ABSTRACT
Introduction
The history of the use of telemedicine in maritime medicine dates back to the 1930s. In the early 2000s, the German Navy built up a telemedicine network which today is installed in all ships and provides a connection to the medical infrastructure ashore. The objective of this study was to optimize the implementation of telemedicine based on the experience gained in the German Navy. For this purpose, qualitative and quantitative methods were used to identify determinants which affect the use of telemedicine in order to determine whether there is any need for optimization.
Methods
The study was conducted using a mixed methods design. First, guideline-based interviews were conducted with Navy medical officers who had been recruited via various email distribution lists. The interviews were then transcribed and coded. In an analysis, deductive and inductive categories were derived from the codes. Hypotheses were deduced from the interviews, too, and used to develop a questionnaire.
Besides the medical officers, other Navy medical personnel with experience in the field of telemedicine took part in the survey. The study was concluded by a descriptive analysis of the quantitative data.
Results
The analysis of the interviews revealed that a regular use of telemedicine workstations increased the users’ confidence and, in their opinion, improved medical treatment. Technical and organizational problems posed obstacles, which increased the use of partly insecure alternatives. A proper technical support was regarded as a precondition for effectively using telemedicine.
The results of the quantitative analysis showed that consultation was mainly sought for dermatological (46%), surgical (24%), and internal (22%) conditions.
Conclusion
The study revealed determinants for the use of telemedicine in the German Navy. Factors improving the motivation of the users should be strengthened in order to optimize the use of telemedicine. Furthermore, it can be assumed that a successful implementation will be supported by reducing or eliminating obstacles. The findings on the main reasons for seeking medical advice could be taken into account in the further planning of specific training.
INTRODUCTION
Telemedicine (in this document, telemedicine is defined as “a collective term for various medical care concepts having in common that health care services for the population in the areas of diagnostics, therapy and rehabilitation, as well as advisory services for physicians are provided over distances (both in terms of space and time). Information and communication technologies are employed for this purpose.”)1 has a long tradition in civilseafaring.2 The Centro Internazionale Radio Medico, founded in Rome in 1935, and the Cuxhaven medical center, founded in 1931, were among the first European institutions to offer this kind of service. In 1998, the Cuxhaven medical center became the Federal Republic of Germany official advice center named MEDICO Cuxhaven.3,4
To ensure the provision of telemedicine services around the world, today, sea areas are subdivided into Maritime Rescue Coordination Center (MRCC) regions. MRCC is associated with different nations and provides Telemedical Maritime Assistance Services (TMAS) in these regions. All participating nations are required by International Labour Organization/International Maritime Organization Convention No. 164 to provide medical support to seafarers. Further regulations are laid down in the International Labour Organization’s 2006 Maritime Labour Convention.4
Going to sea often entails an autonomous life for weeks and months. Particular challenges are posed by the distance to land (in terms of both space and time), the training level of shipboard personnel, limited material resources, and a low standard of medical care in some ports of destination. Reasons for medical treatment onboard span trivial medical conditions to serious illnesses requiring intensive care.5,6 Epidemiological studies have shown that clinical pictures associated with internal and general medical conditions are the most common of those reported on passenger vessels.7–9
Medical services of navies face challenges similar to those faced by civilian shipping. However, differences exist in terms of the material and personnel resources and the sometimes complex reasons for consultation. The spectrum not only includes common illnesses and injuries, but also serious injuries suffered during combat operations. Many ships of the world’s major forces therefore have well-equipped ship’s hospitals, some featuring operating rooms. On longer voyages, a well-trained medical team, often including at least one medical officer, is always on board. Naval operations are often conducted by several units that form a task group, which allows for cooperation between participating units and nations. Nevertheless, military shipping can also face situations that cannot be dealt with using the means provided on board and that, therefore, require telemedical advice.10–12
For this reason, Armed Forces have been developing a telemedicine infrastructure at an early stage. The U.S. Armed Forces have dealt with telemedicine applications since 1992. Since then, a broad range of telemedicine infrastructure has been set up across services, as illustrated by the number of telemedicine consultations, which amounts to 60,000 per year.13 The UK began operating telemedicine programs in 1998.14 In 1993, the German Armed Forces (Bundeswehr) Hospital Ulm launched initial telemedicine pilot projects of the Bundeswehr.15
The German Navy began implementing telemedicine by establishing a workstation aboard a frigate in 2001.3 Over time, it has become clear that telemedicine can help prevent repatriations and, therefore, save money.15
The emergency department of the Bundeswehr Hospital Hamburg has been the central point of contact for clinical questions since mid-2016. The Naval Institute of Maritime Medicine answers questions concerning maritime medicine and diving medicine. The Hamburg emergency department is also connected with the Department of Tropical Medicine, the Center for Mental Health, and the Department of Gynecology of the Bundeswehr Hospital Westerstede.16
The Bundeswehr has a Joint Medical Service and its own Navy medical service which is responsible for the medical care of the sea-going units. Shipboard physicians are part of this medical service and can work on most of the 57 Navy ships in well-equipped sick bays.17 The 10 frigates and three combat support ships always have an embarked medical officers’ team, which, for operations, may be complemented by a fleet surgical team composed of surgeons and anesthetists. All of these ships are equipped with a telemedicine workstation including a video conference system, a radiological device (C-arm), and specialist equipment, such as reflex cameras with additional equipment including an orthoscope and a dermatoscope. These tools can be used for a wide variety of specialized and general matters. In addition, each of the three combat support ships can be equipped with a mobile naval surgical hospital featuring two operating rooms and a separate ward. All other ships house trained medical assistant personnel.10,17,18
At present, 37 medical officers work as shipboard physicians in the Navy, typically serving for 3 years in this assignment. In addition, 71 soldiers in the Navy serve as medical assistants (Table I).
TABLE I.
Socio-demographic Data
| Interviews | Questionnaire | Personnel currently employeda | ||||
|---|---|---|---|---|---|---|
| Gender | Male: 14 (70%) | Female: 6 (30%) | Male: 52 (65%) | Female: 28 (35%) | Male: 63 (58%) | Female: 46 (42%) |
| Age (years) | 41.0 | 35.9 | 36.0 | |||
| Period of service (years) | 14.5 | 15.4 | 13.6 | |||
| Discipline | Surgery | 24% (n = 5) | ||||
| Internal medicine | 24% (n = 5) | |||||
| Anesthesia | 19% (n = 4) | |||||
| General Medicine | 19% (n = 4) | |||||
| Public Health | 10% (n = 2) | |||||
| Dentistry | 5% (n = 1) | |||||
Verbal answer from the Naval Command of the German Armed Forces Rostock.
To optimize the quality of telemedicine services aboard ships, it is necessary to examine the preconditions, requirements, and expectations regarding telemedicine and conduct an accompanying (process) evaluation. These aspects are addressed by implementation science, which focuses on bridging the gap between available evidence and routine practice.19–21
At present, there is a lack of data available to determine which factors promote and limit the further implementation of telemedicine in the Navy.20
The aim of the present study, therefore, was to explore the determinants affecting the implementation of telemedicine in the Navy using qualitative and quantitative data to determine where existing and future telemedicine projects can be optimized to facilitate an effective implementation.
MATERIALS AND METHODS
This study was conducted using a mixed methods design combining successive steps of qualitative and quantitative data collection. This approach is also referred to as “sequential qualitative–quantitative design”. The combination of qualitative and quantitative methods is used to conduct research in largely unexplored fields of study. The focus is on answering the research question as precisely as possible using the selected methods.22
Based on individual interviews, hypotheses were developed for the present study to be either supported by a questionnaire or supplemented by further hypotheses. This approach was used to achieve methodological triangulation.23
Individual Interviews
Semi-structured interviews24 were used to gather the experience of medical officers in telemedicine applications in the Navy.
Based on a literature search2–6,10 focusing on maritime and military telemedicine and discussion with the working group, the following key questions were formulated:
What experiences of telemedicine applications aboard ships have you been able to collect?
Which uncertainties with respect to the application of the equipment have you experienced?
When providing medical care, what other media/material do you use as an alternative to the officially provided equipment?
What further or alternative equipment would you like to have for providing medical care aboard ships?
What are your wishes for the future in this field?
Interview participants were recruited using various email distribution lists which included crews of ships of the German Navy, event distributors of the Bundeswehr, and facilities of the Joint Medical Service. A total of 187 individuals (67 females and 120 males) were contacted. Inclusion criteria for participation in the interviews were experience of telemedicine in the German Navy and being an active German medical officer. In most cases, the duration of service as a shipboard physician does not exceed 3 years. Therefore, we decided to target medical officers who were, at the time, working in other deployments. The criteria were stated in the cover letter and verified at the beginning of the interviews. The participants were asked to send a written informed consent to the study director in advance.
Questionnaire
The non-validated questionnaire was prepared based on the results of the interviews. It was piloted using a think-aloud process that involved two individuals who were familiar with the subject but who were not suitable as interview partners.25 This led to minor changes in language and content. The questionnaire is included in the Supplemented Material.
The questionnaire was subsequently sent to all Bundeswehr medical facilities via several email distribution lists. The inclusion criteria for participation in the survey were experience of telemedicine in the German Navy and being an active German medical officer or medical assistant, which were referred to in the cover letter and verified at the beginning of the questionnaire. The total population can only be approximated using the current personnel of shipboard physicians (37) and a general service time as a shipboard physician of 3 years. This would assume approximately 10 cycles since the early 1990s, which would enable 370 soldiers to gain experiences. We recruited again individuals with prior experience who were, at the time, working in other deployments. The participants could choose to anonymously complete the questionnaire online via SurveyMonkey platform or on paper.26
Analysis
The individual interviews were conducted by the author and digitally recorded. After the interviews had been pseudonymized and transcribed, a content analysis according to Mayring was performed, which resulted in a system of deductive and inductive categories.27 Besides the author, an independent researcher from the Institute of Family Medicine analyzed the interviews. The results were discussed and summarized in a consensus version.28 Here, a third researcher experienced in qualitative methods (JS) supervised the process.
Statistical software SPSS 25.0 (IBM Inc.) was used to perform a descriptive analysis of the questionnaire. Mean values and SDs were used for the metric data, and frequency distributions and percentages were used for the categorical data.29 Table II provides an excerpt of our results.
TABLE II.
Categories in the Qualitative Part
| Major category | Minor category | Sub-category | Quotation | Definition of the categories |
|---|---|---|---|---|
| Assessment | Positive/negative aspects | Telemedicine is important and absolutely has a role (P15) | Overall valuation and satisfaction with telemedicine in the Navy | |
| Motivation | Use of telemedicine applications | Because I always need an official answer outlining the consequences (P12) | Motivation to use the Navy’s official telemedicine facility | |
| Use of alternatives | You receive an answer relatively quickly, even on your smartphone (P18) | Motivation to use an alternative, rather than the official telemedicine system | ||
| Medical reasons for consultation | Consultations held for medical reasons | Positive/negative aspects | In many cases, a simple telemedical consultation can provide a degree of certainty of action, particularly in the case of skin symptoms (P15) | Perceptions regarding the specific medical use of the telemedicine facility |
| Organizational reasons for consultation | Consultations held for organizational reasons | Positive/negative aspects | Of course, the equipment instruction is not the primary reason I have such a telemedicine system, but it can sometimes be used for such a purpose (P4) | Perceptions regarding other organizational uses of the telemedicine facility |
| Technical and organizational determinants | Hardware and technology level | Positive/negative aspects | Two previous times at sea with a tender, it did not work because the device was already broken from the start (P11) | Determinants influencing the use of telemedicine at the hardware and technology level |
| User level | Positive/negative aspects | The usage problems we observed actually are reservations, simply the fear of breaking something (P15) | Determinants influencing the use of telemedicine at the user level | |
| Organizational level | Positive/negative aspects | But it is mostly because of the range (P14) | Determinants influencing the use of telemedicine at the organizational level | |
| Alternatives to telemedicine workstations | Use of alternative officially provided media | Positive/negative aspects | It was just not possible to specifically process a larger amount of data in parallel (P10) | Perceptions regarding officially provided media used as an alternative to the official telemedicine system |
| Use of alternative privately owned media | Positive/negative aspects | In this respect, the smartphone is a really good thing; you can take a photo and send it without delay (P16) | Perceptions regarding alternative privately owned media used as an alternative to the official telemedicine system | |
| Use of alternative medical infrastructure | Positive/negative aspects | As a last resort, because I did not have the findings and the patient could not move his shoulder, I repatriated him (P19) | Perceptions regarding medical infrastructure used as an alternative to the official telemedicine system | |
| Support | Assessment | Positive/negative aspects | “What is still missing, and needs to be established, is a certain support standard.” (P18) | Perceptions regarding the support offered by the Bundeswehr |
RESULTS
Qualitative Results
Twenty-one individuals volunteered to be interviewed. A potential participant was excluded because of lack of experience in military telemedicine and was not interviewed. The return rate was 11.2% (187 contacted people). On average, the interviews took 25.5 minutes (SD = 15.7 min, min.: 6.9 min, max.: 68 min). In total, 70% of the interview partners were male (n = 14) and 30% were female (n = 6). Table I provides further socio-demographic information on the participants (interview and questionnaire).
Table II provides an overview of the categories used in the qualitative section, which is discussed in more detail in the following paragraphs.
Assessment and Motivation
The interviewees generally welcomed the development of telemedicine and highlighted its importance.
However, some participants regarded technological development as backward and the role of telemedicine as of minor importance. In terms of the motivation for using telemedicine facilities, establishing contact with official agencies was considered important for relief. The interviewees also stated that the consultations helped optimize treatments and strengthen the confidence of the medical team, the ship’s command, and the patient.
Medical and Organizational Reasons for Consultation
Consultations were sought for two main reasons: medical and organizational. The medical reasons comprised special, clinically relevant requests to advisory centers. Aspects such as technical issues or equipment handling instructions were classified as organizational reasons for consultation.
Besides strengthened confidence and optimized treatment, the interviewees also mentioned the prevention of repatriations as a positive aspect of medical consultation. However, they reported that telemedicine was only usable to a limited extent. For example, its use in emergency situations was considered impractical in present circumstances. Nevertheless, the interviewees imagined telemedicine being used in these situations under better conditions, as well as in other fields such as psychiatry or diving medicine.
In terms of organizational reasons for consultation, monthly communication checks and equipment handling instructions were assessed as positive by the interviewees. However, the participants stated that internal coordination on board and the effort required to use telemedicine were often an obstacle. These interviewees called for available information on the subject of telemedicine to be expanded.
Technical and Organizational Determinants
The technical and organizational determinants comprised both positive and negative aspects that affected the use of telemedicine applications. This main category was divided into sub-categories for user, hardware, and organizational aspects.
Users who regularly used the applications grew more confident and, therefore, had more positive experiences. However, this also means that not using the applications causes uncertainties. A lack of technical understanding and new problems also increased users’ inhibitions. Desires for the future included trouble-fee operation of the applications as well as persevering and flexible users.
The hardware and technical systems available were assessed differently by the participants and were mainly considered negative. The existing equipment was considered sufficient and the system itself assessed as functional under normal conditions. However, the respondents complained about differences in the equipment, a lack of user friendliness, and the fact that the systems were obsolete. Moreover, non-operational systems were considered an inhibiting factor for users. The interviewees expressed the desire for state-of-the-art technical systems including mobile equipment and greater ease of use.
Alternatives to Telemedicine Workstations
The respondents also used alternative methods to establish contact with experts or seek advice. A distinction was made between using alternative officially provided media, alternative privately owned media, and alternative medical infrastructure like foreign ports.
Officially provided media included satellite phones, radio equipment, and the Bundeswehr email platform. The interviewees highlighted that these media were easier and faster to use compared with telemedicine workstations. Establishing contact with colleagues was also considered important. Negative aspects included restricted data transmission and lack of data protection. In terms of privately owned media, the respondents mainly used messenger services, and they also discussed using their own cell phones in general. These media were reported to be easy and fast to use and where, therefore, considered advantageous. However, the respondents also regarded their use as legally problematic.
The third category of alternatives to telemedicine workstations was other medical infrastructure. The main factors in this category were foreign assistance in foreign ports of call or on other ships and, as a last resort, repatriation to the home port. Here, the greater flexibility and ease of use were regarded as positive aspects. However, problems were encountered especially with respect to foreign assistance because of a lack of both standard medical procedures and, in many cases, written statements.
Support
Experiences with support included the identification of contact persons for matters concerning telemedical consultations as well as the assessment of solutions provided for technical and organizational problems.
Interviewees assessed civilian support and support provided by crews and official Bundeswehr support agencies as positive. However, the respondents mentioned the lack of a standard and, in some cases, clearly identifiable contact persons. They expressed the desire for a greater involvement of the shipboard service and for a more innovative support system including a hotline.
Quantitative Results
A total of 102 questionnaires were returned. Of the respondents, 65% (n = 52) were male, and 35% (n = 28) were female (no information n = 22). A total of 44% (n = 40) of respondents used telemedicine as a medical assistant, 42% (n = 37) had experience with telemedicine from the training course, and 38% (n = 35) used the application as a shipboard physician. Of the resoindents, 9% (n = 8) also had experience as an embarked physician, 7% (n = 6) as an advisor, and 4% (n = 4) as an instructor. This resulted in a return rate of 9% (n = 35) regarding shipboard physicians.
Assessment and Motivation
In total, 52% (n = 41) of participants thought that telemedicine applications had a positive effect on their confidence, 37% (n = 37) did not observe any change, and 1% (n = 1) observed a negative effect. Participants who used telemedicine applications largely approved of the equipment used in telemedicine workstation. A total of 46% of respondents considered the camera to be highly useful, while 41% considered the video conference system, 36% considered the transmission of digital X-ray images, and 29% considered the dermatology equipment useful.
However, other items such as gynecology or otolaryngology equipment were often unused (62%/47%).
Reasons for Consultation
Figure 1 shows the medical reasons for consultation stated by the respondents. The telemedicine workstation was most frequently used for the monthly connection tests (71.8%; n = 61). Official consults were the second most frequently reported reason cited by 48.2% (n = 41). This was followed by organizational matters by 43.3% (n = 37), contact with colleagues from other ships by 34.12% (n = 29), and interdisciplinary exchange by 31.76% (n = 27).
FIGURE 1.
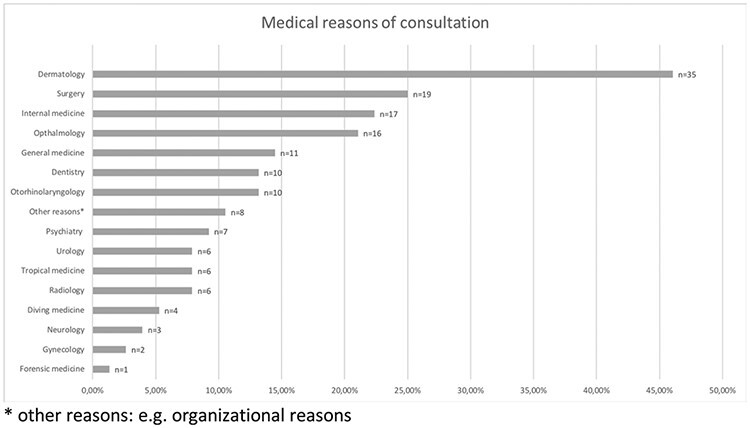
Overview of the consultations conducted for medical reasons (multiple answers possible) (n = 76).
Technical and Organizational Determinants
A total of 58% of respondents said they felt confident in handling the telemedicine workstation, while 42% did not feel confident. Seventy-eight percent of the latter were uncertain because of technical matters, and 29% were because of organizational matters. Other reasons for not using telemedicine workstations are listed in Table III.
TABLE III.
Reasons for Not Using Telemedicine Workstations (Multiple Answers Possible) (n = 77)
| Response options | Result |
|---|---|
| Technical problem with the ship power distribution system/communication system | 48.05% (n = 37) |
| Technical problem with the medical workstation (e.g., system not operational) | 44.16% (n = 34) |
| No medical necessity | 36.36% (n = 28) |
| Other reasons | 27.27% (n = 21) |
| Equipment (e.g., equipment needed was not available) | 23.38% (n = 18) |
| No assistance required in dealing with previous reasons for consultation | 19.48% (n = 15) |
| Technical problem of unknown origin | 16.88% (n = 13) |
| Amount of time required | 16.88% (n = 13) |
| Organizational effort required | 15.58% (n = 12) |
| Lack of time | 3.90% (n = 3) |
| I do not use the system as a matter of principle | 2.60% (n = 2) |
Another important technical factor was the accessibility and availability of remote stations. The survey showed that it took 78 minutes on average to set up a video conference with a Bundeswehr hospital.
In 69% (n = 42) of cases, the non-operability of the system was attributed to the reception conditions at sea, and in 59% (n = 36), the transmission rate was the limiting factor. Further, 30% (n = 18) of the respondents said the workstation needed to be repaired, while 11% (n = 7) stated that it was incomplete.
DISCUSSION
The present study aimed to identify the determinants for optimizing telemedicine in the Navy to develop a more target-oriented implementation.
The results of the study showed that users of telemedicine felt more confident in their treatment when using telemedicine, which also increased their confidence in the application.
The study revealed that telemedicine facilities increased the users’ confidence in employing them and subjectively optimized treatment. However, technical and organizational problems posed obstacles and led to greater use of simple but insecure alternatives to telemedicine workstations. The requirements of the successful implementation of telemedicine included proper support. Further, it was found that consultations were mainly sought to resolve questions concerning dermatological, surgical, and internal conditions. These results could be incorporated into future curricula for medical officers.
Qualitative Results
The average age of currently deployed medical personnel in the Navy is 36.0 years (Table I), which is lower than the average age of participants (41.0 years). This difference could be explained by the recruitment paths used (i.e., specifically selecting medical officers who, because of the duration of their professional training, took up their duties later in life). The percentage of women in the qualitative section of the present study was 30%, which approximately corresponds to the percentage of female medical officers in the Bundeswehr (33.8%).30
Both the assessment of telemedicine applications and participants’ motivation for using them showed that they are widely accepted. In particular, the relief provided through an official statement that acts as a validation appeared to be important for the medical officers. This constitutes a significant difference to the alternatives used so far, as these applications do not allow for an official statement to be obtained. The results confirmed the positive view of those responsible for telemedicine in the Navy.16 The ability to ask for a reliable and actionable statement could be a positive determinant. Other international studies have also considered acceptance of and interest in telemedicine to be important factors in the likelihood of using associated applications.31
In terms of the evaluation of the individual reasons for consultation, increased confidence among both the personnel and patients was observed as a consequence of frequent use of telemedicine. The facts that telemedicine workstations are installed on all ships permanently manned with a medical team and that they are linked to the Bundeswehr Hospital Hamburg are reasons for a frequent use of telemedicine applications.16 Further, with a maximum of 236 soldiers on frigates and 240 soldiers on combat support ships, the number of potential patients is high.32 The actual number of consultations, however, is between 1 and 3 per month.16
Apart from the determinants that are regarded as obstacles to using telemedicine, two additional factors must be considered when analyzing the figures. Although military ships are manned with a specialized medical officer who can use telemedicine to obtain a second opinion, the number of telemedicine consultations is rather low compared with civilian shipping.33 This could be because Navy soldiers always require medical clearance confirming their fitness for sea duty, which includes a comprehensive health check to verify their operational capability.34 The pretest probability for internal conditions could, therefore, be lower compared with civilian shipping.
The results of the present study showed that monthly communication checks are a significant determinant for continuous use, which increased users’ confidence in handling the workstation. During these checks, handling the workstation is also practiced. In addition to the initial workstation training, regular training and qualification measures were regarded as important for implementing telemedicine applications in other projects as well.35
After considering the effectiveness and clinical safety, as well as the motivation of and application by users, the respondents also reported on the technical and organizational determinants.
Lack of user-friendliness was considered a key negative aspect. Ease of operation of equipment was a key factor for the increased use of telemedicine and should, therefore, be ensured. The connection between the success of telemedicine and the ease, flexibility, and user-friendliness of system operations was previously described in a 2007 review. Users should, therefore, be included in the design process.36 The dynamic development of mobile digital media over the past decade means that there is an opportunity to provide systems with an innovative outfit, which should be exploited to improve user-friendliness.
Further, the results showed that a lack of technical reliability significantly limited the use of telemedicine applications. Lack of bandwidth was identified as a problem and, at times, even prevented further use of the equipment. Other studies have also identified both interoperability and standardization problems as reasons for the slow implementation of telemedicine in routine medical care.36
The organizational aspect of technical support was considered in the present study. The results showed that support is seen as useful and valuable; however, the respondents also highlighted the lack of an established standard and reported experiencing availability problems. A 2014 guide on health telematics described the importance of proper technical support for equipment and continuous IT support for users and suggested that a person responsible for IT matters should be included in each team.37 This has also been confirmed in other studies.36
Other process- and structure-related issues cannot be generalized, as the specific processes and structures of the Bundeswehr must be considered. However, Singapore’s National Telemedicine Guidelines, for example, comprise organizational factors that are considered important for implementing telemedicine, including organizational readiness (e.g., planning readiness, workplace environment readiness, and technical readiness).38
Quantitative Results
The average age of currently deployed medical personnel in the Navy is 36.0 years, which is close to the average age of the survey participants (35.9 years). As shown in Table I, the period of service is also approximately the same. The percentage of males in the quantitative section (65%) was higher than the percentage of males currently deployed as medical personnel (58%; Table I).
The exact return rate could not be determined, as the survey invitations were distributed via various paths in order to recruit as many participants as possible.
Some of the hypotheses tested in the qualitative method were confirmed by the results of the questionnaire. The respondents reported that telemedicine strengthened their confidence, although they also confirmed the existence of limiting technical and organizational determinants. Addressing the reasons for not using telemedicine workstations, as listed in Table III, could constitute an important approach to rapidly improving the implementation of telemedicine.
Figure 1 provides an overview of the reasons for consultation collected in the quantitative section of the study. The results correspond to those stated for international shipping where consultation was also mainly sought for dermatological, surgical, and internal conditions.8,9
Bundeswehr’s objective is to ensure that the outcome of medical treatment at sea and during operations conforms with German medical standards. This requirement illustrates the quality of medical care at the Bundeswehr, which is among the highest when internationally compared.32 Meeting these high expectations using telemedicine means that the appropriate conditions should be fostered and proper diagnostics provided in the relevant fields.
Strengths and Weaknesses
This is the first study to be conducted on telemedicine in the German Navy. At an international military level, limited publications are available on the determinants of implementing telemedicine applications onboard ships either.
The results of the present study could be used to formulate hypotheses; however, because of methodological reasons, they should not be generalized.
Documentation of all steps, a comprehensive analysis by researchers, and coding of interviews were conducted to ensure intersubjective conformability.39
Participants’ participation was voluntary. As a result, selection bias could be present, and it could be assumed that the results show a distorted representation of users’ motivation and commitment.
The return rate could only be determined quantitatively by approximation. This value depends on many variables and is not published. Therefore, this constitutes a limitation of the study. However, the good comparability with the sociodemographic of the currently deployed soldiers is a noteworthy strength. Further, the concept of representativeness is used differently in qualitative research than in quantitative research: “Thus, the aim of qualitative research results is not statistical representativeness, but rather qualitative representation.”40
An accompanying evaluation should be conducted to allow for continuous development. In future, an assessment from patients’ point of view would provide further useful information. This could be achieved by conducting an evaluation in accordance with the Model for Assessment of Telemedicine Applications.19
CONCLUSION
The present study revealed which determinants influence the use of telemedicine in the German Navy and where optimization is needed. The focus should be on strengthening the factors that positively affect users’ assessment and motivation, as well as continuous application. Technical and organizational obstacles frustrate ease of use and should be eliminated where possible. Changes in such areas increase user acceptance and improve medical care. Collecting empirical data on the medical reasons for consultation aboard ships is useful for adjusting the application of telemedicine. As part of this process, an evaluation of the systems should be conducted by users. Long-term, randomized controlled studies should be performed to gather data on the clinical effectiveness of the measures.
Supplementary Material
ACKNOWLEDGMENT
The authors would like to thank Ms Leonie Woeltjen (Institute of Family Medicine, University Medical Center Lübeck, Germany) for her input regarding the consensus version.
Contributor Information
Ensign Daniel Valentin Hötker, Institute of Family Medicine, University Medical Center Lübeck, Lübeck 23562, Schleswig-Holstein, Germany; Regional Medical Support Command Kiel, Bundeswehr Medical Service, Kiel 24106, Schleswig-Holstein, Germany.
Markus Matthias Ring, Medical Information Technology Section, Navy Medical Service Directorate, Rostock 18057, Mecklenburg-Vorpommern, Germany.
Jost Steinhäuser, Institute of Family Medicine, University Medical Center Lübeck, Lübeck 23562, Schleswig-Holstein, Germany.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Military Medicine online.
FUNDING
This research was funded by the Institute of Family Medicine, University Medical Center Lübeck. Therefore authors received no funding by any external resources. The content is solely the responsibility of the authors.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS
This study was approved by the ethics committee of the University of Lübeck, Germany, on July 10, 2018, and was financed by the Institute of Family Medicine. No external funding was received.
REFERENCES
- 1. Bundesärztekammer : Ärztliche Positionen zu Einsatzgebieten telemedizinischer Patientenversorgung. Tätigkeitsbericht der Bundesärztekammer. Available at http://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/pdf-Ordner/Telemedizin_Telematik/Telemedizin/118-DAET_EVI07_Einsatzgebiete_Telemedizin.pdf; published 2015; Accessed April 27, 2020.
- 2. Sagaro GG, Amenta F: Past, present, and future perspectives of telemedical assistance at sea: a systematic review. Int Marit Health 2020; 71(2): 97–104. [DOI] [PubMed] [Google Scholar]
- 3. Schepers B-F: Funkärztliche Beratung von Seeschiffen. Available at http://www.maritimemedizin.de/medien/pdf/PublikationNr.4.pdf; published 2004; Accessed April 27, 2020.
- 4. Flesche CW, Jalowy A, Inselmann G: Telemedicine in the maritime environment? Hightech with a fine tradition. Med Klin 2004; 99(3): 163–8. [DOI] [PubMed] [Google Scholar]
- 5. Horneland AM: Maritime telemedicine—where to go and what to do. Int Marit Health 2009; 60(1–2): 36–9. [PubMed] [Google Scholar]
- 6. Jerončić I, Nikolić J, Mulić R: Maritime medicine and medicine for seafarers. 6th IMSC, B Abstr 1847; 2014, pp 1–5. Solin, Croatia. [Google Scholar]
- 7. Taylor CJ: Gastroenteritis outbreaks on cruise ships: are sanitation inspection scores a true index of risk? Int Marit Health 2018; 69(4): 225–32. [DOI] [PubMed] [Google Scholar]
- 8. Dahl E: Medical practice during a world cruise: a descriptive epidemiological study of injury and illness among passengers and crew. Int Marit Health 2005; 56(1–4): 115–28. [PubMed] [Google Scholar]
- 9. Peake DE, Gray CL, Ludwig MR, Hill CD: Descriptive epidemiology of injury and illness among cruise ship passengers. Ann Emerg Med 1999; 33(1): 67–72. Available at https://linkinghub.elsevier.com/retrieve/pii/S0196064499704191; Accessed April 21, 2020. [DOI] [PubMed] [Google Scholar]
- 10. Wölke B: Hospital on the high seas. Military Medicine Worldwide. Available at https://military-medicine.com/article/3411-hospital-on-the-high-seas.html; Accessed January 17, 2021.
- 11. Hartmann V: Medizinische Versorgung in der Deutschen Marine. In: Ottomann C, Seidenstücker K-H, eds. Maritime Medizin. Springer; 2015: 417–25. [Google Scholar]
- 12. Mannhardt J: Die deutsche Marine im Rahmen der Internationalen Kooperation. Available at https://www.dmkn.de/wp-content/uploads/2015/11/Artikel_Multinationale_Kooperation_ueberarbeitet_1.pdf; published 2015; Accessed April 26, 2020.
- 13. Poropatich R, Lai E, McVeigh F, Bashshur R: The U.S. Army telemedicine and m-health program: making a difference at home and abroad. Telemed e-Health 2013; 19(5): 380–6. [DOI] [PubMed] [Google Scholar]
- 14. Withnall RDJ, Smith M, Graham DJ, Morris LE: Telemedicine in the UK Defence Medical Services: time for an upgrade? J R Army Med Corps 2016; 162(5): 318–20. [DOI] [PubMed] [Google Scholar]
- 15. Otto C, Weber T, Thömmes A: Telemedizin im Sanitätsdienst der Bundeswehr: Das Ziel ist ein Telematikverbund. Dtsch Arztebl 2003; 100(3): 99–103. [Google Scholar]
- 16. Braun AM, Beinkofer D: Telemedizin für die Deutsche Marine als Impulsgeber für die Zusammenarbeit des BwKrhs HH und des BwKrhs Westerstede. Wehrmedizin und Wehrpharmazie 2018; 42(4): 39–40. [Google Scholar]
- 17. Germany, Federal Republic of (Navy). Military Medicine Worldwide Web site. Available at https://military-medicine.com/almanac/185-germany-federal-republic-of-navy.html; Accessed January 17, 2021.
- 18. Schulze M, Simon M, Heide-Kattwinkel HW: Diagnostic facilities on board ships GER Navy. Military Medicine Worldwide. Available at https://military-medicine.com/article/3103-diagnostic-facilities-on-board-ships-ger-navy.html; accessed December 20, 2020.
- 19. Allner R, Wilfling D, Kidholm K, Steinhäuser J: Telemedicine projects in rural areas of Germany. A systematic evaluation with the “model for assessment of telemedicine”. Z Evid Fortbild Qual Gesundhwes 2019; 144–145: 102. doi: 10.1016/j.zefq.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 20. Arnold K, Scheibe M, Müller O, Schmitt J: Grundsätze für die Evaluation telemedizinischer Anwendungen—Ergebnisse eines systematischen Reviews und Konsens-Verfahrens [Principles for the evaluation of telemedicine applications: Results of a systematic review and consensus process]. Z Evid Fortbild Qual Gesundhwes 2016; 117: 9–19. [DOI] [PubMed] [Google Scholar]
- 21. Ekeland AG, Bowes A, Flottorp S: Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010; 79(11): 736–71. [DOI] [PubMed] [Google Scholar]
- 22. Creswell JW, Clark VLP: Ch. 3. Choosing a mixed methods design. Des Conduct Mix Methods Res. 1st ed. Sage Publications 2007; 53–107. [Google Scholar]
- 23. Krzaklewska E: Review: Graham Gibbs (2009). Analysing Qualitative Data. Forum: Qualitative Social Research 11(3): 4. Available at http:// nbn-resolving.de/urn:nbn:de:0114-fqs100341; accessed February 02, 2021. [Google Scholar]
- 24. Hopf C: Qualitative Interviews - ein Überblick. In: Flick U, Von Kardorff E, Steinke I, eds. Qualitative Forschung, Ein Handbuch. 13. Aufl. Rowohlt Taschenbuch Verlag; 2019: S.349–60. [Google Scholar]
- 25. Koro-Ljungberg M, Douglas EP, Therriault D, Malcolm Z, McNeill N: Reconceptualizing and decentering think-aloud methodology in qualitative research. Qual Res 2013; 13(6): 735–53. [Google Scholar]
- 26. SurveyMonkey Inc : SurveyMonkey Audience Web site. https://de.surveymonkey.com; Accessed April 26, 2020.
- 27. Mayring P: Qualitative inhaltsanalyse. In: Mey G, Mruck K, eds. Handbuch Qualitative Forschung in Der Psychologie. 1. Aufl. Vol 49. VS Verlag für Sozialwissenschaften; 2010: 601–13. [Google Scholar]
- 28. Schmidt C: Analyse von Leitfadeninterviews. In: Flick U, Von Kardorff E, Steinke I, eds. Qualitative Forschung. Ein Handbuch. 13. Aufl. Rowohlt Taschenbuch Verlag; 2019: 447–56. [Google Scholar]
- 29. Spriestersbach A, Röhrig B, Du Prel JB, Gerhold-Ay A, Blettner M: Deskriptive Statistik: Angabe statistischer Maßzahlen und ihre Darstellung in Tabellen und Grafiken. Dtsch Arztebl 2009; 106(36): 578–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hibbeler B: Ärzte bei der Bundeswehr: Mehr Last auf weniger Schultern. Dtsch Arztebl 2009; 106(31–32): 1546–50. [Google Scholar]
- 31. Saigi-Rubió F, Jiménez-Zarco A, Torrent-Sellens J: Determinants of the intention to use telemedicine: evidence from primary care physicians. Int J Technol Assess Health Care 2016; 32(1–2): 29–36. [DOI] [PubMed] [Google Scholar]
- 32. Hibbeler B: Sanitätsdienst der Marine: Spitzenmedizin auf hoher See. Dtsch Arztebl 2009; 106(44): 2184–6. [Google Scholar]
- 33. Assistance- und Telemedizin. ergo-med Web site. 2006. Available at https://www.ergo-med.de/arbeitsschutz/assistance-und-telemedizin/; Accessed April 28, 2020.
- 34. Torff H, Schwanecke A, Koch A, Greiner B: Körperliche Einschränkungen der Eignung und Leistungsfähigkeit der an Bord einzusetzenden Soldaten. Aktuel Ernahrungsmed 2003; 28(5): 99. [Google Scholar]
- 35. Waschkau A, Zwierlein R, Steinhäuser J: Barriers and enablers for telemedical applications in family physicians’ practices: qualitative results of a pilot study. Z Allgemeinmed 2019; 95(10): 405–12. [Google Scholar]
- 36. Broens THF, Huis in’t Veld RMHA, Vollenbroek-Hutten MMR, Hermens HJ, Van Halteren AT, Nieuwenhuis LJM: Determinants of successful telemedicine implementations: a literature study. J Telemed Telecare 2007; 13(6): 303–9. [DOI] [PubMed] [Google Scholar]
- 37. Telligen, Great Plains Telehealth Resource and Assistance Center (gpTRAC) : Telehealth: start-up and resource guide. 2014. Available at https://www.healthit.gov/sites/default/files/playbook/pdf/telehealth-startup-and-resource-guide.pdf; Accessed February 01, 2021.
- 38. Ministry of Health : National telemedicine guidelines. 2015. Available at https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/guidelines/moh-cir-06_2015_30jan15_telemedicine-guideli nes-rev.pdf; Accessed February 01, 2021.
- 39. Creswell JW, Clark VLP: Choosing a mixed methods design. Des Conduct Mix Methods Res. 3rd ed. Sage Publications; 2017. [Google Scholar]
- 40. Kruse J: Qualitative Interviewforschung. Ein Integrativer Ansatz. Beltz Juventa Verlag; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


