Abstract
The Youth and Young Adults Cancer Knowledge Attitudes and Practices (C-KAP) exploratory study in 2 rural underserved areas in a border community. C-KAP is an interdisciplinary research pilot project led by university scholars in psychology and social work in partnership with community partners. The exploratory cross-sectional mix-method study recruited 141 (n=141) youth and young adults (ages 18-39). This study was informed on empirical research and a bilingual online questionnaire was field-tested, and data was collected via QuestionPro Software. Quantitative analysis was conducted using SPSS version 27. Descriptive statistics and frequency analysis were used for demographics and basic statistics. Chi square tests and Fisher’s exact tests between variables were ran to find statistically significant associations. For the qualitative data, independent coders conducted recurrent content analysis to identify themes. Salient themes include knowledge about cancer types; access to health care; prevention; and the perceived impact of COVID-19 pandemic. Findings highlight a lack of knowledge and orientation on cancer in youth and young adults suggesting the need for community tailored education and screening interventions. Other findings reflect gender differences in knowledge and practices, which indicates that a gender-specific lens is needed when delivering education.
Keywords: Rural Health, Mixed-methods, Cancer Prevention, Youth, U.S.-Mexico Border
SAGE Highlight Questions
-
What do we already know about this topic?
Adolescents, youth, and young adults (AYAS) are an understudied population in cancer research whose knowledge on cancer and prevention measures are key factors in an early cancer diagnosis and survival.
-
How does your research contribute to the field?
The study provides insight from the interest population on their current knowledge, attitudes, and practices as well as their own perspective on how to best deliver education to their age group.
-
What are your research’s implications towards theory, practice, or policy?
The study highlights the need for population-specific programs (ie, age, gender, community-type) that can better implement cancer prevention knowledge, provoke health attitudes, and ensure AYAS are engaging in protective practices.
Introduction
Globally, cancer remains a major cause in both morbidity and mortality across all age groups. The adolescent, youth, and young adult population (AYAs) account for 5% of cancer diagnosis in the United States with about 89,000 young people ages 15 to 39 diagnosed with cancer each year. 1 In Texas, AYAs account for 7,800 diagnoses annually, with 1,000 of these dying. 2 AYAs are defined as those between ages 15-39 years; adolescents, ages 15-19 years; emerging adults, ages 20-25 years; and young adults, ages 26-39 years. 3 The AYAs population is unique in terms of cancer risks and psychological needs. 4 Cancer is 1 of the leading causes of disease-related death in these age groups. 5 The most common types of cancer among these age groups include brain and other central nervous system tumors, breast, cervical, colorectal, leukemia, lymphoma, melanoma, sarcoma, testicular, and thyroid. 1 The importance of addressing the needs of AYAs helps educational programs focus on their developmental stage and learning abilities. Adult learners are more independent, self-driven, tend to seek information surrounding current interests and their roles in society, while adolescents are more likely to seek help from others who are more knowledgeable, gather a drive to learn through social engagement, interaction and appreciate information that is related to their lives outside of a school setting. 6 Adapting educational messages to each age group would enrich the ways information is presented, delivered, and how education may lead to healthy practices and behaviors.
Historically, adolescents and young adults diagnosed with cancer have been an understudied population, and their unique needs, care experiences, and outcomes are not well understood.7-9 In a research study of adolescent narratives and young adult cancer survivorship, participants referenced the importance of building awareness among age groups; encouraging personal health care focus; and expanding knowledge of the far-reaching psychological, social, and medical impacts, both during and beyond the treatment phase. 10 These experiences have important implications for health seeking behaviors, including how they interpret symptoms and make self-management decisions.
Coping mechanisms to understand illness and symptoms are primarily based on cognitive processing, prior experiences, cultural beliefs, and social comparisons. 11 AYAs cancer experiences are diverse, creating challenges for practitioners who seek to optimize health outcomes. They constitute a salient population for digital use to translate and transfer information to improve health outcomes by providing messages geared at the levels of cognitive capacity and psychosocial development. 12 Research indicates gender differences in cancer knowledge, attitudes, and practices. Traditionally males have a history of lower participation in cancer screenings. 13 Not only is health behavior different, so is the generation of health practices among genders. In a meta-analysis study, females in good health were found to actively seek more cancer information than males, and males diagnosed with cancer were more likely to seek cancer information than females. 14
Therefore, we conducted an exploratory study to investigate cancer knowledge, attitudes and practices from the perspective of youth and young adults in 2 rural communities in the border region. Findings will inform cultural and linguistic proficient education efforts to engage AYAs to promote behaviors to reduce cancer risks.
Methods
Knowledge, Attitudes, and Practices (KAP) Survey Model
The study used the KAP survey model which consists of predefined questions in a standardized instrument consisting of closed and open-ended questions using a mixed method approach. KAP surveys reveal misconceptions that may represent barriers and challenges to behavior change and are frequently used to collect information on knowledge (ie, what is known), attitudes (ie, what is thought), and practices (ie, what is done).15-17
The study is exploratory and cross-sectional mixed method. The inclusion criteria consisted of adults 18-39 year of age residing in either of the 2 study locations at the time of the study. A pre-screening tool was used to assess eligibility. Potential participants were asked to provide their zip code number and their birthdate. If the zip code entered was not 1 of the 2 of the study location or if their birthday indicated not being withing the 18-39 age group, they were excluded from the study. The pre-screening tool was set to deny any additional tries from the same device previously used. A total of 189 potential participants were pre-screened with 48 being considered ineligible due to residing in a different zip code. Potential participants who were eligible were then guided to the study consent form and would begin the questionnaire upon consent. The study received IRB approval from the authors’ academic institution. Data collection took place through QuestionPro software institutional license between September 22 and November 22, 2020. Local community partners, and Community Health Workers, bilingual project flyers distributed in study locations, and Facebook ads were used to assist with recruitment. The study used a convenience sampling technique in addition to snowball sampling, which encouraged participants that completed the study to invite others who met inclusion criteria to do the same. Participants who completed the study were welcome to share the study flyers, which included a QR code with study link as well as email contact information for the study, with other potential participants who they knew met study eligibility. Participants received a $20 e-gift card as an incentive for their time.
Study Locations
The study took place in 2 rural communities [outside of the city limits of a border city]. The population estimate for study location A in 2019 was 34,370 with 9,364 households with an average of 5.6 persons, and 33% of the population younger than 65 years old do not have health insurance coverage. 18 The civilian labor force 16 years and older is at 57.4% with 48.9% of those being females. 19 More than 96.3% of the population report being Hispanic or Latino, and 54% identified as female. The median income (from 2015-2019) was $14, 591 U.S. dollars, and 23.7% of people live in poverty. Sixty-three percent of individuals 25 years and older report having a high school diploma, General Educational Development (GED) a high school equivalent certification or higher, and 7.7% an undergraduate or graduate degree.
The population of location B is 9,089 with 2,484 households with an average of 3.67 persons, twenty eight percent of individuals below 65 years do not have health insurance and the civilian labor force above 16 years is at 57%, with 45.8% of those being females.18,20 Close to 99% of the population reported being Hispanic or Latino, and 51.8% reported a female identity. The median income is $14, 762 U.S. dollars, with 35% of people living in poverty. Sixty 1 percent of individuals 25 years and older reported having a high school diploma, and 11.4% a bachelor’s degree or higher.
Measures
Once participants were screened as eligible and consented to participation, they completed the online questionnaire consisting of 6 sections: general and sociodemographic characteristics, knowledge of cancer risks, attitudes about cancer screenings, health practices and health seeking behaviors, prevention practices, and role that COVID-19 played in cancer care. The instrument was developed by the primary authors informed by KAP model literature and health promotion theory. The KAP model is designed to be mixed methods to be able to identify the gaps and how to address these. Instrument was translated to Spanish, back translated, and field-tested with a group of 5 bilingual youth and young adults attending college. The instrument was available in both English and Spanish, participants had the option to complete in their preferred language. The online questionnaire took between 20-30 minutes for participants to complete. With the help of the University Data Analytics Laboratory from the institution, it was determined that a convenience sample of 70 participants from each location (1.3 and 4% of the total age group residing in Location A and Location B) would be a modest sample given the exploratory nature of the study. Therefore, the sample consisted of N = 141 participants, 44% (n = 62) from location A and 56% (n = 79) from location B.
Data Analysis
The research team analyzed the quantitative data using SPSS (Version 27.0). 21 For participant sociodemographic characteristics see Table 1. Descriptive analyses included Chi-square tests and Fisher’s exact tests between variables to find associations, with α = .05. Significant associations between variables relevant to the study were followed-up with odds ratios. Chi-square for association were conducted between gender and (a) sociodemographic characteristics, (b) knowledge of cancer and risk, (c) attitudes about cancer screenings, (d) practice and health seeking behaviors, (e) prevention actions, and (f) COVID-19 and cancer care. Unless noted otherwise, all expected cell frequencies were greater than 5. Fishers’ Exact test was used when expected cell frequencies fell below 5. The Multiple Marginal Independence test (MMI) was utilized to assess the relationship between gender and the source of cancer prevention information since each respondent could have selected multiple responses (eg, select all). 22 Gender was defined as and the source of cancer prevention information was set as . The MMI was conducted in R (version 4.1.0) using the MMI. test function from the MRCV package. Bonferroni adjustments were used to calculate for statistical significance, as per the guideline provided by Bilder and Loughin. 23
Table 1.
Sample sociodemographic and general characteristics (N = 141).
| — | Location a (n = 62) | Location B (n = 79) | |
|---|---|---|---|
| Age | Average | 26.1 (SD 5.7) | 25.4 (SD 5.6) |
| — | 18-19 yrs (N=12) | 6 (50%) | 6 (50%) |
| — | 20-25 yrs (N=73) | 29 (39.7%) | 44 (60.3%) |
| — | 26-39 yrs (N=56) | 27 (48.2%) | 29 (51.8%) |
| Sex, N (%) | Male | 22 (35.5%) | 27 (34.2%) |
| — | Female | 40 (64.5%) | 52 (65.8%) |
| Education | Less than a high school | 3 (4.8%) | 3 (3.8%) |
| — | High School/GED | 3 (4.8%) | 11 (13.9%) |
| — | High school graduate | 16 (25.8%) | 39 (49.4%) |
| — | Technical school | 5 (8.1%) | 8 (10.2%) |
| — | College/University undergraduate | 31 (50%) | 16 (20.3%) |
| — | Graduate | 3 (4.8%) | 1 (1.3%) |
| — | Not applicable/none | 1 (1.6%) | 1 (1.3%) |
| — | 0 – $29,999 | 29 (46.8%) | 39 (49.4%) |
| — | $30,000 – $49,999 | 14 (22.6%) | 17 (21.5%) |
| — | $50,000 – $99,999 | 11 (17.7%) | 22 (27.8%) |
| Annual family income | $100,000 – $349,999 | 8 (12.8%) | 1 (1.3%) |
| Ethnicity | Indian/Alaskan | 1 (1.6%) | 1 (1.3%) |
| — | Asian | 2 (2.2%) | 0 (0%) |
| — | African american | 3 (4.8%) | 1 (1.3%) |
| — | Hispanic/Latino(a) | 47 (75.8%) | 62 (78.5%) |
| — | White | 15 (24.2%) | 21 (26.6%) |
| Marital status | Single | 43 (69.4%) | 50 (63.3%) |
| — | Married | 16 (25.8%) | 21 (26.6%) |
| — | Common law | 1 (1.6%) | 5 (6.3%) |
| — | Divorced | 1 (1.6%) | 1 (1.3%) |
| — | Prefer not to answer | 1 (1.6%) | 1 (1.3%) |
| Employment status | Employed | 32 (51.6%) | 40 (50.6%) |
| Unemployed | 30 (48.4%) | 39 (49.4%) |
aSD = Standard Deviation.
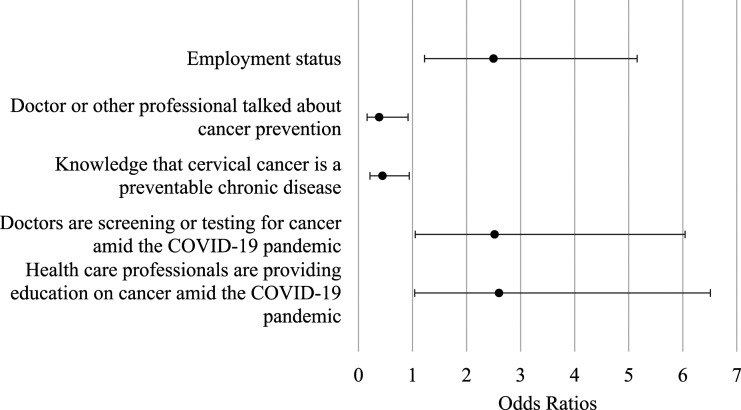
Figure 1 Both thematic and content analyses were conducted with the qualitative data. Content analysis was conducted first to identify and quantify the data and utilized to guide the thematic analysis. Thematic analyses were conducted to identify the patterns across answers from the population of interest and to organize qualitative data in English and Spanish to identify central themes as the team is proficient in both languages. A pre-coding technique was utilized to filter information through highlighting salient words and/or phrases in individual participant responses. The first 2 authors, with more than 15 years of experience with qualitative data, and third author, an undergraduate student with basic experience with thematic data analysis following protocol, observed the data together to develop a consensus way to code. Once the method was established, the authors individually coded the data to later come together and discuss. Standardization of coding by 3 independent coders and triangulation by the first 3 authors was used to reduce bias, enhance intercoder reliability, and reduce error. 24 Disagreements were discussed and resolved during coding meetings. Final codes and categories were generated through collaboration among all 3 independent coders.
Figure 1.
Odds Ratios Output.
Results
Qualitative
Qualitative analysis revealed themes associated with cancer knowledge, attitudes, perceived health status, sources of information, and the impact of COVID-19 on cancer screening.
Knowledge
Participants discussed cancer-warning signs, risks factors, and types of cancers in AYAs (ie, leukemia, breast, cervical, and lung cancer).
In Location A and Location B 57% and 62% respectively reported cancer to be a disease. Participants in Location B defined cancer in terms of physiology like cell abnormalities, tumors, and mutations; and in Location A, they cited types and sites of cancer and referenced the condition as painful and deathly.
“Cancer is an illness that can affect different parts of your body and affect your health. It can even lead to death.” (Location A).
“Disease involving abnormal cell growth with the potential to invade or spread to other part of body.” (Location B).
Warning Signs
In both locations, smoking, diet, and drinking alcohol were the 3 most salient lifestyle risks and warning signs mentioned.
“Cansancio, dolor, falta de apetito.” [Tiredness, pain, lack of appetite]. (Location B)
“Lumps, headaches, fever.” (Location B)
“No energy, tiredness, and low weight.” (Location A).
Attitudes and Perceptions
Participants were asked about cancer attitudes, familiarity with the disease, perceived risk or development, and screenings and perceptions.
Participants were asked about their thoughts when they heard the word cancer. Half of the sample (55.3%) in both locations perceived cancer as a terminal disease or death; 29.8% named chemotherapy as a type of treatment; 37.1 and 29.1% of participants from Location A and Location B respectively reported believing it was not possible for them to develop cancer. In Location A, 51.9 and 33.5%, in Location B reported not knowing if it is possible for them to develop the condition. Participants that reported yes to developing cancer stated genetics and family history as the primary reasons. When asked about cancer prevention, participants identified lifestyle factors like diet, exercise, and not smoking as the primary behaviors in both locations.
“Regular exercise, no bad habits, maintain a good attitude, healthy and scientific diet.” (Location B).
“I don’t smoke. I practice safe sex to reduce the likelihood of cervical cancer.” (Location A).
“Regular checkups, prevention of drug abuse, smoking, decent diet kind of, use of SFP (sunblock).” (Location B)
However, when asked if they were actively doing things to prevent cancer only 72.6 and 67.1% of the participants in Location A and Location B respectively reported practicing prevention.
Perceived Health Status
Participants rated their perceived level of health from a 0 (being the lowest) to a 10 (being the highest). Participants in Location A reported an average of 7.75 (SD = 1.55) and Location B reported an average of 7.70 (SD = 1.76). When asked why they scored their health at that level, participants from both locations referenced physical activity (28.1%) and overall health status (29.1%). On the other hand, a bad diet (23.8%) and a low physical activity (23.7%) were the reasons why their health status was low.
“My health is excellent, but I still need to take preventive measures against cancer.” (Location B).
“Although I take my health serious, sometimes I don’t get enough exercise.” (Location A).
Sources of Cancer Information
One of the study goals was to document the need for cancer interventions in rural communities. It is important to make visible the need for educational programs on cancer prevention, early screening, and care for AYA’s to tailor messaging based on age group and cultural and linguistic needs. The top 4 sources where participants obtain cancer information are the internet, health professionals, TV and radio. The majority of participants from both locations referenced social media as a venue where they would seek information on cancer, 87.1% response in Location A and 88.6% in Location B. When asked if they would share with others the information learned about cancer prevention the majority agreed, 92% Location A and 93.7% in Location B.
Impact of COVID-19 on Cancer Screenings
Questions about the COVID-19 pandemic were included. Participants were asked if they believed that cancer screenings, education, and care were available during the COVID-19 pandemic. Participants reported that COVID-19 has been the primary focus in health care and therefore cancer screening or testing (26.2%), education (24.12%), and treatment (12.05%) were not a priority. Participants stated:
“They [doctors and health professionals] are just focused on COVID.” (Location B).
“Doctor’s main job now is to limit outbreaks (COVID-19) among people, with extremely dangerous consequences, rather than focusing on cancer.” (Location A).
Quantitative
Participants from location A and location B respectively identified as female (64.5%; 65.8%), Hispanic (75.8%; 78.5%), with high school diploma (25.8%; 49.4%), college education (50%; 20.8%); being single (69.4%; 63.35%) and employed (51.6%; 50.6%). The mean age in location A was 26.1 (SD = 5.7), and 25.4 (SD 5.6) in location B.
There was a statistically significant association between gender and employment status, . More males were employed ( ) than not employed ( ). On the other hand, less females were employed ( ) than not employed ( ). Females have 2.5 times higher odds of not having employment compared to males, 95% CI [1.222, 5.156] Table 2.
Table 2.
Response Frequencies on Main Question Items by Gender.
| — | Male | Female | |||
|---|---|---|---|---|---|
| — | n | % | n | % | |
| Internet and social media | Yes | 28 | 57.10 | 53 | 57.60 |
| No | 21 | 42.90 | 39 | 42.40 | |
| Media (ie, television, radio) | Yes | 18 | 36.70 | 35 | 38.00 |
| No | 31 | 63.30 | 57 | 62.00 | |
| Friends and peers | Yes | 11 | 22.40 | 28 | 30.40 |
| No | 38 | 77.60 | 64 | 69.60 | |
| Relatives | Yes | 2 | 4.10 | 23 | 25.00 |
| No | 47 | 95.90 | 69 | 75.00 | |
| Newspaper | Yes | 3 | 6.10 | 10 | 10.90 |
| No | 46 | 93.90 | 82 | 89.10 | |
| Healthcare workers or professionals | Yes | 14 | 28.60 | 40 | 43.50 |
| No | 35 | 71.40 | 52 | 56.50 | |
| Never received cancer information | Yes | 3 | 6.10 | 9 | 9.80 |
| No | 46 | 93.90 | 83 | 90.20 | |
| Able to list 3 cancers that are most frequently found in these age groups | Yes | 21 | 42.90 | 54 | 59.30 |
| No | 28 | 57.10 | 37 | 40.70 | |
| Able to name 3 places that offer health screening for AYAs | Yes | 13 | 26.50 | 38 | 41.80 |
| No | 36 | 73.50 | 53 | 58.20 | |
| Able to mention 3 places that offer cancer screenings for AYAs | Yes | 11 | 22.40 | 29 | 31.90 |
| No | 38 | 77.60 | 62 | 68.10 | |
| Is cancer a preventable chronic disease? | Yes | 21 | 42.90 | 54 | 60.00 |
| No | 28 | 57.10 | 36 | 40.00 | |
| Is cervical cancer a preventable chronic disease? | Yes | 14 | 28.60 | 43 | 47.30 |
| No | 35 | 71.40 | 48 | 52.70 | |
| Is lung cancer a preventable chronic disease? | Yes | 36 | 73.50 | 53 | 58.90 |
| No | 13 | 26.50 | 37 | 41.10 | |
| Do you know somebody with cancer? | Yes | 26 | 53.10 | 43 | 46.70 |
| No | 21 | 42.90 | 46 | 50.00 | |
| don’t know | 2 | 4.10 | 3 | 3.30 | |
| Does cancer risk run in family? | Yes | 12 | 24.50 | 29 | 31.90 |
| No | 22 | 44.90 | 34 | 37.40 | |
| don’t know | 15 | 30.60 | 28 | 30.80 | |
| Is it possible for you to develop any type of cancer? | Yes | 15 | 30.60 | 17 | 18.70 |
| No | 17 | 34.70 | 28 | 30.80 | |
| don’t know | 17 | 34.70 | 46 | 50.50 | |
| Have you ever asked your doctor to perform a screening to know your status and ways to prevent any type of cancer? | Yes | 3 | 6.10 | 24 | 26.40 |
| No | 46 | 93.90 | 67 | 73.60 | |
| Do you practice any healthy behavior in order to prevent cancer? | Yes | 33 | 67.30 | 48 | 52.70 |
| No | 16 | 32.70 | 43 | 47.30 | |
| Have you ever participated in an early cancer prevention program? | Yes | 0 | .00 | 6 | 6.60 |
| No | 49 | 100.00 | 85 | 93.40 | |
| Has a doctor or professional ever talked with you about preventing cancer? | Yes | 8 | 16.30 | 31 | 33.70 |
| No | 41 | 83.70 | 61 | 66.30 | |
| Has a doctor or other professional ever talked with you about physical activity? | Yes | 30 | 61.20 | 69 | 75.00 |
| No | 19 | 38.80 | 23 | 25.00 | |
| Has a doctor or other professional ever talked with you about drinking alcohol or using drugs? | Yes | 28 | 58.30 | 60 | 65.20 |
| No | 20 | 41.70 | 32 | 34.80 | |
| Has a doctor or other professional ever talked with you about smoking? | Yes | 29 | 60.40 | 62 | 67.40 |
| No | 19 | 39.60 | 30 | 32.60 | |
| Which of the following best describes you presently? | Actively doing things to prevent cancer | 33 | 67.30 | 64 | 69.60 |
| Not doing anything to prevent cancer | 16 | 32.70 | 27 | 29.30 | |
| From 0 (lowest) to 10 (highest) how do you grade your health status? | 1 | 0 | .00 | 1 | 1.10 |
| 3 | 1 | 2.00 | 2 | 2.20 | |
| 4 | 0 | .00 | 2 | 2.20 | |
| 5 | 3 | 6.10 | 5 | 5.40 | |
| 6 | 4 | 8.20 | 10 | 10.90 | |
| 7 | 12 | 24.50 | 6 | 6.50 | |
| 8 | 16 | 32.70 | 36 | 39.10 | |
| 9 | 7 | 14.30 | 17 | 18.50 | |
| 10 | 6 | 12.20 | 13 | 14.10 | |
| Would you use digital and social media to learn about cancer? | Yes | 44 | 89.80 | 80 | 87.00 |
| No | 5 | 10.20 | 12 | 13.00 | |
| Do you think it is important to develop programs for AYAs that improve cancer education and prevention? | Yes | 48 | 98.00 | 84 | 93.30 |
| No | 1 | 2.00 | 6 | 6.70 | |
| If you learned about cancer prevention, would you teach to others? | Yes | 45 | 91.80 | 86 | 95.60 |
| No | 4 | 8.20 | 4 | 4.40 | |
| Would you do any volunteer service or raise funds to support someone with cancer? | Yes | 45 | 91.80 | 72 | 80.00 |
| No | 4 | 8.20 | 18 | 20.00 | |
| Do you think that with COVID-19, doctors are screening or testing for cancer? | Yes | 41 | 83.70 | 61 | 67.00 |
| No | 8 | 16.30 | 30 | 33.00 | |
| Since COVID-19, do you think that health care professionals are educating on cancer? | Yes | 41 | 85.40 | 63 | 69.20 |
| No | 7 | 14.60 | 28 | 30.80 | |
| Do you think that with COVID-19 doctors continue providing cancer care? | Yes | 43 | 91.50 | 78 | 85.70 |
| No | 0 | .00 | 0 | .00 | |
There was a statistically significant association between gender and having a doctor or other professional to talk about cancer prevention, . Of the male respondents ( ), only 16.3% ( ) had ever been informed by a doctor or professional about cancer prevention. Similarly, only 33.7% ( ) of female respondents ( ) had ever been informed by a doctor or professional about cancer prevention. Compared to females, males have 1.616 times higher odds of not having a doctor or other professional to talk to about cancer prevention, 95% CI [1.082, 1.840].
There was a statistically significant association between gender and knowledge that cervical cancer is a preventable chronic disease, , . Of the male respondents ( ), only 28.6% ( ) knew that cervical cancer is a preventable chronic condition. For female respondents ( ), 47.3% ( ) knew that cervical cancer is a preventable chronic condition. Compared to females, males have 1.553 times higher odds of not knowing that cervical cancer is a preventable disease, 95% CI [1.060, 1.788].
There was a statistically significant association between gender and the belief that doctors are screening or testing for cancer amid the COVID-19 pandemic, . Of male respondents ( ), 83.7% ( ) think that doctors are screening or testing for cancer during the COVID-19 pandemic. Similarly, 67% ( ) of all females ( ) think that doctors are screening or testing for cancer amid COVID-19. Compared to males, females have 2.520 times higher odds of thinking that doctors are screening or testing for cancer during the COVID-19 pandemic, 95% CI [1.051, 6.044].
There was a statistically significant association between gender and the belief that health care professionals (ie, doctors, nurses and other health workers) were providing education on cancer during the COVID-19 pandemic, . Of male respondents who answered both questions ( ), 85.4% ( ) they think that health care professionals are providing education on cancer amid the COVID-19. Similarly, 69.2% ( ) of all females ( ) think that health care professionals are providing education on cancer during the pandemic. Compared to males, females have 2.603 times higher odds of thinking that health care professionals are providing education on cancer during pandemic, 95% CI [1.041, 6.512]. The null hypothesis of the MMI test was rejected ( ), indicating a significant association between gender and source of cancer prevention information. Of males (n = 49), 95.9% ( ) that received cancer prevention information from family and of female respondents ( ), 75% ( ) received cancer prevention information from a family source.
Discussion
The study findings illustrate a lack of education and knowledge surrounding cancers in youth and young adults; the need for gender-based community tailored messaging and interventions; and the perceived impact of COVID-19 on cancer screenings and care. No differences were found between the 2 study samples, indicating that a gender-based community tailored educational program may be feasible for the 2 communities based on their similar characteristics and results. Findings illustrate that the majority of participants know about the most common types of cancer (ie, breast, lung, blood, cervical, skin), common risk factors (ie, unhealthy diet, environmental risks, family history, tobacco use, chronic and unprotected exposure to sun) and how to prevent them. However, their attitudes and practices indicate that although knowledge about common adult cancers is reported, they are less informed about cancers in their age group, and prevention and health-seeking practices are few.
Gender and cancer knowledge were significantly associated across different variables. The overarching indication from this association illustrates that there is a discrepancy in education and cancer knowledge between males and females. Education programs need to focus on addressing the gaps of cancer knowledge, risk factors, and prevention in males and females and ensure they are gender based.
Hearing about cancer warning signals was associated with knowing venues that offer cancer and health screenings, therefore, awareness of cancer risk may drive the individual to seek additional information. Knowing about warning signals was associated with the understanding that chronic conditions like cervical and breast cancers are preventable. In addition, educational programs need to focus on cultural and linguistic proficient messages on other types of cancer warning signals, especially in low resource settings and with communities of color given the limited or lack of adequate access to cancer screenings and care.
Participants’ limited understanding of what cancer is and how it develops reiterates the importance of addressing the social determinants of health, family history, exposure to chemicals and toxics and include other social and environmental risks. Healthy lifestyle practices like access to affordable nutritious food, avoiding use of tobacco, ensuring an active lifestyle, practicing preventive care like screenings, vaccines and human sexuality education were identified as important practices. Educational programs might increase the knowledge of the level of impact these have and can lead to a more accurate self-rating of level of health. Additional research and intervention programs for and with AYAs are needed to reach underserved and marginalized communities to norm cancer education and care.
Internet, social media and health practitioners were identified as trusted sources of cancer facts. This finding is consistent with the way AYAs prefer to get their information and how comfortable they feel interacting with technology. Although health information is readily attainable, seeking cancer screenings and prevention is not. Identifying trusted and user-friendly sources of information is important for reaching these age groups. If it takes anywhere between 3-5 clicks to find information AYAs tend to lose interest. It is important that health professionals that attend to AYAS health needs communicate according to the cognitive development and in the lingo of the culture and the age group. Participants in the 2 locations identified visual prevention messaging and programs in Spanish and English to foster knowledge, address cancer risks and misconceptions.
Gender differences in cancer prevention is consistent with previous research.25,26 In this study, females reported increased awareness of breast cancer, whereas males reported lower levels of cancer prevention practices. The misconception that breast cancer only affects women may be indicative of the finding. Females reported practicing more healthy behaviors to prevent cancer than males in both locations. Engaging males in cancer prevention efforts is important to raise knowledge and health seeking behaviors. The use of digital and social media to learn about cancer across the age groups was cited as valuable. Virtual and digital platforms may increase AYAs health literacy and engagement.
Cancer prevention and education levels were significantly associated. Younger participants with less than high school reported not practicing as much healthy behaviors to prevent cancer. Participants with finished high school or higher reported practicing cancer prevention healthy behaviors. Younger age may be indicative of having limited to no understanding of cancer risks, which may be associated with not perceiving risks or knowing cancer types.
Participants reported that COVID-19 pandemic might have taken priority over cancer education and care in terms of importance, and they saw the pandemic as an emergent issue and believed that professionals needed to focus on COVID-19 more than on cancer education, prevention, or screening.
Limitations
These findings have several limitations. It is not possible to draw causal inferences due to the exploratory nature of the study. The findings, although transferable, cannot be generalized due to the nature of the research. The administration of the questionnaire online does not allow for environmental control. Though all measures were taken to keep anonymity, the study does not go without social desirability bias, which may create a tendency for participants to over-report desirable and under-report undesirable behavior. Due to confidentiality, the research team could not ensure that participants from only the projected locations participated. COVID-19 disrupted the data collection method and researchers transition to an on-line modality, which might have affected the study and its results in ways that cannot be traceable.
Conclusion
Today’s health problems cannot be solved by any discipline or sector alone. The way forward in cancer prevention and care is to enhance interdisciplinary collaboration between the behavioral social and clinical sciences. There are, however, challenges that need to be overcome before true health interdisciplinary approaches to address AYAs health needs can be achieved. The KAP survey is useful to obtain general information about public health knowledge regarding prevention practices and care. The KAP survey model gather cancer information to inform research and plan public health programs for AYAs. Considering the study findings, we conclude that it is necessary to prepare health and human service professionals to launch gender-based programs focused on AYAs cancer and chronic disease prevention to improve knowledge, attitudes and practices. Health practitioners are instrumental in educating, promoting health literacy and screening for risks and promoting protective factors. It is imperative to design culturally and linguistic proficient educational tools for professionals and peer educators to better connect AYAs with accessible and available venues of prevention and care. Organizational policies to ensure affordable health services and care are needed if not in place and engaging AYAs in generating local knowledge and recommendations to promote healthy practices is important if we want to reach vulnerable communities. Documenting barriers and challenges to cancer care is not enough, creating community-based participatory action research experiences where AYAs are co-researchers and they co-lead the design, data collection, and analysis is fundamental to successful health program implementation.
Supplemental Material
Supplemental Material for Analysis of Cancer Knowledge, Attitudes, and Practices in Adolescents and Young Adults in Two Texas Rural Communities by Eva M Moya, Silvia Chávez-Baray, Araceli Garcia and Robert McCreary in INQUIRY
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes on Minority Health Disparities (2U54MD007592).
ORCID iDs
Eva M Moya https://orcid.org/0000-0001-9893-2110
Araceli Garcia https://orcid.org/0000-0002-7767-2118
References
- 1.Adolescents and Young Adults (AYAS) with Cancer. National Cancer Institute. (Accessed September 24, 2020). https://www.cancer.gov/types/aya.
- 2.Adolescents and Young Adults Cancer.. Texas Department of State Health Services. (Accessed April 20, 2021). https://www.dshs.texas.gov/tcr/data/aya.aspx.
- 3.Close AG, Dreyzin A, Miller KD, Seynnaeve BKN, Rapkin LB. Adolescent and young adult oncology-past, present, and future. CA A Cancer J Clin. 2019;69:485-496. doi: 10.3322/caac.21585. [DOI] [PubMed] [Google Scholar]
- 4.Reid J, McKeaveney C, Martin P. Communicating with adolescents and young adults about cancer-associated weight loss. Curr Oncol Rep. 2019;21(15):15. doi: 10.1007/s119-019-0765-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leading causes of death visualization tool. Centers for Disease Control and Prevention. (Accessed February 10, 2022). https://www.cdc.gov/injury/wisqars/LeadingCauses.html.
- 6.Davis HS. Discussion as a bridge: Strategies that engage adolescent and adult learning styles in the postsecondary classroom. J Scholarsh Teach Learn. 2013;13(1):68-76. [Google Scholar]
- 7.Smith AW, Keegan T, Hamilton A, AYA HOPE Collaborative Group , et al. Understanding care and outcomes in adolescents and young adults with cancer: A review of the AYA HOPE study. Pediatr Blood Cancer. 2019;66:e27486. doi: 10.1002/pbc.27486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greenzang KA, Fasciano KM, Block SD, Mack JW. Early information needs of adolescents and young adults about late effects of cancer treatment. Cancer. 2020;126(14):3281-3288. doi: 10.1002/cncr.32932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avutu V, Lynch KA, Barnett ME, et al. Psychosocial needs and preferences for care among adolescent and young adult cancer patients (ages 15-39): A qualitative study. Cancers. 2022;14(3):710. doi: 10.3390/cancers14030710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy-Banks R, Blanch-Hartigan D, Boehm L, Hamel PC, Parsons SK. Personal narrative: Raising awareness of adolescent and young adult cancer survivors in similarly aged university students. J Adolesc Young Adult Oncol. 2019;8(4):434-441. doi: 10.1089/jayao.2018.0131. [DOI] [PubMed] [Google Scholar]
- 11.Linder LA, Hooke MC. Symptoms in children receiving treatment for cancer-part II: Pain, sadness, and symptom clusters. J Pediatr Oncol Nurs. 2019;36(4):262-279. doi: 10.1177/1043454219849578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grace JG, Schweers L, Anazodo A, Freyer DR. Evaluating and providing quality health information for adolescents and young adults with cancer. Pediatr Blood Cancer. 2019;66:e27931. doi: 10.1002/pbc.27931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis JL, Buchanan KL, Katz RV, Green BL. Gender differences in cancer screening beliefs, behaviors, and willingness to participate. Am J Men’s Health. 2011;6(3):211-217. doi: 10.1177/1557988311425853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manierre MJ. Gaps in knowledge: Tracking and explaining gender differences in health information seeking. Soc Sci Med. 2015;128:151-158. doi: 10.1016/j.socscimed.2015.01.28. [DOI] [PubMed] [Google Scholar]
- 15.Pillay M. Knowledge, Attitude and Practices (KAP) Survey. Unpublished Manuscript. Stellenbosch University; 2015. [Google Scholar]
- 16.The World Health Report 2008. World Health Organization. https://www.who.int/whr/2008/en. 2008. [Google Scholar]
- 17.World Health Statistics 2014. World Health Organization. https://www.who.int/mediacentre/news/releases/2014/world-health-statistics-2014/en/. 2014. [Google Scholar]
- 18.Census Data. U.S . Decennial Census 2020. (Accessed March 28, 2022). https://www.census.gov/data.html. [Google Scholar]
- 19.Census Bureau QuickFacts . Socorro City, Texas. United States Census Bureau; 2019. https://www.census.gov/quickfacts/fact/table/socorrocitytexas/PST045219. [Google Scholar]
- 20.Census Bureau QuickFacts . San Elizario City, Texas. United States Census Bureau; 2019. https://www.census.gov/quickfacts/sanelizariocitytexas. [Google Scholar]
- 21.Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. [Google Scholar]
- 22.Agresti A, Liu I-M. Modeling a categorical variable allowing arbitrarily many category choices. Biometrics. 1999;55:936-943. [DOI] [PubMed] [Google Scholar]
- 23.Bilder CR, Loughin TM. Testing for marginal independence between two categorical variables with multiple responses. Biometrics. 2004;60:241-248. doi: 10.111/j.0006-341X.2004.00147.x. [DOI] [PubMed] [Google Scholar]
- 24.Saldaña J. Goodall’s verbal exchange coding. Qual Inq. 2015;22(1):36-39. doi: 10.1177/1077800415603395. [DOI] [Google Scholar]
- 25.Ramirez A, Wildes K, Napoles-Springer A, Perez-Stable E, Talavera G, Rios E. Physician gender differences in general and cancer-specific prevention attitudes and practices. J Cancer Educ. 2009;24:85-93. doi: 10.1080/08858190802664396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Wom Health. 2012;21(2):140-145. doi: 10.1089/jwh.2011.2876. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Analysis of Cancer Knowledge, Attitudes, and Practices in Adolescents and Young Adults in Two Texas Rural Communities by Eva M Moya, Silvia Chávez-Baray, Araceli Garcia and Robert McCreary in INQUIRY