Abstract
This cross-sectional study of Medicare data from 2012 to 2019 assesses national trends in the use of mitral transcatheter edge-to-edge repair relative to surgical mitral valve repair.
Mitral transcatheter edge-to-edge repair (TEER) has emerged as an alternative to surgical mitral valve repair (SMVR) in patients with a prohibitive surgical risk or advanced heart failure with severe, symptomatic mitral regurgitation (MR).1,2 Characterizing the geographic and demographic dispersion of TEER and SMVR is important for understanding access to care and the populations served by these therapies. As there is a clear learning curve with TEER, understanding the growth in its use is of direct relevance to hospitals, physicians, and patients.3,4,5 In this cross-sectional analysis, we characterize national trends in the use of TEER relative to SMVR in a large Medicare population.
Methods
We queried the Medicare Provider Analysis and Review (MedPAR) File from 2012 to 2019 for all fee-for-service Medicare beneficiaries undergoing SMVR (n = 34 375) and TEER (n = 16 931). We used International Classification of Diseases, Ninth Revision (ICD-9) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes for SMVR and TEER.
The ratio of TEER-to-SMVR procedural counts was stratified according to geographical location and year, as well as age, sex, and race and ethnicity. All analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
Results
The Table shows the trends in the use of TEER vs SMVR stratified according to patient demographic characteristics. There was continued growth in TEER use throughout the study period, while SMVR use remained comparatively constant (Figure, A). In 2012, the rate of TEER use was 0.76 per 100 000 beneficiaries and increased to 17.95 by 2019 (P < .001). In contrast, SMVR use decreased from 16.06 to 13.58 per 100 000 (P = .04). The annualized ratio of TEER to SMVR increased from 0.05 to 1.32 (P < .001) (Figure, B). The number of hospitals performing TEER grew from 91 in 2013 to 396 in 2019, and the median distance to care decreased from 44.2 miles in 2012 to 19.0 in 2019 (P = .003); the number of hospitals performing SMVR remained consistent between 2012 and 2019 (730 and 721), and the median distance to care increased from 17.2 miles in 2012 to 21.7 in 2019 (P = .001).
Table. Biennial Ratios of Transcatheter Edge-to-Edge Repair to Surgical Mitral Valve Repair.
| Characteristic | 2013 | 2015 | 2017 | 2019 | P value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TEER | SMVR | Ratio | TEER | SMVR | Ratio | TEER | SMVR | Ratio | TEER | SMVR | Ratio | ||
| Total | 228 | 4412 | 0.05 | 1592 | 4233 | 0.38 | 3024 | 4629 | 0.65 | 5111 | 3867 | 1.32 | <.001a |
| Age, y | |||||||||||||
| 65-74 | 67 | 2327 | 0.03 | 309 | 2316 | 0.13 | 607 | 2570 | 0.24 | 1146 | 2294 | 0.50 | <.001b |
| 75-84 | 95 | 1801 | 0.05 | 644 | 1680 | 0.38 | 1231 | 1878 | 0.66 | 2248 | 1472 | 1.53 | |
| ≥85 | 66 | 284 | 0.23 | 639 | 237 | 2.70 | 1186 | 181 | 6.55 | 1717 | 101 | 17.00 | |
| Sex | |||||||||||||
| Male | 123 | 2462 | 0.05 | 830 | 2377 | 0.35 | 1550 | 2685 | 0.58 | 2707 | 2323 | 1.17 | <.001b |
| Female | 105 | 1950 | 0.05 | 762 | 1856 | 0.41 | 1474 | 1944 | 0.76 | 2404 | 1544 | 1.56 | |
| Race and ethnicity | |||||||||||||
| White, Non-Hispanic | 208 | 4024 | 0.05 | 1469 | 3877 | 0.38 | 2712 | 4184 | 0.65 | 4538 | 3455 | 1.31 | .02b |
| Otherc | 20 | 388 | 0.05 | 123 | 356 | 0.35 | 312 | 445 | 0.70 | 573 | 412 | 1.39 | |
| Geographic location | |||||||||||||
| South | 87 | 1680 | 0.05 | 588 | 1592 | 0.37 | 1146 | 1743 | 0.66 | 1977 | 1331 | 1.49 | <.001b |
| Midwest | 41 | 1111 | 0.04 | 361 | 1019 | 0.35 | 581 | 1174 | 0.49 | 988 | 1032 | 0.96 | |
| Northeast | 45 | 870 | 0.05 | 251 | 922 | 0.27 | 562 | 954 | 0.59 | 903 | 784 | 1.15 | |
| West | 55 | 751 | 0.07 | 392 | 700 | 0.56 | 735 | 758 | 0.97 | 1243 | 720 | 1.73 | |
Abbreviations: SMVR, surgical mitral valve repair; TEER, transcatheter edge-to-edge repair.
Cochran-Armitage trend test of TEER-to-SMVR ratios.
χ2 Test of TEER-to-SMVR ratios associated with patient characteristics.
Other included Asian or Pacific Islander, American Indian or Alaska Native, Black, Hispanic, and unknown. Specific numbers for these categories are unavailable because of Centers for Medicare & Medicaid reporting policies.6
Figure. Use of Transcatheter Edge-to-Edge Repair (TEER) vs Surgical Mitral Valve Repair (SMVR), 2012-2019.
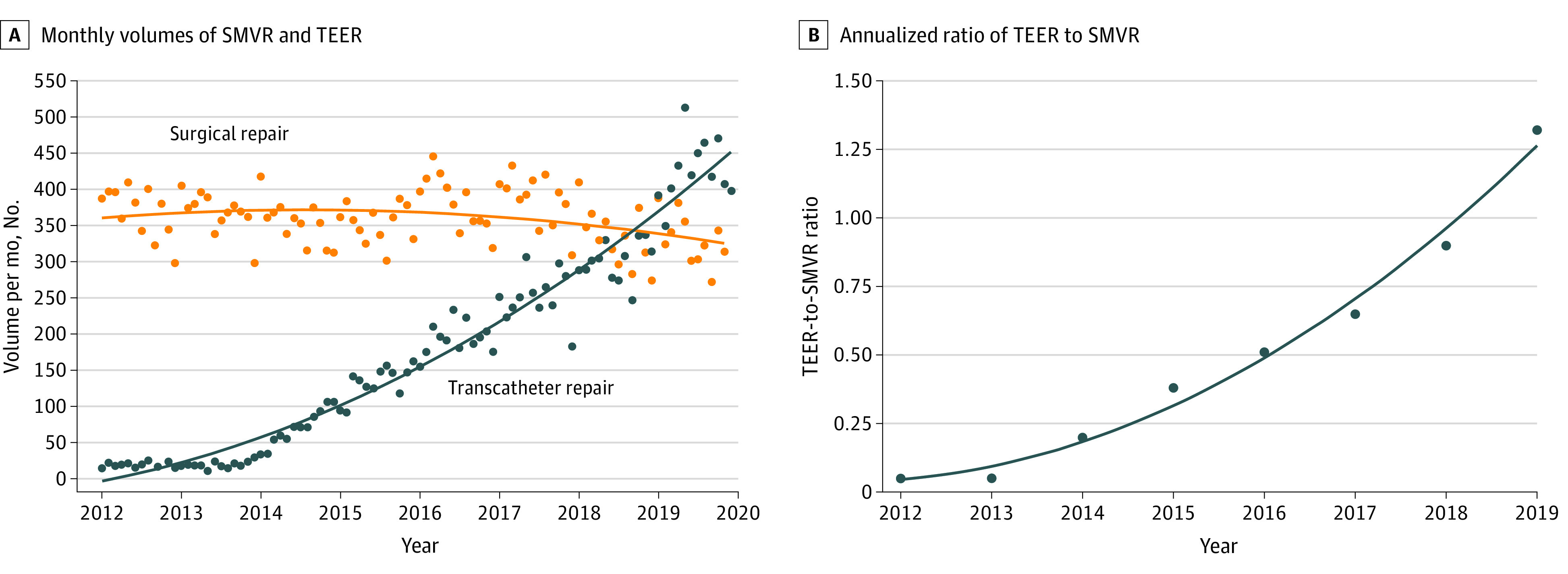
Food and Drug Administration (FDA) approval of TEER for primary mitral repair occurred in 2013. FDA approval of TEER for secondary mitral repair occurred in 2019.
Discussion
We observed a significant increase in the use of TEER relative to use of SMVR among Medicare beneficiaries over the course of 8 years. The growth in TEER closely follows approval of the MitraClip (Abbott), with an initial rise in 2013 after its approval for primary MR and continued growth in 2019 after its approval for secondary MR.2
During the study period, SMVR use remained stable, while TEER continued to grow. This phenomenon has also been observed for transcatheter aortic valve replacement.7 Notably, we found that use of TEER surpassed that of SMVR by mid-2018, suggesting TEER has become a new option for patients who might not have been candidates for surgery, such as those at high surgical risk or with left ventricular dysfunction and secondary MR in whom medical therapy has failed.
We also found significant geographical dispersion of TEER and hospitals performing TEER throughout the US and observed variation in the use of TEER vs SMVR among demographic subgroups, with use of both TEER or SMVR being lower among female patients and members of racial or ethnic minority groups. These disparities could be associated with inherent differences in epidemiological factors as well as other social determinants of health or treatment biases.
This analysis is limited by the exclusion of non-Medicare beneficiaries, as well as the inability to differentiate between the relative use of TEER and SMVR for primary vs secondary MR. We also did not include data on surgical or transcatheter mitral valve replacement. Nevertheless, understanding the continued growth and dispersion of TEER and potential disparities in surgical and transcatheter mitral valve therapies have important clinical and regulatory implications.
References
- 1.Feldman T, Foster E, Glower DD, et al. ; EVEREST II Investigators . Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364(15):1395-1406. doi: 10.1056/NEJMoa1009355 [DOI] [PubMed] [Google Scholar]
- 2.Stone GW, Lindenfeld J, Abraham WT, et al. ; COAPT Investigators . Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018;379(24):2307-2318. doi: 10.1056/NEJMoa1806640 [DOI] [PubMed] [Google Scholar]
- 3.Chhatriwalla AK, Vemulapalli S, Holmes DR Jr, et al. Institutional Experience With Transcatheter Mitral Valve Repair and Clinical Outcomes: Insights From the TVT Registry. JACC Cardiovasc Interv. 2019;12(14):1342-1352. doi: 10.1016/j.jcin.2019.02.039 [DOI] [PubMed] [Google Scholar]
- 4.Chhatriwalla AK, Vemulapalli S, Szerlip M, et al. Operator Experience and Outcomes of Transcatheter Mitral Valve Repair in the United States. J Am Coll Cardiol. 2019;74(24):2955-2965. doi: 10.1016/j.jacc.2019.09.014 [DOI] [PubMed] [Google Scholar]
- 5.Bonow RO, O’Gara PT, Adams DH, et al. 2019 AATS/ACC/SCAI/STS expert consensus systems of care document: operator and institutional recommendations and requirements for transcatheter mitral valve intervention: a joint report of the American Association for Thoracic Surgery, the American College of Cardiology, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2020;76(1):96-117. doi: 10.1016/j.jacc.2019.12.002 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. CMS Cell Suppression Policy. May 8, 2017. Updated January 1, 2020. Accessed March 28, 2022. https://www.hhs.gov/guidance/document/cms-cell-suppression-policy
- 7.Young MN, Kearing S, Malenka D, Goodney PP, Skinner J, Iribarne A. Geographic and demographic variability in transcatheter aortic valve replacement dispersion in the United States. J Am Heart Assoc. 2021;10(12):e019588. doi: 10.1161/JAHA.120.019588 [DOI] [PMC free article] [PubMed] [Google Scholar]


