ABSTRACT
Objectives
The effect of body posture on movement of the jaw and head has not yet been clearly established. The relationship between jaw and head movement has implications for conditions such as temporomandibular joint disorders which can be associated with neck pain. The purpose of this quasi-experimental study was to examine the effect of starting posture on three-dimensional movement of the jaw and head, and to examine the relationship between head and jaw movement during mouth opening.
Material and Methods
Fourteen healthy participants performed jaw opening to comfortable and maximal amounts from three starting body postures (neutral, slumped, upright) while three-dimensional movement of the head, jaw, and trunk was tracked. Separate repeated measures analyses of variance analyses examined the effect of posture on jaw and head rotation and translation, and Pearson product moment correlations examined the relationship between jaw opening and head rotation.
Results
Body posture significantly influenced maximal opening but not comfortable opening (P < 0.0033). There was a positive relationship between head extension and maximum opening in an upright posture (r = 0.74, P = 0.006), and head extension and comfortable opening in neutral and upright postures (r = 0.75 to 0.93, P < 0.0033), although there was no relationship between head extension and jaw opening in a slumped posture when opening comfortably.
Conclusions
Posture can affect three-dimensional movement of the jaw when opening. Negating the normal head extension that occurs with mouth opening when in a slumped posture has implications for the development of temporomandibular and neck problems in some individuals.
Keywords: mandible, movement, kinematics, neck, temporomandibular joint, posture
INTRODUCTION
Temporomandibular joint disorder (TMD) is a general term used to describe abnormal function of the stomatognathic system that comprises the mouth and jaw, including the temporomandibular joints (TMJ) and muscles of mastication. It has been estimated that up to 12% of the general population have experienced signs and symptoms of TMD which can have a significant impact on the quality of life in individuals affected [1-4]. The aetiology of TMD is multifactorial, and postural dysfunction has been proposed as one potential contributor to the development or maintenance of TMD symptoms although a direct link between postural changes and TMD has not been found [5]. However, an indirect relationship between posture and TMD may exist since previous work has shown strong relationships between neck disability and jaw disability [6], and between neck pain and posture [7-9].
Alterations in head posture have been associated with changes in resting jaw position [10-13], movement of the mandibular condyle within the TMJ [14], and neuromuscular activity of the muscles of mastication [15-17]. Urbanowicz [18] suggested a physiological model to describe how changing jaw resting posture could affect craniovertebral extension leading to suboccipital compression, which could be a cause of neck pain. It has also been suggested that head posture can alter resting position of the TMJ and initial tooth contact position and vice versa [19-22].
Although the specific effect of body posture on movement of the jaw and head has not yet been established, Goldstein et al. [20] found a decrease in vertical jaw excursion with increasing forward head position. Visscher et al. [14] showed that the trajectory of the jaw shifts anteriorly if the head is held in an erect head posture and posteriorly if the head is forward compared to the movement trajectory from a neutral head posture. What is not clear though is how initial body posture affects the relationship between head/neck and jaw movement and whether this relationship is altered by the amount of mouth opening. Tasks that require wide diameter opening (e.g., during a dental procedure) may contribute to the development of acute jaw pain. A slumped posture has been shown to be associated with higher spinal moment and reaction forces than flat or lordotic postures [23] which may have implications for the development of chronic musculoskeletal pain, including TMD and neck pain.
Understanding how the relationship between head and jaw changes due to body position has interest to all disciplines concerned with TMD. Establishing the relationship between head and jaw movement across different postures may provide insight into the known relationship between neck disability and jaw disability [6] and the elusive role of posture in the aetiology of TMD [5]. The purpose of this quasi-experimental study was to examine the effect of three starting body postures (neutral, upright, and slumped) on the three-dimensional movement (i.e., kinematics) of the jaw and head and to examine the relationship between head and jaw movement during mouth opening. The hypotheses were: 1) jaw opening during both comfortable and maximum opening would be greatest in the upright posture and least in the slumped posture, and 2) regardless of body posture, head extension and jaw opening would be correlated, without deviation or deflection of the jaw on opening.
MATERIAL AND METHODS
Participants
All participants read and signed an informed consent form. The use of human subjects in this study was reviewed and approved by the Institutional Review Board of Midwestern University, United States of America (Protocol No. 2729). Minimal sample size was calculated a priori using G*Power 3.1.9.7 for a repeated measures ANOVA, assuming an effect size of 0.8 at α error probability of 0.05 and yielded a sample size of 14 subjects. The study was conducted in the Physical Therapy Program at Midwestern University, United States, between November 2018 to May 2020. Fourteen healthy subjects (mean age of 23.6 [SD 4.2] years) were enrolled and completed the study protocol. Inclusion criteria were age 21 to 59 years, males and females of good general health, no signs or symptoms of TMD or history of previous TMJ surgery, not currently undergoing orthodontic treatment, dentures, or prosthetic rehabilitation, and no history of headaches > 12 days/year. Screening of each participant prior to testing was performed to rule out symptomatic TMD elements that may have affected jaw mobility including maximal mouth opening range of motion, evaluation of joint noise on opening, observation of opening pattern to ensure symmetry within a 4 mm window, and joint palpation [24]. All participants had a mandibular pain free opening of between 41 to 49 mm, without deviation, joint noise, or pain to joint palpation. Exclusion criteria were a history of painful TMD identified via TMD screening questionnaire [25], a general medical history suggesting unstable general health, significant neurological history, active treatment for cancer, or presence of an infectious disease.
Procedures
Three-dimensional movements of the head, jaw (mandible) and trunk were recorded at 200 Hz using a four-camera Vicon™ system (Bonita cameras - Vicon Motion Systems Ltd.; Vicon, Oxford, UK) and Nexus™ software version 2.0 (Vicon Motion Systems Ltd, Oxford, UK). Data processing and reduction were performed using The MotionMonitor software version 9 (Innovative Sports Training, Chicago, IL). Four reflective pearl markers, measuring 12.7 mm in diameter, were affixed to rigid marker plates each on the jaw, head, and trunk. For the jaw marker set, a full arch mandibular clutch was fashioned from a dental impression. The impression was used to fashion a three-dimensional printed acrylic dental clutch unique to each subject that contacted all mandibular teeth. The purpose of the dental clutch was to ensure that marker movement represented jaw movement by allowing marker fixation via the mandibular teeth to minimize motion artefact associated with external, skin-mounted, markers. Markers were affixed to the head using an adjustable headpiece and to the thorax using a Velcro® strap. Participants were seated on a standard office chair without arms in the middle of the capture volume. A static calibration trial was recorded for each subject using a standardized, neutral, and comfortable sitting resting position to define the segments of jaw, head, and trunk.
Testing order for body posture was randomized and counterbalanced across participants. Participants adopted one of three seated body postures: neutral, slumped, or upright. A neutral posture was defined as the subject’s self-selected resting, comfortable upright position with eyes level, and ear comfortably in line with the acromion. Slumped posture was defined as the upper back rounded with the head forward while maintaining eyes level to the horizontal. Upright posture was defined as the opposite of slumped posture, with the shoulders, head and chin retracted
while keeping the eyes level to the horizontal in an upright position. After assuming the given body posture, subjects were instructed to wait for a “go” tone, then to perform six jaw opening movements in a block, paced to an auditory metronome equivalent to one complete opening movement every 0.5 seconds. Two-minute rests were provided in between movement blocks. Movement blocks were:
Comfortable opening, defined as opening the mouth to a self-selected amount at least halfway to maximum.
Maximum opening, defined as opening the mouth as wide as possible. The order of movement blocks was randomized across subjects.
The time-series segment rotations and translations were exported from The Motion Monitor Software. Data reduction was performed using custom MATLAB version R2019a (The MathWorks Inc.; Natick, Massachusetts, USA) algorithms. Specifically, three-dimensional rotations and translations were calculated for the head (with respect to the lab coordinate system) and jaw (with respect to the head) segments (Table 1). The time series data were smoothed using a fourth order zero lag Butterworth filter with a cut-off frequency of 6 Hz. Velocity of the segment kinematics was then calculated using custom algorithms in MATLAB. Jaw opening, peak opening, and closing were calculated from the velocity traces. Using a backwards (onset) and forward (offset) searches, onset and offset were defined as the times at which segment velocity dropped below 5% of peak velocity. For each trial, the segment kinematics were then time-normalized to 100% of the jaw opening and closing cycle (i.e., from jaw movement onset– jaw movement offset). The custom software automatically plotted the time series data and the identified onset, offset, and peak angle of jaw opening. These dynamic plots allowed the investigator to visually inspect the fidelity of the data and confirm or adjust values as needed. Each subject performed 6 jaw opening and closing trials for each posture. The third, fourth and fifth opening movements were used for data analysis.
Table 1.
Parameter definitions of the axis system for the jaw and head
| Axis |
Rotation (degrees) |
Positive angle |
Translation (mm) |
Positive translation | |
|---|---|---|---|---|---|
| Jaw | x | Tilt | Axial rotation left (chin tilts to left) | Anterior-posterior | Anterior translation mandible |
|
| |||||
| y | Opening/closing | Sagittal rotation (mouth opening) | Superior-inferior | Superior translation mandible | |
|
| |||||
| z | Lateral deviation | Coronal rotation left (chin moves to left) | Left-right | Left deviation mandible | |
|
| |||||
| Head | x | Lateral flexion | Axial rotation left (head tilts to left) | Anterior-posterior | Forward head |
|
| |||||
| y | Flexion/extension | Sagittal rotation (head/neck flexion) | Left-right | Head translation left | |
|
| |||||
| z | Rotation | Coronal rotation left (head rotates to left) | Superior-inferior | Superior translation head | |
Statistical analysis
Three-dimensional peak jaw and head rotation and translation in the three cardinal planes of movement were the dependent variables. Table 1 shows how each axis of motion was defined and the movement associated with it. To evaluate the effect of starting body posture on head and jaw movement, separate repeated measures analyses of variance analyses examined the effect of posture on each of the dependent variables during both comfortable and maximal mouth opening. A Bonferroni corrected alpha level of 0.0033 was used to determine statistical significance. Significant main effects of posture were followed-up using Tukey’s post hoc testing.
To evaluate the relationships between jaw opening and head rotation, Pearson product moment correlations were calculated. Correlation coefficients were interpreted as 0 to 0.25 - little or no relationship, 0.25 to 0.5 - fair relationship, 0.51 to 0.75 - moderate to good relationship, < 0.75 - good to excellent relationship [26]. IBM® SPSS® Statistics version 25.0 (Armonk; New York, USA) was used for all statistical analyses.
RESULTS
Effect of starting body posture on jaw opening
Figure 1 shows jaw rotation for each of the primary movement directions for a single representative movement trial from a subject completing maximal opening (left panels) and comfortable opening (right panels). One movement trial from each of the three starting postures is shown. Inspection of Figure 1 shows that, as expected, rotation was the primary motion during opening, with very little jaw tilt or deviation during opening.
Figure 1.
Time normalized data of one trial from a representative subject showing jaw rotation around each axis for each of the three starting postures (neutral posture, solid black line; upright posture, grey dashed line, slumped posture, black dash line) during maximal opening (left panels) and comfortable opening (right panels).
A = maximal opening rotation; B = comfortable opening rotation; C = maximal opening tilt; D = comfortable opening tilt; E = maximal opening lateral deviation; F = comfortable opening lateral deviation.
Across subjects, opening to a maximal amount was significantly affected by starting posture (Table 2, Figure 2A). Post-hoc comparisons showed that maximal opening was the most when opening in a neutral posture compared to opening in either an upright or a slumped posture. Opening was the least when opening in a slumped posture. In contrast to opening maximally, starting posture did not significantly affect jaw opening when opening to a comfortable amount (Table 2, Figure 2C). Starting posture did not significantly affect either jaw tilt or deviation during either opening (Table 2). There was a significant increase in forward jaw translation when opening in an upright posture compared to opening in either a neutral or slumped posture.
Table 2.
Repeated measures ANOVA results examining the effect of posture on jaw rotation and translation around x, y and z axes during maximal and comfortable opening
| Maximum opening | Comfortable opening | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| F | P | Post hoc | F | P | Post hoc | |
| Peak tilt | 0.55 | 0.587 | N/A | 1.7 | 0.217 | N/A |
|
| ||||||
| Peak opening | 4.77 | 0.001a | N > U > S | 1.59 | 0.232 | N/A |
|
| ||||||
| Peak lateral deviation | 0.53 | 0.486 | N/A | 0.09 | 0.815 | N/A |
|
| ||||||
| Peak anterior translation | 3.38 | 0.052 | N/A | 8.59 | 0.002a | U > N, U > S |
|
| ||||||
| Peak lateral translation | 0.93 | 0.390 | N/A | 0.32 | 0.629 | N/A |
|
| ||||||
| Peak inferior translation | 66.55 | < 0.0001a | U > N, N > S, U > S | 67.88 | < 0.0001a | U > N, N > S, U > S |
aSignificant ANOVA results at the corrected alpha level of P = 0.0033.
N/A = not applicable; N = neutral posture; U = upright posture; S = slumped posture; F = statistic from ANOVA; P = P-value from ANOVA.
Figure 2.
Mean (SEM) of the absolute value of peak jaw opening (A) and peak head extension (B) during maximal opening, and peak jaw opening (C) and peak head extension (D) during comfortable opening.
Taken together these results show that changing from a neutral posture to an upright or a slumped posture reduced the amount of maximal opening but not comfortable opening, and that changes in starting posture affected only jaw rotation and not jaw tilt or deviation during opening.
Effect of starting posture on head rotation and translation
Regardless of starting posture, the head always moved into a posteriorly rotated or extended position during mouth opening. Changing the starting posture did not significantly change the amount of extension when opening maximally (Table 3, Figure 2B) or comfortably (Table 3, Figure 2D). The average amount of head extension during maximal opening was 7.9° (SD 1.2°) although there was considerable range in the amount of extension across all subjects (1.1° to 22.2°). To illustrate this variability, movement trials during maximal opening from two subjects are shown in Figure 3. The subject in Figure 3A shows a smaller amount of head extension with maximal opening compared to the subject in Figure 3B. In contrast to variability in the amount of extension when opening maximally, the average amount of extension during comfortable opening was lower at 3.2° (SD 0.59°) with a more consistent range across all subjects (2.7° to 3.6°).
Table 3.
Repeated measures ANOVA results examining the effect of posture on head rotation and translation around x, y and z axes, during maximal and comfortable opening
| Maximum opening | Comfortable opening | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| F | P | Post hoc | F | P | Post hoc | |
| Peak head lateral flexion | 0.29 | 0.754 | N/A | 1.1 | 0.335 | N/A |
|
| ||||||
| Peak head flexion/extension | 1.91 | 0.171 | N/A | 0.11 | 0.865 | N/A |
|
| ||||||
| Peak head rotation | 1.97 | 0.017 | N/A | 0.97 | 0.377 | N/A |
|
| ||||||
| Peak head translation anterior/posterior | 1.42 | 0.263 | N/A | 1.97 | 0.016 | N/A |
|
| ||||||
| Peak head translation left/right | 1.4 | 0.267 | N/A | 0.68 | 0.467 | N/A |
|
| ||||||
| Peak head translation superior/inferior | 15.17 | 0.001a | N > S, U > S | 10.62 | 0.003a | N > S, U > S |
aSignificant ANOVA results at the corrected alpha level of P = 0.0033.
N/A = not applicable; N = neutral posture, U = upright posture, S = slumped posture; F = F statistic from ANOVA; P = P-value from ANOVA.
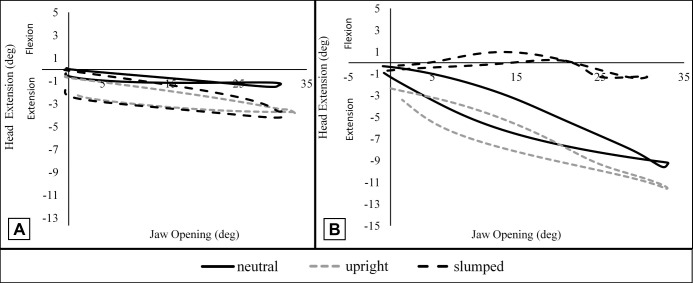
Figure 3.
Phase plots from two subjects showing different amounts of associated mandibular rotation and head rotation during maximal opening from each of the three starting postures (neutral posture, solid black line; upright posture, grey dashed line, slump posture, black dash line).
A = one participant; B = a second participant.
When opening maximally there was a significant moderate to good correlation between head extension and opening when in an upright posture (r = 0.74, P = 0.006) but not when opening in either a neutral posture (r = 0.51, P = 0.089) or a slumped posture (r = 0.16, P = 0.429). When opening comfortably, there was a significant moderate to good correlation between the amount of extension and the amount of opening in a neutral posture (r = 0.75, P = 0.005), and a significant good to excellent correlation in an upright posture (r = 0.93, P ≤ 001).
There was no significant correlation between the amount of extension and the amount of opening when opening comfortably in a slumped posture (r = 0.37, P = 0.242).
Taken together these results show that while opening the mouth was always associated with extension of the head, changing the starting posture did not lead to significantly more or less head extension during opening regardless of the amount of opening. However, the range of head extension across subjects when opening maximally was quite large. A slumped posture removed the positive relationship between head extension and opening.
DISCUSSION
The purpose of this study was to examine the effect of starting posture on movement of the jaw and head, and to examine the relationship between head and jaw movement during mouth opening. There are three novel findings. First, starting body posture significantly influenced the amount of opening but only when opening to a maximal amount, with least opening when in a slumped posture and greatest when in a neutral posture. Second, an upright posture uniquely influenced translation of the jaw forward during comfortable opening. Third, significant correlations were present between head extension and maximum opening in an upright posture, and head extension and comfortable opening in neutral and upright postures. A slumped posture negated the relationship between head extension and mouth opening. Taken together, these findings highlight an important relationship between the biomechanics of jaw opening and head extension for neutral and upright postures that is removed when a slumped posture is assumed. These findings have potential implications for understanding the effect of posture and movement in TMD, as well as on understanding jaw contributions to neck dysfunction.
Adopting a slumped sitting posture has previously been shown to be associated with increased head and neck flexion, forward head translation (i.e. forward head posture), and increased cervical extensor muscle activity compared to other sitting postures [27]. Posture has also been shown to affect resting position of the jaw [20]. Goldstein [20] hypothesized that a forward head position could lead to increased upward forces on the jaw, in part facilitated by the head extension associated with a forward head position. However, the specific influence of body posture on the relationship between jaw and head movement has not been extensively studied. Previous work which tracked the lower incisal point found that the opening movement path of the jaw shifted anteriorly in an upright posture relative to its path in a neutral head posture, and shifted posteriorly in a forward head posture with maximum opening [14]. The current study tracked movement of the jaw using a marker cluster affixed to the mandibular teeth rather than tracking a singular incisal point and showed that vertical translation of the jaw during either opening was greatest in an upright posture and least in a slumped posture. This difference in findings may be explained by the method of tracking, or by differences in subject instructions. Visscher et al. [14] constrained head posture during opening by using visual feedback. In the current study, subjects adopted a starting posture and performed opening while instructed to maintain the position but without visual constraint. As such, more head movement would be expected in the current study. Anecdotally, this is consistent with what is observed clinically: mouth opening is reduced when in a slumped posture and facilitated while in an upright posture. In addition, the results of the current study support that the amount of mouth opening can affect whether posture changes jaw movement. Specifically, opening maximally in a slumped posture reduces jaw rotation while opening in a neutral posture maximizes jaw rotation. This has potential implications for the development of neck pain in some individuals with TMD who may have postural issues. Based on the current results, we hypothesize those individuals who show a habitual slumped posture would have less condylar rotation available during wide mouth opening and thus may extend the head more, straining the sub-occipital and cervical spine tissues potentially leading the development of neck pain. This is an avenue that should be explored in individuals with neck pain and TMD.
The opposite posture to a slumped posture is an upright or so called “military” posture. In the current study, adopting an upright posture uniquely influenced jaw movement by producing jaw tilt when opening comfortably and jaw deviation when opening either comfortably or maximally. Changes in jaw tilt or deviation during opening is consistent with an asymmetry in motion between the left and right TMJs, but why this would be specific to an upright posture is unclear. An upright posture is produced by chin retraction and anterior rotation of the occiput with associated posterior translation of the occipital condyles on the upper cervical spine vertebra. Speculatively, any asymmetry in occipital condylar glide, which is not uncommon in symptom free individuals, may necessitate an increased jaw tilt or glide in compensation during mouth opening. This should be examined further since it would have implications for individuals with jaw dysfunction who have been shown to have comorbid cervical dysfunction [5,28].
Mouth opening is produced by a combination of rotation and translation of the mandibular condyles to produce increased space between the incisors that is functionally necessary to pass food into the mouth. Abnormal motion, either excessive or limited translation or rotation, can have significant functional consequences, producing either excessive or limited mouth opening, and introducing deviation into the path of opening when differences occur between left and right TMJs. This can modify forces on associated soft tissue structures such as the TMJ capsule, ligaments, and masticatory muscles, and potentially lead to pain. Taken together, the functional implications of findings in the current study are that body posture may have a greater impact on TMJ function during wide diameter opening activities such as yawning, opening to eat a large bite of food, or during dental treatment compared to when opening to a lesser amount. Anecdotally, these are the functional activities that individuals with TMD report significant difficulty performing due to pain. Further investigation is required to examine if individuals who show a slumped resting posture tolerate wide diameter opening activities less than individuals who do not have a slumped posture. It is possible that there is not a definitive link between posture and TMD onset, but rather a contribution of posture to TMD onset through the combination of posture and wide diameter opening activities, which should be further explored.
While body posture affected jaw movement in the current study, it did not affect the amount of head extension regardless of the amount of opening. Therefore, a slumped posture by itself did not uniquely affect head extension during mouth opening. Mouth opening itself may be facilitated by head extension since head extension increases suprahyoid muscle length and working angle to produce an improved lever function for drawing the mandible down during mouth opening [29]. Head extension in healthy individuals is accomplished by a combination of rotation and translation of the occipital condyles on the upper cervical vertebra [30,31]. A strong relationship between neck disability and jaw disability has previously been found in individuals with TMD [6] and patients with TMD have reported worse self-reported neck disability compared to individuals without TMD [28], with neck pain considered as one possible contributor to the development of TMD [32-36]. Results of the current study in healthy individuals show that the head extends on average about 8 degrees during mouth opening, although there is a large variation in the amount of extension across subjects particularly when opening wide. Establishing whether the relationship between mouth opening and head extension is intact in individuals with TMD, and if the relationship changes depending on the sub-type of TMD could shed light on how neck pain and TMD may be related and if this relationship is consistent across all sub-types of TMD.
Limitations in this study include the use of young healthy subjects that limits generalizability of findings to older adults, and the lack of diagnostic imaging to rule out structural changes in the temporomandibular joints of participants which, although symptomless, could have an impact on three-dimensional jaw motion. In addition, an adopted body posture is a temporary posture compared to a naturally occurring body posture which would be expected to be associated with joint and soft tissue changes that could affect jaw and head kinematics thus limiting generalizability of finings to individuals with non-typical postures.
CONCLUSIONS
Posture can affect the three-dimensional movement of the jaw during opening which is seen most clearly in the slumped posture as reduced maximal mouth opening. While mouth opening and head extension are linked, there is variability in the amount of head extension when opening wide and the relationship between head extension and mouth opening is negated when opening in a slumped posture. This has implications for the association of neck dysfunction, posture, and temporomandibular joint disorder which should be explored further. Future work should explore how the relationship of head and jaw motion is affected in conditions such as temporomandibular joint disorder that have previously shown a link with neck dysfunction.
Acknowledgments
ACKNOWLEDGMENTS AND DISCLOSURE STATEMENTS
The authors report no conflicts of interest related to this study.
REFERENCES
- 1.Nassif NJ, Al-Salleeh F, Al-Admawi M. The prevalence and treatment needs of symptoms and signs of temporomandibular disorders among young adult males. J Oral Rehabil. 2003 Sep;30(9):944-50. [DOI] [PubMed]
- 2.Rugh JD, Solberg WK. Oral health status in the United States: temporomandibular disorders. J Dent Educ. 1985 Jun;49(6):398-406. [DOI] [PubMed]
- 3.Dworkin SF, Huggins KH, LeResche L, Von Korff M, Howard J, Truelove E, Sommers E. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. J Am Dent Assoc. 1990 Mar;120(3): 273-81. [DOI] [PubMed]
- 4.Von Korff M, Dworkin SF, Le Resche L, Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988 Feb;32(2):173-183. [DOI] [PubMed]
- 5.Armijo-Olivo S, Rappoport K, Fuentes J, Gadotti IC, Major PW, Warren S, Thie NM, Magee DJ. Head and cervical posture in patients with temporomandibular disorders. J Orofac Pain. 2011 Summer;25(3):199-209. [PubMed]
- 6.Armijo-Olivo S, Magee D. Cervical musculoskeletal impairments and temporomandibular disorders. J Oral Maxillofac Res. 2013 Jan 1;3(4):e4. [DOI] [PMC free article] [PubMed]
- 7.Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. 2014 Jul-Aug;18(4):364-71. [DOI] [PMC free article] [PubMed]
- 8.Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. 2009 Apr;90(4):669-74. [DOI] [PubMed]
- 9.Chiu TT, Ku WY, Lee MH, Sum WK, Wan MP, Wong CY, Yuen CK. A study on the prevalence of and risk factors for neck pain among university academic staff in Hong Kong. J Occup Rehabil. 2002 Jun;12(2):77-91. [DOI] [PubMed]
- 10.Solow B, Tallgren A. Head posture and craniofacial morphology. Am J Phys Anthropol. 1976 May;44(3):417-35. [DOI] [PubMed]
- 11.Gonzalez HE, Manns A. Forward head posture: its structural and functional influence on the stomatognathic system, a conceptual study. Cranio. 1996 Jan;14(1):71-80. [DOI] [PubMed]
- 12.McLean LF, Brenman HS, Friedman MG. Effects of changing body position on dental occlusion. J Dent Res. 1973 Sep-Oct;52(5):1041-5. [DOI] [PubMed]
- 13.Moya H, Miralles R, Zuñiga C, Carvajal R, Rocabado M, Santander H. Influence of stabilization occlusal splint on craniocervical relationships. Part I: Cephalometric analysis. Cranio. 1994 Jan;12(1):47-51. [DOI] [PubMed]
- 14.Visscher CM, Huddleston Slater JJ, Lobbezoo F, Naeije M. Kinematics of the human mandible for different head postures. J Oral Rehabil. 2000 Apr;27(4):299-305. [DOI] [PubMed]
- 15.Boyd CH, Slagle WF, Boyd CM, Bryant RW, Wiygul JP. The effect of head position on electromyographic evaluations of representative mandibular positioning muscle groups. Cranio. 1987 Jan;5(1):50-4. [DOI] [PubMed]
- 16.Yotsuya M, Sato T, Kawamura S, Furuya E, Saito F, Hisanaga R, Onodera K. Electromyographic response in inferior head of human lateral pterygoid muscle to anteroposterior postural change during opening and closing of mouth. Bull Tokyo Dent Coll. 2009;50(4):191-8. [DOI] [PubMed]
- 17.Funakoshi M, Fujita N, Takehana S. Relations between occlusal interference and jaw muscle activities in response to changes in head position. J Dent Res. 1976 Jul-Aug;55(4):684-90. [DOI] [PubMed]
- 18.Urbanowicz M. Alteration of vertical dimension and its effect on head and neck posture. Cranio. 1991 Apr;9(2):174-9. [DOI] [PubMed]
- 19.Makofsky H. The effect of head posture on muscle contact position: the sliding cranium theory. Cranio. 1989 Oct;7(4): 286-92. [DOI] [PubMed]
- 20.Goldstein DF, Kraus SL, Williams WB, Glasheen-Wray M. Influence of cervical posture on mandibular movement. J Prosthet Dent. 1984 Sep;52(3):421-6. [DOI] [PubMed]
- 21.Mohl ND. Head posture and its role in occlusion. N Y State Dent J. 1976 Jan;42(1):17-23. [PubMed]
- 22.Huggare JA, Raustia AM. Head posture and cervicovertebral and craniofacial morphology in patients with craniomandibular dysfunction. Cranio. 1992 Jul;10(3):173-7; discussion 178-9. [DOI] [PubMed]
- 23.Kwon Y, Kim JW, Heo JH, Jeon HM, Choi EB, Eom GM. The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technol Health Care. 2018;26(S1):409-418. [DOI] [PMC free article] [PubMed]
- 24.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Jensen R, John MT, De Laat A, de Leeuw R, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014 Winter;28(1):6-27. [DOI] [PMC free article] [PubMed]
- 25.Gonzalez YM, Schiffman E, Gordon SM, Seago B, Truelove EL, Slade G, Ohrbach R. Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc. 2011 Oct;142(10):1183-91. [DOI] [PMC free article] [PubMed]
- 26.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. New Jersey: Pearson Education Inc.; 2008. p. 892-3.
- 27.Caneiro JP, O'Sullivan P, Burnett A, Barach A, O'Neil D, Tveit O, Olafsdottir K. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. 2010 Feb;15(1):54-60. [DOI] [PubMed]
- 28.de Oliveira-Souza AIS, de O Ferro JK, Barros MMMB, Oliveira DA. Cervical musculoskeletal disorders in patients with temporomandibular dysfunction: A systematic review and meta-analysis. J Bodyw Mov Ther. 2020 Oct;24(4): 84-101. [DOI] [PubMed]
- 29.Winnberg A, Pancherz H, Westesson PL. Head posture and hyo-mandibular function in man. A synchronized electromyographic and videofluorographic study of the open-close-clench cycle. Am J Orthod Dentofacial Orthop. 1988 Nov;94(5):393-404. [DOI] [PubMed]
- 30.Ferrario VF, Sforza C, Poggio CE, Schmitz JH, Tartaglia G. A three-dimensional non-invasive study of head flexion and extension in young non-patient subjects. J Oral Rehabil. 1997 May;24(5):361-8. [DOI] [PubMed]
- 31.Levangie PK, Norkin CC. Joint structure and function: a comprehensive analysis. 5th ed. Philadelphia: F.A. Davis Company; 2011.
- 32.Komiyama O, Arai M, Kawara M, Kobayashi K, De Laat A. Pain patterns and mandibular dysfunction following experimental trapezius muscle pain. J Orofac Pain. 2005 Spring;19(2):119-26. [PubMed]
- 33.Hu JW, Yu XM, Vernon H, Sessle BJ. Excitatory effects on neck and jaw muscle activity of inflammatory irritant applied to cervical paraspinal tissues. Pain. 1993 Nov;55(2):243-250. [DOI] [PubMed]
- 34.Carlson CR, Okeson JP, Falace DA, Nitz AJ, Lindroth JE. Reduction of pain and EMG activity in the masseter region by trapezius trigger point injection. Pain. 1993 Dec;55(3):397-400. [DOI] [PubMed]
- 35.Cornelison LE, Hawkins JL, Durham PL. Elevated levels of calcitonin gene-related peptide in upper spinal cord promotes sensitization of primary trigeminal nociceptive neurons. Neuroscience. 2016 Dec 17;339:491-501. [DOI] [PMC free article] [PubMed]
- 36.La Touche R, Fernández-de-las-Peñas C, Fernández-Carnero J, Escalante K, Angulo-Díaz-Parreño S, Paris-Alemany A, Cleland JA. The effects of manual therapy and exercise directed at the cervical spine on pain and pressure pain sensitivity in patients with myofascial temporomandibular disorders. J Oral Rehabil. 2009 Sep;36(9):644-52. [DOI] [PubMed]