Abstract
Objectives
This study investigates the association between childhood socioeconomic status (cSES) and risk of cognitive impairment in older adulthood, and whether the Five-Factor Model personality traits mediated this association.
Methods
A sample of 9,995 participants (mean age = 67.01 years) from the Health and Retirement Study were followed up every 2 years from 2006 to 2018. cSES was tested as a predictor of risk of dementia and risk of cognitive impairment not dementia (CIND). Personality was tested as a mediator of these associations. Models were adjusted for age, gender, ethnicity, race, education, and baseline year.
Results
Although effect sizes were modest, results indicated that lower cSES was associated with a higher risk of dementia (hazard ratio = 0.88 [0.775–0.985]). Higher cSES was also associated with higher conscientiousness and lower neuroticism. Conscientiousness and neuroticism each accounted for 7.9% of the total effect of cSES on dementia. Results were similar for CIND.
Discussion
Early childhood socioeconomic factors may contribute to cognitive impairment in older adulthood, an association mediated, in part, through adult personality traits.
Keywords: CIND, Conscientiousness, cSES, Dementia, Neuroticism, Older adults
Childhood socioeconomic status (cSES) is a multidimensional index of socioeconomic factors (e.g., living conditions associated with parental education, income, and occupation) that are associated with physical and mental health outcomes in adulthood (Luo & Waite, 2005). In particular, higher cSES is associated with cognition throughout adulthood (Lyu & Burr, 2016), including better language and executive function (Greenfield & Moorman, 2019). Ultimately, higher cSES is associated with a lower risk of cognitive impairment, from mild cognitive impairment (MCI) to dementia (Rogers et al., 2009; Zeki Al Hazzouri et al., 2011). Although adult SES also predicts long-term cognitive health, it does not always mitigate the long-term risks associated with low cSES (Luo & Waite, 2005; Lyu & Burr, 2016). Furthermore, SES at different points of the life span contributes independently to cognitive function in adulthood (Fors et al., 2009), indicating that cSES makes unique contributions to cognitive function distinct from adult SES indices, with long-term implications for maintaining cognitive function in older adulthood.
While cSES has been shown to predict cognitive function in late life, the mechanisms behind these associations are less clear. Many mechanisms have been proposed to explain the long-term association between cSES and cognition in older adulthood. For example, health behavior models focus on lifestyle factors related to cSES that contribute to long-term cognitive function, including exercise, alcohol consumption, smoking, and physical health (Norton et al., 2014). Biological models, in contrast, emphasize the interactions between cSES and biological factors, such as genes (e.g., APOE ε4 carrier status; see Moorman et al., 2018), that are associated with cognitive outcomes. Personality traits may be an additional mechanism that explains part of the relation between cSES and cognitive function in older adulthood.
The present research bridges life course theories and life-span theories of personality and health to examine personality traits as mediators between cSES and dementia risk. Many theories of the life course implicate the role of childhood factors in important outcomes in adulthood (Kuh et al., 2003; Willson et al., 2007). These models often specify a cumulative process, in which risk (protective) factors from early in life accumulate over time to contribute to worse (better) outcomes. In the context of cSES and cognition, this perspective predicts that higher cSES would be associated with better cognitive outcomes because the advantages of more economic resources in childhood increase at every stage of life. Chain of risk models further specify that intervening variables account for part of the relation between early-life factors and later outcomes and thus would explain why cSES is associated with cognitive outcomes (Chapman et al., 2010; Kuh et al., 2003; Lyu & Burr, 2016). Personality traits may be one intervening variable in this chain of risk for cSES and cognitive impairment.
Personality
Five-Factor Model (FFM; Costa & McCrae, 1995) personality traits are relatively consistent patterns of thoughts, behaviors, and emotions that have associations with cognition across the life span, including in older adulthood (Luchetti et al., 2016; Sutin et al., 2019). Neuroticism, defined as the tendency to be emotionally distressed, anxious, impulsive, and self-conscious, is associated with a higher risk of Alzheimer’s disease and related dementias (ADRD) in older adulthood, whereas conscientiousness, defined as the tendency to be orderly, disciplined, deliberate, and goal-oriented, is associated with lower ADRD risk (Aschwanden et al., 2021). Lower scores in openness, the tendency to be imaginative, aesthetic, novel, and open-minded; agreeableness, the tendency to be trusting, compliant, altruistic, and straightforward; and extraversion, the tendency to be gregarious, assertive, active, and positive, are also linked with cognitive impairment, although less consistently than neuroticism and conscientiousness (Aschwanden et al., 2021; Terracciano et al., 2014).
Life-span models of personality and health link these traits to long-term health outcomes (Friedman, 2019; Friedman & Martin, 2011; Kern et al., 2014; O’Súilleabháin et al., 2021). Personality traits are thought to shape the thinking, feeling, and behavior in everyday life that can contribute to health outcomes in older adulthood (Friedman & Martin, 2011; Kern et al., 2014). Individuals higher in conscientiousness, for example, tend to manage their stress better (Friedman & Martin, 2011), are less prone to depression (Friedman & Martin, 2011), engage in more physical activity (Sutin et al., 2016), and have better immunological regulation (O’Súilleabháin et al., 2021). Such patterns promote better health across the life span that is likely to culminate in a lower risk of cognitive impairment. And, indeed, a large body of literature suggests that personality is related to dementia risk (Aschwanden et al., 2021; Terracciano et al., 2014; Segerstrom, 2020). There is also evidence that personality traits are associated with key indicators of healthy cognitive aging. For example, higher conscientiousness is related to better cognitive performance on memory recall and verbal fluency tasks, whereas higher neuroticism is related to poorer cognitive performance on similar tasks (Luchetti et al., 2016; Sutin et al., 2019). Similar associations have been observed in childhood and adolescence (Guerin et al., 2003). Furthermore, these relations are also not entirely explained by sociodemographic factors or mental health status (Sutin et al., 2019). Although personality changes are observed in people with clinical dementia (Islam et al., 2019), such personality changes are not found in the preclinical phase, that is, before the onset of MCI or Alzheimer’s disease (AD) (Terracciano, An et al., 2017). Furthermore, personality measured in adolescence has been shown to predict cognitive function in middle adulthood (Sutin et al., 2021) and dementia risk in older adulthood (Chapman et al., 2020). This evidence indicates that the relation between personality and dementia risk is unlikely to be due to reverse causality (i.e., AD-induced personality changes in the preclinical stages), but rather personality is a risk factor for incident impairment. Personality may operate through predisposed and pathoplastic mechanisms that contribute directly or indirectly to dementia risk (Segerstrom, 2020). These pathways include inflammatory markers (Terracciano et al., 2014), health behaviors (Norton et al., 2014), and mental health status (Norton et al., 2014; Terracciano et al., 2014). The accumulation of these effects over time may shape the trajectory of cognitive aging. Some shared genetic factors may also explain part of the association between personality and dementia (Stephan et al., 2018).
cSES and Personality
In addition to the association between personality and cognitive aging and dementia risk, there is both theoretical and empirical evidence for the relation between cSES and personality in adulthood. Socioecological (e.g., the contextual–developmental framework; Chen & Schmidt, 2015) and gene–environment models (e.g., the differential life-span model; Briley & Tucker-Drob, 2017) accommodate the notion that SES factors in childhood affect individual differences in childhood temperament and adult personality development and shape long-term cognitive outcomes. Lower cSES may contribute to resource scarcity, instability, and trigger cognitive shifts toward short-term attention to meet immediate needs in childhood (Sheehy-Skeffington, 2020). These processes may consolidate into trait psychological functioning in adulthood (Sutin et al., 2017). From there, processes associated with some personality traits (e.g., conscientiousness, neuroticism) are likely to contribute to an increased risk of dementia.
Empirical evidence indicates that personality in adulthood is associated with a number of markers of cSES. For example, adult children of parents with higher educational attainment tend to score lower in neuroticism and higher in extraversion and openness (Sutin et al., 2017). Other evidence indicates that a composite marker of parental SES that included family income and parent education is associated with higher conscientiousness, openness, and extraversion and lower neuroticism in adulthood (Ayoub et al., 2018). Linking this process with late-life outcomes, Chapman et al. (2010) suggest that SES factors may account for only a marginal amount of personality-affiliated mortality outcomes, whereas personality traits may account for more SES-related mortality outcomes. Personality may be one long-term mechanism that explains, in part, how cSES predicts significant cognitive outcomes decades later.
Current Study
This study investigates whether personality is one pathway that links cSES to cognitive impairment in older adulthood. Specifically, we test whether cSES is associated with the risk of cognitive impairment not dementia (CIND) and dementia in older adulthood and test whether there is an indirect effect of this association through personality traits. We conducted mediated survival analyses using Cox proportional hazards (CPH) models to evaluate the FFM dimensions as a pathway between cSES and cognitive impairment. We focus primarily on conscientiousness and neuroticism because these traits are associated with cognitive outcomes in older adulthood (Aschwanden et al., 2021; Luchetti et al., 2016). We hypothesized that (a) lower cSES would be associated with a higher risk of developing CIND and dementia than higher cSES, and (b) higher neuroticism and lower conscientiousness would partially mediate the association between cSES and cognitive impairment. Directional hypotheses were not made for the remaining traits.
Method
Participants
Data for this study were from the Health and Retirement Study (HRS), a longitudinal study of American adults. Since 1992, participants have been assessed every 2 years on their health, behavior, cognition, socioeconomic history, and core demographic information. Participants were included in this sample if they completed the personality measures included in the 2006–2008 waves (baseline assessment), scored in the range of normal cognition at baseline, completed at least one follow-up cognitive assessment through the 2018 data collection wave, and were 50 years of age or older at baseline. HRS data are publicly available (http://hrsonline.isr.umich.edu), and all research protocols and informed consent have been approved by the University of Michigan Institutional Review Board. Participants with missing data for cSES and those who were younger than 50 years of age were excluded from the analytic sample. Following the exclusionary criteria, N = 9,995 participants had complete data for analysis.
Measures
Childhood socioeconomic status
A validated index of cSES, conceptualized and constructed by Vable et al. (2017), was derived from publicly available HRS data surveyed from 1992 to 2010 and was made available for public use in 2018 (https://hrsdata.isr.umich.edu/data-products/validated-measures-childhood-socio-economic-status). The cSES index consists of three scales that measure childhood financial capital (average financial resources, financial instability), childhood social capital (family structure, maternal investment), and childhood human capital (parental years of education). For the childhood financial capital measure, financial instability was reverse-coded and summed with financial resources. Higher scores on the cSES index reflect higher SES in childhood. The HRS cSES index has good internal consistency and is a more comprehensive marker of cSES than alternate indices and commonly used proxies like financial resources or parental education (Vable et al., 2017). Individuals with missing data on one or more components had their index scores averaged with the other remaining variables (Vable et al., 2017).
Personality
Personality was measured with the 26-item Midlife Development Inventory (MIDI; Lachman & Weaver, 1997). The MIDI is a validated measure of Big Five personality traits which is frequently used in large-scale, time-limited surveys (Lachman & Weaver, 1997; Zimprich et al., 2012). Items for neuroticism were “nervous,” “calm,” “moody,” and “worrying,” and items for conscientiousness were “organized,” “hardworking,” “thorough,” “responsible,” and “careless.” For extraversion, items included “outgoing,” “friendly,” “lively,” “active,” and “talkative.” Items for openness included “adventurous,” “creative,” “curious,” “imaginative,” “intelligent,” “sophisticated,” and “broadminded,” and items for agreeableness included “warm,” “softhearted,” “helpful,” “caring,” and “sympathetic.” Participants indicated whether each adjective described them (a) “A lot,” (b) “Some,” (c) “A little,” or (d) “Not at all.” Items were reverse-scored when necessary and the mean taken in the direction of the trait label (e.g., higher scores on neuroticism reflect being higher on this trait). The internal consistency for the five traits ranges from 0.67 for conscientiousness to 0.79 for openness (Smith et al., 2017).
Cognition
Cognitive status was assessed every 2 years using a modified version of the Telephone Interview for Cognitive Status (TICSm) assessment (Crimmins et al., 2011). The TICSm included three tasks: memory (immediate and delayed recall of 10 words; up to 20 points), serial 7s (count backwards from 100 by 7s; up to 5 points), and backwards counting from 20 (up to 2 points). All tasks were summed and combined to create a total score value out of a possible 27 points. Validated cutoffs were used to classify dementia (TICSm < 7), CIND (TICSm between 7 and 12), and normal cognition (TICSm > 12; Crimmins et al., 2011). The TICSm is a well-validated measure that has been used to track dementia trends over time (Langa et al., 2017) in many other studies of cognitive impairment and dementia risk (Barber & Stott, 2004; Terracciano, Stephan et al., 2017).
Time to event
Time to event was measured as the number of years from baseline until the incidence of cognitive impairment, measured every 2 years over a 12-year span. Incidence time for CIND was a time in years to first TICSm in the CIND range among participants who scored in the normal range at baseline; participants who developed dementia were excluded. Incidence time for dementia was years to dementia. Across all outcomes, time was censored at the last available assessment for participants who did not score in the impairment range.
Covariates
Sociodemographic covariates were age (in years), gender (0 = male, 1 = female), ethnicity (0 = not Hispanic, 1 = Hispanic), race (dummy-coded into two variables: 1 = African American/Black compared to 0 = White and 1 = otherwise identified compared to 0 = White), education, and baseline year (0 = 2006, 1 = 2008). Education was reported as total number of years of schooling, ranging from a scale of 0 (none) to 17 (17+ years).
Additional markers of health were also included and controlled for in follow-up models (Supplementary Tables 1 and 2). Health covariates included smoking (0 = no, 1 = yes), moderate to vigorous physical activity mean scores, and measures for anxiety and depressive symptoms from the HRS Psychosocial Questionnaire (Smith et al., 2017). Anxiety was measured using the five-item Beck Anxiety Inventory (Beck & Steer, 1990) on a scale of 1 (never) to 4 (most of the time). Depressive symptoms were the sum of yes/no responses to the eight-item Center for Epidemiological Studies—Depression scale (Radloff, 1977). Binary dummy codes were created for anxiety scores equal to or greater than 12 (0 = no, 1 = yes) and for depressive symptom scores greater than or equal to four (0 = no, 1 = yes).
Statistical Analyses
The relation between cSES and risk of cognitive impairment was tested via discrete-time proportional hazards analyses using maximum likelihood estimators and Monte Carlo integrations. Analyses consisted of two uncontrolled and controlled models (including sociodemographic covariates) for CPH models. Estimates for mediation effects on continuous survival time within CPH models were employed following a structural equation model framework (Asparouhov et al., 2006). Checks for normality indicated that distributions for cSES, conscientiousness, and neuroticism were within the limits of a normal distribution. Assessment of Schoenfeld residuals for personality revealed potential violations of the assumption of proportionality for conscientiousness with years to dementia (β = −0.155, p < .001) and for openness to experience with years to CIND (β = −0.052, p = .030). In accordance with the interaction method when a potential violation of assumption occurs (Allison, 2010), we included interaction terms for conscientiousness and years to dementia as a covariate for conscientiousness and for openness and years to CIND as a covariate for openness. A sensitivity test indicated that the violations were protective in both halves of the follow-up, meaning that the violations were mild and did not change the protective nature of the effects for either conscientiousness or openness. We also conducted a number of sensitivity analyses to test the robustness of the associations. First, to address whether the association was due to health-related behavior or mental health, we added smoking, physical activity, anxiety, and depressive symptoms to the model as additional covariates (Supplementary Tables 1 and 2). Second, to address whether the association was biased by the relatively younger (i.e., middle-aged) participants in the sample, we repeated the full pathway analyses with the same model specifications excluding participants younger than the age of 65 years at baseline (Supplementary Table 3). Third, because the HRS data set included spouses and thus the results may be biased by nonindependence, we again repeated the analysis excluding spouses of the target participants (Supplementary Table 4). Finally, to evaluate whether a specific component of cSES drove the association with the cognitive impairment outcomes or whether the associations were similar across components, we tested the individual subcomponents of the cSES index (Supplementary Table 5).
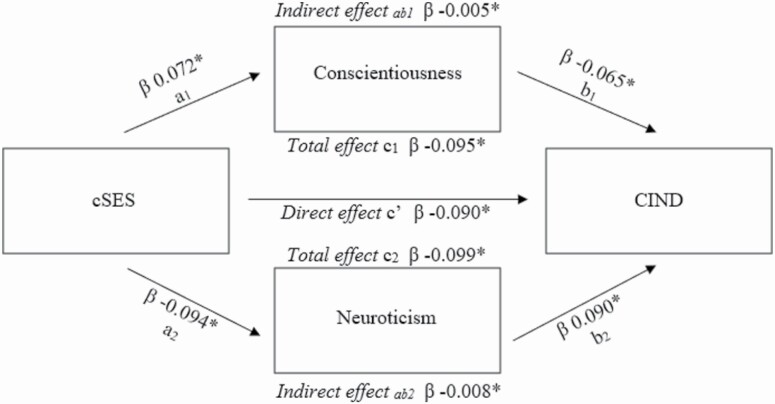
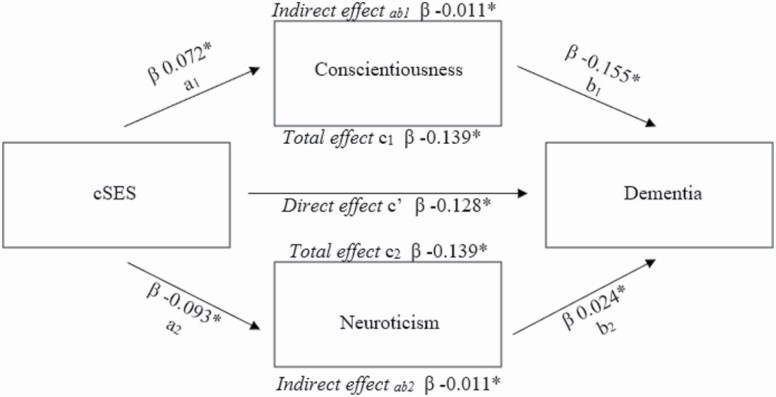
Baseline hazard parameters were treated as actual model parameters. cSES was standardized into a z-score and loaded as an independent predictor variable in the model, with CIND and dementia individually entered as dependent outcome variables over the 12-year follow-up period. Personality traits were standardized into z-scores and entered as mediators in the model to test for indirect and total effects (Figures 1 and 2). Analyses controlled for age, gender, race, ethnicity, years of education, and baseline year. Descriptive statistics for this study were completed using SPSS version 26. All remaining analyses were conducted using Mplus version 8.5 (Muthén & Muthén, 2017). The unstandardized coefficients were exponentiated to get hazard ratios (HRs). Significance was set to p < .05.
Figure 1.
Mediation model path diagram for cSES, CIND, and personality variables. Notes: c1 indicates the total effect pathway for conscientiousness. c2 indicates the total effect pathway for neuroticism. c′ indicates the direct effect pathway between cSES and CIND. Asterisks denote significant pathways. CIND = cognitive impairment not dementia; cSES = childhood socioeconomic status.
Figure 2.
Mediation model path diagram for cSES, dementia, and personality variables. Notes: c1 indicates the total effect pathway for conscientiousness. c2 indicates the total effect pathway for neuroticism. c′ indicates the direct effect pathway between cSES and dementia. Asterisks denote significant pathways. cSES = childhood socioeconomic status.
Results
Descriptive statistics for the overall sample and by cognitive outcome are given in Supplementary Table 1. Participants who developed cognitive impairment over the follow-up were older, had less education, and were more likely to be a race self-identified as other than White. Men were more likely to develop CIND over time; women were more likely to develop dementia. Participants classified with cognitive impairment (either CIND or dementia) were more likely to be from a lower cSES background than the group with normal cognition. Compared to participants in the normal cognitive function range, individuals who later developed CIND scored lower on conscientiousness and marginally higher on neuroticism. The dementia group was associated with higher neuroticism and lower conscientiousness compared to other groups.
CPH Analyses
Deviance statistics for model fit are given in Tables 1 and 2 (see also Supplementary Table 6). For all cognitive outcomes in all models, cSES and cognitive impairment were significantly associated with age, race, and education. Ethnicity was associated with cSES and gender was specifically related to CIND risk (Table 1 and Supplementary Table 6). In both controlled and uncontrolled models, lower cSES was associated with a higher risk of cognitive impairment. In the uncontrolled models, each 1 SD lower in cSES was associated with a 37.4% higher risk of CIND (HR = 0.728 [0.701–0.756], p < .001) and a 45.1% higher risk of dementia (HR = 0.689 [0.631–0.747], p < .001). When adjusted for sociodemographic covariates, the hazard was reduced to an 11% higher risk of CIND (HR = 0.901 [0.856–0.945], p < .001) and a 15.9% higher risk of dementia (HR = 0.863 [0.762–0.965], p = .014). When personality was added, the fully adjusted model further attenuated this effect: Each 1 SD less in cSES was associated with an overall 9.5% higher risk of CIND (HR = 0.914 [0.868–0.959], p < .001) and a 15.3% higher risk of dementia (HR = 0.880 [0.775–0.985], p = .035). cSES remained significant in all models. For the behavioral and mental health covariates, anxiety and physical activity were significantly associated with CIND and dementia in the fully adjusted models, and depressive symptoms were associated with CIND (Supplementary Table 2).
Table 1.
Proportional Hazards Models Predicting Risk in CIND
| Model 1 (uncontrolled) | Model 2 (controlled) | Model 3 (mediated) | |
|---|---|---|---|
| HR [95% CI], p | HR [95% CI], p | HR [95% CI], p | |
| cSES | 0.728 [0.701–0.756], <.001 | 0.901 [0.856–0.945], <.001 | 0.913 [0.867–0.959], <.001 |
| Age (years) | — | 1.067 [1.062–1.072], <.001 | 1.068 [1.063–1.073], <.001 |
| Gender | — | 0.834 [0.768–0.900], <.001 | 0.829 [0.763–0.896], .001 |
| Race: African American/Black | — | 2.210 [1.950–2.469], <.001 | 2.218 [1.951–2.484], <.001 |
| Race: Otherwise identified | — | 1.518 [1.202–1.834], <.001 | 1.507 [1.192–1.822], <.001 |
| Ethnicity | — | 1.126 [0.928–1.324], .19 | 1.116 [0.921–1.312], .22 |
| Education (years) | — | 0.893 [0.878–0.908], <.001 | 0.897 [0.881–0.912], <.001 |
| Year (baseline) | — | 0.952 [0.876–1.029], .23 | 0.965 [0.887–1.043], .38 |
| Conscientiousness | — | — | 0.935 [0.896–0.975], .002 |
| Neuroticism | — | — | 1.098 [1.052–1.144], <.001 |
| Openness | — | — | 0.997 [0.946–1.048], .91 |
| AIC | 23,819.354 | 18,517.066 | 18,341.905 |
| BIC | 23,826.508 | 18,572.837 | 18,425.510 |
Note: CIND = cognitive impairment not dementia; cSES = childhood socioeconomic status; HR = hazard ratio; AIC = Akaike information criterion; BIC = Bayesian information criterion. Values were bolded to denote significance and make it easier for readers to identify this.
Table 2.
Proportional Hazards Models Predicting Risk in Dementia
| Model 1 (uncontrolled) | Model 2 (controlled) | Model 3 (mediated) | |
|---|---|---|---|
| HR [95% CI], p | HR [95% CI], p | HR [95% CI], p | |
| cSES | 0.689 [0.631–0.747], <.001 | 0.863 [0.762–0.965], .014 | 0.867 [0.867–0.959], .018 |
| Age (years) | — | 1.101 [1.088–1.113], <.001 | 1.099 [1.063–1.073], <.001 |
| Gender | — | 1.064 [0.855–1.273], .54 | 1.063 [0.763–0.896], .55 |
| Race: African American/Black | — | 2.708 [2.030–3.386], <.001 | 2.710 [1.951–2.484], <.001 |
| Race: Otherwise identified | — | 1.651 [0.785–2.516], .06 | 1.542 [1.192–1.822], <.001 |
| Ethnicity | — | 1.126 [0.726–1.810], .19 | 1.223 [0.921–1.312], .36 |
| Education (years) | — | 0.910 [0.876–0.944], <.001 | 0.910 [0.881–0.912], <.001 |
| Year (baseline) | — | 0.799 [0.634–0.964], .033 | 0.807 [0.887–1.043], .041 |
| Conscientiousness | — | — | 0.816 [0.895–0.975], <.001 |
| Neuroticism | — | — | 1.134 [1.052–1.144], .017 |
| Openness | — | — | 1.134 [0.946–1.048], .025 |
| AIC | 6,464.925 | 4,721.823 | 4,663.123 |
| BIC | 6,472.135 | 4,778.007 | 4,747.347 |
Note: cSES = childhood socioeconomic status; HR = hazard ratio; AIC = Akaike information criterion; BIC = Bayesian information criterion. Values were bolded to denote significance and make it easier for readers to identify this.
Tests of Mediation
Tests of mediation were conducted to evaluate personality as a pathway between cSES and cognitive impairment. All indirect, direct, and total pathways were significant for conscientiousness and neuroticism (Table 3), and partial mediations were demonstrated with countervailing indirect effects (Figures 1 and 2). Specifically, there was a positive association between cSES and conscientiousness (i.e., higher cSES was associated with higher conscientiousness), followed by a negative association between conscientiousness and cognitive impairment (i.e., conscientiousness was protective against impairment). Conversely, negative associations were observed between cSES and neuroticism (i.e., lower cSES was associated with higher neuroticism) and positive effects between neuroticism and cognitive impairment (i.e., neuroticism was associated with increased risk of impairment). Conscientiousness mediated 5.3% of the total effect of cSES on CIND and 7.9% of the total effect on dementia. Neuroticism mediated 8.1% of the total effect of cSES on CIND and 7.9% of the total effect on dementia. Total effects that included conscientiousness and neuroticism were comparable with lower hazard risk and were stronger in magnitude than indirect and direct effects for CIND. Total effects for conscientiousness were associated with a 9% lower risk in CIND, while total effects for neuroticism contributed a 9.4% lower risk in CIND.
Table 3.
Controlled Mediation Models for cSES, Conscientiousness, and Neuroticism Predicting Cognitive Impairment
| CIND | Dementia | |||
|---|---|---|---|---|
| Conscientiousness | Neuroticism | Conscientiousness | Neuroticism | |
| β/HR [95% CI], p | β/HR [95% CI], p | β/HR [95% CI], p | β/HR [95% CI], p | |
| Indirect effecta,b | −0.005 [−0.08 to −0.001], .006 | −0.008 [−0.013 to −0.004], <.001 | −0.011 [−0.019 to −0.004], .003 | −0.011 [−0.021 to −0.001], .031 |
| Total effectb,c | −0.095 [−0.145 to −0.045], <.001 | −0.099 [−0.148 to −0.049], <.001 | −0.139 [−0.258 to −0.020], .022 | −0.139 [−0.258 to −0.020], .022 |
| Full indirect effectb,d | −0.013 [−0.018 to −0.008], <.001 | −0.022 [−0.034 to −0.011], <.001 | ||
| Direct effecte,f | 0.914 [0.868 to 0.959], <.001 | 0.880 [0.775 to 0.985], .035 | ||
| AIC | 84,604.555 | 70,735.452 | ||
| BIC | 84,878.449 | 71,016.330 |
Note: HR = hazard ratio; AIC = Akaike information criterion; BIC = Bayesian information criterion; CIND = cognitive impairment not dementia; cSES = childhood socioeconomic status. Values were bolded to denote significance and make it easier for readers to identify this.
aEffect of cSES on cognitive impairment through the indirect personality path.
bEstimate is presented.
cEffect of the indirect personality path and direct path of cSES on cognitive impairment.
dSum of the indirect paths.
eDirect effect of cSES on cognitive impairment.
fHR is presented.
The sensitivity analyses supported the results from the main analysis. First, the model that included the additional behavioral and mental health covariates indicated that the indirect effects of conscientiousness and neuroticism on the relation between cSES and CIND remained significant, the indirect effect of conscientiousness on dementia remained significant, but the indirect effect of neuroticism was reduced to nonsignificance for dementia. The direct effect of cSES on cognitive impairment remained significant (Supplementary Table 2). Second, consistent with previous findings (Terracciano, Stephan et al., 2017) excluding individuals younger than 65 at baseline, we found no differences between the older than 50 at baseline group and the older than 65 at baseline group for cSES pathways on CIND risk. For dementia, a similar association was found for both conscientiousness and neuroticism, but the latter pathway fell below the threshold for statistical significance, likely because of the reduced power (Supplementary Table 3). Third, the pattern of results was the same when spouses were excluded from the analysis, but the direct effect of cSES on dementia did not reach significance, again likely because of the reduction in power with the reduced sample size. Indirect effects for conscientiousness remained significant but indirect effects for neuroticism became insignificant for dementia risk (Supplementary Table 4). Finally, the sensitivity analysis for the components of cSES indicated that items related to human capital and financial capital significantly predicted cognitive impairment (Supplementary Table 5). The only significant item for social capital was family structure, which significantly predicted CIND risk.
No mediation effects were observed for extraversion or agreeableness, and openness did not significantly mediate the relation between cSES and dementia (Supplementary Tables 7–9). There was a partial mediation pathway for openness and CIND: countervailing effects showed positive associations between cSES and openness and negative associations between openness and CIND (Supplementary Figure 1). Openness mediated 4.8% of the total effect of cSES on CIND and was associated with a 10% lower risk in CIND.
Discussion
The present study investigated the association between cSES and risk of dementia in older adulthood and whether adult personality traits mediated this association. Survival analyses showed that higher cSES was protective against both CIND and dementia. Higher conscientiousness and lower neuroticism explained, in part, the lower risk of cognitive impairment associated with higher cSES: The socioeconomic environment during childhood was associated with personality traits in adulthood, which were associated with a lower risk of CIND and dementia. However, the indirect effect of cSES on dementia through neuroticism became nonsignificant when behavioral and mental health covariates were included in the model. Openness also partially mediated the association between cSES and CIND. There was no evidence of mediation for the other traits.
Our findings are comparable with contemporary literature that links higher SES in childhood with better cognitive outcomes in adulthood (Luo & Waite, 2005; Lyu & Burr, 2016) and supports similar research that has found a relation between cSES with cognitive impairment and dementia risk in the HRS (Rogers et al., 2009; Vable et al., 2018) and other longitudinal studies (Zeki Al Hazzouri et al., 2011). To explain the association between cSES and cognitive outcomes, a variety of mechanisms have been proposed, including adult SES and cognitive ability (Greenfield & Moorman, 2019; Luo & Waite, 2005; Lyu & Burr, 2016; Zeki Al Hazzouri et al., 2011), and gene × environmental interactions (Moorman et al., 2018).
Building on this literature, the present research suggests that adult personality traits are one mechanism through which early-life socioeconomic status is associated with cognitive outcomes in older adulthood. The association between cSES and personality in our study is consistent with associations found in related research: Lower cSES was associated with higher neuroticism and lower conscientiousness across the life span (Ayoub et al., 2018). It is important to note that higher neuroticism and lower conscientiousness can be adaptive in some contexts: Higher neuroticism can be “healthy” under the right conditions (Friedman, 2019), and lower conscientiousness may be beneficial in situations that require flexibility and creativity (Robert & Cheung, 2010). In other regards, however, these trait profiles inform biopsychosocial processes that contribute to stress sensitivity and maladaptive health behaviors compared to lower neuroticism and higher conscientiousness (Friedman & Martin, 2011). These profiles may be precursors to long-term outcomes like cognitive impairment. Lower conscientiousness and higher neuroticism are associated with greater disease burden (Kern et al., 2014) and behavioral patterns (e.g., physical inactivity; Sutin et al., 2016) that increase the risk of dementia. And, indeed, there is evidence from HRS and other studies that conscientiousness and neuroticism increase the risk of dementia (Aschwanden et al., 2021; Terracciano, Stephan et al., 2017; Terracciano et al., 2014). These findings suggest that cSES is associated with CIND and dementia in older adulthood, both directly and indirectly through neuroticism, conscientiousness, and openness.
Our findings have implications for cognitive health in older adulthood. Although SES factors are known to have a direct impact on physical, mental, and cognitive health across the life span (Luo & Waite, 2005), there are several options available that could minimize potential risks related to some personality traits and/or socioeconomic conditions in childhood. Education is widely recognized as one modifiable socioeconomic risk factor for offsetting dementia risk (Livingston et al., 2020). Even in midlife, targeted interventions for cognitive enrichment may help reduce cognitive decline and dementia risk (Hertzog et al., 2008). Similarly, it is possible that personality-informed interventions in adulthood could help mitigate cognitive impairment risk in adults from low cSES backgrounds and prolong healthy cognition in older adulthood. For example, a nonclinical digital intervention program was found to generate personality change in young adults (Stieger et al., 2021). Additional research is necessary to determine the full effect of personality mediators on the association between cSES and CIND and dementia risk in older adulthood.
Strengths and Limitations
This study has several strengths. It provides new information on how cSES contributes to cognitive impairment and utilizes a large sample of older adults using validated measures of cSES, personality, and cognitive impairment. The analyses used a longitudinal framework and mediated CPH analyses that are optimal for calculating nonlinear effects for hazard risk (i.e., event time) and can flexibly adjust for continuous variables like personality traits.
There are also some limitations. Analyses were restricted to cognition and personality assessments in adulthood, and data on childhood cognitive function and personality were not available. As such, limited inferences can be made about premorbid cognitive ability. Future research would benefit from the inclusion of childhood and adolescent measures of personality (and temperament), which are also important for developing life-span models through which cSES contributes to cognitive outcomes (Sutin et al., 2021). Additionally, the effect sizes were modest, and the mediation effect of neuroticism on cSES in the dementia model was reduced to nonsignificance when behavioral and mental health covariates were included. Neuroticism is a major risk factor for anxiety and depressive symptoms. Not surprisingly, the clinical symptoms accounted for some of the indirect effects of neuroticism on dementia. Furthermore, there was less statistical power for the dementia outcome because fewer participants developed dementia compared to CIND. Our models were also restricted to psychosocial factors and did not include biometric variables in the assessments. Future research may also want to address potential gene × environment interactions that may contribute to the associations observed in this study. Finally, CIND and dementia risk were based on cognitive test performance. While this approach is valid and similar associations have been reported for personality and dementia using this measure and clinical diagnostics (Crimmins et al., 2011; Langa et al., 2017), replication of these results using clinical diagnostic criteria for cognitive impairment would be beneficial.
Conclusions
The socioeconomic environment in which a child grows up is associated with cognitive impairment risk in older adulthood. The mechanisms that link cSES and cognitive impairment are likely to involve multiple factors. The present research contributes to this literature and highlights the role of two broad personality traits as psychosocial mechanisms that mediate the association between cSES and risk of cognitive impairment. Our study provides evidence that adult personality partially mediates the association between cSES and risk for cognitive impairment. Specifically, neuroticism mediates the association between cSES and CIND, and conscientiousness mediates the association between cSES and both CIND and dementia.
Supplementary Material
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The hypotheses and analyses reported in this study were not preregistered. The Mplus scripts used in this study are available from A. A. Sesker upon request.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health (R01AG053297 and R01AG068093). The Health and Retirement Study is sponsored by the National Institute on Aging (NIAU01AG009740) and is conducted by the University of Michigan.
Conflict of Interest
None declared.
Author Contributions
A. A. Sesker conceptualized the study. A. A. Sesker performed the statistical analyses, with assistance from P. S. O’Súilleabháin and A. R. Sutin. A. A. Sesker, P. S. O’Súilleabháin, and A. R. Sutin performed data interpretations. A. A. Sesker completed the initial manuscript draft with contributions from P. S. O’Súilleabháin and A. R. Sutin. J. H. Lee, D. Aschwanden, M. Luchetti, Y. Stephan, A. Terracciano, and A. R. Sutin provided critical revisions to the manuscript. All authors approved the final version of the manuscript for submission.
References
- Allison, P. D. (2010). Survival analysis using SAS: A practical guide. SAS Institute. [Google Scholar]
- Aschwanden, D., Strickhouser, J. E., Luchetti, M., Stephan, Y., Sutin, A. R., & Terracciano, A. (2021). Is personality associated with dementia risk? A meta-analytic investigation. Ageing Research Reviews, 67, 101269. doi: 10.1016/j.arr.2021.101269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov, T., Masyn, K., & Muthén, B. O. (2006, August). Continuous time survival in latent variable models. In: Proceedings of the Joint Statistical Meeting, Seattle, August 2006, ASA section on Biometrics, (pp. 180–187). http://www.statmodel.com/bmuthen/articles/Article_108.pdfxs. [Google Scholar]
- Ayoub, M., Gosling, S. D., Potter, J., Shanahan, M., & Roberts, B. W. (2018). The relations between parental socioeconomic status, personality, and life outcomes. Social Psychological and Personality Science, 9(3), 338–352. doi: 10.1177/1948550617707018 [DOI] [Google Scholar]
- Barber, M., & Stott, D. J. (2004). Validity of the Telephone Interview for Cognitive Status (TICS) in post-stroke subjects. International Journal of Geriatric Psychiatry, 19(1), 75–79. doi: 10.1002/gps.1041 [DOI] [PubMed] [Google Scholar]
- Beck, A. T., & Steer, R. A. (1990). Manual for the Beck Anxiety Inventory. Psychological Corporation. [Google Scholar]
- Briley, D. A., & Tucker-Drob, E. M. (2017). Comparing the developmental genetics of cognition and personality over the life span. Journal of Personality, 85(1), 51–64. doi: 10.1111/jopy.12186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman, B. P., Fiscella, K., Kawachi, I., & Duberstein, P. R. (2010). Personality, socioeconomic status, and all-cause mortality in the United States. American Journal of Epidemiology, 171(1), 83–92. doi: 10.1093/aje/kwp323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman, B. P., Huang, A., Peters, K., Horner, E., Manly, J., Bennett, D. A., & Lapham, S. (2020). Association between high school personality phenotype and dementia 54 years later in results from a national US sample. JAMA Psychiatry, 77(2), 148–154. doi: 10.1001/jamapsychiatry.2019.3120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, X., & Schmidt, L. A. (2015). Temperament and personality. In Lamb M. E. & Lerner R. M. (Eds.), Handbook of child psychology and developmental science: Socioemotional processes (pp. 152–200). John Wiley & Sons, Inc. doi: 10.1002/9781118963418.childpsy305 [DOI] [Google Scholar]
- Costa, P. T.Jr, & McCrae, R. R. (1995). Domains and facets: Hierarchical personality assessment using the revised NEO personality inventory. Journal of Personality Assessment, 64(1), 21–50. doi: 10.1207/s15327752jpa6401_2 [DOI] [PubMed] [Google Scholar]
- Crimmins, E. M., Kim, J. K., Langa, K. M., & Weir, D. R. (2011). Assessment of cognition using surveys and neuropsychological assessment: The Health and Retirement Study and the Aging, Demographics, and Memory Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(Suppl. 1), 162–171. doi: 10.1093/geronb/gbr048 [DOI] [Google Scholar]
- Fors, S., Lennartsson, C., & Lundberg, O. (2009). Childhood living conditions, socioeconomic position in adulthood, and cognition in later life: Exploring the associations. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(6), 750–757. doi: 10.1093/geronb/gbp029 [DOI] [Google Scholar]
- Friedman, H. S. (2019). Neuroticism and health as individuals age. Personality Disorders, 10(1), 25–32. doi: 10.1037/per0000274 [DOI] [PubMed] [Google Scholar]
- Friedman, H. S., & Martin, L. R. (2011). The longevity project: Surprising discoveries for health and long life from the landmark eight decade study. Hay House, Inc. [Google Scholar]
- Greenfield, E. A., & Moorman, S. M. (2019). Childhood socioeconomic status and later life cognition: Evidence from the Wisconsin Longitudinal Study. Journal of Aging and Health, 31(9), 1589–1615. doi: 10.1177/0898264318783489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerin, D. W., Gottfried, A. W., Oliver, P. H., & Thomas, C. W. (2003). Temperament: Infancy through adolescence—The Fullerton Longitudinal Study. Springer US. [Google Scholar]
- Hertzog, C., Kramer, A. F., Wilson, R. S., & Lindenberger, U. (2008). Enrichment effects on adult cognitive development: Can the functional capacity of older adults be preserved and enhanced? Psychological Science in the Public Interest, 9(1), 1–65. doi: 10.1111/j.1539-6053.2009.01034.x [DOI] [PubMed] [Google Scholar]
- Islam, M., Mazumder, M., Schwabe-Warf, D., Stephan, Y., Sutin, A. R., & Terracciano, A. (2019). Personality changes with dementia from the informant perspective: New data and meta-analysis. Journal of the American Medical Directors Association, 20(2), 131–137. doi: 10.1016/j.jamda.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern, M. L., Hampson, S. E., Goldberg, L. R., & Friedman, H. S. (2014). Integrating prospective longitudinal data: Modeling personality and health in the Terman Life Cycle and Hawaii Longitudinal Studies. Developmental Psychology, 50(5), 1390–1406. doi: 10.1037/a0030874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh, D., Ben-Shlomo, Y., Lynch, J., Hallqvist, J., & Power, C. (2003). Life course epidemiology. Journal of Epidemiology and Community Health, 57(10), 778–783. doi: 10.1136/jech.57.10.778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman, M. E., & Weaver, S. L. (1997). The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Brandeis University. [Google Scholar]
- Langa, K. M., Larson, E. B., Crimmins, E. M., Faul, J. D., Levine, D. A., Kabeto, M. U., & Weir, D. R. (2017). A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Internal Medicine, 177(1), 51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., & Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 Report of the Lancet Commission. Lancet (London, England), 396(10248), 413–446. doi: 10.1016/S0140-6736(20)30367-6 [DOI] [Google Scholar]
- Luchetti, M., Terracciano, A., Stephan, Y., & Sutin, A. R. (2016). Personality and cognitive decline in older adults: Data from a longitudinal sample and meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(4), 591–601. doi: 10.1093/geronb/gbu184 [DOI] [Google Scholar]
- Luo, Y., & Waite, L. J. (2005). The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60(2), S93–S101. doi: 10.1093/geronb/60.2.s93 [DOI] [Google Scholar]
- Lyu, J., & Burr, J. A. (2016). Socioeconomic status across the life course and cognitive function among older adults: An examination of the latency, pathways, and accumulation hypotheses. Journal of Aging and Health, 28(1), 40–67. doi: 10.1177/0898264315585504 [DOI] [PubMed] [Google Scholar]
- Moorman, S. M., Carr, K., & Greenfield, E. A. (2018). Childhood socioeconomic status and genetic risk for poorer cognition in later life. Social Science & Medicine (1982), 212, 219–226. doi: 10.1016/j.socscimed.2018.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K. & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K., & Brayne, C. (2014). Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. The Lancet. Neurology, 13(8), 788–794. doi: 10.1016/S1474-4422(14)70136-X [DOI] [PubMed] [Google Scholar]
- O’Súilleabháin, P. S., Turiano, N. A., Gerstorf, D., Luchetti, M., Gallagher, S., Sesker, A. A., Terracciano, A., & Sutin, A. R. (2021). Personality pathways to mortality: Interleukin-6 links conscientiousness to mortality risk. Brain, Behavior, and Immunity, 93, 238–244. doi: 10.1016/j.bbi.2021.01.032 [DOI] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Robert, C., & Cheung, Y. H. (2010). An examination of the relationship between conscientiousness and group performance on a creative task. Journal of Research in Personality, 44(2), 222–231. doi: 10.1016/j.jrp.2010.01.005 [DOI] [Google Scholar]
- Rogers, M. A., Plassman, B. L., Kabeto, M., Fisher, G. G., McArdle, J. J., Llewellyn, D. J., Potter, G. G., & Langa, K. M. (2009). Parental education and late-life dementia in the United States. Journal of Geriatric Psychiatry and Neurology, 22(1), 71–80. doi: 10.1177/0891988708328220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom, S. C. (2020). Personality and incident Alzheimer’s disease: Theory, evidence, and future directions. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(3), 513–521. doi: 10.1093/geronb/gby063 [DOI] [Google Scholar]
- Sheehy-Skeffington, J. (2020). The effects of low socioeconomic status on decision-making processes. Current Opinion in Psychology, 33, 183–188. doi: 10.1016/j.copsyc.2019.07.043 [DOI] [PubMed] [Google Scholar]
- Smith, J., Fisher, G., Ryan, L., Clarke, P., House, J., & Weir, D. (2017). Psychosocial and lifestyle questionnaire 2006–2016 Documentation Report Core Section LB. The HRS Psychosocial Working Group. [Google Scholar]
- Stephan, Y., Sutin, A. R., Luchetti, M., Caille, P., & Terracciano, A. (2018). Polygenic score for Alzheimer’s disease and cognition: The mediating role of personality. Journal of Psychiatric Research, 107, 110–113. doi: 10.1016/j.jpsychires.2018.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stieger, M., Flückiger, C., Rüegger, D., Kowatsch, T., Roberts, B. W., & Allemand, M. (2021). Changing personality traits with the help of a digital personality change intervention. Proceedings of the National Academy of Sciences, 118(8), e2017548118. doi: 10.1073/pnas.2017548118 [DOI] [Google Scholar]
- Sutin, A. R., Luchetti, M., Stephan, Y., Robins, R. W., & Terracciano, A. (2017). Parental educational attainment and adult offspring personality: An intergenerational life span approach to the origin of adult personality traits. Journal of Personality and Social Psychology, 113(1), 144–166. doi: 10.1037/pspp0000137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin, A. R., Stephan, Y., Luchetti, M., Artese, A., Oshio, A., & Terracciano, A. (2016). The five-factor model of personality and physical inactivity: A meta-analysis of 16 samples. Journal of Research in Personality, 63, 22–28. doi: 10.1016/j.jrp.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin, A. R., Stephan, Y., Luchetti, M., Aschwanden, D., Sesker, A. A., O’Súilleabháin, P. S., & Terracciano, A. (2021). Self-reported and mother-rated personality traits at age 16 are associated with cognitive function measured concurrently and 30 years later. Psychological Medicine, 1–11. doi: 10.1017/S0033291721000672 [DOI] [Google Scholar]
- Sutin, A. R., Stephan, Y., Luchetti, M., & Terracciano, A. (2019). Five-factor model personality traits and cognitive function in five domains in older adulthood. BMC Geriatrics, 19(1), 343. doi: 10.1186/s12877-019-1362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano, A., An, Y., Sutin, A. R., Thambisetty, M., & Resnick, S. M. (2017). Personality change in the preclinical phase of Alzheimer’s disease. JAMA Psychiatry, 74(12), 1259–1265. doi: 10.1001/jamapsychiatry.2017.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano, A., Stephan, Y., Luchetti, M., Albanese, E., & Sutin, A. R. (2017). Personality traits and risk of cognitive impairment and dementia. Journal of Psychiatric Research, 89, 22–27. doi: 10.1016/j.jpsychires.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano, A., Sutin, A. R., An, Y., O’Brien, R. J., Ferrucci, L., Zonderman, A. B., & Resnick, S. M. (2014). Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimer’s & Dementia, 10(2), 179–186. doi: 10.1016/j.jalz.2013.03.002 [DOI] [Google Scholar]
- Vable, A. M., Eng, C. W., Mayeda, E. R., Basu, S., Marden, J. R., Hamad, R., & Glymour, M. M. (2018). Mother’s education and late-life disparities in memory and dementia risk among US military veterans and non-veterans. Journal of Epidemiology and Community Health, 72(12), 1162–1167. doi: 10.1136/jech-2018-210771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vable, A. M., Gilsanz, P., Nguyen, T. T., Kawachi, I., & Glymour, M. M. (2017). Validation of a theoretically motivated approach to measuring childhood socioeconomic circumstances in the Health and Retirement Study. PLoS One, 12(10), e0185898. doi: 10.1371/journal.pone.0185898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson, A. E., Shuey, K. M., & Elder, G. H., Jr. (2007). Cumulative advantage processes as mechanisms of inequality in life course health. American Journal of Sociology, 112(6), 1886–1924. doi: 10.1086/512712 [DOI] [Google Scholar]
- Zeki Al Hazzouri, A., Haan, M. N., Kalbfleisch, J. D., Galea, S., Lisabeth, L. D., & Aiello, A. E. (2011). Life-course socioeconomic position and incidence of dementia and cognitive impairment without dementia in older Mexican Americans: Results from the Sacramento area Latino study on aging. American Journal of Epidemiology, 173(10), 1148–1158. doi: 10.1093/aje/kwq483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimprich, D., Allemand, M., & Lachman, M. E. (2012). Factorial structure and age-related psychometrics of the MIDUS personality adjective items across the life span. Psychological Assessment, 24(1), 173–186. doi: 10.1037/a0025265 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.