Abstract
We report two South African serotype 6B pneumococcal isolates with cephalosporin resistance, yet with susceptibility to penicillin. DNA fingerprinting revealed that they were clonal in origin. pbp 2X and 1A genes showed major alterations typical of cephalosporin-resistant pneumococci. The pbp 2B gene was completely unaltered, explaining the penicillin susceptibility of the isolates.
β-Lactam antibiotics inhibit the growth of pneumococci by inactivating penicillin-binding proteins (PBPs), which leads to a loss of cell wall synthesis, cell death, and cell lysis (16). Resistance to β-lactams is due to a complex production of altered PBPs with resultant, decreased antibiotic affinities (6, 17). Streptococcal “resistance” genes coding for altered PBPs are acquired from the environment by natural processes of transformation and are then recombined into the genome of the pneumococcus (2, 11). Penicillin resistance can be established by alteration in PBPs 2X, 2B, and 1A (1), while only altered PBPs 2X and 1A are required for cefotaxime/ceftriaxone resistance (9). Filipe and Tomasz (3) showed that a functional MurMN operon is critical for the expression of penicillin resistance in the pneumococcus. The MurMN operon codes for the MurM and MurN proteins, which control the biosynthesis of branched-stem structured cell wall muropeptides. It has recently been shown that in conjunction with altered PBPs, alteration in MurM assists in the development of β-lactam resistance (13). Our present paper reports two South African serotype 6B pneumococcal isolates with cephalosporin resistance, yet with susceptibility to penicillin.
Properties of the pneumococcal isolates studied are shown in Table 1. Antibiotic MICs were determined using the agar dilution method as specified by the National Committee for Clinical Laboratory Standards (10). The chromosomal DNAs of bacteria were fingerprinted using the previously described methods of pulsed-field gel electrophoresis (7) and BOX-PCR fingerprinting (5). Chromosomal DNAs were extracted from bacterial cells, and pbp 2X, pbp 2B, and pbp 1A genes were amplified from the chromosomal DNAs by PCR using methods that have been described previously (14). For pbp gene PCR, primers have been described previously (12). PCR gene products were fingerprinted using previously described methods of restriction endonuclease analysis (14) and were sequenced using the Big Dye Terminator Cycle Sequencing kit (Applied Biosystems, Foster City, Calif.) and the Applied Biosystems Model 310 automated DNA sequencer. Altered pbp 2B genes from isolates 8303 and 3191 were independently cloned into plasmid pGEM-3Zf and were used as a source of transforming DNA. Isolate 45904 was made competent and was used as recipient in transformation experiments using the following methods. Bacteria were cultured in C medium (15) until the mid-exponential phase (optical density at 620 nm, 0.15) and after the addition of glycerol to 10% were frozen at −70°C in 500-μl aliquots. For transformation, 1 μg of DNA was added to 500 μl of competent cells, which was then incubated at 30°C for 45 min and at 37°C for 90 min. Eighty-microliter amounts were then plated onto Mueller-Hinton blood agar containing penicillin at concentrations ranging from 0.03 to 4 μg/ml, and the plate contents were incubated at 37°C for 48 h. Transformants grew on agar with penicillin concentrations up to 1 μg/ml. Transformants were picked from 1-μg/ml plates and were further analyzed.
TABLE 1.
Properties of pneumococcal isolates
| Isolate | Serotype | Origin (yr) | MIC (μg/ml) of:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Penicillin | Ampicillin | Amoxicillin | Cefotaxime | Ceftriaxone | Cefuroxime | Chloramphenicol | Clindamycin | Tetracycline | Erythromycin | Rifampin | |||
| 45904 | 6B | South Africa (2000) | 0.06 | 0.015 | 0.03 | 4 | 4 | 8 | 2 | 0.06 | 4 | 2 | 0.03 |
| 53349 | 6B | South Africa (2000) | 0.06 | 0.015 | 0.03 | 4 | 4 | 8 | 2 | 0.06 | 4 | 2 | 0.03 |
| 8303 | 23F | South Africa (1995) | 4 | 1 | 2 | 1 | 1 | 2 | 2 | 0.06 | 4 | 0.25 | 0.03 |
| 3191 | 19A | Hungary (1997) | 16 | 4 | 8 | 4 | 4 | 8 | 8 | 1 | 4 | 2 | 0.03 |
Two unique serotype 6B pneumococci were recently isolated in South Africa, which revealed cephalosporin resistance (cefotaxime and ceftriaxone MICs, 4 μg/ml; cefuroxime MIC, 8 μg/ml) yet were susceptible to penicillin (MIC, 0.06 μg/ml). Oxacillin disk (1 μg) screening showed 16-mm zones of inhibition for both isolates. Isolate 45904 was cultured from an ear swab on 30 June 2000 from a 10-month-old child who presented with an ear infection and perforated eardrum. The infection was treated with cefaclor. One month prior to this infection, the child had also suffered from an ear infection which was treated with cefuroxime. Isolate 53349 was cultured from an ear swab on 21 August 2000 from an unrelated 1-year-old child. This child had suffered with recurrent middle ear infections and was treated sporadically with cefpodoxime or amoxicillin/clavulanate over a period of several months before the specimen was taken. During the month of March 2000, the child also developed pneumonia, which was treated with ceftriaxone. Pulsed-field gel electrophoresis and BOX-PCR fingerprinting revealed identical chromosomal DNA fingerprint patterns for isolates 45904 and 53349, indicating that they were clonal in origin. This was supported by identical fingerprint patterns for their pbp 2X, 2B, and 1A genes, indicating identical β-lactam resistance genotypes for both isolates. Our investigations revealed no epidemiological link between the isolates; however, this link cannot be totally excluded. The pbp 2X, 2B, and 1A genes were sequenced from isolate 45904 and were compared to the sequences of the genes from susceptible laboratory strain R6. The penicillin-binding-domain-encoding region of PBP 2X revealed 18% nucleotide sequence divergence, resulting in 39 amino acid mutations in the protein (Fig. 1). The corresponding area of PBP 1A revealed 21% nucleotide sequence divergence, resulting in 41 amino acid mutations in the protein (Fig. 2). However, the pbp 2B gene was completely unaltered, which would explain the penicillin-susceptible phenotype of the isolate, since penicillin resistance is dependent on alterations in PBP 2B. Conservation of penicillin susceptibility via an unaltered PBP 2B was confirmed by transformation studies with altered pbp 2B DNA from penicillin-resistant (MICs, ≥4 μg/ml) isolates 8303 and 3191, which was shown to successfully transform the penicillin MIC for isolate 45904 from 0.06 μg/ml to 2 μg/ml.
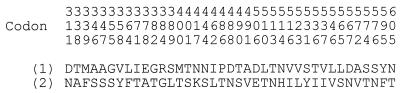
FIG. 1.
Amino acid substitutions in the penicillin-binding domain of PBP 2X from isolate 45904 (line 2) compared to susceptible strain R6 (line 1). Unaltered amino acid codons are not shown. Codons are numbered according to the published sequence of Laible and coworkers (6).
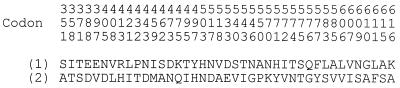
FIG. 2.
Amino acid substitutions in the penicillin-binding domain of PBP 1A from isolate 45904 (line 2) compared to susceptible strain R6 (line 1). Unaltered amino acid codons are not shown. Codons are numbered according to the published sequence of Martin and coworkers (8).
Pneumococci have a total of six PBPs, yet alterations in only two PBPs (PBPs 2X and 1A) are required for cephalosporin resistance (9). Furthermore, the close linkage of pbp 2X and 1A genes on the pneumococcal chromosome is conducive to the transfer of both genes in a single genetic event (4). In the laboratory, one-step transformations have been shown to transform cephalosporin-susceptible strains to MICs of up to 32 μg/ml (9). To the best of our knowledge, isolates 45904 and 53349 are the first pneumococci of this phenotype to be reported that have been isolated in their natural environment and which fulfill laboratory predictions of high cephalosporin resistance emergence coupled with only altered PBPs 2X and 1A. The selective pressure created by cephalosporin therapy has most likely selected the altered pbp genotype in the isolate.
Our study has demonstrated that the pneumococcus can follow various genetic pathways in its pursuit of resistance to β-lactam antibiotics. Alteration in only PBPs 2X and 1A has resulted in the emergence of cephalosporin-resistant pneumococci in their natural setting.
Nucleotide sequence accession numbers.
Sequence data from isolate 45904 appear in the EMBL, GenBank, and DDBJ nucleotide sequence data libraries under the following accession numbers: AF387162 (pbp 2X gene) and AF387163 (pbp 1A gene).
REFERENCES
- 1.Barcus V A, Ghanckar K, Yeo M, Coffey T J, Dowson C G. Genetics of high level penicillin resistance in clinical isolates of Streptococcus pneumoniae. FEMS Microbiol Lett. 1995;126:299–303. doi: 10.1111/j.1574-6968.1995.tb07433.x. [DOI] [PubMed] [Google Scholar]
- 2.Dowson C G, Hutchison A, Brannigan J A, George R C, Hansman D, Linares J, Tomasz A, Manard-Smith J, Spratt B G. Horizontal transfer of penicillin-binding protein genes in penicillin-resistant clinical isolates of Streptococcus pneumoniae. Proc Natl Acad Sci USA. 1989;86:8842–8846. doi: 10.1073/pnas.86.22.8842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Filipe S R, Tomasz A. Inhibition of the expression of penicillin resistance in Streptococcus pneumoniae by inactivation of cell wall muropeptide branching genes. Proc Natl Acad Sci USA. 2000;97:4891–4896. doi: 10.1073/pnas.080067697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gasc A-M, Kauc L, Barraillé P, Sicard M, Goodgal S. Gene localization, size, and physical map of the chromosome of Streptococcus pneumoniae. J Bacteriol. 1991;173:7361–7367. doi: 10.1128/jb.173.22.7361-7367.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koeuth T, Versalovic J, Lupski J R. Differential subsequence conservation of interspersed repetitive Streptococcus pneumoniae BOX elements in diverse bacteria. Genome Res. 1995;5:408–418. doi: 10.1101/gr.5.4.408. [DOI] [PubMed] [Google Scholar]
- 6.Laible G, Spratt B G, Hakenbeck R. Interspecies recombinational events during the evolution of altered PBP 2X genes in penicillin-resistant clinical isolates of Streptococcus pneumoniae. Mol Microbiol. 1991;5:1993–2002. doi: 10.1111/j.1365-2958.1991.tb00821.x. [DOI] [PubMed] [Google Scholar]
- 7.Lefevre J C, Faucon G, Sicard A M, Gasc A M. DNA fingerprinting of Streptococcus pneumoniae strains by pulsed-field gel electrophoresis. J Clin Microbiol. 1993;31:2724–2728. doi: 10.1128/jcm.31.10.2724-2728.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin C, Briese T, Hakenbeck R. Nucleotide sequences of genes encoding penicillin binding proteins from Streptococcus pneumoniae and Streptococcus oralis with high homology to Escherichia coli penicillin binding proteins 1A and 1B. J Bacteriol. 1992;174:4517–4523. doi: 10.1128/jb.174.13.4517-4523.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muñoz R, Dowson C G, Daniels M, Coffey T J, Martin C, Hakenbeck R, Spratt B G. Genetics of resistance to third-generation cephalosporins in clinical isolates of Streptococcus pneumoniae. Mol Microbiol. 1992;6:2461–2465. doi: 10.1111/j.1365-2958.1992.tb01422.x. [DOI] [PubMed] [Google Scholar]
- 10.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7–A5. 5th ed. Wayne, Pa: NCCLS; 2000. [Google Scholar]
- 11.Sibold C, Henrichsen J, Konig A, Martin C, Chalkley L, Hakenbeck R. Mosaic pbpX genes of major clones of penicillin-resistant Streptococcus pneumoniae have evolved from pbpX genes of a penicillin-sensitive Streptococcus oralis. Mol Microbiol. 1994;12:1013–1023. doi: 10.1111/j.1365-2958.1994.tb01089.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith A M, Klugman K P. Alterations in PBP 1A essential for high-level penicillin resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 1998;42:1329–1333. doi: 10.1128/aac.42.6.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith A M, Klugman K P. Alterations in MurM, a cell wall muropeptide branching enzyme, increase high-level penicillin and cephalosporin resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2001;45:2393–2396. doi: 10.1128/AAC.45.8.2393-2396.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith A M, Klugman K P, Coffey T J, Spratt B G. Genetic diversity of penicillin-binding protein 2B and 2X genes from Streptococcus pneumoniae in South Africa. Antimicrob Agents Chemother. 1993;37:1938–1944. doi: 10.1128/aac.37.9.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomasz A, Hotchkiss R D. Regulation of the transformability of pneumococcal cultures by macromolecular cell products. Proc Natl Acad Sci USA. 1964;51:480–487. doi: 10.1073/pnas.51.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waxman D J, Strominger J L. Penicillin-binding proteins and the mechanism of action of β-lactam antibiotics. Annu Rev Biochem. 1983;52:825–869. doi: 10.1146/annurev.bi.52.070183.004141. [DOI] [PubMed] [Google Scholar]
- 17.Zighelboim S, Tomasz A. Penicillin-binding proteins of multiply antibiotic-resistant South African strains of Streptococcus pneumoniae. Antimicrob Agents Chemother. 1980;17:434–442. doi: 10.1128/aac.17.3.434. [DOI] [PMC free article] [PubMed] [Google Scholar]