Abstract
Objectives
Morning stiffness (MS) is characteristic of RA and associates with markers of systemic and local inflammation in RA patients. In patients with arthralgia, MS is a cardinal symptom to recognize arthralgia at-risk for RA development [i.e. clinically suspect arthralgia (CSA)]. In CSA, MS is also assumed to reflect inflammation, but this has never been studied. Therefore we aimed to study whether MS in CSA patients is associated with systemic and subclinical joint inflammation.
Methods
A total of 575 patients presenting with CSA underwent laboratory investigations and contrast-enhanced 1.5 T MRI of the hand and forefoot (scored according to the Rheumatoid Arthritis MRI Score method). Associations of MS (duration ≥60 min) with the presence of subclinical joint inflammation (synovitis, tenosynovitis and osteitis) and increased CRP (≥5 mg/l) were determined with logistic regression. Additionally, the effect of MS duration (≥30, ≥60 and ≥120 min) was studied.
Results
A total of 195 (34%) CSA patients experienced MS. These patients more often had subclinical synovitis [34% vs 21%; odds ratio (OR) 1.95 (95% CI 1.32, 2.87)], subclinical tenosynovitis [36% vs 26%; OR 1.59 (95% CI 1.10, 2.31)] and increased CRP [31% vs 19%; OR 1.93 (95% CI 1.30, 2.88)] than patients without MS. In multivariable analyses, subclinical synovitis [OR 1.77 (95% CI 1.16, 2.69)] and CRP [OR 1.78 (95% CI 1.17–2.69)] remained independently associated with MS. In CSA patients who later developed RA, and thus in retrospect were ‘pre-RA’ at the time of CSA, MS was more strongly associated with subclinical synovitis [OR 2.56 (95% CI 1.04, 6.52)] and CRP [OR 3.86 (95% CI 1.45, 10.24)]. Furthermore, associations increased with longer MS durations.
Conclusion
Inflammation associates with MS in the CSA phase that preceded clinical arthritis. These results increase our understanding of MS when assessing arthralgia in clinical practice.
Keywords: morning stiffness, clinically suspected arthralgia, inflammation, MRI, rheumatoid arthritis
Rheumatology key messages.
In arthralgia patients, morning stiffness is a cardinal symptom to recognize patients at risk for RA development.
Until now, it was unknown if morning stiffness in arthralgia patients also associates with inflammation.
This study showed that in the arthralgia phase preceding arthritis development, morning stiffness already reflects systemic and subclinical joint inflammation.
Introduction
Morning stiffness (MS) is a hallmark of RA. Until the past decade it was included in the classification criteria for RA and is still a pivotal symptom for diagnosis [1, 2]. In patients without clinical arthritis but with arthralgia, MS is a cardinal symptom to clinically recognize arthralgia patients who are at increased risk to develop RA [i.e. clinically suspect arthralgia (CSA)]. This is also reflected by its inclusion in the EULAR definition of arthralgia suspicious for progression to RA [3].
MS is generally considered as a sign of inflammation. Indeed, in established RA and early arthritis, MS has been shown to associate with local joint inflammation as well as disease activity and markers of systemic inflammation, such as acute phase reactants (e.g. CRP) and cytokines (e.g. IFN-γ, TNF-α and IL-6) [2, 4–6]. Although it is presumed that MS in arthralgia is also related to inflammation, this has never been studied.
We therefore hypothesized that in patients with CSA, MS is associated with local subclinical inflammation and systemic inflammation. To investigate this, we studied the association of MS with MRI-detected subclinical synovitis, tenosynovitis, osteitis and CRP using data from >500 CSA patients.
Methods
Patient population
We studied 575 consecutive CSA patients who were included in the Leiden CSA cohort between April 2012 and February 2019 (Supplementary Fig. S1 and Table S1, available at Rheumatology online). This is a population-based inception cohort of patients with recent-onset (<1 year) small-joint arthralgia that is suspected for progression to RA according to the treating rheumatologist based on clinical expertise and pattern recognition. Per the definition, patients were not included in the cohort when arthritis was detected upon physical examination or when a different explanation for the joint pain (e.g. osteoarthritis, fibromyalgia) was more likely than imminent RA, as both conditions preclude the presence of CSA. At inclusion, questionnaires were completed, laboratory investigations were done and an MRI scan was performed. CSA patients were followed for 2 years for the development of clinical arthritis (determined at physical joint examination by the treating rheumatologist). During follow-up, treatment with DMARDs (including steroids) was not allowed. Only after a patient developed arthritis and thus had left the CSA cohort, could DMARD therapy be initiated. The study population is further described in the Supplementary section S1 and elsewhere (available at Rheumatology online) [7].
This study was carried out in compliance with the Helsinki Declaration and all participating patients provided written informed consent. The study was approved by the medical ethical committee of the Leiden University Medical Centre (B19.008).
MS
At inclusion, the duration of MS was assessed by asking the patient about the presence of MS [Are your joints stiff in the morning? (yes/no)] and the duration of MS (How long does it take until your MS improves?). Patients could choose from the following categories: none, 1–29 min, 30–59 min, 60–119 min, 120–239 min or ≥240 min. The primary outcome in the current study was the dichotomized duration of MS into ≥60 min or <60 min [3]. Patients without MS (0 min) were included in the category of patients with <60 min of MS.
CRP
Baseline CRP levels were measured and dichotomized into increased (≥5 mg/l) or normal (<5 mg/l). This cut-off equals the reference value as used by the Leiden University Medical Centre and is based on an international standard work [8].
Subclinical joint inflammation
A gadolinium-enhanced MRI of the MCP, wrist and MTP joints of the most painful side, or the dominant side in case of symmetrically severe symptoms, was performed between 0800 and 1600 h. Patients were asked not to use NSAIDs 24 h prior to the MRI. The MRI protocol can be found in the Supplementary section S1 (available at Rheumatology online).
MRIs were evaluated for osteitis, synovitis and tenosynovitis according to the OMERACT Rheumatoid Arthritis MRI Score [9] and for tenosynovitis as described by Haavardsholm et al. [10]. Two independent trained readers scored the MRIs, blinded to the clinical data. Average scores of the two readers were dichotomized into the presence or absence of an inflammatory feature: a feature was considered present when scored by both readers and present at the same location in <5% of age-matched healthy volunteers. This cut-off was based on a previous study by Mangnus et al. [11] that investigated the prevalence of MRI-detected inflammation in 196 healthy controls. Mangnus et al. developed age-matched and location-specific reference values based on this symptom-free population. The use of this reference was shown to reduce false-positive MRI results compared with using no reference of normality [12]. The presence of any subclinical inflammation was defined as the presence of one or more inflammatory features (osteitis, synovitis or tenosynovitis). The number of locations with subclinical inflammation was assessed as a measure of the severity of subclinical inflammation. This was calculated as the sum of bones, joints and tendons with an inflammatory feature present (corrected for findings in healthy individuals as described above).
RA development
Patients were followed for the development of RA, which was defined a clinical diagnosis of RA and fulfilling either the 1987 or 2010 criteria for RA [1, 13] or starting with DMARD treatment. The 1987 criteria were used in addition to 2010 criteria, as autoantibody-negative patients have difficulties fulfilling the 2010 criteria because >10 involved joints are required [14]. The start of DMARD treatment was used as well to capture patients with a clinical RA diagnosis in whom fulfilment of classification criteria was prevented by early treatment initiation.
Statistical analysis
Associations between MS and local subclinical and systemic inflammation were tested with univariable and multivariable logistic regression with and without adjustment for age and gender. The explained variance of the multivariable model was assessed by Nagelkerke’s R2. The association between MS and the number of locations with inflammatory features was analysed with logistic regression. Additionally, the effect of MS duration(≥30, ≥60, ≥120 min) was studied. Furthermore, analyses were repeated in the subgroup of patients who progressed to RA during follow-up. The univariable association of MS for the development of RA was tested using Cox regression. Patients were censored at the time of their last visit. Data on the development of RA were all-encompassing, since our outpatient clinic is the only referral centre in a healthcare region of ∼400 000 inhabitants and patients (especially those participating in clinical studies) have very easy access to our outpatient clinic. In addition, we questioned if there was a mediating role of MS on the association of CRP or MRI-detected subclinical inflammation and RA development. This analysis is described in detail in Supplementary section S2 (available at Rheumatology online). SPSS version 25 was used (IBM, Armonk, NY, USA) and P-values <0.05 were considered significant.
Results
Associations of inflammation with MS
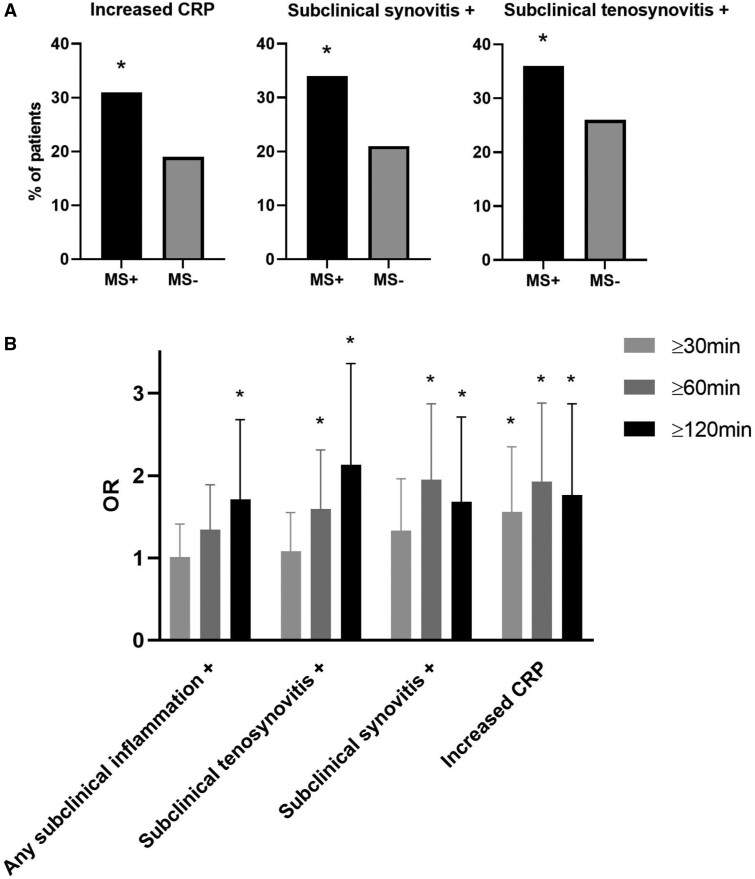
The mean age of the study population was 44 years (s.d. 13), 439 patients (76%) were female, the median 68-joint tender joint count was 5 (interquartile range 2–10) and 79 (14%) patients were ACPA positive (Supplementary Table S2, available at Rheumatology online). MS was present in 195 CSA patients (34%). These patients more often had subclinical synovitis, subclinical tenosynovitis and increased CRP compared with patients without MS (Fig. 1A, Table 1).
Fig. 1.
Inflammatory measures in CSA patients (A) with and without MS and (B) associations for different MS cut-offs
CRP: CRP increased if ≥5 mg/l; MS+: presence of MS with a duration ≥60 min; +: presence of an MRI feature.
Any subclinical inflammation: presence of one or more inflammatory features (osteitis, synovitis and tenosynovitis).
*Statistically significant associations (CI not including 1). (A) Increased CRP levels were more often found in CSA patients with MS (31% vs 19%). Likewise, subclinical synovitis was more often present in CSA patients with MS compared with patients without MS (34% vs 21%). Also, subclinical tenosynovitis was more frequently present in patients with MS (36% vs 26%). (B) Evaluating the univariable association for different MS durations (≥30, ≥60, ≥120 min) showed a ‘dose–response’ relation, with a step-wise increase for the OR for any subclinical MRI inflammation and subclinical tenosynovitis. For subclinical synovitis and CRP, an increase for ≥60 min compared with ≥30 min was observed, but no further increase for ≥120 min. Vertical error bars represent the 95% CI.
Table 1.
MS and inflammatory measures within the CSA cohort and patients who progressed to RA
| Measures | Complete cohort (n = 575), OR (95% CI) | RA subgroup (n = 76), OR (95% CI) |
|---|---|---|
| Univariable | ||
| Increased CRP | 1.93 (1.30, 2.88) | 3.86 (1.45, 10.24) |
| Any subclinical inflammationa | 1.34 (0.95, 1.89) | 5.00 (0.99, 24.41) |
| Subclinical synovitisa | 1.95 (1.32, 2.87) | 2.56 (1.04, 6.52) |
| Subclinical tenosynovitisa | 1.59 (1.10, 2.31) | 3.09 (0.99, 9.60) |
| Subclinical osteitisa | 1.14 (0.76, 1.72) | 1.50 (0.59, 3.84) |
| Multivariableb | ||
| Increased CRP | 1.78 (1.17, 2.69) | 3.24 (1.13, 9.25) |
| Subclinical synovitisa | 1.77 (1.16, 2.69) | 2.07 (0.73, 5.87) |
| Subclinical tenosynovitisa | 1.13 (0.75, 1.72) | 1.47 (0.40, 5.49) |
| Multivariablec | ||
| Increased CRP | 1.79 (1.18, 2.72) | 10.57 (2.27, 49.17) |
| Subclinical synovitisa | 1.69 (1.10, 2.58) | 1.63 (0.52, 5.09) |
| Subclinical tenosynovitisa | 1.23 (0.80, 1.91) | 1.76 (0.42, 7.35) |
Increased CRP: CRP increased if ≥5 mg/l.
Presence of an MRI feature.
Independent variables: increased CRP, subclinical synovitis and subclinical tenosynovitis.
Independent variables: increased CRP, subclinical synovitis, subclinical tenosynovitis, age and gender.
Multivariable analysis including these three inflammatory features revealed that subclinical synovitis [odds ratio (OR) 1.78 (95% CI 1.17, 2.69)] and increased CRP [OR 1.77 (95% CI 1.16, 2.69)] were independently associated with MS. The explained variance of the multivariable model was 5% (Fig. 1A, Table 1). Results remained similar after also adjusting for age and gender (Table 1).
We then studied the number of locations with inflammatory features as a marker of the severity of subclinical inflammation. This showed that an increase in severity was associated with higher odds of having MS [OR 1.06 (95% CI 1.00, 1.20) per increase in location with subclinical inflammation].
Assessment of MS duration
Evaluating the association of different MS durations (≥30, ≥60, ≥120 min), a dose–response relation was found, as analyses showed a step-wise increase in effect sizes for subclinical tenosynovitis and any subclinical MRI inflammation in relation to MS. The effect sizes of subclinical synovitis and CRP increased for MS ≥60 min compared with ≥30 min but did not increase further for MS ≥120 min. In line with the dose–response relation, associations with MRI inflammation were not significant for the 30 min outcome (Fig. 1B). The finding that only tenosynovitis was statistically significant in the multivariable analysis for 120 min is not completely consistent with the dose–response trend, but may be due to lower statistical power for this less frequent outcome (Supplementary Table S3, available at Rheumatology online).
MS and the development of RA
During a median follow-up of 773 days, 76 participants progressed to RA (31 patients fulfilled both the 1987 and 2010 RA criteria, 25 patients fulfilled the 2010 criteria, 8 patients fulfilled the 1987 criteria and 12 patients were prescribed DMARD therapy while not yet fulfilling the 1987 or 2010 criteria). CSA patients with MS (duration ≥60 min) more often progressed to RA (hazard ratio 1.56 (95% CI 0.99, 2.45)]. It should be noted that MS did not predict the onset of RA independent of CRP or MRI-detected subclinical inflammation (i.e. after adjusting for these variables in the Cox model). This is consistent with the associations between MS and inflammation. A mediating role of MS in the path of inflammation and RA development was not found (Supplementary section S2 and Table S4, available at Rheumatology online).
Analyses of MS and the inflammatory measures were repeated in patients who developed RA and thus, in retrospect, were truly ‘pre-RA’ when presenting with arthralgia (Supplementary Table S5, available at Rheumatology online). We hypothesized that associations in this subgroup would be stronger. Indeed, somewhat higher ORs were observed, although statistical significance was lost in some associations due to decreased power. The explained variance of the multivariable model in this subgroup increased to 18%, which was 5% in all CSA patients (Table 1).
Discussion
Inquiring about MS is standard practice in the clinical appraisal of arthralgia patients. In patients with clinical arthritis, MS is a known hallmark of RA that associates with inflammation, both local and systemic [2, 4–6]. In the differential diagnosis of patients with arthralgia, MS is a key factor for considering patients as having CSA or inflammatory-type arthralgia [3]. However, so far it was unknown whether MS in this phase also reflected inflammation. This prompted us to perform the current study. We observed that MS did associate with both subclinical joint inflammation detected on MRI and acute phase reactants. In addition, patients with more subclinical inflammation more often had MS. With respect to subclinical joint inflammation, the association was strongest for subclinical synovitis. These results suggest that inflammation does contribute to MS already in the phase that precedes clinical arthritis.
Our finding that MS associates with local subclinical inflammation in CSA patients is in line with previous ultrasound and MRI studies in early arthritis and RA patients. Previous studies in RA reported that MS was independently associated with both synovitis and tenosynovitis [4, 5]. In the setting with less inflammation than in RA, only subclinical synovitis was independently associated with MS. The involvement of synovial tissue in MS is in line with a recent histological study in 176 RA patients showing that MS may be related to impaired fibrinolysis of neutrophil-enmeshed fibrin deposits along the synovial membrane [15].
This study has some limitations. Although we focussed on the duration of MS, which is the most frequently used measure to define MS, a uniform definition of MS does not exist [16]. Reassuringly, the observed dose–response relationship for the duration of MS and inflammation supports the robustness of this outcome. Interestingly, there appears to be a ceiling to the dose–response effect for synovitis and CRP, while this was not observed for tenosynovitis. Nevertheless, for the associations found, the explained variance was relatively small. This may indicate that the inflammatory measures studied here were incomplete proxies for inflammation. In particular, CRP may have been an insufficient reflection of underlying systemic inflammation. It is known that many cytokines with distinct circadian rhythms (e.g. IFN-γ, TNF-α and IL-6) are increased in RA, yet these were not measured in the current study [2]. Future research could confirm the relationship between MS and systemic inflammation in CSA by measuring pro-inflammatory cytokines, ideally in 24 h levels. Alternatively, the small explained variance may suggest that factors other than inflammation are important.
Finally, analyses were conducted within a selection of arthralgia patients who were identified as having an increased risk of RA, namely CSA, and in whom MS may have contributed to this identification. In this selected group we observed an association of MS with RA development. In clinical practice, MS is also used to differentiate CSA from other arthralgia patients. In our study, patients were selected based on clinical symptoms reflecting the ‘inflammatory nature’ of the arthralgia. Therefore some selection on the presence of subclinical inflammation may have occurred, resulting in a higher prevalence of subclinical inflammation than in a more unselected arthralgia population. Consequently there may be a reduction in variation in MS and subclinical inflammation, possibly resulting in lower effect sizes, compared with a more unselected arthralgia population. The association of MS with RA development may therefore be stronger in a more unselected arthralgia population. This is also a subject for further research.
A strength of the current study is its relatively large sample size and the use of MRI to sensitively detect subclinical inflammation. The used measures of local inflammation (i.e. subclinical MRI inflammation) and systemic inflammation (i.e. CRP) are known to remain stable during the day, minimizing interference with the timing of these investigations and their relationship with MS [17, 18].
In conclusion, MS precedes the development of RA in patients with CSA and is associated with subclinical synovitis and increased CRP levels. This confirms the clinical assumption that MS reflects inflammation in the phase that precedes clinical arthritis. These results increase our understanding of MS when used in the clinical assessment of arthralgia.
Supplementary Material
Acknowledgements
All authors were involved in drafting the article or revising it critically. D.I.K., F.W., E.v.M. and A.H.M.v.d.H.-v.M. were responsible for study conception and design. D.I.K. and F.W. were responsible for the acquisition of data. D.I.K. E.v.M. and A.H.M.v.d.H.-v.M. were responsible for the analysis and interpretation of data.
Funding: This work was supported by the European Research Council under the European Union’s Horizon 2020 Research and Innovation Programme (agreement 714312) and the Dutch Arthritis Society.
Disclosure statement: The authors have declared no conflicts of interest.
Data availability statement
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Supplementary data
Supplementary data are available at Rheumatology online.
References
- 1. Arnett FC, Edworthy SM, Bloch DA. et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. [DOI] [PubMed] [Google Scholar]
- 2. Sierakowski S, Cutolo M.. Morning symptoms in rheumatoid arthritis: a defining characteristic and marker of active disease. Scand J Rheumatol Suppl 2011;125:1–5. [DOI] [PubMed] [Google Scholar]
- 3. van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJ. et al. EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Ann Rheum Dis 2017;76:491–6. [DOI] [PubMed] [Google Scholar]
- 4. Bellis E, Scirè CA, Carrara G. et al. Ultrasound-detected tenosynovitis independently associates with patient-reported flare in patients with rheumatoid arthritis in clinical remission: results from the observational study STARTER of the Italian Society for Rheumatology. Rheumatology (Oxford) 2016;55:1826–36. [DOI] [PubMed] [Google Scholar]
- 5. Boer AC, Boeters DM, Niemantsverdriet E, van der Helm-van Mil A.. Contribution of tenosynovitis of small joints to the symptom morning stiffness in patients presenting with undifferentiated and rheumatoid arthritis. Scand J Rheumatol 2020;49:181–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boers M, Buttgereit F, Saag K. et al. What is the relationship between morning symptoms and measures of disease activity in patients with rheumatoid arthritis? Arthritis Care Res 2015;67:1202–9. [DOI] [PubMed] [Google Scholar]
- 7. van Steenbergen HW, Mangnus L, Reijnierse M, Huizinga TW, van der Helm-van Mil AH.. Clinical factors, anticitrullinated peptide antibodies and MRI-detected subclinical inflammation in relation to progression from clinically suspect arthralgia to arthritis. Ann Rheum Dis 2016;75:1824–30. [DOI] [PubMed] [Google Scholar]
- 8. Burtis CA, Ashwood ER, Bruns DE, eds. Tietz textbook of clinical chemistry and molecular diagnostics, 5th ed.St. Louis, MO: Elsevier, 2012. [Google Scholar]
- 9. Ostergaard M, Edmonds J, McQueen F. et al. An introduction to the EULAR-OMERACT rheumatoid arthritis MRI reference image atlas. Ann Rheum Dis 2005;64(Suppl 1):i3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haavardsholm EA, Ostergaard M, Ejbjerg BJ, Kvan NP, Kvien TK.. Introduction of a novel magnetic resonance imaging tenosynovitis score for rheumatoid arthritis: reliability in a multireader longitudinal study. Ann Rheum Dis 2007;66:1216–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mangnus L, van Steenbergen HW, Reijnierse M, van der Helm-van Mil AH.. Magnetic resonance imaging-detected features of inflammation and erosions in symptom-free persons from the general population. Arthritis Rheumatol 2016;68:2593–602. [DOI] [PubMed] [Google Scholar]
- 12. Boer AC, Burgers LE, Mangnus L. et al. Using a reference when defining an abnormal MRI reduces false-positive MRI results-a longitudinal study in two cohorts at risk for rheumatoid arthritis. Rheumatology (Oxford) 2017;56:1700–6. [DOI] [PubMed] [Google Scholar]
- 13. Aletaha D, Neogi T, Silman AJ. et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 2010;69:1580–8. [DOI] [PubMed] [Google Scholar]
- 14. Boeters DM, Gaujoux-Viala C, Constantin A, van der Helm-van Mil AHM.. The 2010 ACR/EULAR criteria are not sufficiently accurate in the early identification of autoantibody-negative rheumatoid arthritis: results from the Leiden-EAC and ESPOIR cohorts. Semin Arthritis Rheum 2017;47:170–4. [DOI] [PubMed] [Google Scholar]
- 15. Orange DE, Blachere NE, DiCarlo EF. et al. Rheumatoid arthritis morning stiffness is associated with synovial fibrin and neutrophils. Arthritis Rheumatol 2020;72:557–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Halls S, Sinnathurai P, Hewlett S. et al. Stiffness is the cardinal symptom of inflammatory musculoskeletal diseases, yet still variably measured: report from the OMERACT 2016 Stiffness Special Interest Group. J Rheumatol 2017;44:1904–10. [DOI] [PubMed] [Google Scholar]
- 17. Sproston NR, Ashworth JJ.. Role of C-reactive protein at sites of inflammation and infection. Front Immunol 2018;9:754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hug C, Huber H, Terrier F. et al. Detection of flexor tenosynovitis by magnetic resonance imaging: its relationship to diurnal variation of symptoms. J Rheumatol 1991;18:1055–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analysed during the current study are available from the corresponding author on reasonable request.