Abstract
Aims and objectives
The Covid-19 pandemic has had an unprecedented effect on surgical practice and healthcare delivery globally. We compared the impact of the care pathways which segregate Covid-19 Positive and Negative patients into two geographically separate sites, on hip fracture patients in our high-volume trauma center in 3 distinct eras - the pre-pandemic period, against the first Covid-19 wave with dual-site service design, as well as the subsequent surge with single-site service delivery. In addition, we sought to invoke similar experiences of centres worldwide through a scoping literature review on the current evidence on “Dual site” reconfigurations in response to Covid-19 pandemic.
Methods
We prospectively reviewed our hip fracture patients throughout the two peaks of the pandemic, with different service designs for each, and compared the outcomes with a historic service provision. Further, a comprehensive literature search was conducted using several databases for articles discussing Dual-site service redesign.
Results
In our in-house study, there was no statistically significant difference in mortality of hip fracture patients between the 3 periods, as well as their discharge destinations. With dual-site reconfiguration, patients took longer to reach theatre. However, there was much more nosocomial transmission with single-site service, and patients stayed in the hospital longer. 24 articles pertaining to the topic were selected for the scoping review. Most studies favour dual-site service reorganization, and reported beneficial outcomes from the detached care pathways.
Conclusion
It is safe to continue urgent as well as non-emergency surgery during the Covid-19 pandemic in a separate, geographically isolated site.
1. Introduction
Most healthcare services across the globe were largely unprepared for Covid-19 pandemic, which has truly tested their adaptability. Many centres instituted the so-called ‘hot’ and ‘cold’ sites to segregate Covid-19 positive and negative patients separately during their hospital stay.
University Hospitals of Leicester (UHL) is a three sited hospital trust serving the highly ethnically diverse population of Leicestershire and Rutland; a high-volume tertiary trauma centre that stands 4th in the National Hip Fracture Database (NHFD) with respect to the volume of hip fractures treated, with key performance indices well above the national average.1 All hip fractures patients would normally be treated initially at the acute site, with the aim to achieve time to theatre within 36 h of admission to the emergency department (ED), as per best practice tariff.2
The purpose of our study was primarily to assess the detrimental effects of a pandemic like Covid-19 upon the established hip fracture care pathways in a high-volume center, with respect to the established determinants and predictors of clinical outcomes. We compared similar cohorts of patients admitted during 3 distinct timeframes (Fig. 1) - 1. Pre-pandemic era, 2. During the first surge we experienced, when healthcare service pathways were rapidly reconfigured to deliver care in two geographically separated sites (Fig. 2), one for Covid-19 diagnosed and suspected patients and another for Covid-19 negative and asymptomatic patients, and lastly 3. During the second surge where the initial structural reconfiguration was repealed, and patients were managed at a single site, segregating newly admitted & subsequently diagnosed Covid-19 patients as and when the condition was identified.
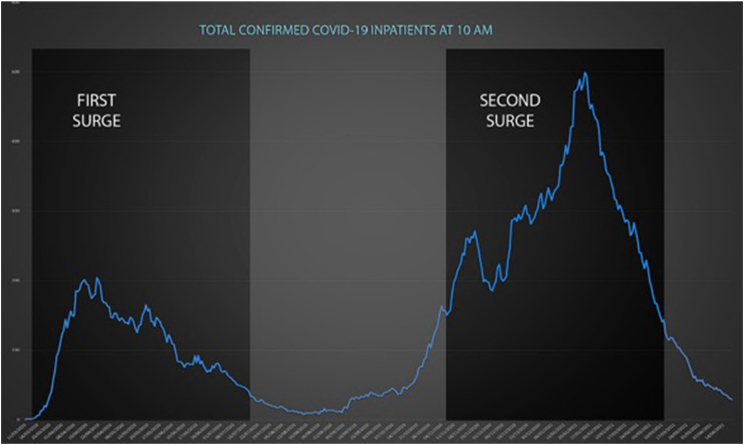
Fig. 1.
Study periods 2020 - First surge (12/03/20–15/07/20), Second surge (07/11/20–12/03/21) Blue line indicates volume of Covid-19 in-patients in the trust at any given time. Number of cases in the Y axis, Dates in the X axis.
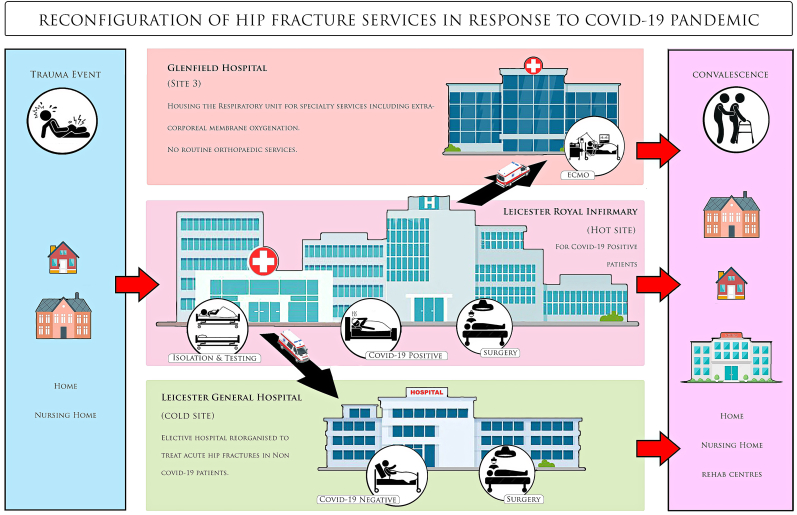
Fig. 2.
The flow of patients during the immediate response phase (First Surge). Leicester Royal Infirmary (LRI) received all acute hip fracture patients in the A&E, where they were isolated in holding bay and tested for Covid-19. The patients were then directed onwards to LGH if tested Covid-19 negative; or stayed in LRI if tested positive. Only those patients that required advanced respiratory input were transferred to the third site, GH. Patients underwent surgery in their respective sites, and were discharged to the community/rehab centre as applicable.
To get “the bigger picture”, we further sought to gather the current literary evidence on split-site service delivery for surgical patients across a broad array of surgical fields around the world. The extensive clinical and statistical heterogeneity in study settings, methods and outcome measures precluded a formal quantitative meta-analysis. This being a complex and emerging topic that has not been hitherto reviewed comprehensively, a scoping review was deemed most appropriate, to map the available evidence and identify gaps in existing literature related to ‘Cold-site’ service provision during the pandemic.
Reorganizing the hospital services to provide Covid-free pathways is often a major undertaking with high cost and logistic implications for the institution and care providers. In the face of newer Covid-19 variants with higher transmissibility and possible future surges, urgent information should be available to ascertain whether such pathways indeed reduce adverse consequences.
2. Materials and method
2.1. In-house study
2.1.1. Design
Data for the hip fracture patients admitted to UHL was collected from three time periods (126 days each in all three cohorts) for comparison. 1. The first surge of Covid-19 in 2020 (12/03/20–15/07/20); 2. The same time period pre-Covid-19 era (12/03/19–15/07/19); and 3. Similar time period during the second surge (07/11/20–12/03/21).
2.1.2. Population
All adult patients admitted with a fractured neck of femur during the study periods were included (n = 1192). Patients who had non-operative management, and those with sub-trochanteric and periprosthetic fractures were excluded.
2.1.3. Data collection
Data is collected prospectively for the NHFD. Patient demographics, dates and time of admission to the hospital, to the orthopaedic ward, and to theatre were collected, as well as the date of discharge from hospital, in-hospital mortality, residence before admission, and discharge destinations. Abbreviated Mental Test (AMT) score, American Society of Anaesthesiologists (ASA) grade, and clinical frailty scores (CFS) were also collected to compare functional baseline between the cohorts. Patients whose initial SARS-CoV-2 PCR swabs results were positive were classified as either positive on admission to hospital, or as nosocomial Covid-19 if they had negative PCR test results on admission and subsequently a positive test at least 7 days after admission.
2.1.4. Data analysis
Mann-Whitney U test was used to compare time to orthopaedic ward, time to theatre, and duration of hospital stay between patients in 2020 and 2019 and patients who tested negative for Covid-19 in 2020. Fisher's exact test was used to compare in-hospital mortality between patients in 2020 and 2019, Covid-19 negative patients from 2020 against the 2019 cohort. A seven-day rolling mean average was calculated for times to ward, time to theatre and length of hospital stay. These were represented graphically, along with the individual's times to ward, theatre and discharge, plotted at time of admission, as well as the number of Covid-19 cases within the trust, to compare 2019 and 2020 over the study period. GraphPad Prism 8 was used to perform statistical analyses.
3. Scoping review
3.1. Eligibility criteria
For inclusion in the literature review, articles were required to be in English language, peer-reviewed, and published from 2019 onwards. To fit in the inclusion criterion of complete patient segregation, geographically separated “hot” and “cold” sites with separate staff rota were included in the review, including specialized units set up in response to the pandemic. Staff segregation was also assessed, wherein care providers catering to non-Covid-19 patients do not encounter patients in “hot” areas on the same day.
3.2. Information sources
The scoping review was conducted by following the reporting checklist of the Preferred Reporting Items for Systematic Review and Meta-Analysis - Scoping Review extension for Scoping Reviews (PRISMA ScR). A comprehensive literature search was conducted using the PubMed, EMBASE, CINAHL, HMIC, Google Scholar databases for articles discussing split-service redesign.
3.3. Electronic search strategy: https://hdas.nice.org.uk/strategy/1080964/#show-searches
The search string had subject headings for Covid-19, with several relevant keywords pertaining to “dual-site”. Two reviewers individually analyzed and extracted the study characteristics and outcome parameters into a Microsoft Excel sheet. Data extracted included location, design, setting, study period and comparator, primary and secondary outcomes, volume of cases compared to historic cohort, peri-operative Covid-19 transmission, time to theatre, length of hospital stay, complication rates, all-cause and Covid-19 related mortality, discharge destinations & readmission rates. As this is a scoping study, we did not attempt to critically appraise the literature included.
4. Results of In-house study
4.1. Baseline characteristics and demographics
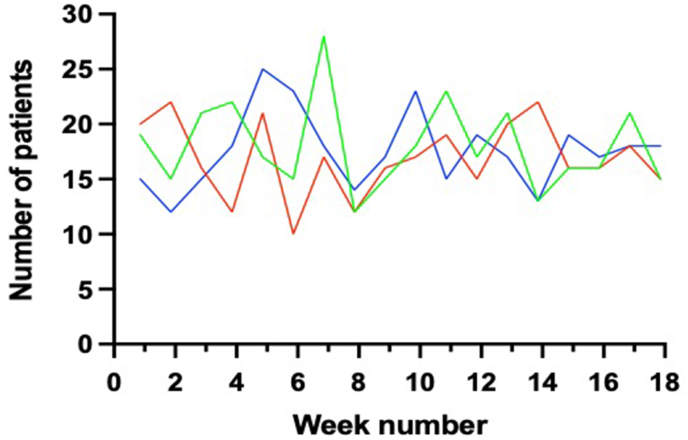
Table 1 summarizes Demographics and baseline characteristics. Age, gender, pre-admission residence, CFS, ASA grade, and pre-operative AMT were largely comparable between the cohorts (Table 2). The rate of admission of hip fractures were similar across the three time periods (Fig. 3), with a seven-day median admission rate of 16.5 (IQR 15.25, 19.75) patients in 2019, 17.5 (IQR 15, 18.75) during the first wave, and 17 (IQR 15, 21) in the second wave.
Table 1.
Baseline characteristics and demographics.
| 2019 | First wave | Second wave | |
|---|---|---|---|
| Total patients | 309 | 317 | 320 |
| Age | 83 (77, 89) | 84 (77, 90) | 85 (78, 90) |
| Gender (female) | 222 (72%) | 225 (71%) | 214 (67%) |
| Pre-admission residence | |||
| Own home/sheltered housing | 250 (81) | 245 (77) | 270 (84) |
| Institutional care | 56 (18) | 71 (22) | 5 (16) |
| Other | 3 (1) | 1 (0.3) | 0 |
Median (IQR), n (%).
Table 2.
Pre-admission functional baseline.
| 2019 | 2020 |
|||
|---|---|---|---|---|
| Total | COVID-19 positive | COVID-19 negative | ||
| Pre-op AMT | 9 (3, 10) | 8 (3, 10) | 5 (0, 9) | 9 (4, 10) |
| ASA grade | ||||
| 1 | 6 (2) | 0 | 0 | 0 |
| 2 | 34 (11) | 37 (12) | 0 | 37 (13) |
| 3 | 193 (63) | 222 (70) | 12 (60) | 210 (71) |
| 4 | 73 (24) | 57 (18) | 8 (40) | 49 (17) |
| 5 | 1 (0.3) | 0 | 0 | 0 |
| Clinical frailty score∗ | ||||
| 1 | 0 | 1 (0.3) | 0 | 1 (0.3) |
| 2 | 12 (4) | 13 (4) | 0 | 13 (5) |
| 3 | 40 (14) | 56 (18) | 0 | 56 (20) |
| 4 | 52 (18) | 65 (21) | 3 (15) | 62 (22) |
| 5 | 30 (10) | 20 (7) | 2 (10) | 18 (6) |
| 6 | 77 (27) | 101 (33) | 8 (40) | 93 (33) |
| 7 | 68 (24) | 47 (15) | 7 (35) | 40 (14) |
| 8 | 6 (2) | 2 (1) | 0 | 2 (1) |
| 9 | 4 (1) | 1 (0.3) | 0 | 1 (0.3) |
Median (IQR), n (%). AMT - Abbreviated mental test; ASA - American Society of Anaesthesiologists.
Fig. 3.
The number of patients admitted over the previous seven-day period. Red line = 2019, Blue line = 2020 First wave, Green = 2020 Second wave.
21 patients (7%) tested positive for Covid-19 in the first wave and 65 patients (20%) in the second. 296 patients (93%) had negative Covid-19 swab results. In the second wave, 4 (6%) patients tested positive on admission and the remainder of infections 61 (93%) were healthcare acquired.
4.2. Time to ward
Median time taken to orthopaedic ward was 5.4 (IQR 4.1, 6.4) hours in 2019, 4.9 (4, 6.3) for the first wave, and 6.1 (IQR 4.9, 7.8) for the second wave (Table 3).
Table 3.
Outcome measures.
| 2019 | First wave | Second wave | 2019 vs first wave | 2019 vs second wave | First vs second wave | |
|---|---|---|---|---|---|---|
| Time to orthopaedic ward (hours) | 5.4 (4.1, 6.4) | 4.9 (4, 6.3) | 6.1 (4.9, 7.5) | p = 0.042 | p < 0.01 | p < 0.01 |
| Time to theatre (hours) | 23 (17, 35) | 31 (20, 51) | 24 (19, 38) | p < 0.01 | 0.057 | P < 0.01 |
| Length of inpatient hospital stay (days) | 11 (8, 14) | 9 (7, 12) | 13 (9, 17) | p < 0.01 | p < 0.01 | p < 0.01 |
| Length of stay including time in rehabilitation (days) | 20 (11, 31) | 14 (8, 23) | 17 (11, 29) | p < 0.01 | p = 0.095 | p < 0.01 |
| In hospital mortality | 9 (3) | 17 (5) | 12 (4) | p = 0.16 | p = 0.66 | p = 0.35 |
Median (IQR), n (%).
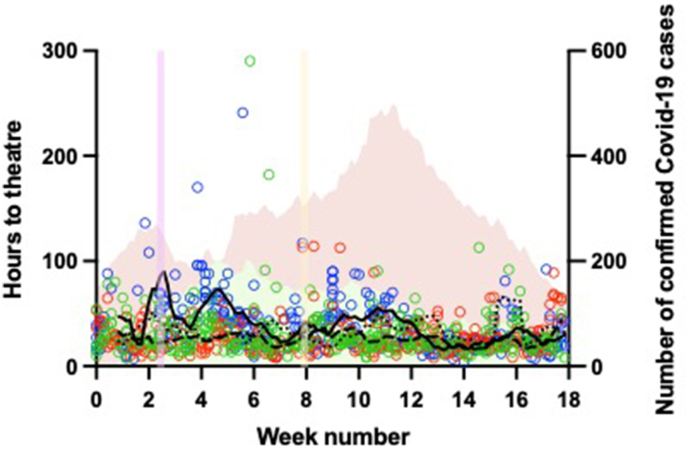
4.3. Time to theatre
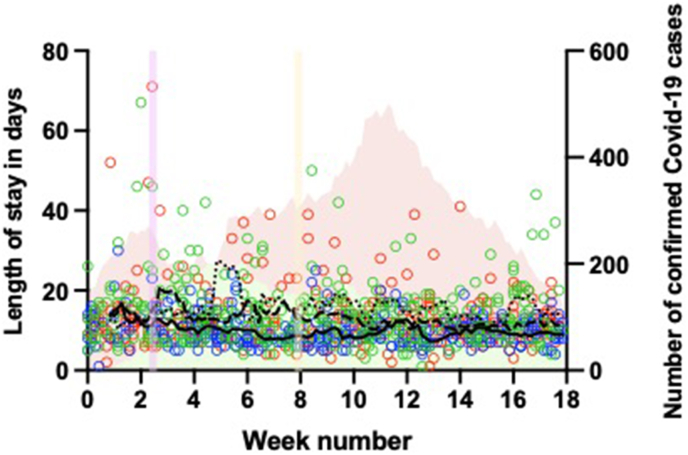
Median time taken to theatre was significantly longer in the first wave compared to 2019; however time to theatre showed no difference in the second wave compared to 2019 (Table' 3). Time to theatre was particularly high earlier in the first wave, and there appeared to be a greater variability in time to theatre in the first wave cohort (Fig. 4).
Fig. 4.
The length of time to theatre in hours by week of admission. Red circles represent individual patients admitted in 2019, blue circles individual patients in 2020 and green circles the second wave. The lines show seven-day rolling mean average, dashed line in 2019, solid line the first wave and dotted line for the second wave. Along the right y-axis the green shaded area show the number of confirmed COVID-19 cases within the hospital trust during the first wave, and red shaded area in the second wave.
4.4. Length of hospital stay
Compared to 2019, median length of inpatient hospital stay in those who survived to discharge was shorter during the first wave, but was longer in the second (Table 3). Compared to 2019, a similar trend was seen in length of hospital stay when including time spent in rehabilitation with the first wave, however the second wave did not show a statistically significant difference (Fig. 5).
Fig. 5.
The length of hospital stay in those who survived to discharge in days by week of admission
Red circles represent individual patients admitted in 2019, blue circles individual patients in 2020 and green circles the second wave. The lines show seven-day rolling mean average, dashed line in 2019, solid line the first wave and dotted line for the second wave. Along right y-axis and the green shaded area show the number of confirmed COVID-19 cases within the hospital Trust during the first wave, and red shaded area in the second wave.
4.5. In-hospital mortality
During the study period in 2019, 9 patients (3%) died in hospital, compared to 17 patients (5%) during the first wave, and 12 (4%) deaths in the second wave. These differences were not statistically significant (Table 3). There was no statistically significant difference in the number of deaths in 2019 and Covid-19 negative patients in the first or second wave (p = 0.39 and p = 0.8, respectively).
4.6. Discharge destination
Of those who survived to discharge, 28% patients were discharged to their own home or sheltered housing in the 2019 cohort, compared to 26% and 30% in the first and second wave respectively (Table 4). Slightly more patients were discharged to a rehabilitation unit or community hospital in 2019, and slightly less directly to institutional care.
Table 4.
Discharge Destinations of patients that survived to discharge.
| 2019 | First wave | Second wave | |
|---|---|---|---|
| Discharge destination (all patients) | |||
| Own home/sheltered housing | 85 (28) | 84 (26) | 96 (30) |
| Institutional care | 49 (16) | 74 (23) | 68 (21) |
| Rehabilitation unit/community hospital | 158 (51) | 136 (43) | 134 (42) |
| Other inc. acute hospital | 7 (2) | 6 (2) | 10 (3) |
| Discharge destination (patients admitted from own home/sheltered housing) | |||
| Own home/sheltered housing | 82 (33) | 84 (36) | 96 (36) |
| Institutional care | 6 (2) | 10 (4) | 24 (9) |
| Rehabilitation unit/community hospital | 153 (62) | 134 (58) | 132 (49) |
| Acute hospital/other | 4 (2) | 4 (2) | 7 (3) |
| Final destination of patients discharged from Rehabilitation unit/community hospital | |||
| Own home/sheltered housing | 131 (85) | 109 (81) | 101 (77) |
| Institutional care | 19 (13) | 14 (11) | 15 (11) |
| Died at rehabilitation unit | 1 (1) | 3 (2) | 5 (4) |
| Other inc. acute hospital | 2 (1) | 5 (4) | 7 (5) |
| Unknown | 3 (2) | 4 (3) | |
n (%).
4.7. Covid-19 Positive vs Negative patients
Age and gender were comparable between Covid-19 positive and negative patients in both waves (Table 5). 33% of those who tested positive were admitted from institutional care in the first wave, a higher percentage compared to Covid-19 negative patients. In the second wave, this was 20% in those who tested positive, compared to 15% in those who didn't.
Table 5.
Baseline characteristics by COVID-19 status.
| First wave |
Second wave |
|||
|---|---|---|---|---|
| COVID-19 positive | COVID-19 negative | COVID-19 positive | COVID-19 negative | |
| Total patients | 21 | 296 | 64 | 256 |
| Age | 85 (81, 90) | 84 (76, 90) | 84 (75, 88) | 86 (79, 90) |
| Gender (female) | 14 (67) | 211 (71) | 40 (62.5) | 174 (68) |
| Pre-admission residence | ||||
| Own home/sheltered housing | 13 (62) | 232 (78) | 51 (80) | 219 (85) |
| Institutional care | 7 (33) | 64 (22) | 13 (20) | 38 (15) |
| Other | 1 (5) | 0 | 0 | 0 |
Median (IQR), n (%).
Postoperative mortality related to Covid-19 in our cohort was 10.9%. In-hospital mortality was high in those who tested positive for Covid-19 at any point; with 15% (n = 4) Covid-19 positive in-patients dying during the first wave. This was lower in the second wave with 9% (n = 6) Covid-19 patients dying in ward.
5. Results of Scoping review
The primary search yielded 258 articles. Two reviewers screened the titles and abstracts from the same search results independently. After removing extraneous results, duplicates, studies not involving surgical patients, and those by non-medical allied health services, full texts of the relevant articles were retrieved and discussed to map key observations and inferences. Papers not specifying geographic separation of patients, or utilizing single-site model without reorganization of workforce were also discarded.
Finally, 24 articles3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 pertinent to the topic in question were shortlisted through an iterative process of mutual discussions among reviewers. Disagreements on study selection and conclusions were resolved by consensus between authors.
As expected, there was considerable heterogenicity in the study settings and outcome parameters. Most articles included in the synthesis compared the outcomes of two-site service delivery (intervention) against a similar period in the pre-pandemic era (comparator), or between the two sites themselves. We summarized the results using descriptive statistics (percentage change in median and IQR), and narrative synthesis. In accordance with the Synthesis Without Meta-analysis (SWiM) guidelines,25 primary outcomes were mapped as per protocol. The secondary outcome (Perioperative Covid-19) being without a comparator, we charted it as an independent variable, informed where possible by statistics. Formal assessment of methodological limitations or risk of bias in the evidence was not performed.
6. Synthesis
6.1. Study characteristics
Median duration of the observations was 69 days (IQR = 57–111). Six articles analyzed emergency/urgent surgical activity alone; nine papers were exclusively about elective surgical procedures. Lastly, nine studies dealt with both elective and emergency surgical services. Median sample size was 146 (IQR 112, 271) in the articles examined (Table 6).
Table 6.
Overview of Studies included in Scoping review.
| Author | Service | Study type | Duration (days) | No. of subjects (n) |
|---|---|---|---|---|
| Vlastos et al. | Aortic valve surgery | PR | 90 | 227 |
| Bonalumi et al. | Cardio vascular surgery | P | 42 | 41 |
| Wickramarachchi et al. | Trauma & Hip fracture | P | 60 | 138 |
| Picardo et al. | Hand surgery | P | 70 | 385 |
| Chiesa et al. | Vascular surgery | P | 70 | 135 |
| Collins et al. | Urology | PR | 60 | 159 |
| Lim et al. | Trauma & Hip fracture | PR | 31 | 185 |
| Ramsingh et al. | Cardiac surgery | P | 67 | 58 |
| Kasivisvanathan et al. | Urological, Thoracic, Gynaecological & General Surgery | P | 48 | 500 |
| Iqbal et al. | Cancer surgery | R | 60 | 153 |
| Rajasekaran et al. | Sarcoma | P | 61 | 56 |
| Chui et al. | Hip fracture | PR | 30 | 47 |
| Kathryn et al. | Trauma surgery | PR | 76 | 400 |
| Chang et al. | Elective Orthopaedic surgery | P | 25 | 121 |
| Bhangu et al. | Cancer surgery | P | 111 | 2481 |
| Stroman et al. | Elective Urological | R | 92 | 495 |
| Ally et al. | Elective ENT surgery | R | 112 | 85 |
| Dayananda et al. | Trauma service & NOF | PR | 28 | 130 |
| Kuusk et al. | Kidney Cancer | R | 197 | 130 |
| Digne-Malcolm et al. | General Surgery, Urology | PR | 120 | 881 |
| Hanna et al. | Colorectal cancer surgery | R | 180 | 24 |
| Ghosh et al. | Colorectal cancer surgery | P | 183 | 166 |
| Hamid et al. | Colorectal cancer surgery | R | 120 | 233 |
| D'Angelo et al. | Trauma & Hip fracture | PR | 68 | 134 |
P – Prospective, R – Retrospective, PR – Prospective with Retrospective cohort.
6.2. Volume of cases
11 authors reported comparative reduction in the volume of patients for the respective service rendered during the pandemic, and another study reported no change. Of the three articles that compared the admission rates of femoral fragility fractures, one reported an increase in case load, another reported a decrease, and yet another reported no change (Table 7).
Table 7.
Masterchart – scoping review outcome parameters.
| Author | Volume of cases | Peri-Op Covid-19 | Time to Theatre | Length of Stay | All-cause Mortality | Covid-19 Mortality | Complication rates | Discharge Destination | Re-admission (30 days) |
|---|---|---|---|---|---|---|---|---|---|
| Vlastos et al. | Reduced | 0% | – | – | No change | No change | – | – | |
| Bonalumi et al. | – | 7.30% | – | – | 0% | 0% | – | – | – |
| Wickramarachchi et al. | – | 1.45% | – | 8.7 days | 0.97% in Trauma. 0% in Hip |
0% in Trauma. 5.7% Hip |
– | – | – |
| Emma Picardo et al. | Reduced | 0% | – | – | 0.36% | 0.36% | 6.75% | – | 1.29% |
| Chiesa et al. | – | – | Less in Cold site (more in covid-19) | – | 2.20% | More in Covid | – | – | |
| Collins et al. | Reduced | 2.50% | – | – | – | 1.25% | – | – | – |
| Lim et al. | Reduced | – | – | – | – | – | – | – | |
| Ramsingh et al. | – | 0% | – | 5.7 ± 1.8 days | – | 0% | 1.72% | No change | – |
| Kasivisvanathan et al. | – | 2% | – | 1 night (median) | 1% | 0% | 18% | – | – |
| Iqbal et al. | – | 0.65% | – | – | 0% | 0% | 4.57% | – | 0.65% |
| Rajasekaran et al. | – | 7.10% | – | – | 3.60% | 3.6% 11.1% hot; 3.1% cold |
23.2% 37% hot vs 10.3% cold |
– | – |
| Chui et al. | No Change | 12.8% | Less in cold site. 52.8 vs 29.8 |
12.6 vs 8.7 (not statistically significant) | 10.6% (no significant difference two sites) | 6.38% 5.7% cold vs 25% hot |
– | – | 0% |
| Kathryn et al. | Reduced in trauma. Hips No change. |
4.50% | Reduced | Reduced | 4% (increased in 2020). In FFF 3.5% rise. |
1.80% | – | – | – |
| Chang et al. | – | 0.80% | – | – | – | – | – | – | |
| Bhangu et al. | – | 2.1% Cold. 3.6% Hot |
– | – | 1.5% Higher in red pathways |
0.64% | Less in Cold 2.2% versus 4.9% |
– | – |
| Stroman et al. | – | 1.6% Total20 (3.3%) - 17 hot, 3 cold |
– | Increased with Covid-19 infection | 0.30% | 0.30% | 0% | – | – |
| Ally et al. | – | 0% | – | – | 0% | 0% | 10.60% | – | – |
| Dayananda et al. | Reduced trauma. NOF increased. |
5% | – | 12 days (for NOFs) | – | 4.16% | – | – | – |
| Kuusk et al. | Reduced | 4% | – | – | – | 0% | – | – | – |
| Digne-Malcolm et al. | – | 0% | – | 1.69 ± 3.42 days. | 0.01% | 12.15% | – | 11.70% | |
| Hanna et al. | Reduced | – | – | Reduced (Non-significant) | No change | No change | – | – | |
| Ghosh et al. | Reduced | 0.60% | Unchanged | – | No change | No change | – | – | |
| Hamid et al. | – | 0% | – | 2.36 ± 3.26 days | 0% | 0% | 24.50% | – | 7.30% |
| D'Angelo et al. | Trauma and NOF reduced | 2.98% | Increased. Within 48 h - 58.7% (2020) vs 83.3 (2019) |
– | 0.74% vs 0.56% - No change from 2019 | 0% | – | – | – |
6.3. Peri-operative Covid-19
24 authors reported the perioperative Covid-19 rates of their institutions (Table 7). All the 6 studies that compared Covid-19 incidence between the hot and cold sites reported less peri-operative Covid-19 incidences in the Cold sites.
6.4. Time to theatre
Waiting times for surgery was shown to be reduced during the pandemic era in 3 studies; however this was increased in one study and unchanged in another. Two studies observed that the time to theatre was less in the cold site compared to hot site.
6.5. Length of hospital stay
The time patients spent in hospital was reported as unchanged by 2 centres; however this was longer in one study and reduced in another.
6.6. Mortality
Descriptive statistics for All-cause Mortality (n = 15) reveal an overall mean score of 1.69% (SD = 2.78). In these hospitals employing the two-site service transformation, all-cause Mortality did not show any statistically significant change in 5 studies, with only one centre reporting an increase in death rates among Orthopaedic trauma patients during the Covid-19 pandemic. One paper showed comparatively higher mortality in their Hot-site, while another reported no difference between the two sites.
Case fatality rate due to Covid-19 overall was 1.42% (SD 2.2) from 17 studies. Only seven articles specified the post-operative mortality of Covid-19 positive patients specifically, and this was 18% (SD 17.3).
6.7. Complication rates
Clavien-Dindo Grade 3 and above surgical complication rates averaged 11.2% ± 9.0 in the nine studies that reported it. No study showed any significant difference in complication rates in the Covid-19 period against the comparator. Three studies that compared complication rates between their two sites reported less incidence of complications in the cold-site cohort.
6.8. Discharge destination & Re-admissions
No changes in discharge destinations or differences in readmission rates were reported by any authors.
7. Discussion
7.1. In-house study
Several authors have reported, similar to our findings, that there was no decline in the incidence or admission rates of fragility hip fractures during the pandemic or lockdown.26, 27, 28, 29 Our results suggest that our ability to provide timely care for hip fracture patients was indeed compromised, as demonstrated by an overall increase in time to theatre during the pandemic, although this was not reflected in the in-hospital mortality observed. Advanced age, male sex, clinical comorbidities, pre-fracture place of residence, cognitive impairment and time-to-surgery have been suggested as significant predictors of postoperative mortality30, 31, 32, 33, 34, 35, 36, 37 in hip fractures. Delays to surgery for hip fractures are widely thought to be associated with poorer outcomes.32,33,38, 39, 40 Although this was not seen in our in-hospital mortality, with longer follow up this may unfortunately bear out.
Despite diverse and strict preventive measures, we saw ward outbreaks and increasing numbers of new cases with the single-site healthcare delivery provision, accounting for 93% of reported Covid-19 infections in the hospital during the second surge. Optimal preventive approaches, including regular surveillance testing of all asymptomatic staff and patients, and meticulous universal PPE and IPC precautions remain the vital strategies to contain nosocomial transmission.
A significant predictor of one-year mortality is reported to be the failure to recover ambulation.37,41,42 We have broadly similar discharge destinations across the two years, particularly in those admitted from their own home. Greater emphasis was likely placed in discharging patients during the pandemic to prevent nosocomial spread to vulnerable patients, as well as to ensure surge capacity, as reflected by the reduced length of hospital stay. This change in discharge practices early in the pandemic might have been at the expense of discharging patients earlier than ideal, and possibly risking missing perioperative complications.
Mortality was high in patients with Covid-19 infection during their hospital stay. There is existing evidence that the combination of Covid-19 infection and fractured neck of femur carries a poor prognosis,43, 44, 45, 46, 47, 48, 49, 50, 51 and that Covid-19 infection is an independent predictor of perioperative mortality.45,52,53 Authors from China and Italy reported mortality rates of 40% and 44% respectively28,44,48,49; studies from Spain demonstrated a mortality rate of 30.4% compared to 5.3% in those testing negative.27,47 There are several reports from the USA45,46 citing increased mortality and perioperative complications and the need for ventilatory support in the Covid-19 positive groups. In the UK43,52, 53, 54 varying reports exist with regard to mortality, as well as postoperative complications, ventilator needs, critical care admissions, clinic reviews and readmissions. These findings warrant further investigation, especially into ways to mitigate negative outcomes in this particularly challenging patient population.
The prime reason for the increased time to theatre in split-site service appeared to be the delay in transferring patients to the designated site, as side beds were often not readily available for patients whose Covid-19 swab results were pending. One of the solutions to circumvent this issue is point-of-care testing which readily provides Covid-19 test results from ED itself, which has been implemented by our trust from January 2021. The other obvious solution is to make more isolation beds available in the hospital, which can be quite challenging with the current capacity constraints experienced across most of the NHS trusts in the UK.
Another important outcome parameter is whether there was a change in the discharge destinations of patients, with regard to their pre-admission residential status. Only one study compared the discharge destinations of their patients, and this constitutes a knowledge gap with respect to this important indicator of clinical outcome.
7.2. Scoping review
Our literature review shows that during the pandemic, elective surgical activity experienced a sharp drop. The trauma admissions also declined initially, presumably on account of social distancing and travel restrictions. However, the geriatric hip fracture admissions remained unaffected during the pandemic.
Early reviewers from Lombardy, an area of extremely high epidemic impact, had advised that differentiation of flows and pathways to create a "Hospital inside a Hospital" is the single most important element in ensuring the safety of patients and operators and maintaining hospital activity.55
Soreide et al. did a scoping review of all available literature pertaining to Covid-19 and surgery, and concluded that in regions where hospital networks already exist, attempts at developing ‘Covid-19’ and ‘non-Covid-19’ hospitals is a reasonable way to preserve surgical services and normal function.56 The European Society of Sports Traumatology, Knee surgery and Arthroscopy (ESSKA) recommended a four-pronged strategy for resuming elective surgery, which includes setting up an isolated institution and a permanent Covid-19 Negative clinical pathway.57
Providing guidelines for resuming elective surgery in the time of pandemic, Al-Omar et al. advised isolating specific facilities for the treatment of Covid-19 patients to keep other facilities untainted, and suggested that isolation should also include healthcare providers and personnel.58 Global guidance for surgical care during the Covid-19 pandemic has also suggested that patients should be cared for by Covid-19 specific surgical teams if possible.59
Not all trusts have the luxury of two independent sites for the dual-site model, and segregation may have to be implemented within the hospital itself. Boyle et al. conducted a national survey among all 148 hospitals providing Colorectal cancer services in England and Wales, and reported that 54% hospitals had access to a ‘cold site’.60 Thinking beyond the Covid-19 crisis, Picardo et al. suggested that streamlining the services separately could also herald a paradigm shift inpatient care, which if widely adopted could drastically ease the annual winter pressures on the NHS as well.6
All papers in our Scoping review favoured structural service reorganization into dual-site configuration for continuing surgical care in the face of Covid-19 pandemic. However, a national study of the administrative hospital data for 14,930 colorectal cancer resection patients undertaken by Kuryba et al. found no evidence that surgery in Covid-free cold sites led to better clinical outcomes.61 It therefore follows that for contingency measures to work, they should rely on the site-specific granular understanding of the logistical issues at play, as well as the real-time data-driven appraisal of dynamic risk-benefit analysis.
Multiple studies have correlated perioperative Covid-19 infections in surgical patients with a significantly increased post-operative mortality.43, 44, 45, 46, 47, 48, 49, 50, 51 Case fatality rate owing to Covid-19 in post-operative cohort was 18% (SD 17.3) as inferred by this review, which is lower than the reports from China (20.5%),62 and by the worldwide COVIDSurg collaborative (23.8%).63
This review is an important first step in understanding the available evidence on this type of service reorganization, and hopefully will inform the future surge responses. With hospitals services returning to a new normal, and potential waves of newer variant Covid-19 related admissions highly likely, further studies to evaluate service adaptations are paramount to prepare contingency plans for future crises.
8. Strengths and limitations
8.1. In-house study
Ours is the only study we have come across which compares the two designs of service delivery by the same facility. Prospective design and sample size are two of its strengths. The data were collected prospectively for the NHFD, and the clinical outcomes were followed over time. A total of 1192 hip fracture patients (883 from during the pandemic and 309 historical) were included in this study which, to our knowledge, is the largest single-centre comparative cohort study in the literature to date examining the impact of the Covid-19 pandemic on the management of hip fracture patients.
Nevertheless, an important limitation is that the other known confounding factors were not taken into consideration when analyzing clinical outcomes, primarily because the focus of this particular inquiry was to look into the impact of a global crisis on the care pathways, rather than account for all the factors affecting clinical outcomes.
8.2. Scoping review
When heterogeneity of study designs and settings preclude a formal meta-analysis, meta-ethnography is generally considered the best tool in healthcare research for synthesizing the published results of qualitative studies in a systematic review. This enables the reviewer to create third-order interpretations consistent with the original researchers' findings, that can be used to inform policy and practice. The topic of dual-site service delivery for Covid-19 patients has no existing meta-ethnography, which makes this review unique. One drawback would be that a multifaceted search was not conducted; the search was limited to the electronic databases available. As is generally held, the non-randomized and observational nature of the review articles could have overestimated the beneficial effects of reconfiguration. Finally, overestimation of the effectiveness of the service intervention could also result from pooling the results of published studies only.
9. Conclusion
Our findings indicate that nosocomial Covid-19 presents a big challenge in single-site service. However, time to theatre was significantly prolonged with the dual-site service, accounted for by the logistical challenges of transferring patients to the operating site. Nevertheless, patients stayed longer in hospital with the dual-site service, despite making it to the theatre faster. No statistical difference in mortality was noted between the two service provisions, and discharge destinations remained largely unchanged with either configuration. In view of the above findings, it appears that the two-site service delivery fared better in terms of infection control and clinical outcomes, despite the longer times to theatre.
It appears to be the general consensus among authors that it is safe and feasible to perform time-sensitive, as well as elective surgeries, at a dedicated Covid-free site. As several SARS-CoV-2 variants have been reported recently that display higher transmissibility and resistance to immunity induced by natural infection or vaccination, there is a potential for more Covid-19 surges, wherein healthcare systems are likely to be severely tested again. The split-site organizational system is a valid infection control measure that efficiently safeguards the continuity of hospital services, while reducing adverse clinical outcomes.
Ethical approval
Institutional and Ethical approval has been obtained from UHL Research and Development department and registered with the trust (Audit Number 10506).
Location
University Hospitals of Leicester, University Hospitals of Leicester, Infirmary square, Leicester, LE1 5WW, United Kingdom.
Declaration of competing interest
None of the authors have any conflicts of interest to declare. The study has been performed in accordance with the ethical standards of the institutional and Health Research Authority guidelines, as well as the Declaration of Helsinki and its further amendments.
Acknowledgments
The authors acknowledge the help of Ms. Susan Court (NHFD Audit Clerk UHL) for her invaluable help and good humour, Ms. Jane Cooper (Richmond Library NGH) and Mr. Peter Roberts (Information Officer UHL) for all the help in data collection. We thank all the medical professionals untiringly fighting epidemic outbreaks in healthcare facilities all over the world.
Contributor Information
Milan Muhammad, Email: milan.valiyakath@nhs.net.
Sarah Ayton, Email: sarah.ayton@uhl-tr.nhs.uk.
Shruthi Hejmadi, Email: shruthibipin@hotmail.com.
Jatinder S. Minhas, Email: jm591@le.ac.uk.
Nicolette Morgan, Email: nicolette.morgan@uhl-tr.nhs.uk.
Anna C. Peek, Email: anna.peek@uhl-tr.nhs.uk.
References
- 1.Natl. Hip Fract. Database. 2019. National hip fracture database annual report. [Google Scholar]
- 2.British Orthopaedic Association Trauma Committee British Orthopaedic Association's Standards for Trauma (BOAST): care of the older or frail patient with orthopaedic injuries. Injury. 2020 doi: 10.1016/j.injury.2020.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Vlastos D. The impact of COVID-19 pandemic on aortic valve surgical service: a single centre experience. 2021. [DOI] [PMC free article] [PubMed]
- 4.Bonalumi G., Giambuzzi I., Barbone A., et al. A call to action becomes practice: cardiac and vascular surgery during the COVID-19 pandemic based on the Lombardy emergency guidelines. Eur J Cardio Thorac Surg. 2020;58:319–327. doi: 10.1093/EJCTS/EZAA204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wickramarachchi L., Peters J., Thakrar A., et al. A dual-site trauma system during COVID-19 pandemic – our experience in a high-risk area with 60-day mortality report. J Orthop. 2021;24:42–46. doi: 10.1016/J.JOR.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emma Picardo N., Walker H., Vanat Q., et al. Service reconfiguration in the department of hand surgery during the UK COVID-19 lockdown: Birmingham experience. Postgrad Med. 2021;97:532–538. doi: 10.1136/postgradmedj-2020-139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiesa R., Kahlberg A., Rinaldi E., Mascia D. Emergency management of the COVID-19 pandemic in a vascular surgery department of a large metropolitan hospital in Italy. Preparation, escalation, de-escalation, and normal activity. J Card Surg. 2021;36:1632–1636. doi: 10.1111/JOCS.14999. [DOI] [PubMed] [Google Scholar]
- 8.Collins P.M., Madden A., O'Connell C., et al. Urological service provision during the COVID-19 period: the experience from an Irish tertiary centre. Ir J Med Sci. 2021;190:455–460. doi: 10.1007/S11845-020-02352-X/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim J., Rehman H., Gaba S., et al. Orthopaedic assessment unit: a service model for the delivery of orthopaedic trauma care in a major trauma centre during the global pandemic (COVID-19) 2021. 101308/rcsann20207069 103:167–172. [DOI] [PMC free article] [PubMed]
- 10.Ramsingh R.A.E., Duval J.L., Rahaman N.C., et al. Adult cardiac surgery in Trinidad and Tobago during the COVID-19 pandemic: lessons from a developing country. J Card Surg. 2020;35:3387–3390. doi: 10.1111/JOCS.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kasivisvanathan V., Lindsay J., Rakshani-Moghadam S., et al. Evaluation of 30-day mortality for 500 patients undergoing non-emergency surgery in a COVID-19 cold site within a multicentre regional surgical network during the COVID-19 pandemic. medRxiv. 2020 doi: 10.1101/2020.06.10.20115543. 2020.6.10.20115543. [DOI] [Google Scholar]
- 12.Iqbal M.R., Dhahri A.A., Darwish N.M.M., Vijay V. Single centre concept of ‘cold site’ elective surgery during the peak of COVID-19 pandemic : a cohort study. Ann Med Surg. 2020;59:245–250. doi: 10.1016/J.AMSU.2020.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stroman L., Russell B., Kotecha P., et al. Safety of “hot” and “cold” site admissions within a high-volume urology department in the United Kingdom at the peak of the COVID-19 pandemic. Bjui Compass. 2021;2:97. doi: 10.1002/BCO2.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chui K., Thakrar A., Shankar S. Evaluating the efficacy of a two-site (‘COVID-19’ and ‘COVID-19-free’) trauma and orthopaedic service for the management of hip fractures during the COVID-19 pandemic in the UK. Bone Jt Open. 2020;1:190–197. doi: 10.1302/2633-1462.16.BJO-2020-0035.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dayananda K.S.S., Mercer S.T., Agarwal R., et al. A comparative review of 1,004 orthopaedic trauma patients before and during the COVID-19 pandemic. Bone Jt Open. 2020;18(1):568–575. doi: 10.1302/2633-1462.19.BJO-2020-0121.R1. (8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang J.S., Wignadasan W., Pradhan R., et al. Elective orthopaedic surgery with a designated COVID-19-free pathway results in low perioperative viral transmission rates. Bone Jt Open. 2020;1:562. doi: 10.1302/2633-1462.19.BJO-2020-0110.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Covids Collaborative. Elective cancer surgery in COVID-19 free surgical pathways during the SARS-CoV-2 pandemic: an international, multi-centre, comparative cohort study. Eur J Surg Oncol. 2021;47:e3–e4. doi: 10.1016/J.EJSO.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ally M., Patel A., Tanna R., et al. Elective ENT surgery during the COVID-19 pandemic: experience from a single UK centre. J Perioperat Pract. 2021;31:407–411. doi: 10.1177/17504589211021264. [DOI] [PubMed] [Google Scholar]
- 19.Kuusk T., Cullen D., Neves J.B., et al. Impact of the first surge of the COVID-19 pandemic on a tertiary referral centre for kidney cancer. BJU Int. 2021;128:752–758. doi: 10.1111/BJU.15441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanna J., Khoory C., Manu N., et al. 1288 colorectal cancer surgery service provision during the COVID-19 pandemic: an assessment of a single trust. Br J Surg. 2021;108 doi: 10.1093/BJS/ZNAB259.426. [DOI] [Google Scholar]
- 21.Ghosh S., Nevins E.J., Hicks G.J., et al. Colorectal cancer care in the COVID-19 Era;Keep calm and carry on? Colorectal Dis. 2021;23 doi: 10.1111/CODI.15825. 74–74. [DOI] [Google Scholar]
- 22.Hamid M., Digne-Malcolm H., Kanwal A., et al. Maintaining elective colorectal surgery during the COVID-19 pandemic. Colorectal Dis. 2021;23 doi: 10.1111/CODI.15825. 54–54. [DOI] [Google Scholar]
- 23.D'Angelo F., Monestier L., De Falco G., et al. Management of traumatology patients during the coronavirus (COVID-19) pandemic: experience in a Hub trauma hospital in Northern Italy. Indian J Orthop. 2020;54:397–402. doi: 10.1007/S43465-020-00282-5/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dayananda KSS COVID-19 The impact and changes to trauma services in cardiff. https://www.boa.ac.uk/resources/knowledge-hub/covid-19-the-impact-and-changes-to-trauma-services-in-cardiff.html
- 25.Synthesis without Meta-Analysis (SWiM) in Systematic Reviews: Reporting Guideline Supplementary File 2 Table S1 Examples Illustrating Synthesis without Meta-Analysis Reporting Items.
- 26.Kumar Jain V., Lal H., Kumar Patralekh M., Vaishya R. Fracture management during COVID-19 pandemic: a systematic review. J Clin Orthop Trauma. 2020;11:S431–S441. doi: 10.1016/J.JCOT.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nuñez J.H., Sallent A., Lakhani K., et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51:1414–1418. doi: 10.1016/J.INJURY.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benazzo F., Rossi S.M.P., Maniscalco P., et al. The orthopaedic and traumatology scenario during Covid-19 outbreak in Italy: chronicles of a silent war. Int Orthop. 2020 doi: 10.1007/s00264-020-04637-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sobti A., Memon K., Bhaskar R.R.P., et al. Outcome of trauma and orthopaedic surgery at a UK district general hospital during the covid-19 pandemic. J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mariconda M., Costa G.G., Cerbasi S., et al. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Jt J. 2015 doi: 10.1302/0301-620X.97B3.34504. [DOI] [PubMed] [Google Scholar]
- 31.Kim S.M., Moon Y.W., Lim S.J., et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012 doi: 10.1016/j.bone.2012.02.633. [DOI] [PubMed] [Google Scholar]
- 32.Nyholm A.M., Gromov K., Palm H., et al. Time to surgery is associated with thirty-day and Ninety-day mortality after proximal femoral fracture. J Bone Jt Surg-Am. 2015 doi: 10.2106/jbjs.o.00029. [DOI] [PubMed] [Google Scholar]
- 33.Rosso F., Dettoni F., Bonasia D.E., et al. Prognostic factors for mortality after hip fracture: operation within 48 hours is mandatory. Injury. 2016 doi: 10.1016/j.injury.2016.07.055. [DOI] [PubMed] [Google Scholar]
- 34.Smith T., Pelpola K., Ball M., et al. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014 doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 35.Chang W., Lv H., Feng C., et al. Preventable risk factors of mortality after hip fracture surgery: systematic review and meta-analysis. Int J Surg. 2018 doi: 10.1016/j.ijsu.2018.02.061. [DOI] [PubMed] [Google Scholar]
- 36.Espinosa K.A., Gélvez A.G., Torres L.P., et al. Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country. Injury. 2018 doi: 10.1016/j.injury.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Young T.B., Gibbs A.C.C. Prognostic factors for the elderly with proximal femoral fracture. Arch Emerg Med. 1984 doi: 10.1136/emj.1.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scottish Itercollagiate Guidelines Network Management of hip fracture in older people. (SIGN Guideline No 111) Scottish Itercollagiate Guidel Netw. 2009;49 [Google Scholar]
- 39.Patczai B., Juhász K., Bűcs G., et al. Non-operative predictors for subsequent interventions after intracapsular femoral neck fractures in elderly: a comprehensive analysis of the Hungarian nationwide health insurance database. Injury. 2020 doi: 10.1016/j.injury.2020.02.055. [DOI] [PubMed] [Google Scholar]
- 40.Sheehan K.J., Sobolev B., Guy P. Mortality by timing of hip fracture surgery: factors and relationships at play. J Bone Jt Surg Am. 2017 doi: 10.2106/JBJS.17.00069. [DOI] [PubMed] [Google Scholar]
- 41.Vochteloo A.J.H., Moerman S., Tuinebreijer W.E., et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013 doi: 10.1111/j.1447-0594.2012.00904.x. [DOI] [PubMed] [Google Scholar]
- 42.Dubljanin-Raspopović E., Marković-Denić L., Marinković J., et al. Does early functional outcome predict 1-year mortality in elderly patients with hip fracture? Hip. Clin Orthop Relat Res. 2013 doi: 10.1007/s11999-013-2955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kayani B., Onochie E., Patil V., et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt J. 2020 doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. [DOI] [PubMed] [Google Scholar]
- 44.Ruan Q., Yang K., Wang W., et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Egol K.A., Konda S.R., Bird M.L., et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York city perspective. J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LeBrun D.G., Konnaris M.A., Ghahramani G.C., et al. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J., et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic. J Bone Jt Surg. 2020 doi: 10.2106/jbjs.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mi B., Chen L., Xiong Y., et al. Characteristics and early prognosis of covid-19 infection in fracture patients. J Bone Jt Surg - Am. 2020 doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Catellani F., Coscione A., D'Ambrosi R., et al. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in Northern Italy. J Bone Joint Surg Am. 2020 doi: 10.2106/JBJS.20.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hall A.J., Clement N.D., MacLullich A.M.J., et al. IMPACT-Scot 2 report on COVID-19 in hip fracture patients. Bone Joint Lett J. 2021:1–10. doi: 10.1302/0301-620x.103b.bjj-2020-2027.r1. [DOI] [PubMed] [Google Scholar]
- 51.Dupley L., Oputa T.J., Bourne J.T., et al. 30-day mortality for fractured neck of femur patients with concurrent COVID-19 infection. Eur J Orthop Surg Traumatol. 2020 doi: 10.1007/s00590-020-02778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Narang A., Chan G., Aframian A., et al. Thirty-day mortality following surgical management of hip fractures during the COVID-19 pandemic: findings from a prospective multi-centre UK study. Int Orthop. 2020 doi: 10.1007/s00264-020-04739-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thakrar A., Chui K., Kapoor A., Hambidge J. Thirty-day mortality rate of patients with hip fractures during the COVID-19 pandemic: a single centre prospective study in the United Kingdom. J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Malik-Tabassum K., Crooks M., Robertson A., et al. Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom. J Orthop. 2020 doi: 10.1016/j.jor.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Magro F., Perazzo P., Bottinelli E., et al. Managing a tertiary orthopedic hospital during the COVID-19 epidemic, main challenges and solutions adopted. Int J Environ Res Publ Health. 2020;17:4818. doi: 10.3390/IJERPH17134818. 2020, 4818 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Søreide K., Hallet J., Matthews J.B., et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. 2020. [DOI] [PMC free article] [PubMed]
- 57.Mouton C, Hirschmann MT, Ollivier M, et al COVID-19-ESSKA guidelines and recommendations for resuming elective surgery. 10.1186/s40634-020-00248-4. [DOI] [PMC free article] [PubMed]
- 58.Al-Omar K., Bakkar Sohail, Khasawneh Laith, et al. Resuming elective surgery in the time of COVID-19: a safe and comprehensive strategy. Updates Surg. 2020;72:291–295. doi: 10.1007/s13304-020-00822-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Covids Collaborative, Bhangu A., Lawani I., et al. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/BJS.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boyle J.M., Kuryba A., Blake H.A., et al. The impact of the first peak of the COVID-19 pandemic on colorectal cancer services in England and Wales: a national survey. Colorectal Dis. 2021;23:1733–1744. doi: 10.1111/CODI.15622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kuryba A., Boyle J.M., Blake H.A., et al. Surgical treatment and outcomes of colorectal cancer patients during the COVID-19 pandemic: a national population-based study in England. Ann Surg. 2021 doi: 10.1097/AS9.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lei S., Jiang F., Su W., et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClin Med. 2020;21:100331. doi: 10.1016/J.ECLINM.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bhangu A., Lawani I., Ng-Kamstra J.S., et al. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/BJS.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]