Abstract
Monteggia fracture is characterized by radial head dislocation combined with proximal ulnar fracture.
If not diagnosed at an early stage, these lesions can gradually lead to forearm deformities and dysfunction, finally resulting in neglected Monteggia fracture. When the radial head is not reduced, several deformities develop at the humeroradial joint, including cubitus valgus and osteoarthritis.
Adequate radiographs are crucial when the surgeons deal with forearm injuries.
At present, proximal ulnar osteotomy and open reduction of chronic radial head dislocation provides satisfactory functional outcomes because of anatomic alignment reconstruction.
Supplementary procedures, including transcapitellar pinning and repair or reconstruction of the annular ligament, which are performed in order to enhance stability of the humeroradial joint, should be thoroughly assessed based on joint rotational stability after reduction and on potential complications.
Keywords: Monteggia fracture, neglected, biomechanics, diagnosis, treatment, complication
Introduction
Monteggia fracture, characterized by proximal 1/3 ulnar shaft fracture combined with radial head dislocation, was first described by Monteggia et al. in 1814, while recent studies included fracture of the olecranon (1, 2, 3, 4, 5, 6). With an incidence of less than 2% of forearm injuries in children and adults, this rare combination injury could eventually lead to forearm deformities and dysfunction if not diagnosed at an early stage, resulting in neglected Monteggia fracture (NMF) (1, 4, 7, 8).
Plenty of researchers have reported managements of NMF with different outcomes in recent years (9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49). This review aims at summarizing and discussing the current knowledge of NMF, including its definition, its pathophysiological characteristics, the biomechanics of which the radial head slips, and surgical intervention.
Definition, causes, classification, and biomechanics of NMF
Definition
Though Monteggia fracture is well defined as radial head dislocation combined with proximal ulna fracture, the exact time point to consider a chronic phase Monteggia fracture is ambiguous. Recent studies recommended over 4 weeks after injury as the dividing line for NMF, as malunion of the ulna had already formed (1, 2, 3, 6, 8, 11, 50).
Causes
A rate of misdiagnosis of up to 28% makes the recognition of Monteggia fracture challenging, especially in pediatric patients (3, 6, 8). Chin et al. (33) proposed several possible causes that could make acute pediatric Monteggia fracture a neglected one. (1) Ossification centers of the elbow emerge sequentially, which hinders the recognition of the alignment of radiocapitellar joint. Also, atypical greenstick fracture of the ulna is difficult to discover. (2) Children are noncompliant during physical and radiological examination, resulting in poor recognition both in the emergency room and on film. (3) Surgeons pay too much attention on the reduction and fixation of the ulnar fracture without inspecting the proper alignment of the radiocapitellar joint. Hence, thorough and precise examination should be carried out when the patient injured his or her forearm, and a comparison to the contralateral is required if necessary (4, 51).
Classification and biomechanics of Monteggia injury
Bado classification was once the most widely utilized classification for Monteggia fracture, whose occurrence is shown in Table 1 (52, 53). However, the injury of the proximal radioulnar joint (PRUJ) is ignored under this classification system, which leads to limited prognostic prediction (1, 3, 31, 35, 54). Thus, subsets of the Monteggia fracture were reestablished as follows: (I) diaphyseal fracture of ulna with anterior angulation, and anterolateral dislocation of the radial head without dislocation of the PRUJ. This subset is most common in children. The biomechanics of this subset of Monteggia fracture is that a direct blow to the posterior ulna, or extreme pronation of the forearm or over-extension of the elbow during the fall induces contract of biceps muscle and consequent fracture and dislocation. (II) Metaphyseal fracture of ulna with posterior angulation, and posterior dislocation of the radial head without dislocation of the PRUJ. Longitudinal force during elbow flexion may be the cause of this subset, similar to the mechanism of posterior dislocaiton of the elbow, though the humeroulnar ligament is often intact. (IIIa) Apex posterior fracture of ulna, and posterior dislocation of the radial head without dislocation of the PRUJ; (IIIb) apex posterior fracture of ulna and posterior dislocation of the radial head with dislocation of the PRUJ. Subset III is mainly due to a strike from the medial aspect of the elbow. (IV) Concomitant fracture of the radius with dislocation of the radial head in any direction, with or without dislocation of the PRUJ. The biomechanics of this subset is similar to subset I, while the radial fracture could be a secondary injury (50, 52, 55). Another alternative classification system was proposed by Letts et al. (56, 57) which accommodates the unique features of pediatric Monteggia lesions.
Table 1.
Bado classification of Monteggia fractures and characteristics.
| Type | Radial head dislocation | Ulnar fracture | Pediatric proportion (%) | Reference |
|---|---|---|---|---|
| Bado I | Anterior | Anterior angulation | 70 | (7) |
| Bado II | Posterior/posterolateral | Posterior angulation | 6 | (8) |
| Bado III | Lateral/anterolateral | Metaphyseal fracture | 23 | (8) |
| Bado IV | Anterior | Concomitant radial fracture | 1 | (8) |
Pathophysiological characteristics
Typical pathological changes of NMF include malunion and angulation of the ulna, refractory dislocation of the radial head, and soft tissue injury (1, 2, 3, 33, 39, 43, 58, 59, 60, 61). With the radial head unreduced, the capitellar facet becomes atrophic and flattened, and the radial head loses its crateriform facet due to its growth without the limitation of the humeral facet. Dislocated PRUJ also results in the degeneration of the radial notch, which could block the reduction of the radial head (3, 27, 55, 56, 62). As a result, the unmatched humeroradial joint becomes painful and may eventually develop osteoarthritis (1, 3, 4, 8, 60).
Normally, the annular ligament ensures the stability of the radiocapitellar joint by surrounding the radial head. This ligament may get torn or entrapped by the dislocation of the radial head due to acute Monteggia fracture (9, 13, 15, 18, 36, 44, 59, 63). Then, the elbow joint may undergo scar tissue proliferation and contracture and ossification, which creates ectopic calcification if not well restored (60). Both the torn annular ligament and the deformed radius decrease the stability of the lateral elbow joint, inducing the deterioration of cubitus valgus. With soft tissue, including vessels and peripheral nerves, stretched or entrapped during this process, forearm motor dysfunction may be combined with paresthesia (3, 4, 61, 64, 65). In pediatric patients, early-developed ossification centers were observed at the injured radial epiphysis, indicating that the trauma stimulated bone growth (60, 62). Forearm interosseous membrane also contributes to the rotational stability of the radial head, whose integrity should be checked during surgical managements of NMF (58, 65).
Diagnosis and differential diagnosis
Manifestations
Unlike an acute fracture, the main symptoms of NMF are usually an antebrachial osseous protuberance and a prolonged history of trauma, rather than pain in the elbow joint, as the fracture has already healed (1, 2, 3, 4, 5, 6, 8, 50, 66).
During physical examination, an abnormal osseous protuberance is usually seen or felt in the forearm. Along with various degrees of cubitus valgus, the rotation of forearm and the flexion of elbow are often limited due to instability of the radialcapitellar joint (1, 2, 3, 4, 5, 6, 8, 50, 66).
Other manifestations, including peripheral nerve impairment, sometimes develop as the aftermath of a delayed diagnosis or improper treatments of Monteggia fracture. Thus, it is essential to carry out a detailed neurovascular examination for all patients (61, 64).
Radiography
The radiological diagnosis of NMF focuses on recognizing the angulation deformity of the ulna, the dislocation of the radial head, and rupture of the ligaments.
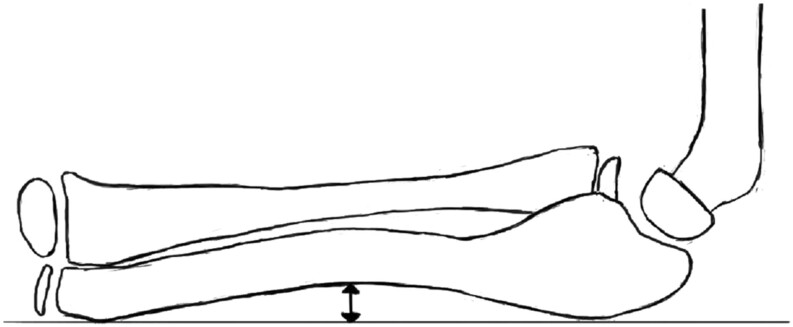
The ulnar fracture in NMF is already healed, while shortening and angulation of the ulna usually exist. Lincoln et al. (67) described the ulnar bow sign as the radiographic parameter for the angulated ulna (Fig. 1). A dorsal line is drawn from olecranon to the distal edge of the ulna on a lateral view, and any point on the ulnar shaft surpassing this line for over 1 mm indicates a significant curvature in the ulna, which also indicates a dislocated radial head.
Figure 1.
The ulnar bow sign. A dorsal line is drawn from olecranon to the distal edge of the ulna on a lateral view, and any point on the ulnar shaft surpassing this line for over 1 mm indicates a curvature in the ulna.
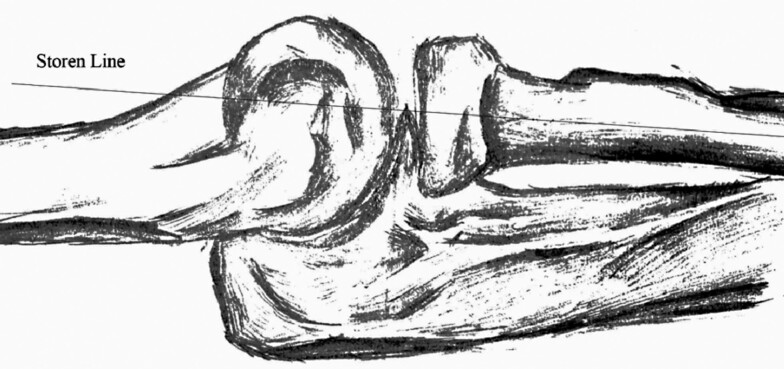
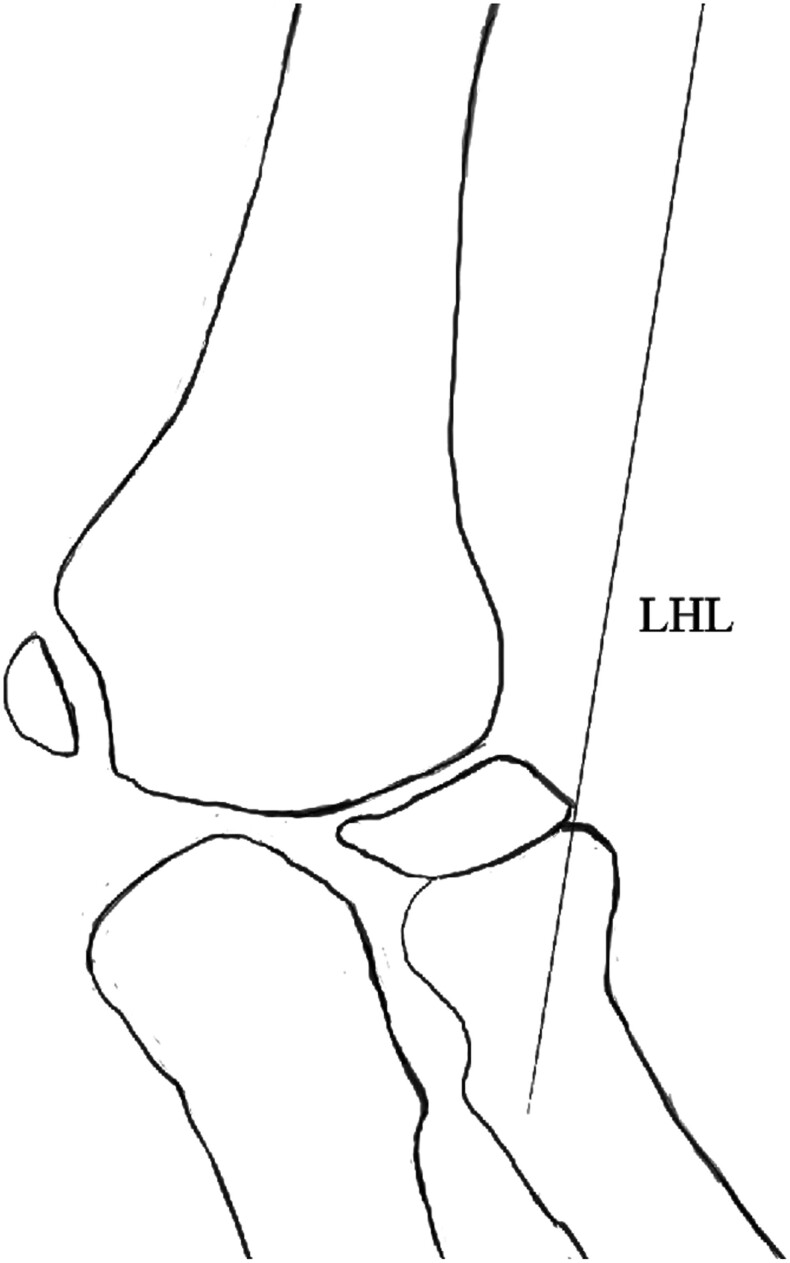
Several approaches have been reported to detect the displaced radial head, among which the method of Storen line (68) is the most widely used (Fig. 2). The axis of a normal radius travels through the center of humeral capitellum. When Storen line misses the center of capitellum, the radial head is considered dislocated. However, Ramirez et al. (69) found this line was more likely to target the middle of capitellum while missing the capitellar ossification center in 16% of the healthy elbows, which was more common before the age of 5 years. In addition to the Storen line, the lateral humeral line (LHL) is one of the most reliable parameters for lateral radial head luxation (66) (Fig. 3). The LHL is drawn along the lateral margin of humeral lateral condyle and is parallel to the axis of distal humeral shaft on an antero-posterior view. Under normal circumstances, the LHL shall be parallel to the radial neck cortex simultaneously. However, in the case of dislocation of radial head, both Storen line and LHL can lose their references.
Figure 2.
The Storen line. The axis of a normal radius travels through the center of humeral capitellum, especially on a lateral view.
Figure 3.
The LHL is drawn along the lateral margin of humeral lateral condyle and is parallel to the axis of distal humeral shaft on an antero-posterior view. Under normal circumstances, the LHL shall be parallel to the radial neck cortex simultaneously. However, in the case of dislocation of radial head, both Storen line and LHL can lose their references.
Three-dimensional reconstruction based on CT can serve as a supplement to the visualization of the deformities in the elbow and forearm (3, 21, 55, 62). MRI has been used to assess the severity of the injury of the annular ligament and to exclude the congenital dislocation of the radial head (1, 50, 70).
Differential diagnosis
Congenital dislocation of the radial head can be identified through the criteria established by Roles (71). This lesion usually occurs bilaterally. Two-thirds of the cases experience a posterior dislocation of the radial head and an anterior angulation of the ulna. The representative shrink of the radial head differs from the hypertrophy observed in NMF radial head. Cleary and Omer type II to IV congenital proximal radioulnar synostosis (CRUS) represents different directions of radial head dislocation and shapes. CRUS is often first observed in the age of 2–5 as fluoroscopic examination concludes chondral or bony fusion at PRUJ, which extrudes the radial head from the humororadial joint (70).
According to the ulnar tether hypothesis, pediatric patients with forearm multiple hereditary exostoses may eventually develop radial head dislocation. When the radius is lengthened and bent, the exostoses supresses the growth of ulnar. The enhanced tension then stretches the radial head out of the annular ligament (72).
Other acute and chronic elbow and forearm injury, for example, Essex-Lopresti injury, should also be excluded according to manifestations and radiological results (73).
Treatment and complications
Since expectant treatment of NMF often results in poor outcomes, early surgical intervention is well recommended to decrease complications (5, 8, 17, 22, 23, 54, 63, 74). Surgical treatment aims at correcting the angular deformity of the ulnar, stably reducing the radial head and restoring the proper alignment of the radiocapitellar joint (1, 2, 3, 15, 19, 20, 32, 40, 41, 42). Though numerous studies have reported different treatments of NMF, which vary from position to perform osteotomy, options for fixation, and the reconstruction of the annular ligament, there still remains no standard protocol or guidelines (9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49). Besides, onset of the chronic deformities is often recognized within childhood, which leads to few reports of adult NMF cases (28, 37, 43).
Forearm osteotomy
It is undisputed that forearm osteotomy should be performed to correct bony malunion of the ulna, as the angulation deformity is the direct reason for blocking the radial head from reduction (14, 15, 16, 17, 19, 21, 34, 38, 44, 47, 48, 49, 62, 75). Ulnar osteotomy and lengthening have been found useful to create intrinsic tension in the interosseous membrane to maintain the reduction of the radial head (1, 2, 40). Bouyala technique, which contains elbow joint clear operation, proximal ulna shaft osteotomy, and correction-over-correction of the angulation deformity of the ulna for radial head reduction through Boyd’s posterior approach or Kocher’s approach and sometimes combined with Henry’s anterior approach, was once universally approved treatment for NMF (2, 15, 17, 23, 24, 29, 39, 48). This technique was also successful in treating adult NMF patients and long-term outcomes were satisfactory (43). However, early recurrence of dislocation was observed within Bado III NMF patients, and severe instability of the radial head in Bado IV NMF may sometimes need additional radial osteotomy for its reduction (19, 34, 42, 43, 55, 62, 75). Recent studies have also confirmed that overcorrection of the ulna might result in consequent postoperative posterior dislocation of the radial head (14). Though radial head resection could improve forearm rotation in NMF, long-term study showed that this would result in instability of the elbow and arthralgia (14, 22, 37). Taking satisfactory outcomes from adult patients with congenital proximal radioulnar synostosis who received radial head resection into consideration, adult patients with NMF may benefit from radial head resection when bony fusion of proximal radioulnar joint develops (70).
Park et al. (19) noted that the location of ulnar bow and its magnitude could likely determine whether osteotomy should be performed. Reduction of the radial head could be performed alone in patient whose maximum ulnar bow is less than 4 mm or whose ulnar bow lies in distal 40% of the ulna (75).
Site for osteotomy
Optimal site for ulnar osteotomy should be considered precisely in order to avoid delayed union or nonunion (6, 12, 34, 76). Proximal ulnar osteotomy should allow insertion of at least two screws at the proximal part. Di Gennaro et al. (32) reported that proximal one-third ulnar osteotomy presents significantly lower rate of nonunion than osteotomy of middle and distal ulna. However, in NMF patients with severe curvature of the ulna, osteotomy could be performed where the deformity is most obvious or based on the center of rotation angulation (21, 30). Whether the meta-to-diaphyseal transitional zone in children represents a reasonable choice for osteotomy needs further investigation (6, 12).
Fixation of the osteotomized ulna
Internal or external fixation should be applied to stabilize the ulnar or to proceed further correction of the deformities. Immediate correction of the bending of the ulna requires 10–15° degrees of dorsal or ulnar angulation for simultaneous radial head reduction (2, 3, 11, 16, 27, 34, 38, 44, 45, 46, 47, 49, 62). Although K wire fixation decreases operating time, rotation of the osteotomized ulna is sometimes unavoidable (1, 11). Locking compression plate could guarantee adequate stability in younger patients with mild deformities, while the gap between two osteotomy sites often requires bone graft (4, 24, 39, 47). Another benefit of plate fixation is that it could be shaped to adapt to the position of the ulna (22, 34).
Bor et al. (10) reported four patients who were treated with closed reduction, proximal ulnar osteotomy, and Ilizarov external fixator received good clinical outcomes. Similar results were then reported by Take et al. (10, 45) and Yuan et al. (49). Minimally invasive operation with external fixation allows gradual and spatial correction of the ulnar deformity to reduce the displaced radial head without invading the humeroradial joint, but long duration of wearing the frame could bring certain inconvenience to daily activities and needs higher compliance of the patients (10, 12, 16, 46, 49). Intraoperative external fixation-assisted one-step correction of the deformities was performed by Wang et al. (16) and Dukan et al. (47), who found it effective for multiple and progressive reduction attempts. Once the result of fluoroscopic examination is satisfactory, the external fixation is then removed. Other studies performed gradual lengthening of the ulna with external fixators, and open reduction of the radial head was added when elongation alone did not promise a stable reduction after removal of the external fixators, known as two-step strategy (44).
Reduction of the radial head and fixation of the radiocapitellar joint
Open reduction of the radial head was employed by most studies (12, 17, 19, 30, 32, 36, 42, 68). Gallone et al. (12) found no significant difference in the rate of recurrence of dislocation between close and open reduction of the radial head. Open reduction is also recommended in pediatric NMF patients with severe dislocation of the PRUJ (26). It should be importantly noted that open reduction may be unavoidable for patients who failed the initial close reduction (6).
It remains still controversial whether transcapitellar pinning should be performed after reduction of the radial head (6, 10, 11, 23, 25, 29, 42). A group of researchers did not recommend fixation of the radiocapitellar joint as this would bother early rehabilitation of the elbow and forearm (42). Other studies suggested transcapitellar fixation at 90° of elbow flexion through the radiocapitellar joint to provide stability for soft tissue reconstruction (22, 23, 25, 29).
Reconstruction of the annular ligament
The repositioning and reconstruction of annular ligament should be taken into consideration in NMF patients because it stabilizes the radial head during forearm rotation and prevents redislocation (1, 3, 4, 9, 15, 20, 23, 36, 39, 42, 48, 60, 77). On the other hand, annular ligament remnant in chronic Monteggia fracture cases may develop heterogenic tissue of which the reconstruction would result in stenosis of the radial neck, delayed growth of the radius, and limited elbow joint movement (9, 15, 42, 60). These shortcomings were also observed in cases reconstructing the annular ligament with tendon and fascia autografts or allografts through Bell-Tawse technique (18, 77). In NMF cases with intact annular ligament, different studies reported improved elbow mobility and stability with or without reconstruction of the annular ligament (36, 39, 42, 48). Other studies suggested that the reconstruction of annular ligament could be avoided unless there was detectable rotational instability of the radial head after reduction intraoperatively (4, 20, 23).
Complications
NMF could develop several complications, including recurrence of radial head dislocation, limited range of motion of the elbow, nonunion after osteotomy, and neural injuries, even if treated with proper surgical managements (2, 12, 15, 16, 29, 34, 35, 38, 39, 44, 61, 62, 64, 76, 77).
Recurrent dislocation of the radial head is ascribed to the deformity of the radial head, mismatching of the radioulnar joint after osteotomy, and operation-related risks (35, 39, 62, 76). Excessive angulation after osteotomy of the ulna could lead to re-dislocation of the radial head and requires a second surgery to enhance stability of the radiocapitellar joint. Besides, Bado III NMF was reported with higher rate of recurrence of radial head luxation, indicating that annular ligament repair is unavoidable (34).
Limited forearm rotation is one of the most common complications after reconstruction of the annular ligament. This is mainly due to a tight surrounding of the radial head and lack of blood supply which leads to ligament adhesion and fibrosis (15, 77).
Nonunion is more likely to happen in cases with external fixations (10, 16, 49). This may be overcome by iliac crest bone grafting after osteotomy and lengthening of the ulna, or the surgeon may choose another moderate technique, for example, Ilizarov external fixation or step-cut technique, to correct the abnormality (38, 45, 49).
The posterior interosseous nerve and the ulnar nerve are two of the most possibly interrupted nerves during open reduction of the radial head and osteotomy of the ulna. Operation and neurolysis may contribute to patients with neural injury not recovered beyond 3 months (29, 61, 64).
Conclusion
In conclusion, Monteggia fractures become challenging if not noticed within 4 weeks after injury. Patients then require surgery to reduce the radial head and correct forearm deformities. Classification system should take dislocation of PRUJ in to consideration, which would direct management and prognosis. Also, detailed examinations, especially radiographs, should be taken when the surgeon deals with forearm trauma. Surgical intervention, including osteotomy and angulation of the ulna, reduction of the radial head, internal or external fixation and reconstruction of the stability of the PRUJ and radiocapitellar joint, could bring satisfactory outcomes to NMF patients, while site for osteotomy of the ulna, fixation method, and whether the annular ligament needs reconstruction varies from studies. Besides, outcomes of surgical treatment may depend on classification type. Further researches are required to throw light on optimal options to treat specific types of NMF.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this study.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author contribution statement
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors are in agreement with the manuscript.
Acknowledgement
All authors would like to show great gratitude to Dr Shenghe Liu, who has given important opinions on the correction of the initial manuscript.
References
- 1.Soni JF, Valenza WR, Pavelec AC. Chronic Monteggia. Current Opinion in Pediatrics 20193154–60. ( 10.1097/MOP.0000000000000710) [DOI] [PubMed] [Google Scholar]
- 2.Miller TC, Fishman FG. Management of Monteggia injuries in the pediatric patient. Hand Clinics 202036469–478. ( 10.1016/j.hcl.2020.07.001) [DOI] [PubMed] [Google Scholar]
- 3.Hubbard J, Chauhan A, Fitzgerald R, Abrams R, Mubarak S, Sangimino M. Missed pediatric Monteggia fractures. JBJS Reviews 20186 e2. ( 10.2106/JBJS.RVW.17.00116) [DOI] [PubMed] [Google Scholar]
- 4.Delpont M, Louahem D, Cottalorda J. Monteggia injuries. Orthopaedics and Traumatology, Surgery and Research 2018104S113–S120. ( 10.1016/j.otsr.2017.04.014) [DOI] [PubMed] [Google Scholar]
- 5.Ramski DE, Hennrikus WP, Bae DS, Baldwin KD, Patel NM, Waters PM, Flynn JM. Pediatric Monteggia fractures: a multicenter examination of treatment strategy and early clinical and radiographic results. Journal of Pediatric Orthopedics 201535115–120. ( 10.1097/BPO.0000000000000213) [DOI] [PubMed] [Google Scholar]
- 6.Tan SHS, Low JY, Chen H, Tan JYH, Lim AKS, Hui JHP.Surgical management of missed paediatric Monteggia fractures: a systematic review and meta-analysis. Journal of Orthopaedic Trauma 20213665––73..( 10.1097/BOT.0000000000002219) [DOI] [PubMed] [Google Scholar]
- 7.Joeris A, Lutz N, Blumenthal A, Slongo T, Audigé L. The AO pediatric comprehensive classification of long bone fractures (PCCF). Acta Orthopaedica 201788123–128. ( 10.1080/17453674.2016.1258532) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal T, Arora SS, Banerjee S, Kandwal P. Neglected Monteggia fracture dislocations in children: a systematic review. Journal of Pediatric Orthopedics: Part B 201524191–199. ( 10.1097/BPB.0000000000000147) [DOI] [PubMed] [Google Scholar]
- 9.Canton G, Hoxhaj B, Fattori R, Murena L. Annular ligament reconstruction in chronic Monteggia fracture-dislocations in the adult population: indications and surgical technique. Musculoskeletal Surgery 2018102 (Supplement 1) 93–102. ( 10.1007/s12306-018-0564-6) [DOI] [PubMed] [Google Scholar]
- 10.Bor N, Rubin G, Rozen N, Herzenberg JE. Chronic anterior Monteggia lesions in children: report of 4 cases treated with closed reduction by ulnar osteotomy and external fixation. Journal of Pediatric Orthopedics 2015357–10. ( 10.1097/BPO.0000000000000203) [DOI] [PubMed] [Google Scholar]
- 11.Soni JF, Valenza WR, Matsunaga CU, Costa ACP, Faria FF. Chronic Monteggia fracture-dislocation in children surgical strategy and results. Acta Ortopédica Brasileira 201927244–247. ( 10.1590/1413-785220192705215273) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallone G, Trisolino G, Stilli S, Di Gennaro GL. Complications during the treatment of missed Monteggia fractures with unilateral external fixation: a report on 20 patients in a 10-year period in a tertiary referral center. Journal of Pediatric Orthopedics: Part B 201928256–266. ( 10.1097/BPB.0000000000000592) [DOI] [PubMed] [Google Scholar]
- 13.Slongo TF.Correction osteotomy of neglected ‘Monteggia’ lesion with an external fixator. Operative Orthopädie und Traumatologie 200820435–449. ( 10.1007/s00064-008-1414-8) [DOI] [PubMed] [Google Scholar]
- 14.Musikachart P, Tisavipat N, Eamsobhana P. Does overcorrection cause any negative effect on pediatric missed Monteggia lesion? European Journal of Orthopaedic Surgery and Traumatology 2020301017–1024. ( 10.1007/s00590-020-02660-z) [DOI] [PubMed] [Google Scholar]
- 15.Datta T, Chatterjee N, Pal AK, Das SK. Evaluation of outcome of corrective ulnar osteotomy with bone grafting and annular ligament reconstruction in neglected Monteggia fracture dislocation in children. Journal of Clinical and Diagnostic Research 20148LC01–LC04. ( 10.7860/JCDR/2014/9891.4409) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Q, Du MM, Pei XJ, Luo JZ, Li YZ, Liu YC, Wang X, Cao JC, Han JH. External fixator-assisted ulnar osteotomy: a novel technique to treat missed Monteggia fracture in children. Orthopaedic Surgery 201911102–108. ( 10.1111/os.12426) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Çevi K HB, Yuvaci F, Ecevi Z E, Bulut G. Four different management strategies in missed Monteggia lesions in children. Journal of Orthopaedics 202021207–212. ( 10.1016/j.jor.2020.03.055) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohan Kumar EG, Yathisha Kumar GM, Noorudheen M. Functional outcome of bell tawse procedure for the management of chronic unreduced Monteggia fracture-dislocation in children. Indian Journal of Orthopaedics 201953745–750. ( 10.4103/ortho.IJOrtho_47_19) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park H, Park KW, Park KB, Kim HW, Eom NK, Lee DH. Impact of open reduction on surgical strategies for missed Monteggia fracture in children. Yonsei Medical Journal 201758829–836. ( 10.3349/ymj.2017.58.4.829) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Song KS, Ramnani K, Bae KC, Cho CH, Lee KJ, Son ES. Indirect reduction of the radial head in children with chronic Monteggia lesions. Journal of Orthopaedic Trauma 201226597–601. ( 10.1097/BOT.0b013e3182548981) [DOI] [PubMed] [Google Scholar]
- 21.Posey SL, Cole HA, Halverson S, Stutz C, Schoenecker JG. Intra-articular Monteggia fracture: a case study of using the center of rotational angulation to improve a functional outcome. Journal of Orthopaedic Case Reports 2018827–30. ( 10.13107/jocr.2250-0685.1242) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakamura K, Hirachi K, Uchiyama S, Takahara M, Minami A, Imaeda T, Kato H. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. Journal of Bone and Joint Surgery: American Volume 2009911394–1404. ( 10.2106/JBJS.H.00644) [DOI] [PubMed] [Google Scholar]
- 23.Stragier B, De Smet L, Degreef I. Long-term follow-up of corrective ulnar osteotomy for missed Monteggia fractures in children. Journal of Shoulder and Elbow Surgery 201827e337–e343. ( 10.1016/j.jse.2018.06.029) [DOI] [PubMed] [Google Scholar]
- 24.Gryson T, Van Tongel A, Plasschaert F. The management of chronic paediatric Monteggia fracture-dislocation. Journal of Orthopaedics 20212465–76. ( 10.1016/j.jor.2021.02.009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu X, Kun Wang Y, Zhang J, Zhu Z, Guo Y, Lu M. Management of missed Monteggia fractures with ulnar osteotomy, open reduction, and dual-socket external fixation. Journal of Pediatric Orthopedics 201333398–402. ( 10.1097/BPO.0b013e3182812762) [DOI] [PubMed] [Google Scholar]
- 26.Eamsobhana P, Chalayon O, Kaewpornsawan K, Ariyawatkul T. Missed Monteggia fracture dislocations treated by open reduction of the radial head. Bone and Joint Journal 2018100-B1117–1124. ( 10.1302/0301-620X.100B8.BJJ-2017-0866.R3) [DOI] [PubMed] [Google Scholar]
- 27.Fabricant PD, Baldwin KD. Missed pediatric Monteggia fracture: a 63-year follow-up. Journal of Pediatrics 2015167 495. ( 10.1016/j.jpeds.2015.05.023) [DOI] [PubMed] [Google Scholar]
- 28.Agarwal A, Pawar I. Neglected type I Monteggia fracture dislocation in adult. Journal of Clinical and Diagnostic Research 201711RD01–RD02. ( 10.7860/JCDR/2017/28250.10468) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liao S, Pan J, Lin H, Xu Y, Lu R, Wu J, Zhao M, Chen H, Cai M, Ding Xet al. A new approach for surgical treatment of chronic Monteggia fracture in children. Injury 2019501237–1241. ( 10.1016/j.injury.2019.04.017) [DOI] [PubMed] [Google Scholar]
- 30.Xu Z, Li Y, Wang Z, Cai H. Open reduction combined with CORA-based osteotomy of the ulna in the treatment of missed Bado type I Monteggia injury: a retrospective study of 5 cases. Medicine 201796 e8609. ( 10.1097/MD.0000000000008609) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garg P, Baid P, Sinha S, Ranjan R, Bandyopadhyay U, Mitra S. Outcome of radial head preserving operations in missed Monteggia fracture in children. Indian Journal of Orthopaedics 201145404–409. ( 10.4103/0019-5413.83946) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Di Gennaro GL, Martinelli A, Bettuzzi C, Antonioli D, Rotini R. Outcomes after surgical treatment of missed Monteggia fractures in children. Musculoskeletal Surgery 201599 (Supplement 1) S75–S82. ( 10.1007/s12306-015-0362-3) [DOI] [PubMed] [Google Scholar]
- 33.Chin K, Kozin SH, Herman M, Horn BD, Eberson CP, Bae DS, Abzug J. Pediatric Monteggia fracture-dislocations: avoiding problems and managing complications. Instructional Course Lectures 201665399–407. [PubMed] [Google Scholar]
- 34.Delpont M, Jouve JL, Sales de Gauzy J, Louahem D, Vialle R, Bollini G, Accadbled F, Cottalorda J. Proximal ulnar osteotomy in the treatment of neglected childhood Monteggia lesion. Orthopaedics and Traumatology, Surgery and Research 2014100803–807. ( 10.1016/j.otsr.2014.06.022) [DOI] [PubMed] [Google Scholar]
- 35.Suzuki T, Seki A, Nakamura T, Ikegami H, Takayama S, Nakamura M, Matsumoto M, Sato K. Re-dislocation after corrective osteotomy for chronic dislocation of the radial head in children. Bone and Joint Journal 201597-B1582–1587. ( 10.1302/0301-620X.97B11.36009) [DOI] [PubMed] [Google Scholar]
- 36.Lu X, Yan G, Wang Y, Zhu Z, You H, Zhang J, Guo Y. Repositioning of the annular ligament in the management of missed Monteggia fracture. Journal of Pediatric Orthopedics 20173720–22. ( 10.1097/BPO.0000000000000584) [DOI] [PubMed] [Google Scholar]
- 37.Jepegnanam TS.Salvage of the radial head in chronic adult Monteggia fractures. Report of four cases. Journal of Bone and Joint Surgery: British Volume 200688645–648. ( 10.1302/0301-620X.88B5.17346) [DOI] [PubMed] [Google Scholar]
- 38.Peshin C, Ratra R, Juyal AK. Step-cut osteotomy in neglected Monteggia fracture dislocation in pediatric and adolescent patients: a retrospective study. Journal of Orthopaedic Surgery 2020282309499020964082. ( 10.1177/2309499020964082) [DOI] [PubMed] [Google Scholar]
- 39.Zheng ET, Waters PM, Vuillermin CB, Williams K, Bae DS. Surgical reconstruction of missed Monteggia lesions in children. Journal of Pediatric Orthopedics 202040e916–e921. ( 10.1097/BPO.0000000000001630) [DOI] [PubMed] [Google Scholar]
- 40.Horii E, Nakamura R, Koh S, Inagaki H, Yajima H, Nakao E. Surgical treatment for chronic radial head dislocation. Journal of Bone and Joint Surgery: American Volume 2002841183–1188. ( 10.2106/00004623-200207000-00014) [DOI] [PubMed] [Google Scholar]
- 41.Langenberg LC, Beumer A, The B, Koenraadt K, Eygendaal D. Surgical treatment of chronic anterior radial head dislocations in missed Monteggia lesions in children: a rationale for treatment and pearls and pitfalls of surgery. Shoulder and Elbow 202012422–431. ( 10.1177/1758573219839225) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen HY, Wu KW, Dong ZR, Huang SC, Kuo KN, Wang TM. The treatment of chronic radial head dislocation in Monteggia fracture without annular ligament reconstruction. International Orthopaedics 2018422165–2172. ( 10.1007/s00264-018-3943-6) [DOI] [PubMed] [Google Scholar]
- 43.Zhou W, Li L, Mu M. Treatment of missed Monteggia fracture with intact annular ligament after an interval of 9 years: a case report and literature review. Journal of International Medical Research 202048300060520949079. ( 10.1177/0300060520949079) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li J, Zhao X, Rai S, Ding Y, Zhang Q, Ze R, Tang X, Liu R, Hong P. Two-stage strategy for neglected Monteggia fracture in children: a retrospective study of 51 patients. Medicine 2021100 e25129. ( 10.1097/MD.0000000000025129) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Take M, Tomori Y, Sawaizumi T, Majima T, Nanno M, Takai S. Ulnar osteotomy and the Ilizarov mini-fixator for pediatric chronic Monteggia fracture-dislocations. Medicine 201998 e13978. ( 10.1097/MD.0000000000013978) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gooi SG, Wang CS, Saw A, Zulkiflee O. Ulnar osteotomy with 2-pin unilateral gradual distraction for treatment of chronic Monteggia fracture: a case report. Malaysian Orthopaedic Journal 20171179–81. ( 10.5704/MOJ.1703.015) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dukan R, Le Hanneur M, Pannier S, Fitoussi F. Use of an external fixator during one-step surgical management of missed chronic Monteggia injuries. Orthopaedics and Traumatology, Surgery and Research 2022108102963. ( 10.1016/j.otsr.2021.102963) [DOI] [PubMed] [Google Scholar]
- 48.Baydar M, Ozturk K, Orman O, Akbulut D, Keskinbıçkı MV, Şencan A. Use of corrective ulnar osteotomy and radial head relocation into preserved annular ligament in the treatment of radiocapitellar instability secondary to pediatric chronic Monteggia fracture-dislocation. Journal of Hand Surgery 2021. ( 10.1016/j.jhsa.2021.05.025) [DOI] [PubMed] [Google Scholar]
- 49.Yuan Z, Xu HW, Liu YZ, Li YQ, Li JC, Canavese F. The use of external fixation for the management of acute and chronic Monteggia fractures in children. Journal of Children’s Orthopaedics 201913551–559. ( 10.1302/1863-2548.13.190115) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ring D.Monteggia fractures. Orthopedic Clinics of North America 20134459–66. ( 10.1016/j.ocl.2012.08.007) [DOI] [PubMed] [Google Scholar]
- 51.Gopinathan NR, Rangasamy K, Vatsya P, Behera P. Management of missed type-2 Monteggia fracture equivalent in a 9-year-old child: a case report. JBJS Case Connector 202111e20, ., 00179. ( 10.2106/JBJS.CC.20.00179) [DOI] [PubMed] [Google Scholar]
- 52.Josten C, Freitag S. Monteggia and Monteggia-like-lesions: classification, indication, and techniques in operative treatment. European Journal of Trauma and Emergency Surgery 200935296–304. ( 10.1007/s00068-008-8028-6) [DOI] [PubMed] [Google Scholar]
- 53.Bado JL.The Monteggia lesion. Clinical Orthopaedics and Related Research 19675071–86. [PubMed] [Google Scholar]
- 54.Ko KR, Shim JS, Park J, Won J. Predictors of ideal outcomes after reconstructive surgery for chronic Monteggia fracture in children. Journal of Orthopaedic Science 2021. ( 10.1016/j.jos.2021.06.009) [DOI] [PubMed] [Google Scholar]
- 55.Oka K, Tanaka H, Shigi A, Abe S, Miyamura S, Shiode R, Kazui A, Murase T. Quantitative analysis for the change in lengths of the radius and ulna in missed Bado type I Monteggia fracture. Journal of Pediatric Orthopedics 202040e922–e926. ( 10.1097/BPO.0000000000001648) [DOI] [PubMed] [Google Scholar]
- 56.Rehim SA, Maynard MA, Sebastin SJ, Chung KC. Monteggia fracture dislocations: a historical review. Journal of Hand Surgery 2014391384–1394. ( 10.1016/j.jhsa.2014.02.024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Letts M, Locht R, Wiens J. Monteggia fracture-dislocations in children. Journal of Bone and Joint Surgery: British Volume 198567724–727. ( 10.1302/0301-620X.67B5.4055869) [DOI] [PubMed] [Google Scholar]
- 58.Farr LD, Werner FW, McGrattan ML, Zwerling SR, Harley BJ. Anatomy and biomechanics of the forearm interosseous membrane. Journal of Hand Surgery 201540 1145–51.e2. ( 10.1016/j.jhsa.2014.12.025) [DOI] [PubMed] [Google Scholar]
- 59.Tan J, Mu M, Liao G, Zhao Y, Li J. Biomechanical analysis of the annular ligament in Monteggia fractures using finite element models. Journal of Orthopaedic Surgery and Research 201510 30. ( 10.1186/s13018-015-0170-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kamble P, Prabhakar A, Wankhade A. Heterotopic ossification of annular ligament: a case report and review of literature. Journal of Clinical Orthopaedics and Trauma 202121101511. ( 10.1016/j.jcot.2021.101511) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nishimura M, Itsubo T, Horii E, Hayashi M, Uchiyama S, Kato H. Tardy ulnar nerve palsy caused by chronic radial head dislocation after Monteggia fracture: a report of two cases. Journal of Pediatric Orthopedics: Part B 201625450–453. ( 10.1097/BPB.0000000000000302) [DOI] [PubMed] [Google Scholar]
- 62.Miyake J, Moritomo H, Kataoka T, Murase T, Sugamoto K. In vivo three-dimensional motion analysis of chronic radial head dislocations. Clinical Orthopaedics and Related Research 20124702746–2755. ( 10.1007/s11999-012-2325-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yildirim A, Nas K. Rehabilitation of neglected Monteggia fracture: dislocations in children. Journal of Back and Musculoskeletal Rehabilitation 2017301251–1257. ( 10.3233/BMR-169621) [DOI] [PubMed] [Google Scholar]
- 64.Demirel M, Saglam Y, Tunali O. Posterior interosseous nerve palsy associated with neglected pediatric Monteggia fracture-dislocation: a case report. International Journal of Surgery Case Reports 201627102–106. ( 10.1016/j.ijscr.2016.08.011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anderson A, Werner FW, Tucci ER, Harley BJ. Role of the interosseous membrane and annular ligament in stabilizing the proximal radial head. Journal of Shoulder and Elbow Surgery 2015241926–1933. ( 10.1016/j.jse.2015.05.030) [DOI] [PubMed] [Google Scholar]
- 66.Souder CD, Roocroft JH, Edmonds EW. Significance of the lateral humeral line for evaluating radiocapitellar alignment in children. Journal of Pediatric Orthopedics 201737e150–e155. ( 10.1097/BPO.0000000000000853) [DOI] [PubMed] [Google Scholar]
- 67.Lincoln TL, Mubarak SJ. ‘Isolated’ traumatic radial-head dislocation. Journal of Pediatric Orthopedics 199414454–457. ( 10.1097/01241398-199407000-00006) [DOI] [PubMed] [Google Scholar]
- 68.Storen G.Traumatic dislocation of the radial head as an isolated lesion in children; report of one case with special regard to roentgen diagnosis. Acta Chirurgica Scandinavica 1959116144–147. [PubMed] [Google Scholar]
- 69.Ramirez RN, Ryan DD, Williams J, Wren TA, Ibrahim D, Weiss JM, Kay RM, Lightdale-Miric N, Skaggs DL. A line drawn along the radial shaft misses the capitellum in 16% of radiographs of normal elbows. Journal of Pediatric Orthopedics 201434763–767. ( 10.1097/BPO.0000000000000199) [DOI] [PubMed] [Google Scholar]
- 70.Rutkowski PT, Samora JB. Congenital radioulnar synostosis. Journal of the American Academy of Orthopaedic Surgeons 202129563–570. ( 10.5435/JAAOS-D-20-01133) [DOI] [PubMed] [Google Scholar]
- 71.Roles NC.Congenital dislocation of the head of the radius. BMJ 19712 712. ( 10.1136/bmj.2.5763.712-a) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stieber JR, Dormans JP. Manifestations of hereditary multiple exostoses. Journal of the American Academy of Orthopaedic Surgeons 200513110–120. ( 10.5435/00124635-200503000-00004) [DOI] [PubMed] [Google Scholar]
- 73.Adams JE, Osterman AL. The Essex-Lopresti injury: evaluation and treatment considerations. Hand Clinics 202036463–468. ( 10.1016/j.hcl.2020.07.012) [DOI] [PubMed] [Google Scholar]
- 74.Alajmi TAS.Neglected Monteggia fracture dislocations in children: a case series. Journal of Orthopaedic Case Reports 20201057–62. ( 10.13107/jocr.2020.v10.i07.1918) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shinohara T, Horii E, Koh S, Fujihara Y, Hirata H. Mid- to long-term outcomes after surgical treatment of chronic anterior dislocation of the radial head in children. Journal of Orthopaedic Science 201621759–765. ( 10.1016/j.jos.2016.07.018) [DOI] [PubMed] [Google Scholar]
- 76.Kozin SH, Abzug JM, Safier S, Herman MJ. Complications of pediatric elbow dislocations and Monteggia fracture-dislocations. Instructional Course Lectures 201564493–498. [PubMed] [Google Scholar]
- 77.Pari C, Puzzo A, Paderni S, Belluati A. Annular ligament repair using allograft for the treatment of chronic radial head dislocation: a case report. Acta Bio-Medica 201890154–157. ( 10.23750/abm.v90i1-S.8010) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a