Abstract
The physis of the distal femur contributes to 70% of femoral growth and 37% of the total limb growth; therefore, physeal injury can lead to important alterations of axes and length.
Distal metaphyseal corner-type fracture prior to walking is classically associated with child abuse. In children aged >10 years, sports-related fractures and car accidents are significant contributors.
Imaging includes a two-plane radiographic study of the knee. It is recommended to obtain radiographs that include the entire femur to rule out concomitant injuries. In cases of high suspicion of distal metaphyseal fractures and no radiographic evidence, CT or MRI can show the existence of hidden fractures.
Fractures with physeal involvement are conventionally classified according to the Salter–Harris classification, but the Peterson classification is also recommended as it includes special subgroups.
Conservative and surgical management are valid alternatives for the treatment of these fractures. Choosing between both alternatives depends on factors related to the fracture type.
As there is a high risk of permanent physeal damage, long-term follow-up is essential until skeletal maturity is complete.
Keywords: femur, paediatrics, trauma, surgery
Introduction
Distal femur fractures have a variable frequency of approximately 27% of all femur fractures (1), increasing due to a rise incidence of high-energy trauma. This acquires greater relevance when we understand that the main complication is growth disturbances secondary to growth-plate injury (2).
Most bone growth arises from the physis of the distal femur; thus, achieving a complete understanding of the anatomy, the mechanism of the injuries, and the most appropriate management option will be of vital importance when addressing these issues and avoiding future complications (2).
Any patient suspected of having a distal femur fracture should be examined carefully and subjected to complementary imaging studies, as other associated injuries can often be overlooked and become critical if improperly managed.
We present herein a review of the available literature to analyse the corresponding anatomy, epidemiology, and pertinent treatment for these fractures.
Anatomy
The distal femur in the immature skeleton is divided into the metaphysis, physis, and epiphysis. The epiphysis consists of two condyles, which articulate with the tibial plateau, forming a trochlear-type joint. In the anterior metaphyseal-epiphyseal area, we find a groove between two protrusions that form the femoro-patellar canal.
The distal femur circulation is multifocal, with blood vessels entering the epiphysis from the medial, lateral, and posterior sides. However, the most important blood supply comes from the posterior femoral notch, mainly from the middle genicular artery (3). The condyles have less circulation, especially the medial one, and are more susceptible to ischemic changes (4).
The femur develops through endochondral ossification. Morphologically, a mesenchymal condensation begins between 37 and 44 days of gestation, followed by a chondrification process between 42 and 48 days, and finally, an endochondral ossification between 54 and 60 days. Morphologically, the intercondylar fossa begins to form at 51–52 days of gestation, and spherical condyles form between 54 and 58 days (5).
Of all the long bones, the femur is the second, after the clavicle, where the ossification process begins. This begins in the central area of the diaphysis and extends to both ends. The primary ossification centre at the diaphysis level appears in the 7th week of gestation, and the secondary ossification centres in the proximal and distal epiphysis appear later in gestation (6), with only one ossification centre in the lower epiphysis. This centre begins its ossification between 23 and 40 weeks of gestation (7), being present in 94.5% of fetuses at 32 weeks (8), and can be observed in neonatal radiographs (Fig. 1). Initially, this ossification centre has a circular or oval shape and is centrally located (Fig. 2). Later, two condyles can be seen with irregular areas at both ends and a wavy physis (Fig. 3). This epiphysis is one of the last to join its respective metaphysis, between 14 and 16 years in girls and between 16 and 18 years in boys (Fig. 4) (3, 4).
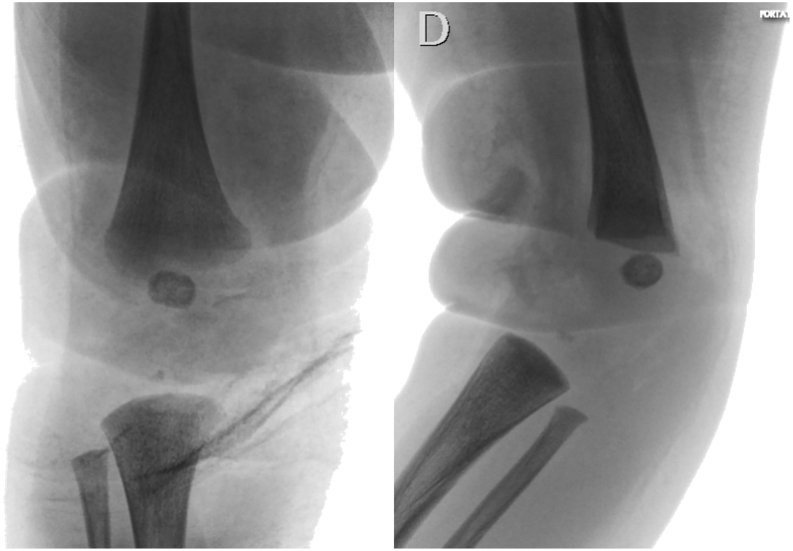
Figure 1.
Radiographic images of the right knee of a neonate. The spherical epiphyseal ossification centre of the distal femur is seen.
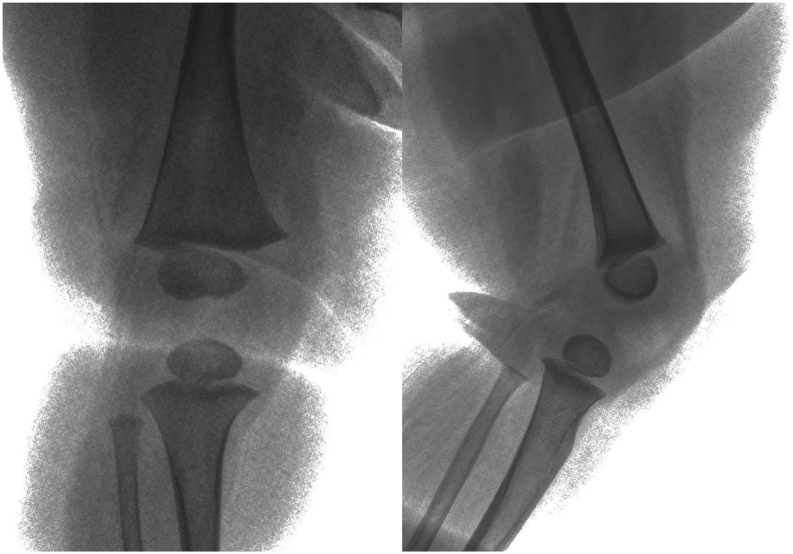
Figure 2.
Radiographic images of the right knee of a 6-month-old girl. The epiphyseal ossification centre of the distal femur develops curves corresponding to the two condyles.
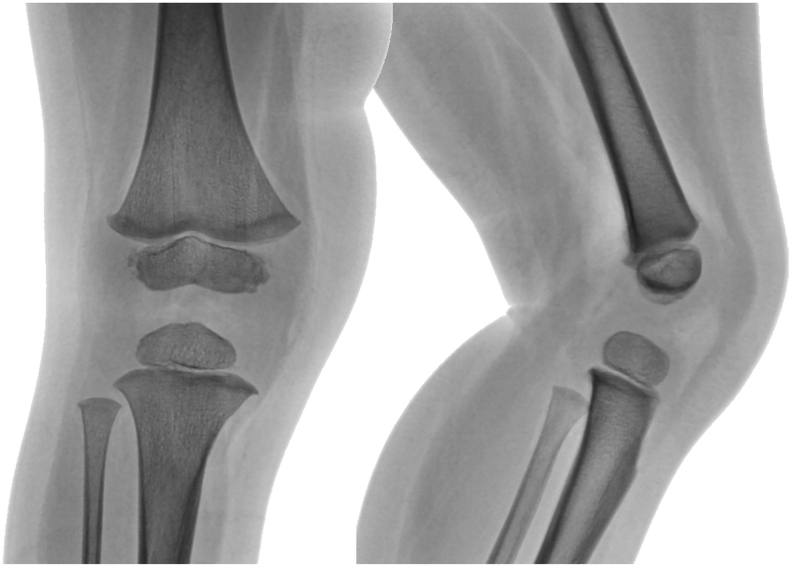
Figure 3.
Radiographic images of right knee of a 2-year-old boy. The distal femoral physis with undulating shape and usual irregularities of the distal margins of the medial and lateral condyle are noted.
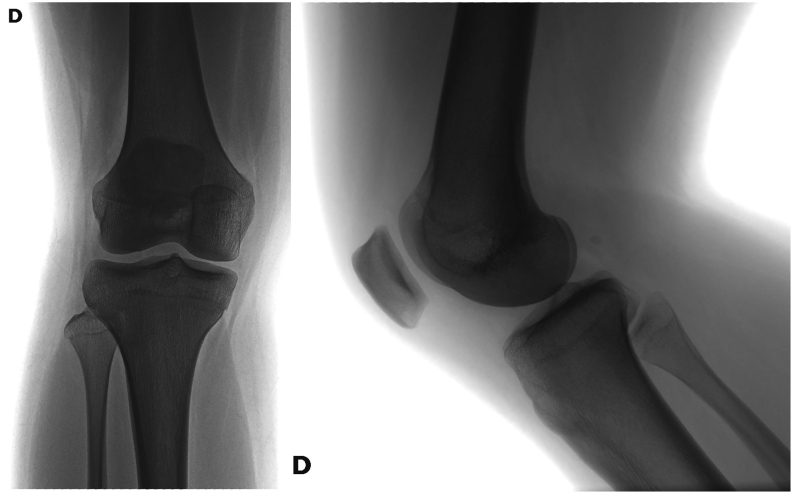
Figure 4.
Radiographic images of the right knee of a 15-year-old girl. Physeal closure ending.
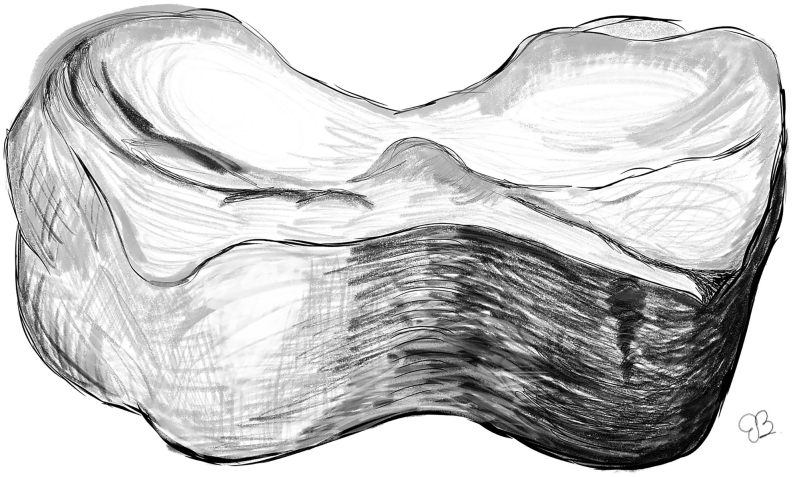
The physis of the distal femur contributes to 70% of femoral growth and 37% of the total growth of the limb, which is approximately 1 cm per year (9), and hence the most active physis-epiphysis unit in the body (4). MRI studies have determined that the physis has a stable pattern, with flat and concave anterior and posterior surfaces, respectively. Its greatest concavity is at the level of the medial condyle (9). The physis has three main undulations, namely the central ridge, the lateral ridge, and the medial peak (Fig. 5). The lateral ridge extends from the central ridge to the lateral border of the physis, and the medial peak extends from the medial border to the centre of the physis, failing to join the central ridge. The central ridge is the highest point of this physis. These undulations divide the physis into four "mamelons" (10). The height of the ridges decreases with growth. This suggests that the stability of the physis decreases with growth, with the decrease in height of the central ridge (10). The physeal closure begins in the central area of the physis and continues in a centrifugal manner. The closure of the physis occurs between 14 and 16 years in girls and between 16 and 18 years in boys, but can also occur up to 20 years of age in boys (11).
Figure 5.
Scheme of the physis surface with the three main undulations.
Epidemiology
The incidence of femoral fractures in the paediatric population varies according to the affected segment; the most frequently occurring ones are diaphyseal fractures. According to the Swedish national registry, distal femur fractures are the second most frequent type (27%) and tend to occur more in female than in male subjects (12).
Distal femur fractures can be divided into supracondylar fractures and fractures with physeal involvement. Although distal femur fractures are reportedly rare, Smith et al. (13) in their retrospective study described an incidence of 12% for distal femur fractures of all femoral fractures in children. Regarding physeal fractures of the distal femur, these correspond to 1.2% of all physeal fractures in children (14), and 7% of all physeal fractures of the lower limb (15). The average age of presentation in girls and boys is 9.8 and 10.8 years, respectively (16).
Pathophysiology
Femur fractures in the paediatric population occur as a result of different damage mechanisms depending on age. The most frequent mechanism of femoral fractures is falls, except in adolescents, wherein motor vehicle accidents contribute to most fractures (12). This trend is supported by Loder et al. (17), who used an extensive United States-based database to study the epidemiology and mechanisms of femur fractures in children. Typically, fractures tend to be more frequent in the spring and summer months than in other seasons, with the exception of Nordic countries, where there is an increase in fractures in winter months associated with the ski season (12).
The most mentioned mechanism of distal femur fracture is the so-called ‘wagon wheel’ fracture, in which the child’s foot is trapped between the spokes of the wagon wheel, with transmission of excessive forces towards the distal femur and its consequent fracture. With the extensive changes in transportation methods over time, this mode of fracture is very rare (3).
Fractures due to falls, motor vehicle accidents, and non-accidental trauma tend to be more common in young children. Regarding the latter, the distal metaphyseal corner-type fracture is classically associated with non-accidental trauma in children prior to walking. Humeral and femoral fractures are the most frequent long-bone fractures associated with violence in children aged <1 year. Reports have shown that such fractures comprise between 60 and 93% of all distal femur fractures in children prior to walking age (18). According to the Swedish national registry, distal femur fractures are most frequently attributed to non-accidental trauma in this population (12).
Obstetric trauma is a rare cause of distal femur fracture. It usually corresponds to a Salter–Harris I physeal lesion, which is frequently misdiagnosed as dislocation, septic arthritis, osteomyelitis, or pseudo-paralysis (3, 4). The fracture is produced by a hyperflexion mechanism of the knee.
In children aged >10 years, sports-related fractures and car accidents become more significant causes. Associated sports fractures are those that generate a lever after a lateral blow with knee valgus and fixed foot, as seen in American football or rugby, where shoes with studs remain attached to the ground while the player is tackled (3). The lateral and medial collateral ligaments are inserted distal to the physis, on the lateral and medial aspects respectively, at the level of the distal epiphysis. These are more resistant than the physis; therefore, it yields to forces exerted on the femur or tibia, generating a physeal fracture (3). Thus, owing to the strength of the medial collateral ligament, a medial condyle fracture is most common.
Clinical evaluation
The patient with suspected distal femur fracture should be carefully examined, especially if they have had a severe trauma, and the appropriate advanced trauma life support protocol should be executed. A paediatric patient with a distal femur fracture will present pain in the knee on palpation and mobilization, both active and passive, ecchymosis with increased volume, joint effusion, deformity, and impossible weight bearing (15). It is necessary to evaluate the skin, to rule out bone exposure, and distal pulses to evaluate possible vascular compromise (19).
Although the physis is classically described as weaker than the ligaments, the latter are affected in 24–45% of fractures (3), and it is common to find some laxity of the anterior cruciate ligament after a fracture. In a retrospective study, Bertin et al. (20) found a 37.5% presence of anterior cruciate ligament injury in distal femur fractures.
In metaphyseal fractures, the gastrocnemius is the main deforming force, angulating the distal fragment towards the popliteal fossa. The proximal fragment can be trapped through the fibres of the quadriceps, especially involving the vastus medialis, restricting knee flexion, and generating a posterior scar (4).
Vascular involvement is rare but may be present because of the position of the popliteal artery in relation to the fracture. In case of poor perfusion or no perfusion, it is suggested to perform a CT-angiographic evaluation and be prepared for a vascular examination.
In high-energy trauma, neurological compromise can occur, with neuropraxia, neurotmesis, and laceration of the tibial or common fibular nerve. Valgus deformity has been more frequently associated with the common peroneal nerve (3). Given the high energy of the trauma, it is important to rule out compartment syndrome and manage it accordingly.
Imaging study
In most cases, a distal femur fracture can be diagnosed with a simple two-plane radiographic study of the knee. It is recommended to obtain radiographs that include the entire femur to rule out concomitant injuries at the hip or diaphyseal femur level.
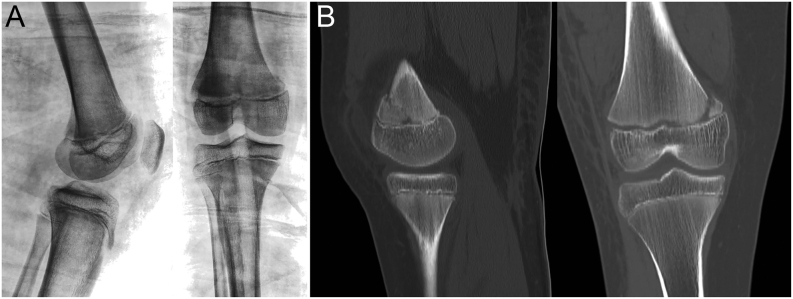
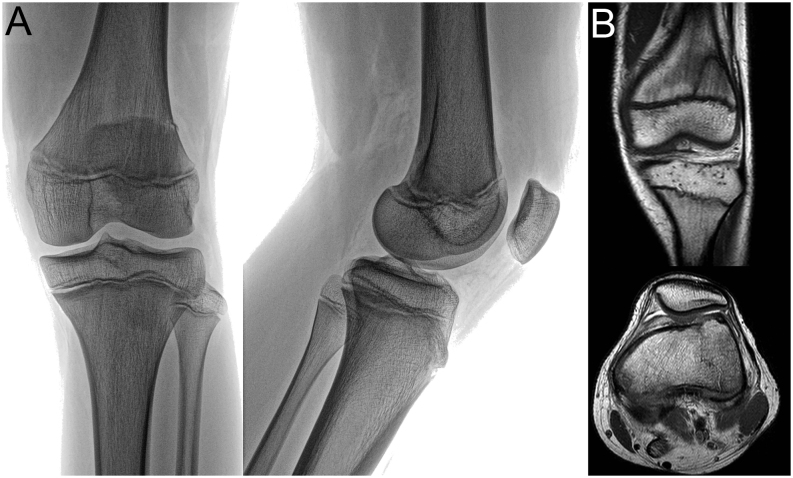
If there is suspicion of a fracture without radiographic evidence, further studies should be requested. CT can provide more information, as it can demonstrate hidden fractures or physeal involvement (Fig. 6). Furthermore, MRI can reveal the presence of bone oedema and allow clinicians/surgeons to evaluate the existence of hidden fractures (Fig. 7), ligament, or meniscal involvement (15). A prospective study that evaluated the MRI images of children with joint trauma associated with pain and functional impotence, but without radiographic fracture evidence, showed the presence of hidden fractures in 35% of cases (21). Finally, ultrasound is useful for the study of fractures in young children, especially newborns, because in addition to detecting the fracture, it can reveal subperiosteal haematoma (4).
Figure 6.
(A) Radiographic images of the right knee of a 10-year-old girl, with a distal physeal femoral fracture. (B) CT: sagittal and coronal views show a Salter–Harris type II physeal injury.
Figure 7.
(A) Radiographic images of the left knee of a 14-year-old boy, with a distal femoral fracture. (B) MRI: coronal and axial T1 views shows a Salter–Harris II distal femoral physis fracture.
Doppler ultrasound or CT-angiography are recommended in patients with suspected vascular injury (15).
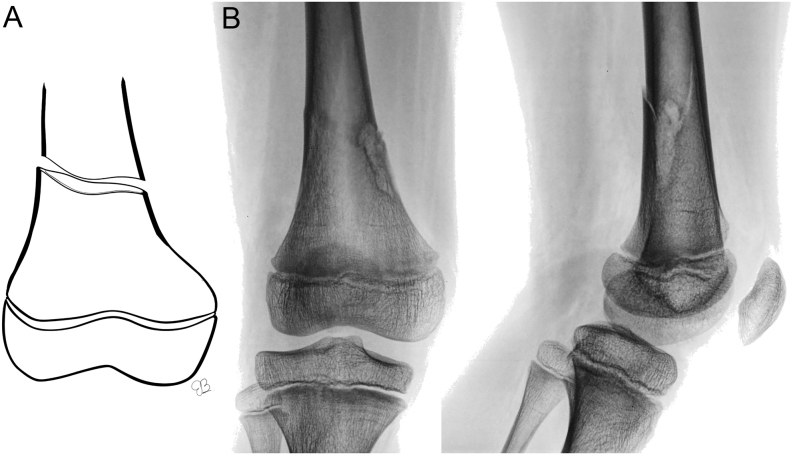
Classification
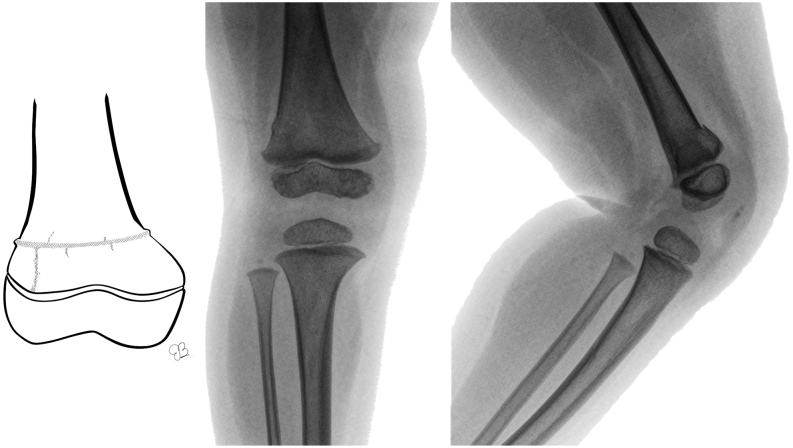
Different classification systems are described for distal femur fractures in the paediatric population. Descriptively, they are divided into supracondylar or metaphyseal fractures (Fig. 8) and joint fractures, with physeal involvement.
Figure 8.
(A) Schematic of distal metaphyseal femoral fracture. (B) Radiographic images of the right knee of a 6-year-old boy with a pathologic bone distal femoral fracture (non-osteogenic fibroma).
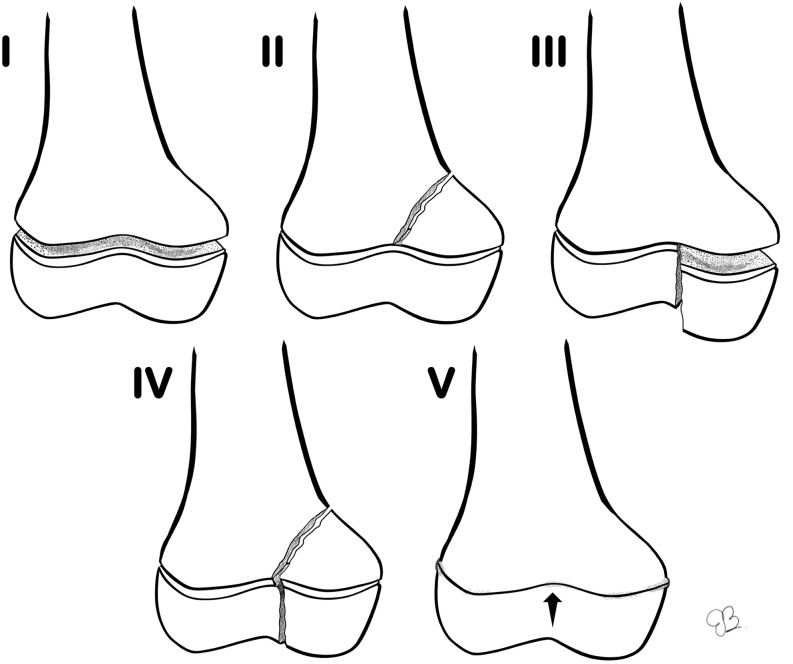
Fractures with physeal involvement are typically classified according to the Salter–Harris classification system, which is the most widely used (Fig. 9) (1). Peterson classification is also recommended (Fig. 10) (3, 22), which includes special subgroups that include metaphyseal fractures that indirectly reach the physis (Fig. 11). Salter–Harris II type fractures are described as the most frequent with an incidence of 64% (3).
Figure 9.
Classification according to Salter and Harris for distal femoral fractures in children. Type I, complete separation of the epiphysis from the metaphysis without any bone fracture; type II, line of separation extends along the epiphyseal plate and then out through a portion of the metaphysis; type III, extends from the joint surface to the weak zone of the epiphyseal plate and then extends along the plate to its periphery; type IV, extends from the joint surface through the epiphysis, across the full thickness of the epiphyseal plate, and through a portion of the metaphysis; type V, crushing force applied through the epiphysis to one area of the epiphyseal plate.
Figure 10.
Classification according to Peterson for distal femoral fractures in children. Type I, transverse fracture of the metaphysis with extension to the physis; type II, separation of the physis with a portion of metaphysis attached to the physis; type III, separation of the epiphysis from the metaphysis through any layer of the physis disrupting the complete physis; type IV, fracture of the epiphysis extending to and along the physis; type V, fracture that traverses the metaphysis, physis and epiphysis; type VI, Portion of the physis has been removed or is missing.
Figure 11.
(A) Schematic of distal Peterson type 1 physeal injury. (B) Radiographic images of the right knee of a 2-year-old girl with this type of fracture.
Treatment
Conservative and surgical management are valid alternatives for the treatment of these fractures. Choosing between both alternatives depends on factors related to the type of fracture such as its classification, displacement, and associated injuries (1).
Alhammoud et al. (2) showed that there are no significant differences between conservative and surgical treatment in stable fractures. When opting for conservative treatment, a strict, periodic, and close follow-up is essential to observe any displacement that may occur. Stable, undisplaced fractures can be treated conservatively with a long-boot cast (23). Close clinical monitoring should be performed and, if displacement is seen, closed reduction and fixation should be considered (11).
The cast should be applied from the groin region and include the foot. For this, the patient stands on the edge of the table or with a bulge under the sacrum to facilitate the bandage on the groin. An assistant supports the leg with a 45–60˚ hip flexion and 60˚ knee flexion, which will prevent the cast from moving. The distal edge of the cast extends to the base of the toes. The proximal border is just above the greater trochanter on the lateral side and just below the groin on the medial side. If more stability is required, a single-leg spica cast can be used (Fig. 12).
Figure 12.

Photographs of a 3-year-old girl, with a distal femoral fracture, treated with a single-leg hip spica cast, with 15˚ knee flexion.
Surgical treatment includes closed or open reduction, along with stabilization using some type of implant. Most patients are treated with closed reduction and percutaneous fixation using K-wires and are protected with cast immobilization (23). Stabilization with internal fixation is recommended for displaced fractures, including Salter–Harris I or II fractures, even if they have been successfully reduced with closed methods (1). According to Garret et al. (24), the passage of the K-wires through the physis does not contribute to growth arrest, so it is a reliable technique when done correctly.
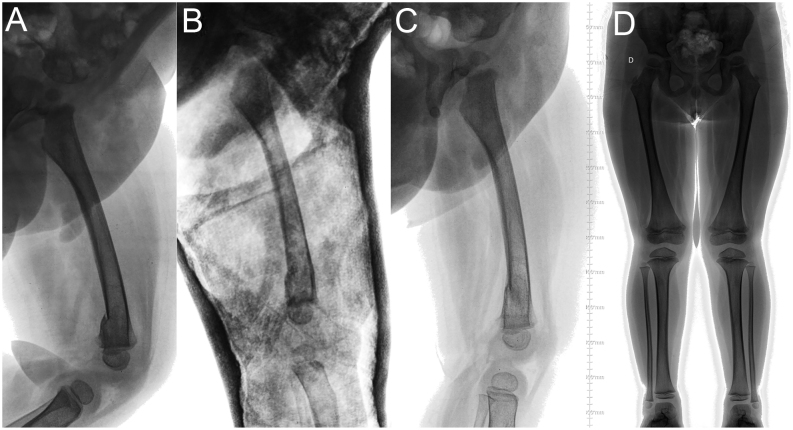
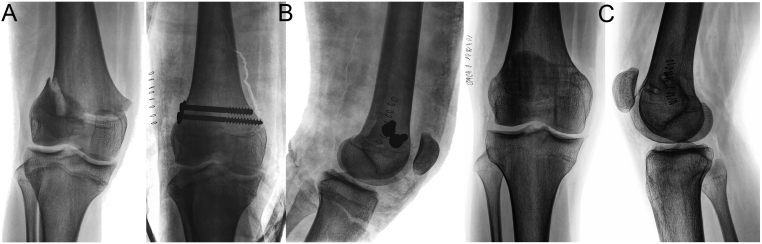
Treatment of undisplaced distal third and undisplaced Salter–Harris type I fractures consists of 2–3 weeks of cast immobilization and weekly follow-up radiographs (Fig. 13).
Figure 13.
(A) Lateral radiographic image of the right femur of a 2-year-old boy, with a distal femoral fracture. (B) Radiographic control at 1 week. (C) Radiographic image after cast removal at 4 weeks. (D) Radiographic images (anteroposterior view) of both legs when standing, after 1 year, with no limb-length discrepancy or axis deviation.
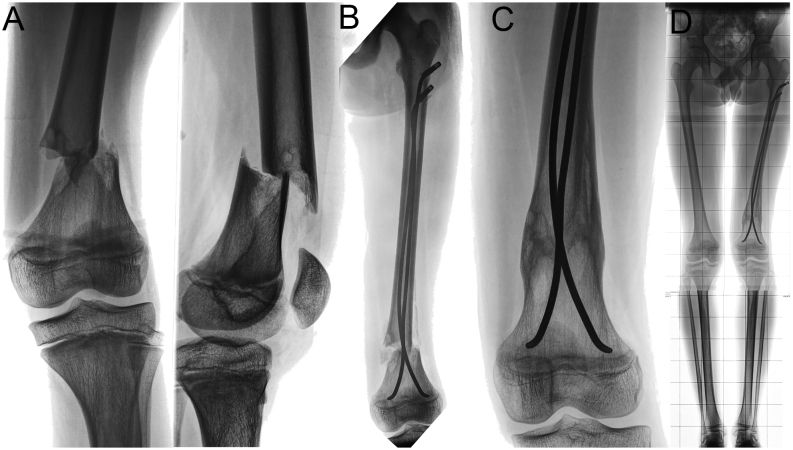
For displaced fractures of the distal third of the femur without physeal compromise, there are several alternatives considering the potential for remodelling in this area, especially given its proximity to the physis. The use of elastic stable intramedullary nailing, plate osteosynthesis, and the use of external fixator is described as definitive management alternatives, each with its advantages and disadvantages. Elastic stable intramedullary nailing is a useful and well-documented technique for the treatment of distal third femur fractures, with retrograde configuration providing the best stability (25). However, its configuration will depend on the proximity of the fracture to the physis, being more frequent the use of an antegrade configuration for the treatment of these cases (Fig. 14). Nails extraction is usually recommended, about a year after the operation. The use of plates in the distal third of the femur is reportedly associated with the possibility of secondary valgus deformity (26). Furthermore, the incision for the surgical approach and the need for an operation to remove the implant makes it unacceptable for most patients’ parents (27). Reduction and stabilization with an external fixator is an option for special cases, given its greater association with malunion, delayed union, refracture, and infection (28).
Figure 14.
(A) Radiographic images of the knee of a 10-year-old boy, with a pathologic bone distal femoral fracture (non-osteogenic fibroma). (B) One-week postoperative radiographic image after closed reduction and anterograde elastic stable endomedular nailing with use of endcaps, maintaining tension for the distal fragment stabilization. (C) Two-month postoperative radiographic images with advance bone healing. (D) The 1-year postoperative radiographic image with no limb length differences or axis deviation.
A displaced Salter–Harris type I lesion can be gently manipulated, by avoiding damage to the physis with traumatic manoeuvres, and fixed percutaneously with K-wires (Fig. 15) (29). Ideally, all reduction manoeuvres should be carried out in a single attempt, demonstrating an association between reduction attempts and the risk of arrest of the physis in other anatomical locations (30). Therefore, it is possible that repeated attempts to reduce the distal femoral physis could cause additional damage to the growth plate. The periosteum interposed at the fracture site is usually the main cause of an irreducible fracture (31).
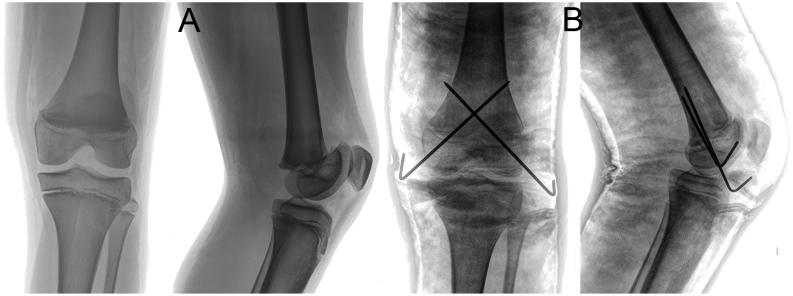
Figure 15.
(A) Radiographic images of the knee of a 13-year-old boy with a distal physeal femoral fracture Salter–Harris type III. (B) Postoperative radiographic images after closed reduction and percutaneous pinning, with two crossed 2.0-mm K-wires and cast protection.
The size of the K-wire is chosen according to the age of the patient and the size of the fragment. In children younger than 5–6 years, 1.6-mm K-wires are used, while in older children, 2.0-mm K-wires are usually used. The entry point, along with the direction of the K-wire, is a key to optimal fixation. For most fractures, two K-wire will provide sufficient stabilization if the K-wires are of the correct size and penetrate two cortices. K-wire osteosynthesis requires additional protection with a cast. Timing of K-wire removal depends on the treating surgeon’s judgement and is based on the patients’ age, injury pattern, and presence or absence of additional injuries. It is highly unlikely that a fracture will displace after 3–4 weeks, so K-wires are usually removed at that time.
Salter–Harris type II lesions are the most common and require a special therapeutic approach (19). In other segments, this type of injury has a low rate of growth alteration; however, in the distal femur, the rate is approximately 58% (32). Hence, parents or legal guardians of the patients should be informed in advance. If the fracture has not been displaced, it can be treated conservatively, immobilizing the limb with a long-leg cast (33). If it is displaced, open or closed reduction is recommended, along with fixation with osteosynthesis. This can be done using screws at the level of the metaphyseal fragment (Fig. 16), or transphyseal K-wires.
Figure 16.
(A) Radiographic images of the knee of a 15-year-old boy with a distal physeal femoral fracture type Salter–Harris II. (B) Postoperative radiographic images after open reduction with periosteal sleeve, screw fixation, and cast protection. (C) Radiographic images after 6 months following screw removal, showing no axis deviation, with physeal closure.
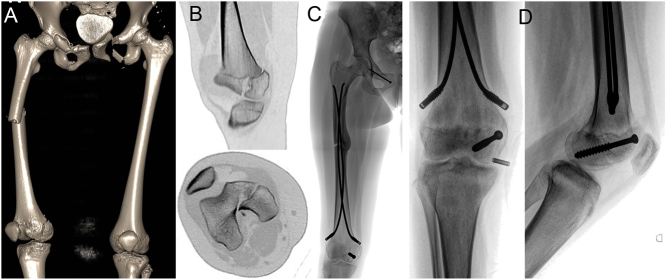
Salter–Harris type III and IV injuries affect the articular surface and therefore require anatomic reduction and fixation. Moreover, CT imaging is recommended, which is useful for surgical planning and to determine the orientation of the screws to be used (Fig. 17) (23). Arthroscopic control of reduction is appropriate for these injuries (Fig. 18). Although the literature is scarce, it shows satisfactory results (34). Fixation of these injuries require subsequent immobilization with a long-leg cast or removable long splint for 3–4 weeks, because fixation alone does not provide sufficient stability in the initial phase of consolidation.
Figure 17.
(A) CT scan reconstruction of lower extremities of a 14-year-old girl with polytrauma. Pelvic unstable injuries, a left femur diaphyseal fracture, and distal femoral fracture are diagnosed. (B) CT scan sagittal and axial views show a displaced physeal femoral fracture type Salter–Harris III. (C) The distal femoral fracture was treated by closed reduction and percutaneous stabilization with a cannulated screw. (D) X-ray of the knee after 6 months, with advanced healing of the fracture.
Figure 18.
(A) Radiographic images of the knee of a 11-year-old girl, with a distal femoral fracture. (B) Coronal and axial CT views show a displaced Salter–Harris type III fracture. (C) Intraoperative images of arthroscopic-assisted closed reduction. (D) Postoperative radiographic images after fixation with cannulated percutaneous screws.
Weight bearing should be avoided for 5–6 weeks, and a rehabilitation programme should be offered. Return-to-sports activities can be considered after 3–4 months.
Complications
Neurovascular complications are rare. A popliteal artery injury would be associated with a hyperextension injury, with anterior displacement of the epiphysis, and the reported incidence is 0–2.6%. Peroneal neuropraxia has a reported incidence of 1–7% and invariably recovers spontaneously (35).
Malunion, infection, recurrent instability, and stiffness of the knee have also been observed. After treatment of the bone injury, residual articular instability should be assessed to rule out ligamentous injury. An MRI should be performed if there is any clinical suspicion after the clinical examination (15).
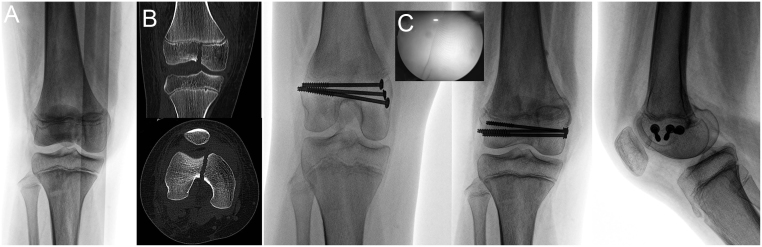
For all physeal fractures of the distal femur, there is a high risk of permanent physeal damage, so long-term follow-up is essential, ideally until the child completes skeletal maturity. Physeal damage can present as a complete or partial premature closure, with a limb length difference (Fig. 19) or an angular deformity (36). This damage usually occurs early, within the first 6 months after the injury; however, it can be evident up to 2 years after the trauma. Its early detection gives the opportunity for early treatment, avoiding more invasive and extensive procedures in the future.
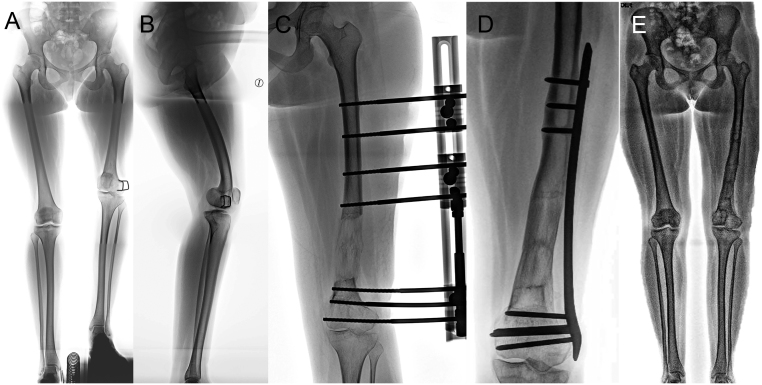
Figure 19.
(A) One year after fracture. Limb-length discrepancy of 1 cm, with no axis deviation. (B) Two years after the fracture. Limb-length discrepancy of 2 cm, with no axis deviation. (C) Epiphysiodesis with percutaneous cannulated screws was performed at age 15 years. (D) Control at 1 month after surgery. (E) Control after 1 year. Final limb-length discrepancy is <1 cm.
The general risk of physeal injury in these fractures is described as approximately 52%, being higher according to the classification of Salter and Harris (2). Another factor that influences the risk of growth disturbances is the degree of displacement. Arkader et al. (11) described an incidence of growth disturbances of 48.8% for displaced fractures, compared with 26.6% in non-displaced ones; however, they were unable to detect a relationship with the magnitude or direction of the displacement.
Gomes and Volpon (37) investigated the evolution of the physeal bars after Salter–Harris IV lesions, at the histological level. They showed that if the transphyseal fracture plane was not surgically closed and stabilized, the vessels invaded the fracture plane and formed a bony bridge across the physis, leading to a growth arrest locus. Therefore, it is essential to achieve an anatomical reduction of these lesions. It is important to note that some physeal bars will form even after anatomic reduction due to germinal layer injury, so explaining this potential complication in advance is critical.
In general, resection of the physeal bar is recommended when it affects <50% of the physis and an adequate growth time remains (at least 2 cm or 2 years) (38). Fat has traditionally been used as an interposition material after bar resection, with polymethylmethacrylate as the alternative. Resection of the physeal bar can lead to incomplete correction, as the injured physis may still stop growing before time (38). If there are deformities or residual length differences or delayed diagnosis, techniques such as guided growth or osteotomies can be used for correction (Fig. 20).
Figure 20.
(A) Radiographic images of both legs (when standing) of a 20-year-old girl with distal femoral fracture sequelae. A 9-cm left femur shortening and 15˚ distal femur varus deformity on the frontal plane were observed. (B) Lateral one-leg standing radiography shows a 20˚ distal femur procurvatum deformity. (C) Acute distal axis correction and gradual lengthening with a monolateral external fixator was performed. (D) After achieving length correction, percutaneous plating. (E) Radiographic images of both legs standing after 6 months of hardware removal.
Conclusions
Distal femur fractures present an important challenge for trauma specialists. Research on the topic and advances in treatments have established principles that are essential to respect, whether we perform conservative or surgical management. If the treatments are timely and adequate, the prognosis is good, which contrasts sharply with inappropriate and delayed management in this type of fracture, wherein no case can be classified as benign because of the anatomy of the physis and its growth rate.
It is very important to educate patients and their families about the possibility of a complication that is not always restricted to deformities. Hence, follow-up until the patient reaches skeletal maturity will always be recommended, and subsequent treatment will depend on the type and degree of complication.
ICMJE Conflict of Interest Statement
M S declares receiving lecture fees from Promedon. All other authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this work.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Acknowledgements
The authors would like to acknowledge the help provided by the Vicerrectoría de Investigación, Desarrollo y Creación Artística, and by the Escuela de Graduados of the Facultad de Medicina, Universidad Austral de Chile in order to publish this work.
References
- 1.Salter RB, Harris WR. Injuries involving the epiphyseal plate. Journal of Bone and Joint Surgery 196345587–622. ( 10.2106/00004623-196345030-00019) [DOI] [Google Scholar]
- 2.Alhammoud A, Younis MH, Ahmed AF, Ibrahim T. Surgical versus nonsurgical treatment of distal femur physeal fractures: a systematic review and meta-analysis. Journal of Musculoskeletal Surgery and Research 20193179–183. ( 10.4103/jmsr.jmsr_53_18) [DOI] [Google Scholar]
- 3.Peterson HA.Part 2. Physeal fractures: anatomic sites. Chapter 18. Distal femur. In Epiphyseal Growth Plate Fractures, pp. 595–640. Berlin, Heidelberg: Springer-Verlag, 2007. ( 10.1007/978-3-540-33802-4) [DOI] [Google Scholar]
- 4.Ogden J.Chapter 21: Femur. In Skeletal Injury in the Child, 3rded., pp.857–928. New York: Springer-Verlag, 2000. ( 10.1007/b97655) [DOI] [Google Scholar]
- 5.Suzuki Y, Matsubayashi J, Ji X, Yamada S, Yoneyama A, Imai H, Matsuda T, Aoyama T, Takakuwa T. Morphogenesis of the femur at different stages of normal human development. PLoS ONE 201914 e0221569. ( 10.1371/journal.pone.0221569) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumgart M, Wiśniewski M, Grzonkowska M, Badura M, Małkowski B, Szpinda M. Quantitative anatomy of the primary ossification center of the femoral shaft in human fetuses. Surgical and Radiologic Anatomy 2017391235–1242. ( 10.1007/s00276-017-1861-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burkus JK, Ganey TM, Ogden JA. Development of the cartilage canals and the secondary center of ossification in the distal chondroepiphysis of the prenatal human femur. Yale Journal of Biology and Medicine 199366193–202. [PMC free article] [PubMed] [Google Scholar]
- 8.Gentili P, Trasimeni A, Giorlandino C. Fetal ossification centers as predictors of gestational age in normal and abnormal pregnancies. Journal of Ultrasound in Medicine 19843193–197. ( 10.7863/jum.1984.3.5.193) [DOI] [PubMed] [Google Scholar]
- 9.Ladenhauf HN, Jones KJ, Potter HG, Nguyen JT, Green DW. Understanding the undulating pattern of the distal femoral growth plate: implications for surgical procedures involving the pediatric knee: a descriptive MRI study. Knee 202027315–323. ( 10.1016/j.knee.2020.02.003) [DOI] [PubMed] [Google Scholar]
- 10.Liu RW, Armstrong DG, Levine AD, Gilmore A, Thompson GH, Cooperman DR. An anatomic study of the distal femoral epiphysis. Journal of Pediatric Orthopedics 201333743–749. ( 10.1097/BPO.0b013e31829d55bf) [DOI] [PubMed] [Google Scholar]
- 11.Arkader A, Warner WC, Jr, Horn BD, Shaw RN, Wells L. Predicting the outcome of physeal fractures of the distal femur. Journal of Pediatric Orthopedics 200727703–708. ( 10.1097/BPO.0b013e3180dca0e5) [DOI] [PubMed] [Google Scholar]
- 12.Engström Z, Wolf O, Hailer YD. Epidemiology of pediatric femur fractures in children: the Swedish Fracture Register. BMC Musculoskeletal Disorders 202021 796. ( 10.1186/s12891-020-03796-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith NC, Parker D, McNicol D. Supracondylar fractures of the femur in children. Journal of Pediatric Orthopedics 200121600–603. ( 10.1097/01241398-200109000-00009) [DOI] [PubMed] [Google Scholar]
- 14.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. Journal of Trauma 197212275–281. ( 10.1097/00005373-197204000-00002) [DOI] [PubMed] [Google Scholar]
- 15.Bailey MEA, Wei R, Bolton S, Richards RH. Paediatric injuries around the knee: bony injuries. Injury 202051611–619. ( 10.1016/j.injury.2019.12.033) [DOI] [PubMed] [Google Scholar]
- 16.Stephens DC, Louis E, Louis DS. Traumatic separation of the distal femoral epiphyseal cartilage plate. Journal of Bone and Joint Surgery: American Volume 1974561383–1390. ( 10.2106/00004623-197456070-00006) [DOI] [PubMed] [Google Scholar]
- 17.Loder RT, O’Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur fractures in children. Journal of Pediatric Orthopedics 200626561–566. ( 10.1097/01.bpo.0000230335.19029.ab) [DOI] [PubMed] [Google Scholar]
- 18.Arkader A, Friedman JE, Warner WC, Jr, Wells L. Complete distal femoral metaphyseal fractures: a harbinger of child abuse before walking age. Journal of Pediatric Orthopedics 200727751–753. ( 10.1097/BPO.0b013e3181558b13) [DOI] [PubMed] [Google Scholar]
- 19.Young EY, Stans AA. Distal femoral physeal fractures. Journal of Knee Surgery 201831486–489. ( 10.1055/s-0038-1627465) [DOI] [PubMed] [Google Scholar]
- 20.Bertin KC, Goble EM. Ligament injuries associated with physeal fractures about the knee. Clinical Orthopaedics and Related Research 1983177188–195. ( 10.1097/00003086-198307000-00029) [DOI] [PubMed] [Google Scholar]
- 21.Gufler H, Schulze CG, Wagner S, Baumbach L. MRI for occult physeal fracture detection in children and adolescents. Acta Radiologica 201354467–472. ( 10.1177/0284185113475606) [DOI] [PubMed] [Google Scholar]
- 22.Peterson HA.Physeal fractures: part 3. Classification. Journal of Pediatric Orthopedics 199414439–448. ( 10.1097/01241398-199407000-00004) [DOI] [PubMed] [Google Scholar]
- 23.Riccio AI, Wilson PL, Wimberly RL. Lower extremity injuries. In Tachdijan’s Pediatric Orthopaedics: from the Texas Scottish Rite Hospital for Children, 5th ed., pp. 1353–1516. Ed Herring JA.Elsevier Health Sciences, 2013. [Google Scholar]
- 24.Garrett BR, Hoffman EB, Carrara H. The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. Journal of Bone and Joint Surgery: British Volume 201193689–694. ( 10.1302/0301-620X.93B5.25422) [DOI] [PubMed] [Google Scholar]
- 25.Hubbard EW, Thompson RM, Jo CH, Pierce WA, Riccio AI, Wimberly RL. Retrograde stainless steel flexible nails have superior resistance to bending in distal third femoral shaft fractures. Journal of Pediatric Orthopedics 201939e258–e263. ( 10.1097/BPO.0000000000001301) [DOI] [PubMed] [Google Scholar]
- 26.Heyworth BE, Hedequist DJ, Nasreddine AY, Stamoulis C, Hresko MT, Yen YM. Distal femoral valgus deformity following plate fixation of pediatric femoral shaft fractures. Journal of Bone and Joint Surgery: American Volume 201395526–533. ( 10.2106/JBJS.K.01190) [DOI] [PubMed] [Google Scholar]
- 27.Li Y, Hedequist DJ. Submuscular plating of pediatric femur fracture. Journal of the American Academy of Orthopaedic Surgeons 201220596–603. ( 10.5435/JAAOS-20-09-596) [DOI] [PubMed] [Google Scholar]
- 28.Kong H, Sabharwal S. External fixation for closed pediatric femoral shaft fractures: where are we now? Clinical Orthopaedics and Related Research 20144723814–3822. ( 10.1007/s11999-014-3554-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah IP, Fernandes JA. Injuries to the distal femur and patella. Surgery 202038554–559. ( 10.1016/j.mpsur.2020.06.014) [DOI] [Google Scholar]
- 30.Leary JT, Handling M, Talerico M, Yong L, Bowe JA. Physeal fractures of the distal tibia: predictive factors of premature physeal closure and growth arrest. Journal of Pediatric Orthopedics 200929356–361. ( 10.1097/BPO.0b013e3181a6bfe8) [DOI] [PubMed] [Google Scholar]
- 31.Gruber HE, Phieffer LS, Wattenbarger JM. Physeal fractures, part II: fate of interposed periosteum in a physeal fracture. Journal of Pediatric Orthopedics 200222710–716. ( 10.1097/01241398-200211000-00003) [DOI] [PubMed] [Google Scholar]
- 32.Basener CJ, Mehlman CT, DiPasquale TG. Growth disturbance after distal femoral growth plate fractures in children: a meta-analysis. Journal of Orthopaedic Trauma 200923663–667. ( 10.1097/BOT.0b013e3181a4f25b) [DOI] [PubMed] [Google Scholar]
- 33.Eid AM, Hafez MA. Traumatic injuries of the distal femoral physis. Retrospective study on 151 cases. Injury 200233251–255. ( 10.1016/s0020-1383(0100109-7) [DOI] [PubMed] [Google Scholar]
- 34.Accadbled F, N’Dele D. Arthroscopic treatment of pediatric fractures. Journal of Pediatric Orthopedics 201838 (Supplement 1) S29–S32. ( 10.1097/BPO.0000000000001163) [DOI] [PubMed] [Google Scholar]
- 35.Duffy S, Gelfer Y, Trompeter A, Clarke A, Monsell F. The clinical features, management options and complications of paediatric femoral fractures. European Journal of Orthopaedic Surgery and Traumatology 202131883–892. ( 10.1007/s00590-021-02933-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cassebaum WH, Patterson AH. Fractures of the distal femoral epiphysis. Clinical Orthopaedics and Related Research 19654179–91. ( 10.1097/00003086-196500410-00009) [DOI] [PubMed] [Google Scholar]
- 37.Gomes LS, Volpon JB. Experimental physeal fracture-separations treated with rigid internal fixation. Journal of Bone and Joint Surgery: American Volume 1993751756–1764. ( 10.2106/00004623-199312000-00004) [DOI] [PubMed] [Google Scholar]
- 38.Khoshhal KI, Kiefer GN. Physeal bridge resection. Journal of the American Academy of Orthopaedic Surgeons 20051347–58. ( 10.5435/00124635-200501000-00007) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a