Abstract
Background:
Poor social health is prevalent in older adults and may be associated with worse cognition, and increased dementia risk. The aim of this study was to determine whether social isolation, social support and loneliness are independently associated with cognitive function and incident dementia over 5 years in older adults, and to investigate potential gender differences.
Methods:
Participants were 11,498 community-dwelling relatively healthy Australians aged 70–94, in the ASPREE Longitudinal Study of Older Persons (ALSOP). Social isolation, social support, loneliness and cognitive function were assessed through self-report. Outcomes examined were cognitive decline (>1.5 SD decline in cognitive performance since baseline) and incident dementia (adjudicated according to DSM-IV criteria).
Results:
Most participants self-reported good social health (92%) with very few socially isolated (2%), with low social support (2%) or lonely (5%). Among women, social isolation and low social support were consistently associated with lower cognitive function (e.g., social support and cognition β = −1.17, p < 0.001). No consistent longitudinal associations were observed between baseline social health and cognitive decline (over median 3.1 years) or incident dementia (over median 4.4 years; social isolation: HR = 1.00, p = 0.99; low social support: HR = 1.79, p = 0.11; loneliness: HR = 0.72, p = 0.34 among women and men).
Conclusion:
Our study provides evidence that social isolation and a low social support are associated with worse cognitive function in women, but not men. Social health did not predict incident cognitive decline or dementia, but we lacked power to stratify dementia analyses by gender.
Keywords: age factors, aged, aged 80 and over, ageing, cognition, cognitive health, dementia, geriatrics, interpersonal relations, loneliness, older adult, social connection, social interaction, social isolation, social support
1 ∣. INTRODUCTION
Social health is a broad term, encompassing an individual's interactions, engagement with their community, perception of their relationships and how content they are with these.1 Social health is being recognised with increasing importance; individuals with poor social health are more likely to engage in risky behaviours, and are at increased risk of all-cause mortality.2-8
Social isolation, social support and loneliness are commonly described as components of social health. Social isolation is an objective measure, assessed through counts of social interaction and integration into one's social environment.1,9,10 Social support is subjective, defined as the degree to which an individual feels their social needs are met.11,12 Loneliness is defined as a subjective view of insufficient social connection.1 Historically, these terms have been conflated and used synonymously, not allowing for investigation into the potential separate effects.13 More recently, combinations of social support, social isolation, and loneliness have been assessed. For example, as positive (i.e., not isolated, supported, and not lonely), negative (i.e., isolated, low support, and lonely) and discordant (i.e., dissimilar; isolated, low support, but not lonely).14 Composite measures such as this could define robustness or susceptibility to poor social health, and is key to effective targeting of specific preventative interventions.1
Two recent systematic reviews, of 39 and 43 studies, show that better social health is associated with higher average cognitive function in older adults.13,15 Furthermore, poor social health has been associated with an increased risk of dementia in two additional systematic reviews, including 19 and 33 studies, respectively; however, the extent to which the individual components influence cognitive health remains unclear.16,17 Additionally, there is evidence of gender differences in social health, cognitive change and dementia risk throughout the ageing process.18,19 Gender differences have also been reported in social health, with women feeling more socially supported and less socially isolated, but at greater risk of loneliness than men.20,21
This study aims to determine the associations of social isolation, social support and loneliness with cognitive function at baseline, and cognitive decline and dementia over a median of 4.7 years, in initially healthy, community-dwelling older adults, and to explore potential gender differences in these relationships.
2 ∣. METHODS
2.1 ∣. Study population
This is a secondary data analysis utilising data from the ASPirin in Reducing Events in the Elderly (ASPREE) study, and the ASPREE Longitudinal Study of Older Persons (ALSOP) sub-study. ASPREE was a randomised, double-blind, placebo-controlled trial which demonstrated that low-dose aspirin had no benefit to extension of disability-free life, or risk of dementia, over median 4.7 years.22-24 Australian participants were community-dwelling older adults aged 70+ years with no overt disease likely to cause death in the next 5 years.25 Exclusion criteria included the presence of function limiting physical disability, diagnosed cardiovascular disease or dementia, and/or a Modified Mini-Mental State Examination (3MS) score of less than 78 (Table A1 in supporting information S1).
The majority (89%) of Australian ASPREE participants also participated in ALSOP (Figure A1 in supporting information S1).24 For <15% of participants, there was a delay of up to 15 months in administration of the baseline ALSOP questionnaire.24
Participants were excluded from our study if they had incomplete social health data (n = 1471), reported living in residential care facilities or nursing homes at baseline (n = 31), or did not complete any cognitive assessment at baseline (n = 133). Our study consisted of 11,498 older Australians.
2.2 ∣. Study measures
2.2.1 ∣. Social health
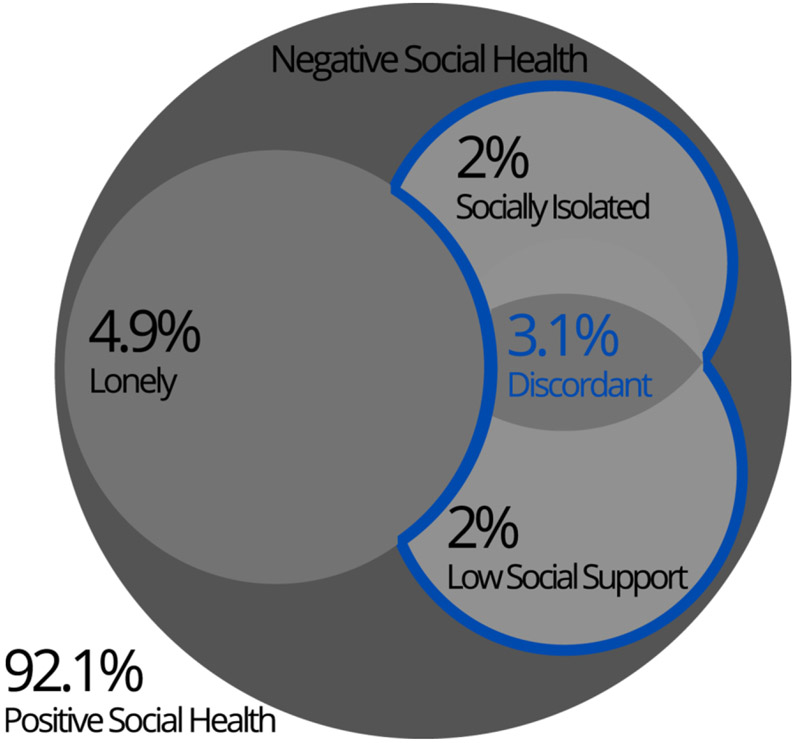
From the validated Revised Lubben Social Network Scale (LSNS),26 social isolation was defined as engaging in community activities less than once per month and having contact with four or fewer relatives and close friends in a month (Tables B1 and B2 in supporting information S1). Social support was defined as having four or more relatives or close friends with whom private matters could be discussed, in combination with friends or relatives who could be called upon for help. Loneliness was defined by feeling lonely occasionally (3–5 days/week) or all of the time (5–7 days/week) based on one Center for Epidemiological Studies—Depression (CES-D-10) Scale question. The social health composite categories were defined as positive (not isolated, supported and not lonely), discordant (isolated and/or low support, but not lonely), and lonely (regardless of isolation or support; Figure 1).
FIGURE 1.
Components of social health
2.2.2 ∣. Cognitive function
The 3MS measured global cognitive function27; the Controlled Oral Word Association Test (COWAT) assessed phonemic verbal fluency28; the Symbol Digit Modalities Test (SDMT) measured attention and psychomotor speed29; the delayed recall task from the Hopkins Verbal Learning Test—Revised (HVLT-R) was used to assess episodic memory.27 Cognitive function was assessed at baseline, years 1, 3, 5 and 7 (or close-out visit—last visit before study completion).23 Cognitive decline was defined as an inter-individual drop of at least 1.5 SD in follow-up score, compared to baseline, on any of the four cognitive tests at any follow-up, as described previously.23
2.2.3 ∣. Dementia incidence
Suspected dementia cases, titled ‘triggers’, were individuals with a 3MS score below 78, an age-education-gender-adjusted fall in 3MS score of over 10 points from baseline, a diagnosis of dementia by a medical practitioner, report by the participant of thinking or memory concerns mentioned to a medical practitioner, or the prescription of cholinesterase inhibitors.22,23 These triggered further cognitive and functional testing. Dementia was adjudicated by an international committee of specialist neurologists and geriatricians, according to criteria found in the fourth edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV).
2.2.4 ∣. Covariates
We intended to stratify by gender. Covariates (other than age) were chosen based on current literature and included if p < 0.10 in our main analysis.17,30 Potential covariates not included were employment, partner and smoking status. The final model adjusted for age at randomisation, education (≤12, >12 years), country of birth (Australia, other), body mass index (BMI; kg/m2) and depressive symptoms (CES-D 10: ≥8 high vs. <8 none/low).31
2.3 ∣. Data analysis
The data were analysed using Stata version 15.1. Social health was assessed (1) as separate components (isolation, support, and loneliness) independently, (2) components mutually adjusted for one another, and (3) as a composite measure. Baseline associations between social health and cognitive function were assessed using multivariable linear regression. Longitudinal associations between social health components and cognitive decline, dementia triggers and confirmed dementia cases were assessed using Cox proportional-hazards regression. Sensitivity analyses assessed potential dose–response relationships. To test whether the findings were robust, we (1) excluded participants with a dementia trigger or diagnosis, or participants who were censored in the first half-year, and then year, to account for potential for reverse causality and the delay between date of randomisation and ALSOP questionnaire completion; (2) reran longitudinal analyses utilising an adjusted CES-D covariate without the loneliness item; and (3) assessed for potential effect modification from the intervention (aspirin vs. placebo), given ASPREE was a clinical trial.
The ASPREE and ALSOP studies followed the National Health and Medical Research Council Guidelines on Human Experimentation, run in accordance with the Declaration of Helsinki 1964, and ethics approval was received through Monash University Human Research Ethics Committee.
3 ∣. RESULTS
3.1 ∣. Study population
The vast majority of men (91.9%) and women (92.2%) were classified with positive social health (Figure 1; Table C1 in supporting information S1). Men were more likely to be socially isolated or have low social support, but less likely to be lonely. Just over 3% of the sample were categorised as discordant (socially isolated and/or low social support, but not lonely), with more men than women in this category.
3.2 ∣. Social health and demographic associations
Undertaking paid or volunteer work, or having lower depressive symptoms were associated with better social health, and being younger was associated with less loneliness. Being born overseas increased risk of poor social health, excepting loneliness in men. Among men, higher education, having a partner and not living alone were associated with better social health. Among women, having never smoked was associated with better social health, and higher BMI was associated with greater loneliness. Women with a partner were more socially supported and less lonely, and women who lived with others were also less lonely.
3.3 ∣. Social health and baseline cognitive function
The SDMT and COWAT scores were approximately normally distributed across the whole sample, whereas 3MS and HVLT-R scores were negatively skewed (data not shown). Women scored higher in average cognitive ability across all four cognitive tests when compared with men (Table 1).
TABLE 1.
Fully adjusted multivariable analyses of baseline social health and baseline cognitive function in women
| 3MS |
COWAT |
SDMT |
HVLT-R delayed recall |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | |
| 94.5 ± 4.0 | 12.9 ± 4.6 | 39.1 ± 9.7 | 8.4 ± 2.6 | |||||||||||||
| Socially isolated (vs. not) | 93.2 ± 4.5 | −1.11 | (−1.95, −0.26) | 0.01+ | 11.6 ± 4.5 | −1.18 | (−2.15, −0.20) | 0.02+ | 36.7 ± 10.5 | −2.15 | (−4.13, −0.17) | 0.03 | 7.6 ± 2.9 | −0.78 | (−1.33, −0.22) | 0.01+ |
| Low social support (vs. not) | 93.0 ± 4.7 | −1.37 | (−2.12, −0.62) | <0.001+ | 11.8 ± 4.5 | −0.98 | (−1.84, −0.11) | 0.03 | 36.3 ± 10.8 | −2.61 | (−4.36, −0.85) | <0.001+ | 7.5 ± 2.8 | −0.85 | (−1.35, −0.35) | <0.001 |
| Lonely (vs. not) | 94.0 ±4.1 | −0.28 | (−0.74, 0.17) | 0.22 | 12.5 ± 4.8 | −0.19 | (−0.71, 0.34) | 0.49 | 37.0 ± 9.9 | −1.02 | (−2.08, 0.05) | 0.06 | 8.3 ± 2.6 | 0.03 | (−0.27, 0.33) | 0.85 |
| Mutually adjusted | ||||||||||||||||
| Socially isolated (vs. not) | −0.72 | (−1.60, 0.17) | 0.11 | −0.93 | (−1.95, 0.08) | 0.07+ | −1.42 | (−3.49, 0.65) | 0.18 | −0.54 | (−1.12, 0.04) | 0.07 | ||||
| Low social support (vs. not) | −1.17 | (−1.96, −0.39) | <0.001+ | −0.72 | (−1.63, 0.18) | 0.12 | −2.20 | (−4.03, −0.36) | 0.02+ | −0.70 | (−1.23, −0.18) | 0.01 | ||||
| Lonely (vs. not) | −0.27 | (−0.72, 0.19) | 0.25 | −0.17 | (−0.70, 0.35) | 0.51 | −0.98 | (−2.05, 0.08) | 0.07 | 0.04 | (−0.26, 0.34) | 0.79 | ||||
| Composite social health | ||||||||||||||||
| Positive | 94.6 ± 4.0 | Reference | 13.0 ± 4.6 | Reference | 39.3 ± 9.6 | Reference | 8.4 ± 2.6 | Reference | ||||||||
| Discordanta | 93.0 ± 4.5 | −1.45 | (−2.10, −0.80) | <0.001+ | 12.0 ± 4.7 | −0.82 | (−1.57, −0.08) | 0.03 | 36.7 ± 10.4 | −2.59 | (−4.11, −1.08) | <0.001 | 7.6 ± 2.8 | −0.87 | (−1.30, −0.44) | <0.001+ |
| Lonely | 94.0 ±4.1 | −0.33 | (−0.78, 0.12) | 0.15 | 12.5 ± 4.8 | −0.21 | (−0.73, 0.31) | 0.43 | 37 ± 9.9 | −1.10 | (−2.16, −0.04) | 0.04 | 8.3 ± 2.6 | 0.00 | (−0.30, 0.30) | 0.99 |
Note: Adjusted for age (continuous), gender, level of education (≤12 or >12 years), place of birth (Australia or not Australia), BMI (continuous) and CES-D score (<8 or ≥8).
signifies a statistically significant (p < 0.05) gender interaction.
Abbreviations: 3MS, Modified Mini-Mental State Examination; CI, confidence interval; COWAT, Controlled Oral Word Association Test; HVLT-R, Hopkin’s Verbal Learning Test–Revised; SD, standard deviation; SDMT, Symbol-Digit Modalities Test; β, Coefficient.
Discordant Social Health = socially isolated and/or low social support, but not lonely.
Among women, both social isolation and low social support were associated with poorer average performance on all cognitive tests (Tables 1 and D1). Following mutual adjustment for other social health components, social support displayed the strongest relationship among women (all outcomes except COWAT; Table 1). Among women, social health discordance was associated with lower average scores on all cognitive tests in both adjustment models, compared with positive social health (p < 0.05).
Among men, only social isolation was consistently associated with a lower score on the SDMT (Table 2).
TABLE 2.
Fully adjusted multivariable analyses of baseline social health and baseline cognitive function in men
| 3MS |
COWAT |
SDMT |
HVLT-R delayed recall |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | Mean ± SD | β | 95% CI | p Value | |
| 93.1 ± 4.5 | 11.8 ± 4.6 | 36.4 ± 9.7 | 7.4 ± 2.8 | |||||||||||||
| Socially isolated (vs. not) | 92.9 ± 4.6 | 0.14 | (−0.59, 0.86) | 0.71+ | 11.7 ± 4.6 | 0.24 | (−0.51, 0.99) | 0.53+ | 33.8 ± 8.8 | −1.79 | (−3.28, −0.30) | 0.02 | 7.2 ± 3.0 | 0.02 | (−0.44, 0.48) | 0.94+ |
| Low social support (vs. not) | 93.0 ± 4.5 | 0.32 | (−0.45, 1.09) | 0.41+ | 11.2 ± 4.5 | −0.34 | (−1.13, 0.46) | 0.40 | 36.0 ± 8.9 | 0.54 | (−1.06, 2.14) | 0.51+ | 6.9 ± 2.8 | −0.29 | (−0.77, 0.20) | 0.25 |
| Lonely (vs. not) | 92.4 ± 4.4 | −0.09 | (−0.70, 0.52) | 0.78 | 11.3 ± 4.1 | −0.33 | (−0.96, 0.30) | 0.31 | 34.3 ± 9.0 | −0.35 | (−1.60, 0.91) | 0.59 | 6.9 ± 2.9 | −0.17 | (−0.55, 0.22) | 0.40 |
| Mutually adjusted | ||||||||||||||||
| Socially isolated (vs. not) | 0.07 | (−0.68, 0.82) | 0.86 | 0.35 | (−0.42, 1.12) | 0.37+ | −2.03 | (−3.56, −0.49) | 0.01 | 0.10 | (−0.38, 0.57) | 0.69 | ||||
| Low social support (vs. not) | 0.31 | (−0.49, 1.10) | 0.45+ | −0.42 | (−1.24, 0.40) | 0.31 | 1.08 | (−0.57, 2.73) | 0.20+ | −0.31 | (−0.81, 0.19) | 0.23 | ||||
| Lonely (vs. not) | −0.09 | (−0.70, 0.52) | 0.77 | −0.33 | (−0.96, 0.30) | 0.30 | −0.30 | (−1.56, 0.95) | 0.64 | −0.17 | (−0.55, 0.22) | 0.40 | ||||
| Composite social health | ||||||||||||||||
| Positive | 93.1 ± 4.5 | Reference | 11.8 ± 4.6 | Reference | 36.6 ± 9.7 | Reference | 7.4 ± 2.8 | Reference | ||||||||
| Discordanta | 93.0 ± 4.6 | 0.24 | (−0.36, 0.83) | 0.44+ | 11.2 ± 4.4 | −0.40 | (−1.02, 0.21) | 0.20 | 34.7 ± 9.0 | −0.98 | (−2.22, 0.25) | 0.12 | 7.2 ± 2.9 | −0.07 | (−0.45, 0.31) | 0.71+ |
| Lonely | 92.4 ± 4.4 | −0.07 | (−0.68, 0.54) | 0.81 | 11.3 ± 4.1 | −0.35 | (−0.98, 0.28) | 0.27 | 34.3 ± 9.0 | −0.40 | (−1.66, 0.85) | 0.53 | 6.9 ± 2.9 | −0.17 | (−0.56, 0.22) | 0.39 |
Note: Adjusted for age (continuous), gender, level of education (≤12 or >12 years), place of birth (Australia or not Australia), BMI (continuous) and CES-D score (<8 or ≥8).
signifies a statistically significant (p < 0.05) gender interaction.
Abbreviations: 3MS, Modified Mini-Mental State Examination; CI, confidence interval; COWAT, Controlled Oral Word Association Test; HVLT-R, Hopkin’s Verbal Learning Test–Revised; SD, standard deviation; SDMT, Symbol-Digit Modalities Test; β, coefficient.
Discordant Social Health = socially isolated and/or low social support, but not lonely.
3.4 ∣. Social health and cognitive decline/dementia
Cognitive decline was observed in 14% (n = 1604) of the sample with 1.2% missing data (n = 133) over a median of 3.1-year follow-up (Table 3). There were no statistically significant associations between any of the social health components and cognitive decline (Table D2 in supporting information S1).
TABLE 3.
Fully adjusted multivariable analyses of longitudinal associations between social health and cognitive decline
| No cognitive decline n (%) |
Cognitive decline n (%) |
HR | 95% CI | p Value | |
|---|---|---|---|---|---|
| Women | 5230 (85.3%) | 824 (13.4%) | |||
| Socially isolated (vs. not) | 64 (81%) | 15 (19%) | 1.28 | (0.77, 2.15) | 0.35 |
| Low social support (vs. not) | 82 (80.4%) | 20 (19.6%) | 1.39 | (0.89, 2.18) | 0.14 |
| Lonely (vs. not) | 282 (85.2%) | 49 (14.8%) | 0.96 | (0.71, 1.30) | 0.81 |
| Mutually adjusted | |||||
| Socially isolated (vs. not) | 1.17 | (0.68, 2.01) | 0.57 | ||
| Low social support (vs. not) | 1.35 | (0.84, 2.15) | 0.21 | ||
| Lonely (vs. not) | 0.95 | (0.70, 1.29) | 0.75 | ||
| Composite social health | |||||
| Positive | 4836 (86.6%) | 750 (13.4%) | Reference | ||
| Discordanta | 112 (81.8%) | 25 (18.3%) | 1.31 | (0.87, 1.95) | 0.19 |
| Lonely | 282 (85.2%) | 49 (14.8%) | 0.97 | (0.72, 1.32) | 0.85 |
| Men | 4531 (84.4%) | 780 (14.5%) | |||
| Socially isolated (vs. not) | 122 (86.5%) | 19 (13.5%) | 0.92 | (0.58, 1.45) | 0.71 |
| Low social support (vs. not) | 103 (83.7%) | 20 (16.3%) | 1.19 | (0.76, 1.85) | 0.45 |
| Lonely (vs. not) | 181 (81.5%) | 41 (18.5%) | 0.91 | (0.64, 1.27) | 0.57 |
| Mutually adjusted | |||||
| Socially isolated (vs. not) | 0.88 | (0.55, 1.40) | 0.59 | ||
| Low social support (vs. not) | 1.22 | (0.77, 1.94) | 0.39 | ||
| Lonely (vs. not) | 0.91 | (0.64, 1.27) | 0.57 | ||
| Composite social health | |||||
| Positive | 4169 (85.5%) | 709 (14.5%) | Reference | ||
| Discordanta | 181 (85.8%) | 30 (14.2%) | 0.97 | (0.67, 1.40) | 0.88 |
| Lonely | 181 (81.5%) | 41 (18.5%) | 0.90 | (0.64, 1.27) | 0.57 |
Note: Derived from a population of 11,498 followed for mean 4.5 ± 1.2 SD years. Cognitive decline had 40,249 person years of observation (mean 3.5 ± 1.5 SD years; median 3.1, IQR 5.0-2.9 years; range 0.6 - 7.1 years). Adjusted for age (continuous), gender, level of education (≤12 or >12 years), place of birth (Australia or not Australia), BMI (continuous) and CES-D score (<8 or ≥8).
Abbreviations: CI, confidence interval; HR, hazard ratio.
Discordant Social Health = socially isolated and/or low social support, but not lonely.
Due to a small number of events and low prevalence of poor social health, gender stratification was not possible for the dementia analyses. Over a median 4.6-year follow-up, 3.5% (n = 406) of participants had a dementia trigger and 2% of participants (n = 229) had an adjudicated dementia event (Table 4). A slightly higher frequency of dementia cases was seen in men compared to women (2.4% and 1.7%, respectively; p = 0.007). Of socially isolated participants, 2.7% were diagnosed with dementia; among participants with low social support, 3.9% were diagnosed; and among lonely participants, 1.8% were diagnosed. Low social support was associated with an increased risk of a dementia trigger and subsequent adjudicated dementia diagnosis (but the latter was not significant). Social health discordance was associated with higher risk of dementia trigger in minimally adjusted models only (Table D4 in supporting information S1).
TABLE 4.
Fully adjusted multivariable analyses of longitudinal associations between social health and dementia
| No dementia n (%) |
Dementia n (%) |
HR | 95% CI | p Value | |
|---|---|---|---|---|---|
| Dementia trigger | 11,092 (96.5%) | 406 (3.5%) | |||
| Socially isolated (vs. not) | 216 (96%) | 9 (4%) | 0.94 | (0.46, 1.89) | 0.86 |
| Low social support (vs. not) | 215 (93.5%) | 15 (6.5%) | 1.75 | (1.04, 2.94) | 0.03 |
| Lonely (vs. not) | 536 (95.9%) | 23 (4.1%) | 0.92 | (0.59, 1.43) | 0.71 |
| Mutually adjusted | |||||
| Socially isolated (vs. not) | 0.76 | (0.37, 1.59) | 0.47 | ||
| Low social support (vs. not) | 1.87 | (1.09, 3.21) | 0.02 | ||
| Lonely (vs. not) | 0.91 | (0.58, 1.42) | 0.69 | ||
| Composite social health | |||||
| Positive | 10,223 (96.6%) | 362 (3.4%) | Reference | ||
| Discordanta | 333 (94.1%) | 21 (5.9%) | 1.54 | (0.98, 2.42) | 0.06 |
| Lonely | 536 (95.9%) | 23 (4.1%) | 0.94 | (0.60, 1.47) | 0.79 |
| Dementia case | 11,269 (98%) | 229 (2%) | |||
| Socially isolated (vs. not) | 219 (97.3%) | 6 (2.7%) | 1.22 | (0.54, 2.75) | 0.64 |
| Low social support (vs. not) | 221 (96.1%) | 9 (3.9%) | 1.78 | (0.91, 3.48) | 0.09 |
| Lonely (vs. not) | 549 (98.2%) | 10 (1.8%) | 0.72 | (0.37, 1.41) | 0.34 |
| Mutually adjusted | |||||
| Socially isolated (vs. not) | 1.00 | (0.42, 2.38) | 0.99 | ||
| Low social support (vs. not) | 1.79 | (0.88, 3.63) | 0.11 | ||
| Lonely (vs. not) | 0.72 | (0.37, 1.40) | 0.34 | ||
| Composite social health | |||||
| Positive | 10,378 (98%) | 207 (2%) | Reference | ||
| Discordanta | 342 (96.6%) | 12 (3.4%) | 1.54 | (0.86, 2.76) | 0.15 |
| Lonely | 549 (98.2%) | 10 (1.8%) | 0.74 | (0.38, 1.44) | 0.38 |
Note: Derived from a population of 11,498 followed for mean 4.5 ± 1.2 SD years. Dementia trigger had 51,151 person years of observation (mean 4.4 ± 1.3 SD years; median 4.5, IQR 5.5-3.5 years; range 0.2 - 7.3 years). Dementia cases had 51,400 person years of observation (mean 4.5 ± 1.2 SD years; median 4.5, IQR 5.5-3.5 years; range 0.2–7.3 years). Adjusted for age (continuous), gender, level of education (≤12 or >12 years), place of birth (Australia or not Australia), BMI (continuous) and CES-D score (<8 or ≥8).
Abbreviations: CI, confidence interval; HR, hazard ratio.
Discordant Social Health = socially isolated and/or low social support, but not lonely.
There was no difference in findings when depressive symptoms was removed as a confounder (Appendix E in supporting information S1), when depressive symptoms were redefined without inclusion of the loneliness item (data not shown), or when events/participants censored in the first half-year were removed (data not shown). There were no interaction with aspirin treatment for any of the analyses (data not shown). No dose-response relationships were observed (Appendix F in supporting information S1). When inclusion was restricted to active participants without events after one year from randomisation, the magnitude of associations became stronger (low social support with dementia trigger HR = 1.91, p = 0.01; after mutual adjustment HR = 2.01, p = 0.01). Additionally, low social support was associated with incident dementia (HR = 1.98, p = 0.05) and the social health category ‘discordant, not lonely’ with dementia trigger (HR = 1.70, p = 0.02).
4 ∣. DISCUSSION
Among women, social isolation, low social support and social health discordance were consistently cross-sectionally associated with lower cognitive function. However, social health was not associated with cognitive decline or dementia among men or women. Despite men reporting more social isolation and less social support than women, the relation between social health and cognitive function was largely absent among men. By assessing the individual contribution of different components of social health, our study was able to identify that they do not contribute separately to cognitive health, providing a strong foundation for future studies.
4.1 ∣. Social health and baseline cognitive function
Despite reporting of gender differences in social health, there is scarce consideration of these differences in current literature.20,21 The cross-sectional findings observed for women in our study are broadly supported by previous research indicating that poor social support and social isolation are associated with worse cognitive function. Four of the five studies assessing cross-sectional social support and global cognition in Kelly et al.'s systematic review reported positive associations, with the fifth study reporting null findings.32-35 Half (n = 3) of the studies assessing cross-sectional associations between network size (comparable to ‘social isola-tion’) and global cognitive function in Kelly et al.’s review, reported an association, and the other half (n = 3) not.36-41 Given the lack of gender stratification in these earlier studies, it is possible that the effect magnitudes reported are being diluted by the inclusion of men (who comprise between 31.6% and 55.1% of the samples).
Our finding of no association between loneliness and baseline cognition, among women or men, is inconsistent with prior research. Kelly et al. did not specifically assess loneliness, but included loneliness as a component of social relationships, and reported an association between the latter and cognitive health.15 The only identifiable study that sought a cross-sectional relationship between loneliness and cognitive function was that of Ellwardt et al., who reported that loneliness was indirectly associated with lower global cognition in men and women aged 55–85.32,42
Among women, poor social support, social isolation and social health discordance were associated with worse cognitive function across different domains of cognition. Among men, the only association observed was social isolation with poorer performance on the SDMT. Despite not specifically analysing episodic memory as an outcome, Kelly et al. and Kuiper et al. incidentally included seven unique studies, assessing a component of episodic memory (delayed recall).33,42-47 All of these studies reported significant associations between social health and episodic memory, with none discussing effect size comparative to measures of other aspects of cognition.33,42-47 Many of the initial signs of poor cognition and dementia, in particular Alzheimer's disease, reflect episodic memory problems before it is displayed in other cognitive domains.48 Hence the large effect size we observed for women in the HVLT-R could be indicative of the early stages of cognitive impairment which is not yet demonstrated in other cognitive domains.48
McHugh Power et al. performed two studies, one utilising 3098 participants aged over 60 from the Irish and English Longitudinal Studies of Ageing (TILDA and ELSA), and one utilising TILDA and Swedish National Study on Aging and Care in Kungholmen (SNAC-K) cohorts.1,49 In both studies, McHugh Power et al. reported associations between social health discordance (socially isolated but not lonely) and higher cross-sectional cognitive function, which was consistent with our finding among women.1,49 McHugh Power et al. also reported an association between concordant groups (low and high lonely) and cognition, which is inconsistent with our concordant social health (positive and negative social health) null finding.1 However, the results in these studies are not directly comparable as (1) McHugh Power et al. did not stratify by gender, had a younger sample aged 60 years and over, and did not exclude individuals with serious chronic diseases and (2) our definitions of concordance and discordance varied slightly due to a lack of power.1,49 This could mean that the associations between social health and cognitive health observed at younger ages and/or in less healthy populations are not generalisable to older individuals in relatively good health.
4.2 ∣. Social health and cognitive decline/dementia
We did not identify an association between social health (any of its components) and either cognitive decline or dementia. This contrasts with some previous findings from the literature that have used different definitions of social health. Among 5604 individuals aged 60–99 years participating in the ELSA, discrepancy in social health was predictive of immediate and delayed recall at 2 years; however, no association was found over longer periods.1 A systematic review including 33 studies with a median follow-up of 7 years (range 1–32 years) found that poor social engagement was associated with a 56% increased risk of dementia; low social interaction, a small social network and a low level of social activity (i.e., being socially isolated), and low social support were all risk factors for this disorder.17 Penninkilampi's meta-analysis reported a statistically non-significant association between loneliness and dementia (magnitude of effect p = 0.063); however, included only four studies directly assessing this relationship over a median follow-up of 5.9 years, thus, the findings are not conclusive.17 Kuiper et al. conducted two systematic reviews: one on social relationships and risk of dementia, and one on social relationships and cognitive decline. The latter review utilised 43 studies with follow-ups of 1–15 years, and reported an overall association between poor social relationships, small social networks, loneliness and increased cognitive decline.13 Kuiper's study on dementia included 19 studies with follow-up ranging from 2 to 15 years. They reported that low social participation and less social contact were associated with a 41% increased risk of dementia, while loneliness was found to increase the risk of dementia by 58%.16
In contrast to Penninkilampi et al., but consistent with our study, Kuiper et al. reported that low social support or satisfaction for social network (comparable to social support) was not associated with dementia.13,17 Similarly, a recent study across two cohorts of 4514 Dutch and 2112 Swedish older people (≥10-year follow-up) reported no associations between social support with cognitive decline or incident dementia; however, loneliness was associated.50 In a study of 823 older adults followed for up to 4 years, risk of Alzheimer's disease was reported to double in lonely people when compared with those who were not lonely.51 While we observed no association between lower social health and dementia diagnosis, we did observe an association between low social support and experiencing a dementia trigger. As only about 60% of participants triggering a dementia assessment were subsequently adjudicated as demented in ASPREE,23 these findings might suggest that a lack of statistical power could partly account for the null findings in our analysis, especially because the study population was relatively healthy at baseline and a low proportion experienced poor social health. Other explanations for the discordant findings between our study and previous reports must also be considered. Many previous studies did not adjust for depressive symptoms in their analyses when assessing the relationship between social health and dementia, although depression is a likely confounding factor. Prior studies have observed that poor social health leads to a higher rate of depressive symptoms, and there are recent reports of the reverse causation also holding true.52 However, when presence of depressive symptoms was removed as a confounder, our findings of null relationships between social health with a dementia trigger or incidence did not alter. Finally, we observed gender differences in the association between social health and dementia; however, this study did not have the power to stratify by gender for longitudinal analyses. Despite two recent papers reporting no gender difference, we recommend based on our findings, future analyses should consider further the potential effect modification by gender on these associations.53,54
Several possible pathways for the link between social health and cognitive health have been proposed: the stress hypothesis in which glucocorticoid hypersecretion increases rate of hippocampal degeneration55; the vascular hypothesis which states poor social health increases the risk of cardiovascular and chronic disease, which in turn increases the risk of neurodegenerative disease56; and the cognitive reserve hypothesis which postulates that social environments and support provide cognitive resilience, and those with poor social health experience cognitive deficits, putting them more at risk of developing a dementia.57-59 Alternatively, the health selection model suggests that a decline in cognitive functioning limits social involvement, via behavioural and cognitive changes.60
4.3 ∣. Limitations and strengths
The initially healthy sample coupled with the 5-year follow-up period did not provide enough power to stratify longitudinal analyses by gender. The study could be improved by a longer follow-up period as the extended pre-clinical non-symptomatic stage of dementia and slow progression of cognitive decline means a longer duration of follow-up may be required in an initially healthy sample to reach a stage of clinical symptoms. The initially healthy sample also lacked variability in social health; 92% reported positive social health across all three constructs, a much higher proportion than other studies.61-64 High rates of positive social health were likely due to the recruitment strategy and general good health of the sample, but could be considered as a limiting factor when appraising the generalisability of these findings to the broader population. Residual confounding through unmeasured variables (diabetes mellitus, hypertension, rurality and socio-economic status) may be present. Additionally, as our participants were relatively healthy at baseline, and were mainly white and community-dwelling, generalisability may be further restricted due to culture, healthcare systems, and socio-economic standing.24 Loneliness was part of the depressive symptoms scale, however adjustment (or not) for depressive symptoms did not alter finding.
Strengths include analysis of a large study with high integrity, very little attrition, validated measurement of outcomes (cognition and dementia), and low misclassification bias due to continuing review of medical records even in the event of attrition. Findings are generalisable to community-dwelling people who reach age 70 without overt disease. Past studies have utilised inconsistent definitions of social health, have not assessed multiple constructs of social health, or have utilised a one-dimensional definition (e.g., social network size as the definition of social isolation). Our project's multifaceted definitions of social isolation and social support increase the strength of the results.
5 ∣. CONCLUSION
Our findings demonstrate that poor social health in women was consistently associated with lower cognitive function at baseline. The longitudinal analyses reported that social health did not predict incident cognitive decline or dementia, but we lacked power to stratify these by gender; we hypothesise that these longitudinal associations are also gender-dependent. As social health is cross-sectionally associated with cognition in older adults, health professionals may need to consider simultaneously approaches to cognitive maintenance and social health, which is currently not commonly assessed as a part of primary care.
Supplementary Material
Key points.
Low social isolation and greater social support were consistently associated with higher cognitive function among healthy Australian women aged 70–94
Over 5 years, no consistent longitudinal associations were observed between social isolation, social support, or loneliness with cognitive change or incident dementia
The relationships between social health and cognitive health are likely gender-specific; as our sample was healthy at baseline, a longer observation is required for gender-stratified analyses
ACKNOWLEDGEMENTS
We are incredibly appreciative of all participants, funding bodies, and research and administration teams for their contributions, without whom this research would not have been possible.
The ASPREE trial was funded by the US National Institute on Aging and the National Cancer Institute at the National Institutes of Health (grant number U01AG029824); the National Health and Medical Research Council of Australia (grant numbers 334047, 1127060); Monash University (Australia); and the Victorian Cancer Agency (Australia; 2009001512). ALSOP was supported by funding from Monash University, ANZ Trustees, the Wicking Trust and the Mason Foundation (2012001813). RFP is supported by an Australian Heart Foundation post-doctoral fellowship (101927).
Footnotes
CONFLICT OF INTERESTS
The authors declare no conflicts of interest. All data collection, analysis, and interpretation; the writing of the manuscript and its submission for publication were performed solely at the discretion of the researchers, independent of the funders.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher's website.
DATA AVAILABILITY STATEMENT
Data cannot be shared for legal and ethical reasons. Data cannot be shared publicly as data are part of a large ongoing observational cohort with a rigorous process to access data. Data are available from Monash University for researchers who meet the criteria (contact via https://aspree.org/aus/for-researchers; aspree@monash.edu).65
REFERENCES
- 1.McHugh Power JE, Kenny RA, Lawlor BA, Steptoe A, Kee F. The discrepancy between social isolation and loneliness as a clinically meaningful metric: findings from the Irish and English longitudinal studies of ageing (TILDA and ELSA). Int J Geriatr Psychiatry. 2017;32(6):664–674. [DOI] [PubMed] [Google Scholar]
- 2.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. [DOI] [PubMed] [Google Scholar]
- 3.Boden-Albala B, Litwak E, Elkind MSV, Rundek T, Sacco RL. Social isolation and outcomes post stroke. Neurology. 2005;64(11):1888–1892. [DOI] [PubMed] [Google Scholar]
- 4.Brock AM, O'Sullivan P. A study to determine what variables predict institutionalization of elderly people. J Adv Nurs. 1985;10(6): 533–537. [DOI] [PubMed] [Google Scholar]
- 5.Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eng PM, Rimm EB, Fitzmaurice G, Kawachi I. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am J Epidemiol. 2002;155(8):700–709. [DOI] [PubMed] [Google Scholar]
- 7.Holt-Lunstad J, Smith TB. Social relationships and mortality. Soc Personality Psychol Compass. 2012;6(1):41–53. [Google Scholar]
- 8.Nicholson N. A review of social isolation: an important but under-assessed condition in older adults. J Prim Prev. 2012;33(2):137–152. [DOI] [PubMed] [Google Scholar]
- 9.Commissioner for Senior Victorians. Ageing Is Everyone's Business. Victorian Government, Department of Health and Human Services; 2016. [Google Scholar]
- 10.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. [DOI] [PubMed] [Google Scholar]
- 11.Hale CJ, Hannum JW, Espelage DL. Social support and physical health: the importance of belonging. J Am Coll Health. 2005;53(6):276–284. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan HB, Cassel CJ, Gore CS. Social support and health. Med Care. 1977;15(5):47–58. [DOI] [PubMed] [Google Scholar]
- 13.Kuiper J, Zuidersma M, Zuidema S, et al. Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol. 2016;45(4):1169–1206. [DOI] [PubMed] [Google Scholar]
- 14.Freak-Poli R, Ryan J, Tran T, et al. Social isolation, social support and loneliness as independent concepts, and their relationship with health-related quality of life among older women. Aging Ment Health. 2021:1–10. [DOI] [PubMed] [Google Scholar]
- 15.Kelly ME, Duff H, Kelly S, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev. 2017;6(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuiper JS, Zuidersma M, Oude Voshaar RC, et al. Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015;22(1):39–57. [DOI] [PubMed] [Google Scholar]
- 17.Penninkilampi R, Casey A-N, Singh MF, Broadaty H. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J Alzheimer's Dis. 2018;66(4):1619–1633. [DOI] [PubMed] [Google Scholar]
- 18.Schaie KW. The course of adult intellectual development. Am Psychol. 1994;49(4):304–313. [DOI] [PubMed] [Google Scholar]
- 19.Nebel RA, Aggarwal NT, Barnes LL, et al. Understanding the impact of sex and gender in Alzheimer's disease: a call to action. Alzheimers Dement. 2018;14(9):1171–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aartsen M, Jylha M. Onset of loneliness in older adults: results of a 28 year prospective study. Eur J Ageing. 2011;8(1):31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gul SN, Chishti R, Bano M. Gender differences in social support, loneliness, and isolation among old age citizens. Peshawar J Psychol Behav Sci. 2018;4(1):15–31. [Google Scholar]
- 22.McNeil JJ, Woods RL, Nelson MR, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379(16):1499–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryan J, Storey E, Murray AM, et al. Randomized placebo-controlled trial of the effects of aspirin on dementia and cognitive decline. Neurology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McNeil JJ, Woods RL, Ward SA, et al. Cohort profile: the ASPREE Longitudinal Study of Older Persons (ALSOP). Int J Epidemiol. 2019;48(4):1048–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McNeil JJ, Woods RL, Nelson MR, et al. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J Gerontol A Biol Sci Med Sci. 2017;72(11):1586–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lubben EJ. Assessing social networks among elderly populations. Fam Commun Health. 1988;11(3):42–52. [Google Scholar]
- 27.Ryan J, Woods RL, Britt C, et al. Normative performance of healthy older individuals on the Modified Mini-Mental State (3MS) examination according to ethno-racial group, gender, age, and education level. Clin Neuropsychologist. 2019;33(4):779–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nutter-Upham KE, Saykin AJ, Rabin LA, et al. Verbal fluency performance in amnestic MCI and older adults with cognitive complaints. Arch Clin Neuropsychol. 2008;23(3):229–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith A. Symbol Digit Modalities Test (SDMT) Manual (Revised). Western Psychological Sevices; 1982. [Google Scholar]
- 30.Kuiper JS, Smidt N, Zuidema SU, Comijs HC, Oude Voshaar RC, Zuidersma M. A longitudinal study of the impact of social network size and loneliness on cognitive performance in depressed older adults. Aging Ment Health. 2019:1–9. [DOI] [PubMed] [Google Scholar]
- 31.Grimm R, McNeil JJ, Applegate W, et al. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials. 2013;36(2):555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellwardt L, Aartsen M, Deeg D, Steverink N. Does loneliness mediate the relation between social support and cognitive functioning in later life? Soc Sci Med. 2013;98(1):116–124. [DOI] [PubMed] [Google Scholar]
- 33.Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychol. 2001;20(4):243–255. [DOI] [PubMed] [Google Scholar]
- 34.Hughes TF, Andel R, Small BJ, Borenstein AR, Mortimer JA. The association between social resources and cognitive change in older adults: evidence from the charlotte county healthy aging study. J Gerontol B Psychol Sci Soc Sci. 2008;63(4):241–244. [DOI] [PubMed] [Google Scholar]
- 35.Chen T-Y, Chang H-Y. Developmental patterns of cognitive function and associated factors among the elderly in Taiwan. Sci Rep. 2016;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barnes LL, Mendes De Leon FC, Wilson SR, Bienias LJ, Evans AD. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. 2004;63(12):2322–2326. [DOI] [PubMed] [Google Scholar]
- 37.Holtzman RE, Rebok GW, Saczynski JS, Kouzis AC, Wilcox Doyle K, Eaton WW. Social network characteristics and cognition in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2004;59(6):P278–P84. [DOI] [PubMed] [Google Scholar]
- 38.Fo B, Zunzunegui M-V, Alvarado B, Otero A, del Ser T. Trajectories of cognitive decline and social relations. J Gerontol B Psychol Sci Soc Sci. 2005;60(6):320–330. [DOI] [PubMed] [Google Scholar]
- 39.Kimura D, Takeda T, Ohura T, Imai A. Evaluation of facilitative factors for preventing cognitive decline: a 3-year cohort study of community intervention. Psychogeriatrics. 2017;17(1):9–16. [DOI] [PubMed] [Google Scholar]
- 40.Ma -V Zunzunegui, Alvarado BE, Del Ser T, Otero A. Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):S93–S100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ho SC, Woo J, Sham A, Chan SG, Yu ALM. A 3-year follow-up study of social, lifestyle and health predictors of cognitive impairment in a Chinese older cohort. Int J Epidemiol. 2001;30(6):1389–1396. [DOI] [PubMed] [Google Scholar]
- 42.Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom Med. 2013;75(2):161–170. [DOI] [PubMed] [Google Scholar]
- 43.Albert MS, Jones K, Savage CR, et al. Predictors of cognitive change in older persons: MacArthur studies of successful aging. Psychol Aging. 1995;10(4):578–589. [DOI] [PubMed] [Google Scholar]
- 44.Bosma H, van Boxtel MPJ, Ponds RWHM, et al. Engaged lifestyle and cognitive function in middle and old-aged, non-demented persons: a reciprocal association? Z für Gerontol Geriatr. 2002;35(6):575–581. [DOI] [PubMed] [Google Scholar]
- 45.Bourassa KJ, Memel M, Woolverton C, Sbarra DA. Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging Ment Health. 2017;21(2):133–146. [DOI] [PubMed] [Google Scholar]
- 46.Ertel KA, Glymour MM, Berkman LF. Effects of social integration on preserving memory function in a nationally representative US elderly population. Am J Publ Health. 2008;98(7):1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nelson L, Noonan C, Goldberg J, Buchwald D. Social engagement and physical and cognitive health among American Indian participants in the health and retirement study. J Cross-Cult Gerontol. 2013;28(4):453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vandenberghe R, Tournoy J. Cognitive aging and Alzheimer’s disease. Postgrad Med J. 2005;81(956):343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McHugh Power J, Sjöberg L, Kee F, Kenny R, Lawlor B. Comparisons of the discrepancy between loneliness and social isolation across Ireland and Sweden: findings from TILDA and SNAC-K. Int J Res Soc Genet Epidemiol Ment Health Serv. 2019;54(9):1079–1088. [DOI] [PubMed] [Google Scholar]
- 50.Freak-Poli R, Wagemaker N, Wang R, et al. Loneliness, not social support, is associated with cognitive decline and dementia across two longitudinal population-based cohorts. J Alzheimer's Dis. 2021. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson RS, Krueger KR, Arnold SE, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. 2007;64(2):234–240. [DOI] [PubMed] [Google Scholar]
- 52.McHugh Power J, Hannigan C, Hyland P, Brennan S, Kee F, Lawlor BA. Depressive symptoms predict increased social and emotional loneliness in older adults. Aging Ment Health. 2020;24(1):110–118. [DOI] [PubMed] [Google Scholar]
- 53.Sutin AR, Stephan Y, Luchetti M, Terracciano A. Loneliness and risk of dementia. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luchetti M, Terracciano A, Aschwanden D, Lee JH, Stephan Y, Sutin AR. Loneliness is associated with risk of cognitive impairment in the Survey of Health, ageing and Retirement in Europe. Int J Geriatr Psychiatry. 2020;35(7):794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McEwen BS, Krey LC, Sapolsky RM. The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Endocr Rev. 1986;7(3):284–301. [DOI] [PubMed] [Google Scholar]
- 56.Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3(6):343–353. [DOI] [PubMed] [Google Scholar]
- 57.Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355(9212):1315–1319. [DOI] [PubMed] [Google Scholar]
- 58.Miceli S, Maniscalco L, Matranga D. Social networks and social activities promote cognitive functioning in both concurrent and prospective time: evidence from the SHARE survey. Eur J Ageing. 2018;16(2):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Evans I, Llewellyn D, Matthews F, Brayne C, Clare L. Social isolation, cognitive reserve, and cognition in healthy older people. PLoS One. 2018;13(8):e0201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hackett RA, Steptoe A, Cadar D, Fancourt D. Social engagement before and after dementia diagnosis in the English Longitudinal Study of ageing.(Research article)(Report). PLoS One. 2019;14(8):e0220195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bolton M. The State We're in: A Report of Evidence Compiled for the Campaign to End Loneliness. Age UK Oxfordshire; 2012. [Google Scholar]
- 62.Consumers Health Forum of Australia. Time for national action on loneliness, the unnoticed epidemic. Target News Serv. 2021. [Google Scholar]
- 63.Crowe CL, Domingue BW, Graf GH, Keyes KM, Kwon D, Belsky DW. Associations of loneliness and social isolation with health span and life span in the U.S. health and retirement study. J Gerontol A. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jamieson HA, Gibson HM, Abey-Nesbit R, Ahuriri-Driscoll A, Keeling S, Schluter PJ. Profile of ethnicity, living arrangements and loneliness amongst older adults in Aotearoa New Zealand: a national cross-sectional study. Australas J Ageing. 2018;37(1):68–73. [DOI] [PubMed] [Google Scholar]
- 65.ASPREE Protocol Version 9. Monash University Department of Epidemiology and Preventative Medicine, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared for legal and ethical reasons. Data cannot be shared publicly as data are part of a large ongoing observational cohort with a rigorous process to access data. Data are available from Monash University for researchers who meet the criteria (contact via https://aspree.org/aus/for-researchers; aspree@monash.edu).65