Abstract
Objectives
Research suggests that self-perceptions of aging (SPA) have effects on physical, mental, cognitive, and emotional well-being among older adults. Few studies have examined the effects of SPA on social well-being. This study investigates the association of SPA with trajectories of social disconnectedness and loneliness in older Americans and explores mechanisms linking SPA and the 2 forms of social isolation.
Methods
We conducted Latent Growth Curve Modeling and path analysis using 3-wave data spanning 8 years (2008/2010–2016/2018) from the Health and Retirement Study. The sample included respondents aged 65 and older (N = 3,597) at baseline (2008/2010). SPA was measured by the Attitudes Toward Own Aging Scale. Social disconnectedness was an index including 6 indicators of social networks and social engagement. Loneliness was measured using the 11-item UCLA Loneliness Scale.
Results
Older adults with more negative SPA at baseline were more lonely but had slower rates of increase in loneliness during the 8-year study period. More negative SPA also predicted greater social disconnectedness but was not significantly related to the rate of change in social disconnectedness over time. The effects of SPA on social disconnectedness were primarily indirect through loneliness, whereas SPA had direct effects on loneliness. Overall, SPA had a stronger association with loneliness than with social disconnectedness.
Discussion
The results suggest that older adults with negative SPA are at risk of loneliness which then leads to social disconnectedness. Asking about SPA during individual assessment with older adults may help to discern issues with loneliness.
Keywords: Ageism, Loneliness, Social isolation, Social networks
Social isolation, a long-standing problem with older adults, has both objective and subjective dimensions (Shiovitz-Ezra et al., 2018). Objective isolation refers to a lack of social contact and involvement and is often indicated by social disconnectedness (Cornwell & Waite, 2009b). Subjective isolation, which is frequently indicated by loneliness, refers to the subjective experience of a shortfall in one’s social relationships (Cornwell & Waite, 2009b). While the two forms (or dimensions, used interchangeably herein) of social isolation are significantly correlated, they are not the same (Santini et al., 2020). Both social disconnectedness and loneliness are prevalent among older adults in the United States. Depending on the operational definition, 24%–40% of community-living older Americans (age 65+) are reported to be socially disconnected (Cudjoe et al., 2020), and 43% of adults aged 60+ reported feeling lonely (Perissinotto et al., 2012). Several systematic reviews have concluded that both subjective and objective social isolation have adverse effects on physical and mental health, quality of life, cognitive functions, and mortality (Evans et al., 2019; Holt-Lunstad et al., 2015; Mehrabi & Béland, 2020; Valtorta et al., 2016). In addition, research suggests that the health effects of social disconnectedness and loneliness are independent of each other (Cornwell & Waite, 2009a; Luo & Waite, 2014; Yu et al., 2021).
Prior studies have reported that sociodemographic characteristics (age, gender, marital status, socioeconomic status), self-rated health, functional health, depression, and cognitive function are risk factors for both social disconnectedness (Cudjoe et al., 2020; Merchant et al., 2020; Nagarajan et al., 2020) and loneliness (Ayalon et al., 2016; Fierloos et al., 2021; Santini et al., 2020; see review Dahlberg et al., 2021) among older adults. Few studies, however, have examined the role of self-perceptions of aging (SPA) in either form of social isolation.
SPA and Social Isolation
SPA refers to individuals’ attitudes and expectations toward their own aging. Stereotype embodiment theory (Levy, 2009) suggests that beginning in early life, people formulate age stereotypes through socialization experiences. Throughout the life course, age stereotypes are reshaped, reinforced, and internalized. At older ages, these age stereotypes become self-relevant and constitute SPA (Levy, 2003). It has been suggested that stereotypes long accepted as truth can produce powerful expectations and lead to chronic activation of self-relevant schemas concerning decline in physical and socioemotional well-being (Levy et al., 2002). During the last two decades, a growing body of research has shown that SPA is associated with psychological well-being, quality of life, physical and cognitive functioning, morbidity, and mortality (see reviews: Chang et al., 2020; Hu et al., 2020; Westerhof et al., 2014). Some researchers suggest that the SPA–health association operates as a self-fulfilling prophecy (Robertson et al., 2016; Tovel et al., 2019). For instance, older adults with more positive SPA employ more selection, optimization, and compensation strategies to cope with daily life stressors, which, in turn, contribute to better health outcomes (Wurm et al., 2013).
Perceptions about aging can also affect social isolation through self-fulfilling prophecies. Cognitive theories assume that beliefs and thoughts are the primary determinants of emotion and behavior (Beck, 1979; DiGiuseppe et al., 2016; Dozois & Beck, 2008). If an older person views loneliness as a natural part of aging, they are less likely to take action to change their behavior or situation. Consequently, they are likely to continue feeling lonely, reinforcing their negative views about aging (Pikhartova et al., 2016). In addition, common stereotypes of older persons, such as being unattractive, boring, and lonely (Steverink et al., 2001), if internalized, may affect social behavior including motivation to engage socially (Shiovitz-Ezra et al., 2018). For instance, persons who feel less attractive due to aging may withdraw from or be sensitive to rejection during social interactions. Another perspective offered by Cheng (2017) posits that older adults with negative SPA, such as a belief that older people are weak and need help, may expect more support from others. When such high expectations are not met, particularly when not in proportion with objective needs, their dissatisfaction with social relationships and feelings of loneliness increase.
Empirical studies examining the association between SPA and social isolation are scarce. Analyzing two waves of data (2008 and 2014) from the German Aging Survey, Schwartz and colleagues (2021) found that positive SPA in 2008 was associated with an increase in social involvement, including informal social interactions and participation in groups and organizations, over 6 years. Menkin and colleagues’ (2017) study found that positive expectations regarding aging were associated with new friendship development 2 years later and greater perceived support availability 12 months later. More negative SPA was associated with lower satisfaction with the support of one’s offspring among older Chinese adults in Hong Kong (Cheng, 2017). Other studies report associations between SPA and loneliness. Pikhartova et al. (2016) found that older adults holding expectations of loneliness in old age, compared to those who did not, reported greater loneliness 8 years later. Negative SPA, especially the perception of oneself as a burden, was associated with an increase in loneliness during the coronavirus disease 2019 lockdown period (Losada-Baltar et al., 2021).
The Present Study
The present study used three-wave longitudinal data (across 8 years) with a nationally representative sample of older adults in the United States to examine the association of SPA with objective and subjective social isolation. We sought to answer two questions. First, is SPA associated with trajectories of objective and subjective social isolation? Based on cognitive theories (Beck, 1979; DiGiuseppe et al., 2016; Dozois & Beck, 2008) and prior empirical research, we hypothesize that SPA is associated with trajectories of social disconnectedness and loneliness. Specifically, we expect older adults with more negative SPA to have higher levels of social disconnectedness and loneliness and faster rates of increase in both over time.
As mentioned above, subjective and objective isolation are two distinct concepts (Cornwell & Waite, 2009a; Luo & Waite, 2014; Yu et al., 2021). Prior research has shown that objective and subjective indicators of social isolation have reciprocal influence (Santini et al., 2020). So it is possible that SPA’s effects on social disconnectedness are indirect via loneliness. Likewise, SPA’s effects on loneliness may be indirect via social disconnectedness. Hence, our second research question is: How does SPA influence each of the two dimensions of social isolation? We took an exploratory approach to this question as no studies have examined the relationship between SPA, loneliness, and social disconnectedness. Given the evidence of reciprocal influence between the two forms of isolation (Santini et al., 2020), we expect to observe indirect effects of SPA on each. The question is how much the total effects of SPA on each of the two dimensions of social isolation are indirect. In other words, what is the role of social disconnectedness in linking SPA and loneliness, and what is the role of loneliness in linking SPA and social disconnectedness? The answer would provide a better understanding of the mechanisms underlying the associations of SPA with the two forms of social isolation and suggest the form of isolation that individuals with negative SPA are at greater risk of.
Method
Data and Sample
We conducted a secondary data analysis using data from the Health and Retirement Study (HRS), a biennial longitudinal study of a national representative sample of individuals aged 50 and older in the United States. The HRS has a psychosocial and lifestyle questionnaire, known as the Leave-Behind Questionnaire (LBQ), that includes questions on SPA (Smith et al., 2017). The LBQ is left to respondents who have completed the core in-person interview to fill out and return by mail. In each wave, half of the respondents are asked to fill out the LBQ. Thus, LBQ questions are completed by respondents every 4 years. For this analysis, we selected respondents aged 65 years and older who returned the LBQ in 2008/2010 (T1, the first time that the SPA measure was administered) as the baseline sample (N = 3,597). Three waves of data (2012/2014 [T2] and 2016/2018 [T3]), with each wave 4 years apart, were analyzed. At T2 and T3, 81 and 81 respondents, respectively, did not return the LBQ. Respondents who did not mail back the LBQ at any of the follow-ups, compared to those who had all three waves of data, were not significantly different in any of the study variables measured at T1.
Variables and Measures
Self-perception of aging
The Attitudes Toward Own Aging Scale was used to assess SPA (Kleinspehn-Ammerlahn et al., 2008; Liang & Bollen, 1983). Respondents were asked their perspectives on their own aging (1 = strongly disagree, 6 = strongly agree). A sample statement is “things keep getting worse as I get older.” We created an SPA scale by reverse-coding four positively worded items, standardizing each item, and then averaging the scores across all eight items. Higher SPA scores indicated more negative SPA and were set to missing if four or more items had missing values. The SPA scale had a Cronbach’s alpha of 0.80 at T1.
Social disconnectedness
We created an index modified from the Social Disconnectedness Scale developed by Cornwell and Waite (2009a, 2009b). We standardized and averaged six items: social network size, number of friends, average network contact frequency, socializing with relatives and friends, attending group meetings, and volunteering. Social network size was the number of people that respondents felt close to. Number of friends was the number of friends that respondents have a close relationship with. We top-coded social network size and number of friends at the 99th percentile to trim outliers. For network size, values of 43 and above were top-coded (43–59 cases across T1, T2, and T3). For number of friends, the top value was 25 (34–37 cases across the three time points). To gauge frequency of contact with network members, we averaged in-person, phone, letter/email, and social media contact. Socializing with relatives and friends was the average of in-person contact with both relationship types; each was rated on a 6-point scale (1 = less than once a year or never, 6 = three or more times a week). Attending group meetings and volunteering was assessed by a single item on a 7-point scale (1 = never/not relevant, 7 = daily). All six items for the Social Disconnectedness Index were reverse-coded before being standardized so that higher scores of the index (range: −5.14 to 2.68) indicated more social disconnectedness. The index had a Cronbach’s alpha of 0.65 at T1, 0.66 at T2, and 0.68 at T3.
Loneliness
We used the 11-item UCLA Loneliness Scale, which has shown good factorability and internal validity, to measure loneliness (Lee & Cagle, 2017). A sample item is “How much of the time do you feel left out?” Respondents were asked to rate each item on a 3-point scale (1 = often, 2 = sometimes, 3 = hardly ever or never). We reverse-coded the four negatively worded items so that higher scores indicated greater loneliness. Each item was standardized, then summed and averaged. The final loneliness score was set to missing if more than five items had missing values. The loneliness scale had a Cronbach’s alpha of 0.88, 0.86, and 0.87 at T1, T2, and T3, respectively.
Covariates
We included two sets of covariates, sociodemographic characteristics and health-related factors, to estimate the associations of SPA with social disconnectedness and loneliness net of these potential confounders. All covariates were measured at T1. Sociodemographic characteristics included sex (0 = male, 1 = female), race (0 = White, 1 = Black, 2 = others), years of education (range 0–17), marital status (0 = not currently married/partnered, 1 = currently married/partnered), and employment status (0 = not currently employed, 1 = currently employed). Health-related factors included number of chronic conditions (range 0–8), limitations in activities of daily living (ADL; 0 = none, 1 = 1+ limitation), limitations in instrumental activities of daily living (IADL; 0 = none, 1 = 1+ limitation), memory (range 0–20), and depressive symptoms (range 0–8). Chronic conditions were a count of doctor-diagnosed conditions, including high blood pressure, diabetes, cancer, lung disease, heart condition, congestive heart failure, stroke, and arthritis, as reported by respondents. The ADL included dressing, walking, bathing, eating, getting in or out of bed, and using the toilet. The IADL included meal preparation, grocery shopping, making phone calls, taking medication, house/yard work, and managing finances. Having difficulty in one or more of the tasks (ADL, IADL) was considered as having limitations. Memory was assessed by recall of a 10-word list. A memory score was calculated by adding up the number of words correctly recalled immediately and after a short delay. Depressive symptoms were assessed by the eight-item Center for Epidemiological Studies—Depression scale (Turvey et al., 1999). Each item was rated yes (=1) or no (=0). We summed the eight items. The scale had a Cronbach’s alpha of 0.81.
Data Analysis
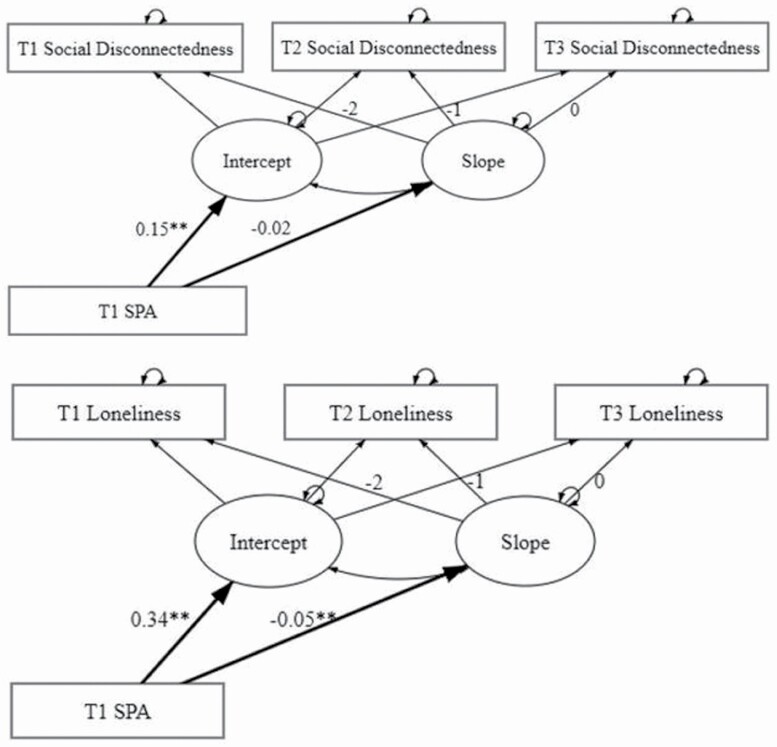
To test the associations of T1 SPA with trajectories of social disconnectedness and loneliness, we used Latent Growth Curve Modeling that is based on Structural Equation Modeling. For each isolation dimension, we first estimated an unconditional growth model with two latent variables—intercept and slope—using observations at the three time points as manifest variables. We fixed the factor loading of the slope latent variable to −2, −1, and 0, so the intercept represents the status at T3 (Duncan & Duncan, 1995). Then we added T1 SPA and covariates as predictors of the intercept and slope (see Figure 1). Goodness-of-fit statistics, including the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (sRMR), were used to evaluate the models. Values greater than 0.95 for the CFI, and of 0.06 or less for the RMSEA and sRMR, were considered to reflect a good model fit (Hoyle & Panter, 1995).
Figure 1.
Latent growth curve models for social disconnectedness and loneliness. Notes: SPA = self-perceptions of aging. The figures shown are standardized coefficients. The models control for age, gender, race, marital status, employment, functional limitations, chronic conditions, depressive symptoms, and memory (see Supplementary Table 1 for more results). *p < .01, **p < .001.
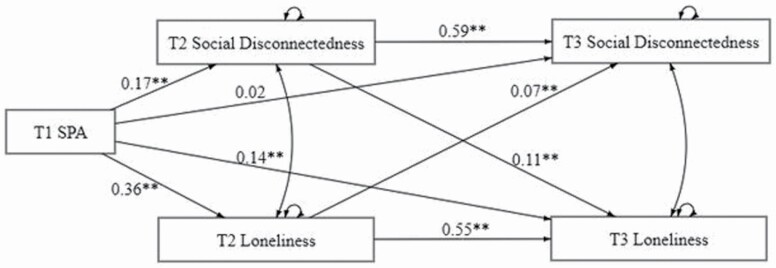
To answer the second research question about mechanisms linking SPA with social disconnectedness and loneliness, we conducted a path analysis. The model was constructed as a fully saturated model, with direct paths from T1 SPA to social disconnectedness and loneliness at T2 and T3, and direct paths from T2 social disconnectedness to T3 loneliness and from T2 loneliness to T3 social disconnectedness (see Figure 2). We then determined whether the model could be simplified by restricting statistically nonsignificant paths to zero. Based on the better fit model, we calculated the direct, indirect, and total effects of T1 SPA on T3 social disconnectedness and T3 loneliness. Of key interest are the indirect effects (T1 SPA → T2 social disconnectedness → T3 loneliness; T1 SPA → T2 loneliness → T3 social disconnectedness). We computed the size of the indirect effects using MacKinnon’s (2008) formula (Preacher & Kelley, 2011).
Figure 2.
Results of a fully saturated model to estimate longitudinal associations of SPA with social disconnectedness and loneliness. Notes: SPA = self-perceptions of aging. The figures shown are standardized path coefficients. Direct paths from T1 covariates to T2 and T3 social disconnectedness and loneliness are not shown. *p < .01, **p < .001.
To maximize statistical power while minimizing bias, full information maximum likelihood estimation was used. This method to address missing data is termed a principled missing data method in that it does not replace missing values directly; instead, it uses available information to estimate population parameters without bias (Dong & Peng, 2013). In all analyses, estimates are adjusted for stratification and clustering in the T1 sample and weighted using the HRS-provided respondent-level weight for the LBQ. This weight is the product of the HRS respondent-level weight, a face-to-face interview adjustment factor, and a nonresponse adjustment factor for the LBQ, which adjusts for selection into the face-to-face sample and nonresponse to the psychosocial questionnaire (Smith et al., 2017). Given the large sample size, we set statistical significance at p < .01 (two-tailed). Robust standard errors were used.
Results
Table 1 shows the baseline characteristics of the sample (N = 3,597). After applying weights, their mean age was 72 years old. Most of the sample were female (57.2%), White (89.8%), married (64.7%), and not employed (78.6%). On average, they had 13 years of education. A majority had no ADL (89.3%) and IADL limitations (79.9%), and few depressive symptoms (mean = 0.21, range 0–7). They had, on average, two chronic conditions (range 0–7) and a memory score of 10.11 (range 0–20).
Table 1.
Sample Characteristics (N = 3,597)
| Weighted | Unweighted | ||
|---|---|---|---|
| Variables | Range | Mean (SD) | Mean (SD) |
| % | % | ||
| Age (in years) | 65–93 | 71.94 (5.53) | 72.30 (5.20) |
| Female | 57.2% | 59.6% | |
| Race | |||
| White | 89.8% | 85.8% | |
| Black | 6.9% | 11.0% | |
| Other | 3.3% | 3.2% | |
| Years of education | 0–17 | 13.01 (2.85) | 12.90 (2.85) |
| Married/partnered | 64.1% | 64.7% | |
| Employed | 21.4% | 19.7% | |
| Number of chronic conditions | 0–7 | 2.08 (1.23) | 2.13 (1.23) |
| Depressive symptoms | 0–7 | 0.21 (1.04) | 0.20 (1.03) |
| Memory | 0–20 | 10.11 (3.07) | 10.0 (3.02) |
| Having ADL limitations | 10.7% | 10.5% | |
| Having IADL limitations | 20.1% | 19.8% |
Notes: ADL = activities of daily living; IADL = instrumental activities of daily living; SD = standard deviation. Depressive symptoms were measured using the eight-item Center for Epidemiological Studies—Depression scale. Memory was measured using immediate and delayed word list recall task.
Table 2 shows the Pearson correlation between the key study variables. SPA at T1 was significantly correlated with social disconnectedness and loneliness at all three time points, having stronger correlations with loneliness (rs = 0.38–0.46) than with social disconnectedness (rs = 0.17–0.19). Social disconnectedness and loneliness were correlated cross-sectionally (rs = 0.30–0.38) and longitudinally (rs = 0.29–0.34).
Table 2.
Pearson Correlations of SPA, Social Disconnectedness, and Loneliness (Weighted)
| T1 SPA | T1 Social disconnectedness | T2 Social disconnectedness | T3 Social disconnectedness | T1 Loneliness | T2 Loneliness | T3 Loneliness | |
|---|---|---|---|---|---|---|---|
| T1 SPA | 1 | 0.19 | 0.18 | 0.17 | 0.46 | 0.4 | 0.38 |
| T1 Social disconnectedness | 1 | 0.63 | 0.58 | 0.36 | 0.32 | 0.30 | |
| T2 Social disconnectedness | 1 | 0.62 | 0.33 | 0.37 | 0.34 | ||
| T3 Social disconnectedness | 1 | 0.29 | 0.30 | 0.38 | |||
| T1 Loneliness | 1 | 0.65 | 0.57 | ||||
| T2 Loneliness | 1 | 0.63 | |||||
| T3 Loneliness | 1 |
Notes: All correlations are significant at p < .001. SPA = self-perceptions of aging.
Associations of SPA With Trajectories of Social Disconnectedness
The unconditional growth model for social disconnectedness shows a statistically significant positive linear slope (β = 0.07, SE = 0.01, p < .001), indicating an average increase of 0.07 standardized units every 4 years (χ 2 = 14.42 (1), CFI = 1.00, RMSEA = 0.06, sRMR = 0.01). After adding T1 SPA and the covariates as exogenous variables predicting the intercept and slope, the model still fits the data quite well (χ 2 = 36.61 (14), CFI = 1.00, RMSEA = 0.02, sRMR = 0.01). The results show that SPA is significantly and positively related to the intercept, indicating that older people with more negative SPA at T1 are more socially disconnected at T3 (β = 0.15, SE = 0.02, p < .001; see Figure 1). SPA does not significantly predict the slope (β = −0.02, SE = 0.01, p = .08), which means that SPA does not affect the rate of change in social disconnectedness over the 8-year period. All estimates of the model are shown in Supplementary Table 1.
Associations of SPA With Trajectories of Loneliness
The unconditional growth model for loneliness indicates that loneliness, on average, increases 0.05 standardized units every 4 years (β = 0.05, SE = 0.01, p < .001; χ 2 = 6.86 (1), CFI = 1.00, RMSEA = 0.04, sRMR = 0.01). The fit of the model is good after including SPA and the covariates as predictors of the intercept and slope (χ 2 = 44.01 (14), CFI = 0.99, RMSEA = 0.03, sRMR = 0.01). The estimates show that SPA is a significant predictor of the intercept (β = 0.34, SE = 0.02, p < .001) and the slope (β = −0.05, SE = 0.01, p < .001; see Figure 1). That is, older people with more negative SPA at T1 are lonelier at T3 and have slower rates of increase in loneliness over time (see Supplementary Table 1 for the full results).
Direct, Indirect, and Total Effects of SPA on Social Disconnectedness and Loneliness
To examine how SPA influences each dimension of social isolation, we estimated a fully saturated model as shown in Figure 2. Except for the path from T1 SPA to T3 social disconnectedness, which is not statistically significant (β = 0.02, SE = 0.02, p = 0.14), all other paths are statistically significant at p < .01. In other words, the direct effects of T1 SPA on T3 social disconnectedness are not statistically significant after adjusting for T2 loneliness, T2 social disconnectedness, and the covariates. This finding indicates that the association between T1 SPA and T3 social disconnectedness is mediated by loneliness.
We then estimated a reduced model in which the path from T1 SPA to T3 social disconnectedness was restricted to zero (results shown in Supplementary Table 2). The reduced model fits the data quite well (χ 2 = 2.14 (1), CFI = 1.00, RMSEA = 0.018, sRMR = 0.001). T1 SPA has significant effects on T3 loneliness (β = 0.13, SE = 0.01, p < .001), after controlling for T2 social disconnectedness, T2 loneliness, and T1 covariates. Social disconnectedness and loneliness have significant cross-leg effects.
We decomposed the total effects of T1 SPA on T3 social disconnectedness and loneliness based on the reduced model (Table 3). The path from T1 SPA → T2 loneliness → T3 social disconnectedness, which indicates indirect effects of T1 SPA on T3 social disconnectedness via T2 loneliness, is statistically significant (β = 0.03, SE = 0.01, p < .001). That is, more negative SPA at T1 leads to higher levels of loneliness at T2 (β = 0.36, SE = 0.02, p < .001), which contributes to more social disconnectedness at T3 (β = 0.08, SE = 0.02, p < .001; see Supplementary Table 2). The model shows that the total effects between T1 SPA and T3 social disconnectedness are 0.13 (SE = 0.01, p < .001), of which 23.1% is contributed by indirect effects via loneliness.
Table 3.
Direct, Indirect, and Total Effects of T1 SPA on T3 Social Disconnectedness and Loneliness
| Model | β | SE | Effect size |
|---|---|---|---|
| Total effects of T1 SPA on T3 social disconnectedness | 0.13** | 0.01 | |
| Indirect effects of T1 SPA on T3 social disconnectedness | |||
| T1 SPA → T2 social disconnectedness → T3 social disconnectedness | 0.10** | 0.01 | 76.9% |
| T1 SPA → T2 loneliness → T3 social disconnectedness | 0.03** | 0.01 | 23.1% |
| Total effects of T1 SPA on T3 loneliness | 0.35** | 0.02 | |
| Direct effects of T1 SPA on T3 loneliness | 0.13** | 0.01 | 37.1% |
| Indirect effects of T1 SPA on T3 loneliness | |||
| T1 SPA → T2 loneliness to → loneliness | 0.20** | 0.01 | 57.1% |
| T1 SPA → T2 social disconnectedness → T3 loneliness | 0.02** | 0.003 | 5.7% |
Notes: SE = standard error; SPA = self-perceptions of aging.
*p < .01. **p < .001.
Regarding the relationship between T1 SPA and T3 loneliness, the indirect effects (T1 SPA → T2 social disconnectedness → T3 loneliness) are statistically significant (β = 0.02, SE = 0.003, p < .001) and suggest that more negative SPA at T1 leads to more social disconnectedness at T2 (β = 0.17, SE = 0.02, p < .001), which increases loneliness at T3 (β = 0.11, SE = 0.01, p < .001; see Supplementary Table 2). The total effects between T1 SPA and T3 loneliness are 0.35 (SE = 0.02, p < .001), about 5.7% of which is indirect effects via T2 social disconnectedness. Compared to the indirect effect of T1 SPA → T3 social disconnectedness via T2 loneliness (23.1%), the indirect effects of T1 SPA → T3 loneliness via T2 social disconnectedness (5.7%) is much smaller. The total effects of T1 SPA on T3 loneliness (0.35) are almost three times the total effect of T1 SPA on T3 social disconnectedness (0.13).
Discussion
This study set out to examine the role of SPA in social isolation among older adults. We found that SPA is associated with trajectories of loneliness. Specifically, more negative SPA is associated with higher levels, but slower rates of increase, of loneliness during the 8-year study period. Regarding social disconnectedness, more negative SPA is associated with more social disconnectedness throughout the 8 years, but SPA is not significantly related to changes in social disconnectedness over time. We also found that the association of SPA and social disconnectedness is primarily mediated by loneliness, whereas social disconnectedness plays a minor role in linking the association between SPA and loneliness.
Our study, to our knowledge, is the first to examine the longitudinal association between SPA, social disconnectedness, and loneliness in later life. Our findings are consistent with the few studies that report SPA to be related to new friendship development (Menkin et al., 2017), social engagement (Schwartz et al., 2021), perceptions of social support (Cheng, 2017), and loneliness (Losada-Baltar et al., 2021). These studies, however, only focused on one dimension of social isolation. We have expanded on prior studies by investigating both subjective and objective social isolation in the same study. This examination not only allows us to compare the relative strength of the association between SPA and the two forms of social isolation, but also the role of each form in the association between SPA and the other form of isolation.
Two of our findings are somewhat unexpected. First, we found older people with more negative SPA to have slower increase of loneliness over time (β = −0.05, SE = 0.01, p < .001). This finding may be interpreted through the lens of the evolutionary theory of loneliness (Cacioppo & Cacioppo, 2018; Cacioppo & Patrick, 2009). This theory suggests that the feeling of loneliness is part of an evolutionary warning system to signal threats or damage to our social well-being. In other words, older adults with high negative SPA at T1 may be lonely and distressed which motivate them to seek ways to alleviate the feeling of loneliness. Our post-hoc descriptive analysis shows that those with high negative SPA at T1 (1 SD above the mean) had high levels of loneliness at T1 and a reduction of loneliness between T1 and T2, which seems to be consistent with the evolutionary theory. The reduction was not observed between T2 and T3; instead, their loneliness scores slightly increased.
Another unexpected finding is that T1 SPA does not significantly predict the rate of change in social disconnectedness, although T1 SPA is significantly associated with the level of social disconnectedness 8 years later. The path analysis we conducted to disentangle the direct and indirect effects of SPA on social disconnectedness helps explain this finding. We found that SPA’s effects on social disconnectedness are primarily indirect via loneliness, which means that SPA does not influence social disconnectedness directly and that loneliness is a linchpin through which SPA is associated with social disconnectedness. From a practical standpoint, the findings suggest that older people with negative SPA are at greater risk of loneliness than social disconnectedness.
Overall, our findings support the premise of cognitive theory that negative thoughts lead to disturbing emotions (Beck, 1979; Dozois & Beck, 2008). In the case of SPA, negative views toward aging may arouse feelings of loneliness which, in turn, lowers motivation to engage socially and foster social withdrawal. DeWall and colleagues (2009) note that people who feel lonely display a heightened vigilance against social threats.
This current study’s findings add to the existing literature about the relationship between SPA and health. Several systematic reviews have concluded that SPA is significantly associated with a wide range of health outcomes including cognitive functions, functional limitations, mental health, and quality of life (Chang et al., 2020; Hu et al., 2020; Westerhof et al., 2014), although the pathways between SPA and health outcomes are not clear. Our findings suggest that perhaps social isolation, particularly loneliness, is one of the pathways. SPA has a significant and medium effect size relationship with loneliness. Numerous studies have shown that loneliness is associated with cardiovascular disease (see review: Valtorta et al., 2016), depression (Santini et al., 2020), cognitive impairment (Ayalon et al., 2016), poor functional health, and mortality (see reviews: Holt-Lunstad et al., 2015; Mehrabi & Béland, 2020). It is therefore quite possible that negative SPA increases feelings of loneliness, which then lead to adverse health outcomes. Whether and how social isolation mediates between SPA and different health domains is an agenda for future research.
This study has several methodological strengths. First, we used three-wave longitudinal data to examine the associations between SPA and the trajectories of objective and subjective social isolation. The growth curve analysis provides a clearer picture of the effects of SPA on the level of social disconnectedness and loneliness, and on their changes over time. Second, we conducted path analyses in which measures of the predictor (T1 SPA), mediator (T2 social disconnectedness and T2 loneliness), and outcome (T3 social disconnectedness and T3 loneliness) were taken at different time points. Given that SPA, social disconnectedness, and loneliness are all based on self-report and hence subject to common method variance, differentiation of the temporal order of these variables helps reduce common method bias. Third, we used multiple items to assess SPA, loneliness, and social disconnectedness. The UCLA Loneliness Scale (Lee & Cagle, 2017) and the Attitudes Toward Own Aging Scale (Liang & Bollen, 1983) have been widely used and demonstrated factorial validity and internal consistency reliability. We constructed the Social Disconnectedness Index based on the Social Disconnectedness Scale developed by Cornwell and Waite (2009a, 2009b). The Cronbach’s alpha of our Social Disconnectedness Index falls between 0.65 and 0.68 across the three time points, which means that estimates of relationships between social disconnectedness and other variables may be correspondingly attenuated (Schmitt, 1996). It is probable that our study has underestimated the association between SPA and social disconnectedness.
Our study has limitations. The first is that we have not considered the dynamics of SPA. We chose to use T1 SPA as the independent variable because we wanted to clarify the temporal order when estimating the effects of SPA on trajectories of social disconnectedness and loneliness. A second limitation is that we have not examined the influence of social isolation on SPA. Studies have indicated that SPA may be affected by informal social involvement and loneliness (Diehl et al., 2021; Schwartz et al., 2021). A third limitation is that we have only three data points, which limits us from estimating polynomial models for trajectories of loneliness and social disconnectedness. A fourth limitation is that even though we have included a wide range of covariates in the models, unobserved heterogeneity is still a threat to the validity of the findings. In addition, we treated the covariates as time-fixed variables. It is possible that some respondents experienced significant life events and health changes during the 8-year study period. Finally, we acknowledge that other advanced methods, such as Instrumental Variables Estimation for Panel Data, could be used to clarify the directionality of the key study variables.
Given that we are the first to report the associations between SPA and the two dimensions of social isolation, more research is needed to replicate our findings. Future studies should also examine reciprocal influences between SPA and the two forms of isolation and investigate whether either or both forms are pathways between SPA and health outcomes. Although it may be premature to suggest policy or practice interventions based on our findings, the evidence we present here supports a significant and moderately strong association between SPA and loneliness. Assessing the SPA of older persons may help to identify those who are at risk of loneliness. In particular, some older people may have a hard time admitting they are lonely as loneliness carries a social stigma. Asking about their perceptions of aging may be less threatening.
In conclusion, we found that SPA have differential effects on loneliness and social disconnectedness among older adults. While more negative SPA is related to higher levels of loneliness and social disconnectedness over an 8-year period, the association between SPA and loneliness is much stronger than that between SPA and social disconnectedness. Further, SPA predicts changes in loneliness but not social disconnectedness over time. Our path analysis shows that the effects of SPA on social disconnectedness are primarily mediated by loneliness, whereas SPA has direct effects on loneliness. More research is needed to examine potential reciprocal effects between SPA and the two forms of social isolation, and to investigate whether and how each form of isolation mediates the relationship of SPA with physical and mental health outcomes.
Supplementary Material
Funding
This work is supported by the University of Michigan Elizabeth Douvan Junior Scholars Fund in Life Course Development and the Henry J. Meyer Scholarship awarded to the first author. The Health and Retirement Study is supported by the National Institute on Aging (NIA U01AG009740).
Conflict of Interest
None declared.
Author Contributions
R. X. Hu conceived the study, conducted data analysis, and wrote up a first draft of the manuscript. L. W. Li was involved in the conceptualization of the study, interpretation of findings, and revisions of the manuscript.
References
- Ayalon, L., Shiovitz-Ezra, S., & Roziner, I. (2016). A cross-lagged model of the reciprocal associations of loneliness and memory functioning. Psychology and Aging, 31(3), 255–261. doi: 10.1037/pag0000075 [DOI] [PubMed] [Google Scholar]
- Beck, A. T. (1979). Cognitive therapy and the emotional disorders. Penguin. [Google Scholar]
- Cacioppo, J. T., & Cacioppo, S. (2018). Chapter three—Loneliness in the modern age: An evolutionary theory of loneliness (ETL). Advances in Experimental Social Psychology, 58, 127–197. doi: 10.1016/bs.aesp.2018.03.003 [DOI] [Google Scholar]
- Cacioppo, J. T., & Patrick, W. (2009). Loneliness: Human nature and the need for social connection. W. W. Norton. [Google Scholar]
- Chang, E.-S., Kannoth, S., Levy, S., Wang, S.-Y., Lee, J. E., & Levy, B. R. (2020). Global reach of ageism on older persons’ health: A systematic review. PLoS One, 15(1), e0220857. doi: 10.1371/journal.pone.0220857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, S.-T. (2017). Self-Perception of aging and satisfaction with children’s support. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72(5), 782–791. doi: 10.1093/geronb/gbv113 [DOI] [PubMed] [Google Scholar]
- Cornwell, E. Y., & Waite, L. J. (2009a). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. doi: 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell, E. Y., & Waite, L. J. (2009b). Measuring social isolation among older adults using multiple indicators from the NSHAP study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 64(suppl_1), i38–i46. doi: 10.1093/geronb/gbp037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudjoe, T. K. M., Roth, D. L., Szanton, S. L., Wolff, J. L., Boyd, C. M., & Thorpe, R. J. (2020). The epidemiology of social isolation: National Health and Aging Trends Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 107–113. doi: 10.1093/geronb/gby037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg, L., McKee, K. J., Frank, A., & Naseer, M. (2021). A systematic review of longitudinal risk factors for loneliness in older adults. Aging & Mental Health, 0(0), 1–25. doi: 10.1080/13607863.2021.1876638 [DOI] [PubMed] [Google Scholar]
- DeWall, C. N., Twenge, J. M., Gitter, S. A., & Baumeister, R. F. (2009). It’s the thought that counts: The role of hostile cognition in shaping aggressive responses to social exclusion. Journal of Personality and Social Psychology, 96(1), 45–59. doi: 10.1037/a0013196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl, M., Wettstein, M., Spuling, S. M., & Wurm, S. (2021). Age-related change in self-perceptions of aging: Longitudinal trajectories and predictors of change. Psychology and Aging, 36(3), 344–359. doi: 10.1037/pag0000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGiuseppe, R., David, D., & Venezia, R. (2016). Cognitive theories. In Norcross J. C., VandenBos G. R., Freedheim D. K., & Olatunji B. O. (Eds.), APA handbook of clinical psychology: Theory and research, vol. 2 (pp. 145–182). American Psychological Association. doi: 10.1037/14773-006 [DOI] [Google Scholar]
- Dong, Y., & Peng, C.-Y. J. (2013). Principled missing data methods for researchers. SpringerPlus, 2, 222. doi: 10.1186/2193-1801-2-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozois, D. J. A., & Beck, A. T. (2008). Chapter 6—Cognitive schemas, beliefs and assumptions. In Dobson K. S. & Dozois D. J. A. (Eds.), Risk factors in depression (pp. 119–143). Elsevier. doi: 10.1016/B978-0-08-045078-0.00006-X [DOI] [Google Scholar]
- Duncan, T. E., & Duncan, S. C. (1995). Modeling the processes of development via latent variable growth curve methodology. Structural Equation Modeling: A Multidisciplinary Journal, 2(3), 187–213. doi: 10.1080/10705519509540009 [DOI] [Google Scholar]
- Evans, I. E. M., Martyr, A., Collins, R., Brayne, C., & Clare, L. (2019). Social isolation and cognitive function in later life: A systematic review and meta-analysis. Journal of Alzheimer’s Disease, 70(s1), S119–S144. doi: 10.3233/JAD-180501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fierloos, I. N., Tan, S. S., Williams, G., Alhambra-Borrás, T., Koppelaar, E., Bilajac, L., Verma, A., Markaki, A., Mattace-Raso, F., Vasiljev, V., Franse, C. B., & Raat, H. (2021). Socio-demographic characteristics associated with emotional and social loneliness among older adults. BMC Geriatrics, 21(1), 114. doi: 10.1186/s12877-021-02058-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 10(2), 227–237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hoyle, R. H., & Panter, A. T. (1995). Writing about structural equation models. In Hoyle R .A. (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 158–176). Sage Publications, Inc. [Google Scholar]
- Hu, R. X., Luo, M., Zhang, A., & Li, L. W. (2021). Associations of Ageism and Health: A Systematic Review of Quantitative Observational Studies. Research on Aging, 43(7–8), 311–322. doi: 10.1177/0164027520980130 [DOI] [PubMed] [Google Scholar]
- Kleinspehn-Ammerlahn, A., Kotter-Grühn, D., & Smith, J. (2008). Self-perceptions of aging: Do subjective age and satisfaction with aging change during old age? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(6), P377–P385. doi: 10.1093/geronb/63.6.P377 [DOI] [PubMed] [Google Scholar]
- Lee, J., & Cagle, J. G. (2017). Validating the 11-item revised University of California Los Angeles Scale to assess loneliness among older adults: An evaluation of factor structure and other measurement properties. The American Journal of Geriatric Psychiatry, 25(11), 1173–1183. doi: 10.1016/j.jagp.2017.06.004 [DOI] [PubMed] [Google Scholar]
- Levy, B. (2009). Stereotype embodiment: A psychosocial approach to Aging. Current Directions in Psychological Science, 18(6), 332–336. doi: 10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy, B. R. (2003). Mind matters: Cognitive and physical effects of aging self-stereotypes. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58(4), P203–P211. doi: 10.1093/geronb/58.4.P203 [DOI] [PubMed] [Google Scholar]
- Levy, B. R., Slade, M. D., & Kasl, S. V. (2002). Longitudinal benefit of positive self-perceptions of aging on functional health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57(5), P409–P417. doi: 10.1093/geronb/57.5.P409 [DOI] [PubMed] [Google Scholar]
- Liang, J., & Bollen, K. A. (1983). The structure of the Philadelphia Geriatric Center morale scale: A reinterpretation. Journals of Gerontology, 38(2), 181–189. doi: 10.1093/geronj/38.2.181 [DOI] [PubMed] [Google Scholar]
- Losada-Baltar, A., Martínez-Huertas, J. Á., Jiménez-Gonzalo, L., Pedroso-Chaparro, M., Gallego-Alberto, L., Fernandes-Pires, J., & Márquez-González, M. (2021). Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 77(4), 652–660. doi: 10.1093/geronb/gbab012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, Y., & Waite, L. J. (2014). Loneliness and mortality among older adults in China. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(4), 633–645. doi: 10.1093/geronb/gbu007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. Taylor & Francis Group/Lawrence Erlbaum Associates. [Google Scholar]
- Mehrabi, F., & Béland, F. (2020). Effects of social isolation, loneliness and frailty on health outcomes and their possible mediators and moderators in community-dwelling older adults: A scoping review. Archives of Gerontology and Geriatrics, 90, Article 104119. doi: 10.1016/j.archger.2020.104119 [DOI] [PubMed] [Google Scholar]
- Menkin, J. A., Robles, T. F., Gruenewald, T. L., Tanner, E. K., & Seeman, T. E. (2017). Positive expectations regarding aging linked to more new friends in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72(5), 771–781. doi: 10.1093/geronb/gbv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merchant, R. A., Liu, S. G., Lim, J. Y., Fu, X., & Chan, Y. H. (2020). Factors associated with social isolation in community-dwelling older adults: A cross-sectional study. Quality of Life Research, 29(9), 2375–2381. doi: 10.1007/s11136-020-02493-7 [DOI] [PubMed] [Google Scholar]
- Nagarajan, D., Lee, D. A., Robins, L. M., & Haines, T. P. (2020). Risk factors for social isolation in post-hospitalized older adults. Archives of Gerontology and Geriatrics, 88, Article 104036. doi: 10.1016/j.archger.2020.104036 [DOI] [PubMed] [Google Scholar]
- Perissinotto, C. M., Cenzer, I. S., & Covinsky, K. E. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14), 1078–1083. doi: 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikhartova, J., Bowling, A., & Victor, C. (2016). Is loneliness in later life a self-fulfilling prophecy? Aging & Mental Health, 20(5), 543–549. doi: 10.1080/13607863.2015.1023767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K. J., & Kelley, K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16(2), 93–115. doi: 10.1037/a0022658 [DOI] [PubMed] [Google Scholar]
- Robertson, D. A., King-Kallimanis, B. L., & Kenny, R. A. (2016). Negative perceptions of aging predict longitudinal decline in cognitive function. Psychology and Aging, 31(1), 71–81. doi: 10.1037/pag0000061 [DOI] [PubMed] [Google Scholar]
- Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., Meilstrup, C., Madsen, K. R., & Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet Public Health, 5(1), e62–e70. doi: 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- Schmitt, N. (1996). Uses and abuses of coefficient alpha. Psychological Assessment, 8(4), 350–353. doi: 10.1037/1040-3590.8.4.350 [DOI] [Google Scholar]
- Schwartz, E., Ayalon, L., & Huxhold, O. (2021). Exploring the reciprocal associations of perceptions of aging and social involvement. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(3), 563–573. doi: 10.1093/geronb/gbaa008 [DOI] [PubMed] [Google Scholar]
- Shiovitz-Ezra, S., Shemesh, J., & McDonnell/Naughton, M. (2018). Pathways from ageism to loneliness. In Ayalon L. & Tesch-Römer C. (Eds.), Contemporary perspectives on ageism (pp. 131–147). Springer International Publishing. doi: 10.1007/978-3-319-73820-8_9 [DOI] [Google Scholar]
- Smith, J., Ryan, L. H., Fisher, G. G., Sonnega, A., & Weir, D. R. (2017). HRS psychosocial and lifestyle questionnaire 2006–2016. Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Steverink, N., Westerhof, G. J., Bode, C., & Dittmann-Kohli, F. (2001). The personal experience of aging, individual resources, and subjective well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(6), P364–P373. doi: 10.1093/geronb/56.6.P364 [DOI] [PubMed] [Google Scholar]
- Tovel, H., Carmel, S., & Raveis, V. H. (2019). Relationships among self-perception of aging, physical functioning, and self-efficacy in late life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 74(2), 212–221. doi: 10.1093/geronb/gbx056 [DOI] [PubMed] [Google Scholar]
- Turvey, C. L., Wallace, R. B., & Herzog, R. (1999). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics, 11(2), 139–148. doi: 10.1017/s1041610299005694 [DOI] [PubMed] [Google Scholar]
- Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S., & Hanratty, B. (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart, 102(13), 1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerhof, G. J., Miche, M., Brothers, A. F., Barrett, A. E., Diehl, M., Montepare, J. M., Wahl, H.-W., & Wurm, S. (2014). The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychology and Aging, 29(4), 793–802. doi: 10.1037/a0038016 [DOI] [PubMed] [Google Scholar]
- Wurm, S., Warner, L. M., Ziegelmann, J. P., Wolff, J. K., & Schüz, B. (2013). How do negative self-perceptions of aging become a self-fulfilling prophecy? Psychology and Aging, 28(4), 1088–1097. doi: 10.1037/a0032845 [DOI] [PubMed] [Google Scholar]
- Yu, B., Steptoe, A., Chen, Y., & Jia, X. (2021). Social isolation, rather than loneliness, is associated with cognitive decline in older adults: The China Health and Retirement Longitudinal Study. Psychological Medicine, 51(14), 2414–2421. doi: 10.1017/S0033291720001014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.