffic Psychol Behav. 2018;58:93–105. [Google Scholar]
- 46.Stark SM, Kirwan CB, Stark CEL. Mnemonic similarity task: A tool for assessing hippocampal integrity. Trends Cogn Sci. 2019;23:938–951. doi: 10.1016/j.tics.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yassa MA, Stark SM, Bakker A, Albert MS, Gallagher M, Stark CE. High-resolution structural and functional MRI of hippocampal CA3 and dentate gyrus in patients with amnestic mild cognitive impairment. Neuroimage. 2010;51:1242–1252. doi: 10.1016/j.neuroimage.2010.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ally BA, Hussey EP, Ko PC, Molitor RJ. Pattern separation and pattern completion in Alzheimer's disease: Evidence of rapid forgetting in amnestic mild cognitive impairment. Hippocampus. 2013;23:1246–1258. doi: 10.1002/hipo.22162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suwabe K, Byun K, Hyodo K, et al. Rapid stimulation of human dentate gyrus function with acute mild exercise. Proc Natl Acad Sci U S A. 2018;115:10487–10492. doi: 10.1073/pnas.1805668115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stark Lab. Mnemonic Similarity Task (MST) (Behavioral Pattern Separation Task (BPS-O)). Available at: https://faculty.sites.uci.edu/starklab/mnemonic-similarity-task-mst/. [accessed 08.07.2020].
- 51.Suwabe K, Hyodo K, Byun K, et al. Aerobic fitness associates with mnemonic discrimination as a mediator of physical activity effects: Evidence for memory flexibility in young adults. Sci Rep. 2017;7:5140. doi: 10.1038/s41598-017-04850-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 53.Walther-Larsen S, Petersen T, Friis SM, Aagaard G, Drivenes B, Opstrup P. Immersive virtual reality for pediatric procedural pain: A randomized clinical trial. Hosp Pediatr. 2019;9:501–507. doi: 10.1542/hpeds.2018-0249. [DOI] [PubMed] [Google Scholar]
- 54.Chittaro L, Buttussi F. Assessing knowledge retention of an immersive serious game vs. a traditional education method in aviation safety. IEEE Trans Vis Comput Graph. 2015;21:529–538. doi: 10.1109/TVCG.2015.2391853. [DOI] [PubMed] [Google Scholar]
- 55.Feodoroff B, Konstantinidis I, Froböse I. Effects of full body exergaming in virtual reality on cardiovascular and muscular parameters: Cross-sectional experiment. JMIR Serious Games. 2019;7:e12324. doi: 10.2196/12324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McDonough DJ, Pope ZC, Zeng N, Lee JE, Gao Z. Comparison of college students’ energy expenditure, physical activity, and enjoyment during exergaming and traditional exercise. J Clin Med. 2018;7:433. doi: 10.3390/jcm7110433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dębska M, Polechoński J, Mynarski A, Polechoński P. Enjoyment and intensity of physical activity in immersive virtual reality performed on innovative training devices in compliance with recommendations for health. Int J Environ Res Public Health. 2019;16:3673. doi: 10.3390/ijerph16193673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nacke L. Blekinge Institute of Technology; Blekinge, Sweden: 2009. Affective ludology: Scientific measurement of user experience in interactive entertainment. [Google Scholar]
- 60.Sánchez JG, Zea NP, Gutiérrez FL. Playability: How to identify the player experience in a video game. Paper presented at: IFIP Conference on Human-Computer Interaction. Uppsala, Sweden. August 24–28, 2009.
- 61.Cullen KW, Baranowski T, Smith SP. Using goal setting as a strategy for dietary behavior change. J Am Diet Assoc. 2001;101:562–566. doi: 10.1016/S0002-8223(01)00140-7. [DOI] [PubMed] [Google Scholar]
- 62.Baranowski T, Maddison R, Maloney A, Medina Jr E, Simons M. Building a better mousetrap (exergame) to increase youth physical activity. Games Health J. 2014;3:72–78. doi: 10.1089/g4h.2014.0018. [DOI] [PubMed] [Google Scholar]
- 63.Mandigout S, Lacroix J, Perrochon A, Svoboda Z, Aubourg T, Vuillerme N. Comparison of step count assessed using wrist- and hip-worn ActiGraph gt3x in free-living conditions in young and older adults. Front Med (Lausanne) 2019;6:252. doi: 10.3389/fmed.2019.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ogawa EF, You T, Leveille SG. Potential benefits of exergaming for cognition and dual-task function in older adults: A systematic review. J Aging Phys Act. 2016;24:332–336. doi: 10.1123/japa.2014-0267. [DOI] [PubMed] [Google Scholar]
- 65.Maggio MG, De Cola MC, Latella D, et al. What about the role of virtual reality in Parkinson disease's cognitive rehabilitation? Preliminary findings from a randomized clinical trial. J Geriatr Psychiatry Neurol. 2018;31:312–318. doi: 10.1177/0891988718807973. [DOI] [PubMed] [Google Scholar]
- 66.Moyle W, Jones C, Dwan T, Petrovich T. Effectiveness of a virtual reality forest on people with dementia: A mixed methods pilot study. Gerontologist. 2018;58:478–487. doi: 10.1093/geront/gnw270. [DOI] [PubMed] [Google Scholar]
- 67.Sayma M, Tuijt R, Cooper C, Walters K. Are we there yet? Immersive virtual reality to improve cognitive function in dementia and mild cognitive impairment. Gerontologist. 2020;60:e502–e512. doi: 10.1093/geront/gnz132. [DOI] [PubMed] [Google Scholar]
- 68.Suwabe K, Hyodo K, Byun K, et al. Aerobic fitness associates with mnemonic discrimination as a mediator of physical activity effects: Evidence for memory flexibility in young adults. Sci Rep. 2017;7:5140. doi: 10.1038/s41598-017-04850-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ferris LT, Williams JS, Shen CL. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med Sci Sports Exerc. 2007;39:728–734. doi: 10.1249/mss.0b013e31802f04c7. [DOI] [PubMed] [Google Scholar]
- 70.Winter B, Breitenstein C, Mooren FC, et al. High impact running improves learning. Neurobiol Learn Mem. 2007;87:597–609. doi: 10.1016/j.nlm.2006.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.