Abstract
OBJECTIVES
Evaluation of smoke capture efficiency of different mobile smoke evacuation devices with respect to volatile organic compounds and their noise emission.
METHODS
Electrosurgical incisions were performed on fresh porcine liver in an operating room with vertical laminar flow. The generated surgical smoke was analysed with proton-transfer-reaction mass spectrometry with and without the use of a mobile smoke evacuation system consisting of a smoke evacuator machine, a suction hose and a handpiece. The inlet of the mass spectrometer was positioned 40 cm above the specimen. Various devices were compared: a hard plastic funnel, a flexible foam funnel, an on-tip integrated aspirator of an electrosurgical knife and a standard secretion suction (Yankauer). Also, sound levels were measured at a distance of 40 cm from the handpieces’ inlet.
RESULTS
The smoke capture efficiency of the secretion suction was only 53%, while foam funnel, plastic funnel and integrated aspirator were all significantly more effective with a clearance of 95%, 91% and 91%, respectively. The mean sound levels were 68 and 59 A-weighted decibels with the plastic and foam funnel, respectively, 66 A-weighted decibels with the integrated aspirator and 63 A-weighted decibels with the secretion suction.
CONCLUSIONS
Carcinogenic, mutagenic and reprotoxic volatile organic compounds in surgical smoke can be efficiently reduced by mobile smoke evacuation system, providing improved protection for medical personnel. Devices specifically designed for smoke evacuation are more efficient than standard suction tools. Noise exposure for the surgeon was lowest with the flexible foam funnel and higher with the other handpieces tested.
Keywords: Smoke, Plume, Electrocautery, Evacuation system, Mass spectrometry, Volatile organic compound
Surgical smoke contains inorganic, small organic and fragments of larger biological compounds.
INTRODUCTION
Surgical smoke contains inorganic, small organic and fragments of larger biological compounds. In addition, fragments of bacteria or viruses as well as particles (carbon with associated small and large molecules) and aerosols/bioaerosols are present [1, 2]. The chemical compounds include volatile organic compounds (VOCs), which are often gases even at room temperature with high vapour pressure. Therefore, the removal of VOCs from the operating theatre is not trivial. Since some of these VOCs may pose a significant health hazard to medical personnel, especially with repeated exposure, safety precautions are indicated. We have previously demonstrated that surgical masks and current smoke evacuations systems may provide only insufficient protection from toxic and/or carcinogenic compounds of surgical smoke [3]. Our aim was to evaluate the smoke capture efficiency of different mobile smoke evacuation system (SES) and their handpieces in terms of VOCs and to assess the noise exposure for the operator when using these handpieces.
MATERIALS AND METHODS
Formal ethics approval was waived by the cantonal ethics committee (Kantonale Ethikkommission, KEK, Bern) because neither patient data nor any patient tissue was used for the experiments conducted in this study.
Electrosurgical smoke was produced by the application of radiofrequency current on porcine liver tissue in an open surgery model in the operating theatre, which was equipped with a vertical laminar flow of 35–40 l/min (Fig. 1). Tissue specimens were purchased fresh from the butcher on the day of the experiments and were at room temperature (∼24°C) at the beginning of the experiments. The tissue was placed on a sheet of tin foil serving as the neutral electrode, which in turn was placed in a plastic box (length: 40 cm, width: 20 cm, height: 5 cm) that was positioned on the operating table. The inlet of the mass spectrometer (Vocus PTR-TOF, TOFWERK AG, Thun, Switzerland) had a diameter of 0.5 cm for smoke collection and was placed 40 cm above the tissue specimens (according to the average distance of the surgeon’s mouth/nose as measured during routine thoracic surgical procedures). Through this inlet, the air samples were directly and continuously transferred to the mass spectrometer via a heated suction catheter. For each experimental condition, 10 electrosurgical cuts with a length of ∼3 cm and an activation time of 10 s each were performed with a stainless steel spatula electrode of a monopolar electrosurgical knife powered by a VIO® 300 D generator (both Erbe Elektromedizin GmbH, Tuebingen, Germany). Generator settings were SPRAY COAG E2 mode and a power limit of 80 W. These settings are most commonly used in the operating theatre (OR) of our thoracic surgical unit. In between the experimental conditions, a break of 2–3 min was taken until the mass spectrometer showed that the indicator VOC concentrations were back to baseline levels (as measured before the beginning of the experiments).
Figure 1:
Experimental setup. Tin foil with neutral electrode. Four different evacuation instruments/handpieces were examined: an integrated aspirator of an electrosurgical knife, a hard plastic suction funnel, a self-adhesive flexible foam suction funnel and a secretion suction tip (type Yankauer). NE: neutral electrode; RF: radiofrequency.
Surgical smoke evacuation system: IES 3
The basic components of a mobile SES are a smoke evacuator machine with a vacuum pump and a filter system, a suction hose and a handpiece/evacuation instrument. The IES 3, manufactured by Erbe Elektromedizin GmbH (Tuebingen, Germany), was used as the surgical smoke evacuator machine (Fig. 2). The IES 3 is designed to reduce and eliminate surgical smoke, bioaerosols and odours during surgical procedures. It incorporates 2 motors/turbines with which aspiration amounts up to 300 l/min (with inserted filter cartridge) may be set. The series-connected turbines increase the maximum achievable suction pressure. Thus, an increased volume flow is obtained depending on the instrument connected and the response of the suction is accelerated. The motors carry surgical smoke aspirated from the surgical field to a filter via a suction hose. The filter has a 3-stage design: the first stage, which uses ceramic paper as the filter material, acts as a pre-filter that eliminates large particles and liquid components. The second stage, which uses two layers of high-performance activated carbon, eliminates and absorbs odours and volatile compounds. The third stage is an Ultra-Low Penetration Air (ULPA) filter that retains fine particles and microorganisms down to 0.10 μm with an efficiency of 99.9995% (according to DIN EN 1822-3:2011 and EN 1822-5:2011).
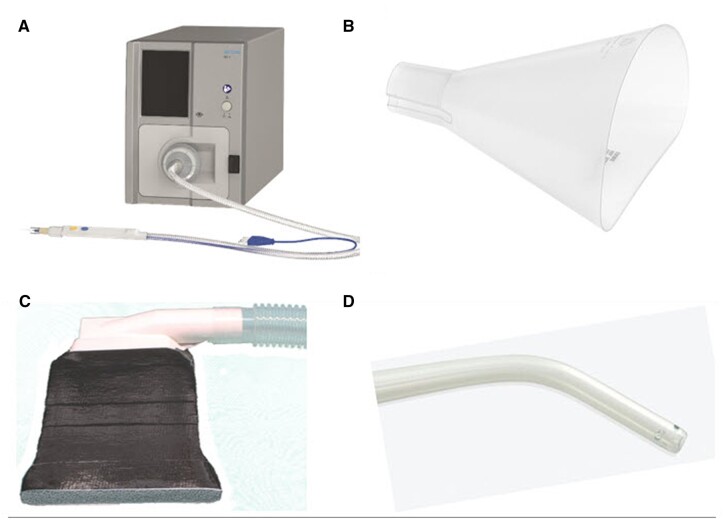
Figure 2:
(A) Smoke evacuator and electrosurgical knife with an integrated aspirator. (B) Hard plastic suction funnel. (C) Self-adhesive flexible foam suction funnel. (D) Secretion suction tip.
Smoke evacuation instruments
The evacuation instrument was either an integrated aspirator of a monopolar electrosurgical knife for the IES 3 (Fig. 2A, telescoping with spatula electrode, Erbe Elektromedizin GmbH, Tuebingen, Germany), a hard plastic suction funnel (Fig. 2B, Erbe Elektromedizin GmbH), a self-adhesive flexible foam suction funnel (Fig. 2C, miniSQUAIR® by Nascent Surgical LLC, Eden Prairie, MN, USA) or a Yankauer suction tip (Fig. 2D, flexible, big, CH22; Cardinal Health Switzerland 515 GmbH, Zug, Switzerland), intended to remove blood and similar liquids during surgery. Each evacuation instrument was used with the IES 3 except the Yankauer suction tip, which was used with the integrated OR vacuum as is common practice in the OR of our thoracic surgical unit. The volume flow rate of the mobile SES was adjusted to 100% suction power (Table 1).
Table 1:
Properties and settings of mobile smoke evacuation systems in this study
"/>
| Evacuation instrument | Hose length (m) | Smoke evacuator machine: settinga | Volume flow rate (l/min) |
|---|---|---|---|
| Integrated aspirator of an electrosurgical knife | 3.0 | IES 3: Turbo | 135 |
| Hard plastic suction funnel | 2.7 | IES 3: 70% | 235 |
| Self-adhesive flexible foam suction funnel (miniSQUAIR)b | 2.5 | IES 3: 80% | 260 |
| Secretion suction tip | 3.0 | OR vacuum: Max. (corresponds to IES 3: 80%) | 65 |
Smoke evacuator machine setting was adjusted for maximum possible volume flow with each instrument.
The device was modified to work with the IES 3, i.e. the width of funnel opening was reduced to 10 cm for equal suction capability per area with a reduced volume flow rate (260 l/min) compared to recommended volume flow rate (∼700 l/min).
Data analysis
Data were analysed using Tofware, a TOF data analysis software package (TOFWERK AG, Thun, Switzerland), SciLab V.6.1.0 (Scilab Enterprises S.A.S, Rungis, France) and GraphPad Prism V.7.05. Data are reported as medians with interquartile range for each experimental condition (i.e. 10 surgical incisions). The mass calibration of the spectra was done with internal water clusters and benzene, toluene and xylene peaks. The independently verified mass accuracy using other known peaks in the spectrum (i.e. acetone) was verified to be <3 parts per million, allowing molecular compositions to be assigned from the mass spectra. The resolving power of the instrument was RFWHM = 5000, allowing reliable separation of isobars in the region of the mass spectrum of interest. When possible the measured isotopic distribution was used as an additional constraint to help confirm molecular assignment in addition to the mass accuracy of the instrument.
Selection of volatile organic compounds for analysis
A literature search in the PubMed database (May 2021) comprised the following search terms: ‘chemical composition’ AND ‘surgical smoke’, ‘volatile organic compounds’ AND ‘surgical smoke’, ‘health hazard’ AND ‘surgical smoke’, ‘liver’ AND ‘surgical smoke’, ‘porcine liver’ AND ‘smoke’, ‘pig liver’ AND ‘smoke’, ‘air contaminants’ AND ‘medical application’, ‘toxic byproducts’ AND ‘surgery’. These search terms yielded 68 results and thereof 16 original research articles [3–18] contained VOC analyses of laser-generated or electrosurgical smoke and were included as references to accumulate a list of candidate VOCs contained in the surgical smoke from porcine liver. In addition, 1 review article [19] and 2 relevant articles [20,21], not listed in the PubMed database, were included. Several of these articles explicitly refer to electrosurgical smoke generated from porcine liver tissue [4, 16, 18, 20], which was also used in this study. These publications were given preferential consideration. On the one hand, the final selection of VOCs was based on this literature search and, on the other hand, on the observed concentrations of individual ion identities in a separate baseline/control experiment without the additional use of a mobile SES. A general detection limit of 50 parts per trillion by volume was defined, corresponding approximately to the mean detection limit of ion identities measurable with the mass spectrometer. VOC concentrations were measured both 40 cm above the tissue (similar to the oral/nasal position of first surgeon) and in the exhaust of the smoke evacuator machine. VOCs that could not be measured, e.g. do not ionize, could not be included, and VOCs that are not carcinogenic, mutagenic, reprotoxic and not toxic if inhaled were also excluded (Fig. 3). After exclusion of 95 VOCs in total, 30 VOCs, which were matched to 24 ion identities, were identified for the definition of total VOC concentration (TVOC). The calculation of smoke capture efficiency was based on the analysis of this custom TVOC concentration in test and control conditions.
Figure 3:

Selection of volatile organic compounds for further analyses in this study. pptv: parts per trillion by volume; TVOC: total VOC concentration; VOC: volatile organic compound.
Smoke capture efficiency
Smoke capture efficiency in the individual test conditions was defined as the percentage of removed TVOC concentration relative to the baseline/control condition without the additional use of a mobile SES measured 40 cm above the tissue. In the baseline measurement, TVOC concentration increased approximately by 20 ppbv, i.e. the removal of e.g. 10 ppbv translated to a smoke capture efficiency of 50%.
Noise exposure
Sound levels were measured in a separate bench test to evaluate the noise exposure for the operator due to the different handpieces in this study. A sound level meter (Trotec SL400, Trotec GmbH, Heinsberg, Germany) was positioned 40 cm from the inlet of each handpiece. The integrated data logger of the sound level meter was used to record the sound level during 30 s activation of the smoke evacuator machine with the settings specified in Table 1. Mean sound levels with standard deviation are reported from the middle 28 s, excluding the onset and offset of the activation of the smoke evacuator.
RESULTS
Volatile organic compounds identified in surgical smoke
According to the European CMR Report (EU regulation 1272/2008, Table 3 Annex VI CLP) of carcinogenic, mutagenic and reprotoxic (CMR) substances and the globally harmonized system for hazard classification, the generated surgical smoke from the porcine liver contained four Class 1 CMR substances (CMR or probably CMR), 6 Class 2 CMR substances (suspected to be CMR) and 18 further substances, which are toxic if inhaled according to the globally harmonized system for hazard classification. Two not-CMR and not-toxic isomers (pyrrole and indane) are also listed for completeness (Table 2). The Class 1 CMR substances were 1,3-butadiene, benzene, formaldehyde and acrylonitrile. The Class 2 CMR substances were furfural, toluene, phenol, styrene, crotonaldehyde and allyl cyanide. Amongst the further substances, the ones with the highest concentrations were methanol and acetonitrile.
Table 2:
List of VOCs analysed in this study
| VOC name | Ion identity | European CMR Report classification | Relevant GHS classification(s) regarding toxicity | Lowest 8 h limit value worldwidea (ppm) [ISO country code] |
|---|---|---|---|---|
| Class 1 CMR (CMR or probably CMR) | ||||
| 1,3-Butadiene | C4H6H+ | C-1A and M-1B | n/a | 0.05 [NZL] |
| Benzene | C6H6H+ | C-1A and M-1B | H372 | 0.05 [NZL] |
| Formaldehyde | CH2OH+ | C-1B and M-2 | H331 | 0.016 [USA] |
| Acrylonitrile | C3H3NH+ | C-1B | H331, H335 | 0.05 [NZL] |
| Class 2 CMR (suspected to be CMR) | ||||
| Furfural | C5H4O2H+ | C-2 | H331, H335 | 0.2 [NZL] |
| Toluene | C7H8H+ | RD-2 | H373 | 14 [LVA] |
| Phenol | C6H6OH+ | M-2 | H331, H373 | 1 [AUS, DNK, NZL, NOR, SWE] |
| Styrene | C8H8H+ | RD-2 | H332, H372 | 10 [SWE] |
| Crotonaldehyde | C4H6OH+ | M-2 | H330, H335, H373 | 0.1 [FIN] |
| Allyl cyanide | C4H5NH+ | n/a but H360 | H331, H373 | n/a |
| Pyrrole (not CMR) | n/a | n/a | ||
| Toxic substances | ||||
| Methanol | CH4OH+ | n/a | H331, H370 | 100 [DEU, NOR] |
| Acetonitrile | C2H3NH+ | n/a | H319, H332 | 10 [DEU] |
| Acetone | C3H6OH+ | n/a | H319, H336 | 125 [NOR] |
| Propanal | n/a | H319, H335 | 20 [BEL, CAN, FIN, IRL, ESP] | |
| Propionitrile | C3H5NH+ | n/a | H319, H332 | 0.040 [ROU] |
| Methanethiol | CH4SH+ | n/a | H331 | 0.5 [18 countries] |
| ‘C5 Aldehydes’ | ||||
| Pentanal | C5H10OH+ | n/a | H319, H335, H332 | 25 [NOR] |
| Isovaleraldehyde | H319, H335 | 10 [AUT, DEU] | ||
| 2-Methylbutyraldehyde | H319, H335 | n/a | ||
| 2-Methylbutanenitrile | C5H9NH+ | n/a | H331 | n/a |
| Isovaleronitrile | C5H9NH+ | n/a | H319, H335 | n/a |
| Pyridine | C5H5NH+ | n/a | H332 | 1 [BEL, CAN, FIN, NZL, ESP] |
| Butyrolactone | C4H6O2H+ | n/a | H319, H331, H336 | 50 [DNK, FIN] |
| 3-Methyl-2-butenal | C5H8OH+ | n/a | H318, H331 | n/a |
| Methyl methacrylate | C5H8O2H+ | n/a | H335 | 10 [FIN] |
| 2,5-Dimethylfuran | C6H8OH+ | n/a | H319, H335 | n/a |
| 3-Methylstyrene | C9H10H+ | n/a | H319, H332, H335 | 20 [DEU] |
| Indane (not toxic) | n/a | n/a | n/a | |
| Propylbenzene | C9H12H+ | n/a | H335 | n/a |
Source: GESTIS International Limit Values database.
CMR: carcinogenic, mutagenic, reprotoxic; ppm: parts per million; VOC: volatile organic compound.
Permissible exposure limits
The permissible exposure limits for specific compounds are set by national institutes dealing with occupational health and safety. Typically, these institutes define 2 limit values: one refers to a long-term average (8 h) and the second to a short-term average (15 min) or a ceiling limit value that must not be exceeded. Since there is no global consensus on these limit values, we have considered the lowest long-term (8 h) limit value worldwide (Table 2). These permissible exposure limits were not exceeded for any specific VOC even without the use of an additional mobile SES (Fig. 4).
Figure 4:
Median (± interquartile range) concentration increase of volatile organic compounds without mobile smoke evacuation system measured at the oral/nasal position of the experimenter/chief surgeon (40 cm above tissue). Permissible exposure limits were not exceeded for any specific volatile organic compound. Formaldehyde, acetone/propanal and propylbenzene showed a decrease in concentration but were included since they showed an increase (>50 parts per trillion by volume) in the exhaust of the smoke evacuator. ppbv: parts per billion by volume.
Smoke capture efficiency
The calculated percentage smoke capture efficiency of the integrated aspirator of the electrosurgical knife and the hard plastic suction funnel were 91%, the self-adhesive flexible foam suction funnel (miniSQUAIR) achieved 95%, while the secretion suction tip performed worse with 53% (Fig. 5). There was no significant difference in smoke capture efficiency of integrated aspirator and hard plastic funnel (P > 0.99). However, all other comparisons of smoke capture efficiency showed highly significant differences (P < 0.0001 in each case).
Figure 5:

Median total VOC concentration concentration (± interquartile range) of test and control conditions. Calculated percentage smoke capture efficiency of different smoke evacuation instruments are given in bold numbers. The endorsed evacuation instruments performed better (>90%) than the standard secretion suction tip (53%), which is often used as a replacement for this functionality. *Significant difference P < 0.0001, n.s.: not significant; TVOC: total VOC concentration.
Noise exposure
The mean sound levels at a distance of 40 cm from the inlet of the respective handpiece were 66 A-weighted decibels (dBA) with the integrated aspirator of the electrosurgical knife, 68 dBA with the hard plastic suction funnel, 59 dBA with the self-adhesive flexible foam suction funnel (miniSQUAIR) and 63 dBA with the secretion suction tip. The mean sound level of each handpiece was significantly different from the mean values of all other handpieces (P < 0.0001 in each case) (Fig. 6).
Figure 6:

Sound level of different smoke evacuation instruments measured at a distance of 40 cm from the inlet of the respective handpiece. Mean and standard deviation. The means of all instruments were significantly different from each other (P-value <0.0001 in each case). dBA: A-weighted decibels.
DISCUSSION
Health hazard from surgical smoke is still underestimated and endorsed smoke evacuation devices are not used in every case (hospital and outpatient) [22]. The health risk posed by surgical smoke is not primarily based on the concentration of a single VOC, but rather on the total concentration of VOCs and other chemical and biological compounds and the daily exposure to this mixture. Permissible exposure limits of individual VOCs were not exceeded in our study setting, even without the use of an additional mobile SES. From a legal point of view, occupational health and safety are ensured in a modern operating theatre such as in our study setting, which is equipped with a state-of-the-art room ventilation system. Nevertheless, our study shows that health hazards from the mixture of substances in surgical smoke and repeated exposure can be significantly reduced by the consistent use of additional mobile evacuation systems designed for this purpose. Currently, not every operating theatre is equipped with a room ventilation system, and the mobile evacuation system is a more economical solution in such a case.
Surgical procedures are usually performed in an operating room equipped with a positive laminar airflow system to reduce surgical site infections and it contributes at the same time to the evacuation of VOCs. In cases where surgery must be performed in a room equipped with a negative-pressure ventilation system because of infectious conditions, smoke evacuation devices are the only solution to prevent or reduce the exposition to VOCs.
The long-term consequences of surgical teams after exposure to VOCs in an operating theatre are difficult to detect. Nevertheless, the toxicity of various VOCs, which arise when electrocautery devices are used in the OR, is well known and precautions should be taken. Yokuda et al. showed the effectiveness of various evacuation systems [22,23] and especially with the emergence of infectious patients, equipment with such evacuation devices is highly recommended. As Schultz et al. [24] reported , smoke evacuation devices reduce the amount of aerosolized viable bacteria, thus reducing the contamination rate of surgical wounds.
Another observation was that the whole ventilation system of the operating theatre is most efficient concerning the reduction and exposition to VOCs but only smoke evacuation devices can prevent fire risk that can occur when the skin is cut with a monopolar electrosurgical knife after skin disinfection with chlorhexidine-alcohol [24,25].
A further important aspect that was not separately addressed in our experiments, but has become increasingly essential since the coronavirus disease 2019 pandemic started, is the evacuation/filtering of the aerosol particles that contain virus material and might travel through the air in the operating theatre. An experimental study showed [26] that the minimum size of respiratory particles carrying SARS-CoV-2 is 4.7 μm. Taking these values into consideration and knowing that the SESs carry/have filters that can ‘block’ particles larger than 0.1 μm, we can assume that the various SES could potentially offer some benefit in controlling the spread of coronavirus disease 2019 in the OR. Smoke evacuation devices have been shown to reduce the amount of aerosolized viable bacteria [24].
The smoke capture efficiency of the integrated aspirator of the electrosurgical knife, the hard plastic suction funnel and the self-adhesive flexible foam suction funnel were comparable and very high (>90%), while the secretion suction tip performed significantly worse (53%). Although in our experiments, the flexible foam funnel was the device combining most effective smoke evacuation (i.e. reduction of 95%) with the lowest noise emission (59 dB), this device can only be used for very limited incisions and in case of a very small operative field. For a broader applicability, the integration of the smoke evacuation into the surgical knife seems to be the better option, offering better flexibility together with very good smoke evacuation (i.e. reduction of 91%) and acceptable noise emission rates (66 dB).
Limitations
The experiments were restricted to the analysis of VOCs and only quantitative measurements were made and observed. No conclusions on the direct/immediate or long-term harm on surgeons can be made. The experiments were not designed for infectious particles and thus a reduction of infectious risks cannot be concluded, although the results can be possibly extrapolated based on the filtration properties of the device.
CONCLUSION
Smoke evacuation devices are an economical and efficient alternative or complementary system to an operating theatre equipped with laminar airflow system. Their daily usage can drastically reduce the exposition to VOCs. While the flexible foam suction device was the most effective tool with the least noise emission rates, it is only applicable for limited surgical incisions. The cautery-integrated smoke evacuation device on the other hand seems to be the optimal solution also for larger incision, combining good evacuation properties with low noise emission rates. Concerning the latter, it should be mentioned that none of the devices produced higher dBA levels than those emerging during a normal conversation.
ACKNOWLEDGEMENTS
We thank Lars Blobel and Klaus Fischer for their excellent laboratory assistance.
Funding
This study was funded by the Lungenliga Bern (awarded to Gregor J. Kocher) and the dedicated smoke evacuation system, including the different inlet pieces, was provided by Erbe Elektromedizin GmbH.
Conflict of interest: Ulrich Biber is an employee of Erbe Elektromedizin GmbH. Otherwise, the authors declare no conflicts of interests.
Data availability statement
All relevant data are within the manuscript and its Supporting Information files.
Author contributions
Thanh-Long Nguyen: Investigation; Validation; Writing—original draft; Writing—review & editing. Konstantinos Gioutsos: Investigation; Validation; Writing—original draft; Writing—review & editing. Ulrich Biber: Methodology; Resources; Supervision; Validation. Markus D. Enderle: Investigation; Methodology; Project administration; Resources; Validation; Visualization. Abigail Koss: Resources; Supervision; Validation. Gregor J. Kocher: Conceptualization; Data curation; Formal analysis; Funding acquisition; Methodology; Writing—review & editing.
Conflict of interest: Ulrich Biber and Markus Enderle are both employees of Erbe Elektromedizin GmbH.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Bartosz Kubisa, Paolo Scanagatta and the other anonymous reviewers for their contribution to the peer review process of this article.
ABBREVIATIONS
- CMR
Carcinogenic, mutagenic, reprotoxic
- dBA
A-weighted decibels
- SES
Smoke evacuation system
- TVOC
Total VOC concentration
- VOC
Volatile organic compound(s)
REFERENCES
- 1. Tomita Y, Mihashi S, Nagata K, Ueda S, Fujiki M, Hirano M. et al. Mutagenicity of smoke condensates induced by CO2-laser irradiation and electrocauterization. Mutat Res 1981;89:145–9. [PubMed] [Google Scholar]
- 2. Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A.. Surgical smoke and infection control. J Hosp Infect 2006;62:1–5. [DOI] [PubMed] [Google Scholar]
- 3. Kocher GJ, Sesia SB, Lopez-Hilfiker F, Schmid RA.. Surgical smoke: still an underestimated health hazard in the operating theatre: still an underestimated health hazard in the operating theatre. Eur J Cardiothorac Surg 2019;55:626–31. [DOI] [PubMed] [Google Scholar]
- 4. Hensman C, Baty D, Willis RG, Cuschieri A.. Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. An in vitro study. Surg Endosc 1998;12:1017–9. [DOI] [PubMed] [Google Scholar]
- 5. Choi SH, Kwon TG, Chung SK, Kim T-H.. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc 2014;28:2374–80. [DOI] [PubMed] [Google Scholar]
- 6. Al Sahaf OS, Vega-Carrascal I, Cunningham FO, McGrath JP, Bloomfield FJ.. Chemical composition of smoke produced by high-frequency electrosurgery. Ir J Med Sci 2007;176:229–32. [DOI] [PubMed] [Google Scholar]
- 7. Ha HI, Choi MC, Jung SG, Joo WD, Lee C, Song SH. et al. Chemicals in surgical smoke and the efficiency of built-in-filter ports. JSLS 2019;23:e2019.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cheng M-H, Chiu C-H, Chen C-T, Chou H-H, Pao L-H, Wan G-H.. Sources and components of volatile organic compounds in breast surgery operating rooms. Ecotoxicol Environ Saf 2021;209:111855. [DOI] [PubMed] [Google Scholar]
- 9. Choi SH, Choi DH, Kang DH, Ha Y-S, Lee JN, Kim BS. et al. Activated carbon fiber filters could reduce the risk of surgical smoke exposure during laparoscopic surgery: application of volatile organic compounds. Surg Endosc 2018;32:4290–8. [DOI] [PubMed] [Google Scholar]
- 10. Lee T, Soo J-C, LeBouf RF, Burns D, Schwegler-Berry D, Kashon M. et al. Surgical smoke control with local exhaust ventilation: experimental study. J Occup Environ Hyg 2018;15:341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Benson SM, Maskrey JR, Nembhard MD, Unice KM, Shirley MA, Panko JM.. Evaluation of personal exposure to surgical smoke generated from electrocautery instruments: a pilot study. Ann Work Expo Health 2019;63:990–1003. [DOI] [PubMed] [Google Scholar]
- 12. Hahn KY, Kang DW, Azman ZAM, Kim S-Y, Kim S-H.. Removal of hazardous surgical smoke using a built-in-filter trocar: a study in laparoscopic rectal resection. Surg Laparosc Endosc Percutan Tech 2017;27:341–5. [DOI] [PubMed] [Google Scholar]
- 13. Yeganeh A, Hajializade M, Sabagh AP, Athari B, Jamshidi M, Moghtadaei M.. Analysis of electrocautery smoke released from the tissues frequently cut in orthopedic surgeries. World J Orthop 2020;11:177–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dobrogowski M, Wesołowski W, Kucharska M, Sapota A, Pomorski LS.. Chemical composition of surgical smoke formed in the abdominal cavity during laparoscopic cholecystectomy–assessment of the risk to the patient. Int J Occup Med Environ Health 2014;27:314–25. [DOI] [PubMed] [Google Scholar]
- 15. Liu Y, Zhao M, Shao Y, Yan L, Zhu X.. Chemical composition of surgical smoke produced during the loop electrosurgical excision procedure when treating cervical intraepithelial neoplasia. World J Surg Onc 2021;19:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gianella M, Sigrist MW.. Infrared spectroscopy on smoke produced by cauterization of animal tissue. Sensors (Basel) 2010;10:2694–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pierce JS, Lacey SE, Lippert JF, Lopez R, Franke JE.. Laser-generated air contaminants from medical laser applications: a state-of-the-science review of exposure characterization, health effects, and control. J Occup Environ Hyg 2011;8:447–66. [DOI] [PubMed] [Google Scholar]
- 18. Wu JS, Luttmann DR, Meininger TA, Soper NJ.. Production and systemic absorption of toxic byproducts of tissue combustion during laparoscopic surgery. Surg Endosc 1997;11:1075–9. [DOI] [PubMed] [Google Scholar]
- 19. Barrett WL, Garber SM.. Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 2003;17:979–87. [DOI] [PubMed] [Google Scholar]
- 20. Krones CJ, Conze J, Hoelzl F, Stumpf M, Klinge U, Möller M. et al. Chemical composition of surgical smoke produced by electrocautery, harmonic scalpel and argon beaming—a short study. Eur Surg 2007;39:118–21. [Google Scholar]
- 21. Cesaretti M, , Le Zarzavadjian Bian A.. Surgical smoke management should be a priority during or after COVID-era. Br J Surg 2021;108:e251. [DOI] [PubMed] [Google Scholar]
- 22. Michaelis M, Hofmann FM, Nienhaus A, Eickmann U.. Surgical smoke-hazard perceptions and protective measures in German operating rooms. Int J Environ Res Public Health 2020;17:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tokuda Y, , OkamuraT, , MarutaM, , OritaM, , NoguchiM, , Suzuki T. et al. Prospective randomized study evaluating the usefulness of a surgical smoke evacuation system in operating rooms for breast surgery. J Occup Med Toxicol 2020;15:13. 10.1186/s12995-020-00259-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schultz L. Can efficient smoke evacuation limit aerosolization of bacteria? AORN J 2015;102:7–14. [DOI] [PubMed] [Google Scholar]
- 25. Carmichael H, , SamuelsJM, , WikielKJ, , RobinsonTN, , BarnettCC, , Jones TS. et al. Surgical Smoke Evacuators Reduce the Risk of Fires From Alcohol-Based Skin Preparations. Surg Laparosc Endosc Percutan Tech 2019;29:e94–7. 10.1097/SLE.0000000000000734 31633578 [DOI] [PubMed] [Google Scholar]
- 26. Prather KA, Wang CC, Schooley RT.. Reducing transmission of SARS-CoV-2. Science 2020;368:1422–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.