Abstract
This cross-sectional study uses US vital statistics data to evaluate alcohol use disorder–related mortality rates from 2012 to 2021, with a focus on trends during the COVID-19 pandemic.
Introduction
The US mortality rate has surged during the COVID-19 pandemic. Therefore, it is imperative to identify diseases and health conditions that have been affected disproportionately. Mounting evidence indicates that alcohol sales, alcohol consumption, and complications of alcohol use have increased during the pandemic.1,2,3 However, there are limited data on nationwide alcohol use disorder (AUD)–related mortality. Here, we use projective modeling to evaluate AUD-related mortality rates in the US from 2012 to 2021, with a focus on trends during the COVID-19 pandemic.
Methods
This cross-sectional study used deidentified publicly available data, so informed consent and institutional review board approval were not required in accordance with the Common Rule. The study followed the STROBE reporting guideline.
We obtained deidentified data from the National Vital Statistics System (NVSS) through the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database.4 The NVSS database registers more than 99% of deaths in the US, and this study used data updated to January 22, 2022.5 We included decedents with AUD, defined by International Classification of Diseases, Tenth Revision diagnosis codes, as one cause of death (multiple causes were possible). Age-standardized mortality rates were estimated with the indirect method using the 2000 US Census as the standard population. We performed linear regression analysis to determine 2020 and 2021 projected mortality rates based on trends between 2012 and 2019. We quantified the association of the pandemic with AUD-related deaths by calculating percentage differences between the projected and observed mortality rates. To enrich robustness, we also performed a sensitivity analysis by setting AUD as the underlying (primary) cause of death. Statistical analyses were performed using the CDC WONDER database (age standardization), R version 4.0.2 (data cleaning and management), and PyCharm version 3.9.0 (modeling analysis).
Results
There were 343 384 AUD-related deaths between 2012 and 2021. We stratified these deaths into decedent groups by age (25 to 44 years, 56 985 [16.6%]; 45 to 64 years, 192 346 [56.0%]; and ≥65 years, 94 053 [27.4%]) and by sex (266 755 men [77.7%]). By comparing observed and projected mortality rates, we noticed a surge in AUD mortality both overall and among all subgroups during the pandemic (Figure and Table). The observed AUD-related mortality rates increased by 24.79% in 2020 and 21.95% in 2021 vs the projected rates. Increased mortality rates were evident even when AUD was set as the underlying cause of death (30.74% in 2020 vs 28.77% in 2021).
Figure. Trends in Alcohol Use Disorder–Related Mortality Before and During the COVID-19 Pandemic, 2012 to 2021.
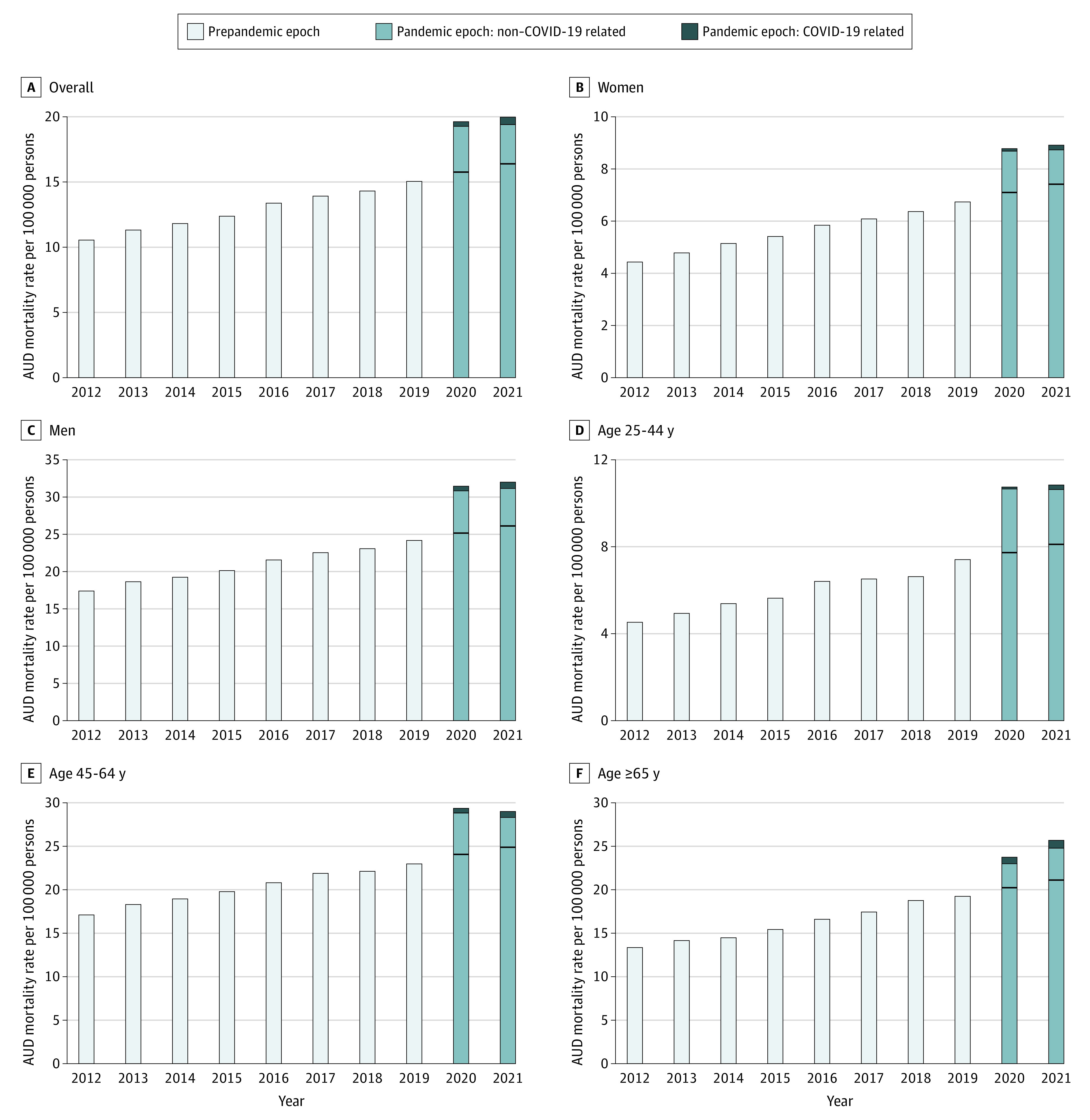
Mortality rates are presented for decedent groups stratified by sex and age. Linear regression was used to obtain projected values according to trends from 2012 to 2019. Horizontal black lines denote projected mortality rates.
Table. Age-Standardized and Projected Mortality Rates of Alcohol Use Disorder–Related Mortality Stratified by Decedent Age Group and Sex, 2012 to 2021.
| Variable | Age-standardized mortality rate per 100 000 persons | |||||||
|---|---|---|---|---|---|---|---|---|
| 2012 Observed |
2019 Observed |
2020 | 2021 | |||||
| Observed | Projected (95% CI) | % Differencea | Observed | Projected (95% CI) | % Differencea | |||
| AUD-related mortality | ||||||||
| Multiple causes of death | 10.63 | 15.11 | 19.68 | 15.77 (15.38-16.15) | +24.79 | 20.00 | 16.40 (15.99-16.82) | +21.95 |
| Multiple causes of death (non–COVID-19)b | 10.63 | 15.11 | 19.34 | 15.77 (15.38-16.15) | +22.64 | 19.48 | 16.40 (15.99-16.82) | +18.78 |
| Underlying cause of deathc | 3.05 | 4.57 | 6.21 | 4.75 (4.58-4.92) | +30.74 | 6.40 | 4.97 (4.78-5.15) | +28.77 |
| Age, y | ||||||||
| 25-44 | 4.55 | 7.43 | 10.83 | 7.71 (7.17-8.25) | +40.47 | 10.85 | 8.10 (7.52-8.68) | +33.95 |
| 45-64 | 17.14 | 23.00 | 29.21 | 24.01 (23.28-24.74) | +21.66 | 28.95 | 24.84 (24.06-25.62) | +16.55 |
| ≥65 | 13.53 | 19.40 | 23.83 | 20.31 (19.48-21.14) | +17.33 | 25.83 | 21.19 (20.30-22.08) | +21.90 |
| Sex | ||||||||
| Women | 4.47 | 6.77 | 8.85 | 7.10 (6.96-7.23) | +24.65 | 8.91 | 7.42 (7.28-7.57) | +20.08 |
| Men | 17.37 | 24.15 | 31.35 | 25.15 (24.48-25.83) | +24.65 | 31.96 | 26.11 (25.39-26.84) | +22.41 |
| Referent | ||||||||
| All-cause mortality | 1097.84 | 1071.78 | 1254.44 | 1077.69 (1056.87-1098.50) | +16.40 | 1271.54 | 1074.99 (1052.68-1097.30) | +18.28 |
Abbreviation: AUD, alcohol use disorder.
Percentage differences were calculated as follows: (Observed – Projected)/Projected × 100%.
Excluded decedents with COVID-19 infection as the underlying cause of death.
Included decedents with AUD listed as the primary cause of death.
In this study, the youngest age group (25-44 years) demonstrated the largest increase in AUD mortality (40.47% in 2020 vs 33.95% in 2021) across all age groups. The increase was similar for both sexes (approximately 24.65% for women and men in 2020 vs 20.08% and 22.41% in 2021, respectively). Less than 10.00% of excess deaths overall and among all subgroups were attributable to COVID-19 infection (Figure).
Discussion
In this cross-sectional study, we used data from 2012 to 2019 to project 2020 and 2021 mortality rates and found that AUD-related mortality rates increased among all ages and sexes during the pandemic. Younger persons, particularly those aged 25 to 44 years, had the steepest upward trend. The small proportion of COVID-19–related deaths suggests that excess deaths were more likely attributable to indirect effects of the pandemic such as stay-at-home policies and reduced medical and social resources for patients with AUD.
Our study is limited by potential misclassification bias in death certificate data. However, AUD is typically underrecognized, and we would expect such factors to result in lower observed death rates. Our findings suggest that the pandemic may have had a disproportionate association with AUD-related deaths and subgroups with high vulnerability and that tailored strategies are needed for AUD prevention and intervention to combat this public health crisis.
References
- 1.Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen PH, Ting PS, Almazan E, Chander G, Cameron AM, Gurakar A. Inter-hospital escalation-of-care referrals for severe alcohol-related liver disease with recent drinking during the COVID-19 pandemic. Alcohol. 2022;57(2):185-189. doi: 10.1093/alcalc/agab047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Micallef JV. How the COVID-19 pandemic is upending the alcoholic beverage industry. Forbes. April 4, 2020. Accessed January 10, 2022. https://www.forbes.com/sites/joemicallef/2020/04/04/how-the-covid-19-pandemic-is-upending-the-alcoholic-beverage-industry/?sh=27fe1c5f4b0b
- 4.Centers for Disease Control and Prevention . CDC WONDER (Wide-Ranging Online Data for Epidemiologic Research) Database. 2021. Accessed February 15, 2022. https://wonder.cdc.gov/
- 5.Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B. Deaths: final data for 2018. Natl Vital Stat Rep. 2021;69(13):1-83. [PubMed] [Google Scholar]


