Abstract
The stability and compatibility of ceftazidime have been examined in the context of its potential use in concentrated solutions for continuous infusion in patients suffering from severe nosocomial pneumonia and receiving other intravenous medications by the same route. Ceftazidime stability in 4 to 12% solutions was found satisfactory (<10% degradation) for 24 h if kept at a temperature of 25°C (77°F) maximum. Studies mimicking the simultaneous administration of ceftazidime and other drugs as done in clinics showed physical incompatibilities with vancomycin, nicardipine, midazolam, and propofol and a chemical incompatibility with N-acetylcystein. Concentrated solutions (50 mg/ml) of erythromycin or clarithromycin caused the appearance of a precipitate, whereas gentamicin, tobramycin, amikacin, isepamicin, fluconazole, ketamine, sufentanil, valproic acid, furosemide, uradipil, and a standard amino acid solution were physically and chemically compatible.
In their original review, Craig and Ebert (7) pointed out to the many potential advantages of the administration of β-lactams by continuous infusion (optimization of outcome based on their pharmacodynamic properties [time-dependent antibiotics {5, 6}] as well as pharmacoeconomic advantages [decrease in the amount of drug which needs to be administered each day and reduction of nursing workload {21}]). Yet, because β-lactams are known to be unstable in aqueous media (intrinsic fragility of the β-lactam ring), particular attention must be paid to the practical conditions of this type of administration. β-Lactam antibiotics are also known to be chemically and physically incompatible with many other drugs. Even though several authors have examined the stability and degradation of ceftazidime in aqueous solutions, sometimes specifically in view of its potential use by continuous infusion (8, 10, 11, 18, 26, 28–30, 34, 37), none of them has specifically tested the potential temperatures and concentrations that may be encountered in the treatment of intensive care patients. The same consideration applies also largely to the problem of drug incompatibilities, although useful information has already been assembled in this context (2, 14, 16, 23, 31, 33). The present study was therefore initiated to specifically and critically assess the stability and compatibility of ceftazidime within the context of its potential use by continuous infusion for patients hospitalized in intensive care units for severe nosocomial pneumonia. We selected ceftazidime for normative studies, since this third-generation cephalosporin has a well-established efficacy in empirical therapy for this type of patient (9). Moreover, pharmacokinetic studies have indicated that a stable concentration of ∼20 mg/liter in serum can be reached using acceptable daily doses (∼4 g) of ceftazidime in humans (17, 21).
Overall design of study and methods.
We wanted to mimic as closely as possible a projected routine use of ceftazidime. Successful therapy was considered to require a stable serum drug concentration of 25 mg/liter, i.e., above most accepted breakpoints for ceftazidime, which can be achieved with a daily infusion of 6 g/day. This would also yield an area under the concentration time curve from 0 to 24 h of 600 mg × h/liter (which some studies have ruled optimal for β-lactams when considering organisms for which the MIC is up to 4 mg/liter [25]) and would also be within the the limits of the registered daily dosages of ceftazidime in most countries. Clinical usage dictated that this amount of drug be administered from a single 48-ml syringe (as used in most conventional infusion pumps) maintained at room temperature and changed only once daily (to minimize handling risks and costs). Finally, the intravenous line might need to be used for simultaneous administration of other parenteral drugs commonly needed for patients with severe, life-threatening nosocomial pneumonia.
All solutions of ceftazidime were prepared using the branded product distributed for hospital usage in Belgium and contained up to 6 g of ceftazidime per 48 ml. The pH of the solutions was ∼7.4, and unless stated otherwise, no adjustment of pH was made. After the solutions had been maintained at appropriate temperatures for the necessary lengths of time, the ceftazidime content of the solutions was determined by high-pressure liquid chromatography (HPLC) in comparison with freshly prepared standards (Lichrosorb 100RP-18 column [25 by 0.4 cm; 5-μm pore size; Merck KGaA, Darmstadt, Germany] with Novapack C18 precolumn; isocratic elution with 10 mM sodium acetate buffer [pH 4.0]; acetonitrile [89:11 vol/vol]; UV detector [absorption wavelength, 254 nm]; range of linearity, 0 to 400 μg/ml [r2 = 0.999]; and quality control samples with each series of assay [maximum deviation, 5%; intraday and interday coefficients of variation, ∼0.3 and ∼5%, respectively]). Stability was considered satisfactory if the ceftazidime content remained within 90% of its original value at any time point (1). Degradation products were detected and characterized by HPLC analysis coupled with mass spectrometry (Finnigan LCQ mass spectrometer, Thermoquest, San Jose, Calif., with an Electrospray ionization and data processing with Xcalibur software), as well as by cochromatography with genuine samples of the putative degradation products when available.
Compatibility was tested by mixing ceftazidime at its maximally projected concentration (∼12% [wt/vol]) and each potentially coadministered drug (at the highest commercially available or clinically used concentration) in a volume ratio corresponding to their respective projected flow rates (2 ml/h for ceftazidime and the flow rate compatible with the highest accepted daily dosage and schedule of administration of each of the other drugs, as routinely performed in our clinical environment [Table 1]). All drugs were obtained and used under the pharmaceutical form distributed in Belgium for parenteral use by or on behalf of the original marketing authorization holder. Physical compatibility was assessed by the naked eye for signs of precipitation or other evidence of alteration (repeated mirroring) followed by independent, professional examination using an Allen LV28 Liquid Viewer (P. W. Allen & Co. Ltd., Tewkesbury, United Kingdom) operated with two polarizing filters. Chemical compatibility was assessed by determining the ceftazidime content by HPLC, followed by thin-layer chromatography if a decrease of the ceftazidime content of ≥10% was detected in HPLC without the simultaneous appearance of an identifiable new compound or of a ceftazidime degradation product. The chemical intactness of the accompanying drug has not been tested systematically. For compounds administered in a short period of time, indeed, the molar ratio of each drug to ceftazidime was usually much greater than 1, making a loss of ceftazidime a more accurate means of evidencing a chemical reaction between them. The intactness of the aminoglycosides was, however, systematically examined, since interaction between these drugs and β-lactams has been documented (22). No evidence of degradation was noted, using an automated fluorescence polarization immunoassay (Abbott TdX system, Abbott Laboratories, Abbott Park, Ill.; Dainabot Co. Ltd., Tokyo, Japan) with standards prepared in the same vehicle as the samples for constructing the calibration curves (intraday coefficient of variation, <5%; all assays were done in 1 day). Concerning compounds administered over a 24-h period and for which no physical instability was detected, available pharmaceutical information indicated no interaction with ceftazidime (31).
TABLE 1.
Drugs, conditions, and results of compatibility studies mimicking the coadministration of ceftazidime with other drugs through the same line of infusiona
| Drug | Dose (mg) | Vol per administration (ml) | Time of infusion (h) | Drug:ceftazidime ratio in final infusate
|
Resultb | |
|---|---|---|---|---|---|---|
| Wt ratio | Molar ratio | |||||
| Anti-infectives | ||||||
| Amikacin | 1,500c | 100 | 0.25 | 27.7 | 25.9 | c |
| Isepamicin | 1,500c | 100 | 0.25 | 27.7 | 26.6 | c |
| Tobramycin | 600d | 100 | 0.25 | 11.1 | 12.9 | c |
| Gentamicin | 600d | 100 | 0.25 | 11.1 | 13.1 | c |
| Vancomycin | 1,500 | 50 | 1 | 9.0 | 3.3 | I (phys)* |
| Erythromycin | 1,000 | 20 | 0.33 | 13.9 | 10.3 | I (phys)* |
| 100 | 0.33 | 12.4 | 9.2 | c+ | ||
| Clarithromycin | 500 | 10 | 0.33 | 12.4 | 9.2 | I (phys)* |
| 50 | 0.33 | 12.4 | 9.2 | c+ | ||
| Fluconazole | 200 | 100 | 0.5 | 1.59 | 2.8 | c |
| Sedatives/anticonvulsants | ||||||
| Ketamine | 480 | 48 | 24 | 0.08 | 0.19 | c |
| Propofol | 300 | 300 | 24 | 0.05 | 0.17 | I (phys)** |
| Sufentanil | 0.12 | 24 | 24 | 1.98 | 2.8 | c |
| Midazolam | 600 | 120 | 24 | 0.1 | 0.17 | I (phys)* |
| Valproic acid | 1,200 | 12 | 24 | 0.2 | 0.76 | c |
| Antihypertensives/diuretics | ||||||
| Nicardipine | 120 | 120 | 24 | 0.02 | 0.02 | I (phys)* |
| Uradipil | 2,400 | 480 | 24 | 0.4 | 0.56 | c |
| Furosemide | 960 | 96 | 24 | 0.16 | 0.26 | c |
| Miscellaneous | ||||||
| N-Acetylcystein | 10,000 | 100 | 24 | 1.7 | 5.69 | I (chim) |
| Amino acid solution | 18,000e | 1,000 | 24 | 30.1 | c | |
All conditions are meant to mimic one administration to a patient with a body weight of 100 kg; ceftazidime was assumed to be infused at a rate of 4 g/24 h in a volume of 48 ml.
c, compatible (c+, very slight precipitate with complete recovery of ceftazidime upon dilution); I (phys), physically incompatible [I (phys)*, immediate precipitation; I (phys)**, trapping in emulsion]; I (chem), chemically incompatible (>10% ceftazidime degradation).
Dose, 15 mg/kg of body weight once daily.
Dose, 6 mg/kg, once daily.
VAMIN (standard amino acid solution for parenteral nutrition). Dose was 18 g of amino acid nitrogen/liter.
Stability of ceftazidime in concentrated solutions.
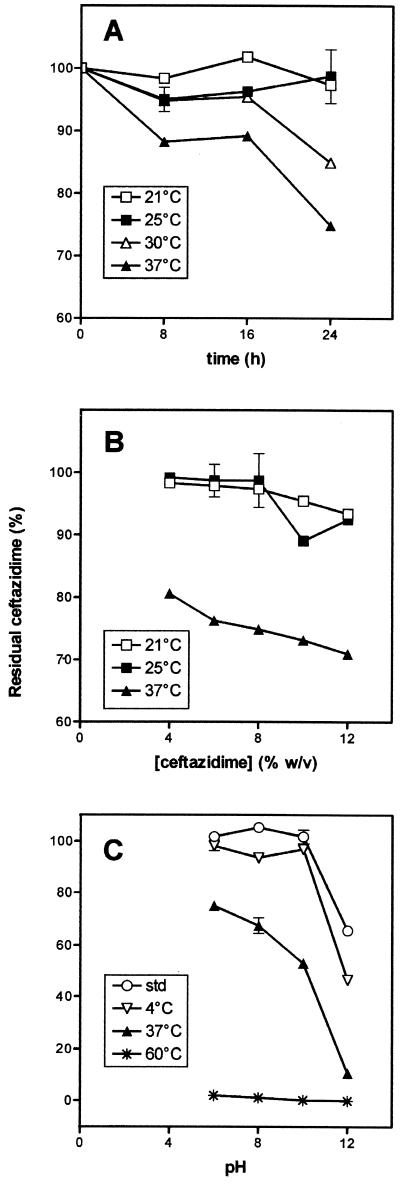
Figure 1 shows the stability of ceftazidime when incubated at increasing temperatures for up to 24 h (Fig. 1A), at concentrations up to 12% (wt/vol) (Fig. 1B), and at pH values ranging from 6 to 12 (Fig. 1C; exposure of ceftazidime to a pH of ≤4 resulted in immediate precipitation). Taking 90% stability as a limit, it clearly appears that ceftazidime must be kept at temperatures not higher than 25°C, whatever its concentration in the 4 to 12% (wt/vol) range. As reported earlier, the pH of the solutions appeared critical and could not exceed 10 even at 4°C (the pH of a freshly prepared solution lies between 7.1 and 7.7). Upon dissolution, all ceftazidime preparations displayed a pale yellow when their concentrations exceeded 8%. Only a minor increase in color intensity (to light yellow) was noted in samples kept at 25°C for 24 h. In contrast, samples brought to 37°C or higher progressively turned reddish and, thereafter, reddish-brown over time while giving rise to a definite sulfide odor. This sets up a definite limit in the application of the continuous infusion approach with ceftazidime not clearly evidenced from previous studies.
FIG. 1.
Stability of ceftazidime at various temperatures. (A) Influence of the time of incubation (12% solution); (B) influence of the drug concentration (24-h incubation); (C) influence of the pH (12% solution; 24-h incubation) (std, unincubated samples). All values are the mean of three independent determinations ± standard deviations (symbols without bars correspond to values for which the standard deviation is smaller than the symbol size). w/v, wt/vol.
Identification of ceftazidime degradation products and mechanism of ceftazidime degradation.
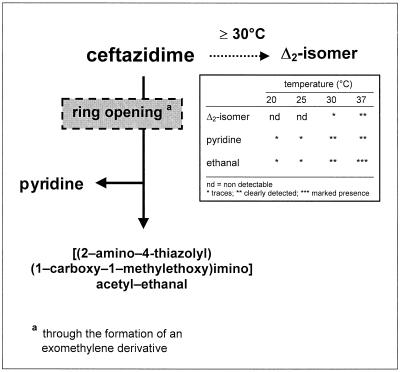
After maintaining a sample of ceftazidime (12%) at 40°C for 70 h, we could positively identify the appearance of [(2-amino-4-thiazolyl) (1-carboxy-1-methylethoxy) imino] acetyl-ethanal and of pyridine (both detected also in small amounts at 25°C) as well as of the Δ-2 isomer of ceftazidime (data not shown). This suggests a dual degradation pathway, largely dependent on the temperature and partly involving the opening of the β-lactam ring as illustrated in Fig. 2. Base catalysis by water, as well as electrophilic as well as nucleophilic attacks (on the carbonyl and on the nitrogen of the β-lactam ring, respectively), are probably responsible for this degradation, as shown with several penicillins and cephalosporins (3, 12, 19, 20, 32, 35, 36). Opening of the β-lactam ring is considered dangerous in the case of pencillins since the resulting penicilloic acids easily react with albumin to cause the formation of potent allergenic haptens (4, 27). Yet the actual concentrations of the corresponding open-ring derivative of ceftazidime (exomethylene derivative) will be vanishingly small because this compound is very unstable, and this should, in the case of ceftazidime, minimize the risk of hapten formation. No toxicological data, however, are available for the [(2-amino-4-thiazolyl) (1-carboxy-1-methylethoxy) imino] acetyl-ethanal. Finally, the amount of pyridine liberated will remain lower than the USP limit of 1.1 mg/ml for pharmaceutically acceptable ceftazidime solutions (based on published data showing that a 10% degradation of ceftazidime in a 5.8% solution over 24 h is associated with the liberation of only ∼0.5 mg of pyridine/ml [26]). The total amount which could be passed on to a patient will, therefore, be 800 to 1,000-fold lower than the published median lethal doses for either oral or subcutaneous administration of pyridine to rats (24; see also http://physchem.ox.ac.uk/MSDS/P/pyridine.html).
FIG. 2.
Degradation pathways of ceftazidime as determined by HPLC-mass spectrometry and cochromatography studies of 12% (wt/vol) samples maintained at various temperatures for up to 70 h. The opening of the β-lactam ring occurs through the formation of an exomethylene derivative (with a free carboxylate function), which is then converted into the [(2-amino-4-thiazolyl) (1-carboxy-1-methylethoxy) imino] acetyl-ethanal (13).
Compatibility studies.
Table 1 shows that all four aminoglycosides, fluconazole, ketamine, sufentanil, valproic acid, furosemide, uradipil, and the standard amino acid solutions (VAMIN) were all found physically and chemically compatible as far as ceftazidime was concerned (for aminoglycosides, we also checked for intactness of these drugs and found no evidence of significant effect after 1 h of contact at 25°C; this lack of aminoglycoside-ceftazidime interaction, in spite of reports pointing to aminoglycoside–β-lactam incompatibilities [15, 22] probably stems from our mimicking of the practical conditions of their coadministration, i.e., a rapid infusion of the aminoglycoside, consistent with its now widely accepted once daily schedule [13]). In contrast, erythromycin and clarithromycin generated a precipitate when used at high concentration (50 mg/ml). Drugs incompatible for physical reasons most notably included vancomycin (even if diluted [33]), midazolam (31), nicardipine, and propofol (the latter incompatibility was due to ceftazidime being trapped in the phospholipid emulsion [INTRALIPD] in which propofol is supplied; this incompatibility was not observed in conventional compatibility studies [31]). N-Acetylcystein caused a linear decrease of the ceftazidime content at a rate of ∼20% per h at 25°C. Additional studies using other sulfhydril donors suggested this decrease to most likely result from a thiol-dependent attack of ceftazidime.
In conclusion, the data presented here have validated the potential use of ceftazidime by continuous infusion with regard to the pharmaceutical point of view and ceftazidime's application in patients who are hospitalized in intensive care units and are receiving drugs commonly used for the overall management of severe nosocomial pneumonia. It also sets the limits of the approach in terms of temperature and coadministration of specific drugs. We suggest that any drug not listed here should be studied in detail before its coadministration with ceftazidime can be considered safe. Our studies cannot be extended without regard to other β-lactams. Although all of them basically show a similar chemical instability, meaningful differences can nevertheless be observed between individual molecules. Compatibility of individual β-lactams with other drugs may also be markedly dependent on the nature of their side chains, making general recommendations hazardous. Thus, beyond its informative aspect concerning ceftazidime, the present study should perhaps be also viewed as normative for other β-lactams as well as for other specific clinical conditions in which administration of antibiotics by continuous infusion may be rationally envisioned.
Acknowledgments
M. P. Mingeot-Leclercq provided general guidance in our studies, E. de Hoffmann and B. Rollmann (Université catholique de Louvain, Louvain-la-Neuve, and Brussels, Belgium) provided essential help in our analytical studies, and E. Dussart (SmithKline Biologicals Manufacturing S.A., Rixensart, Belgium) provided professional assessment of drug physical compatibility. F. Renoird-Andries and R. Rozenberg gave technical assistance.
This work was supported by the Belgian Fonds National de la Recherche Scientifique (grant no. 3.4516.94).
REFERENCES
- 1.Anonymous. United States Pharmacopeial Convention (ed.), United States pharmacopeia (the national formulary). Rockville, Md: United States Pharmacopeial Convention; 1995. Ceftazidime for injection; p. 310. [Google Scholar]
- 2.Bosso J A, Prince R A, Fox J L. Compatibility of ondansetron hydrochloride with fluconazole, ceftazidime, aztreonam, and cefazolin sodium under simulated Y-site conditions. Am J Hosp Pharm. 1994;51:389–391. [PubMed] [Google Scholar]
- 3.Bundgaard H. Intramolecular nucleophilic attack of an ureido group on the beta-lactam carbonyl moiety of penicillins. Acta Pharm Suec. 1973;10:309–316. [PubMed] [Google Scholar]
- 4.Bundgaard H. Allergenic reactions to drugs mediated by chemically reactive impurities or degradation products. In: Bundgaard H, et al., editors. Drug design and adverse reactions. Copenhagen, Denmark: Munksgaard; 1977. pp. 165–187. [Google Scholar]
- 5.Craig W A. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1–12. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 6.Craig W A, Andes D. Pharmacokinetics and pharmacodynamics of antibiotics in otitis media. Pediatr Infect Dis J. 1996;15:255–259. doi: 10.1097/00006454-199603000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Craig W A, Ebert S C. Continuous infusion of β-lactam antibiotics. Antimicrob Agents Chemother. 1992;36:2577–2583. doi: 10.1128/aac.36.12.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das-Gupta V, Bethea C, Dela-Torre M. Chemical stabilities of cefoperazone sodium and ceftazidime in 5% dextrose and 0.9% sodium chloride injections. J Clin Pharm Ther. 1988;13:199–205. doi: 10.1111/j.1365-2710.1988.tb00181.x. [DOI] [PubMed] [Google Scholar]
- 9.Donowitz G R, Mandell G L. Acute pneumonia. In: Mandell G L, Bennett J E, Dolin R, editors. Principles and practice of infectious diseases. 5th ed. Edinburgh, Scotland: Churchill Livingstone; 2000. pp. 717–743. [Google Scholar]
- 10.Faouzi M A, Dine T, Luyckx M, Gressier B, Brunet C, Goudaliez F, Mallevais M L, Cazin M, Cazin J C. Stability and compatibility studies of cefaloridine, cefuroxime and ceftazidime with PVC infusion bags. Pharmazie. 1994;49:425–427. [PubMed] [Google Scholar]
- 11.Farina A, Porra R, Cotichini V, Doldo A. Stability of reconstituted solutions of ceftazidime for injections: an HPLC and CE approach. J Pharm Biomed Anal. 1999;20:521–530. doi: 10.1016/s0731-7085(99)00057-6. [DOI] [PubMed] [Google Scholar]
- 12.Fubara J O, Notari R E. A kinetic oxymoron: concentration-dependent first-order rate constants for hydrolysis of ceftazidime. J Pharm Sci. 1997;87:53–58. doi: 10.1021/js970179k. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert D N. Aminoglycosides. In: Mandell G L, Bennett J E, Dolin R, editors. Principles and practice of infectious diseases. 5th ed. Edinburgh, Scotland: Churchill Livingstone; 2000. pp. 307–335. [Google Scholar]
- 14.Inagaki K, Tagaki J, Lor E, Lee K-J, Nii L, Gill M A. Stability of fluconazole in commonly used intravenous antibiotic solution. Am J Hosp Pharm. 1993;50:1206–1208. [PubMed] [Google Scholar]
- 15.Konishi H, Goto M, Nakamoto Y, Yamamoto I, Yamashina H. Tobramycin inactivation by carbenicillin, ticarcillin, and piperacillin. Antimicrob Agents Chemother. 1983;23:653–657. doi: 10.1128/aac.23.5.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lor E, Sheybani T, Tagaki J. Visual compatibility of fluconazole with commonly used injectable drugs during simulated Y-site administration. Am J Hosp Pharm. 1991;48:744–746. [PubMed] [Google Scholar]
- 17.MacGowan A P, Bowker K E. Continuous infusion of beta-lactam antibiotics. Clin Pharmacokinet. 1998;35:391–402. doi: 10.2165/00003088-199835050-00004. [DOI] [PubMed] [Google Scholar]
- 18.Nahata M C, Morosco R S, Fox J L. Stability of ceftazidime (with arginine) stored in plastic syringes at three temperatures. Am J Hosp Pharm. 1992;49:2954–2956. [PubMed] [Google Scholar]
- 19.Neftel K A. Effect of storage of penicillin-G solutions on sensitization to penicillin-G after intravenous administration. Lancet. 1982;i:986–988. doi: 10.1016/s0140-6736(82)91991-2. [DOI] [PubMed] [Google Scholar]
- 20.Neftel K A, Walti M, Schulthess H K. Adverse reactions following intravenous penicillin-G relate to degradation of the drugs in vitro. Klin Wochenschr. 1984;62:25–29. doi: 10.1007/BF01725189. [DOI] [PubMed] [Google Scholar]
- 21.Nicolau D P, McNabb J C, Lacy M K, Jing Li, Quintiliani R, Nightingale C H. Pharmacokinetics and pharmacodynamics of continuous and intermittent ceftazidime during the treatment of nosocomial pneumonia. Clin Drug Investig. 1999;18:133–139. [Google Scholar]
- 22.Pickering L K, Gearhart P. Effect of time and concentration upon interaction between gentamicin, tobramycin, netilmicin, or amikacin and carbenicillin or ticarcillin. Antmicrob Agents Chemother. 1979;15:592–596. doi: 10.1128/aac.15.4.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pleasants R A, Vaughan L M, Williams D M, Fox J L. Compatibility of ceftazidime and aminophylline admixtures for different methods of intravenous infusion. Ann Pharmacother. 1992;26:1221–1226. doi: 10.1177/106002809202601004. [DOI] [PubMed] [Google Scholar]
- 24.Pollock L J, Finkelman I, Arieff A J. Toxicity of pyridine in man. Arch Intern Med. 1943;71:95–106. [Google Scholar]
- 25.Schentag J J. Antimicrobial action and pharmacokinetics/pharmacodynamics: the use of AUIC to improve efficacy and avoid resistance. J Chemother. 1999;11:426–439. doi: 10.1179/joc.1999.11.6.426. [DOI] [PubMed] [Google Scholar]
- 26.Stendal T L, Klem W, Tonnesen H H, Kjonniksen I. Drug stability and pyridine generation in ceftazidime injection stored in an elastomeric infusion device. Am J Health Syst Pharm. 1998;55:683–685. doi: 10.1093/ajhp/55.7.683. [DOI] [PubMed] [Google Scholar]
- 27.Stewart G T. Allergy to penicillin and related antibiotics: antigenic and immunochemical mechanism. Annu Rev Pharmacol. 1973;13:309–324. doi: 10.1146/annurev.pa.13.040173.001521. [DOI] [PubMed] [Google Scholar]
- 28.Stewart J T, Warren F W, Johnson S M, Fox J L, Mullaney J. Stability of ceftazidime in plastic syringes and glass vials under various storage conditions. Am J Hosp Pharm. 1992;49:2765–2768. [PubMed] [Google Scholar]
- 29.Stiles M L, Allen L V, Jr, Fox J L. Stability of ceftazidime (with arginine) and of cefuroxime sodium in infusion-pump reservoirs. Am J Hosp Pharm. 1992;49:2761–2764. [PubMed] [Google Scholar]
- 30.Stiles M L, Tu Y-H, Allen L V. Stability of cefazolin sodium, cefoxitin sodium, ceftazidime, and penicillin G sodium in portable pump reservoirs. Am J Hosp Pharm. 1989;46:1408–1412. [PubMed] [Google Scholar]
- 31.Trissel L A. Handbook in injectable drugs. Bethesda, Md: American Society of Health-System Pharmacists; 1998. pp. 236–244. [Google Scholar]
- 32.Van Krimpen P C, Van Bennekom W P, Bult A. Penicillins and cephalosporins. Physicochemical properties and analysis in pharmaceutical and biological matrices. Pharm Weekbl S. 1987;9:1–23. doi: 10.1007/BF01956487. [DOI] [PubMed] [Google Scholar]
- 33.Vaughan L M, Poon C Y. Stability of ceftazidime and vancomycin alone and in combination in heparinized and nonheparinized peritoneal dialysis solution. Ann Pharmacother. 1994;28:572–576. doi: 10.1177/106002809402800503. [DOI] [PubMed] [Google Scholar]
- 34.Wade C S, Lampasona V, Mullins R E, Parks R B. Stability of ceftazidime and amino acids in parenteral nutrient solutions. Am J Hosp Pharm. 1991;48:1515–1519. [PubMed] [Google Scholar]
- 35.Yamana T, Tsuji A. Comparative stability of cephalosporins in aqueous solution: kinetics and mechanisms of degradation. J Pharm Sci. 1976;65:1563–1574. doi: 10.1002/jps.2600651104. [DOI] [PubMed] [Google Scholar]
- 36.Yamana T, Tsuji A, Kiya E, Miyamoto E. Physicochemical properties of beta-lactam antibacterials: deuterium solvent isotope effect on penicillin G degradation rate. J Pharm Sci. 1977;66:861–866. doi: 10.1002/jps.2600660632. [DOI] [PubMed] [Google Scholar]
- 37.Zhou M, Notari R E. Influence of pH, temperature and buffers on the kinetics of ceftazidime degradation in aquous solutions. J Pharm Sci. 1995;84:534–538. doi: 10.1002/jps.2600840504. [DOI] [PubMed] [Google Scholar]