Abstract
Purpose of Review
The purpose of this review is to describe Trauma-Informed Guilt Reduction Therapy (TrIGR), the Non-Adaptive Guilt and Shame (NAGS) model that underlies TrIGR, and the research supporting the use of TrIGR to treat the guilt and shame components of moral injury. TriGR is a 6-session individual psychotherapy that helps clients consider their role in the traumatic event and find constructive ways to express important values, so that they no longer need to express values by suffering through guilt and shame.
Recent Findings
A recently completed randomized controlled trial of TrIGR versus supportive care therapy included 144 post-9/11 veterans. TriGR showed greater reductions in trauma-related guilt, PTSD symptoms, and depression symptoms. Participants in TrIGR had greater likelihood of losing their PTSD diagnosis and showing clinical meaningful change in PTSD and depression symptoms. Mean attendance was high; 5.3 out of 6 sessions.
Summary
TrIGR is efficacious in reducing guilt that is common to moral injury as well as PTSD and depression symptoms among combat veterans. The next steps in the program of research to develop and evaluate TrIGR are studies with diverse trauma types and populations as well as relative effectiveness studies comparing TrIGR to other evidence-based treatments for moral injury and PTSD.
Keywords: Moral injury, Trauma-related guilt, Trauma-related shame, PTSD, Depression, Psychotherapy
Introduction
The purpose of this review is to describe Trauma-Informed Guilt Reduction Therapy (TrIGR), the Non-Adaptive Guilt and Shame (NAGS) model that underlies TrIGR, and the research supporting the use of TrIGR to treat the guilt and shame components of moral injury.
Guilt and shame are hallmark features of moral injury
While there is no one consensus definition of moral injury, it is generally considered to be the long-term psychological, behavioral, social, and sometimes spiritual distress that occurs after one experiences an event that violates deeply held morals and values [1, 2•]. Two hallmark symptoms of moral injury are guilt and shame [1, 2•, 3]. Guilt is a hybrid of negative thoughts and emotions that arises when people blames themselves for all or part of the negative outcome of an event (e.g., “I did something bad”) [4]. Shame is when one judges not just their actions but their entire self negatively (e.g., “I am bad”) [5]. Difficulty forgiving oneself for the transgression of values is also considered common in moral injury [6].
Trauma-related guilt such as that seen in moral injury occurs frequently among trauma survivors [7]. For example, one study of VA enrolled veterans who had experienced trauma found that over 40% reported that they had experienced guilt in the past month [7]. In addition to being common, trauma-related guilt is associated with a variety of negative post-traumatic mental health outcomes. In our research with veterans, we have found that trauma-related guilt is positively associated with the severity of PTSD and depression symptoms [8, 9], with aggression [10], and with poorer overall psychosocial functioning and in the specific domains of interpersonal functioning, professional functioning, and self-care [11]. Extent work shows it is also associated with suicidal ideation, even when controlling for combat exposure or PTSD symptoms [12, 13].
For people with PTSD, trauma-related guilt is one of the symptoms likely to linger, even after successful PTSD treatment [14, 15]. Research with clinicians shows that they find moral injury, and guilt specifically, challenging to treat and an area where they would like more intervention strategies [16, 17]. Less is known about trauma-related shame because a measure to assess such shame was only recently validated and published [18]. However, studies suggest that trauma-related guilt in the absence of shame is rare and that shame may in fact explain much of the variance in the associations between guilt and negative outcomes [10, 19]. Because moral injury and the associated hallmark symptoms of guilt and shame are common, distressing, debilitating, and challenging to treat, we developed Trauma-Informed Guilt Reduction Therapy (TrIGR).
Developing TrIGR
Our study team’s attention was first drawn to moral injury and specifically the guilt and shame components in our clinical work with combat veterans who had served in Iraq and Afghanistan. Many were coming in for mental health treatment with primary presentation of moral injury, having to live with something they did or did not do in the context of war that went against their morals and values, with guilt and shame prominent in their clinical presentation. Many had PTSD but some did not, so not all were appropriate for PTSD treatment. Some had completed disorder specific treatment (e.g., PTSD, depression) but still had prominent and debilitating guilt. We saw in our work and in the extent literature [16, 17] that therapists were asking for more information on how to treat this kind of moral injury based, trauma-related guilt.
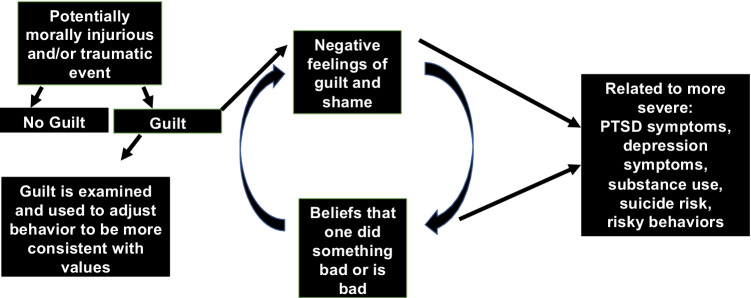
To develop TrIGR, we first conceived a model of how trauma-related guilt and shame affect mental health which we called the Non-Adaptive Guilt and Shame (NAGS) model (Fig. 1) [9, 20]. According to the NAGS model, some people experience guilt after a traumatic event, while some do not. Among those who do experience guilt, some use the negative feelings of guilt as an opportunity to assess what values were violated (e.g., “What did I do that makes me feel so awful? How do I avoid feeling this way again?”). In such cases, guilt may help people make choices that are more in line with their values. However, sometimes people avoid thinking about the event and guilt feelings. Or their guilt stems from an event where there was no good choice and any choice would have led to a negative outcome (e.g., certain combat situations). The negative feeling of guilt may be seen as evidence that someone did something wrong, and the sense that someone did something wrong may lead to further negative feelings, creating a cycle of feeling more guilt and more guilty. The guilt becomes shame if the person comes to believe that not only did they do something bad, but that they are bad because of what they did. This cycle of negative thoughts and affect contributes to the severity of symptoms of common posttraumatic mental health problems such as PTSD and depression. This cycle can also contribute to self-destructive behaviors such as substance use, suicide risk, and high-risk behaviors. It may also contribute to poor or ambivalent engagement in treatment because people may come to believe that they do not deserve to feel good or do well.
Fig. 1.
Non-adaptive guilt and shame (NAGS) model.
We mapped the TrIGR intervention onto the NAGS model to end the cycle of guilt and shame that contributes to the severity of mental health problems and high-risk behaviors [9, 20]. The goal is to target guilt and shame to reduce some of the psychological, behavioral, social, and sometimes spiritual distress of moral injury. The overarching objective of TrIGR is to help clients consider their role in the traumatic event more comprehensively than they have previously and to help them find constructive ways to express important values, so that they no longer need to express values through suffering and high-risk behaviors (e.g., “I did something awful so now I deserve to suffer).” To help clients appraise their role in the trauma, the therapist guides the client through evaluation of four types of cognitions identified by Kubany and colleagues [4, 21]. Hindsight bias (e.g., “I knew exactly how things would turn out that day”) is challenged by helping clients remember what they really knew and had the power to do at the time. The therapist and client then examine what options the client had during at the time and how each option may have played out. Clients often come to terms during this exercise with the idea that there were no good options available at the time, and that all options would have led to some bad outcome. We then help people consider the full context of what happened and the many factors that contributed to the outcome. Finally, we help people consider whether they purposely intended the bad outcome that occurred. In the last module of TrIGR, the therapist helps the client find ways to express their values in more positive ways than by feeling guilt and shame, and helps people make plan to spend time doing activities that are meaningful to them and consistent with their values.
In terms of logistics, TriGR is a 6-session individual manualized intervention. The first two sessions of TriGR cover psychoeducation about trauma-related guilt and shame and the NAGS model. The second two sessions focus on processing the trauma and guilt and shame by debriefing the four common cognitions. The final two sessions focus on understanding what values were violated during the trauma, identifying important values, and creating a plan for how to live more in-line with important values. Clients are assigned homework after each session which includes reading psychoeducational materials about guilt, listening to a recording of the session, and keeping a log of cognitions that cause feelings of guilt and shame (e.g., “I should have known better than to…”). Clients track their activities leading into the values portion of the treatment (i.e., the final two sessions) to help identify ways to build more value-driven activities into their schedule. TrIGR can be delivered in person or through video conferencing.
TrIGR was designed to be easy to learn and implement by therapists familiar with cognitive behavioral therapy models. In our research studies, therapists have included clinical psychology pre- and post-doctoral trainees and licensed psychologists and social workers. Therapists new to TrIGR can learn the intervention through the manual and workbook which are published together in one book [20]. The treatment manual walks therapists through delivering the intervention session by session with clinical examples based on different kinds of traumas. The workbook includes client psychoeducational materials and assignments. The book also includes chapters on preparing clients for TrIGR, troubleshooting clinical situations that may arise, and therapist self-care.
TrIGR is one of several interventions that was developed to address one or more aspects of moral injury. Others include Adaptive Disclosure [22] which focuses on strategies that are consistent with military culture to promote self-forgiveness and reparative action. The therapy is also designed to help with anger and grief from moral injury if they are present. Impact of Killing is a cognitive behavioral intervention focused on moral injury from killing others in combat [23]. The therapy discusses physiology of killing responses, self-forgiveness, spirituality, making amends, and maintaining functional gains. Building Spiritual Strength [24] addresses the spiritual strain of moral injury and works to enhance religious meaning making. The Self-Forgiveness Workbook is a 6-h self-guided intervention designed to facilitate self-forgiveness and reduce self-condemnation among people who perpetrated of interpersonal offenses [25]. TrIGR is best suited when guilt and shame are present and prominent in a client’s presentation. If a client prefers to take a more spiritual focus to their guilt and shame, Building Spiritual Strength may be a better choice. If a client’s moral injury presents most strongly as anger or loss, Adaptive Disclosure may be the better choice. For someone who prefers self-help, the Self-Forgiveness Workbook may be a good starting point. It is likely that for some clients there is no one right choice. For example, someone who has guilt from killing in combat may benefit from TrIGR or Impact of Killing. If these are both available, shared decision making with the therapist and client may be a good method by which to decide on a treatment direction.
TrIGR research
We set out to evaluate TrIGR using Onken’s stages of behavioral treatment development [26]. In summary, stage I is development and preliminary testing of the intervention, usually focused on gathering feasibility and pilot data. Studies at this stage often use single condition pre-post designs. Stage II is efficacy testing in a research setting. Randomized controlled trials are the most common design used for stage II studies. Stage III continues efficacy work while introducing elements of “real world” effectiveness such as conducting the trial in community settings or with community-based providers but maintaining a high level of control to maintain high internal validity. Stage IV moves further into effectiveness and stage V focuses on dissemination and implementation.
First pilot and feasibility study
Our first pilot trial of TrIGR (stage I) was a pre-post study with thirteen veterans who served in Iraq or Afghanistan, had guilt from a combat trauma, and met diagnostic criteria for PTSD [9]. Ten completed the intervention. We measured trauma-related guilt, PTSD symptoms and depression. Results showed pre to post reductions in all three outcomes. Overall trauma-related guilt distress (from 3.0, SD = .48 to 2.4, SD = .89, Cohen’s d = 1.37) and trauma-related cognitions (from 2.1, SD = .99 to 1.3, SD = .75, Cohen’s d = 1.53) as measured by the Trauma-Related Guilt Inventory [27] reduced significantly.
In addition to examining if pre- to post-treatment change in PTSD and depression symptoms was statistically significant, we examined if change in PTSD symptoms was clinically noticeable (computed in previous studies to be a 10-point decrease on the Clinician Administered PTSD Scale for DSM-IV [CAPS] [28]; defined as representing a meaningful improvement in the life of someone with chronic PTSD [29, 30, 31]; and if change in depression was clinically significant (computed in a previous study to be 5-point decrease on the Physician Health Questionnaire-9 [PHQ-9] [32, 33]. Specifically, a 5-point change on the PHQ-9 has been shown to correspond with a moderate effect size on multiple domains of health-related quality of life and functional status [33]. Scores on the CAPS showed clinically meaningful change of over 18 points, from M = 81.4 (SD = 20.3) to M = 62.0 (SD = 36.5). Depression symptom change was also clinically meaningful going from M = 14.2 (SD = 6.4) to 9.3 (SD = 8.04) on the PHQ-9. Both PTSD and depression change showed large effect sizes (Cohen’s D = 1.98 and 1.44, respectively). Participants were highly satisfied with the intervention, with a mean of over 28 out of 30 on The Client Satisfaction Questionnaire [34], our measure of treatment satisfaction. These preliminary findings suggested to us that further study of TrIGR using a rigorous randomized controlled trial design (stage II) was warranted.
First randomized controlled trial
We recently completed the first stage II, randomized controlled trial of TriGR [35•]. We randomized 144 Veterans who served in the conflicts in Iraq or Afghanistan and had guilt from a trauma that occurred on a deployment. Veterans were recruited from two sites, the San Diego and Providence VAs, and were randomized to receive either TrIGR or supportive care therapy [36]. In supportive care therapy, clients choose the topics that are discussed in therapy and therapists respond with positive regard and support, but do not offer skills or strategies [36]. Supportive care therapy is similar to Present Centered Therapy but without the active elements of problem solving. There is no homework in this therapy. It was selected as the control condition because it has all of the non-specific elements of good therapy without active intervention strategies. This kind of passive control is appropriate for stage II behavioral intervention studies [26]. Both therapies were delivered in six individual weekly sessions. Therapists delivered both treatments with careful fidelity monitoring for both therapies which included weekly supervision and having supervisors and fidelity raters listen to audio recordings of sessions.
Results using intent-to-treat analyses showed TriGR was more effective than supportive care therapy in reducing trauma-related guilt (treatment × time, −0.22; F (1, 455.2) = 18.49, p = .001; d = 0.92) and PTSD (treatment × time, −2.26; F (1, 468.3) = 6.76, p = .010; d = 0.81) and depression symptoms (treatment × time, −1.28; F (1, 454.6) = 7.51, p = .006; d = 0.43). Surprisingly, 50% of people in TrIGR lost their PTSD diagnosis between baseline and 6 months (compared to 14% in supportive care therapy; OR [95% CI] = 6.21 [2.23–17.29], p = .001), 67% showed clinically meaningful PTSD symptom reduction (compared to 40% in supportive care therapy; defined as a > 10 point improvement in CAPS-5 severity [37]; odds ratio [OR] [95% confidence interval {CI}] = 3.00 [1.32–6.84], p = .015), and 54% had clinically meaningful depression symptom reduction (compared to 27% in supportive care therapy; defined as >5 on the PHQ-9, [38]; OR [95% CI] = 3.05 [1.27–7.34], p = .023). These findings suggests that for those with PTSD and/or depression who have high trauma-related guilt, a treatment that is brief but targets the guilt can be effective in treating PTSD and depression symptoms.
We also measured general distress using the Brief Symptom Inventory-18 (BSI-18) [39] and quality of life using the World Health Organization Quality of Life measure [40]. We did not find differences between TrIGR and supportive care therapy. We speculated that the BSI-18, which has heavy emphasis on anxiety and somatization, may not capture the type of distress experienced by our high-guilt sample. Regarding quality of life, it was not clear if the treatments did not improve this outcome, or if this measure, which has not been validated with PTSD samples, did not capture change that may have occurred. We look forward to using more robust measures of quality of life in future studies to try to answer this question.
One surprising result was the high session attendance across both therapies (M = 5.3, SD = 1.6, in TrIGR and also 5.3, SD = 1.8, t (143) = 0.15, p = .88] in supportive care therapy, out of six sessions in both cases). Rates of treatment completion, a priori defined as attending four or more of six sessions, were also high and did not differ between treatment conditions [TrIGR n = 63; 85.1%; SCT n = 61; 85.9%), χ2 (1, N = 145) = 0.02, p = .90]. Such high attendance is unusual in any PTSD study but in particular in a sample of Iraq and Afghanistan veterans who have shown low attendance and high attrition across PTSD treatment trials [41, 42, 43]. We speculated that this may be because TrIGR is shorter than many PTSD treatments or that the focus on guilt felt more germane to the sample we recruited, and thus they continued to attend therapy.
COVID-19 pandemic study
We have a small stage II–III trial in progress to evaluate TrIGR for guilt from COVID-19 pandemic related events. The pandemic created ethically difficult scenarios for many people where they may have felt like they could not do enough or live up to their own standards [44•]. Examples include not being able to be with a loved who was very ill or dying, exposing someone to infection, or not being able to provide for family financially because of loss of a job or income. Our goal is to see if TrIGR may help reduce guilt from these kinds of ethically difficult, potentially morally injurious scenarios. We are in the process of randomizing 72 veterans who deployed in service of Iraq or Afghanistan who have guilt from an event that occurred during the pandemic or guilt that got worse due to the pandemic. The goal was to conduct this study quickly during the pandemic; thus, sample size was based on feasibility of recruitment in the study time frame. Participants are recruited to one of three sites — the Boston, Providence or San Diego VA, and randomized to TrIGR or supportive care therapy. This study is allowing us to stretch our understanding of the applicability of TrIGR in several important ways. This study is the first evaluation of TriGR to treat guilt from incidents that may be morally distressing and cause guilt but are do not necessarily meet Criterion A for PTSD. In our previous research, guilt had to stem from a trauma that would meet criterion A. Examples that would not meet criterion A are guilt over parenting or relationship behavior during the pandemic, or not being able to support one’s family because of loss of income. It is also our first evaluation of TriGR for non-warzone and non-military events. Also, in our previous studies the events that caused guilt generally occurred years before study entry, whereas in the pandemic study, events often occurred just months before participants entered the study. Thus, results of the trial will help inform if TrIGR can be efficacious to reduce guilt and related symptoms from recent morally distressing events and from non-military events.
Next steps in research
Our goal for the next steps of studying TrIGR is to understand how broadly applicable the treatment may be as the data we have so far are from a specific era of veterans with guilt from a specific type of trauma. This will move us further into stage III and IV research. Specifically, next steps are to evaluate TrIGR’s ability to reduce guilt and related symptoms from any type of trauma (e.g., car accidents, assaults) or morally challenging life events, to evaluate its efficacy with people who are not veterans and with veterans from any service era (thus far, our research has been with post-9/11 veterans). We also appreciate that there are several efficacious treatment options for moral injury and for PTSD and believe it is important to understand TrIGR’s effectiveness relative to these other treatments. This will allow clients to make informed decisions when presented with treatment options. Thus, another goal is to conduct studies comparing TrIGR to other effective treatments for moral injury and for common co-occurring problems such as PTSD.
We often get asked if there is the ideal time for someone to receive TrIGR relative to other treatments; that is, should it be a first line treatment, should it be offered after a diagnosis specific treatment when there is residual guilt, or should multiple treatments occur concurrently. It is likely that the answer to this question varies person to person based on clinical presentation and client preference, but we also see this as an empirical question that we would like to research in future studies.
Conclusions
TrIGR is a brief intervention focused on the guilt and shame components of moral injury and/or trauma. Evidence thus far suggests it is effective in reducing trauma-related guilt as well as symptoms of PTSD and depression. Future studies will assess its effectiveness with non-veterans, veterans of all eras of service, and with a broad range of traumas and stressors that violate deeply held moral beliefs and values.
Acknowledgements
Acknowledgements go to the dedicated team that has written and revised the TrIGR protocol over the years including Carolyn Allard, PhD; Kendall Browne, PhD; Christy Capone, PhD; Brittany Davis, PhD; and Moira Haller, PhD. I wish to thank Edward Kubany, PhD whose foundational work and mentorship made TrIGR possible. Thank you to our research team and the veterans who have participated in TriGR research.
Funding
The study received financial support from the Department of Defense Congressionally Directed Medical Research Program Grant # W81XWH-15-1-0330.
Declarations
Conflict of Interest
This work was supported by a grant from the Department of Defense Congressionally Directed Medical Research Program, Grant # W81XWH-15-1-0330. The author, Sonya Norman, earns royalties from Elsevier Press for a book titled “Trauma Informed Guilt Reduction Therapy: Treating Guilt and Shame Resulting from Trauma and Moral Injury.”
Footnotes
This article is part of the Topical Collection on Moral Injury.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 2.•.Griffin BJ, Purcell N, Burkman K, Litz BT, Bryan CJ, Schmitz M, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350–62. Excellent review of relationship between moral injury and mental health. [DOI] [PubMed]
- 3.Frankfurt S, Frazier P. A review of research on moral injury in combat veterans. Mil Psychol. 2016;28(5):318–30. doi: 10.1037/mil0000132. [DOI] [Google Scholar]
- 4.Kubany ES, Watson SB. Guilt: elaboration of a multidimensional model. Psychol Rec. 2003;53(1):51–90. [Google Scholar]
- 5.Tangney JP, Stuewig J, Mashek DJ. Moral emotions and moral behavior. Annu Rev Psychol. 2006;58(1):345–72. doi: 10.1146/annurev.psych.56.091103.070145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maguen S, Norman SB. Moral injury. PTSD Res Q [Internet]. 2022 [cited 2022 Mar 15];33(1). Available from: https://www.ptsd.va.gov/publications/rq_docs/V33N1.pdf
- 7.Miller MW, Wolf EJ, Kilpatrick DG, Resnick HS, Marx BP, Holowka DW, et al. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychol Trauma [Internet]. 2013 [cited 2020 May 12]; Available from: https://www.scienceopen.com/document?vid=8ead3b36-5fc9-4abb-a947-3c29978d8aa4
- 8.Browne KC, Trim RS, Myers US, Norman SB. Trauma-related guilt: conceptual development and relationship with posttraumatic stress and depressive symptoms. J Trauma Stress. 2015;28(2):134–41. doi: 10.1002/jts.21999. [DOI] [PubMed] [Google Scholar]
- 9.Norman SB, Wilkins KC, Myers US, Allard CB. Trauma informed guilt reduction therapy with combat veterans. Cogn Behav Pract. 21(1):78–88. [DOI] [PMC free article] [PubMed]
- 10.Crocker LD, Haller M, Norman SB, Angkaw AC. Shame versus trauma-related guilt as mediators of the relationship between PTSD symptoms and aggression among returning veterans. Psychol Trauma. 2016;8(4):520–7. doi: 10.1037/tra0000151. [DOI] [PubMed] [Google Scholar]
- 11.Norman SB, Haller M, Kim HM, Allard CB, Porter KE, Stein MB, et al. Trauma related guilt cognitions partially mediate the relationship between PTSD symptom severity and functioning among returning combat veterans. J Psychiatr Res. 2018;100:56–62. doi: 10.1016/j.jpsychires.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Bryan CJ, Morrow CE, Etienne N, Ray-Sannerud B. Guilt, shame, and suicidal ideation in a military outpatient clinical sample. Depress Anxiety. 2013;30(1):55–60. doi: 10.1002/da.22002. [DOI] [PubMed] [Google Scholar]
- 13.Marx BP, Foley KM, Feinstein BA, Wolf EJ, Kaloupek DG, Keane TM. Combat-related guilt mediates the relations between exposure to combat-related abusive violence and psychiatric diagnoses. Depress Anxiety. 2010;27(3):287–93. doi: 10.1002/da.20659. [DOI] [PubMed] [Google Scholar]
- 14.Larsen SE, Fleming CJE, Resick PA. Residual symptoms following empirically supported treatment for PTSD. Psychol Trauma. 2019;11(2):207–15. doi: 10.1037/tra0000384. [DOI] [PubMed] [Google Scholar]
- 15.Owens GP, Chard KM, Cox TA. The relationship between maladaptive cognitions, anger expression, and posttraumatic stress disorder among veterans in residential treatment. J Aggress Maltreat Trauma. 2008;17(4):439–52. doi: 10.1080/10926770802473908. [DOI] [Google Scholar]
- 16.Nash WP. Combat/operational stress adaptations and injuries. In: Combat stress injury: Theory, research, and management. New York, NY, US: Routledge/Taylor & Francis Group; 2007. p. 33–63. (Routledge psychosocial stress series).
- 17.Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behav Res Ther. 2004;42(3):277–92. doi: 10.1016/S0005-7967(03)00138-4. [DOI] [PubMed] [Google Scholar]
- 18.Øktedalen T, Hagtvet KA, Hoffart A, Langkaas TF, Smucker M. The Trauma related shame inventory: measuring trauma-related shame among patients with PTSD. J Psychopathol Behav Assess. 2014;36(4):600–15. doi: 10.1007/s10862-014-9422-5. [DOI] [Google Scholar]
- 19.Bannister JA, Colvonen PJ, Angkaw AC, Norman SB. Differential relationships of guilt and shame on posttraumatic stress disorder among veterans. Psycholog Trauma. 2019;11(1):35–42. doi: 10.1037/tra0000392. [DOI] [PubMed] [Google Scholar]
- 20.Norman S, Allard C, Browne K, Capone C, Davis B, Kubany E. Trauma informed guilt reduction therapy: treating guilt and shame resulting from trauma and moral injury. San Diego, CA, US: Elsevier Academic Press; 2019. xiii, 78 p. (Trauma informed guilt reduction therapy: treating guilt and shame resulting from trauma and moral injury).
- 21.Kubany ES, Abueg FR, Owens JA, Brennan JM, Kaplan AS, Watson SB. Initial examination of a multidimensional model of trauma-related guilt: applications to combat veterans and battered women. J Psychopathol Behav Assess. 1995;17(4):353–76. doi: 10.1007/BF02229056. [DOI] [Google Scholar]
- 22.Litz BT, Rusowicz-Orazem L, Doros G, Grunthal B, Gray M, Nash W, et al. Adaptive disclosure, a combat-specific PTSD treatment, versus cognitive-processing therapy, in deployed marines and sailors: a randomized controlled non-inferiority trial. Psychiatry Res. 2021;297:113761. doi: 10.1016/j.psychres.2021.113761. [DOI] [PubMed] [Google Scholar]
- 23.Maguen S, Burkman K, Madden E, Dinh J, Bosch J, Keyser J, et al. Impact of killing in war: a randomized, controlled pilot trial. J Clin Psychol. 2017;73(9):997–1012. doi: 10.1002/jclp.22471. [DOI] [PubMed] [Google Scholar]
- 24.Harris JI, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, et al. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. J Clin Psychol. 2011;67(4):425–38. doi: 10.1002/jclp.20777. [DOI] [PubMed] [Google Scholar]
- 25.Griffin BJ, Worthington EL, Jr, Lavelock CR, Greer CL, Lin Y, Davis DE, et al. Efficacy of a self-forgiveness workbook: a randomized controlled trial with interpersonal offenders. J Couns Psychol. 2015;62(2):124–36. doi: 10.1037/cou0000060. [DOI] [PubMed] [Google Scholar]
- 26.Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: unifying the discipline to improve the public health. Clin Psychol Sci. 2014;2(1):22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the trauma-related guilt inventory (TRGI) Psychol Assess. 1996;8(4):428–44. doi: 10.1037/1040-3590.8.4.428. [DOI] [Google Scholar]
- 28.Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol Assess. 2018;30(3):383–95. doi: 10.1037/pas0000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schnurr PP, Friedman MJ, Lavori PW, Hsieh FY. Design of Department of Veterans Affairs Cooperative Study no. 420: group treatment of posttraumatic stress disorder. Control Clin Trials. 2001;22(1):74–88. [DOI] [PubMed]
- 30.Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13(3):132–56. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 31.Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA. 2007;297(8):820–30. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer R. The PHQ-9: a new depression diagnostic and severity measure. psychiatric annals. 2002;32:509–21.
- 34.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 35.•.Norman SB, Capone C, Panza KE, Haller M, Davis BC, Schnurr PP, et al. A clinical trial comparing trauma-informed guilt reduction therapy (TrIGR), a brief intervention for trauma-related guilt, to supportive care therapy. Depress Anxiety (2022). https://onlinelibrary.wiley.com/doi/abs/10.1002/da.23244. First randomized controlled trial of TrIGR with 144 post-9/11 veterans. Findings show greater guilt, PTSD symptom, and depression symptom reduction in TrIGR than supportive care therapy. [DOI] [PubMed]
- 36.Walters EM, Jenkins MM, Nappi CM, Clark J, Lies J, Norman SB, et al. The impact of prolonged exposure on sleep and enhancing treatment outcomes with evidence-based sleep interventions: a pilot study. Psychol Trauma. 2020;12(2):175–85. doi: 10.1037/tra0000478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schnurr PP, Chard KM, Ruzek JI, Chow BK, Shih M-C, Resick PA, et al. Design of VA Cooperative Study #591: CERV-PTSD, comparative effectiveness research in veterans with PTSD. Contemp Clin Trials. 2015;41:75–84. doi: 10.1016/j.cct.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 38.McMillan D, Gilbody S, Richards D. Defining successful treatment outcome in depression using the PHQ-9: a comparison of methods. J Affect Disord. 2010;127(1–3):122–9. doi: 10.1016/j.jad.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 39.Derogatis L. Brief symptom inventory 18. MN: Pearson.; 2001.
- 40.Skevington SM, Lotfy M, O’Connell KA, WHOQOL Group. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13(2):299–310. [DOI] [PubMed]
- 41.Erbes CR, Curry KT, Leskela J. Treatment presentation and adherence of Iraq/Afghanistan era veterans in outpatient care for posttraumatic stress disorder. Psychol Serv. 2009;6(3):175–83. doi: 10.1037/a0016662. [DOI] [Google Scholar]
- 42.Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress. 2015;28(5):401–9. doi: 10.1002/jts.22038. [DOI] [PubMed] [Google Scholar]
- 43.Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, Teng EJ. Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. J Trauma Stress. 2014;27(3):265–73. [DOI] [PubMed]
- 44.•.Haller M, Norman SB, Davis BC, Capone C, Browne K, Allard CB. A model for treating COVID-19-related guilt, shame, and moral injury. Psychol Trauma. 2020. This article tackles why moral injury and guilt in particular may be common consequences of the pandemic and a model to use TrIGR to help resolve the resulting distress. [DOI] [PubMed]