Abstract
Brief therapy for insomnia (BTI) is a short-term cognitive behavioral therapy for insomnia. At present, there is no study combining BTI with digital technology. However, in the context of the outbreak of coronavirus disease 2019 (COVID-19), patients with acute insomnia may need an online treatment which can quickly improve insomnia symptoms. Our team built a digital BTI (dBTI) platform based on the WeChat mini program. This research provides a framework design and a course design of dBTI, and evaluates the system via recruiting participants suffering from acute insomnia in pandemic. What's more, it explores patients’ adherence, the efficiency of the system and their relationship. As the result demonstrates, 68% of participants have completed more than half of the course with medium to high adherence. Gender, pre-sleep arousal scale (PSAS) somatic score and insomnia severity index (ISI) score have affected participants’ adherence, and higher adherence has led to better improvement in the severity of insomnia and somatic pre-sleep arousal. It is proved that the platform we built is effective, which not only offers an entry point for the study of how to set up a dBTI platform, but also provides theoretical basis for its clinical application.
Keywords: Digital Medicine, dBTI, Platform Development, WeChat Mini Program, Adherence, COVID-19
1. Introduction
Driven by the Internet, Internet of Things, big data and artificial intelligence, the Fourth Industrial Revolution centers on the great integration of networks, information and intelligence [1]. The application of these technologies to medical industry has brought about the booming of digital medicine, and even the emerging of numerous concepts such as m-health and digital therapeutics [2], [3]. The advantages of remote monitoring, portability and personalized treatment characteristic of digital therapeutics have been on full display since the breakout of coronavirus disease 2019 (COVID-19) Pandemic in 2020, and thereupon have drastically accelerated the digital revolution of the world [4]. In this context, digital behavioral therapy technology came into being.
Brief therapy for insomnia (BTI) is a short-term cognitive behavioral therapy, which takes only 1–2 weeks [5]. The basic principle of BTI is to regulate sleep by changing behaviors when awake, thereby directly affecting homeostasis and circadian clock driving. Stimulus control and sleep restriction are the core components of BTI, which can improve sleep quality by restricting sleeping time and environment. At present, it has been found that BTI can rapidly reduce the insomnia severity and alleviate insomnia symptoms, which is reflected in the shortening of sleep latency, the improvement of sleep efficiency and the reduction of PSQI [6]. Additionally, it has been pointed out that BTI is also helpful for reducing anxiety and depression of patients [7]. However, BTI in almost all current studies is a face-to-face offline treatment, and the effect of BTI combined with digital technology has not been clarified.
Due to the outbreak of COVID-19 Pandemic, most people throughout the world are facing unprecedented pressures of unknown duration, and thus are suffering anxiety, depression and even insomnia symptoms [8]. According to the 3P model (predisposing, precipitating, and perpetuating) of acute insomnia [9], the COVID-19 outbreak is considered as a trigger for acute insomnia. Some people without sleep problems before are also troubled by it. One of the useful suggestions given by the European Academy for Cognitive-Behavioral Treatment of Insomnia (CBTI) tackling worse sleep quality since the pandemic is cognitive and behavioral intervention [10]. However, the mass lockdown restriction resulting from the pandemic also largely affects the application of face-to-face treatment. On this ground, how to improve acute insomniacs’ sleep quality under unexpected events via digital technology becomes a heated issue in the academic field. Due to the outbreak of the pandemic, transmissibility and timeliness of behavioral therapy put forward higher requirements.
Therefore, the combination of BTI and digital technology has become a feasible scheme. Digital technology will supplement visual elements, creative interaction, record summary and progress evaluation report to BTI, which will be more attractive to individuals [11]. Moreover, convenient and efficient digital mode is also conducive to massive online patients with insomnia. Our team has coordinated with a technology company on developing the first dBTI platform and recruited participants during the COVID-19 Pandemic to assess it. Our paper attempts to study the platform development, adherence and efficacy of dBTI. To fulfill this goal, we:
(1) Describe in detail the framework design and course design of dBTI based on WeChat mini program.
(2) Analyze the relevant factors affecting adherence.
(3) Analyze the relationship between adherence and efficacy.
The ultimate goal is to tackle the issues of: (1) how to develop a dBTI platform rapidly and effectively; (2) how to increase the adherence of individuals and improve the efficacy of dBTI.
2. Methodology
2.1. The development of a dBTI platform based on WeChat mini program
2.1.1. The introduction and advantages of WeChat mini program
WeChat is an extremely popular social application in China. It is easy to operate and can offer multiple functions such as text and voice messages, video calls, subscription to public accounts and mini programs. WeChat mini program is an application built into WeChat and can be opened directly in WeChat. It has almost the same functions and forms as the Native APP, and will not occupy too much mobile phone memory under the premise of maintaining smooth use [12]. Compared with other digital platforms, WeChat mini-programs have the following advantages in the platform development of dBTI:
(1) Convenient: Individuals can find in WeChat by scanning the quick response (QR) code or searching the name and do not need to download or install any applications on their devices [13]. What’s more, they don’t need to register a new account and relearn how to use it. For people of various ages and educational levels who suffer from insomnia, the dBTI platform can be easily and quickly used.
(2) Lower development requirements, lower maintenance cost: Given the suddenness of the COVID-19 pandemic, it is important to develop a product as soon as possible to help individuals who are suffering from insomnia. WeChat mini program has low technical requirements and can automatically adapt to various operating systems, such as IPhone operation system (IOS) and Android. Thus, we can reduce development costs, and make development process quick so that people can use the dBTI platform early.
(3) Easy to spread and popularize: According to the Tencent’s report, the number of active accounts of WeChat in 2020 reached 1.112 billion [14]. The wide audience also makes WeChat an effective technology of disease management [15].
(4) Outstanding function, better individual experience: WeChat mini program can obtain more system permissions. For example, compared with hypertext markup language 5 (HTML5) websites, the WeChat mini program has access to get data-cache function, network communication status and so on. These system-level permissions can be seamlessly interlinked with WeChat mini program which makes it have better fluency and improve the individual experience.
2.1.2. The framework design of the dBTI platform
The dBTI platform is based on the multipurpose infrastructure for network applications (MINA) framework, which includes View, Application (APP) Service and Native.
The View is developed by WeiXin/WeChat markup language (WXML) and WeiXin/WeChat style sheets (WXSS). The WXSS is a set of style languages that describes the component styles of WXML, and which determines how the components of WXML are displayed, and implement the rendering structure of the page [16]. The View enables the interactions of functions, and the output of the dBTI platform. For example, the course interface, sleep diary interface, questionnaire tool interface, etc. And all the interactive event data will pass to App Service by View at the same time.
The APP Service is developed by JavaScript language, which processes data and sends it to View for updated output. At the same time, the App Service accepts the reflections of View which can be used to make logical processing, data requests and interface calls [17]. For example, when individuals click to switch different interfaces, the View sends that information to the App Service. After processing it, the App Service sends the data of interface that needs to be presented to the View. The View renders the data and ultimately presents it to individuals. Also, the data transmission between the View and the App Service need to pass the Native.
Through the JavaScript Bridge (JSBridge) of the Native, we build the channel in order to transmit data between the View and the App Service. What’s more, the Native also contains WeChat abilities, document storage, network request and so on. The WeChat abilities include WeChat individual information, WeChat public account, QR code, scanning, WeChat Pay and many other built-in basic functions. The dBTI platform can invoke those functions through the App Service. Document storage includes temporary data, local cache, web storage and data invoking. And the net request will involve a third server.
With a network request, data transmission between the application server and the third server can only be carried out. In the individuals’ interaction of using the dBTI platform, the individuals’ data such as daily sleep time and questionnaire score will be stored in the server. In addition to software file storage, the Web server also has functions such as core logic implementation and individual authority authentication. The historical data stored in the server can be invoked by individuals, even if individuals change their devices, the previous usage record can be received on the new device [18]. The specific architecture of the MINA framework is shown in Fig. 1 .
Fig. 1.
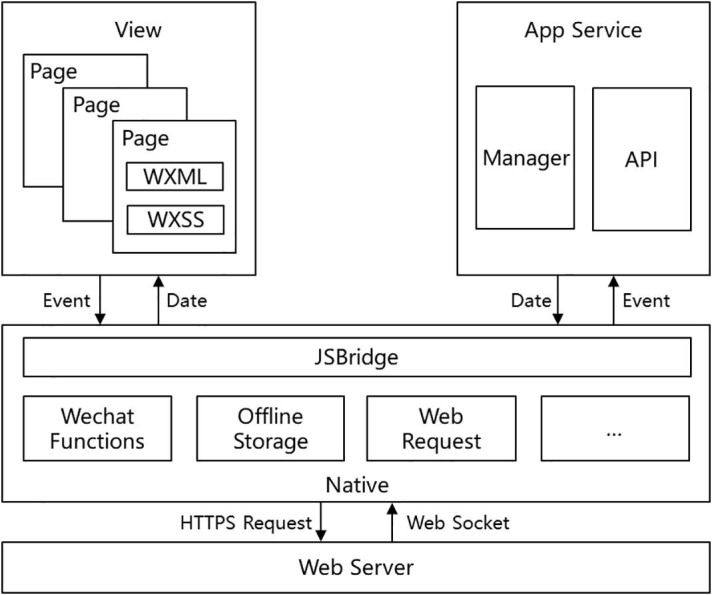
The MINA framework. MINA: Multipurpose Infrastructure for Network Applications; WXML: WeiXin/WeChat Markup Language; WXSS: WeiXin/WeChat Style Sheets; APP: Application; API: Application Programming Interface; JSBridge: JavaScript Bridge; HTTPS: Hypertext Transfer Protocol Secure.
2.1.3. The course design of the dBTI platform
The one-week course design of dBTI is based on BTI, including seven modules: sleep hygiene education, sleep restriction, stimulus control, relaxation tools, cognitive reconstruction, correct thoughts about sleeping medicine and summary and review. All of these modules are assigned to study each day during the period in one week.
The dBTI platform can be accessed using the WeChat mini program of any smartphone. When individuals log into their WeChat account to enter the mini program for the first time, they need to complete an online self-assessment process for short-term insomnia disorders so that the dBTI can collect the baseline of insomnia’s extent. Another post-assessment will be conducted on the end of the week. The individual also need to fill out personal information (sleep problem, medical history and so on), and the sleep routine of the past week. All sleep data are then presented on the applet homepage including the progress of treatment, daily task (including sleep diary, course, and daytime behaviour), sleep efficiency report, relaxation audio and other self-assessment questionnaires. Besides the homepage, there is another page entitled “Me”, which presents personal information, results of questionnaires and sleep efficiency reports. See Fig. 2 for a detailed schematic of the dBTI platform framework.
Fig. 2.
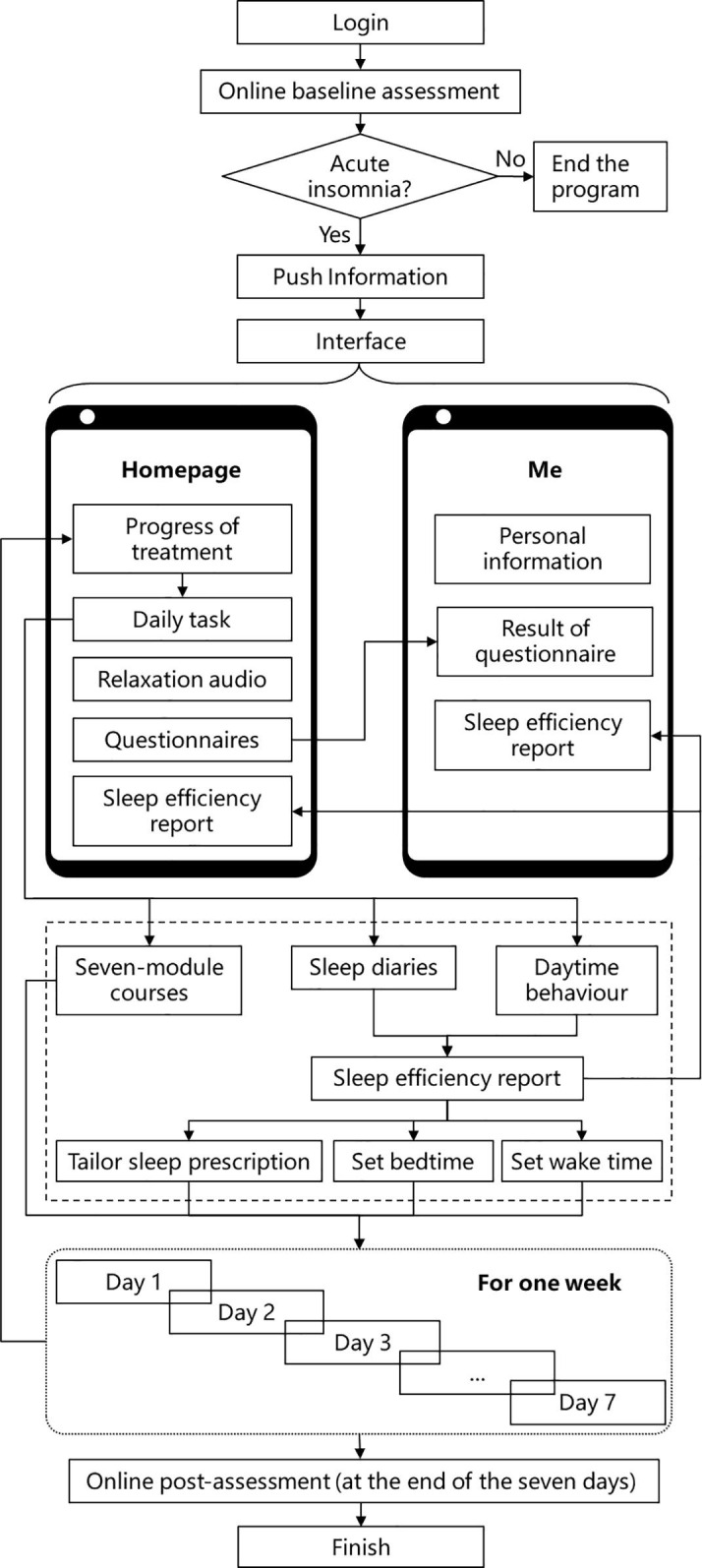
The dBTI platform’s framework.
The seven-module course is the dominant approach to improve individuals' sleep quality. Every module includes various photos, articles and audios, and individuals will receive one module every day of the week. The program will push reminder information at 8p.m. every day to complete the session, and send another reminder information to review the previous session at 12p.m. In the courses learning process, the individual has to complete previous sessions and assignments to unlock the following session. The main contents are shown in Table 1 .
Table 1.
Schedule of course topics and objectives.
| Date | Topic | Objectives |
|---|---|---|
| Day 1 | Sleep Hygiene Education | Leads to a quality sleep by incorporating new habits into nighttime routine. |
| Day 2 | Sleep Restriction | Learn how to fill out sleep dairy and it’s request individuals decrease the time stay in bed when you awaking, to increase the sleep efficiency which means the ratio of the duration of fall sleep to the duration of stay in bed. In this part, there is a essential point to individuals known about the importance of sleep diary. |
| Day 3 | Stimulus Control | To teach individuals about not do anything that’s unrelated with fall in sleep for increasing the contact with bed and sleep, like do not play games in bed. |
| Day 4 | Relaxation Tools | To teach individuals about several relaxation tools to help decrease nervous, like body scan, breathing exercise and gradual relaxation training |
| Day 5 | Cognitive Reconstruction | To decrease the positive influence from our worried mind about sleep |
| Day 6 | Correct Thoughts about Sleeping Medicine | To teach individuals have a deep insight about sleep medicine for medicine’s using security |
| Day 7 | Summary and Review | To give individuals a brief review about the courses studied before, and reinforce the confidence to be better |
While completing the daily course, individuals are requested to record sleep diary every day, and the WeChat mini program will push information at 9 a.m. every day to remind individuals complete sleep diary. The sleep diary includes 5 items about individual’s sleep situation, which are the time to get into bed, time to fall asleep, time of awakening, time of getting out of bed, the duration of night awakening and a 5-point scale to rate the sleep quality from very poor to very good. Daytime behaviour is asked to complete every day, which is consists of medicine usage, the length of sunshine, napping time, the length of exercise and intake of alcohol, tea or coffee. Then sleep diary and daytime behaviour information are used by the mini program to auto-generate a sleep efficiency report, and a tailored sleep prescription, a set bedtime and set wake time, in order to increase sleep efficiency. During this period, individuals can also conduct a self-questionnaire survey to understand their sleeping and emotional status. Sleep efficiency and questionnaire score are calculated through the App Service of WeChat mini program. Sleep diary and questionnaire filling buttons are placed on the home page. After clicking, the individuals will jump to the secondary page to fill in. After submitting, the system will automatically generate sleep efficiency and questionnaire score. The historical results can be viewed by clicking the questionnaire results or sleep efficiency report on page “Me”.
The individuals are asked to continue to study the course and fill in the sleep diary, and adjust the daytime activities, sleep latency and bedtime according to the results. After one week, dBTI is completed, and individuals need to fill in the scale again to evaluate the therapeutic effect.
2.2. Evaluation method for adherence and efficacy of dBTI
After the establishment of online platform, we recruited participants via a campaign called “Epidemic Prevention, Control and Protection Handbook” supported by the local government. Residents can participate in the treatment by scanning QR code of the WeChat mini program printed at the end of the manual. A total of 280 participants were registered by scanning the QR code. However, not all registrants were suitable to participate in the evaluation of compliance and efficacy. Therefore, we formulated the inclusion criteria: (1) participants were Guangzhou citizens who suffered from acute insomnia (insomnia severity index score >7, duration <1 month) from March to April 2020. (2) age of 18 years or older. A total of 86 participants were excluded because they did not meet criteria for acute insomnia. Finally, our study included 194 participants with acute insomnia who volunteered to participate in the program and signed written consent. We collected their demographic data and recorded the times they logged in.
Participants were divided into three groups based on the times of logins they have: low adherence (logged on 0–3 days), medium adherence (logged on 4–6 days), and high adherence (logged on 7 days). In an attempt to evaluate their degree of insomnia and efficacy, the following sleep-related scales were used:
Pre-sleep Arousal Scale (PSAS): Rating scale that measures pre-sleep somatic arousal and cognitive arousal. The scale includes two parts, and each part contains eight items respectively. The score ranges from 8 to 40. Higher score suggest a greater pre-sleep problem of somatic/cognitive arousal. The cutoff in clinical evaluation is 14 score in somatic arousal and 20 score in cognitive arousal [19]. For the Chinese version of the PSAS, the Cronbach α was 0.88 [20].
Insomnia Severity Index (ISI): Rating scale that measures severity of insomnia. The rating scale contains seven items with score ranging from 0 to 28. 0–7 score suggest no clinically significant insomnia; 8–14 score mild insomnia; 15–21 score moderate insomnia; and 22–28 score severe insomnia. For the Chinese version of the ISI, the Cronbach α was 0.81 [21].
Hospital Anxiety and Depression Scale (HADS): Rating scale that measures patients’ anxiety and depression. It consists of anxiety subscale and depression subscale. Each subscale comprises seven items. The final score ranges from 0 to 21, corresponding to clinical minimal severities (0–7), mild severities (8–10), moderate severities (11–13), and severe (14–21). For the Chinese version of the HADS, the Cronbach α is 0.77 for anxiety subscale, and 0.82 for depression subscale [22].
Baseline sale scores were collected. After the first login, the dBTI would end a week later, and participants would be reminded to complete the post-treatment scale within 3 days.
All analyses were performed using SPSS22.0. The relationship between efficacy score and adherence was analyzed by the spearman correlation analysis. In order to explore the relationship between demographic factors, sleep-related symptoms before the course and adherence, chi-square test, spearman correlation analysis and multinomial logistic regression analysis were used. The relationship between efficacy and adherence in three groups was analyzed by the repeated measures analysis of variance (ANOVA). All the analyses were two-tailed with an alpha level set at P = 0.1.
3. Result
3.1. Characteristics and adherence of the participants
After one week courses, 75 of 194 acute insomnia participants logged in for 7 days and completed all lessons. Among others, 14 didn’t log in. 18 participants logged on 1 day, 14 on 2 days, 16 on 3 days, 17 on 4 days, 21 on 5 days, and 19 on 6 days.
The low-adherence group (logged on 0–3 days) accounted for 32.0% of all participants, compared to 29.4% for the medium-adherence (logged on 4–6 days) and 38.7% for the high-adherence groups (logged on 7 days).
Table 2 demonstrates the features of eligible participants and the correlation analysis of groups with various adherences. All participants completed demographic data, ISI baseline assessments, and PSAS baseline assessments. 186 participants completed the HADS baseline assessment. The result of the single-factor analysis showed that gender (p = 0.002), PSAS somatic score (p = 0.012) and ISI score (p = 0.030) were statistically associated with adherence. The above three factors were considered to be adherence-related.
Table 2.
Comparison of demographics and sleep-related scales scores among participants with different adherences.
| Low-adherence(n = 62) | Medium-adherence(n = 57) | High-adherence(n = 75) | P-value | |
|---|---|---|---|---|
| Gender | 0.002a | |||
| Male | 10(16.1) | 26(45.6) | 22(29.3) | |
| Female | 52(83.9) | 31(54.4) | 53(70.7) | |
| Age | 37.8 ± 11.2 | 36.6 ± 11.0 | 36.6 ± 10.2 | 0.590b |
| BMI | 21.8 ± 2.7 | 22.8 ± 3.7 | 20.8 ± 2.6 | 0.162b |
| Education level | 0.304a | |||
| High school or below | 11(17.7) | 16(28.1) | 10(13.3) | |
| Bachelor degree | 36(58.1) | 30(52.6) | 45(60.0) | |
| Graduate degree | 15(24.2) | 11(19.3) | 20(26.7) | |
| Monthly Income | 0.492a | |||
| <3,000 RMB | 7(11.3) | 8(14.0) | 7(9.3) | |
| 3000–5000 RMB | 19(30.6) | 20(35.1) | 17(22.7) | |
| 5000–10000 RMB | 19(30.6) | 12(21.1) | 28(37.3) | |
| >10000 RMB | 17(27.4) | 17(29.8) | 23(30.7) | |
| PSAS somatic score | 0.012a | |||
| ≤14 | 27(43.5) | 37(64.9) | 30(40.0) | |
| >15 | 35(56.5) | 20(35.1) | 45(60.0) | |
| PSAS cognitive score | 0.812a | |||
| ≤20 | 28(45.2) | 29(50.9) | 35(46.7) | |
| >21 | 34(54.8) | 28(49.1) | 40(53.3) | |
| ISI score | 0.030a | |||
| 8–14 | 34(54.8) | 35(61.4) | 35(46.7) | |
| 15–21 | 17(27.4) | 14(24.6) | 35(46.7) | |
| 22–28 | 11(17.7) | 8(14.0) | 5(6.7) | |
| HADS anxiety score | 0.360a | |||
| ≤7 | 25(40.3) | 29(50.9) | 34(45.3) | |
| 8–10 | 16(25.8) | 10(17.5) | 21(28.0) | |
| 11–13 | 10(16.1) | 7(12.3) | 12(16.0) | |
| 14–21 | 9(14.5) | 9(15.8) | 4(5.3) | |
| HADS depression score | 0.694a | |||
| ≤7 | 28(45.2) | 31(54.4) | 34(45.3) | |
| 8–10 | 16(25.8) | 10(17.5) | 19(25.3) | |
| 11–13 | 12(19.4) | 7(12.3) | 11(14.7) | |
| 14–21 | 4(6.5) | 7(12.3) | 7(9.3) |
P-values in bold indicate statistical significance. The sample characteristics significantly associated with adherence would be further controlled in multinomial logistic regression models.
Low-adherence: logged on 0–3 days; Medium-adherence: logged on 4–6 days; High-adherence: logged on 7 days; BMI: Body Mass Index; PSAS: Pre-sleep Arousal Scale; ISI: Insomnia Severity Index; HADS: Hospital Anxiety and Depression Scale.
χ2 test.
Analysis of variance.
3.2. Factors associated with adherence
The result of multinomial logistic regression analysis on adherence-related factors is shown in Table 3 . Participants scoring 15–21 in ISI might appear higher adherence than those scoring 22–28 in ISI (OR: 4.752; 95% CI: 1.278–17.674), but there was no significant difference between participants scoring 8–14 and participants scoring 22–28. Males were less likely to show low-adherence (OR: 0.199; 95% CI: 0.082–0.481) and high-adherence (OR: 0.455; 95% CI: 0.212–0.978) than females. Participants scoring 14 and below in PSAS somatic were less likely to show low-adherence (OR: 0.332; 95% CI: 0.144–0.770) and high-adherence (OR: 0.320; 95% CI: 0.145–0.709) than participants with higher score.
Table 3.
Multinomial Logistic Regression Analysis of Adherence-related Factors.
| Low-adherence(ref: Medium-adherence) |
High-adherence(ref: Medium-adherence) |
|||||
|---|---|---|---|---|---|---|
| Regression coefficient | Odds ratio | 95% CI | Regression coefficient | Odds ratio | 95% CI | |
| Gender(ref: Female) | ||||||
| Male | −1.617 | 0.199 | (0.082–0.481)*** | −0.787 | 0.455 | (0.212–0.978)* |
| PSAS somatic score(ref: >15) | ||||||
| ≤14 | −1.101 | 0.332 | (0.144–0.770)* | −1.139 | 0.320 | (0.145–0.709)** |
| ISI score(ref: 22–28) | ||||||
| 8–14 | 0.182 | 1.199 | (0.383–3.758) | 1.021 | 2.776 | (0.763–10.093) |
| 15–21 | −0.005 | 0.995 | (0.295–3.362) | 1.559 | 4.752 | (1.278–17.674)* |
Low-adherence: logged on 0–3 days; Medium-adherence: logged on 4–6 days; High-adherence: logged on 7 days; PSAS: Pre-sleep Arousal Scale; ISI: Insomnia Severity Index; CI: confidence interval.
*P < 0.05, **P < 0.01, ***P < 0.001.
3.3. The correlation between adherence and efficiency
At the end of the one-week course, the number of participants who completed PSAS, ISI and HADS was 142, 137, and 130. In the low-adherence group, 35 (24.6%) completed PSAS, 31 (22.6%) for ISI, and 30 (23.1%) for HADS. In the mid-adherence group, 49 (34.5%) completed PSAS, 46 (33.6%) for ISI, and 45 (34.6%) for HADS. In the high-adherence group, 58 (40.8%) completed PSAS, 60 (43.8%) for ISI, and 55 (42.3%) for HADS. Table 4 shows the repeated measures ANOVA of participants in the three groups before and after treatment. Significant group effects were found for PSAS somatic score (F = 6.473, p = 0.002), PSAS cognitive score (F = 3.752, p = 0.002) and HADS anxiety score (F = 2.515, p = 0.085). Significant time effects were found for PSAS cognitive score (F = 20.869, p < 0.001), ISI score (F = 107,194, p < 0.001), HADS anxiety score (F = 12.447, p = 0.001) and HADS depression score (F = 28.990, p < 0.001). Significant group × time effects were found for PSAS somatic score (F = 2.600, P = 0.078) and ISI score (F = 2.762, p = 0.067).
Table 4.
Repeated-measures ANOVAs of measurements between three groups with different adherence from baseline to follow up.
| Baseline |
Follow-up |
Group effect | Time effect | Group × time effect | |||||
|---|---|---|---|---|---|---|---|---|---|
| Low- adherence | Medium- adherence | High- adherence | Low- adherence | Medium- adherence | High- adherence | ||||
| PSAS score | |||||||||
| Somatic | 15.6 ± 5.0 | 14.3 ± 6.3 | 15.4 ± 4.9 | 18.5 ± 9.1 | 15.3 ± 7.8 | 12.8 ± 6.4 | 0.002 | 0.992 | 0.078 |
| Cognitive | 21.6 ± 6.6 | 22.2 ± 7.1 | 21.0 ± 5.3 | 20.8 ± 9.5 | 17.9 ± 8.6 | 15.8 ± 7.1 | 0.026 | <0.001 | 0.107 |
| ISI score | 14.9 ± 5.3 | 14.5 ± 5.3 | 14.7 ± 4.2 | 10.4 ± 4.0 | 10.4 ± 4.2 | 8.3 ± 3.9 | 0.206 | <0.001 | 0.067 |
| HADS score | |||||||||
| Anxiety | 8.2 ± 4.5 | 8.2 ± 5.0 | 8.1 ± 3.4 | 7.5 ± 3.6 | 6.9 ± 3.4 | 5.8 ± 3.4 | 0.085 | 0.001 | 0.635 |
| Depression | 7.5 ± 4.0 | 7.8 ± 4.6 | 7.8 ± 4.0 | 5.5 ± 3.4 | 5.5 ± 3.3 | 4.6 ± 2.4 | 0.463 | <0.001 | 0.604 |
P-values in bold indicate statistical significance.
Low-adherence: logged on 0–3 days; Medium-adherence: logged on 4–6 days; High-adherence: logged on 7 days; PSAS: Pre-sleep Arousal Scale; ISI: Insomnia Severity Index; HADS: Hospital Anxiety and Depression Scale.
Table 4 Repeated-measures ANOVAs of Measurements between Three Groups with.
4. Discussion
Our paper provides a framework design and a course design of dBTI based on the WeChat mini-program. Other digital therapy platforms rely on 4–6 weeks of CBTI, but our team focuses on rapidly improving individuals’ insomnia symptoms, using BTI which has only one-week course. Compared with digital CBTI (dCBTI), our dBTI platform is more convenient to use and have a better personal experience for Chinese individuals. It has the characteristics which are improved development efficiency and shortened development time for Chinese developers. After reading the framework design and course design we provide, experienced teams are able to set up their own dBTI and put them into use in a fairly short time. Of course, building dBTI on platforms such as Web and mobile APP is also an option. At present, there are various dCBTI platforms in the world for clinical use. Platforms based on Web applications include Sleepio, Shuti Platform, etc., and based on mobile applications include Sleepio, Sleeprate App, CBTI Coach, Night Owl, etc. Interactive elements, managerial features and supportive motivational features are different on each platform [23]. The specific platform selection needs to be determined according to the individual habits and network policies of different countries and regions.
Nearly all online interventions feature a defect of low adherence [24], and the dBTI is no exception. Compared with off-line behavioral therapy, patients without the supervision of therapists need to have a strong will and self-discipline in order to complete all the courses [25]. Nevertheless, the feedback of our platform shows that, with only the daily reminder that comes with the system, the proportion of participants who have completed more than half of the course with medium to high adherence is 68%. Our data is from the real world study (RWS), but the completion rate of participants is no lower than that of some digital behavioral therapy clinical trials [26].
Further study on factors relative to adherence and characteristics of participants was conducted and subsequently revealed ISI score is one of the important influencing factors. Participants suffering from moderate insomnia, who scored 15–21 in ISI, were more likely to complete one-week dBTI lessons than participants scoring 8–14 and 22–28 in ISI. The possible reason for it is that participants scoring 8–14 in ISI suffered from less severity of insomnia and thus were not much highly motivated to receive treatment. Patients scoring 22–28 in ISI, on the other hand, suffered from more severe insomnia. Thereupon, their cognitive and physical functions were more impaired and they were diffident about the treatment efficacy [27]. After a few days’ lessons without notable improvement, participants with severe insomnia tended to give up and consequently failed to achieve prospective efficacy. It reminds us that we should evaluate patients’ insomnia severity in advance while we are promoting dBTI. For patients with mild and severe insomnia, notes could be sent more frequently to urge them to finish lessons, or they could be given other treatments such as health education or medication.
PSAS somatic score and gender were also associated with adherence, and the results show that lower PSAS score and men were more inclined to medium adherence. We hope participants to have as high adherence as possible, so these two factors are not suitable for making decisions to improve adherence. Previous studies have shown that age is closely related to acceptance of digital platforms [28]. Nevertheless, it is worth noting that our study showed no significant correlation between age and adherence. This may be resulted from self-selection bias, that is, older users with higher acceptance of digital medicine were more likely to participate in our dBTI, leading to their adherence not lower than that of young individuals. Besides, adherence is not significantly associated with anxiety and depression. This reminds us that we should not exclude patients with severe anxiety and depression in dBTI treatment.
Apart from the relevant factors studied in this paper, there are other measures to increase adherence. From the perspective of systems, methods like enhancing interactivity, improving individual experience and adopting the form of playing games would effectively engage people in the course, thus boosting adherence [23]. Meanwhile, it is proved that the combination of Adjunctive Wearable Technology and digitalized therapy can increase the adherence and efficacy of dBTI [29], making it one of the possible important research fields in the future.
Further research we discovers that efficacy improved with increased adherence, especially at the ISI and PSAS somatic levels. It also indicates the effectiveness of our dBTI platform. With such measures as strengthening monitoring to increase adherence of patients, better efficacy of dBTI would be accessible. Moreover, ISI, PSAS cognitive, HADS anxiety and depression in patients with acute insomnia during COVID-19 had significant time effects. In other words, even in the low-adherence group, participants’ sleep was improved after one week. It reminds us to be careful of placebo effect in studies [30]. Further research is needed to determine whether dBTI itself or the active treatment-seeking behavior alleviates symptoms for low-adherence participants.
The key of dBTI to treat insomnia is to change behavior and then to improve sleep. Therefore, only when individuals truly abide by the guide can dBTI make a difference. In other words, if individuals do not pay enough attention to dBTI in their busy daily life and have low adherence, dBTI will not play a role as expected. The design mode and the relevant analysis of adherence and efficiency demonstrated above can serve as guidelines for researchers and designers, assisting them to develop a digital intervention system with higher adherence.
5. Conclusion
This paper described in detail the course design and the framework design of dBTI. Explore the adherence-related factors of individuals and the efficiency of the system. Gender, PSAS somatic score before treatment and ISI score before treatment are those factors affecting adherence, which provides an entry point for the study of how to increase patients’ adherence. Meanwhile, we proved that adherence would affect the efficacy of dBTI-higher adherence leads to better improvement in the severity of insomnia and somatic pre-sleep arousal. dBTI, as a practical therapeutic technique, only has its significance in clinical practice. This paper exactly provides the theoretical basis for its clinical application.
6. Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board, Nanfang Hospital of Southern Medical University. The patients/participants provided their written informed consent to participate in this study.
Funding
This work was supported by the National key R&D Program of China (Grant No. 2021YFC2501500), the National Natural Science Foundation of China (Grant No. 82071488 and 81901348), the President Foundation of Nanfang Hospital, Southern Medical University (Grant No. 2019Z014) and Education Research Projects of Nanfang Hospital (Grant No. 21NJ-ZDPY01).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Jung M. Digital health care and the fourth industrial revolution. Health Care Manager. 2019;38(3):253–257. doi: 10.1097/HCM.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 2.R.S.H. Istepanian, T. Al-Anzi, m-Health 2.0: New perspectives on mobile health, machine learning and big data analytics, Methods 151(2018) 34-40. 10.1016/j.ymeth.2018.05.015. [DOI] [PubMed]
- 3.Sverdlov O., van Dam J., Hannesdottir K., Thornton-Wells T. Digital therapeutics: an integral component of digital innovation in drug development. Clin. Pharmacol. Ther. 2018;104(1):72–80. doi: 10.1002/cpt.1036. [DOI] [PubMed] [Google Scholar]
- 4.Scott B.K., Miller G.T., Fonda S.J., Yeaw R.E., Gaudaen J.C., Pavliscsak H.H., Quinn M.T., Pamplin J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed J. E Health. 2020;26(10):1226–1233. doi: 10.1089/tmj.2020.0140. [DOI] [PubMed] [Google Scholar]
- 5.Gunn H.E., Tutek J., Buysse D.J. Brief behavioral treatment of Insomnia. Sleep Med. Clin. 2019;14(2):235–243. doi: 10.1016/j.jsmc.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Germain A., Moul D.E., Franzen P.L., et al. Effects of a brief behavioral treatment for late-life insomnia: preliminary findings. J. Clin. Sleep Med. 2006;2(4):403–406. [PubMed] [Google Scholar]
- 7.Troxel W.M., Conrad T.S., Germain A., et al. Predictors of treatment response to brief behavioral treatment of insomnia (BBTI) in older adults. J. Clin. Sleep Med. 2013;9(12):1281–1289. doi: 10.5664/jcsm.3270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spielman A.J., Caruso L.S., Glovinsky P.B. A behavioral perspective on insomnia treatment. Psychiatr. Clin. NorthAm. 1987;10(4):541–553. doi: 10.1016/S0193-953X(18)30532-X. [DOI] [PubMed] [Google Scholar]
- 10.Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., Schlarb A., Frase L., Jernelöv S., Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020;29(4):13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 11.Luik A.I., Kyle S.D., Espie C.A. Digital cognitive behavioral therapy (dCBT) for Insomnia: a state-of-the-science review. Curr. Sleep Med. Rep. 2017;3(2):48–56. doi: 10.1007/s40675-017-0065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu W. Analysis on application of Wechat small program. Wireless Internet Technol. 2016;23:11–12. doi: 10.3969/j.issn.1672-6944.2016.23.004. [DOI] [Google Scholar]
- 13.Hao, Wan F., Ma N., Wang Y. Analysis of the development of WeChat mini program. J. Phys. Conf. Ser. 2018;1087(6):62040. doi: 10.1088/1742-6596/1087/6/062040. [DOI] [Google Scholar]
- 14.Sun M., Yang L., Chen W., Luo H., Zheng K., Zhang Y., Lian T., Yang Y., Ni J. Current status of official WeChat accounts for public health education. J. Public Health (Oxf) 2021;43(3):618–624. doi: 10.1093/pubmed/fdz163. [DOI] [PubMed] [Google Scholar]
- 15.He C., Wu S., Zhao Y., et al. Social media-promoted weight loss among an occupational population: cohort study using a wechat mobile phone app-based campaign. J. Med. Internet Res. 2017;19(10):357. doi: 10.2196/jmir.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang Z., et al. SSM-based intelligent WeChat Applet for pick-up. J. Phys., Conf. Ser. 1883;2021:12119. doi: 10.1088/1742-6596/1883/1/012119. [DOI] [Google Scholar]
- 17.Deng W.-X., Zhu J.-P., Liu Y.-J., Zhang Y.-G., Huang H.-Y., Zhang W.-A. Design of a WeChat learning platform for syndrome differentiation. Digital Chin. Med. 2018;1(2):143–154. doi: 10.1016/S2589-3777(19)30019-9. [DOI] [Google Scholar]
- 18.Wang J., Wang W., Zhu Q. Design and implementation of WeChat mini program for university dormitory based on SOA. J. Phys. 2018;1069(1):12086. doi: 10.1088/1742-6596/1069/1/012086. [DOI] [Google Scholar]
- 19.Puzino K., Amatrudo G., Sullivan A., Vgontzas A.N., Fernandez-Mendoza J. Clinical significance and cut-off scores for the pre-sleep arousal scale in Chronic Insomnia Disorder: a replication in a clinical sample. Behav. Sleep Med. 2020;18(6):705–718. doi: 10.1080/15402002.2019.1669604. [DOI] [PubMed] [Google Scholar]
- 20.Jan Y.W., Chen C.W., Yang C.M., Lin S.C. Validation of the Chinese version of the pre-sleep arousal scale (PSAS) Arch. Clin. Psycho. 2009;4:51–58. [Google Scholar]
- 21.Yu D. S, Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66:2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 22.Leung C.M., Wing Y.K., Kwong P.K., Shum A.L. K, Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison with the hamilton rating scale of depression. Acta Psychiatr. 1999;100:456–461. doi: 10.1111/j.1600-0447.1999.tb10897.x. [DOI] [PubMed] [Google Scholar]
- 23.Erten Uyumaz B., Feijs L., Hu J. A review of digital cognitive behavioral therapy for insomnia (CBT-I Apps): are they designed for engagement? Int. J. Environ. Res. Public Health. 2021;18(6):2929. doi: 10.3390/ijerph18062929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Christensen H., Griffiths K.M., Farrer L. Adherence in internet interventions for anxiety and depression. J. Med. Internet Res. 2009;11(2):13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beun R.J. Persuasive strategies in mobile insomnia therapy: alignment, adaptation, and motivational support. Pers. Ubiquit. Comput. 2013;17:1187–1195. doi: 10.1007/s00779-012-0586-2. [DOI] [Google Scholar]
- 26.Cheng P., Kalmbach D.A., Tallent G., Joseph C.L., Espie C.A., Drake C.L. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. 2019;42(10):150. doi: 10.1093/sleep/zsz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J. Clin. Sleep Med. 2007;15(3):7–10. [PMC free article] [PubMed] [Google Scholar]
- 28.Hieftje K., Edelman E.J., Camenga D.R., Fiellin L.E. Electronic media-based health interventions promoting behavior change in youth: a systematic review. JAMA Pediatr. 2013;167(6):574–580. doi: 10.1001/jamapediatrics.2013.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aji M., Glozier N., Bartlett D.J., Grunstein R.R., Calvo R.A., Marshall N.S., White D.P., Gordon C. The effectiveness of digital insomnia treatment with adjunctive wearable technology: a pilot randomized controlled trial. Behav. Sleep Med. 2021;20:1–14. doi: 10.1080/15402002.2021.1967157. [DOI] [PubMed] [Google Scholar]
- 30.Brody H. Meaning and an overview of the placebo effect. Perspect. Biol. Med. 2018;61(3):353–360. doi: 10.1353/pbm.2018.0048. [DOI] [PubMed] [Google Scholar]


