Abstract
Subchondral insufficiency fracture of the knee (SIFK) is a common cause of knee joint pain in older adults. SIFK is a type of stress fracture that occurs when repetitive and excessive stress is applied to the subchondral bone. If the fracture does not heal, the lesion develops into osteonecrosis and results in osteochondral collapse, requiring surgical management. Because of these clinical features, SIFK was initially termed “spontaneous osteonecrosis of the knee (SONK)” in the pre-MRI era. SONK is now categorized as an advanced SIFK lesion in the spectrum of this disease, and some authors believe the term “SONK” is a misnomer. MRI plays a significant role in the early diagnosis of SIFK. A subchondral T2 hypointense line of the affected condyle with extended bone marrow edema-like signal intensity are characteristic findings on MRI. The large lesion size and the presence of osteochondral collapse on imaging are associated with an increased risk of osteoarthritis. However, bone marrow edema-like signal intensity and osteochondral collapse alone are not specific to SIFK, and other osteochondral lesions, including avascular necrosis, osteochondral dissecans, and osteoarthritis should be considered. Chondral lesions and meniscal abnormalities, including posterior root tears, are also found in many patients with SIFK, and they are considered to be related to the development of SIFK. We review the clinical and imaging findings, including the anatomy and terminology history of SIFK, as well as its differential diagnoses. Radiologists should be familiar with these imaging features and clinical presentations for appropriate management.
Keywords: Subchondral insufficiency fracture, Spontaneous osteonecrosis of the knee, Subchondral plate, Meniscal root tear
Introduction
Subchondral insufficiency fracture of the knee (SIFK) is a microfracture related to repetitive physiological stress on the knee joint. It is a common cause of knee pain in middle-aged and older people [1]. Insufficiency fractures are a type of stress fracture, and they tend to occur in the weight bearing joints of the lower leg, such as the femoral head and talar dome of the ankle joint, apart from the knee joint [2–4].
As SIFK is a type of fracture, patients often present with an acute onset of knee pain, which usually lasts for several months. If bone morphology is maintained without bone collapse, conservative management with non-weight bearing of the affected limb is often the first treatment choice. The lesion does not heal in some patients, and subchondral collapse associated with bone necrosis eventually occurs. Surgical management, such as joint replacement, is often required in advanced cases or affected individuals with osteoarthritis (OA) [5, 6]. Early diagnosis and appropriate management are important for improving the prognosis of SIFK. However, early-stage lesions often do not show any abnormalities on radiographs at the initial visit, leading to delays in proper treatment [7]. On the other hand, MRI is an excellent tool for the early detection of osteochondral abnormalities. Therefore, MRI should be considered for older people presenting with sudden onset knee pain and normal radiographs. With the increasing number of older people, there is an ever-increasing need for accurate assessment of their knee pain. Herein, we discuss the current concept of SIFK and its imaging findings, including the differential diagnoses that should be considered.
History of SIFK
SIFK was first described by Ahlbäck et al. in 1968 as “spontaneous osteonecrosis of the knee (SONK).” They concluded that it was a primary osteonecrosis because osteonecrosis was observed on the specimen, although no apparent cause could be identified [8]. In the 1990s, the concept of subchondral insufficiency fracture (SIF) of the femoral head gradually spread. The pathogenesis of SONK was also reconsidered, and in 2000, Yamamoto et al. reported in their histological study that the true nature of SONK is a subchondral fracture, while osteonecrosis is a secondary finding [9]. Similar reports followed their conclusions [6, 10, 11], and it is now widely accepted that SONK is the end-stage of the subchondral fracture and is a part of the spectrum of SIFK (Fig. 1). Considering the history of the terminology, both SONK and SIFK have been used to describe this disease. Recently, some researchers have suggested that the word “spontaneous” in SONK does not reflect the pathogenesis and that the term “SONK” should no longer be used [1, 12]. Although the pathological mechanism leading from fracture to bone necrosis has not been elucidated, it has been suggested that increased intraosseous pressure and diminished local blood circulation associated with subchondral microfractures may be involved in osteonecrosis [13].
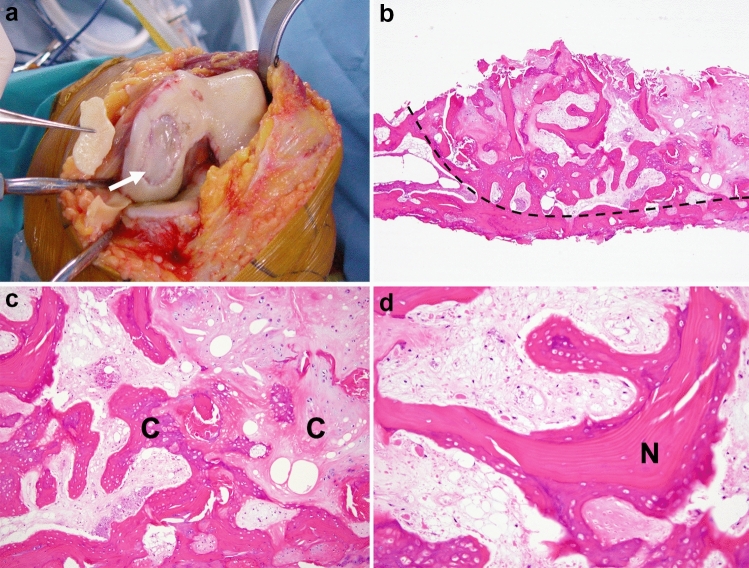
Fig. 1.
a Photograph obtained during total knee arthroplasty for SIFK in the medial femoral condyle. An osteochondral detachment from the subchondral bone can be seen (arrow). b–d Histology of subchondral insufficiency fracture (hematoxylin–eosin stain). b The lower surface indicates denuded subarticular bone of the distal femoral condyle, which is caused by secondary osteoarthritic change. The right field (right side of the dashed line) corresponds to an area of osteonecrosis (original magnification × 20). c The necrotic area shows marked callus formation (C), which indicates cellular appositional new bone and metaplastic cartilage formation (original magnification × 100). d Necrotic bone trabeculae (N) consisting of appositionally formed fiber bone on the original lamellar bone. The intertrabecular space is filled with loose fibrous connective tissue that is incompletely necrotic. These findings support a scenario in which a necrotic event occurs after preceding subchondral fracture (original magnification × 200)
Anatomy
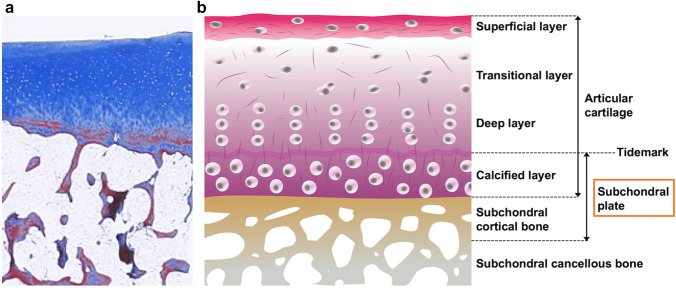
The target lesion of SIFK is the epiphyseal lesion of the knee joint. The epiphysis consists of articular cartilage, subchondral cortical bone, and underlying subarticular trabecular bone. Articular cartilage comprises an extracellular matrix consisting of a large amount of water, collagen, proteoglycans, and a small number of chondrocytes [14]. Articular cartilage in adults consists of four layers with different cellular profiles and collagen organization as follows: the superficial, transitional, deep, and calcified layers, in order from the articular surface. Between the deep and calcified layers of articular cartilage, an area known as the tidemark exists, which stains darkly with hematoxylin [14, 15]. The tidemark corresponds to the mineralization front and has several biomechanical functions. The deepest calcified layer and the underlying subchondral cortical bone are collectively referred to as the subchondral plate, which supports the superficial cartilage layers (Fig. 2) [16]. The subchondral plate is not uniform in thickness, and it is thicker at the weight bearing area and thinner at the peripheral region of the condyle. It is difficult to distinguish between the two layers of the subchondral plate in MRI used in daily practice, and a single linear low-signal band can only be recognized on T2-weighted image (T2WI) or proton density-weighted image (PDWI) [17]. In the field of radiology, the term “subchondral bone” or “subchondral region” is often used ambiguously and generally refers to the subchondral plate and nearby cancellous bone [13]. Diseases of the articular cartilage and subchondral bone are collectively referred to as osteochondral lesions.
Fig. 2.
a Frontal section of the tibial plateau (Masson trichrome stain). b Detailed schematic drawing of the articular cartilage and underlying subchondral bone
Clinical presentation
SIFK is a type of insufficiency fracture that occurs with the sudden onset of knee pain without any history of trauma. Patients can often precisely recall when and what they were doing when the pain started. The pain increases with weight bearing and exercise of the knee and often persists even at rest, including at night. Physical examination reveals tenderness in the affected area, and joint effusion is commonly observed [7, 8, 18–20]. These symptoms are sometimes similar to other medical conditions, including meniscus and cartilage injuries [17, 21, 22].
SIFK is more common in women over 50 years of age [19, 21, 23, 24]. Plett et al. reported that 64.4% (47/73) of 73 SIFK patients were women [5]. Advanced lesions have also been reported to be more common in women [24]. Low bone mineral density (BMD) associated with menopause may play a role in why SIFK is more common in older women.
SIFK is most common in the weight bearing area of the medial femoral condyle [25]. It also infrequently occurs in the medial tibial condyle, lateral femoral condyle, and lateral tibial condyle compared with the medial femoral condyle [26–28]. Wilmot et al. analyzed 74 cases of SIFK and found that 64.9% (48/74) of the cases were in the medial femoral condyle, 16.2% (12/74) each in the lateral femoral and medial tibial condyles, and 2.7% (2/74) in the lateral tibial condyle, with a preference for the central one-third of each condyle (70–77%) [24]. Most cases are unilateral, but multiple or bilateral condyles may be affected simultaneously or at different times [19, 29]. Reddy and Frederick reported in a cadaveric study that the medial femoral condyle had a poorer intraosseous blood supply with watershed areas compared with the lateral femoral condyle, which may be related to the preference for the medial femoral condyle [30]. It may also be related to differences in bone strength at each condyle [31] or the frequency of meniscus injuries, which will be discussed later.
Imaging findings
Radiography
Radiography of the lesion is usually performed to evaluate bony morphology, determine the most appropriate therapeutic strategy, and differentiate SIFK from other diseases. The fracture line in SIFK is often not clear on radiographs; as a result, their initial imaging evaluations are often negative. As the lesion progresses, radiographic abnormalities, including osteochondral defects or deformities of the epiphyses, are visualized (Fig. 3) [7, 8, 23, 32]. In 1979, Koshino et al. advocated a clinical classification system for SONK based on symptoms and radiographic findings. Since SONK is now considered part of the SIFK spectrum as described above, it is reasonable to apply the Koshino classification to SIFK. The classification is as follows: stage 1, patients with knee symptoms without any radiographic findings; stage 2, patients with bone flattening and subchondral radiolucencies; stage 3, patients with subchondral collapse; and stage 4, patients with degenerative osteoarthritic changes (Table 1) [33]. The Koshino classification is still often used as a reference for determining treatment strategies.
Fig. 3.

Plain radiograph of SIFK in a 75-year-old female patient. Saucerized defect (arrow) of the epiphysis can be observed in the medial femoral condyle of the left knee
Table 1.
Koshino classification of SIFK
| Stage | Radiographic finding |
|---|---|
| Stage I | Normal radiograph |
| Stage II | Radiolucency in subchondral weight-bearing area |
| Stage III | Expanded lucent area surrounded by sclerosis, subchondral bone collapse |
| Stage IV | Osteophytes and osteosclerosis on affected condyle |
Magnetic resonance imaging
Radiographs are not sensitive for the early diagnosis of SIFK, while MRI is excellent for detecting osteochondral lesions and is optimal for early diagnosis when SIFK is suspected [32, 34]. The characteristic findings on MRI are a bone marrow edema-like signal intensity and a subchondral hypointense line of the affected condyle (Fig. 4) [9, 35, 36].
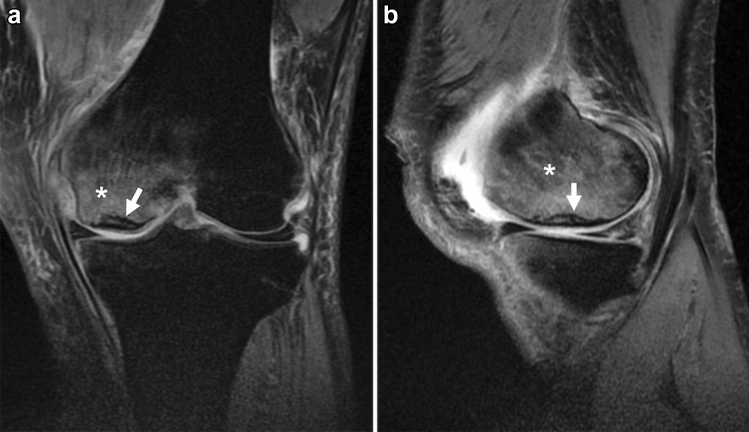
Fig. 4.
MRI of a 50-year-old man with a complaint of sudden left knee pain. a Coronal fat-suppressed proton density-weighted image (FS-PDWI), and b sagittal FS-PDWI show extensive bone marrow edema-like signal intensity over the medial femoral condyle (asterisk). A subchondral hypointense line is observed a few millimeters above the subchondral plate (arrow). Note that the line is almost parallel to the subchondral plate and open-ended in the medial part
The term “bone marrow edema” was first used by Wilson et al. in 1988 to describe abnormal bone marrow signal intensity on MRI. They found subtle low signal intensity on T1-weighted image (T1WI) and subtle high signal intensity on fat-suppressed T2WI in patients complaining of knee pain. They believed that it represented bone marrow edema, but there was no histological evidence [37]. With the spread of MRI, this finding has been observed in knees with various conditions, including SIFK, OA, trauma, inflammation, and tumors [38]. Pathologically, this finding has been proven not to be mainly edema, but a mixture of lymphoid infiltrates, fibrosis, increased vascularization, blood products, granulomatous foci of fragmented bone, and cartilage debris in various proportions [11, 12, 39–43]. For this reason, it is increasingly being referred to as bone marrow lesions, bone marrow edema-like lesions, or bone marrow edema-like signal intensity instead of “bone marrow edema” [12]. As mentioned above, this bone marrow edema-like signal intensity is seen in various conditions and is not specific to SIFK. However, it is characteristic of SIFK in that it extends over a wide area of the affected condyle [17, 35]. Ramnath et al. reported that 82% (9/11) of SIFK patients had this signal change, extending over two-thirds of the condyle [36]. Although there is no pathological proof in the literature that explains the reason for this widespread signal abnormality in SIFK patients, it may be due to the reactive changes in bone related to fracture as well as mechanical stress on bone associated with osteochondral and meniscal injuries in SIFK. Nevertheless, the extent of this bone marrow edema-like signal intensity on initial MRI is not associated with the prognosis of SIFK [5, 35].
The subchondral hypointense line on T2WI and PDWI is a more characteristic finding of SIFK. Unlike acute trauma, the fracture line in SIFK usually shows a low signal in any sequence, including fluid-sensitive MR sequences [12]. Histologically, this hypointense line corresponds to a fracture callus, thickened collapsed bone trabeculae, reactive cartilage, and granulation tissue [6, 9, 44]. This subchondral hypointense line often runs roughly parallel or curvilinear to the subchondral plate a few millimeters away from the epiphyseal surface. It may also be discontinuous or open-ended [17, 45]. Similarly, a subchondral area of low signal intensity may be observed, which is a mixture of fracture callus, granulation tissue, and secondary osteonecrosis of the superficial layer. This subchondral area of low signal intensity is often integrated with the subchondral plate, and radiologists should not overlook it because it resembles a thickened subchondral plate (Fig. 5) [17].
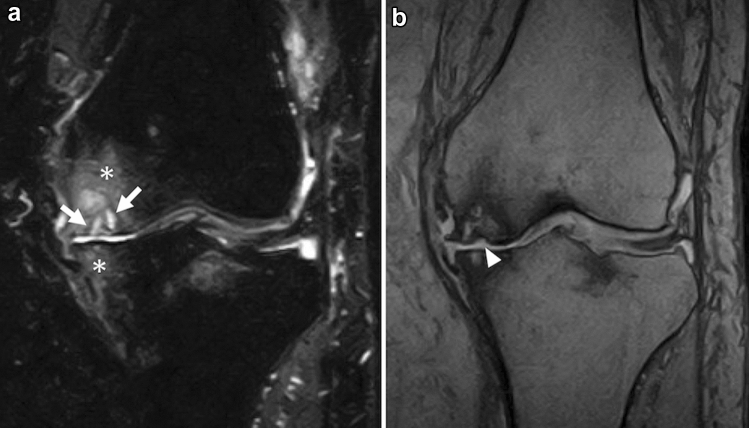
Fig. 5.
MRI of a 73-year-old female patient with SIFK in the medial femoral condyle of the right knee. a Coronal FS-PDWI shows extensive bone marrow edema-like signal intensity over the medial femoral condyle (asterisk) and a subchondral area of low signal intensity (arrow), which is integrated with the subchondral plate and resembles a thickened subchondral plate. Note the medial meniscal extrusion which is an associated finding. b A sagittal T2-weighted image (T2WI) showing a subtle hypointense line (arrowhead) above the subchondral area of low signal intensity
In addition, a slight contour deformity or flattening of the epiphysis could be visualized, which reflects a fracture of the subchondral plate [17]. In advanced cases, a fluid-filled cleft under the subchondral plate or an apparent osteochondral defect of the bone may be seen, corresponding to bone collapse or dissection associated with osteonecrosis after the fracture (Fig. 6) [46].
Fig. 6.
Coronal FS-PDWI of a 71-year-old female patient with SIFK in the medial femoral condyle of the left knee. a The initial MR image shows a subchondral hypointense line (arrow) with subtle bone marrow edema-like signal intensity around the lesion. b An MRI obtained 6 months later shows a fluid-filled cleft under the subchondral plate (arrow) and a large cyst with necrotic bone fragments beneath the lesion (arrowhead). The bone marrow edema-like signal intensity appears to expand over the medial femoral condyle (asterisk). c An MRI obtained 4 years later shows an osteochondral defect of the condyle (arrow). There is also an osteochondral defect on the tibial side (arrowhead) because the patient developed another SIFK in the medial tibial condyle during the disease
Bone scintigraphy
Bone scintigraphy shows uptake at the lesion site, but its sensitivity and specificity are low [7, 47]. Therefore, bone scintigraphy is no longer recommended for the diagnosis of SIFK in the current MRI era.
Associated findings
The etiology of SIFK is considered multifactorial, and several risk factors or associated findings have been reported to date.
Bone mineral density
SIFK is a type of insufficiency fracture. Based on this definition, low BMD can be considered a risk factor for SIFK. Several studies have reported an association between low BMD and SIFK [5, 19, 48, 49]. However, Nelson et al. found that only 16% (5/32) of SIFK patients were classified as osteoporotic. In comparison, 44% (14/32) of patients showed normal BMD, suggesting that low BMD is not the main risk factor for SIFK [50]. To date, the relationship between BMD and SIFK is still controversial, and there is no clear evidence regarding a threshold BMD that is associated with the risk of SIFK.
Meniscal abnormalities
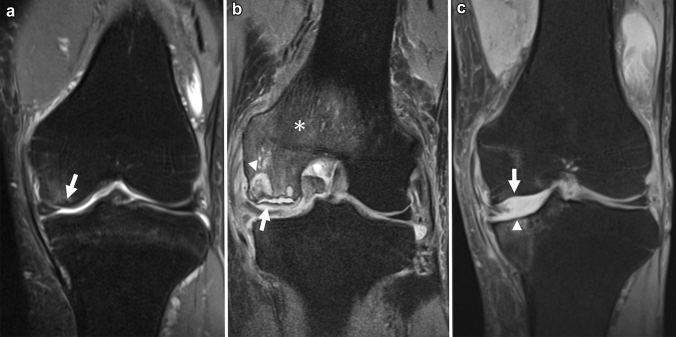
Many retrospective studies have mentioned the association between meniscal tears and SIFK, and meniscal abnormalities likely play a role in the development of the disease [1]. Most of these meniscal abnormalities are medial meniscal tears, often ipsilateral to the SIFK [5, 28, 36, 51, 52]. The most common tear is a posterior root tear, followed by a radial tear in the posterior horn (Fig. 7) [6, 28, 53, 54]. There are some reports of an association between SIFK and medial meniscal extrusion (Fig. 5) [6, 53–55], as well as some reports about SIFK and meniscectomy [11, 56, 57].
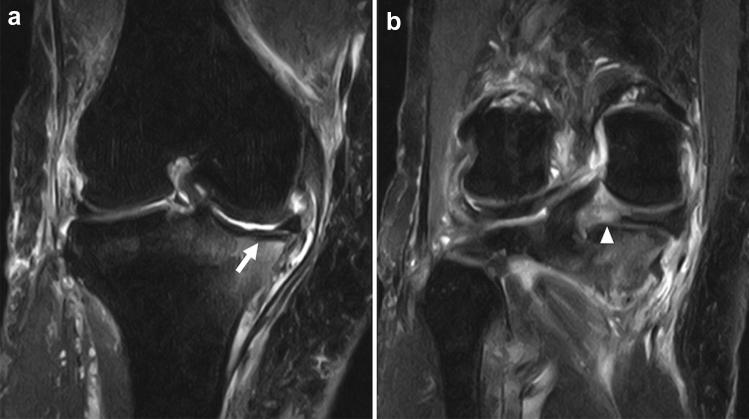
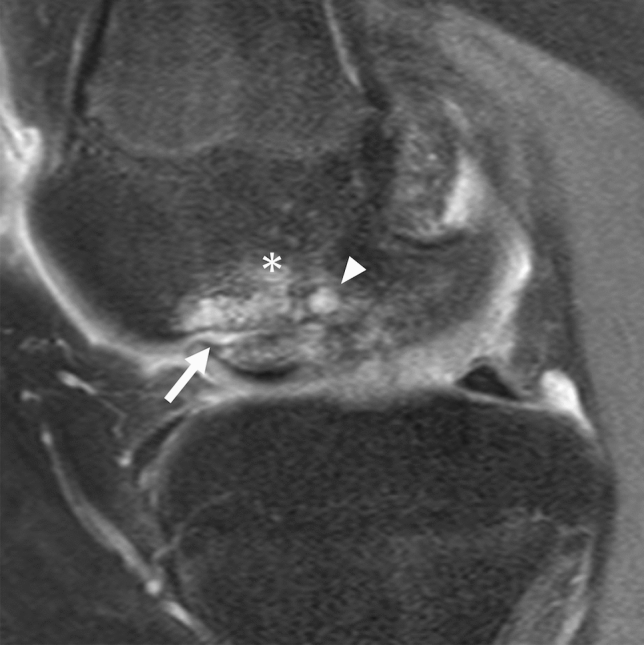
Fig. 7.
Coronal and sagittal FS-PDWI of a 79-year-old female patient who complained of a sudden worsening of knee pain during follow-up for osteoarthritis of the right knee. a A subchondral hypointense line (arrow) with bone marrow edema-like signal intensity can be seen in the medial tibial condyle. b Note the posterior root tear of the medial meniscus (arrowhead)
The meniscus plays an essential role in the movement and stability of the knee joint [58, 59]. The meniscus is a C-shaped structure consisting of fibrocartilage, which is firmly attached to the tibia at the anterior and posterior roots. In the deep central main layer of the meniscus, collagen fibers run circumferentially and convert the vertical load on the knee joint into circumferential hoop stress [60]. Owing to this structure, called “the hoop mechanism,” the load applied to the knee is distributed in the circumferential direction of the meniscus. In particular, the posterior root of the meniscus is known to contribute more to meniscal stability than the anterior root. Tears in the attachment of the posterior root of the meniscus are considered a risk factor for meniscal extrusion [53, 61, 62]. If this hoop mechanism is disrupted due to meniscal tears, extrusion, or resections, the contact pressure on the loading surface of the knee increases, which may lead to the development of SIFK [63].
Osteoarthritis
Several reports have shown an association between knee OA and SIFK [5, 10, 64]. Recently, Allam et al. reported that the degree of chondrosis was related to the severity of SIFK [64]. As meniscus has a role to protect the knee articular surface from mechanical stress, meniscal injury is also known to be related to the development of knee OA [63]. Plett et al. reported that 75.7% (53/70) of SIFK patients had overlying full-thickness cartilage loss, and 94.1% (64/68) had ipsilateral meniscal injuries [5], and meniscal injury may be associated with the development of both SIFK and OA.
Overweight/obesity
Studies on the relationship between patient weight and SIFK have shown that overweight patients have more stress on the joints in the lower limb. Zanetti et al. found that 40.6% (13/32) of SIFK patients were overweight or obese (body mass index > 25.0 kg/m2) [48]. However, it has been recently reported that body weight is not associated with the prognosis of SIFK [46].
Prognosis and treatment
Prognostic factor
The prognosis of patients with SIFK varies. Some patients recover with conservative management, while others fail to heal, resulting in necrosis of the subchondral bone of the lesion and eventual need for knee joint replacement surgery [5, 17, 46]. In hip SIF, the prognosis is influenced by factors including age, weight, BMD, fracture size, patient activity, and initial treatment [3]. These factors may also be associated with the prognosis of SIFK.
In SIFK, lesion size has been reported to be related to prognosis in several publications. Generally, the larger the lesion, the worse the prognosis, although there are several methods for measuring lesion size, and there is no standardized method of measurement or cutoff value for determining a poor prognosis [21, 64]. Aglietti et al. measured the maximum diameter of the lesion in two directions, anteroposterior and transverse, on plain radiographs and reported that the prognosis was poor if the lesion area was more than 5 cm2 or if the maximum width ratio of the lesion in the anteroposterior view exceeded 40% of the affected condyle [19]. Similarly, Lotke et al. found the cutoff ratio of the width of the lesion to exceed 50% of the condyle in those with a poor prognosis [20]. Lecouvet et al. reported in their study using MRI that subchondral areas of low signal intensity with a length of more than 14 mm or a thickness of more than 4 mm on T2WI were associated with a poor prognosis [35].
Osteochondral defects in SIFK are considered irreversible, and the prognosis of patients with this finding is unfavorable [35]. Recently, Sayyid et al. proposed an MRI grading system for SIFK to evaluate its prognosis [46]. They defined low-grade lesions as those with only bone marrow edema-like signal intensity and fracture lines on initial MRI, and high-grade lesions as those with cystic changes in the subchondral bone or osteochondral defects. They mentioned that high-grade lesions were more frequently associated with posterior meniscal root tears, moderate or severe meniscal extrusion (> 3 mm), and severe chondrosis. In 92.7% (38/41) of patients with low-grade lesions, more than 50% improvement in the range of bone marrow edema-like signal intensity in the follow-up MRI was noted within 1 year, suggesting that changes in bone marrow edema-like signal intensity over time may also reflect the prognosis of SIFK (Fig. 6).
Treatment
Conservative management is the first choice in the early stages of SIFK. It includes protected weight bearing, insole therapy, administration of non-steroidal anti-inflammatory drugs, and, in some cases, bisphosphonates. Bisphosphonates are known to act on osteoclasts to inhibit bone resorption and are widely used for osteoporosis. Although bisphosphonates were shown to be effective in an animal study, Meier et al. found no efficacy in a randomized, placebo-controlled trial in humans, and their effectiveness for SIFK is controversial [65]. Recently, teriparatide, a drug for osteoporosis, has attracted attention regarding SIF treatment. Teriparatide is a recombinant parathyroid hormone that activates osteoblasts and promotes bone formation [66–69]. Teriparatide has been reported to be more effective than bisphosphonates in osteonecrosis of the femoral head [70] and has also been reported to be effective in SIFK [71, 72]. It usually takes several months for SIFK to heal with conservative management. Yates et al. followed 20 conservatively treated SIFK patients and reported that it took an average of 4.8 (range 3–8) months for symptoms to disappear and an average of 8 (range 3–18) months for the MRI to normalize [72].
When conservative management fails to improve, surgical treatment is selected according to the size and progression of the lesion [73]. Both MRI and radiographic evaluations are important in the treatment decision-making process. The Koshino classification system for radiographs is often used since it was the first method developed to classify diseases according to the degree of progression and determine the most appropriate treatment. MRI is often used to determine the size of the lesion, differentiate between other types of osteochondral lesions, and evaluate concomitant meniscal or chondral abnormalities. For patients with relatively preserved bone morphology under stage 2 of the Koshino classification, joint-preserving surgeries such as bone grafting, osteochondral grafting, core decompression, and high tibial osteotomy are indicated [21, 33, 74]. Lesions classified as stage 3 or higher are considered to have little chance of cure. Unicompartmental knee arthroplasty is a good indication if the lesion is confined to a single condyle. High tibial osteotomy may also be indicated if the patient is young and the lesion is limited to the medial side or if the patient has medial OA along with SIFK without osteochondral collapse [75, 76]. Total knee arthroplasty is the treatment of choice when multiple condyles are affected or when patients develop severe knee OA along with SIFK [73, 74].
Differential diagnosis
Transient bone marrow edema syndrome (transient BMES) of the knee is a rare, self-limiting disease that can be difficult to differentiate from SIFK. Other osteochondral lesions include avascular necrosis (AVN), osteochondral dissecans (OCD), knee OA, and acute trauma, such as tibial plateau fractures. Since these osteochondral lesions often present with similar imaging findings, it is important to know the clinical conditions and radiological features to differentiate these diseases.
Transient bone marrow edema syndrome
Transient BMES is a rare but reversible condition characterized by pain and bone marrow edema-like signal intensity on MRI. Various terms have been used to describe this condition, including transient osteoporosis or regional migratory osteoporosis when it migrates to a different joint or within the same joint over several months [77–79]. Although transient BMES is much rarer than SIFK, it may be overlooked because of its self-limited nature. Transient BMES affects the weight-bearing joints of middle-aged men and young women exclusively in the third trimester of pregnancy or postpartum period [80].
Transient BMES is primarily characterized by extensive bone marrow edema-like signal intensity on MRI, and focal osteopenia may be present on radiographs in 3–6 weeks after the onset of symptoms. Most cases occur in the hip, and there are only a few reports of imaging findings in the knee [81]. Usually, diffuse bone marrow edema-like signal intensity is the only finding on MRI, and most cases are not associated with meniscal tears or other morphologic alterations (Fig. 8) [78, 82]. Conversely, some authors have reported that more than 77% of patients with transient BMES in the hip had subchondral line or subchondral focal hypointensity on the initial MRI [83, 84], which suggested that transient BMES may be related to a previous subchondral fracture healed with conservative treatment. However, many factors remain unclear, such as the pathogenesis of osteopenia, mechanism of migration in some cases, and the reasons healthy, young to middle-aged patients are more affected. Considering the findings of the previous studies, it may be difficult to clearly distinguish transient BMES from SIFK based on images alone. Both the patient background and clinical course should be considered to obtain a proper clinical diagnosis.
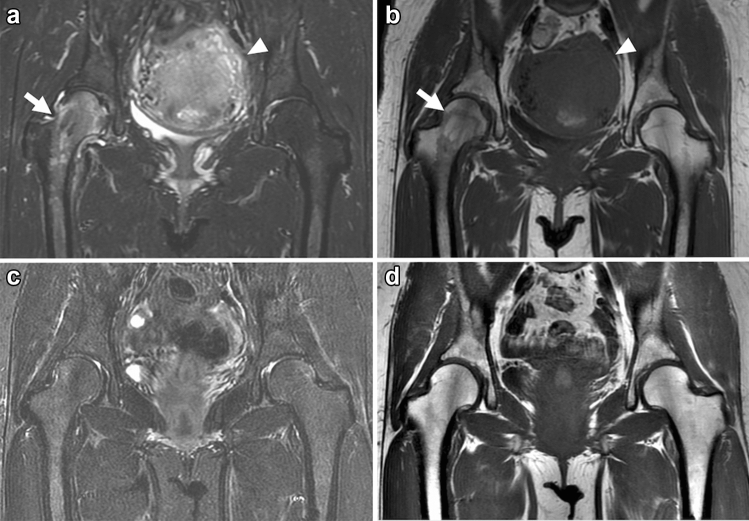
Fig. 8.
Coronal FS-PDWI and T1WI of a 40-year-old female patient in the postpartum period with transient BMES in the right hip. MRI was performed on the 12th day post-cesarean section for the complaint of severe right hip pain. a, b Initial MRI shows a diffuse bone marrow edema-like lesion extending from the right femoral head to the trochanteric region (arrow). No other obvious abnormal findings are noted, and the postpartum uterus is still enlarged (arrowhead). c, d The patient was treated conservatively, and her symptoms improved. A follow-up MRI taken 4 months later shows the disappearance of the bone marrow edema-like lesion in the right hip
Avascular necrosis (bone infarction)
AVN is referred to as bone infarction of the epiphyses caused by ischemia [17]. It is an entirely different condition from SIFK/SONK, but some previous studies confused SIFK/SONK with AVN. Although AVN is more common in patients in their 30s and 40s, the presence of risk factors plays a more significant role in its occurrence than age [45, 73]. There are several risk factors for AVN, including alcohol consumption, steroid therapy, tobacco abuse, connective tissue disease, caisson disease, sickle cell anemia, and Gaucher’s disease. Vaso-occlusive effects, high intraosseous pressure, or altered fat metabolism due to these factors are thought to involve bone ischemia [85–88]. Unlike AVN of the hip joint, AVN of the knee joint rarely develops after a fracture. The onset of AVN is typically slower than that of SIFK. The pain of infarction is relatively non-severe, and some cases are asymptomatic [17, 89].
AVN appears as a sclerotic geographic change on plain radiography and CT (Fig. 9). Sclerotic changes surround the necrotic area and are often serpentine in shape. On MRI, the irregularly shaped necrotic area is circumscribed with a distinct rim. This rim often consists of a double line of low and high signals on T2WI called a “double-line sign” and is regarded as a characteristic finding of AVN (Fig. 10) [17, 88]. This sign was introduced by Mitchell et al. in 1987, who considered that the inner high-signal-intensity band corresponds to granulation tissue, while the outer low-signal-intensity band corresponds to sclerotic reactive new bone [90]. However, it has been recently suggested that this “double-line sign” is related to a chemical shift artifact [91]. The center of the lesion is the necrotic area, but the signal of the fatty marrow is often preserved, especially in the early stages of the disease. AVN/bone infarction tends to be multiple, with bilateral (> 80%) or multiple joint involvements (60–90%) [92].
Fig. 9.

A 60-year-old female patient with sarcoidosis who had been treated with steroids for years. A reformatted CT coronal image shows multiple lesions with a serpiginous sclerotic border (arrows), which corresponds to lesions of AVN/bone infarction
Fig. 10.
A 60-year-old male patient with AVN. a A sagittal T2WI shows necrotic areas surrounded by a high and low-signal-intensity rim (arrow). The rim is displayed as a “double-line sign”. b A sagittal FS-T2WI shows that the signal of the center of the lesion is preserved with a fatty marrow signal, although it is composed of necrotic bone marrow tissue
Fractures and subchondral collapses may occur secondary to AVN, which is clinically meaningful because this often leads to eventual joint destruction and the need for surgical intervention. Sakai et al. reported that necrotic lesions that occupy more than one-third of the condyle on coronal images are at high risk of subchondral collapse [93]. Fractures and subchondral collapse often cause severe pain, and MRI shows bone marrow edema-like signal intensity around the lesion. As the disease progresses, findings similar to those seen in SIFK, such as depression of the articular surface and subchondral fluid-filled fracture cleft, may be observed [17, 45].
Osteochondral dissecans
OCD is a disorder that mainly affects young children and adolescents. Although the pathogenesis of this disease is still not fully understood, it is currently suggested that it results from growth disturbance of the secondary physis caused by repeated stress on the joints, including intense sports activity [17, 94, 95]. OCD sometimes develops into osteochondral fragmentation and dissection of the lesion, leading to juvenile OA of the knee [96]. In contrast to SIFK, symptoms are often absent in the early stage, and vague pain during exercise develops slowly over months or years [97]. Most knee OCD cases occur in the medial femoral condyle (85%). Compared to SIFK, OCD is more likely to occur slightly lateral to the weight bearing area of the medial femoral condyle (Fig. 11). OCD can also be found in the lateral parts of the femoral condyle (13%) and trochlea (2%) but is extremely rare in the tibia [98, 99]
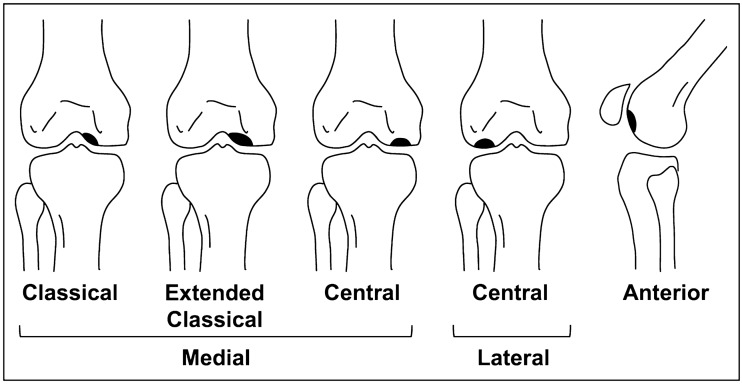
Fig. 11.
Frequent sites of OCD. The areas colored in black correspond to OCD lesions. OCD tends to occur slightly lateral to the weight bearing area of the medial femoral condyle. The classical and extended classical types both account for 75% of OCD. The lateral (13%) and medial (10%) central weight bearing surfaces of the femoral condyle are less common. OCD rarely occurs in the anterior part of the femur (2%)
In the early stages of OCD, radiographs are usually normal. As the disease progresses, fragmentation and detachment of the subchondral bone are observed [97, 100]. Interestingly, this process of osteochondral fragmentation begins in the deep portion under the articular surface and eventually involves the superficial articular cartilage, suggesting an “inside-out” mechanism [17]. MRI reflects this finding as abnormal signals are observed around the subchondral plate, and the continuity of articular cartilage is preserved in the early stages of the disease. A T2 low-signal band is observed between the lesion and the parent bone, which may be the initial arrest of the advancing ossification front (Fig. 12) [94]. Care should be taken because this low-signal band may resemble the fracture line of SIFK. As the disease progresses and the lesion becomes unstable, a rim of fluid signal intensity surrounding the lesion can be observed, representing the articular fluid between the lesion and the parent bone. Cyst formation beneath the lesion, detachment, or missing osteochondral fragments are also observed in advanced cases (Fig. 13) [101–103]. Bone marrow edema-like signal intensity may occasionally be observed around the lesion, but it is usually subtle compared to SIFK (Figs. 11, 12).
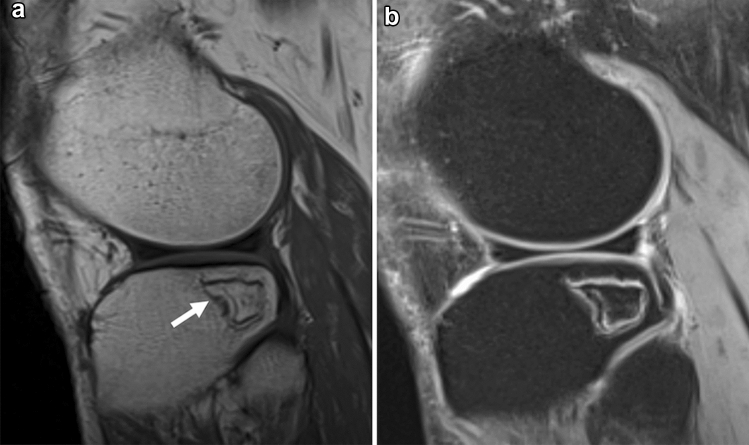
Fig. 12.
a Coronal FS-PDWI, b Sagittal FS-PDWI, and c T1-weighted image of a 14-year-old girl with stable OCD in the lateral femoral condyle in the left knee. The continuity of articular cartilage is preserved. There is no fluid signal or cyst formation around the lesion. Note the low signal band-like intensity observed between the lesion and the parent bone (arrows)
Fig. 13.
MRI of a 16-year-old boy with unstable OCD in the medial femoral condyle in the right knee. A sagittal FS-PDWI shows a rim of fluid signal intensity surrounding the OCD lesion (arrow). There is also cyst formation in the parent bone (arrowhead). Subtle bone marrow edema-like signal intensity can be observed around the cyst (asterisk)
Osteoarthritis
Knee OA is the most common osteochondral lesion in middle-aged and older people, and 37% of people over the age of 60 show some evidence of OA on imaging [104, 105]. It usually develops slowly. Patients complain of pain during daily activities, such as walking. As the disease progresses, it is associated with pain, even at rest and deformity of the limb [106].
MRI shows thinning of the articular cartilage, sclerotic changes, formation of osteophytes, subchondral cysts, bone marrow edema-like signal intensity in the subchondral bone, joint effusion, and secondary synovitis (Fig. 14) [107, 108]. Sclerotic changes in the subchondral bone in OA may resemble the subchondral low-signal intensity area in SIFK. However, OA is often associated with other degenerative findings, such as severe cartilage damage and osteophyte formation [17]. Bone marrow edema-like signal intensity in OA corresponds to a mixture of necrosis, fibrosis, and abnormal trabeculae [43, 109] and tends to be confined to a limited area of subchondral bone, compared with SIFK. The clinical course is important for differentiating between SIFK and OA because it may be difficult to distinguish when a certain amount of time has passed since the onset of subchondral fracture.
Fig. 14.
A 72-year-old female patient with knee OA. The patient complained of knee pain lasting for more than a year. a A coronal FS-T2WI shows severe cartilage damage and bony spur formation in the left medial femorotibial joint. Multiple subchondral cysts (arrows) and extended bone marrow edema-like signal intensity (asterisks) can be observed in the medial femoral and medial tibial condyles. b A coronal T2*-weighted image shows a slight deformity of the subchondral bone in the medial femoral condyle (arrowhead). This patient had been diagnosed with knee OA based on the clinical course, but the relatively old SIFK lesion was also a differential diagnosis
Conclusion
SIFK is an osteochondral lesion that commonly affects older women. Excessive contact stress related to cartilage and meniscal injury plays a major role in its development. The lesion size and the presence of osteochondral defects are associated with prognosis. The differential diagnosis of SIFK includes other osteochondral lesions, such as AVN, OCD, and OA. These diseases sometimes have similar imaging findings, and radiologists should be familiar with their imaging features and clinical presentations for appropriate management.
Author contributions
Conceptualization: JO, TN; literature search and data analysis: JO; writing—original draft: JO; writing—review and editing: JO, TN, AN, TY, NK; critically revised the work: TN, NK; supervision: TN.
Declarations
Information concerning grants
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hussain ZB, Chahla J, Mandelbaum BR, Gomoll AH, LaPrade RF. The role of meniscal tears in spontaneous osteonecrosis of the knee: a systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47:501–507. doi: 10.1177/0363546517743734. [DOI] [PubMed] [Google Scholar]
- 2.Lee S, Saifuddin A. Magnetic resonance imaging of subchondral insufficiency fractures of the lower limb. Skelet Radiol. 2019;48:1011–1021. doi: 10.1007/s00256-019-3160-4. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto T. Subchondral insufficiency fractures of the femoral head. Clin Orthop Surg. 2012;4:173–180. doi: 10.4055/cios.2012.4.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bangil M, Soubrier M, Dubost JJ, Rami S, Carcanagues Y, Ristori JM, et al. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed. 1996;63:859–861. [PubMed] [Google Scholar]
- 5.Plett SK, Hackney LA, Heilmeier U, Nardo L, Yu A, Zhang CA, et al. Femoral condyle insufficiency fractures: associated clinical and morphological findings and impact on outcome. Skelet Radiol. 2015;44:1785–1794. doi: 10.1007/s00256-015-2234-1. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka Y, Mima H, Yonetani Y, Shiozaki Y, Nakamura N, Horibe S. Histological evaluation of spontaneous osteonecrosis of the medial femoral condyle and short-term clinical results of osteochondral autografting: a case series. Knee. 2009;16:130–135. doi: 10.1016/j.knee.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Houpt JB, Pritzker KPH, Alpert B, Greyson ND, Gross AE. Natural history of spontaneous osteonecrosis of the knee (SONK): a review. Semin Arthritis Rheum. 1983;13:212–227. doi: 10.1016/0049-0172(83)90008-2. [DOI] [PubMed] [Google Scholar]
- 8.Ahlbäck S, Bauer GCH, Bohne WH. Spontaneous osteonecrosis of the knee. Arthritis Rheum. 1968;11:705–733. doi: 10.1002/art.1780110602. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Jt Surg Am. 2000;82:858–866. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Mears SC, McCarthy EF, Jones LC, Hungerford DS, Mont MA. Characterization and pathological characteristics of spontaneous osteonecrosis of the knee. Iowa Orthop J. 2009;29:38–42. [PMC free article] [PubMed] [Google Scholar]
- 11.Higuchi H, Kobayashi Y, Kobayashi A, Hatayama K, Kimura M. Histologic analysis of postmeniscectomy osteonecrosis. Am J Orthop (Belle Mead NJ) 2013;42:220–222. [PubMed] [Google Scholar]
- 12.Gorbachova T, Amber I, Beckmann NM, Bennett DL, Chang EY, Davis L, et al. Nomenclature of subchondral nonneoplastic bone lesions. AJR Am J Roentgenol. 2019;213:963–982. doi: 10.2214/AJR.19.21571. [DOI] [PubMed] [Google Scholar]
- 13.Madry H, van Dijk CN, Mueller-Gerbl M. The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc. 2010;18:419–433. doi: 10.1007/s00167-010-1054-z. [DOI] [PubMed] [Google Scholar]
- 14.Pathria MN, Chung CB, Resnick DL. Acute and stress-related injuries of bone and cartilage: pertinent anatomy, basic biomechanics, and imaging perspective. Radiology. 2016;280:21–38. doi: 10.1148/radiol.16142305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark JM, Huber JD. The structure of the human subchondral plate. J Bone Jt Surg Br. 1990;72:866–873. doi: 10.1302/0301-620X.72B5.2211774. [DOI] [PubMed] [Google Scholar]
- 16.Duncan H, Jundt J, Riddle JM, Pitchford W, Christopherson T. The tibial subchondral plate. A scanning electron microscopic study. J Bone Jt Surg Am. 1987;69:1212–1220. doi: 10.2106/00004623-198769080-00015. [DOI] [PubMed] [Google Scholar]
- 17.Gorbachova T, Melenevsky Y, Cohen M, Cerniglia BW. Osteochondral lesions of the knee: differentiating the most common entities at MRI. Radiographics. 2018;38:1478–1495. doi: 10.1148/rg.2018180044. [DOI] [PubMed] [Google Scholar]
- 18.Lotke PA, Ecker ML, Alavi A. Painful knees in older patients: radionuclide diagnosis of possible osteonecrosis with spontaneous resolution. J Bone Jt Surg Am. 1977;59:617–621. doi: 10.2106/00004623-197759050-00006. [DOI] [PubMed] [Google Scholar]
- 19.Aglietti P, Insall JN, Buzzi R, Deschamps G. Idiopathic osteonecrosis of the knee. Aetiology, prognosis and treatment. J Bone Jt Surg Br. 1983;65:588–597. doi: 10.1302/0301-620X.65B5.6643563. [DOI] [PubMed] [Google Scholar]
- 20.Lotke PA, Abend JA, Ecker ML. The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop Relat Res. 1982;171:109–116. doi: 10.1097/00003086-198211000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Mont MA, Marker DR, Zywiel MG, Carrino JA. Osteonecrosis of the knee and related conditions. J Am Acad Orthop Surg. 2011;19:482–494. doi: 10.5435/00124635-201108000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Huizinga JL, Shah N, Smith SE, Notino A, Kluczynski MA, Jordan K, et al. Prevalence of undiagnosed subchondral insufficiency fractures of the knee in middle age adults with knee pain and suspected meniscal tear. Osteoarthr Cartil Open. 2020;2:100089. doi: 10.1016/j.ocarto.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pape D, Seil R, Fritsch E, Rupp S, Kohn D. Prevalence of spontaneous osteonecrosis of the medial femoral condyle in elderly patients. Knee Surg Sports Traumatol Arthrosc. 2002;10:233–240. doi: 10.1007/s00167-002-0285-z. [DOI] [PubMed] [Google Scholar]
- 24.Wilmot AS, Ruutiainen AT, Bakhru PT, Schweitzer ME, Shabshin N. Subchondral insufficiency fracture of the knee: a recognizable associated soft tissue edema pattern and a similar distribution among men and women. Eur J Radiol. 2016;85:2096–2103. doi: 10.1016/j.ejrad.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 25.al-Rowaih A, Björkengren A, Egund N, Lindstrand A, Wingstrand H, Thorngren KG. Size of osteonecrosis of the knee. Orthop Relat Res. 1993;287:68–75. [PubMed] [Google Scholar]
- 26.Ohdera T, Miyagi S, Tokunaga M, Yoshimoto E, Matsuda S, Ikari H. Spontaneous osteonecrosis of the lateral femoral condyle of the knee: a report of 11 cases. Arch Orthop Trauma Surg. 2008;128:825–831. doi: 10.1007/s00402-008-0623-9. [DOI] [PubMed] [Google Scholar]
- 27.Lotke PA, Nelson CL, Lonner JH. Spontaneous osteonecrosis of the knee: tibial plateaus. Orthop Clin N Am. 2004;35:365–70, x. doi: 10.1016/j.ocl.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 28.Yao L, Stanczak J, Boutin RD. Presumptive subarticular stress reactions of the knee: MRI detection and association with meniscal tear patterns. Skelet Radiol. 2004;33:260–264. doi: 10.1007/s00256-004-0751-4. [DOI] [PubMed] [Google Scholar]
- 29.Sokoloff RM, Farooki S, Resnick D. Spontaneous osteonecrosis of the knee associated with ipsilateral tibial plateau stress fracture: report of two patients and review of the literature. Skelet Radiol. 2001;30:53–56. doi: 10.1007/s002560000290. [DOI] [PubMed] [Google Scholar]
- 30.Reddy AS, Frederick RW. Evaluation of the intraosseous and extraosseous blood supply to the distal femoral condyles. Am J Sports Med. 1998;26:415–419. doi: 10.1177/03635465980260031201. [DOI] [PubMed] [Google Scholar]
- 31.Harada Y, Wevers HW, Cooke TD. Distribution of bone strength in the proximal tibia. J Arthroplast. 1988;3:167–175. doi: 10.1016/S0883-5403(88)80082-2. [DOI] [PubMed] [Google Scholar]
- 32.Pollack MS, Dalinka MK, Kressel HY, Lotke PA, Spritzer CE. Magnetic resonance imaging in the evaluation of suspected osteonecrosis of the knee. Skelet Radiol. 1987;16:121–127. doi: 10.1007/BF00367759. [DOI] [PubMed] [Google Scholar]
- 33.Koshino T, Okamoto R, Takamura K, Tsuchiya K. Arthroscopy in spontaneous osteonecrosis of the knee. Orthop Clin N Am. 1979;10:609–618. doi: 10.1016/S0030-5898(20)30754-9. [DOI] [PubMed] [Google Scholar]
- 34.Fotiadou A, Karantanas A. Acute nontraumatic adult knee pain: the role of MR imaging. Radiol Med. 2009;114:437–447. doi: 10.1007/s11547-009-0380-z. [DOI] [PubMed] [Google Scholar]
- 35.Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M, et al. Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. AJR Am J Roentgenol. 1998;170:71–77. doi: 10.2214/ajr.170.1.9423603. [DOI] [PubMed] [Google Scholar]
- 36.Ramnath RR, Kattapuram S. MR appearance of SONK-like subchondral abnormalities in the adult knee: SONK redefined. Skelet Radiol. 2004;33:575–581. doi: 10.1007/s00256-004-0777-7. [DOI] [PubMed] [Google Scholar]
- 37.Wilson AJ, Murphy WA, Hardy DC, Totty WG. Transient osteoporosis: transient bone marrow edema? Radiology. 1988;167:757–760. doi: 10.1148/radiology.167.3.3363136. [DOI] [PubMed] [Google Scholar]
- 38.Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthr Cartil. 2009;17:1115–1131. doi: 10.1016/j.joca.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 39.Taljanovic MS, Graham AR, Benjamin JB, Gmitro AF, Krupinski EA, Schwartz SA, et al. Bone marrow edema pattern in advanced hip osteoarthritis: quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skelet Radiol. 2008;37:423–431. doi: 10.1007/s00256-008-0446-3. [DOI] [PubMed] [Google Scholar]
- 40.Eriksen EF, Ringe JD. Bone marrow lesions: a universal bone response to injury? Rheumatol Int. 2012;32:575–584. doi: 10.1007/s00296-011-2141-2. [DOI] [PubMed] [Google Scholar]
- 41.Starr AM, Wessely MA, Albastaki U, Pierre-Jerome C, Kettner NW. Bone marrow edema: pathophysiology, differential diagnosis, and imaging. Acta Radiol. 2008;49:771–786. doi: 10.1080/02841850802161023. [DOI] [PubMed] [Google Scholar]
- 42.Akhavan S, Martinkovich SC, Kasik C, DeMeo PJ. Bone marrow edema, clinical significance, and treatment options: a review. J Am Acad Orthop Surg. 2020;28:e888–e899. doi: 10.5435/JAAOS-D-20-00142. [DOI] [PubMed] [Google Scholar]
- 43.Zanetti M, Bruder E, Romero J, Hodler J. Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology. 2000;215:835–840. doi: 10.1148/radiology.215.3.r00jn05835. [DOI] [PubMed] [Google Scholar]
- 44.Takeda M, Higuchi H, Kimura M, Kobayashi Y, Terauchi M, Takagishi K. Spontaneous osteonecrosis of the knee. J Bone Jt Surg Br. 2008;90:324–329. doi: 10.1302/0301-620X.90B3.18629. [DOI] [PubMed] [Google Scholar]
- 45.Lecouvet FE, Malghem J, Maldague BE, Vande Berg BC. MR imaging of epiphyseal lesions of the knee: current concepts, challenges, and controversies. Radiol Clin N Am. 2005;43:655–72, vii–viii. doi: 10.1016/j.rcl.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 46.Sayyid S, Younan Y, Sharma G, Singer A, Morrison W, Zoga A, et al. Subchondral insufficiency fracture of the knee: grading, risk factors, and outcome. Skelet Radiol. 2019;48:1961–1974. doi: 10.1007/s00256-019-03245-6. [DOI] [PubMed] [Google Scholar]
- 47.Mont MA, Ulrich SD, Seyler TM, Smith JM, Marker DR, McGrath MS, et al. Bone scanning of limited value for diagnosis of symptomatic oligofocal and multifocal osteonecrosis. J Rheumatol. 2008;35:1629–1634. [PubMed] [Google Scholar]
- 48.Zanetti M, Romero J, Dambacher MA, Hodler J. Osteonecrosis diagnosed on MR images of the knee. Relationship to reduced bone mineral density determined by high resolution peripheral quantitative CT. Acta Radiol. 2003;44:525–531. doi: 10.1080/j.1600-0455.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 49.Akamatsu Y, Mitsugi N, Hayashi T, Kobayashi H, Saito T. Low bone mineral density is associated with the onset of spontaneous osteonecrosis of the knee. Acta Orthop. 2012;83:249–255. doi: 10.3109/17453674.2012.684139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nelson FR, Craig J, Francois H, Azuh O, Oyetakin-White P, King B. Subchondral insufficiency fractures and spontaneous osteonecrosis of the knee may not be related to osteoporosis. Arch Osteoporos. 2014;9:194. doi: 10.1007/s11657-014-0194-z. [DOI] [PubMed] [Google Scholar]
- 51.Norman A, Baker ND. Spontaneous osteonecrosis of the knee and medial meniscal tears. Radiology. 1978;129:653–656. doi: 10.1148/129.3.653. [DOI] [PubMed] [Google Scholar]
- 52.Yamagami R, Taketomi S, Inui H, Tahara K, Tanaka S. The role of medial meniscus posterior root tear and proximal tibial morphology in the development of spontaneous osteonecrosis and osteoarthritis of the knee. Knee. 2017;24:390–395. doi: 10.1016/j.knee.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 53.Robertson DD, Armfield DR, Towers JD, Irrgang JJ, Maloney WJ, Harner CD. Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Jt Surg Br. 2009;91:190–195. doi: 10.1302/0301-620X.91B2.21097. [DOI] [PubMed] [Google Scholar]
- 54.Sung JH, Ha JK, Lee DW, Seo WY, Kim JG. Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: comparison with horizontal tear. Arthroscopy. 2013;29:726–732. doi: 10.1016/j.arthro.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 55.Yasuda T, Ota S, Fujita S, Onishi E, Iwaki K, Yamamoto H. Association between medial meniscus extrusion and spontaneous osteonecrosis of the knee. Int J Rheum Dis. 2018;21:2104–2111. doi: 10.1111/1756-185X.13074. [DOI] [PubMed] [Google Scholar]
- 56.Muscolo DL, Costa-Paz M, Makino A, Ayerza MA. Osteonecrosis of the knee following arthroscopic meniscectomy in patients over 50-years old. Arthroscopy. 1996;12:273–279. doi: 10.1016/S0749-8063(96)90058-4. [DOI] [PubMed] [Google Scholar]
- 57.Kobayashi Y, Kimura M, Higuchi H, Terauchi M, Shirakura K, Takagishi K. Juxta-articular bone marrow signal changes on magnetic resonance imaging following arthroscopic meniscectomy. Arthroscopy. 2002;18:238–245. doi: 10.1053/jars.2002.29938. [DOI] [PubMed] [Google Scholar]
- 58.Radin EL, de Lamotte F, Maquet P. Role of the menisci in the distribution of stress in the knee. Clin Orthop Relat Res. 1984;185:290–294. doi: 10.1097/00003086-198405000-00046. [DOI] [PubMed] [Google Scholar]
- 59.Aagaard H, Verdonk R. Function of the normal meniscus and consequences of meniscal resection. Scand J Med Sci Sports. 1999;9:134–140. doi: 10.1111/j.1600-0838.1999.tb00443.x. [DOI] [PubMed] [Google Scholar]
- 60.Fox AJS, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health. 2012;4:340–351. doi: 10.1177/1941738111429419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Villegas DF, Hansen TA, Liu DF, Donahue TLH. A quantitative study of the microstructure and biochemistry of the medial meniscal horn attachments. Ann Biomed Eng. 2008;36:123–131. doi: 10.1007/s10439-007-9403-x. [DOI] [PubMed] [Google Scholar]
- 62.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Jt Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 63.Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 64.Allam E, Boychev G, Aiyedipe S, Morrison W, Roedl JB, Singer AD, et al. Subchondral insufficiency fracture of the knee: unicompartmental correlation to meniscal pathology and degree of chondrosis by MRI. Skelet Radiol. 2021;50:2185–2194. doi: 10.1007/s00256-021-03777-w. [DOI] [PubMed] [Google Scholar]
- 65.Meier C, Kraenzlin C, Friederich NF, Wischer T, Grize L, Meier CR, et al. Effect of ibandronate on spontaneous osteonecrosis of the knee: a randomized, double-blind, placebo-controlled trial. Osteoporos Int. 2014;25:359–366. doi: 10.1007/s00198-013-2581-5. [DOI] [PubMed] [Google Scholar]
- 66.Dobnig H, Turner RT. The effects of programmed administration of human parathyroid hormone fragment (1–34) on bone histomorphometry and serum chemistry in rats. Endocrinology. 1997;138:4607–4612. doi: 10.1210/endo.138.11.5505. [DOI] [PubMed] [Google Scholar]
- 67.Shen V, Dempster DW, Birchman R, Xu R, Lindsay R. Loss of cancellous bone mass and connectivity in ovariectomized rats can be restored by combined treatment with parathyroid hormone and estradiol. J Clin Investig. 1993;91:2479–2487. doi: 10.1172/JCI116483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mosekilde L, Søgaard CH, Danielsen CC, Tørring O. The anabolic effects of human parathyroid hormone (hPTH) on rat vertebral body mass are also reflected in the quality of bone, assessed by biomechanical testing: a comparison study between hPTH-(1–34) and hPTH-(1–84) Endocrinology. 1991;129:421–428. doi: 10.1210/endo-129-1-421. [DOI] [PubMed] [Google Scholar]
- 69.Jiang Y, Zhao JJ, Mitlak BH, Wang O, Genant HK, Eriksen EF. Recombinant human parathyroid hormone (1–34) [teriparatide] improves both cortical and cancellous bone structure. J Bone Miner Res. 2003;18:1932–1941. doi: 10.1359/jbmr.2003.18.11.1932. [DOI] [PubMed] [Google Scholar]
- 70.Arai R, Takahashi D, Inoue M, Irie T, Asano T, Konno T, et al. Efficacy of teriparatide in the treatment of nontraumatic osteonecrosis of the femoral head: a retrospective comparative study with alendronate. BMC Musculoskelet Disord. 2017;18:24. doi: 10.1186/s12891-016-1379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Horikawa A, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y, Kodama H, et al. Treatment of spontaneous osteonecrosis of the knee by daily teriparatide: a report of 3 cases. Medicine (Baltim) 2020;99:e18989. doi: 10.1097/MD.0000000000018989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yates PJ, Calder JD, Stranks GJ, Conn KS, Peppercorn D, Thomas NP. Early MRI diagnosis and non-surgical management of spontaneous osteonecrosis of the knee. Knee. 2007;14:112–116. doi: 10.1016/j.knee.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 73.Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee: review. Ann Transl Med. 2015;3:6. doi: 10.3978/j.issn.2305-5839.2014.11.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sibilska A, Góralczyk A, Hermanowicz K, Malinowski K. Spontaneous osteonecrosis of the knee: what do we know so far? A literature review. Int Orthop. 2020;44:1063–1069. doi: 10.1007/s00264-020-04536-7. [DOI] [PubMed] [Google Scholar]
- 75.Choi HG, Kim JS, Yoo HJ, Jung YS, Lee YS. The fate of bone marrow lesions after open wedge high tibial osteotomy: a comparison between knees with primary osteoarthritis and subchondral insufficiency fractures. Am J Sports Med. 2021;49:1551–1560. doi: 10.1177/03635465211002160. [DOI] [PubMed] [Google Scholar]
- 76.Kumagai K, Akamatsu Y, Kobayashi H, Kusayama Y, Saito T. Mosaic osteochondral autograft transplantation versus bone marrow stimulation technique as a concomitant procedure with opening-wedge high tibial osteotomy for spontaneous osteonecrosis of the medial femoral condyle. Arthroscopy. 2018;34:233–240. doi: 10.1016/j.arthro.2017.08.244. [DOI] [PubMed] [Google Scholar]
- 77.Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Bone marrow edema syndrome. Skelet Radiol. 2009;38:425–436. doi: 10.1007/s00256-008-0529-1. [DOI] [PubMed] [Google Scholar]
- 78.Hofmann S, Kramer J, Vakil-Adli A, Aigner N, Breitenseher M. Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin N Am. 2004;35:321–333. doi: 10.1016/j.ocl.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 79.Balfousias T, Karadimas EJ, Kakagia DD, Apostolopoulos A, Papanikolaou A. Lower limb pain attributed to bone marrow edema syndrome: a commonly ignored pathology. Cureus. 2020;12:e7679. doi: 10.7759/cureus.7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cahir JG, Toms AP. Regional migratory osteoporosis. Eur J Radiol. 2008;67:2–10. doi: 10.1016/j.ejrad.2008.01.051. [DOI] [PubMed] [Google Scholar]
- 81.Karantanas AH, Nikolakopoulos I, Korompilias AV, Apostolaki E, Skoulikaris N, Eracleous E. Regional migratory osteoporosis in the knee: MRI findings in 22 patients and review of the literature. Eur J Radiol. 2008;67:34–41. doi: 10.1016/j.ejrad.2008.01.054. [DOI] [PubMed] [Google Scholar]
- 82.Berman N, Brent H, Chang G, Honig S. Transient osteoporosis: not just the hip to worry about. Bone Rep. 2016;5:308–311. doi: 10.1016/j.bonr.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Miyanishi K, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Noguchi Y, et al. Subchondral changes in transient osteoporosis of the hip. Skelet Radiol. 2001;30:255–261. doi: 10.1007/s002560100350. [DOI] [PubMed] [Google Scholar]
- 84.Yamaguchi R, Yamamoto T, Motomura G, Ikemura S, Iwasaki K, Zhao G, et al. Radiological morphology variances of transient osteoporosis of the hip. J Orthop Sci. 2017;22:687–692. doi: 10.1016/j.jos.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 85.Motomura G, Yamamoto T, Miyanishi K, Yamashita A, Sueishi K, Iwamoto Y. Bone marrow fat-cell enlargement in early steroid-induced osteonecrosis—a histomorphometric study of autopsy cases. Pathol Res Pract. 2005;200:807–811. doi: 10.1016/j.prp.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 86.Wright JL, Zhou S, Churg A. Pulmonary hypertension and vascular oxidative damage in cigarette smoke exposed eNOS−/− mice and human smokers. Inhal Toxicol. 2012;24:732–740. doi: 10.3109/08958378.2012.715698. [DOI] [PubMed] [Google Scholar]
- 87.Lemonne N, Lamarre Y, Romana M, Mukisi-Mukaza M, Hardy-Dessources M-D, Tarer V, et al. Does increased red blood cell deformability raise the risk for osteonecrosis in sickle cell anemia? Blood. 2013;121:3054–3056. doi: 10.1182/blood-2013-01-480277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chancelier MD, Hélénon O, Page B, Rousselin B, Legendre C, Moreau JF. Aseptic osteonecrosis of the knee induced by corticoids. MRI aspects. J Radiol. 1992;73:191–201. [PubMed] [Google Scholar]
- 89.Narváez J, Narváez JA, Rodriguez-Moreno J, Roig-Escofet D. Osteonecrosis of the knee: differences among idiopathic and secondary types. Rheumatology (Oxf) 2000;39:982–989. doi: 10.1093/rheumatology/39.9.982. [DOI] [PubMed] [Google Scholar]
- 90.Mitchell DG, Rao VM, Dalinka MK, Spritzer CE, Alavi A, Steinberg ME, et al. Femoral head avascular necrosis: correlation of MR imaging, radiographic staging, radionuclide imaging, and clinical findings. Radiology. 1987;162:709–715. doi: 10.1148/radiology.162.3.3809484. [DOI] [PubMed] [Google Scholar]
- 91.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007;63:16–28. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 92.Mont MA, Baumgarten KM, Rifai A, Bluemke DA, Jones LC, Hungerford DS. Atraumatic osteonecrosis of the knee. J Bone Jt Surg Am. 2000;82:1279–1290. doi: 10.2106/00004623-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 93.Sakai T, Sugano N, Ohzono K, Matsui M, Hiroshima K, Ochi T. MRI evaluation of steroid- or alcohol-related osteonecrosis of the femoral condyle. Acta Orthop Scand. 1998;69:598–602. doi: 10.3109/17453679808999263. [DOI] [PubMed] [Google Scholar]
- 94.Ellermann J, Johnson CP, Wang L, Macalena JA, Nelson BJ, LaPrade RF. Insights into the epiphyseal cartilage origin and subsequent osseous manifestation of juvenile osteochondritis dissecans with a modified clinical MR imaging protocol: a pilot study. Radiology. 2017;282:798–806. doi: 10.1148/radiol.2016160071. [DOI] [PubMed] [Google Scholar]
- 95.Laor T, Zbojniewicz AM, Eismann EA, Wall EJ. Juvenile osteochondritis dissecans: is it a growth disturbance of the secondary physis of the epiphysis? AJR Am J Roentgenol. 2012;199:1121–1128. doi: 10.2214/AJR.11.8085. [DOI] [PubMed] [Google Scholar]
- 96.Kessler JI, Nikizad H, Shea KG, Jacobs JC, Jr, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42:320–326. doi: 10.1177/0363546513510390. [DOI] [PubMed] [Google Scholar]
- 97.Masquijo J, Kothari A. Juvenile osteochondritis dissecans (JOCD) of the knee: current concepts review. EFORT Open Rev. 2019;4:201–212. doi: 10.1302/2058-5241.4.180079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Jt Surg Br. 1971;53:440–447. doi: 10.1302/0301-620X.53B3.440. [DOI] [PubMed] [Google Scholar]
- 99.Hefti F, Beguiristain J, Krauspe R, Möller-Madsen B, Riccio V, Tschauner C, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231–245. [PubMed] [Google Scholar]
- 100.Wall EJ, Polousky JD, Shea KG, Carey JL, Ganley TJ, Grimm NL, et al. Novel radiographic feature classification of knee osteochondritis dissecans: a multicenter reliability study. Am J Sports Med. 2015;43:303–309. doi: 10.1177/0363546514566600. [DOI] [PubMed] [Google Scholar]
- 101.Smet AAD, De Smet AA, Fisher DR, Graf BK, Lange RH. Osteochondritis dissecans of the knee: value of MR imaging in determining lesion stability and the presence of articular cartilage defects. AJR Am J Roentgenol. 1996;155:549–553. doi: 10.2214/ajr.155.3.2117355. [DOI] [PubMed] [Google Scholar]
- 102.De Smet AA, Ilahi OA, Graf BK. Reassessment of the MR criteria for stability of osteochondritis dissecans in the knee and ankle. Skelet Radiol. 1996;25:159–163. doi: 10.1007/s002560050054. [DOI] [PubMed] [Google Scholar]
- 103.Kijowski R, Blankenbaker DG, Shinki K, Fine JP, Graf BK, De Smet AA. Juvenile versus adult osteochondritis dissecans of the knee: appropriate MR imaging criteria for instability. Radiology. 2008;248:571–578. doi: 10.1148/radiol.2482071234. [DOI] [PubMed] [Google Scholar]
- 104.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 105.Andrianakos AA, Kontelis LK, Karamitsos DG, Aslanidis SI, Georgountzos AI, Kaziolas GO, et al. Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol. 2006;33:2507–2513. [PubMed] [Google Scholar]
- 106.Michael JW-P, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107:152–162. doi: 10.3238/arztebl.2010.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Spector T, Cooper C. Radiographic assessment of osteoarthritis in population studies: whither Kellgren and Lawrence? Osteoarthr Cartil. 1993;1:203–206. doi: 10.1016/S1063-4584(05)80325-5. [DOI] [PubMed] [Google Scholar]
- 108.Oo WM, Linklater JM, Hunter DJ. Imaging in knee osteoarthritis. Curr Opin Rheumatol. 2017;29:86–95. doi: 10.1097/BOR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 109.Xu L, Hayashi D, Roemer FW, Felson DT, Guermazi A. Magnetic resonance imaging of subchondral bone marrow lesions in association with osteoarthritis. Semin Arthritis Rheum. 2012;42:105–118. doi: 10.1016/j.semarthrit.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]