Summary
Background
COVID-19 has had a profound impact on the health systems of the 11 countries of the WHO South East Asia Region. We conducted a systematic review of studies that used quantitative and comparative approaches to assess the impact of the pandemic on the service provision of four noncommunicable diseases (NCDs) (cancer, cardiovascular disease, chronic respiratory diseases, and diabetes) in the region.
Methods
A systematic search was conducted in PubMed, Embase, MedRxiv, and WHO COVID-19 databases in December 2021. The quality of studies was evaluated using the Joanna Briggs Institute Critical Appraisal Checklist and the ROBINS-I risk of bias tool. A narrative synthesis was conducted following the ‘synthesis without meta-analysis’ reporting guidelines.
Findings
Two review authors independently screened 5,397 records with 31 studies included, 26 which were cross-sectional studies. Most studies (n=24, 77%) were conducted in India and 19 (61%) were single-site studies. Compared to a pre-pandemic period, 10/17 cancer studies found a >40% reduction in outpatient services, 9/14 cardiovascular disease found a reduction of 30% or greater in inpatient admissions and 2 studies found diagnoses and interventions for respiratory diseases reduced up to 78.9% and 83.0%, respectively. No eligible studies on the impact of COVID-19 on diabetes services were found.
Interpretation
COVID-19 has substantially disrupted the provision of essential health services for NCDs in the WHO South East Asia Region, particularly cancer and cardiovascular disease. This is likely to have serious and potentially long-term downstream impacts on health and mortality of those living with or at risk of NCDs in the region.
Funding
This work was supported by the WHO Sri Lanka Country Office.
Keywords: COVID-19, Noncommunicable diseases, South East Asia, Health services
Research in context.
Evidence before this study
The COVID-19 pandemic has placed enormous strain on health systems in the South East Asia region (SEAR), with the WHO PULSE survey estimating that up to 60% of essential services have been at least partially disrupted. Disruptions in access to noncommunicable disease (NCD) services may lead to delayed diagnosis and advanced disease, potentially setting back hard-fought gains in NCD control across the region. However, no comprehensive analysis of quantitative evidence documenting the displacement of NCD services from the SEAR has been undertaken to date.
Added value of this study
This study represents the first systematic review and evidence synthesis of published evidence to estimate the quantitative impact of the COVID-19 pandemic on essential service provision for NCDs in the SEAR. We document that the pandemic substantially disrupted the provision of health services for NCDs, and in particular - cancer and cardiovascular disease, across multiple SEA countries. All aspects of NCD care, including screening, diagnosis, treatment, palliative care, and follow-up management were reduced during the pandemic. We did not identify any relevant studies in Bhutan, North Korea, Maldives, Myanmar, Thailand, or Timor-Leste, nor for services related to the diagnoses, treatment or management of diabetes.
Implications of all the available evidence
Our findings demonstrate that essential services for a range of NCDs were substantially disrupted by the COVID-19 pandemic across the SEAR. The downstream effects of these disruptions are potentially dire and could result in delayed diagnoses, faster disease progression, and ultimately – higher rates of mortality. Further research is required to understand the impact of subsequent waves of COVID-19 infection on NCD service provision, effective strategies to recover and protect disrupted services, and how countries across the SEAR can utilise this evidence towards informing policy for building more resilient health systems for future pandemic preparedness.
Alt-text: Unlabelled box
Introduction
The COVID-19 pandemic has placed enormous strain on health systems globally, and there is increasing evidence from numerous settings that it has impacted adversely on the provision of a wide range of essential health services.1 Management of the COVID-19 pandemic is particularly challenging for the 11 countries in the WHO South East Asia (SEA) Region, which has the lowest level of health spending of all WHO Regions at less than 5% on average.2, 3 The SEA Region is home to over a quarter of the world's population and comprises eleven countries: Bangladesh, Bhutan, Democratic People's Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand, and Timor-Leste. The pandemic toll in SEA Region has been severe – the region had experienced approximately one-fifth of global COVID-19 cases as of June 11, 2021.3
Besides its direct impact on health, COVID-19 has indirectly impacted health services due to lockdowns and other public health policies such as voluntary social distancing. In turn, these have led to decline in service utilization. The WHO PULSE survey on the continuity of essential health services during the COVID-19 pandemic has now published two rounds of information captured from 2020 and 2021.4,5 According to the WHO Pulse survey conducted in 2020, 77% of all countries have experienced health service disruptions to some extent 4. The services that were most frequently disrupted were routine immunization, noncommunicable disease (NCD) diagnosis and treatment, family planning and contraception, treatment for mental health disorders, antenatal care and cancer diagnosis and treatment. On average, close to 60% of essential services were at least partially disrupted in the SEA Region.4
Prior to the pandemic, all countries in the region had made improvement according to the WHO overall essential health service coverage index with the regional average increasing from 49% in 2010 to 63% in 2020.3 The largest progress was made in Indonesia, where the service coverage index increased by 18 percentage points.3 However, progress was largely uneven: the biggest gains were made in providing infectious diseases-related services, such as tuberculosis treatment and HIV antiretroviral therapy, while improvements related to noncommunicable diseases (NCDs) have been less rapid. In addition to being considered at higher risk for worse outcomes from COVID-19, people with NCDs may also experience disruptions or delays in access to health services due to mitigation measures such as national lockdowns.
NCDs account for an estimated 8.5 million deaths annually in the WHO SEA Region.6 In India for instance, NCDs present a substantial burden to the health system, and it is estimated that 35% of all outpatient visits to hospitals in 2004 were for NCDs, and 40% of hospitalizations.7 The continued increase in NCDs and chronic care conditions necessitates available, accessible, and affordable NCD health services yet the impact of the COVID-19 pandemic on service provision threatens to slow down progress and even reverse the gains in controlling NCDs.
We review the published quantitative evidence on the impact of COVID-19, compared to pre-pandemic data, on the provision of essential prevention, detection, treatment, and management services for NCDs across the SEA Region. We focus on four NCDs selected on the basis that they have the highest burden of disease in adults in the region, accounting for over 80% of all premature NCD deaths: cardiovascular diseases and stroke, cancers, chronic respiratory diseases, and diabetes.6 This review also characterizes the various policy responses implemented across the region and their impact on health service provision during the COVID-19 pandemic.
Methods
Approach and design of review
A systematic review was conducted to identify quantitative evidence regarding the provision of essential health service for NCD services in each of the 11 countries within the SEA Region. The review was reported according to PRISMA guidelines.
Search strategy
Between 1st and 15th of December 2021, we electronically searched the following databases: Ovid Medline, Embase and Global Health. The search included relevant medical subject heading terms, keywords, and word variant for NCDs, service disruption, COVID-19 and countries that belong to the SEA Region. The search was limited to English language sources published from 2020 to the time of the search. The complete search strategy is available in supplementary file 1. Additional nonstructured searches for grey literature were conducted in the WHO COVID-19 database and a pre-print database (e.g., https://www.medrxiv.org/).
Eligibility criteria
We limited eligibility to studies where one of the primary objectives was to determine the impact of the COVID-19 pandemic on the provision of health services for one or more of the NCD conditions of interest. Articles were included if the title and/or abstract indicated the report of results using quantitative and comparative approaches (i.e., 2020/21 estimates compared to 2019 and prior) that examine the impact of COVID-19 on the provision of any health service related to the prevention, diagnosis, treatment, or management for one of the four NCDs of interest in a SEA setting. Studies were excluded if they did not contain data from one of the listed countries, did not include a NCD of interest, were published outside the specified date range, contained only qualitative results, or did not include comparison groups.
Screening
Abstracts and potentially relevant full-texts were reviewed independently by two authors (TG and LD) with any conflicts resolved by consensus. Duplicates were removed from the initial search. Thereafter, full-texts of potentially relevant studies were reviewed to determine eligibility for inclusion. A full list of inclusion and exclusion criteria for the studies is provided in Table 1. All articles identified in the searches were imported into the Covidence systematic review software (version 2, Veritas Health Innovation, Melbourne, VIC, Australia), and title and abstract screening, full-text review, data extraction, and quality assessment were all performed in Covidence.
Table 1.
Review protocol inclusion and exclusion criteria.
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Date range | Published at any time in 2020 onwards | Published prior to 2020 |
| Population | Adult, adolescent, and child populations in the WHO SEA Region* | Countries outside of the WHO SEA Region |
| Study design | Comparative study designs that quantify the impact of the COVID-19 pandemic and associated public health response measures on health service provision | Qualitative studies, non-longitudinal studies, studies without comparison groups, commentaries, opinions, letters and clinical guidelines data |
| Conditions of interest | All types of cancers, cardiovascular diseases and stroke, chronic respiratory diseases, chronic kidney disease and diabetes | Infectious diseases, acute infections or episodes, other conditions not otherwise classified as non-communicable diseases |
| Other | Published in English language | Published in language other than English |
Bangladesh, Bhutan, Democratic People's Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste.
Quality Appraisal
The methodological quality of the included studies was evaluated using validated tools for each study design. For cross-sectional before-after studies we used the six-item Joanna Briggs Institute (JBI) Critical Appraisal Checklist for analytical cross-sectional studies. The JBI is an international, membership-based research and development organization within the Faculty of Health Sciences at the University of Adelaide. The instrument was developed by the JBI before being reviewed by an international methodological group. For cohort or case control studies we used the ROBINS-I [9] risk of bias tool, as recommended by the Cochrane Collaboration to assess non-randomized studies of interventions. Quality appraisal was undertaken by a single reviewer (TG) and any points of uncertainty were addressed through discussion and consensus with a second reviewer (LD).
Data extraction and analysis
Data were extracted in Covidence by two reviewers (TG, LD) using a standard template that was modified to include key parameters of interest. The following data were extracted: country; condition of interest; service of interest; study design; sampling period; % change in service delivery metrics from pre-COVID to peri-COVID. Essential health services were divided into the following categories of interest, in line with patient pathways of care: outpatient services (e.g., presentation rates), inpatient services (e.g., admission rates), diagnosis and case finding, pharmacological services, condition management and follow-up services. The following COVID-19 related information was also extracted from papers where possible: whether data collection coincided with a ‘peak’ of infection and/or lockdown; whether any service protection/mitigation measures were in place during the period of data collection; the reported efficacy of the mitigation measures; and reported consequences of forgone or displaced health services as a consequence of COVID-19.
Evidence synthesis
Given the heterogeneity in setting, population, condition, and service area, a meta-analysis was not undertaken. A narrative synthesis was conducted following the ‘synthesis without meta-analysis (SWIM)’ in systematic review reporting guidelines to explore, describe, and interpret key findings related to the impact of COVID-19 on the provision of essential health services for NCDs during 2020 and 2021 in the SEA Region.
Role of the funding source
This study was funded by the World Health Organisation Sri Lanka (WHO-SL) Country Office. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The WHO-SL office and the WHO South East Asia Regional Office (WHO-SEARO) have reviewed and approved this manuscript for publication.
TG is supported by a university post graduate award from the University of New South Wales. VDRV receives a salary from the World Health Organisation South East Asia Regional Office. DP and SJ are both supported by individual investigator grants from the Australian National Health and Medical Research Council.
Ethical approval
Ethical approval was not required for this review as all information collected was available in the public domain.
Results
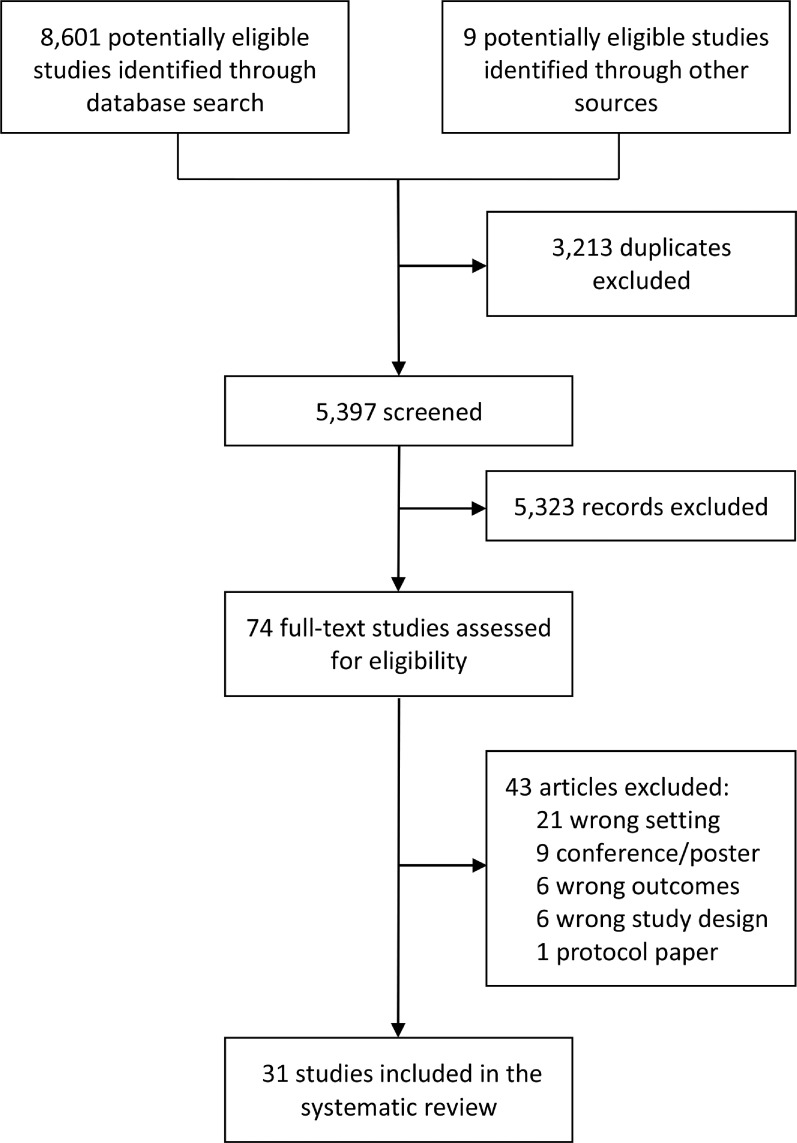
An initial 8,601 papers were identified through a database search and 9 through the grey literature. 5,397 records remained after duplicates were removed. 74 were relevant for full-text review and 31 met the inclusion criteria for systematic review (Figure 1).8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Forty-three studies were excluded. Primary reasons for exclusion included the study setting outside SEA (n=21), conference abstract or poster presentation (n=9) inappropriate study design (i.e., not comparative; n=6) and reporting on outcomes outside of the scope of this review (n=6).
Figure 1.
PRISMA diagram. Abbreviations: PRISMA, preferred reporting items for systematic reviews and meta-analyses.
Table 2 shows the characteristics of the 31 included studies. Five countries in the region were represented: India (24 studies; 77.4%), Bangladesh (2), Sri Lanka (2), Indonesia (1) and Nepal (1). There were no relevant papers identified for Bhutan, North Korea, Maldives, Myanmar, Thailand, or Timor-Leste.
Table 2.
Studies included in the systematic review.
| Author, Year | Country | Study design | Setting | Disease area | Sample size | Control period | Pandemic period |
|---|---|---|---|---|---|---|---|
| Akhtar 2020 | India | Cross sectional analysis | Single-site | Cancer | NR | Apr to Sept 2019 | Apr to Sept 2020 |
| Basu 2021 | Bangladesh | Cross sectional analysis | National | Cancer | 1,070,713 | Jan to Dec 2018, 2019 | Jan to Dec 2020 |
| Cherian 2020 | India | Cross sectional analysis | 6 radiology centres | Cardiovascular disease | NR | Apr 1 to June 30, 2019 | Apr 1 to June 30, 2020 |
| Choubey 2021 | India | Cross sectional analysis | 24 paediatric cardiac centres | Cardiovascular disease | NR | Apr 1 to Aug 31, 2019 | Apr 1 to Aug 31, 2020 |
| Choudhary 2020 | India | Cross sectional analysis | 4 hospitals | Cardiovascular disease | 2,607 | Jan 25 to Feb 24, 2020 | Feb 25 to Mar 24, 2020 |
| Choudhary 2021 | India | Cross sectional analysis | 2 hospitals | Cardiovascular disease | 1,023 | Dec 5, 2019 to Mar 24, 2020 | Mar 25 to July 14, 2020 |
| Das 2021 | India | Cross sectional analysis | Single-site | Cancer | 281 | Apr 1 to June 30, 2019 | Apr 1 to June 30, 2020 |
| Deshmukh 2021 | India | Cross sectional analysis | Single-site | Cancer | NR | Mar 22 to May 31, 2019 | Mar 22 to May 31, 2020 |
| Dewi 2021 | Indonesia | Cross sectional analysis | Single-site | Cancer | 5,412 | Oct 2019 to Feb 2020 | Mar to July 2020 |
| Dharma 2021 | Indonesia | Cross sectional analysis | Single-site | Cardiovascular disease | 324 | Mar 1 to May 31, 2019 | March 1 to May 31, 2020 |
| Hasan 2021 | Bangladesh | Cross sectional analysis | Single-site | Cardiovascular disease | 1,394 | Jan 1 to Mar 25, 2020 | Mar 25 to June 25, 2020 |
| Hewamana 2021 | Sri Lanka | Cross sectional analysis | Single-site | Cancer | 1,633 | Apr 1 to Dec 31, 2019 | Apr 1 to Dec 31, 2020 |
| Jayagopal 2021 | India | Cross sectional analysis | 7 hospitals | Cardiovascular disease | 1,582 | Mar 25 to July 25, 2019 | Mar 25 to July 25, 2020 |
| Kawthalkar 2021 | India | Cross sectional analysis | Single-site | Cancer; Cardiovascular disease; Respiratory | NR | Feb 22 –Mar 24, 2020 | Mar 25 to June 25, 2020 |
| Kumanan 2020 | Sri Lanka | Cross sectional analysis | 3 hospitals | Cancer; Cardiovascular disease | NR | Mar to Apr 2019 | Mar to Apr 2020 |
| Kute 2021 | India | Prospective observational study | Single-site | Nephrology | NR | 2019 | 2020 |
| Mallick 2021 | India | Cross sectional analysis | Single-site | Cancer | 10,381 | Jan 1 to Mar 23, 2019 | Mar 23 to May 16, 2020 |
| Pareek 2021 | India | Cross sectional analysis | Single-site | Cancer | 5,258 | Jan 1 to May 31 2019 | Jan 1 to May 31 2020 |
| Prajapati 2021 | India | Cross sectional analysis | Single-site | Cancer | 304 | Mar 16 to June 30, 2019 | Mar 16 to June 30, 2020 |
| Ramakrishnan 2021 | India | Cross sectional analysis | Single-site | Cancer | NR | Apr 1 to Sept 30, 2019 | Apr 1 to Sept 30, 2020 |
| Ranganathan 2021 | India | Ambidirectional cohort study | 41 cancer centres | Cancer | NR | Mar 1 to May 31, 2019 | Mar 1 to May 31, 2020 |
| Rangashamaiah 2021 | India | Cross sectional analysis | Single-site | Cardiovascular disease | NR | Feb 11 to Mar 24, 2020 | Mar 25 to May 7, 2020 |
| Reddy 2021 | India | Retrospective matched cohort study | Regional | Cardiovascular disease | NR | July to Sept 2019 | Jan to June 2020 |
| Riju 2021 | India | Cross sectional analysis | Single-site | Cancer | NR | Apr 2019 to Mar 2020 | Apr to June 2020 |
| Sapkota 2021 | Nepal | Prospective descriptive study | Single-site | Cancer | 50 | NR | 1 Mar to 1 Aug 2020 |
| Senthilkumaran 2020 | India | Cross sectional analysis | 12 hospitals | Cardiovascular disease | 20,878 | Feb 2020, Apr 2019 | Apr 2020 |
| Sharma 2021 | India | Prospective mixed-quantitative methods study | 30 cancer centres | Cancer | 1,146 | Jan 1 to Mar 23, 2020 | Mar 24 to May 31, 2020 |
| Subbiah 2020 | India | Cross sectional analysis | Single-site | Cancer | 10,996 | Oct 2019 to Feb 2020 | Mar to July 2020 |
| Tyagi 2021 | India | Cross sectional analysis | Single-site | Respiratory | 203 | Jan 2020 | Mar 24 to Jul 23, 2020 |
| Yalamanchi 2020 | India | Cross sectional analysis | Single-site | Cardiovascular disease | 845 | Mar 22 to Aug 1, 2018, 2019 | Mar 22 to Aug 1, 2020 |
| Zachariah 2021 | India | Emulated natural interrupted time series | 187 hospitals | Cardiovascular disease | 41,832 | Mar 15 to June 15, 2019 | Mar 15 to June 15, 2020 |
NR=not reported.
Fifteen studies (48.4%) reported on disruptions to cancer related health services9,14,16,18,23,25, 26, 27, 28, 29,32,34, 12 (38.7%) on cardiovascular diseases10, 11, 12, 13,17,19,24,30,31,36, 37, 38, one (3.2%) on respiratory services35 and diabetes services.22 Additionally, one study reported on disruptions to both cancer and cardiovascular services21 and one on disruptions to diagnostic procedures for cancer, cardiovascular and respiratory diseases.20 There was one report using a national registry, 11 multi-site studies and the remaining 19 were single-site studies.
Nearly all studies were cross-sectional in nature (n=30), though different study design labels were applied including ‘ambi-directional’ cohort study,29 prospective mixed-quantitative methods study33 and emulated natural interrupted time series.37 One study was a retrospective matched cohort study where clusters of geographic districts were exposed to a different form of follow-up provision.31 Eighteen studies compared a period of time during the COVID-19 pandemic, often during lockdown, with the corresponding period in the prior year (i.e., 2019) while nine studies obtained a comparison group from a period immediately preceding the pandemic or lockdown. Sample sizes varied from 50 to 41,832 (Table 2).
Among analytical cross-sectional studies, 21 were considered moderate quality 8, 9, 10, 11, 12, 13, 14,17, 18, 19, 20,23,25,27, 28, 29,32,33,36, 37, 38 and 9 low quality.15,16,21,22,24,26,30,34,35 The majority of studies outlined clear time periods for comparison, the study setting, outcomes for measurement and their data source. Comparatively, sample size was not reported in 12 studies, and studies commonly did not explain their statistical analysis methods nor provide confidence intervals. Only one study – the retrospective matched cohort study – controlled for confounding and was found to have a moderate risk of bias.31 None of the included studies were scored a high methodological quality. Results of the quality assessment are contained in supplementary file 2.
Impact of COVID-19 on patient pathways for cancer care
Of the 17 studies that assessed disruptions to cancer related health services, 13 were conducted in India (Table 3). The majority (n=11) assessed services provision in tertiary oncology departments (for all types of cancer) while others focused specifically on cervical (n=1), paediatric (n=1), oral (n=1), blood (n=1), gastrointestinal (n=1) and head and neck (n=1) cancers.
Table 3.
Change in cancer service provision by study and patient pathway.
| Author, Year | Country | Service of interest | Control period | Pandemic period | Percentage change (95% CI)⁎⁎ |
|---|---|---|---|---|---|
| Akhtar 2020 | India | Outpatient visits | 20,822 | 7,973 | -62 |
| Inpatient admissions | 2,840 | 1,184 | -58 | ||
| Surgical treatment provisions | 598 | 410 | -31 | ||
| Pharmacological treatment | 4,896 | 2,150 | -56 | ||
| Basu 2020 | Bangladesh | Diagnostic services | 2018: 379,006 2019: 391,531 |
336,407 | 2018: -11.2 2019: -14.1 |
| Das 2021 | India | Surgical treatment provisions | 209 | 72 | -66 (p<0.05) |
| Deshmukh 2021 | India | Surgical treatment provisions | 929 | 28 | -97 |
| Pharmacological treatment | 8,392 | 525 | -94 | ||
| Dewi 2021 | Indonesia | Outpatient visits | 5,399 | 1,927 | -35 |
| Hewamana 2021 | Sri Lanka | Outpatient visits | 1,059 | 977 | -8 (6.2%, 9.5%) |
| Inpatient admissions | 574 | 422 | -26 (22.9%, 30.3%) | ||
| Kawthalkar 2021 | India | Diagnostic services | 62 | 17 | -72.6 |
| Kumanan 2020 | Sri Lanka | Pharmacological treatment | 342 | 274 | -20 |
| Mallick 2021 | India | Outpatient visits | 5,291 | 5,090 | -58 |
| Pareek 2021 | India | Outpatient visits | 4,363 | 895 | -80 |
| Pharmacological treatment | 3,051 | 308 | -90 | ||
| Prajapati 2021 | India | Outpatient visits | 235 | 69 | -70 |
| Surgical treatment provisions | 132 | 66 | -50 | ||
| Ramakrishnan 2021 | India | Inpatient admissions | 796 | 681 | -14.4 |
| Surgical treatment provisions | 1,871 | 1,427 | -23.7 | ||
| Ranganathan 2021* | India | Outpatient visits | 634,745 | 340,984 | -46 |
| Inpatient admissions | 88,801 | 56,885 | -36 | ||
| Diagnostic services | 398,373 | 246,616 | -38 | ||
| Surgical treatment provisions | 17,120 | 8,677 | -49 | ||
| Pharmacological treatment | 173,634 | 109,107 | -37.5 | ||
| Riju 2021 | India | Outpatient visits | 5,904 | 549 | -63 |
| Inpatient admissions | 288 | 35 | -51.4 | ||
| Surgical treatment provisions | 192 | 26 | -86 | ||
| Sapkota 2021 | Nepal | Outpatient visits | NR | NR | -80 |
| Inpatient admissions | 796 | 681 | -50 | ||
| Sharma 2021 | India | Outpatient visits | 797 | 349 | -56.3 |
| Subbiah 2020 | India | Outpatient visits | 4,096 | 2,602 | -63.5 |
| Inpatient admissions | 749 | 462 | -61.6 | ||
| Surgical treatment provisions | 1,972 | 1,115 | -60 |
NR=not reported.
Study presents a range of service utilisation and disruption measures;
Where available, p-values and confidence intervals reported.
Studies commonly reported on multiple services of interest. Eleven reported on outpatient services, of which 10 found a >40% reduction in service delivery post the onset of COVID-19 as compared to a pre-pandemic period (range 8 to 80%). Seven studies reported on inpatient admissions finding reductions ranging from 14.4 to 61.6%. To some extent, the magnitude of service reduction reported, depended on the timeline of the study. Studies that only analysed service provision during a lockdown period were likely to report higher reductions than those that covered the whole of 2020. For instance, in Bangladesh the national cervical cancer screening program dropped 94.9% in the first month of the lockdown yet only 14.1% across the whole year.9
Of these 17 studies, only two reported on the impact of mitigation measures to maintain service provision during the pandemic.18,23 In the absence of any national guidelines in India, Mallick and colleagues prioritised radiotherapy treatment for oncology patients, continued services for patients already undergoing treatment and deferred new starts for adjuvant therapy.23 Additionally, a staff rotation policy was implemented to ensure that human resources could be redeployed to prevent delays and deliver full services for those with the highest priority. Although outpatient consultations dropped by 58% during lockdown, more than 90% of high-priority cancer treatments (specifically radiotherapy and chemotherapy) were implemented as planned.
Similarly, Hewamana documented mitigation strategies used in a tertiary blood cancer centre in Sri Lanka.18 These included triaging patients via telephone prior to attendance, monitoring patients following discharge via telephone to reduce attendance, and providing prophylaxis and oral antibacterial medications to minimize presentations. Compared to same period in 2019, the number of outpatient services reduced by 8% (p=0.002, 95% CI: 6.2 to 9.5%) during the pandemic period, while inpatient admissions decreased by 26% (p=0.002, 95% CI: 22.9 to 30.3%).
Impact of COVID-19 on patient pathways for cardiovascular diseases
Fourteen studies assessed the impact of the pandemic on cardiovascular related services – 11 were conducted in India, and one each in Bangladesh, Indonesia, and Sri Lanka (Table 4). Most studies (n=10) reported on disruption to inpatient admissions, of which five found a reduction of 50% or greater (range: 13 to 81%). Four studies reported on disruption to the number of surgeries conducted (range: 10.4 to 73%), four studies on diagnostic procedures (range: 48 to 73.4%) and one on outpatient services (74.4%).
Table 4.
Change in cardiovascular disease service provision by study and patient pathway.
| Author, Year | Country | Service of interest | Control period | Pandemic period | Percentage change (95% CI)⁎⁎ |
|---|---|---|---|---|---|
| Cherian 2020 | India | Diagnostic services | 186 | 76 | -59 |
| Surgical treatment provisions | 874 | 273 | -55 (p <0.001) | ||
| Choubey 2021 | India | Outpatient visits | 54,213 | 13,878 | -74.4 (p <0.001) |
| Inpatient admissions | 5,766 | 1,910 | -66.8 (p <0.001) | ||
| Diagnostic services | 3,454 | 887 | -74.3 (p <0.001) | ||
| Surgical treatment provisions | 4,586 | 1,238 | -73 (p <0.001) | ||
| Choudhary 2020* | India | Inpatient admissions | 1,488 | pre-lockdown: 830 lockdown: 289 |
pre-lockdown: -45 lockdown: -81 |
| Choudhary 2021 | India | Inpatient admissions | 241 | 782 | -69 |
| Dharma 2021 | Indonesia | Inpatient admissions | 208 | 116 | -64 |
| Hasan 2021 | Bangladesh | Inpatient admissions | 907 | 487 | -46.3 |
| Jayagopal 2021 | India | Inpatient admissions | 1,056 | 526 | -50 |
| Kawthalkar 2021* | India | Diagnostic services | 73 | 48 | -34.3 |
| Kumanan 2020 | Sri Lanka | Inpatient admissions | 54.5 | 47.5 | -13 |
| Diagnostic services | 221 | 124.5 | -44 | ||
| Rangashamaiah 2021 | India | Inpatient admissions | NR | NR | -31.0 |
| Reddy 2021 | India | Follow-up service provision | Intervention: 86% Control: 74% |
Intervention: 78% Control: 36% |
Intervention: -5 Control: -51 |
| Senthilkumaran 2020* | India | Surgical treatment provisions | Feb 2020: 4,068 Apr 2019: 4,674 |
3,341 | Feb 2020: -17.9 Apr 2019: -28.5 |
| Yalamanchi 2020* | India | Inpatient admissions | 2018: 307 2019: 322 |
216 | 2018: -30 2019: -33 |
| Zachariah 2021 | India | Inpatient admissions | 25,418 | 16,414 | -35.4 |
| Surgical treatment provisions | 8,855 | 14,738 | -4 | ||
| Diagnostic services | 21,176 | 11,973 | -10.4 |
NR=not reported.
Study presents a range of service utilisation and disruption measures.
Where available, p-values and confidence intervals reported.
Nine studies reported gender disaggregated data, four of which reported large discrepancies in access by gender. Two multi-site studies in India found a reduction in the proportion of women accessing cardiovascular care during the COVID-19 pandemic. Among four hospitals during lockdown the proportion of women accessing cardiovascular services reduced from 28.1 to 11%;12 and among two hospitals patients admitted with acute heart failure during the lockdown were more commonly male (82.6 vs 71.6%; p value <0.02);13 Two other studies reported low levels of females patients before and during the pandemic. A cross-sectional analysis of 187 Indian hospitals reported that across 2019 and 2020 only 21.6% (9,018/41,832) of hospitalised patients with acute myocardial infarction were female;37 similarly, of 324 patients undergoing primary angioplasty in a tertiary care hospital in Jakarta, Indonesia, approximately 90% were male.38
Only one study examined the impact of the pandemic on the availability of condition management and follow-up services. Reddy et al (2021) examined whether the decentralization of hypertension follow-up services improved continuity of care for hypertensive patients and helped to mitigate disruption during the pandemic.31 In the decentralised group, registered hypertensive patients received free medication and care from an auxiliary nurse midwife at subcentres, the most peripheral component of the primary healthcare system. In the control group, registered hypertensive patients were required to travel to the primary health centre to receive free medication and care from a nurse. During the pandemic, follow-up services under the decentralized model of care reduced by 5% compared to 51% under the centralised model.31
Impact of COVID-19 on patient pathways for other NCD services
Only one study, conducted in India, examined the impact of the pandemic on access to nephrology services, specifically in terms of outpatients, inpatient admissions, and kidney transplant services (Table 5). Kute et al found reported that these measures reduced by 20%, 31% and 56%, respectively, during 2020.22 Regarding respiratory services, Tyagi and colleagues reported that, in India, the number of interventional pulmonology procedures reduced by 83% from March 24 to July 23, 2020, compared with January 2020.35
Table 5.
Change in other service provision by study and patient pathway.
| Author, Year | Country | Condition of interest | Service of interest | Control period | Pandemic period | Percentage change |
|---|---|---|---|---|---|---|
| Kawthalkar 2021 | India | Respiratory | Diagnostic services | 118 | 25 | -78.9 |
| Kute 2021 | India | Nephrology | Outpatient visits | 132,181 | 109,572 | -20 |
| Inpatient admissions | 7,471 | 5,157 | -31 | |||
| Surgical treatment provisions | 412 | 183 | -56 | |||
| Pharmacological treatment | 56,699 | 56,312 | -1 | |||
| Tyagi 2021 | India | Respiratory | Surgical treatment provisions | 174 | 29 | -83 |
Discussion
This review finds that the provision of NCD services in the SEA Region was substantially affected by the COVID-19 pandemic. The provision of cancer services was consistently reported to be 50% less when compared to the pre-pandemic period including disruptions to all aspects of care, such as outpatient services, inpatient admissions, surgical procedures, and pharmacological treatments. The provision of services for cardiovascular disease was similarly impacted, with 7 out of 14 studies reporting >50% reductions in service provision. Evidence of the pandemic's impact on nephrology and respiratory services was limited yet the available information reports service reductions ranging from 20% to 83%.
Whilst some level of health service disruption is an expected impact of the COVID-19 pandemic, our findings document a magnitude of disruption potentially greater than previously postulated. A recent systematic review of disruptions in cancer care, which included studies mostly (84%) from high income countries, found reductions in hospitalization rates of up to 30% compared to the pre-pandemic period.39 Our findings also highlight a potentially higher level of service disruption than that reported in large scale surveys, such as the WHO PULSE survey.4,5,40 For example, the first PULSE survey (2020) reported that much of the disruption to NCD services was incurred in prevention activities with reductions in inpatient services observed to be ‘generally less affected’, however we identified data from multiple studies in this review that highlighted substantial reduction in the use of inpatient services, as well as NCD-related surgical services.
One of the difficulties in interpreting these findings is in disentangling the effect of such disruption from supply-side and demand-side factors, the latter related to lockdowns, social distancing regulations, financial burden, and fear of infection within patient populations. Based largely on data from multiple studies in India, reductions in service provision appeared greatest when national lockdowns were first announced, which coincided with stricter restrictions, but with less COVID‑19 cases.10, 11, 12, 13,19,29,37 However, by the time India's first national lockdown ended in June 2020, case numbers were rapidly increasing. As a result, anticipated rebounds in patient load were limited due to continuing travel restrictions and fear of infection.10 For instance, Jayagopal et al (2021) reported a surge in patient admissions following the end of India's national lockdown in June 2020, yet this was followed by another drop in late June as the number of COVID-19 cases rapidly increased.19
It is worth noting that service utilisation by gender was rarely reported by studies. Three studies from India found reductions in access to cardiovascular services among females, contrasted with the increase in service utilisation amongst males.12,13,37 This aligns with evidence of gender discrimination in healthcare access in the country.41,42 Decision makers need to ensure that disparities in access to care, particularly by gender, are not exacerbated by the pandemic and further research is needed to track how access to services may have been affected across sub-populations such as rural, the poor and displaced populations.
To our knowledge, this is the first systematic review to comprehensively assess the evidence base for service disruption due to COVID-19 across the SEA Region. The study design is advantageous in that it focuses on quantitative estimates of service disruption rather than commentary and qualitative assessment. As such, this review provides a much needed means of validating the enormous amount of commentary that has surrounded this topic and in informing policy responses. The systematic search also incorporates a review of the grey literature, which is important given the rapidly changing epidemiology and policy environment and the potentially slow process of academic peer review. Lastly, this review was commissioned by WHO SEARO and was conducted with a rapid turnaround time with the aim of providing real time evidence to not only support the WHO and country response to the pandemic, but also provide clear and timely guidance on research priorities.
A primary limitation of this review is the relatively limited published literature, and the retrospective design of the identified included studies, many of which were single-site studies. The nature of the pandemic and the associated extreme burden on the clinical workforce has undoubtedly had a detrimental impact on the ability and motivation of clinical academic staff to take time out of their challenging schedules to identify, analyse, write-up and publish any findings in relation to service delivery disruptions, necessarily limiting the published literature on this topic. Second, the small number of studies conducted outside of India, and the dearth of relevant studies in Bhutan, North Korea, Maldives, Myanmar, Thailand, or Timor-Leste, means that the generalisability of our conclusions to the SEA Region is extremely limited. This review searched studies published in English language only, which is a potentially important limiting factor in our ability to identify and assess all possible relevant literature across the region.
Furthermore, by adopting a regional perspective, our ability to analyse the contextual dynamics of the pandemic as it evolved in each country was limited. This is especially relevant in relation to country-specific health system configuration, quality, accessibility, and resilience, and to local policies and baseline characteristics of the provision of essential health services for the prevention, detection, treatment, and ongoing management of NCDs. We were also unable to make a comprehensive assessment of the impact of any local service protection or pandemic mitigation measures put into place over the course of the time period of interest. Only two studies provided a detailed account of mitigation measures and their subsequent impact on service disruption.18,23 This finding is not unique and reinforces the need for greater research to monitor the impact of mitigation strategies to reduce the impact of COVID-19 on health services.43
This review raises a number of important insights in relation to the need for more robust, representative, and timely research into the impact of COVID-19 on essential health services for NCDs across the South East Asia Region. Analysis of evidence from those numerous SEA countries absent from this review is an essential first step to recognising which services may have been most disrupted by the pandemic, and in which countries. Our findings further highlight an imbalance in research in relation to specific NCDs. This should also be rectified by comprehensive research into the impact of COVID-19 on essential services for high-burden conditions such as respiratory diseases and chronic kidney diseases, for which few studies were identified. Quantitative estimates of service disruption should be supplemented with a focus on gender and equity issues as well as local qualitative studies to understand the true nature of any service disruptions, reasons for these, and identify promising opportunities for service recovery and strengthening. As the evidence base grows, reviews such as this study should be updated to incorporate new evidence and offer a ‘living’ resource to inform future pandemic preparedness policy. Finally, as this review only found studies reporting on the first wave of COVID-19 in 2020, research analysing the impact of later ‘waves’ of COVID-19 infection would provide valuable information about the impact of subsequent waves and strains of COVID-19 on SEA populations and whether services were able to recover, and to what extent, between and post major waves of infection.
In summary, the COVID-19 pandemic has significantly disrupted the provision of essential health services for noncommunicable diseases in the South East Asia Region. This systematic review found substantial evidence of disruptions to services for cancer and cardiovascular disease, primarily in India but also including Indonesia and Sri Lanka. A small number of studies suggest ophthalmology services in India were similarly affected. Mitigation measures in response to the pandemic, such as national lockdowns and movement restrictions, were primarily responsible for reductions in service access. These reductions will likely result in delayed diagnosis, and suboptimal treatment for at least a proportion of patients and downstream effects will likely include more advanced disease.
Contributors
Conceptualisation: SJ, LD, VDRV, DP, TG; Data collection: TG, LD; Data analysis and interpretation: TG, LD, SJ; Drafting the article: TG, LD, SJ; Critical revision of the article: DP, VDRV.
Declaration of interests
This work was supported by the WHO Sri Lanka Country office. TG is supported by a university post graduate award from the University of New South Wales. VDRV receives a salary from the World Health Organisation South East Asia Regional Office. DP and SJ are both supported by individual investigator grants from the Australian National Health and Medical Research Council.
Data sharing statement
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lansea.2022.04.006.
Appendix. Supplementary materials
References
- 1.Lal A, Lim C, Almeida G, Fitzgerald J. Minimizing COVID-19 disruption: ensuring the supply of essential health products for health emergencies and routine health services. Lancet Regional Health - Americas. 2021 doi: 10.1016/j.lana.2021.100129. 2021/12/06/100129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. Global spending on health: weathering the storm. [Google Scholar]
- 3.World Health Organization . 2021. Crisis or opportunity? Health financing in times of uncertainty: Country profiles from the SEA Region. [Google Scholar]
- 4.World Health Organization . 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic.https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 Interim report. [Google Scholar]
- 5.World Health Organization . 2021. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic.https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 Interim report. [Google Scholar]
- 6.World Health Organization . 2020. Second South-East Asia Regional Forum to accelerate NCD prevention and control in the context of SDGs. New Delhi, India, 30 October –1 November 2019. [Google Scholar]
- 7.Liu C, Tang S. 2021. Integrated care for chronic diseases in Asia Pacific countries.https://apo.who.int/publications/i/item/integrated-care-for-chronic-diseases-in-asia-pacific-countries [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akhtar N, Rajan S, Chakrabarti D, et al. Continuing cancer surgery through the first six months of the COVID-19 pandemic at an academic university hospital in India: A lower-middle-income country experience. J Surg Oncol. 2021;123(5):1177–1187. doi: 10.1002/jso.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu P, Lucas E, Zhang L, Muwonge R, Murillo R, Nessa A. Leveraging vertical COVID-19 investments to improve monitoring of cancer screening programme - a case study from Bangladesh. Prev Med. 2021;151 doi: 10.1016/j.ypmed.2021.106624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherian M, Mehta P, Barath S, et al. Impact of COVID-19 pandemic on interventional radiology practice—a multicenter observational study. J Clin Intervent Radiol ISVIR. 2020;4(03):167–174. doi: 10.1055/s-0040-1718790. [DOI] [Google Scholar]
- 11.Choubey M, Ramakrishnan S, Sachdeva S, et al. Impact of COVID-19 pandemic on pediatric cardiac services in India. Ann Pediatr Cardiol. 2021;14(3):260–268. doi: 10.4103/apc.apc_133_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choudhary R, Gautam D, Mathur R, Choudhary D. Management of cardiovascular emergencies during the COVID-19 pandemic. Emerg Med J. 2020;37(12):778–780. doi: 10.1136/emermed-2020-210231. [DOI] [PubMed] [Google Scholar]
- 13.Choudhary R, Mathur R, Sharma JB, Sanghvi S, Deora S, Kaushik A. Impact of Covid-19 outbreak on clinical presentation of patients admitted for acute heart failure in India. Am J Emerg Med. 2020;39:162–163. doi: 10.1016/j.ajem.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Das G, Khanna S, Purkayastha J, et al. Impact of COVID-19 pandemic on a tertiary care center's surgical volume and outcomes: a single institutional study from Northeast India. Indian J Surg Oncol. 2021:1–5. doi: 10.1007/s13193-021-01410-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deshmukh S, Naik S, Zade B, et al. Impact of the pandemic on cancer care: Lessons learnt from a rural cancer center in the first 3 months. J Surg Oncol. 2020;122(5):831–838. doi: 10.1002/jso.26144. [DOI] [PubMed] [Google Scholar]
- 16.Dewi YA, Permana AD, Oktrivianto DA. The impact of covid-19 pandemic to head and neck cancer care in hasan sadikin hospital Bandung, Indonesia. Int J Pharmacy Pharmaceut Sci. 2021:63–66. doi: 10.22159/ijpps.2021v13i7.41264. [DOI] [Google Scholar]
- 17.Hasan A, Das SC, Islam MS, et al. Impact of COVID-19 on hospital admission of acute stroke patients in Bangladesh. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0240385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hewamana S, Skandarajah T, Jayasinghe C, et al. Blood cancer care in a resource limited setting during the Covid-19 outbreak; a single center experience from Sri Lanka. PLoS One. 2021;16(9) doi: 10.1371/journal.pone.0256941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jayagopal PB, Abdullakutty J, Sridhar L, et al. Acute decompensated heart failure (ADHF) during COVID-19 pandemic-insights from South India. Indian Heart J. 2021;73(4):464–469. doi: 10.1016/j.ihj.2021.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kawthalkar AS, Somani SD, Bhalde RP. Where have the others gone? Impact of lockdown during COVID-19 pandemic on patient populations undergoing Computed Tomography imaging in a public tertiary care hospital in India. Indian J Radiol Imaging. 2021;31(Suppl 1):S134–S138. doi: 10.4103/ijri.IJRI_424_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumanan T, Rajasooriyar C, Guruparan M, Sreeharan N. The impact of COVID-19 on the delivery of critical health care: experience from a non-high-income country. Asia Pac J Public Health. 2020;32(8):473–475. doi: 10.1177/1010539520963626. [DOI] [PubMed] [Google Scholar]
- 22.Kute VB, Gupta A, Patel HV, et al. The impact of COVID-19 pandemic on nephrology and transplant services and clinical training in India. Exp Clin Transplant. 2021;19(7):651–658. doi: 10.6002/ect.2021.0018. [DOI] [PubMed] [Google Scholar]
- 23.Mallick I, Chakraborty S, Baral S, et al. Prioritizing delivery of cancer treatment during a COVID-19 lockdown: the experience of a clinical oncology service in India. JCO Glob Oncol. 2021;7:99–107. doi: 10.1200/GO.20.00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meenakshisundaram R, Senthilkumaran S, Thirumalaikolundusubramanian P, et al. Status of acute myocardial infarction in southern india during COVID-19 lockdown: a multicentric study. Mayo Clin Proc Innov Qual Outcomes. 2020;4(5):506–510. doi: 10.1016/j.mayocpiqo.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pareek A, Patel AA, Harshavardhan A, et al. Impact of nationwide lockdown on cancer care during COVID-19 pandemic: a retrospective analysis from western India. Diabetes Metab Syndr. 2021;15(4) doi: 10.1016/j.dsx.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prajapati A, Gupta S, Nayak P, Gulia A, Puri A. The effect of COVID-19: Adopted changes and their impact on management of musculoskeletal oncology care at a tertiary referral centre. J Clin Orthopaed Trauma. 2021;23 doi: 10.1016/j.jcot.2021.101651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Priyadarshini M, Sapkota S. Impact of the COVID-19 on cancer management at birat medical college and teaching hospital, Nepal. Asian J Med Sci. 2021;12(5):21–24. doi: 10.3126/ajms.v12i5.34024. [DOI] [Google Scholar]
- 28.Ramakrishnan A, Somasundaram A, Srinivasan N, et al. Management of gastrointestinal services in Tamil Nadu, India, during COVID-19. Lancet Gastroenterol Hepatol. 2021;6(8):609–610. doi: 10.1016/s2468-1253(21)00193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ranganathan P, Sengar M, Chinnaswamy G, et al. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol. 2021;22(7):970–976. doi: 10.1016/s1470-2045(21)00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rangashamaiah S, Hayagreev V, Krishnan S, Prabhavathi B, Manjunath CN. The impact of COVID19 nationwide lock-down on STEMI hospitalization and outcomes in South India. Indian Heart J. 2021;73(3):379–381. doi: 10.1016/j.ihj.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reddy T, Kunwar A, Durgad K, et al. Decentralization of India Hypertension Control Initiative services to maintain continuum of care for hypertensive patients during COVID-19 pandemic in Telangana. Policy and practice. WHO South-East Asia J Public Health. 2021;10(3):49–58. doi: 10.4103/2224-3151.309873. [DOI] [Google Scholar]
- 32.Riju J, Tirkey AJ, Mathew M, et al. Analysis of early impact of COVID-19 on presentation and management of oral cancers - an experience from a tertiary care hospital in South India. Indian J Surg Oncol. 2021:1–8. doi: 10.1007/s13193-021-01302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma J, Mahajan A, Bakhshi S, et al. The impact of COVID-19 pandemic on access to treatment for children with cancer in India and treating center practices. Cancer. 2021 doi: 10.1002/cncr.33945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Subbiah S, Hussain SA, Samanth Kumar M. Managing cancer during COVID pandemic - Experience of a tertiary cancer care center. Eur J Surg Oncol. 2021;47(5):1220–1224. doi: 10.1016/j.ejso.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tyagi R, Mittal S, Madan K, et al. Assessment of the impact and reorganization of interventional pulmonology services at a tertiary care centre during nationwide lockdown for COVID-19 pandemic. Monaldi Arch Chest Dis. 2021;91(1) doi: 10.4081/monaldi.2021.1615. [DOI] [PubMed] [Google Scholar]
- 36.Yalamanchi R, Dasari BC, Narra L, et al. Cardiac intensive care unit admissions during COVID-19 Pandemic-A Single Center Experience. Ind J Crit Care Med. 2020;24(11):1103–1105. doi: 10.5005/jp-journals-10071-23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zachariah G, Ramakrishnan S, Das MK, et al. Changing pattern of admissions for acute myocardial infarction in India during the COVID-19 pandemic. Indian Heart J. 2021;73(4):413–423. doi: 10.1016/j.ihj.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dharma S, Dakota I, Firdaus I, et al. Performance of primary angioplasty for STEMI during the COVID-19 outbreak. Int J Angiol. 2021;30(02):148–154. doi: 10.1055/s-0041-1727133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riera R, Bagattini AM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Global Oncol. 2021;(7):311–323. doi: 10.1200/go.20.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization . 2020. The Impact of the COVID-19 Pandemic on Noncommunicable Disease Resources and Services: Results of a Rapid Assessment.https://www.who.int/publications/i/item/ncds-covid-rapid-assessment [Google Scholar]
- 41.Kapoor M, Agrawal D, Ravi S, Roy A, Subramanian SV, Guleria R. Missing female patients: an observational analysis of sex ratio among outpatients in a referral tertiary care public hospital in India. BMJ Open. 2019;9(8) doi: 10.1136/bmjopen-2018-026850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramakrishnan S, Khera R, Jain S, et al. Gender differences in the utilisation of surgery for congenital heart disease in India. Heart. 2011;97(23):1920. doi: 10.1136/hrt.2011.224410. [DOI] [PubMed] [Google Scholar]
- 43.Pacheco RL, Martimbianco ALC, Roitberg F, Ilbawi A, Riera R. Impact of strategies for mitigating delays and disruptions in cancer care due to COVID-19: systematic review. JCO Global Oncol. 2021;(7):342–352. doi: 10.1200/go.20.00632. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.