Highlights
-
•
News sources are central in predicting college students’ COVID-19 vaccine hesitancy.
-
•
Conservative political ideology promotes the consumption of right wing media.
-
•
Right wing media consumption is associated with COVID-19 vaccine hesitancy.
-
•
Gender indirectly affects hesitancy through political ideology and news consumption.
Keywords: COVID-19, Vaccine hesitancy, Media, Right wing media, Misinformation, College students
Abbreviations: SEM, Structural Equation Modeling; KABB, Knowledge, Attitudes, Beliefs & Behaviors
Abstract
COVID-19 vaccine hesitancy is context specific and highly dynamic in the United States. The objective of this study was to examine the underlying causes of COVID-19 vaccine use and hesitancy among students at two colleges in Central New York (USA) in order to better understand how to promote vaccination in this demographic. A Knowledge, Attitudes, Beliefs & Behaviors survey was designed to measure the relationship between gender, political ideology, media consumption, beliefs, mental health and anxiety, and pandemic-related behaviors. The survey was distributed by email to students in April 2021. Of 8,894 eligible respondents, 627 students completed the survey. Structural Equation Modeling was utilized to explore both direct and indirect relationships. Modeling suggests that the effect of political ideology (being more conservative) is to promote the consumption of right wing news, which in turn tends to increase vaccine hesitancy. Conservative political ideology does not directly lead to vaccine hesitancy, but it does encourage the consumption of news from sources that promote fear and hesitation about the vaccines. News sources significantly contribute to vaccine attitudes among this demographic.
1. Introduction
The coronavirus vaccines authorized for use in the United States remain effective at preventing hospitalization and death from COVID-19, despite the emergence of variants of concern such as B.1.617 (Delta) and B.1.1.529 (Omicron). Nevertheless, over a year after vaccines were first made available to adults, Americans who remain hesitant about vaccination are disproportionately younger, less educated, and more politically conservative (Hamel et al., 2022). According to the SAGE Working Group on Vaccine Hesitancy, vaccine hesitancy refers to the “delay in acceptance or refusal of vaccination despite availability of vaccination services,” shaped strongly by complacency, convenience, and confidence (MacDonald, 2015). As preventable COVID-19 deaths continue to rise, understanding and addressing vaccine hesitancy is a pressing public health issue.
COVID-19 vaccine hesitancy is context specific and highly dynamic (Daly et al., 2021, Fridman et al., 2021). Analysis of the US Census Bureau’s Household Pulse data (n=459,235) collected between January and March 2021 identified low income, low education, young age, and Republican political leaning as factors predicting vaccine hesitancy (Tram et al., 2021). The authors distinguished between degrees of hesitancy, as women and Black Americans were more likely to be reluctant and “deliberative,” while others firmly rejected the vaccine based on “dissent” and “distrust.” Additional literature has identified rural residents and younger male Republicans as groups likely to refuse vaccination (Fisher et al., 2020, KFF COVID-19 Vaccine Monitor, 2021, Kirzinger et al., 2021a). Gender differences demand further research; while some studies have indicated women are more hesitant (Galasso et al., 2021, Kricorian et al., 2021), others have produced conflicting results regarding levels of and reasons for hesitancy among women and men (KFF COVID-19 Vaccine Monitor, 2021, Liu and Li, 2021, Willis et al., 2021). There are also racial differences in COVID-19 vaccine hesitancy. A national survey of 1,878 participants in June 2020 noted that hesitancy was highest among African Americans and Hispanics, as well as those with children at home, rural residents, those who identified as Republican, and those with lower levels of education and income (Khubchandani et al., 2021). Gaps in booster dose uptake continue to mirror these trends (Hamel et al., 2022).
Literature suggests that concerns around safety and side effects, effectiveness, the vaccine’s novelty, and the amount of information published on the vaccine contribute to hesitancy, as does distrust for vaccines and/or the government more broadly (Allen et al., 2021, King et al., 2021, Kirzinger et al., 2021b).
1.1. Political partisanship and vaccine hesitancy
The Kaiser Family Foundation (KFF) has stated that one of the largest remaining gaps in vaccination rates is by partisanship; 91% of Democrats are vaccinated, compared to 76% of independents and 63% of Republicans (Hamel et al., 2022). Literature frequently alludes to this association between COVID-19 vaccine hesitancy and political affiliation, however, the mechanism to explain hesitancy among Republicans is not well defined.
Liu and Li (2021) presented survey data from 443,680 individuals between January and March 2021, showing a strong correlation between state partisanship and vaccine hesitancy. States with more votes for Donald Trump relative to Joe Biden in the 2020 presidential election had a significantly higher mean level of COVID-19 vaccine hesitancy over three dimensions: confidence, circumspection, and complacency. Allington et al. (2021) also revealed a negative association between vaccination intent and having voted for Donald Trump in 2016. A cross-sectional study conducted among college students concluded that a Republican political affiliation was significantly associated with vaccine hesitancy (Sharma et al., 2021). Cowan et al. (2021) found that this partisan divide grew over time between November 2020 and February 2021, and by 2021, it could no longer be explained by personal characteristics or trust in the government. The authors instead discuss party affiliation as a source of identity that strongly guides COVID-19 decision-making.
1.2. Vaccine hesitancy and misinformation among young adults
Particular attention has been paid to reluctance among young adults who may view themselves at a lower risk of severe illness (Adams et al., 2021, Baack et al., 2021). A “wait and see” mentality is common among this population due to concerns about the safety of the vaccine, as well as its side effects (Adams et al., 2021, Berenson et al., 2021). Reports of myocarditis disproportionately impacting younger adults may contribute to these concerns (Gargano et al., 2021). Young adults have also been particularly vulnerable to stress, anxiety, and depression during the pandemic (Varma et al., 2021) and are more likely than other age groups to be uninsured (Conway, 2020). Many work low-wage jobs without paid sick leave, and when already reluctant, these barriers may enhance hesitancy.
As frequent users of social media, young adults are vulnerable to health misinformation, which has strongly contributed to the decline in vaccination rates since the initial vaccine rollout in January – April 2021 (Allington et al., 2021, Muric et al., 2021, Xiang and Lehmann, 2021). The COVID States Project revealed that 25–44-year-olds were most likely to believe COVID-19 misinformation, followed by 18–24-year-olds. Americans 65 + were the least likely group. Political differences were also highlighted; “25% of Republicans held misperceptions compared to 17%–19% among other groups” (Ognyanova et al., 2021).
In July 2021, a Surgeon General’s Advisory warned the public of the threat of vaccine misinformation, reporting that, “As of late May, 67% of unvaccinated adults had heard at least one COVID-19 vaccine myth and either believed it to be true or were not sure of its veracity” (Murthy, 2021). The advisory also revealed that false news stories were 70% more likely to be shared than stories that were true (Murthy, 2021). From infertility to DNA alteration, misinformation on social media platforms “cause confusion, sow mistrust, and undermine public health efforts” U.S. Surgeon General Dr. Vivek Murthy stated.
1.3. Role of right wing media
In the United States, studies have shown that misinformed COVID-19 beliefs are strongly associated with exposure to right wing, or conservative news media (Borah et al., 2022, Dhawan et al., 2021, Fridman et al., 2021, Jamieson and Albarracín, 2020, Motta et al., 2020, Pinna et al., 2021). This misinformation has significant consequences on viewer’s health behaviors. One national survey from June 2020 found that Fox News viewers (57.3%) had less intent to vaccinate than CNN/MSNBC viewers (76.4%) (Ruiz and Bell, 2021), a finding congruent with Viswanath et al. (2021). A year later, Pinna et al. (2021) revealed that higher local viewership of Fox News did in fact lead to lower local vaccination rates, an effect the authors argue was driven by younger individuals. Romer and Jamieson (2021) also report that though conservative media viewers supported vaccination and trusted the Centers for Disease Control and Prevention at the beginning of the pandemic, continued exposure to these media sources reduced support and trust overtime.
Evidence suggests right wing media sources utilize messaging that highlights the risks of the vaccine while downplaying the risks of the virus (Fridman et al., 2021, Hsu, 2021) and enhances belief in conspiracies (Romer and Jamieson, 2021). Media Matters documented that from June 28 through July 11, 2021, 57% of Fox News segments about coronavirus vaccines included claims that undermined vaccination efforts (Monroe and Savillo, 2021). Even early in the pandemic, Fox News was more likely to discuss drug treatments, whereas CNN was more likely to discuss testing and vaccines (Muddiman et al., 2020). Misinformation that promotes fear and hesitation about the vaccine is a major public health threat, as communities with lower vaccination rates suffer from greater COVID-19 hospitalizations and deaths (Scobie et al., 2021).
1.4. Local context and study objective
The establishment of such relationships at the national level (e.g., KFF COVID-19 Vaccine Monitor, 2021) is appropriate for national policy, but officials “on the ground” in local contexts cannot apply such data without committing an ecological fallacy (Selvin, 1958, Lipsky, 2010). For this reason, studies of behavioral correlates with vaccine hesitancy must be conducted at the regional level to be of service to officials hoping to positively affect vaccine uptake. This approach is also better science; multi-level replication ensures not only that data can be applied at a local level but also addresses the reliance on a number of macro level studies.
Counties in Central New York (NY) have had lower levels of COVID-19 vaccine uptake than the state as a whole (NYS Department of Health, 2022). A survey of 875 adults in Northern NY found that questions regarding safety, effectiveness, and necessity were the greatest predictors of hesitancy, rather than political affiliation (Dixon, 2021). The study revealed increased hesitancy among ages 18–39, prompting our research team to explore reasons for vaccine hesitancy among young adults in our region. Literature has also shown low influenza vaccine uptake among college students (Bednarczyk et al., 2015, Poehling et al., 2012), and college campuses’ historical vulnerability to vaccine-preventable disease outbreaks (Golwalkar et al., 2018, Lu et al., 2021). Local efforts to increase vaccination uptake and hence decrease preventable deaths from COVID-19 requires a thorough understanding of vaccine hesitancy in this population. The objective of this study was to examine the underlying causes of COVID-19 vaccine use and hesitancy among students at two colleges in Central NY to better understand how to promote vaccination among this demographic.
2. Methods
2.1. Survey sample
Survey research on the impacts of the COVID-19 pandemic was carried out between fall 2020 and spring 2021 at two respected but non-elite four-year colleges—one small private college (College A) and one medium-sized public college (College B). All enrolled students were invited to participate through a distribution list that was held confidential by college administration. This census led to successive samples of the student body (Table 1). The study sites’ institutional review boards approved the study procedures and consent protocols.
Table 1.
Demographic Comparison (Waves 1–6, KABB Survey).
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 296 (25.6%) | 261 (25.2%) | 183 (22.2%) | 374 (28.5%) | 185 (27.9%) | 115 (25.5%) |
| Female | 838 (72.6%) | 757 (73.1%) | 619 (75.2%) | 911 (69.5%) | 458 (69.2%) | 319 (70.7%) |
| Non-Binary | 20 (1.7%) | 18 (1.7%) | 21 (2.6%) | 25 (1.9%) | 19 (2.9%) | 17 (3.8%) |
| Race | ||||||
| White | 981 (85.2%) | 814 (78.7%) | 650 (79.2%) | 1039 (79.4%) | 544 (82.2%) | 380 (84.4%) |
| Non-White | 170 (14.8%) | 220 (21.3%) | 171 (20.8%) | 270 (20.6%) | 118 (17.8%) | 70 (15.6%) |
| Ethnicity | ||||||
| Latinx | 67 (5.8%) | 87 (8.4%) | 54 (6.6%) | 96 (7.3%) | 59 (8.9%) | 27 (6.0%) |
| Asian | 22 (1.9%) | 29 (2.8%) | 28 (3.4%) | 33 (2.5%) | 14 (2.1%) | 11 (2.4%) |
| Other | 1062 (92.3%) | 918 (88.8%) | 736 (90.0%) | 1180 (90.2%) | 589 (89.0%) | 412 (91.6%) |
| Class Status | ||||||
| First-Year | 263 (23%) | 298 (28.9%) | 204 (24.9%) | 354 (27.1%) | 143 (21.8%) | 97 (21.6%) |
| Sophomore | 224 (19.6%) | 232 (22.5%) | 178 (21.7%) | 276 (21.1%) | 145 (22.1%) | 98 (21.8%) |
| Junior | 289 (25.3%) | 215 (20.9%) | 202 (24.6%) | 311 (23.8%) | 161 (24.5%) | 118 (26.2%) |
| Senior | 368 (32.2%) | 285 (27.7%) | 236 (28.8%) | 365 (27.9%) | 208 (31.7%) | 137 (30.4%) |
In this student population, the level of education is controlled and all are subject to the liberal messaging found in academia. These colleges are located in a region characterized by medium-sized metropolitan areas and adjoining rural hinterlands. In effect, these are students in comparatively “average” colleges located in comparatively “average” communities. It is notable however, that College B experienced a large COVID-19 outbreak early in the pandemic prior to vaccines becoming available. In a secondary analysis, we examined whether this outbreak had an effect on vaccine hesitancy.
2.2. Survey content
The research team developed a psychometric instrument, the Knowledge, Attitudes, Beliefs & Behaviors (KABB) survey, to measure the relationship between beliefs, mental health, and pandemic-related behaviors. The KABB was administered in six waves, using Qualtrics, with the link emailed directly to students in the sampling frame. The core survey was administered in each wave and supplementary question sets were added to test specific hypotheses. The analysis presented here uses the sixth wave, conducted in late April 2021. The survey contained 62 questions, including items pertaining to vaccine use and hesitancy. Earlier waves preceded the COVID-19 vaccines. The total sample size for the sixth wave was 627 students, out of 8,894 eligible respondents (7.1 percent). Because this was the sixth wave and incentives were not provided, there was attrition in participation. Earlier waves were used to ensure comparable representativeness by comparing select demographic items.
Survey questions measured vaccine hesitancy using the question, “When a vaccine for the coronavirus becomes available, I will get vaccinated,” with answer categories: I have already received the vaccine; yes, definitely; yes, with some concern; not sure; not at this time until more information is available; no, definitely not. Political ideology was measured by a question that asked, “Which description best represents your political ideology?,” followed by a five point Likert scale from Progressive/Very Liberal (0) to Very Conservative (4). Source of news was measured by a question asking where the respondent got their news followed by a list of news sources and a request to click all that apply.
2.3. Analytic strategy and modeling
Structural Equation Modeling (SEM) was used to explore direct and indirect relationships. SEM offered the ability to assess overall model fit, allowing us to draw conclusions about which models were better approximations of the data. Model fit was optimized by reviewing several indicators as detailed in the results section. The standardized path coefficients were used to examine the relationships between variables and draw conclusions about our hypotheses.
Based on prior studies, we identified several hypotheses for key variables and how they inform our understanding of vaccine hesitancy. As noted, in some studies, women were more likely than men to be hesitant, while other studies have concluded the opposite. We expected a weak gender relationship with vaccine hesitancy but offer no directionality. Beyond gender, prior research has suggested that Republican Party affiliation, conservative political ideology, and consumption of right wing news media are all associated with higher levels of vaccine hesitancy. The latter, news sources, is relevant to concerns about COVID-19 misinformation. We examined the direct effects of political ideology and news media consumption on vaccine hesitancy and how these variables moderate the effect of gender. We explored the complex relationship between political ideology, news media consumption, and vaccine hesitancy, by modeling competing configurations and optimizing model fit through comparisons of various path configurations before arriving at a final model.
3. Results
3.1. Demographic characteristics
Table 1 presents a comparison of select demographic characteristics for the two combined colleges across waves of the survey to provide a basis for comparison. As we discuss, the analysis data from wave six are comparable to the prior waves.
The percent male ranged from 22.2 to 28.5% with an average of 25.8%, making the wave six estimate 0.3% lower than the average. The percent non-binary ranged from 1.7 to 3.8%, with an average of 2.4%, making wave six estimate higher by 1.2%. In terms of race, the percent non-white (African American, Bi- or multi-racial, Latinx, Asian, Native American) ranged from 14.8 to 21.3% with an average of 18.5%, making the wave six estimate lower by 2.9%. For ethnicity, we found that the Latinx population ranged from 5.8 to 8.9% with an average of 7.2%, making wave six estimate 1.2% lower than the sampling average. For Asian students, the range was from 1.9 to 3.4% with an average of 2.5%, making the wave six estimate 0.1% lower than the mean. Finally, for class status, the percent of first-year students ranged from 21.6 to 28.9% with an average of 24.6%, making the wave six estimate 3% lower than the mean. Overall, when compared to the previous waves, wave six has similar proportionality across demographic characteristics. Though it was the smallest, wave six was close to the sampling averages, within 2–3%. We therefore believe this sample is representative of the population from the two combined colleges.
3.2. Analysis variables and descriptive statistics
Our research questions examined the underlying causes of vaccine use and hesitancy, based on several variables identified in the literature, including gender, political ideology, and news sources. Race was removed from the analysis, as preliminary models did not find a statistically significant effect. Although, the combining of non-white categories due to small sample sizes may have eliminated any effect. The remaining analysis variables are presented in Table 2.
Table 2.
Descriptive statistics and bivariate correlations.
| Statistics | V1 | V2 | V3 | V4 | V5 | V6 | V7 | |
|---|---|---|---|---|---|---|---|---|
| V1 Vaccine Hesitancy (0–5) (High = Hesitant) |
= 1.08, SD = 1.71 |
--- | ||||||
| V2 Gender (1 = Male) | 25.56% |
−0.002 | --- | |||||
| V3 Political Ideology (1–4) (High = Conservative) |
= 2.49, SD = 1.11 |
0.434** | 0.234*** | --- | ||||
| V4 NPR (News Source Consumption) |
6.70% |
−0.085ϯ | 0.145** | −0.026 | --- | |||
| V5 NBC/MNBC (News Source Consumption) |
21.65% |
−0.039 | −0.180*** | −0.147** | 0.184*** | --- | ||
| V6 Fox News (News Source Consumption) |
14.35% |
0.084 ϯ | −0.318*** | 0.427*** | 0.127*** | 0.215*** | --- | |
| V7 Parler (News Source Consumption) |
0.8% |
0.119** | −0.232*** | 0.180*** | 0.119** | −0.004 | 0.117** | --- |
Alpha= ϯ.10, *0.05, **0.01, ***0.001.
As the table shows, the dependent variable, vaccine hesitance, ranges from 0 to 5. For this variable, 0 indicates the respondent had already received the vaccine, while 1 indicates a low level of hesitancy and 5 a high level. The average of 1.08 indicates that many students were vaccinated before they completed the survey, and among those who were not, the majority were not very hesitant. The sample of students includes a higher proportion of females than males, at about a 3:1 ratio, as is the case for the two colleges under investigation. Political ideology ranges from 1 to 4, with 1 being more progressive or liberal and 4 being more conservative. The average of 2.5 indicates that most students are near the middle, but lean in the conservative direction. The most frequent news source was NBC/MSNBC (21.65%), followed by Fox News (14.35%), NPR (6.7%), and the highly conservative social media site, Parler (0.8%). Table 2 also includes the initial zero-order bivariate correlations for our analysis variables. Among the highest correlations with vaccine hesitancy are political ideology (0.434) and getting news from Parler (0.119). The independent effects of these variables were examined in multivariate models as discussed below.
3.3. The Structural Equation Model
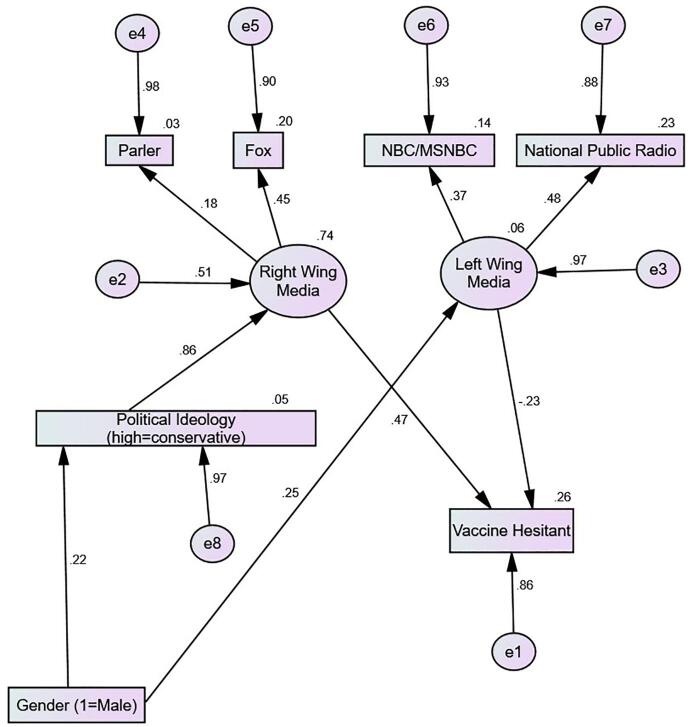
Fig. 1 displays the final SEM with standardized effects in order to inform us about the relative strength of each path. Model fit for this analysis was deemed acceptable as determined by fit indices that approach 1 (NFI = 0.760, IFI = 0.793, CFI = 0.780), the chi-square to degrees of freedom ratio (70.3/12 = 5.8), and the RMSEA (0.088). These values are superior to preliminary model specifications that are not reported here. All path coefficients in the model are statistically significant at the alpha = 0.05 level. The total squared-multiple correlation (R2) of the model explains 0.26, or 26% of the variation in vaccine hesitancy.
Fig. 1.
Structural Equation Model of Gender, Political Ideology, Media Consumption, and Vaccine Hesitancy (Low = Already Vaccinated to High = Extremely Hesitant).
3.3.1. Total effects
Table 3 provides information on the standardized total effects, which are different from the direct effects shown in Fig. 1. Of primary importance are the total effects of the different independent variables on the dependent outcome of vaccine hesitancy. The total effect of gender is very weak (0.035), as the arrows pointing to conservative political ideology and left wing media act to cancel each other out. The total effect of political ideology is moderate (0.403). This is entirely an indirect effect by way of right wing media consumption. Finally, the total effect of left wing media consumption is simply the direct effect shown in Fig. 1 (−0.23), as there are no intervening variables.
Table 3.
Standardized Total Effects (significant at 0.05 level or better).
| Gender (Male) | Political Ideology | Left Wing | Right Wing | |
|---|---|---|---|---|
| Political Ideology | 0.224 | 0.000 | 0.000 | 0.000 |
| Left Wing | 0.246 | 0.000 | 0.000 | 0.000 |
| Right Wing | 0.192 | 0.858 | 0.000 | 0.000 |
| NBC/MSNBC | 0.118 | 0.000 | 0.477 | 0.000 |
| NPR | 0.091 | 0.000 | 0.370 | 0.000 |
| Parler | 0.035 | 0.157 | 0.000 | 0.183 |
| Fox | 0.086 | 0.382 | 0.000 | 0.446 |
| Vaccine Hesitant | 0.035 | 0.403 | −0.226 | 0.470 |
3.3.2. Direct effects
The direct effects in the model suggest that gender (being male) has a modest direct effect on both political ideology (being more conservative) (0.22) and left wing news media consumption (0.25). The direct effect of political ideology on right wing media consumption is strong and robust (0.86), as noted previously. The model suggests males are more likely to consume media in general, but through the effects of political ideology, males are much more likely to consume right wing media content. The model shows a moderately strong effect of right wing news media consumption on vaccine hesitancy (0.47) and a weaker and negative relationship (statistically) of left wing media consumption on vaccine hesitancy (−0.23).
3.3.3. Secondary analysis
An additional SEM (not shown but available by request) demonstrated that the College B outbreak did not have a significant effect on vaccine hesitancy among students. Students who experienced a campus outbreak were not significantly more likely to be vaccinated or consider being vaccinated than students who did not experience a campus outbreak.
4. Discussion
The effect of conservative political ideology is to promote the consumption of right wing news, which in turn tends to increase vaccine hesitancy. This finding, consistent with Pinna et al., 2021, Fridman et al., 2021, challenges the notion that being conservative inherently impacts vaccine attitudes and beliefs. Indeed, political affiliation has progressed as a factor in vaccine-related attitudes and behavior over the course of the COVID-19 pandemic. Our results from surveys of college students in Central NY clearly point to one’s source of news media as a mechanism for this politicization.
Our model also shows that though not linked to political ideology, consumption of left wing news media is associated with diminished vaccine hesitancy. Other studies support this finding (Lazer et al., 2021, Romer and Jamieson, 2020). A key point this study underscores is that news sources significantly contribute to levels of vaccine hesitancy, even as these are a product of complex gender and political ideology configurations.
Political ideology and gender are thus relevant to vaccine hesitancy, but indirectly. We have found that political ideology is relevant in its power to guide people to specific new sources. Conservative political ideology does not directly lead to vaccine hesitancy, but it does encourage the consumption of news from sources that promote fear and hesitation about the vaccines. Based on our analysis, we find that gender has an effect on both political ideology and left wing media consumption. Gender does not ultimately have a relationship with vaccine hesitancy once these variables are considered. Gender is therefore only indirectly connected to vaccine hesitancy, which may explain why previous studies have not detected a clear gender effect. However, being male is associated with identifying on either end of the political spectrum as opposed to in the middle. Men are thereby more likely to consume news that promotes hesitancy than women.
Interestingly, our secondary analysis found that a campus outbreak did not have a significant effect on vaccine hesitancy later in the pandemic. This may reflect the power of media messaging such that it can override at least some pandemic-related experiences.
4.1. Limitations
Our sample is not generalizable outside of the institutions from which it was drawn and does not provide the full range of variability that would be found in a sample from the wider demographic. Specifically, a college population is unique in its homogeneous education level, a factor correlated with vaccine hesitancy (Khairat et al., 2022). In addition, data on urban versus rural residency, found to be relevant in prior research (Fisher et al., 2020, Khubchandani et al., 2021, Kirzinger et al., 2021a, Saelee et al., 2022, Sun and Monnat, 2021), are complicated by questions about whether students identify their home as the location of their college residence or the location of their original home. We did not investigate urban–rural difference, based on concerns over the reliability of these data. We also have not collected data around messaging, so the mechanism connecting specific news sources to feelings of vaccine hesitancy is not known. Future research could explore how the content of news stories influences vaccine hesitancy and the steps necessary to remediate this effect.
5. Conclusion
Where people obtain information is highly relevant in their decision-making process about whether to receive the COVID-19 vaccination. Our findings suggest that conservative political ideology promotes the consumption of right wing news, which then tends to increase vaccine hesitancy. This underscores the threat misinformation poses on public health and the importance of interventions to combat it. As the pandemic persists, it is critical that we continue to increase vaccination uptake among hesitant groups, including young adults and importantly, consumers of right wing media.
6. Sources of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Emily Lasher: Writing – original draft, Writing – review & editing, Investigation. Gregory Fulkerson: Conceptualization, Methodology, Investigation, Formal analysis. Elizabeth Seale: Investigation, Data curation. Alexander Thomas: Conceptualization, Methodology, Resources, Supervision, Project administration. Anne Gadomski: Writing – original draft, Writing – review & editing, Supervision, Conceptualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge Michael McCarthy at Utica College for his role in data processing and Dr. Caroline Gomez-DiCesare for her early work in survey design.
References
- Adams S.H., Schaub J.P., Nagata J.M., Park M.J., Brindis C.D., Irwin C.E., Jr. Young adult perspectives on COVID-19 vaccinations. J. Adolesc. Health. 2021;69(3):511–514. doi: 10.1016/j.jadohealth.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J.D., Feng W., Corlin L., Porteny T., Acevedo A., Schildkraut D., King E., Ladin K., Fu Q., Stopka T.J. Why are some people reluctant to be vaccinated for COVID-19? A cross-sectional survey among U.S. adults in May-June 2020. Prev. Med. Rep. 2021;24:101494. doi: 10.1016/j.pmedr.2021.101494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allington D., McAndrew S., Moxham-Hall V.L., Duffy B. Media usage predicts intention to be vaccinated against SARS-CoV-2 in the US and the UK. Vaccine. 2021;39(18):2595–2603. doi: 10.1016/j.vaccine.2021.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baack B.N., Abad N., Yankey D., Kahn K., Razzaghi H., Brookmeyer K., Kolis J., Wilhelm E., Nguyen K.H., Singleton J.A. COVID-19 vaccination coverage and intent among adults aged 18–39 years — United States, March–May 2021. Centers Dis. Control Prev. 2021;70(25):928–933. doi: 10.15585/mmwr.mm7025e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednarczyk R.A., Chu S.L., Sickler H., Shaw J., Nadeau J.A., McNutt L.-A. Low uptake of influenza vaccine among university students: Evaluating predictors beyond cost and safety concerns. Vaccine. 2015;33(14):1659–1663. doi: 10.1016/j.vaccine.2015.02.033. [DOI] [PubMed] [Google Scholar]
- Berenson A.B., Chang M., Hirth J.M., Kanukurthy M. Intent to get vaccinated against COVID-19 among reproductive-aged women in Texas. Human Vaccines Immunotherapeut. 2021;17(9):2914–2918. doi: 10.1080/21645515.2021.1918994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borah, P., Austin, E., Yan, S., 2022. Injecting disinfectants to kill the virus: Media literacy, information gathering sources, and the moderating role of political ideology on misperceptions about COVID-19. Mass Commun. Soc., https://doi.org/10.1080/15205436.2022.2045324.
- Conway, D., 2020, October 26. Uninsured rates highest for young adults aged 19 to 34. United States Census Bureau. Retrieved September 24 from https://www.census.gov/library/stories/2020/10/uninsured-rates-highest-for-young-adults-aged-19-to-34.html.
- Cowan, S.K., Mark, N., Reich, J.A., 2021. COVID-19 vaccine hesitancy is the new terrain for political division among Americans. Socius: Sociol. Res. Dynamic World, 7. https://doi.org/10.1177/23780231211023657.
- Daly M., Jones A., Robinson E. Public trust and willingness to vaccinate against COVID-19. JAMA. 2021;325(23):2397–2399. doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhawan D., Bekalu M., Pinnamaneni R., McCloud R., Viswanath K. COVID-19 news and misinformation: Do they matter for public health prevention? J. Health Commun. 2021;26(11):799–808. doi: 10.1080/10810730.2021.2010841. [DOI] [PubMed] [Google Scholar]
- Dixon, P., 2021, May 10. JCC & Syracuse University Partner to Study COVID Vaccine Hesitancy in Northern New York. Jefferson Community College. Retrieved September 9 from https://sunyjefferson.edu/news/jcc_su_ccs_covid_hesitancy_nny.php.
- Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman A., Gershon R., Gneezy A., Capraro V. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE. 2021;16(4):e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galasso, V., Profeta, P., Foucault, M., Pons, V., 2021. COVID-19 vaccine's gender paradox. medRxiv preprint. https://doi.org/10.1101/2021.03.26.21254380.
- Gargano J., Wallace M., Hadler S., Langley G., Su J., Oster M., Broder K., Gee J., Weintraub E., Shimabukuro T., Scobie H.M., Moulia D., Markowitz L.E., Wharton M., McNally V.V., Romero J.R., Talbot H.K., Lee G.M., Daley M.F., Oliver S.E. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: Update from the advisory committee on immunization practices — United States, June 2021. Centers Dis. Control Prev. 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golwalkar M., Pope B., Stauffer J., Snively A., Clemmons N. Mumps outbreaks at four universities – Indiana, 2016. MMWR Morb. mortal. wkly rep. 2018;67(29):793–797. doi: 10.15585/mmwr.mm6729a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamel, L., Lopes, L., Sparks, G., Kirzinger, A., Kearney, A., Stokes, M., Brodie, M., 2022, January 28. KFF COVID-19 vaccine monitor: January 2022. Kaiser Family Foundation. Retrieved February 11 from https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-january-2022/.
- Hsu, T., 2021, July 11. Despite outbreaks among unvaccinated, Fox News hosts smear shots. The New York Times. https://www.nytimes.com/2021/07/11/business/media/vaccines-fox-news-hosts.html.
- Jamieson, K.H., Albarracín, D., 2020. The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US. Harvard Kennedy School Misinformation Review. https://doi.org/10.37016/mr-2020-012.
- KFF COVID-19 Vaccine Monitor, 2021. Kaiser Family Foundation. Retrieved August 31 from https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/.
- Khairat S., Zou B., Adler-Milstein J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am. J. Infect. Control In Press. 2022;50(3):262–267. doi: 10.1016/j.ajic.2021.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Commun. Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King W.C., Rubinstein M., Reinhart A., Mejia R. COVID-19 vaccine hesitancy January-May 2021 among 18–64 year old US adults by employment and occupation. Prev. Med. Rep. 2021;24 doi: 10.1016/j.pmedr.2021.101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirzinger, A., Sparks, G., Brodie, M., 2021, April 9. KFF COVID-19 vaccine monitor- rural America. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-rural-america/.
- Kirzinger, A., Sparks, G., Hamel, L., Lopes, L., Kearney, A., Stokes, M., Brodie, M., 2021, August 4, 2021. KFF COVID-19 vaccine monitor: July 2021. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-july-2021/.
- Kricorian K., Civen R., Equils O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunotherapeut. 2021;1–8 doi: 10.1080/21645515.2021.1950504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazer, D., Green, J., Ognyanova, K., Baum, M. A., Lin, J., Druckman, J., Perlis, R. H., Santillana, M., Lin, J., Simonson, M., Uslu, A., 2021. Social media news consumption and COVID-19 vaccination rates. The COVID States Project: A 50-State COVID-19 Survey. https://covidstates.org/.
- Lipsky, M., 2010. Street-Level Bureaucracy: Dilemmas of the Individual in Public Service. In: 30th Anniversary Expanded Edition. New York: Russell Sage Foundation.
- Liu R., Li G.M. Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. Social Sci. Med. – Popul. Health. 2021;15:100896. doi: 10.1016/j.ssmph.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Weintz C., Pace J., Indana D., Linka K., Kuhl E. Are college campuses superspreaders? A data-driven modeling study. Comput. Methods Biomech. Biomed. Eng. 2021;24(10):1136–1145. doi: 10.1080/10255842.2020.1869221. [DOI] [PubMed] [Google Scholar]
- MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Monroe, T., Savillo, R., 2021, July 16, 2021. Fox has undermined vaccination efforts in nearly 60% of all vaccination segments in a 2-week period. Media Matters for America. Retrieved September 2 from https://www.mediamatters.org/fox-news/fox-has-undermined-vaccination-efforts-nearly-60-all-vaccination-segments-2-week-period.
- Motta M., Stecula D., Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the U.S. Canad. J. Polit. Sci. 2020;53(2):335–342. doi: 10.1017/s0008423920000396. [DOI] [Google Scholar]
- Muddiman A., Budak C., Romas B., Kim Y., Murray C., Burniston M.M., Geiger J., Purcell A., Ludzenski J., Turner M., Duchovany M., Stroud N.J. Cable and nightly network news coverage of coronavirus. Center for Media Engagement. 2020 https://mediaengagement.org/research/coronavirus-network-coverage [Google Scholar]
- Muric G., Yusong W., Ferrara E. COVID-19 vaccine hesitancy on social media: Building a public Twitter data set of antivaccine content, vaccine misinformation, and conspiracies. JMIR Public Health Surveillance. 2021;7(11):e30642. doi: 10.2196/30642. https://publichealth.jmir.org/2021/11/e30642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy V. Surgeon General’s Advisory on Building a Healthy Information Environment; 2021. Confronting Health Misinformation: The U.S. [PubMed] [Google Scholar]
- NYS Department of Health, 2022, February 8. Vaccination progress to date. Retrieved February 9, 2022, from https://coronavirus.health.ny.gov/vaccination-progress-date.
- Ognyanova, K., Lazer, D., Baum, M. A., Druckman, J., Green, J., Perlis, R. H., Santillana, M., Lin, J., Simonson, M., Uslu, A., 2021. Vaccine misinformation, from uncertainty to resistance. The COVID States Project: A 50-State COVID-19 Survey. https://covidstates.org/.
- Pinna, M., Picard, L., Goessmann, C., 2021. Cable news and COVID-19 vaccine compliance. Social Sci. Res. Netw. Preprint. https://dx.doi.org/10.2139/ssrn.3890340.
- Poehling K.A., Blocker J., Ip E.H., Peters T.R., Wolfson M. 2009–2010 seasonal influenza vaccination coverage among college students from 8 universities in North Carolina. J. Am. Coll. Health. 2012;60(8):541–547. doi: 10.1080/07448481.2012.700973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D., Jamieson K.H. Conspiratorial thinking, selective exposure to conservative media, and response to COVID-19 in the US. Soc. Sci. Med. 2021;291:114480. doi: 10.1016/j.socscimed.2021.114480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelee R., Zell E., Murthy B.P., Castro-Roman P., Fast H., Meng L., Shaw L., Gibbs-Scharf L., Chorba T., Harris L.Q., Murthy N. Disparities in COVID-19 vaccination coverage between urban and rural counties — United States, December 14, 2020–January 31, 2022. Centers Dis. Control Prev. 2022;71(9):335–340. doi: 10.15585/mmwr.mm7109a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scobie H.M., Johnson A.G., Suthar A.B., Severson R., Alden N.B., Balter S., Bertolino D., Blythe D., Brady S., Cadwell B., Cheng I., Davidson S., Delgadillo J., Devinney K., Duchin J., Duwell M., Fisher R., Fleischauer A., Grant A., Griffin J., Haddix M., Hand J., Hanson M., Hawkins E., Herlihy R.K., Hicks L., Holtzman C., Hoskins M., Hyun J., Kaur R., Kay M., Kidrowski H., Kim C., Komatsu K., Kugeler K., Lewis M., Lyons B.C., Lyons S., Lynfield R., McCaffrey K., McMullen C., Milroy L., Meyer S., Nolen L., Patel M.R., Pogosjans S., Reese H.E., Saupe A., Sell J., Sokol T., Sosin D., Stanislawski E., Stevens K., Vest H., White K., Wilson E., MacNeil A., Ritchey M.D., Silk B.J. Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status — 13 U.S. Jurisdictions, April 4–July 17, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70(37):1284–1290. doi: 10.15585/mmwr.mm7037e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvin H.C. Durkheim’s Suicide and Problems of Empirical Research. Am. J. Sociol. 1958;63(6):607–619. doi: 10.1086/222356. [DOI] [Google Scholar]
- Sharma M., Davis R.E., Wilkerson A.H. COVID-19 vaccine acceptance among college students: A theory-based analysis. Int. J. Environ. Res. Public Health. 2021;18(9):4617. doi: 10.3390/ijerph18094617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Monnat S.M. Rural-urban and within-rural differences in COVID-19 vaccination rates. J. Rural Health. 2021;1–7 doi: 10.1111/jrh.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tram K.H., Saeed S., Bradley C., Fox B., Eshun-Wilson I., Mody A., Geng E. Deliberation, dissent, and distrust: Understanding distinct drivers of COVID-19 vaccine hesitancy in the United States. Clin. Infect. Dis. 2021 doi: 10.1093/cid/ciab633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma P., Junge M., Meaklim H., Jackson M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Progr. Neuropsychopharmacol. Biol. Psychiatry. 2021;109:110236. doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K., Bekalu M., Dhawan D., Pinnamaneni R., Lang J., McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21(818) doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis D.E., Andersen J.A., Bryant-Moore K., Selig J.P., Long C.R., Felix H.C., Curran G.M., McElfish P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021;00:1–8. doi: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang D., Lehmann L.S. Confronting the misinformation pandemic. Health Policy Technol. 2021;10(3):100520. doi: 10.1016/j.hlpt.2021.100520. [DOI] [PMC free article] [PubMed] [Google Scholar]