Abstract
OBJECTIVES:
Calcium administration during cardiac arrest is limited in some circumstances, mainly due to lack of consistent evidence. This study aims to investigate whether calcium therapy administered during cardiac arrest at the Emergency Department is associated with good outcomes, including the probability of return of spontaneous circulation (ROSC), survival to hospital admission, survival to hospital discharge, and favorable neurological outcome at discharge.
METHODS:
We retrospectively reviewed 599 consecutive adult cardiac arrest events between 2016 and 2018. The primary outcome was the ROSC rate. Secondary outcomes included survival to hospital admission, survival to hospital discharge, and favorable neurologic outcome at hospital discharge. Multivariable logistic regression with inverse probability of treatment weighting was analyzed to examine the association between calcium administration and outcomes.
RESULTS:
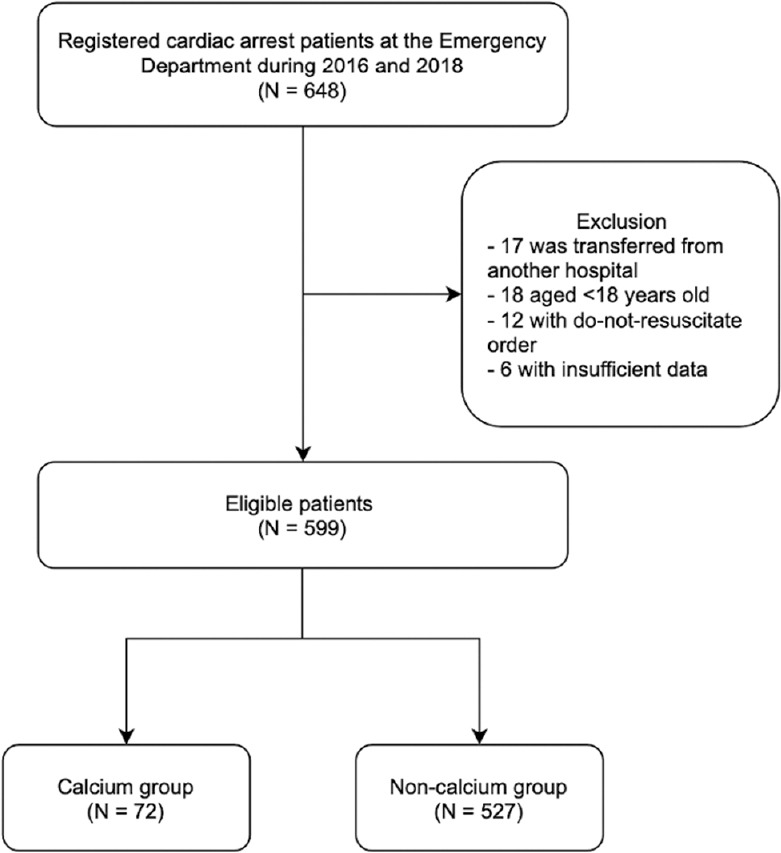
Of 599 events, calcium was administered in 72 (12%) cases. The use of calcium during cardiopulmonary resuscitation (CPR) after adjusting for confounding factors was not associated with any better outcomes, including ROSC (adjusted odds ratio (aOR) 0.53, 95% confidence interval [CI] 0.24–1.17), survival to hospital admission (aOR 1.07, 95% CI 0.47–2.41), survival to hospital discharge (aOR 1.93, 95% CI 0.43–8.56), and favorable neurological outcome (aOR 6.60, 95% CI 0.72–60.74). Besides, calcium use in traumatic cardiac arrest patients was associated with unfavorable outcomes, including ROSC (aOR 0.02, 95% CI 0.00–0.09) and survival to hospital admission (aOR 0.16, 95% CI 0.03–0.84).
CONCLUSION:
The use of calcium during an adult cardiac arrest was not associated with better outcomes. Although associations drawn from this study did not indicate the causality, given calcium during CPR was linked to poorer outcomes in traumatic cardiac arrest patients, including ROSC and survival to hospital admission.
Keywords: Calcium, cardiac arrest, emergency department, outcomes, survival
Box-ED Section
What is already known on the study topic?
Calcium administration during adult cardiac arrest is currently limited in some circumstances.
What is the conflict on the issue? Has it importance for readers?
According to the current guidelines for cardiopulmonary resuscitation (CPR) in 2020, a routine administration of calcium for the treatment of cardiac arrest was not recommended. However, calcium therapy during CPR continues to be used frequently during cardiac arrest.
How is this study structured?
This was a single.center, retrospective cohort study includes data from approximately 600 cardiac arrest patients.
What does this study tell us?
The use of calcium during an adult cardiac arrest was not associated with better outcomes.
Although associations drawn from this study did not indicate the causality, given calcium during CPR was linked to poorer outcomes in traumatic cardiac arrest patients.
Introduction
Cardiac arrest remains one of the most important causes of mortality worldwide. Each year, cardiac arrest accounts for up to 3.7 million lives across the world.[1,2] The role of calcium administration during cardiopulmonary resuscitation (CPR) has been debated for decades.[3] An administration of calcium resulted in a better function of excitation-contraction coupling of ventricular cardiomyocytes.[4] Low serum calcium level has been reported to be associated with the development of cardiac arrest.[5,6] Hypocalcemia, defined by serum calcium of <8.5 mmol/L, causes QT interval prolongation, as a result, torsade de pointes; therefore, hypocalcemia should be aggressively and promptly managed.[7] A previous study found that hypocalcemia is associated with an increased risk of sudden cardiac arrest in dialysis patients.[8] A high ionized calcium level obtained during CPR was associated with an increased likelihood of a return of spontaneous circulation (ROSC), according to a study by Kim and colleagues.[9]
Nonetheless, calcium was removed from the protocols for the treatment of cardiac arrest in 1980 because the benefits of calcium administration during CPR were not demonstrated.[10] Furthermore, administering calcium during CPR may be harmful.[3] The final common pathway of cell death, resulting in cellular necrosis, has been mentioned as cytoplasmic calcium accumulation after calcium administration during CPR.[3] According to the previous systematic review, calcium administration during CPR did not improve survival regardless of the initial rhythm.[5] The current CPR guidelines for 2020 do not recommend routine calcium administration for the treatment of cardiac arrest.[11] Calcium is only recommended for use in certain resuscitation situations, according to the guidelines: Severe hyperkalemia, severe hypocalcemia, severe hypermagnesemia, and calcium channel blockade overdose.[5]
Despite limited recommendations, calcium therapy during CPR is still commonly used. Moskowitz et al. discovered that calcium was used twice as frequently in the United States in 2016 as it was in 2001.[12] Thus, this study investigates whether calcium therapy administered during cardiac arrest at the Emergency Department (ED) associated with good outcomes, including the probability of ROSC, survival to hospital admission, survival to hospital discharge, and favorable neurological outcome.
Methods
The study was prepared and reported in accordance with the strengthening of the reporting of observational studies in epidemiology statement.[13]
Study design and study population
We conducted a retrospective cohort study at Maharaj Nakorn Chiang Mai Hospital, located in the northern of Thailand. Our hospital represents a tertiary care hospital where complicated and severe patients are transferred from other hospitals. We apply the Advanced Cardiac Life Support (ACLS) protocol in our ED as well as other standard best practice guidelines. Our staff, including emergency doctors, nurses, and paramedics, are all required to participate in standard ACLS training courses certified by the Thai Resuscitation Council which is accredited by the American Heart Association (AHA). The administration of calcium in the ED as a part of resuscitation may be due to the fact that calcium is a well-known antidote for treating hyperkalemia, one of the reversible causes of arrest (5Hs and 5Ts). Adult patients (aged ≥18 years) with an index cardiac arrest at the ED, both Out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA), who received chest compressions, were included in this study. OHCA patients were those who received CPR in the field but did not receive ROSC and were transported to the ED. Patients were not eligible if they had a terminal illness or had an advanced care plan. Patients with missing data on calcium administration and resuscitation outcomes were excluded from the main analysis.
Data collection
We extracted clinical information from our cardiac arrest registry between January 2016 and December 2018. Cardiac arrest is defined as a pulselessness that necessitates CPR, which includes chest compression and/or defibrillation. After a structured review of hospital medical records, trained abstractors record registry data. The relevant data were selected and entered into REDcap (Vanderbilt University, Nashville, TN, India) at the same time. Specifically, we collected sex, age, the timing of presenting to the ED, mechanisms of cardiac arrest, types of initial presenting rhythm, a total administered dose of epinephrine, calcium, and bicarbonate, point-of-care-testing glucose, usage of glucose, amiodarone, and lidocaine, blood tests acquired at ED, including calcium and variables parameters known to affect calcium level, such as potassium, bicarbonate, and arterial pH. Blood tests and arterial pH were primarily measured during CPR or not more than 20 min before CPR. Blood tests were measured by the central laboratory and arterial pH was measured by a point-of-care gas analyzer. These results were immediately available at the ED. Since we did not have an ionized calcium level of each patient which represents the biological active calcium level, we use serum calcium obtained during cardiac arrest instead. In addition, calcium use is not a part of routine Emergency Medical Service protocol in Thailand. The Institutional Review Board of the Faculty of Medicine, Chiang Mai University approved the study protocol (IRB No. 7477/2020).
Outcomes
The primary outcome was the ROSC rate, and secondary outcomes included survival to hospital admission, survival to hospital discharge, and favorable neurologic outcome at hospital discharge. Favorable neurological outcome was classified as having a cerebral performance category score of 1 or 2.
Data analysis
We estimated our study size based on prior statistical evidence.[14] A study size of at least 456 patients is required to achieve 80% statistical power and a two-sided alpha error of 0.05. Frequency and percentage were used to describe categorical variables. Mean and standard deviation or median and interquartile range were used for continuous variables, as appropriate. We used standardized differences (STD) to compare the clinical characteristics between the two groups. A value of STD >10% in either direction was regarded as a significant difference and may reflect potential confounding by indication or confounding by contraindication at baseline.[15]
To account for the imbalance in prognostic variables, we employed an inverse probability treatment weighting (IPTW) method.[16] First, we created a multivariable logistic regression model to predict the probability of being prescribed with calcium. The following variables were included in the propensity model: Age, gender, mechanism of cardiac arrest, location of cardiac arrest, the timing of arrival at the ED, initial shockable rhythm, epinephrine administration, bicarbonate administration, lidocaine administration, amiodarone administration, glucose administration, and CPR duration. The model predicted probabilities of being prescribed with calcium were used as treatment weights for the group with calcium administration, whereas the model predicted probabilities of not being prescribed with calcium were used as treatment weights for the group without calcium administration. A balance diagnostic plot to compare the difference in characteristics between weighted and unweighted samples was presented. Variables with an STD of more than 10% after weighting would be adjusted in the weighted logistic regression model for double robustness.[17,18] To evaluate the association between calcium administration during CPR and the occurrence of outcomes, we used a weighted multivariable logistic regression. The logistic model was performed separately for each outcome.
Furthermore, since the Utstein reporting Guidelines recommended reporting those two cardiac arrest settings (OHCA and IHCA) in two different methods,[19,20] we also performed an additional analysis. First, we created an extra model using a multivariable logistic regression model to predict the probability of being prescribed calcium, model 1 for OHCA patients, and model 2 for cardiac arrests at the ED. Notably, the type of cardiac arrest was not included in these models. Variables with an STD of more than 10% after weighting would be adjusted in the weighted logistic regression model for double robustness. To evaluate the association between calcium administration during CPR and the occurrence of outcomes, we used a weighted multivariable logistic regression. The logistic model was performed separately for each outcome and categorized by type of cardiac arrest (OHCA and cardiac arrest at the ED) and mechanism of cardiac arrest (traumatic and nontraumatic cause).
We performed a subgroup analysis by stratifying serum potassium and calcium levels acquired during cardiac arrest into three categories: Low, normal, and high levels, to explore the connection of calcium therapy and its influence on serum potassium and calcium. Normal serum potassium levels were defined as those between 3.5 and 5.5 mmol/L, while normal serum calcium levels were defined as those between 8.5 and 10.2 mg/dL. Stata 16 (StataCorp, College Station, TX, USA) was used to conduct all the analyses. A P < 0.05 was considered statistically significant.
Results
General characteristics
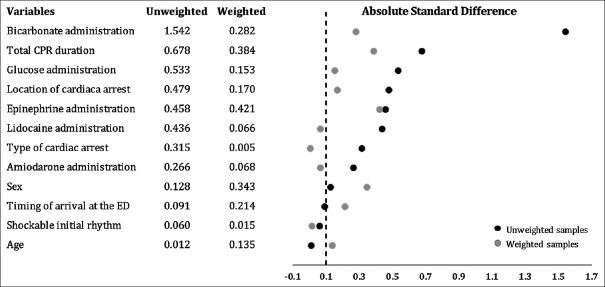
During the study, the cardiac arrest registry recorded a total of 648 cases. Patients transferred from other hospitals (n = 17), under the age of 18 (n = 14), with a do-not-resuscitate order (n = 12), or with insufficient data (n = 6) were all excluded from the study [Figure 1]. Finally, 599 patients were participated in this study. There were 374 men (62.4%), and the average age was 57.8 years. The overall ROSC, survival to hospital admission, survival to hospital discharge, and favorable neurological outcome rates in this study were 66.3%, 52.4%, 15.1%, and 7.0%, respectively. Almost all baseline characteristics were different between the two groups except for age, time on arrival at the ED, and initial presenting rhythm [Table 1]. The most different characteristic across the two groups was the administration of bicarbonate (STD + 1.536). Most of the mechanisms of cardiac arrest was nontrauma (70.1%) and out-of-hospital (61.8%). Total CPR duration was longer in the calcium group (STD + 0.678). The calcium group had a higher potassium level (STD + 0.677), whereas the noncalcium group had a higher bicarbonate and arterial pH level (STD-0.329 and-0.264, respectively).
Figure 1.
Study flowchart
Table 1.
Characteristics of patients included in this study
| Variables | Total (n=599) | Calcium (n=72) | Noncalcium (n=527) | STD (%) |
|---|---|---|---|---|
| Age (years), mean±SD | 57.8±21.3 | 57.6±19.4 | 57.9±21.6 | −0.012 |
| Sex – male, n (%) | 374 (62.4) | 41 (56.9) | 333 (63.2) | −0.127 |
| Time on arrival, n (%) | ||||
| Day (8.01-16.00) | 206 (34.4) | 27 (37.5) | 179 (34.0) | +0.090 |
| Evening (16.01-24.00) | 172 (28.7) | 21 (29.2) | 151 (28.7) | |
| Night (0.01-8.00) | 221 (36.9) | 24 (33.3) | 197 (37.4) | |
| Mechanism of cardiac arrest, n (%) | ||||
| Trauma | 179 (29.9) | 13 (18.1) | 166 (31.5) | −0.314 |
| Nontrauma | 420 (70.1) | 59 (81.9) | 361 (68.5) | |
| Location of cardiac arrest, n (%) | ||||
| Out-of-hospital | 370 (61.8) | 58 (80.6) | 312 (59.2) | +0.477 |
| Emergency department | 229 (38.2) | 14 (19.4) | 215 (40.8) | |
| Shockable initial presenting rhythm, n (%) | 68 (11.4) | 7 (9.7) | 61 (11.6) | −0.060 |
| Total CPR duration (min), median (IQR) | 12 (5-28) | 28 (13-32) | 10 (4-23) | +0.678 |
| Received epinephrine during CPR, n (%) | 549 (91.7) | 72 (100.0) | 477 (90.5) | +0.457 |
| Total administered dose of adrenaline (mg), median (IQR) | 3 (1-7) | 7 (4-8.5) | 2 (1-6) | +0.912 |
| Received bicarbonate during CPR, n (%) | 196 (32.7) | 62 (86.1) | 134 (25.4) | +1.536 |
| Received glucose during CPR, n (%) | 68 (11.4) | 21 (29.2) | 47 (8.9) | +0.530 |
| Received amiodarone during CPR, n (%) | 54 (9.0) | 12 (16.7) | 42 (8.0) | +0.265 |
| Received lidocaine during CPR, n (%) | 22 (3.7) | 10 (13.9) | 12 (2.3) | +0.433 |
| Serum calcium level (mg/dL), mean±SD | 8.1±1.6 | 8.4±2.2 | 8.1±1.5 | +0.164 |
| Serum potassium level (mmol/L), mean±SD | 4.6±1.6 | 5.9±2.7 | 4.5±1.3 | +0.677 |
| Serum bicarbonate level (mmol/L), mean±SD | 15.3±6.5 | 13.4±6.2 | 15.5±6.5 | −0.329 |
| Serum arterial pH, mean±SD | 7.03±0.24 | 6.97±0.26 | 7.03±0.24 | −0.264 |
CPR: Cardiopulmonary resuscitation, IQR: Interquartile range, SD: Standard deviation, STD: Standardized difference
Primary and secondary outcomes
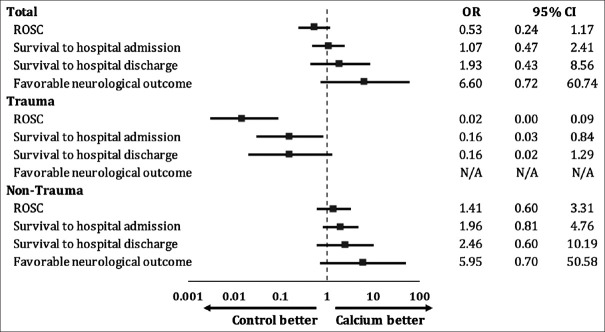
Figure 2 shows the absolute STD between unmatched and matched samples. Most variables before matching were not well-balanced. After adjusting by the IPTW method, several factors have been still unbalanced (absolute STD >0.1). However, all these variables were included in the multivariable analysis.
Figure 2.
Balance in prognostic factors at baseline based on absolute standardized difference in the unweighted and weighted samples. CPR: Cardiopulmonary resuscitation, ED: Emergency department
Figure 3 demonstrates odds ratio of each outcome classified by mechanisms of cardiac arrest. Calcium administration during cardiac arrest was not associated with any better outcomes. For a traumatic cardiac arrest, giving calcium might decrease the chance of ROSC (P < 0.001) and survival to hospital admission (P = 0.03). Table 2 summarizes the outcomes following a cardiac arrest based on serum potassium and serum calcium levels.
Figure 3.
Weighted multivariable logistic regression analysis separated by outcomes and stratified by mechanism of cardiac arrest. CI: Confidence interval, N/A: not applicable, OR: Odds ratio, ROSC: Return of spontaneous circulation
Table 2.
Outcomes after cardiac arrest stratified by serum potassium and serum calcium levels
| Total | Calcium | Noncalcium | P | |
|---|---|---|---|---|
| Patients with serum potassium level <3.5 mmol/L | ||||
| ROSC (n=103) | 84 (81.6) | 7 (87.5) | 77 (81.1) | 0.65 |
| Survival to hospital admission (n=103) | 60 (58.3) | 6 (75.0) | 54 (56.8) | 0.32 |
| Survival to hospital discharge (n=100) | 22 (22.0) | 2 (25.0) | 20 (21.7) | 0.83 |
| Favorable neurological outcome (n=99) | 9 (9.1) | 1 (12.5) | 8 (8.8) | 0.73 |
| Patients with serum potassium level between 3.5 and 5.5 mmol/L | ||||
| ROSC (n=248) | 205 (82.7) | 6 (40.0) | 199 (85.4) | <0.001 |
| Survival to hospital admission (n=246) | 136 (55.3) | 4 (26.7) | 132 (57.1) | 0.02 |
| Survival to hospital discharge (n=240) | 52 (21.7) | 3 (20.0) | 49 (21.8) | 0.87 |
| Favorable neurological outcome (n=235) | 25 (10.6) | 2 (13.3) | 23 (10.5) | 0.73 |
| Patients with serum potassium level >5.5 mmol/L | ||||
| ROSC (n=248) | 108 (43.5) | 18 (36.7) | 90 (45.2) | 0.28 |
| Survival to hospital admission (n=248) | 46 (18.5) | 5 (10.2) | 41 (20.6) | 0.09 |
| Survival to hospital discharge (n=243) | 14 (5.8) | 2 (4.1) | 12 (6.2) | 0.57 |
| Favorable neurological outcome (n=238) | 6 (2.5) | 0 | 6 (3.1) | 0.22 |
| Patients with serum calcium level <8.5 mg/dL | ||||
| ROSC (n=265) | 216 (81.5) | 13 (65.0) | 203 (82.9) | 0.05 |
| Survival to hospital admission (n=264) | 131 (49.6) | 6 (30.0) | 125 (51.2) | 0.07 |
| Survival to hospital discharge (n=252) | 45 (17.9) | 2 (10.0) | 43 (18.5) | 0.34 |
| Favorable neurological outcome (n=247) | 21 (8.5) | 0 | 21 (9.2) | 0.17 |
| Patients with serum calcium level between 8.5 and 10.2 mg/dL | ||||
| ROSC (n=163) | 138 (84.7) | 12 (66.7) | 126 (86.9) | 0.03 |
| Survival to hospital admission (n=162) | 100 (61.7) | 8 (44.4) | 92 (63.9) | 0.11 |
| Survival to hospital discharge (n=161) | 40 (24.8) | 5 (27.8) | 35 (24.5) | 0.76 |
| Favorable neurological outcome (n=155) | 17 (11.0) | 3 (17.6) | 14 (10.1) | 0.35 |
| Patients with serum calcium level >10.2 mg/dL | ||||
| ROSC (n=171) | 43 (25.1) | 6 (17.6) | 37 (27.0) | 0.26 |
| Survival to hospital admission (n=171) | 11 (6.4) | 1 (2.9) | 10 (7.3) | 0.35 |
| Survival to hospital discharge (n=170) | 3 (1.8) | 0 | 3 (2.2) | 0.38 |
| Favorable neurological outcome (n=170) | 2 (1.2) | 0 | 2 (1.5) | 0.48 |
ROSC: Return of spontaneous circulation
In addition, the administration of calcium during CPR was not associated with good outcomes across OHCA and cardiac arrest at the ED. The details of each outcome categorized by type of cardiac arrest and mechanism of cardiac arrest are summarized in Table S1 in the Supplementary Data.
Table S1.
Weighted multivariable logistic regression analysis stratified by outcomes and categorized by type of cardiac arrest (out-of-hospital cardiac arrest and cardiac arrest at the emergency department) and mechanism of cardiac arrest (traumatic and nontraumatic cause)
| Total study population | Presumed traumatic cause | Presumed nontraumatic cause | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| mOR | 95% CI | mOR | 95% CI | mOR | 95% CI | ||||
| Model 1: Out-of-hospital cardiac arrest (n=370) | |||||||||
| ROSC | 0.53 | 0.20 | 1.41 | 0.01 | 0.00 | 0.12 | 2.42 | 0.94 | 6.22 |
| Survival to hospital admission | 1.53 | 0.53 | 4.40 | 0.36 | 0.40 | 3.19 | 3.86 | 1.22 | 12.22 |
| Survival to hospital discharge | 0.99 | 0.33 | 3.00 | 0.49 | 0.42 | 5.77 | 1.49 | 0.40 | 5.53 |
| Favorable neurological outcomes | 0.73 | 0.11 | 4.71 | N/A | N/A | N/A | 0.63 | 0.79 | 5.16 |
| Model 2: Cardiac arrest at the emergency department (n=229) | |||||||||
| ROSC | 0.58 | 0.17 | 197 | N/A | N/A | N/A | 0.52 | 0.12 | 2.23 |
| Survival to hospital admission | 0.82 | 0.22 | 3.07 | N/A | N/A | N/A | 1.29 | 0.27 | 6.19 |
| Survival to hospital discharge | 3.66 | 0.39 | 34.22 | N/A | N/A | N/A | 5.15 | 0.58 | 45.53 |
| Favorable neurological outcomes | 22.68 | 0.86 | 600.12 | N/A | N/A | N/A | 22.12 | 1.19 | 409.84 |
CI: Confidence interval, mOR: Multivariable odds ratio, N/A: Not applicable, ROSC: Return of spontaneous circulation
Discussion
This study documents 599 consecutive adults. Seventy-two (12%) were given calcium during resuscitation at the ED. Calcium administration during cardiac arrest was not associated with a better chance of ROSC. Besides, calcium therapy administered during a traumatic cardiac arrest was associated with unfavorable outcomes. Moreover, giving calcium during resuscitation in patients with hypocalcemia may decrease the chances of ROSC.
Previous research found that calcium administration during CPR may benefit some groups of patients with asystole and pulseless electrical activity;[21,22] however, subsequent studies of calcium administration during resuscitation found no benefits and may be detrimental.[3] Consequently, the AHA has recommended that calcium be used only in specific resuscitation situations.[23] Van Walraven et al. reported the association of calcium administration during CPR with a decreased survival at 1 h at ED among 773 adult IHCAs (adjusted odds ratio [aOR] 0.32, 95% confidence interval [CI] 0.18–0.55).[14]
Furthermore, calcium uses in patients with serum potassium levels >5.5 mmol/L was not associated with improved outcomes. Wang et al., on the other hand, discovered that giving calcium and sodium bicarbonate to patients with hyperkalemia during cardiac arrest may be beneficial.[24] The main distinction is that Wang et al. only studied IHCA, whereas our study included both OHCA and IHCA. Besides, CPR duration has been shown to be an independent predictor for the resuscitation outcomes.[25] Wang et al. did not demonstrate the CPR duration in each group whereas our study found that patients with cardiac arrest who received calcium had more CPR duration compared to the control group. It should be imperative that the mortality rate from cardiac arrest rises dramatically over time. As a result, the fact that calcium was given while CPR was being performed could influence the results of our study.
Interestingly, calcium administered during CPR in traumatic cardiac arrest was associated with significantly decreased ROSC (aOR 0.02, 95% CI 0.00–0.09) and survival to hospital admission (aOR 0.16, 95% CI 0.03–0.84). Major traumatic patients who received calcium replacement during resuscitation had a higher in-hospital mortality (P < 0.05), which was consistent with Cornelius et al.[26] Recently, trends in the management of severely traumatic patients have recommended implementing a massive transfusion protocol, which has the unintended consequence of worsening hypocalcemia.[26] However, current international guidelines for calcium replacement in major traumatic patients and massive transfusion are limited.[27] Despite the increased risk of mortality associated with hypocalcemia is well documented,[28] the use of calcium therapy in improving these outcomes is debatable.[26] As a result, this study may provide some insight into the use of calcium in trauma patients.
This study provides some important implications. Despite earlier evidence demonstrated that the rate of use of calcium has increased over time[12], our study revealed the difference. The rate of calcium administration in our study was only 12%. This study also demonstrated that calcium administration during cardiac arrest without certain indications is associated with unfavorable outcomes, possibly because of effects of reperfusion injury to the ischemic heart, brain, and other vital organs mediated by calcium.[29]
Limitations
This study has some limitations since it is retrospective. First, the study design resulted in a lack of explicit documentation of the specific indications for calcium use during CPR. The reasons for calcium administration could have provided further evidence for the influence of calcium on outcomes. Second, this study did not collect the time in which calcium was administered during CPR. Since the outcomes of CPR were mainly influenced by the CPR duration, it might not be concluded that calcium administration is solely associated with unfavorable outcomes. However, we have attempted to minimize these biases by using inverse probability weighting with double adjustment. Further study should also focus on the timing and dosage of calcium administration as it corresponds to the outcomes. Furthermore, our study did not address the calcium dose given to patients. Finally, despite the use of appropriate analytical methods, it is possible that the existing data from our registry did not capture other unmeasured confounders of outcomes. As a result, the observed associations between calcium use and unfavorable outcomes may not be causal, and the possibility that calcium is used more frequently in cardiac arrest patients with a lower chance of survival cannot be ruled out.
Conclusion
Calcium administration during adult cardiac arrest is not associated with better resuscitation outcomes. Although the findings of this study do not prove causation, calcium administration during CPR is associated with poorer outcomes in traumatic cardiac arrest patients, including ROSC and survival to hospital admission. Further research should concentrate on specific situations where calcium supplementation is beneficial.
Author contributions statement
Authorship provides credit for a researcher's contributions to a study and carries accountability. Authors are expected to fulfill the criteria below:
Wachira Wongtanasarasin: Conceptualization, Methodology, Validation, Formal analysis, Resources, Writing – Original draft, Writing – Review & Editing, Visualization, Supervision, Funding acquisition
Nat Ungrungseesopon: Conceptualization, Methodology, Investigation, Formal analysis, Writing – Original draft, Writing - Review & Editing
Nutthida Namsongwong: Conceptualization, Methodology, Investigation, Writing – Original draft, Writing - Review & Editing
Pongsatorn Chotipongkul: Conceptualization, Methodology, Investigation, Writing – Original draft, Writing - Review & Editing
Onwara Visavakul: Conceptualization, Methodology, Investigation, Writing – Original draft, Writing - Review & Editing
Napatsakorn Banping: Conceptualization, Investigation, Writing - Review & Editing
Worapot Kampeera: Conceptualization, Investigation, Writing - Review & Editing
Phichayut Phinyo: Conceptualization, Methodology, Validation, Formal analysis, Data curation, Writing - Review & Editing.
Abstract was presented virtually at the European Emergency Medicine Congress 2021 between 28-31 October 2021 at Lisbon, Portugal.
Conflicts of interest
None Declared.
Ethical approval
This study protocol was approved by the Institutional Review Board of the Faculty of Medicine, Chiang Mai University (IRB No. 7477/2020).
Consent to participate
Not applicable.
Financial support and sponsorship
We received funding from Faculty of Medicine, Chiang Mai University (No. 7477/2020).
Acknowledgment
The authors gratefully acknowledge Ms. Thanchanok Srisawang for an elaborative language editing on our manuscript.
References
- 1.Kudenchuk PJ, Sandroni C, Drinhaus HR, Böttiger BW, Cariou A, Sunde K, et al. Breakthrough in cardiac arrest: Reports from the 4th Paris International Conference. Ann Intensive Care. 2015;5:22. doi: 10.1186/s13613-015-0064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, et al. Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131:1415–25. doi: 10.1161/CIRCULATIONAHA.114.014542. [DOI] [PubMed] [Google Scholar]
- 3.Srinivasan V, Morris MC, Helfaer MA, Berg RA, Nadkarni VM, Association AH. Calcium use during in-hospital pediatric cardiopulmonary resuscitation: A report from the National Registry of Cardiopulmonary Resuscitation. Pediatrics. 2008;121:E1144–51. doi: 10.1542/peds.2007-1555. [DOI] [PubMed] [Google Scholar]
- 4.Yarmohammadi H, Uy-Evanado A, Reinier K, Rusinaru C, Chugh H, Jui J, et al. Serum calcium and risk of sudden cardiac arrest in the general population. Mayo Clin Proc. 2017;92:1479–85. doi: 10.1016/j.mayocp.2017.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kette F, Ghuman J, Parr M. Calcium administration during cardiac arrest: A systematic review. Eur J Emerg Med. 2013;20:72–8. doi: 10.1097/MEJ.0b013e328358e336. [DOI] [PubMed] [Google Scholar]
- 6.Landry A, Foran M, Koyfman A. Does calcium administration during cardiopulmonary resuscitation improve survival for patients in cardiac arrest? Ann Emerg Med. 2014;64:187–9. doi: 10.1016/j.annemergmed.2013.07.510. [DOI] [PubMed] [Google Scholar]
- 7.American Heart Association. Part 10.1: Life-threatening electrolyte abnormalities. Circulation. 2005;112(Suppl 24):121–5. [Google Scholar]
- 8.Pun PH, Abdalla S, Block GA, Chertow GM, Correa-Rotter R, Dehmel B, et al. Cinacalcet, dialysate calcium concentration, and cardiovascular events in the EVOLVE trial. Hemodial Int. 2016;20:421–31. doi: 10.1111/hdi.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SJ, Kim HS, Hwang SO, Jung WJ, Roh YI, Cha KC, et al. Ionized calcium level at emergency department arrival is associated with return of spontaneous circulation in out-of-hospital cardiac arrest. PLoS One. 2020;15:e0240420. doi: 10.1371/journal.pone.0240420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Current Standards and Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC) JAMA. 1980;244:453–509. [PubMed] [Google Scholar]
- 11.Duff PJ, Panchal AR, Hazinski MF. Highlights of the 2018 Focused Updates to the American Heart Association Guidelines for CPR and ECC: Advanced Cardiovascular Life Support and Pediatric Advanced Life Support. American Heart Association. 2018. [Last accessed on 2020 Jun 30]. Available from: https://eccguidelines.heart.org/wp-content/uploads/2018/10/2018-Focused-Updates_Highlights.pdf .
- 12.Moskowitz A, Ross CE, Andersen LW, Grossestreuer AV, Berg KM, Donnino MW, et al. Trends over time in drug administration during adult in-hospital cardiac arrest. Crit Care Med. 2019;47:194–200. doi: 10.1097/CCM.0000000000003506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gharaibeh A, Koppikar S, Bonilla-Escobar FJ. Strengthening the reporting of observational studies in epidemiology (STROBE) in the International Journal of Medical Students. Int J Med Stud. 2014;2:36–37. [Google Scholar]
- 14.van Walraven C, Stiell IG, Wells GA, Hébert PC, Vandemheen K. Do advanced cardiac life support drugs increase resuscitation rates from in-hospital cardiac arrest? The OTAC Study Group. Ann Emerg Med. 1998;32:544–53. doi: 10.1016/s0196-0644(98)70031-9. [DOI] [PubMed] [Google Scholar]
- 15.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34:3661–79. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X, Shen C. Doubly robust estimation of causal effect: Upping the odds of getting the right answers. Circ Cardiovasc Qual Outcomes. 2020;13:e006065. doi: 10.1161/CIRCOUTCOMES.119.006065. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen TL, Collins GS, Spence J, Daurès JP, Devereaux PJ, Landais P, et al. Double-adjustment in propensity score matching analysis: choosing a threshold for considering residual imbalance. BMC Med Res Methodol. 2017;17:78. doi: 10.1186/s12874-017-0338-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nolan JP, Berg RA, Andersen LW, Bhanji F, Chan PS, Donnino MW, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the utstein resuscitation registry template for in-hospital cardiac arrest. Circulation. 2019;140:e746–57. doi: 10.1161/CIR.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 20.Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the international liaison committee. Circulation. 2015;132:1286–300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 21.Stueven HA, Thompson B, Aprahamian C, Tonsfeldt DJ, Kastenson EH. The effectiveness of calcium chloride in refractory electromechanical dissociation. Ann Emerg Med. 1985;14:626–9. doi: 10.1016/s0196-0644(85)80874-x. [DOI] [PubMed] [Google Scholar]
- 22.Harrison FE, Amey BD. The use of calcium in cardiac resuscitation. Am J Emerg Med. 1983;1:267–73. doi: 10.1016/0735-6757(83)90103-1. [DOI] [PubMed] [Google Scholar]
- 23.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16 Suppl 2):S366–468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 24.Wang CH, Huang CH, Chang WT, Tsai MS, Yu PH, Wu YW, et al. The effects of calcium and sodium bicarbonate on severe hyperkalaemia during cardiopulmonary resuscitation: A retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation. 2016;98:105–11. doi: 10.1016/j.resuscitation.2015.09.384. [DOI] [PubMed] [Google Scholar]
- 25.Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85:987–92. doi: 10.1016/j.resuscitation.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Cornelius B, Ferrell E, Kilgore P, Cox R, Golden R, Cvek U, et al. Incidence of hypocalcemia and role of calcium replacement in major trauma patients requiring operative intervention. AANA J. 2020;88:383–9. [PubMed] [Google Scholar]
- 27.Giancarelli A, Birrer KL, Alban RF, Hobbs BP, Liu-DeRyke X. Hypocalcemia in trauma patients receiving massive transfusion. J Surg Res. 2016;202:182–7. doi: 10.1016/j.jss.2015.12.036. [DOI] [PubMed] [Google Scholar]
- 28.Mackay EJ, Stubna MD, Holena DN, Reilly PM, Seamon MJ, Smith BP, et al. Abnormal calcium levels during trauma resuscitation are associated with increased mortality, increased blood product use, and greater hospital resource consumption: A pilot investigation. Anesth Analg. 2017;125:895–901. doi: 10.1213/ANE.0000000000002312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wongtanasarasin W, Siri-Angkul N, Wittayachamnankul B, Chattipakorn SC, Chattipakorn N. Mitochondrial dysfunction in fatal ventricular arrhythmias. Acta Physiol (Oxf) 2021;231:e13624. doi: 10.1111/apha.13624. [DOI] [PubMed] [Google Scholar]