Abstract
Objective
The objective of the study was to translate the revised dyadic adjustment scale into Chinese and evaluate its psychometric properties in gynaecological cancer patients and their male partners.
Methods
A cross-sectional design with a random subsample re-tested at the one-week interval was adopted. Gynaecological cancer patients and their partners were asked to complete the Chinese version of the revised dyadic adjustment and quality of marriage index. Internal consistency, test-retest reliability, convergent validity, structural validity and known-group validity was assessed.
Results
A total of 252 participants (i.e., 126 female patients and 126 male partners) were recruited. The Chinese version of the Revised Dyadic Adjustment showed good internal consistency (Cronbach's α = 0.85), test–retest reliability (r = 0.88), known group validity and adequate convergent validity with a significant positive correlation (r = 0.60) with the Quality of Marriage Index. Confirmatory factor analysis indicated an acceptable model fit to a second-order three-factor structure (GFI = 0.913, RMR = 0.046, CFI = 0.932).
Conclusions
The Chinese version of revised dyadic adjustment demonstrated good reliability and acceptable validity in gynaecological cancer patients and male partners. The scale can be used to assess the effectiveness of clinical nursing services for couples on their relationship and to compare marital satisfaction and adjustment between China and other parts of the world.
Keywords: Chinese, Gynaecological cancer, Marital satisfaction, Psychometric evaluation, Revised Dyadic Adjustment Scale, Validation
Introduction
In 2020, China accounted for the highest number of gynaecological cancer (GC) new cases (252,010) in the world.1 Intimate relationship is often challenged when the woman is diagnosed with GC.2,3 Surgery and adjuvant treatment of GC can cause sexual difficulties in up to 90% of patients, affecting intimate relationship and health status of GC patients.4
Intimate relationships are a major source of social support in couples that affects the quality of life.5 Patients' chronic illnesses not only affect themselves but also their health and relationship with their intimate partners.6 It is known that women's sexual dysfunction adversely affects their relationship with their partners7,8 and increase arguments and marital discord, which further increases concern about possible separation or divorce.9,10 GC patients who attempted sexual relations after treatment, most experienced significant levels of discomfort, fatigue, dyspareunia, vaginal dryness, and decreased libido,11,12 and studies reported sexual dysfunction in a large number of patients.13 A qualitative study found that women with GC have concerns about losing their position in marital life and the possibility of divorce and separation.14 A study also shows that GC patients had poorer marital satisfaction and adjustment compared to norms from general population.15 A study reported that 27% of GC women in a relationship experienced marital dysfunction.16 Poorer marital adjustment can lead to slowed recovery trajectories and poor physical outcomes.17 In contrast, good marital satisfaction can lead to better emotional adjustment, sexual functioning, quality of life, body image,17 less stress, and inflammation.18 Patients could then further obtain benefits in survival and functioning19 after a cancer diagnosis because of better economic and social support to receive effective medical treatments20 and sharing their emotional burdens.21,22 Since then, to live through cancer, a good marital relationship becomes significant for GC patients. Nevertheless, an effective, validated and brief tool to measure marital satisfaction and adjustment in China is scarce, which hinders the development of targeted intervention for intimate relationship promotion in couples coping with GC.
Similarly in the Chinese and Western populations, unmarried is associated with increased cancer mortality in patients.23,24 The reasons could be access to more resources, healthier lifestyles and behaviours, and earlier contact with health personnel when having a partner.25 A lot of marital problems can be related to stress, especially financial stress.26 GC poses threat to the life of patients and treatments of patients also brings economic burden to the family of patients, which might threaten the relationship between GC patients and partners.26, 27, 28 Marital satisfaction and adjustment describe couples' adaptation that is used to predict marital success. Since then, effective measurement of marital satisfaction and adjustment is important for GC patients to benefit in cancer survival. The dyadic adjustment scale (DAS) is the most widely used tool for assessing marital satisfaction and marital adjustment.29 To eliminate some problems in the subscales and individual items of the 32-item DAS, Busby and colleagues improved the original DAS to a 14-item brief version, the revised dyadic adjustment scale (R-DAS).30 This version evaluates three dimensions, namely consensus, satisfaction and cohesion, and is substantially consistent and convergent with the original full-scale version. Busby and colleagues30 also assessed the internal consistency of the R-DAS and found that Cronbach's α ranged from 0.80 to 0.85 across the three domains and demonstrated its construct validity by correlating it with another instrument used for assessing the quality of marital relationship, namely the Locke–Wallace marital adjustment test.
The R-DAS has been translated into many languages, e.g., Persian, Romania, and Portuguese and validated for use in couples.31, 32, 33, 34 However, the R-DAS has not yet been translated into simplified Chinese and psychometrically validated in mainland Chinese GC patients and their partners. This aim of this study was to fill this gap in assessing marital satisfaction and marital adjustment in Chinese GC patients and their partners by translating the R-DAS into Chinese and validating, thereby facilitating widespread use of the tool in China and improving intimate relationships in couples coping with GC.
Methods
Study design
A cross-sectional design with a random subsample re-tested at one-week interval was used to examine the psychometric properties of the Chinese version of the R-DAS (CR-DAS) in Chinese GC patients and their partners.
The translation process of the CR-DAS
The translation process was conducted according to the guidelines developed by the World Health Organization, which focus on cross-cultural equivalence.35 This method adopts four steps: forward-translation, expert panel, back-translation, pre-testing and cognitive interviewing. Forward-translation was performed by two bilingual doctoral-level nursing students who were native-speakers of Chinese and had research experience in female oncology. An expert panel was established in the early phase of the translation process to identify and resolve the inadequate expressions of the translation and identify discrepancies between the forward translation and the existing or comparable previous versions of the tool. The expert panel in this study comprised two translators from step one, a professor skilled in instrument translation, and a registered nurse in the gynaecological oncology department. Backward-translation was performed by two bilingual doctoral-level nursing students who have lived abroad for more than three years and not aware of the original items. Discrepancies was discussed and the previous three steps were iterated until a satisfactory version was reached. Pre-testing and cognitive interviewing in 10 GC patients and 10 partners were conducted and the final version of the translated R-DAS was completed.
Setting and sampling
The participants were GC patients and their partners visiting the gynaecological oncological department of a tertiary hospital in Shaanxi, China. A convenience sampling method was adopted. The inclusion criteria for the GC patients and their partners were as follows:
GC patients: (1) diagnosed with GC (ovarian, uterine, cervical, vulvar or vaginal cancer); (2) married or living in a committed relationship for at least 12 months; and (3) can speak Mandarin.
Partners: (1) have wife/girlfriend diagnosed with GC; (2) married or living in a committed relationship for at least 12 months with the wife/girlfriend; and (3) can speak Mandarin.
Exclusion criteria were (1) women with other types of cancer in addition to GC; (2) women with partners who had cancer or other severe diseases; or (3) women with partners who were unwilling or refused to participate in the study.
Sample size
The adequate sample size to examine the psychometric properties of the CR-DAS was determined as follows. For convergent validity, using G∗Power 3.1, it was estimated that a sample of 84 participants would be adequate to detect a small to moderate correlation of 0.3 with 80% power at 5% level of significance. For structural validity, Stevens indicated that at least 15 cases are required for each variable in a factor analysis,36 a minimum of 210 participants were considered necessary for this study.
For test–retest reliability, 51 participants were considered to be adequate to confine the precision of the test–retest reliability assessed by intraclass correlation coefficient (ICC) to ± 0.1, assuming that the reliability coefficient was 0.7 or more.
In this study, a total of 252 participants (126 GC patients and 126 partners) were ultimately enrolled. Of these, a random subsample of 51 patients and 51 partners were chosen for the test–retest assessment of the CR-DAS. Meanwhile, a random subsample of 84 patients and 84 partners were chosen for convergent validity.
Data collection
Data were collected after obtaining written consent from each participant. Data was collected at two time points one week apart from participants included in the test–retest assessment.
The 14-item R-DAS has seven dimensions within three overarching categories, including consensus in decision making, values and affection, satisfaction in the relationship with respect to stability and conflict regulation, and cohesion as seen through activities and discussion.30 The R-DAS has good internal consistency with Cronbach's α of 0.90 for the total score.30 Participants were asked to indicate the approximate extent of agreement or disagreement between them and their partner on certain aspects of their relationship using a five- or six-point scale.30 Scores on the R-DAS range from 0 to 69, with a cut-off at 48, with higher scores indicating greater relationship satisfaction.37
The quality of marriage index (QMI) was used to establish the convergent validity of the CR-DAS.38 The QMI is a tool for global assessment of the quality of marriage and comprises six items, each querying the participants about the extent to which they agree or disagree with the quality of their relationship satisfaction.39 The first five items are rated on a seven-point Likert scale ranging from 1 (very strong disagreement) to 7 (very strong agreement), and the last item is rated on a 10-point scale, ranging from 1 (very unhappy) to 10 (perfectly happy).39 Higher scores indicated greater satisfaction with marriage.39
Data analysis
IBM SPSS AMOS 23.0 was used for confirmatory factor analysis (CFA), and IBM SPSS 25.0 was used to perform other statistical analyses. All of the statistical tests were two-sided with the level of significance set at 0.05.
Semantic equivalence of the CR-DAS
The expert panel assessed the semantic equivalence of the completed version of CR-DAS. A four-point Likert scale ranging from 1 (not appropriate) to 4 (most appropriate) was developed to assess the degree to which the meaning of each item in the translated text (simplified Chinese) expressed the same meaning as that in the source language (English). An item was considered not equivalent if more than 20% of the panellists rated that item less than 3 on the Likert scale.
Reliability
The internal consistency of the CR-DAS was assessed by calculating Cronbach's α. The stability of the CR-DAS was evaluated by assessing the 1-week interval test–retest reliability.
The internal consistency and stability of the CR-DAS were evaluated using the Cronbach's α statistics and the ICC, respectively. Cronbach's α of an instrument must ≥ 0.7 to ensure good internal consistency. An ICC of > 0.75 is considered to indicate good test–retest reliability. The items with an item–total correlation value of ≥ 0.30 are considered to represent similar behaviours and indicate a high internal consistency of the test.
Validity
An item-content validity index (I-CVI) and scale-content validity index (S-CVI) were used to determine the content validity of the CR-DAS. An I-CVI ≥ 0.78 and an S-CVI ≥ 0.80 are considered to be acceptable.40
CFA was conducted in AMOS to determine the theoretical second-order 3-factor structure of CR-DAS according to the structure of original R-DAS.30 The three subscales (consensus, satisfaction and cohesion) were predefined as first-order factors, and the seven dimensions within the three subscales were predefined as second-order factors.30 Model fit was assessed using the following indices (criteria indicating good model fit are given in parentheses): χ2/df (2–5), goodness-of-fit index (GFI; > 0.9), root-mean-square error of approximation (RMSEA; < 0.08), root-mean-square residual (RMR; < 0.08), standardised root-mean-square residual (SRMR; < 0.08), comparative fit index (CFI; > 0.9), parsimonious normed-fit index (PNFI; > 0.5) and parsimony goodness-of-fit index (PGFI; > 0.5).41
The convergent validity of the CR-DAS with the QMI was assessed using Pearson's correlation coefficient, with a correlation coefficient > 0.5 considered to indicate an adequate convergent validity. The known-group validity was tested using an independent t-test.
Ethical considerations
The study was conducted according to the Helsinki Declaration and was approved by all responsible ethics committees in the institutions to which the researchers were affiliated. Informed written consent was obtained from all participants before their enrolment in this study.
Results
Participant characteristics
A total of 542 participants were screened, 393 of whom were found to be eligible. Among them, 141 participants refused to participate because of lack of interest or physical discomfort. Ultimately, a total of 252 participants entered the study, including 126 GC patients and 126 partners. Patients were 48.49 ± 7.38 years old while partners were 48.95 ± 8.36 years old (Table 1).
Table 1.
Sociodemographic and clinical information and scores on the Chinese version of the Revised Dyadic Adjustment Scale (n = 252).
| Characteristics | Patients (n = 126) |
Partners (n = 126) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Age (years), Mean ± SD | 48.49 ± 7.38 | 48.95 ± 8.36 | ||
| ≤ 45 | 34 | 27.0 | 35 | 27.8 |
| > 45 | 92 | 73.0 | 91 | 72.2 |
| Diagnosis b | ||||
| Cervical cancer | 101 | 80.2 | 100 | 79.4 |
| Ovarian cancer | 13 | 10.3 | 10 | 7.9 |
| Endometrial/Vaginal cancer | 12 | 9.5 | 16 | 12.7 |
| Medical treatment typesa,b | ||||
| 1 type | 27 | 22.1 | 28 | 22.8 |
| 2 or more types | 95 | 77.9 | 95 | 77.2 |
| Cancer stagea,b | ||||
| Stage I–II | 84 | 74.3 | 66 | 59.5 |
| Stage III–IV | 29 | 25.7 | 45 | 50.5 |
| Months since diagnosisa,b | ||||
| ≤ 5 | 84 | 67.2 | 75 | 62.5 |
| > 5 | 41 | 32.8 | 45 | 37.5 |
| Educational levela | ||||
| Below Middle school | 92 | 73.6 | 65 | 51.6 |
| High school or higher | 33 | 26.4 | 61 | 48.4 |
| Employment | ||||
| Have work | 90 | 71.4 | 119 | 94.4 |
| No work | 36 | 28.6 | 7 | 5.6 |
| Parity a | ||||
| Less than two | 33 | 26.8 | 52 | 42.3 |
| Two or more | 90 | 73.2 | 71 | 57.7 |
| Monthly income per capita (RMB) | ||||
| Less than 2000 | 45 | 35.7 | 44 | 34.9 |
| 2000–6000 | 70 | 55.6 | 69 | 54.8 |
| > 6000 | 11 | 8.7 | 13 | 10.3 |
| Medical insurance reimbursement rateb | ||||
| < 30% | 0 | 0 | 3 | 2.4 |
| 30–50% | 36 | 28.6 | 37 | 29.3 |
| 51–80% | 81 | 64.3 | 80 | 63.5 |
| > 80% | 9 | 7.1 | 6 | 4.8 |
With missing data.
For partners refers to information of their wives.
Semantic equivalence and content validity of the Chinese version of the CR-DAS
All items were semantically equivalent, with less than 20% of the participants giving items a rating less than 3 on the Likert scale.
The I-CVI of the CR-DAS for each item ranged from 83.3% to 100%, and the S-CVI was 0.94, indicating that the representativeness of the CR-DAS items was good.
Reliability of the CR-DAS
Internal consistency
The CR-DAS showed good internal consistency for the total score (α = 0.85) and the consensus (α = 0.76), satisfaction (α = 0.87) and cohesion (α = 0.84) subscales in all participants (Table 2). Furthermore, the CR-DAS showed good internal consistency for the total score in both GC patients (α = 0.86) and their partners (α = 0.85).
Table 2.
Reliability of the Chinese version of the Revised Dyadic Adjustment Scale (n = 252).
| Factor/No. item | Item-factor correlation | Corrected item-total correlation | Cronbach’s α | Cronbach’s α if item deleted |
|---|---|---|---|---|
| Consensus | 0.755 | |||
| 1. Religious matters | 0.398 | 0.246 | 0.775 | |
| 2. Demonstrations of affection | 0.722 | 0.583 | 0.715 | |
| 3. Making major decisions | 0.751 | 0.535 | 0.695 | |
| 4. Sex relations | 0.728 | 0.529 | 0.696 | |
| 5. Conventionality (correct or proper behavior) | 0.681 | 0.338 | 0.712 | |
| 6. Career decisions | 0.705 | 0.371 | 0.709 | |
| Satisfaction | 0.866 | |||
| 7. How often do you discuss or have you considered divorce, separation, or terminating your relationship? | 0.819 | 0.626 | 0.840 | |
| 8. How often do you and your partner quarrel? | 0.871 | 0.597 | 0.821 | |
| 9. Do you ever regret that you married (or lived together)? | 0.828 | 0.678 | 0.833 | |
| 10. How often do you and your mate ‘get on each other's nerves’? | 0.870 | 0.594 | 0.817 | |
| Cohesion | 0.838 | |||
| 11. Do you and your mate engage in outside interests together? | 0.780 | 0.379 | 0.823 | |
| 12. Have a stimulating exchange of ideas | 0.832 | 0.607 | 0.786 | |
| 13. Work together on a project | 0.819 | 0.419 | 0.802 | |
| 14. Calmly discuss something | 0.854 | 0.551 | 0.770 | |
In the overall sample, the item analysis of the CR-DAS revealed that the item–total correlation value for item 1 was 0.246. For the other 13 items, the value was between 0.338 and 0.678. All items appeared to be worthy of retention because the maximum increase in Cronbach's α, which resulted from deleting item 1 from the measure, was small (0.02).
Test–retest reliability
The ICC between the test and 1-week retest in the randomly selected participants (n = 102) was 0.88 (P < 0.001). Furthermore, ICCs in the GC patient and partner subsamples were 0.88 (P < 0.001) and 0.89 (P < 0.001), respectively. These results indicated that the CR-DAS had an excellent test–retest reliability in both CG patients and their partners.
Validity of the CR-DAS
Confirmatory factor analysis
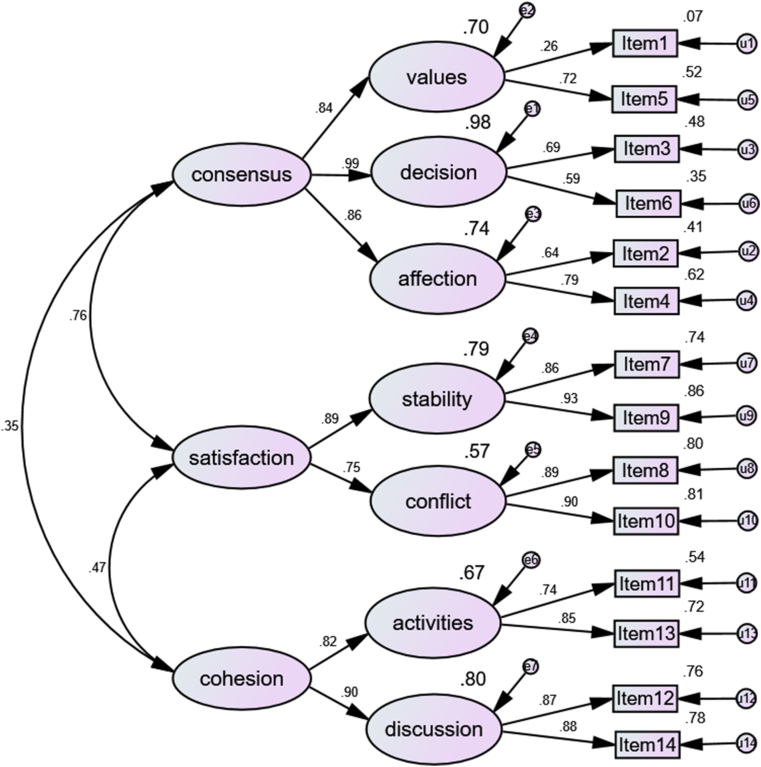
A CFA was conducted to examine the structural validity of the CR-DAS based on the hierarchical model proposed by Busby.30 Figure 1 shows the CFA results of the second-order 3-factor structure of the CR-DAS. The fit indices indicated that the model adequately fitted the data (Table 3).
Figure 1.
Structure of the Chinese version of the revised dyadic adjustment scale measurement model of confirmatory factor analysis.
Table 3.
Model fit indices for the confirmatory factor analysis.
| Index | Value |
|---|---|
| χ2/df | 2.560 |
| GFI | 0.913 |
| RMSEA | 0.079 |
| RMR | 0.046 |
| SRMR | 0.073 |
| CFI | 0.932 |
| PNFI | 0.688 |
| PGFI | 0.608 |
Abbreviations: GFI, goodness-of-fit index; RMSEA, root-mean-square error of approximation; RMR, root-mean-square residual; SRMR, standardised root-mean-square residual; CFI, comparative fit index; PNFI, parsimonious normed-fit index; PGFI, parsimony goodness-of-fit index.
Convergent validity
In participants, the correlation coefficient between the QMI and the total score of the CR-DAS was 0.60 (P < 0.001). Furthermore, in GC patients, the correlation coefficient between the QMI and the total score of the CR-DAS was 0.70 (P < 0.001). In partners, the correlation coefficient was 0.52 (P < 0.001). These results support the convergent validity of the scale.
Known-group validity
It was hypothesised that the CR-DAS can discriminate marital satisfaction and adjustment between patients who undergo more types of treatments and those who undergo fewer types of treatment. The independent t-test results indicated that women undergoing two and more types of treatments reported significantly higher CR-DAS score (Cohen's d = 0.50) than women undergoing one type of treatment. While in male partners, the independent t-test results indicated that male partners whose female partner was five or fewer months since diagnosis reported significantly higher CR-DAS score (Cohen's d = 0.38) than their counterparts whose female partner was more than five months after diagnosis.
Discussion
GC is known to adversely affect the sexual life and intimacy of couples, and thus marital satisfaction and adjustment is crucial to assist couples.42,43 In this context, a psychometrically sound scale to measure marital satisfaction and adjustment is essential. Our findings suggest that the CR-DAS has good reliability and acceptable content and convergent validity in Chinese GC patients and their partners.
Reliability
The reliability of the overall scale and subscales was high, with Cronbach's α coefficient of 0.85 and test–retest ICC of 0.88 in total participants and were also found to be high for the overall scale in both the patient and partner subsamples. This finding is consistent with that of some previous reports that evaluated the reliability of traditional Chinese version of 32-item DAS in Hong Kong.44 These results are also similar to other studies that translated and validated the R-DAS in other languages and countries in healthy population and patients with diseases. For these versions of R-DAS, Cronbach's α values range from 0.79 to 0.898 and test–retest ICCs range from 0.71 to 0.98.31,32,34
An item–total correlation analysis was used to determine the reliability of the items in the CR-DAS. The correlation coefficient of the first item ‘the level of agreement in the couple about religious matters’ was lower than those of the other 13 items. This indicated that religious subjects may be less important for agreement between couples, consistent with the fact that over 93% of participants in this study had no religion. This could be attributable to the fact that the study was conducted in a less religiously diverse area of China. Therefore, this item needs to be tested in a more religiously diverse area in China. The high values of the remaining items indicated that each item measured a similar behaviour, indicating a high internal consistency of the scale.
Validity
Analysis of the structural validity revealed that the 14 items could be grouped into seven first-order factors, with decision, values and affection contributing to the consensus subscale; stability and conflict contributing to the satisfaction subscale; and activities and discussion contributing to the cohesion subscale. In the overall scale, only item 1 exhibited low variance and a weak correlation to the original factor, indicating that the item needs to be validated in a multi-religious area in China.
Further, our results showed that the correlation coefficients of the CR-DAS with the quality of marriage measured by the QMI were high and statistically significant, supporting the convergent validity of the CR-DAS. Similarly, Shek44 previously reported that the traditional Chinese version of the DAS correlated significantly and substantially with the quality of marital relationship assessed using the Kansas marital satisfaction scale and the marital comparison level index in the Hong Kong population. These results confirm our hypothesis that better marital satisfaction and adjustment indicates higher quality of marriage.
Our results also confirmed that marital satisfaction and adjustment in GC patients were positively associated with the number of the types of treatment that the patients were undergoing. That is, as GC patients undergoing more types of treatment receive more attention and care from their partners, such support can help to build their intimate relationship.45 Marital satisfaction in male partners is significantly higher for those whose female partner is five or fewer months since diagnosis than those with a female partner for more than five months since diagnosis. This difference is consistent with the study by Harju,46 it might result from male partners' decreased support and active engagement in female partners’ cancer treatment with time after diagnosis,47 which causes decreased marital satisfaction and adjustment over time.
Implications for clinical practice
Promoting marital satisfaction and adjustment between GC patients and their partners can improve interpersonal support and relationship between the couples, which may, in turn, promote the patients’ recovery and survival from GC and treatment. This study demonstrated the reliability and validity of the CR-DAS in GC patients and their partners and has several important practical and research implications. First, the CR-DAS may serve as a succinct and effective tool for evaluating the effectiveness of the clinical nursing services on intimate relationships provided to either married or unmarried cohabiting couples coping with GC. The R-DAS measures marital adjustment, which is a process rather than an unchanging state.29 Specifically, the R-DAS measures whether couples agree or disagree on certain aspects of their relationship.30 If more disagreement exists, there are more conflicts on consensus, decision making, values, affection, satisfaction and cohesion, indicating poor marital satisfaction and adjustment.30 The outcome of marital adjustment is determined by the degree of troublesome dyadic differences; interpersonal tensions and personal anxiety; dyadic satisfaction; dyadic cohesion and consensus on matters of importance to dyadic functioning.29 Better marital adjustment is associated with better patient health via better emotional and physical support from partner, better adherence to therapies due to possible encouragement by partners, better problem solving, communication and perform better family roles, fewer conflicts and solve problems easier,48 and better access to medical care and health utilisation.49 By measuring marital adjustment, we can find out couples in marital distress and then provide them couple therapy and educate partners to provide more support and fulfil their roles as a caregiver to better care for patient and then promote the health of patients. Second, the study fills the gap of psychometrically testing the reliability and validity of CR-DAS in measuring marital adjustment in Chinese GC patients and partners. The scale provides an opportunity to compare marital adjustment and satisfaction between China and other parts of the world. The CR-DAS can help researchers and clinicians compare interventions to find one that more effectively improves marital satisfaction and adjustment in Chinese GC patients and their partners, as well as provide couple therapy to patients and partners to achieve better and targeted care. Third, the CR-DAS can be considered as an instrument to distinguish people who are undergoing marital/relationship distress from non-distress after having been admitted to a hospital for treatment if a cut-off value of CR-DAS is established. Couples who are married or unmarried cohabiting in a committed relationship coping with GC could be measured by the CR-DAS, which could be helpful in individualising psychosocial assessment and intervention. The cut-off score of the English version of R-DAS has obtained a value at 4837 but it has not been established in the Chinese population yet and future studies are needed.
Limitations
The study subjects were mainly rural-dwelling Chinese who did not have religious beliefs; therefore, a validation of the CR-DAS in people of different working classes and with religious beliefs is warranted. Furthermore, only GC patients and their partners were included in the study, the generalisability of the CR-DAS used in patients with other diseases is limited. However, the scale has the possibility to be used as a standard for all married couples to test whether they are in marital distress. We recommend further research on patients with different types of cancer that compromise intimate relationships to further validate the psychometric properties of the CR-DAS. In addition, the design of the study is unable to establish an accurate and effective cut-off score in Chinese GC patients and future studies should further explore this issue. Considering the limitation of this study, the conclusion should be interpreted with caution.
Conclusions
The internal consistency, test–retest reliability, convergent validity, known-group validity and structural validity of the CR-DAS were satisfactory in Chinese GC patients and their partners. Clinicians can therefore use the CR-DAS to measure the intimate relationship of Chinese GC patients with their partners and improve their mutual support.
Funding
Nil.
Declaration of competing interest
None declared.
References
- 1.WHO . 2020. Cancer Today.http://gco.iarc.fr/today/fact-sheets-populations Accessed Jan 22, 2022. [Google Scholar]
- 2.Carr S.V. Psychosexual health in gynecological cancer. Int J Gynecol Obstet. 2015;131:S159–S163. doi: 10.1016/j.ijgo.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Iżycki D., Woźniak K., Iżycka N. Consequences of gynecological cancer in patients and their partners from the sexual and psychological perspective. Prz menopauzalny. 2016;15:112–116. doi: 10.5114/pm.2016.61194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tornatta J.M., Carpenter J.S., Schilder J., Cardenes H.R. Representations of vaginal symptoms in cervical cancer survivors. Cancer Nurs. 2009;32:378–384. doi: 10.1097/NCC.0b013e3181a54c39. [DOI] [PubMed] [Google Scholar]
- 5.Rostami A., Ghazinour M., Nygren L., Nojumi M., Richter J. Health-related quality of life, marital satisfaction, and social support in medical staff in Iran. Appl Res Qual Life. 2013;8:385–402. doi: 10.1007/s11482-012-9190-x. [DOI] [Google Scholar]
- 6.Lyons K.S., Lee C.S. The association of dyadic symptom appraisal with physical and mental health over time in care dyads living with lung cancer. J Fam Nurs. 2020;26:15–25. doi: 10.1177/1074840719889967. [DOI] [PubMed] [Google Scholar]
- 7.Chow K.M., So W.K.W., Choi K.C., Chan C.W.H. Sexual function, psychosocial adjustment to illness, and quality of life among Chinese gynaecological cancer survivors. Psycho Oncol. 2018;27:1257–1263. doi: 10.1002/pon.4663. [DOI] [PubMed] [Google Scholar]
- 8.Zimmermann T. Intimate relationships affected by breast cancer: interventions for couples. Breast Care. 2015;10:102–108. doi: 10.1159/000381966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moules N.J., Laing C.M., Estefan A., Schulte F., Guilcher G.M.T. “Family is who they say they are”: examining the effects of cancer on the romantic partners of adolescents and young adults. J Fam Nurs. 2018;24:374–404. doi: 10.1177/1074840718786985. [DOI] [PubMed] [Google Scholar]
- 10.Ratner E.S., Foran K.A., Schwartz P.E., Minkin M.J. Sexuality and intimacy after gynecological cancer. Maturitas. 2010;66:23–26. doi: 10.1016/j.maturitas.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 11.Graziottin A., Lukasiewicz M., Serafini A. In: Cancer, intimacy and sexuality. Reisman Y.G.W., editor. Springer International Publishing; Cham: 2017. Sexual rehabilitation after gynaecological cancers; pp. 205–222. [Google Scholar]
- 12.Liavaag A.H., Dørum A., Bjøro T., Oksefjell H., Fosså S.D., Tropé C., et al. A controlled study of sexual activity and functioning in epithelial ovarian cancer survivors. A therapeutic approach Gynecol Oncol. 2008;108:348–354. doi: 10.1016/j.ygyno.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Damast S., Alektiar K., Goldfarb S., Eaton A., Patil S., Mosenkis J., et al. Sexual functioning among endometrial cancer patients treated with adjuvant high-dose-rate intra-vaginal radiation therapy. Int J Radiat Oncol Biol Phys. 2012;84:e187–e193. doi: 10.1016/j.ijrobp.2012.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mofrad S.A., Nasiri A., Mahmoudirad G., Shandiz F.H. Challenges in the marital life of women with gynecological cancers: a qualitative study. Model Care J. 2021;18 doi: 10.5812/modernc.115558. [DOI] [Google Scholar]
- 15.Fischer O.J., Marguerie M., Brotto L.A. Sexual function, quality of Life, and experiences of women with ovarian cancer: a mixed-methods study. Sex Med. 2019;7:530–539. doi: 10.1016/j.esxm.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guntupalli S.R., Sheeder J., Ioffe Y., Tergas A., Wright J.D., Davidson S.A., et al. Sexual and marital dysfunction in women with gynecologic cancer. Int J Gynecol Cancer. 2017;27:603–607. doi: 10.1097/IGC.0000000000000906. [DOI] [PubMed] [Google Scholar]
- 17.Brandao T., Pedro J., Nunes N., Martins M.V., Costa M.E., Matos P.M. Marital adjustment in the context of female breast cancer: a systematic review. Psycho Oncol. 2017;26:2019–2029. doi: 10.1002/pon.4432. [DOI] [PubMed] [Google Scholar]
- 18.Shrout M.R., Renna M.E., Madison A.A., Alfano C.M., Povoski S.P., Lipari A.M., et al. Relationship satisfaction predicts lower stress and inflammation in breast cancer survivors: a longitudinal study of within-person and between-person effects. Psychoneuroendocrinology. 2020;118 doi: 10.1016/j.psyneuen.2020.104708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li M., Chan C.W.H., Chow K.M., Xiao J., Choi K.C. A systematic review and meta-analysis of couple-based intervention on sexuality and the quality of life of cancer patients and their partners. Support Care Cancer. 2020;28:1607–1630. doi: 10.1007/s00520-019-05215-z. [DOI] [PubMed] [Google Scholar]
- 20.Aizer A.A., Chen M.H., McCarthy E.P., Mendu M.L., Koo S., Wilhite T.J., et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31:3869–3876. doi: 10.1200/JCO.2013.49.6489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ali R., Mathew A., Prev BR-APJC, 2008 U Effects of socio-economic and demographic factors in delayed reporting and late-stage presentation among patients with breast cancer in a major cancer hospital in South India. Asian Pac J Cancer Prev APJCP. 2008;9:703–707. [PubMed] [Google Scholar]
- 22.Osazuwa-Peters N., Christopher K.M., Cass L.M., Massa S.T., Hussaini A.S., Behera A., et al. What’s love got to do with it? Marital status and survival of head and neck cancer. Eur J Cancer Care (Engl) 2019;28 doi: 10.1111/ecc.13022. [DOI] [PubMed] [Google Scholar]
- 23.Va P., Yang W.S., Nechuta S., Chow W.H., Cai H., Yang G., et al. Marital status and mortality among middle age and elderly men and women in urban Shanghai. PLoS One. 2011;6 doi: 10.1371/journal.pone.0026600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gomez S.L., Hurley S., Canchola A.J., Gomez S.L., Cheng I., Clarke C.A., et al. Effects of marital status and economic resources on survival after cancer: a population-based study. Cancer. 2016;122:1618–1625. doi: 10.1002/cncr.29885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Syse A., Lyngstad T.H. In sickness and in health: the role of marital partners in cancer survival. SSM - Popul Heal. 2017;3:99–110. doi: 10.1016/j.ssmph.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Little W. Introduction to sociology. 2nd ed. BC campus; Vancouver, Canada: 2016. [Google Scholar]
- 27.Wu Q., Jia M., Chen H., Zhang S., Liu Y., Prem K., et al. The economic burden of cervical cancer from diagnosis to one year after final discharge in Henan Province, China: a retrospective case series study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0232129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yue X., Pruemer J.M., Hincapie A.L., Almalki Z.S., Guo J.J. Economic burden and treatment patterns of gynecologic cancers in the United States: evidence from the medical expenditure panel survey 2007–2014. J Gynecol Oncol. 2020;31 doi: 10.3802/jgo.2020.31.e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spanier G.B. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. doi: 10.2307/350547. [DOI] [Google Scholar]
- 30.Busby D.M., Christensen C., Crane D.R., Larson J.H. A revision of the Dyadic Adjustment for use with distressed and nondistressed couples: construct hierarchy and multimensional scales. J Marital Fam Ther. 1995;21:289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x. [DOI] [Google Scholar]
- 31.Assari S., Moghani Lankarani M., Tavallaii S.A. Revised Dyadic Adjustment Scale as a reliable tool for assessment of quality of marital relationship in patients on long-term hemodialysis. Iran J Kidney Dis. 2009;3:242–245. [PubMed] [Google Scholar]
- 32.Hollist C.S., Falceto O.G., Ferreira L.M., Miller R.B., Springer P.R., Fernandes C.L.C., et al. Portuguese translation and validation of the revised dyadic adjustment scale. J Marital Fam Ther. 2012;38:348–358. doi: 10.1111/j.1752-0606.2012.00296.x. [DOI] [PubMed] [Google Scholar]
- 33.Turliuc M.N., Muraru A.A. Psychometric properties of the revised dyadic adjustment scale on a sample of married adults. J Psychol Educ Res. 2013;21:49–76. doi: 10.7334/psicothema2013.85. [DOI] [Google Scholar]
- 34.Isanezhad O., Ahmadi S.A., Bahrami F., Baghban-Cichani I., Farajzadegan Z., Etemadi O. Factor structure and reliability of the revised dyadic adjustment scale (RDAS) in Iranian population. Iran J psychiatry Behav Sci. 2012;6:55–61. [PMC free article] [PubMed] [Google Scholar]
- 35.WHO . 2010. Process of translation and adaptation of instruments.https://www.who.int/substance_abuse/research_tools/translation/en/ [Google Scholar]
- 36.Stevens J.P. 4th ed. Lawrence Erlbaum Associates; Mahwah: NJ: 2002. Applied multivariate statistics for the social sciences. [Google Scholar]
- 37.Crane D.R., Middleton K.C., Bean R.A. Establishing criterion scores for the Kansas marital satisfaction scale and the revised dyadic adjustment scale. Am J Fam Ther. 2000;28:53–60. doi: 10.1080/019261800261815. [DOI] [Google Scholar]
- 38.Hou J., Fang X. Marital stress and marital quality: the moderating effect of marital commitment and spouse support. Stud Psychol Behav. 2015;13:87–98. [Google Scholar]
- 39.Norton R. Measuring marital quality: a critical look at the dependent variable. J Marriage Fam. 1983;45:141. doi: 10.2307/351302. [DOI] [Google Scholar]
- 40.Polit D.F., Beck C.T. The content validity index: are you sure you know what’s being reported? critique and recommendations. Res Nurs Health. 2006;29:489–497. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 41.Hooper D., Coughlan J., Mullen M. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 42.Chow K.M., Chan C.W.H., Choi K.C., Shiu A.T.Y., Cheng K.K.F., Ip W.Y., et al. Psychometric properties of the Chinese version of sexual function after gynecologic illness scale (SFAGIS) Support Care Cancer. 2013;21:3079–3084. doi: 10.1007/s00520-013-1890-8. [DOI] [PubMed] [Google Scholar]
- 43.Gu C., Chan C.W.H., Twinn S. How sexual history and knowledge of cervical cancer and screening influence Chinese women’s screening behavior in Mainland China. Cancer Nurs. 2010;33:445–453. doi: 10.1097/NCC.0b013e3181e456dc. [DOI] [PubMed] [Google Scholar]
- 44.Shek D.T.L. Psychometric properties of the Chinese version of the dyadic adjustment scale. Psychol An Int J Psychol. 1994;37:7–17. [Google Scholar]
- 45.Lichtman R.R., Taylor S.E., Wood J.V. Social support and marital adjustment after breast cancer. J Psychosoc Oncol. 1988;5:47–74. doi: 10.1300/J077v05n03_03. [DOI] [Google Scholar]
- 46.Harju E., Rantanen A., Helminen M., Kaunonen M., Isotalo T., Åstedt-Kurki P. Marital relationship and health-related quality of life of patients with prostate cancer and their spouses: a longitudinal clinical study. J Clin Nurs. 2018;27:2633–2639. doi: 10.1111/jocn.14343. [DOI] [PubMed] [Google Scholar]
- 47.Hinnen C., Hagedoorn M., Sanderman R., Ranchor A.V. The role of distress, neuroticism and time since diagnosis in explaining support behaviors in partners of women with breast cancer: results of a longitudinal analysis. Psycho Oncol. 2007;16:913–919. doi: 10.1002/pon.1153. [DOI] [PubMed] [Google Scholar]
- 48.Basharpoor S., Sheykholeslami A. The relation of marital adjustment and family functions with quality of life in women. Eur J Psychol. 2015;11:432–441. doi: 10.5964/ejop.v11i3.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruiz-Marin C., Molina-Barea R., Slim M., Calandre E. Marital adjustment in patients with cancer: association with psychological distress, quality of life, and sleep problems. Int J Environ Res Publ Health. 2021;18 doi: 10.3390/ijerph18137089. [DOI] [PMC free article] [PubMed] [Google Scholar]