Abstract
Health care delivery shifted and adapted with the COVID-19 pandemic caused by the novel severe acute respiratory syndrome coronavirus 2. Stroke care was negatively affected across the care continuum and may lead to poor community living outcomes in those who survived a stroke during the ongoing pandemic. For instance, delays in seeking care, changes in length of stays, and shifts in discharge patterns were observed during the pandemic. Those seeking care were younger and had more severe neurologic effects from stroke. Increased strain was placed on caregivers and public health efforts, and community-wide lockdowns, albeit necessary to reduce the spread of COVID-19, had detrimental effects on treatment and recommendations to support community living outcomes. The American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group Health and Wellness Task Force convened to (1) discuss international experiences in stroke care and rehabilitation and (2) review recently published literature on stroke care and outcomes during the pandemic. Based on the findings in the literature, the task force proposes recommendations and interdisciplinary approaches at the (1) institutional and societal level; (2) health care delivery level; and (3) individual and interpersonal level spanning across the care continuum and into the community.
Keywords: COVID-19, Delivery of health care; Rehabilitation; Stroke; Stroke rehabilitation
List of abbreviations: CoV, coronavirus; PPE, personal protective equipment; SARS, severe acute respiratory syndrome
Statement of purpose
The COVID-19 pandemic caused by the novel severe acute respiratory syndrome (SARS) coronavirus (CoV) 2 posed unprecedented challenges to health care systems around the world. It is expected that the fallout from the COVID-19 pandemic will directly affect people who experience stroke during this time. The Health and Wellness Task Force within the American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group is concerned that during the ongoing pandemic, fewer people are seeking stroke care, and more people with stroke are living with the effects of untreated stroke or being discharged with minimal rehabilitation or without critical early and intensive rehabilitation that is recommended for improving stroke outcomes.1 The purpose of this position article is to describe ongoing challenges and opportunities to support the short- and long-term needs of people surviving stroke during the COVID-19 pandemic. The task force proposes potential solutions across the care continuum to support a multilevel and interdisciplinary approach that addresses this major public health problem.
Rationale for position paper
Enduring a stroke during the pandemic
Before the COVID-19 pandemic, stroke was widely regarded as a leading global cause of disability2, 3, 4 and the second leading cause of death (11.6% of global mortality).5 Despite advancements in medical interventions that increased stroke survival, disparities in stroke mortality and disability were prevalent, partly because of differences in country income and medical care quality (eg, cost, access, availability).3 The COVID-19 pandemic presented an additional risk factor for stroke: COVID-19 infection. While there is no exact mechanism linking COVID-19 to stroke, vascular symptoms associated with COVID-19 such as hypercoagulability and arterial and venous thrombosis are believed to be contributing factors to increased risk of stroke.6 , 7 Other coronavirus respiratory syndromes of the same nature including the SARS-CoV-1 and Middle East Respiratory Syndrome coronavirus were also related to increased incidence of acute ischemic stroke.7 Further, people with stroke risk factors (eg, diabetes, smoking) have an increased COVID-19 mortality rate, possibly because of the same mechanisms attributed to stroke risk, such as large expression of angiotensin-converting enzyme 2 cell receptors for binding to SARS-CoV-2.8
Common deficits after stroke include impaired motor function; impaired ability to carry out activities of daily living; cognitive impairments in memory, language, attention, and executive function; and affected mood, sensation, and perception.9 , 10 Stroke attributed to the SARS-CoV-2 infection can cause greater severity of stroke,11 potentially leading to prolonged acute care and rehabilitation.12 Natural recovery of broad stroke-related impairments often occurs with haste within the first 6 months post stroke and then tends to plateau, although this may vary for cognitive, physical, and sensory-perceptual impairments.13 It is difficult to predict individual recovery because sequelae are multifaceted across multiple domains. As such, rehabilitation clinicians rely on their own judgment as to when to end rehabilitation post stroke.13 The long-term effects and recovery trajectory for individuals with simultaneous SARS-CoV-2 infection and stroke is unknown.
Stroke care
Before the COVID-19 pandemic, patients with stroke symptoms received hyperacute and acute treatment at the nearest specialist stroke unit, primary stroke center, or comprehensive stroke center.14 After acute treatment, the patient entered 1 of 2 main pathways for poststroke rehabilitation: (1) subacute rehabilitation (eg, inpatient rehabilitation, skilled nursing facility); or (2) community rehabilitation, normally delivered via an outpatient facility or in the patient's home.15 A large-scale RCT of working-aged survivors of stoke across the UK, Australia, and Southeast Asia found that within 3 months post stroke, 67% of survivors of stroke received either inpatient or community rehabilitation, and only 8% of those were still receiving rehabilitation 12 months post stroke.15 Those with milder strokes had the highest rates of receiving no rehabilitation (40%), followed by a lower proportion of those with moderate strokes (12%) and severe strokes (4%) who required no rehabilitation.15
During the pandemic, regions with high incidence of COVID-19 were forced to reorganize health care services. This included implementation of triage systems, separating patients with confirmed or suspected COVID-19 from patients without COVID-19 and redeploying health care professionals to the frontline to deal with the influx of patients with COVID-19.16, 17, 18 Resources and clinicians were spread across usual clinical care and COVID-19 specific care, increasing the potential short- and long-term negative consequences of high stress and burnout.19 An overwhelmed health care system, attributed to reassignment of staff or beds, increased patient admissions without adequate staffing, and increased resource strain, likely led to care and service limitations.20
Overarching rationale
Given the substantial number of adults enduring stroke annually, it is necessary to understand and address their needs during the ongoing COVID-19 pandemic. While it is well-documented that interdisciplinary stroke rehabilitation can enhance outcomes after stroke, the substantial shift in health care delivery during the COVID-19 pandemic may have major effects on short- and long-term outcomes. Researchers must further examine stroke outcomes related to the COVID-19 pandemic. Practitioners must be prepared to identify problems and challenges among this population to address the fallout the pandemic has imparted on a generation of survivors of stroke.
Health care delivery during the COVID-19 pandemic
Delays in stroke care
There was a reduction in the number of patients seeking medical emergency care for stroke, particularly at the start of the pandemic.21 Recent data demonstrates an average decrease in stroke presentation of 15.3% per week in 2020 compared with 2019.22 This may be because of the fear of acquiring COVID-19 during hospital stays.23 Additionally, patients who survived stroke and present with a clinical indication for inpatient rehabilitation may decline care related to fear of contagion or fewer choices related to bed allocation in community facilities. Although stroke is considered a medical emergency that requires immediate treatment and patients with acute stroke continue to receive immediate care during the pandemic, several problems exist across the care continuum that may restrict patients’ access to necessary treatment across the continuum of care and lead to poor long-term outcomes.
Emergency departments often rerouted patients with stroke, limiting access to acute stroke diagnostic testing. This sometimes left other areas of the hospital or stroke centers to allocate already strained resources and staff to treat patients with stroke.24 Some hospitals converted nontraditional spaces (eg, meeting rooms, hallways) to inpatient units to handle surges in patients.20 During the ongoing pandemic, a delay in acute and postacute rehabilitation care was observed. Sielger et al25 completed a single tertiary stroke care center study and discovered a reduction in new stroke diagnosis (38% reduction) and mild stroke presentation (29% reduction) through emergency services. However, the study also demonstrated a proportional doubling of severe stroke presentation (38% vs 21%) during the same period. Emergency services for patients with stroke were and continue to be compromised, which could translate to poor outcomes.
Some people experiencing stroke symptoms may not seek health care. In a recent study, 53% of participants with stroke reported missed or delayed health care visits.26 For instance, people who experience mild symptoms, such as subtle aphasia or paresis, may have been unaware of their deficit. With social isolation related to public health measures designed to mitigate the spread of COVID-19, these individuals may have lacked awareness and social support required to seek care for these problems.23
Length of stay
Hospital lengths of stay are an indicator of efficiency, but during the pandemic, changes in length of stay were observed among some patients with stroke. First, the reallocation of stroke beds to patients with COVID-19, redeployment of stroke physicians and health care teams to look after patients, the delay in intravenous thrombolysis access, and the reduction of patients entering hospitals all potentially contributed to increased severity of patients with stroke27 and subsequently increased lengths of stay. Alternatively, a significantly shorter length of stay was observed for patients with coronary symptoms during the COVID-19 era compared with records from a prepandemic period.28 Some observational studies concluded no change to quality of care indicators such as hospital length of stay, rate of successful reperfusion after thrombectomy, and good clinical outcome rates after discharge from hospitalization compared with hospital data from 2019.29 However, an analysis form Get With The Guidelines Stroke registry from more than 2000 hospitals and 81,084 patients in the US found a decreased odds of length of stay >4 days during the COVID-19 pandemic.22 Nonetheless, each site or center across the globe is different and may observe various differences in length of stay.
Discharge to postacute care
Several observational studies report changes in postacute care discharge patterns. Although discharge to inpatient rehabilitation remained relatively unchanged, more patients were discharged to hospice or home, with fewer discharged to skilled nursing facilities, likely triaging patients away from high-risk COVID-19 environments.22 Additionally, home health care and outpatient therapies were often limited. A study of home health and home aid agencies in the Northeastern US showed a 98.7% reduction in requests for in-home services secondary to caution with face-to-face contact, resulting in family caregivers assuming additional roles.30 The majority of candidates for home health services are older than 65 years and have at least 1 comorbidity increasing their risk of infection.31 Home health services experienced greater demand for personal protective equipment (PPE) and disinfecting procedures, social distancing guidelines, and staffing shortages because of staff COVID-19 infections, triggering a reduction of provided services.30 Service reduction may prompt greater delay of care in a population of people with stroke where recovery is heightened within the first 3-6 months.
Potential effects on stroke outcomes
Individual and interpersonal level: worse outcomes for survivors of stroke with COVID-19
Patients affected by COVID-19 have increased risk of cerebrovascular events because of inflammatory responses and thrombotic risks.29 , 32 It has been documented that stroke severity is significantly different at discharge from hospitalization between patients with and without COVID-19, where patients with the virus had higher National Institute of Health Stroke Scale scores indicating more neurologic impairment, higher risk for severe disability, and death. A multicenter cohort study in Spain found that despite similar acute management of stroke, patients with COVID-19 had greater stroke severity and greater level of disability and dependency at discharge.33 Similar, a recent study found that patients presenting with COVID-19 who had a history of stroke have shown more severe clinical symptoms and worse outcomes than those without history of stroke.34
Individual and interpersonal level: younger acute stroke presentations
The demographic of patients presenting to emergency departments has shifted. Patients presenting for acute stroke are younger. A rapid review concluded that age of stroke onset has decreased globally and there is an association between COVID-19 and stroke in young populations without the typically occurring vascular risk factors.35 Rudilosso et al29 also observed this trend but speculated older adults may be seeking stroke care less frequently out of fear for acquiring COVID-19, which has been shown to have a higher mortality rate in this population.
Systems-level effects contributing to stroke outcomes
Increased stress has been placed on the health care system to face long-term sequelae of COVID-19. The reorganization of stroke care during the COVID-19 pandemic has led to reduced access to intravenous thrombolysis and the stop of “nonurgent” care.27 In a recent global observational study, stroke care was observed to have a global decline across 124 centers with high, mid-, and low COVID-19 hospitalization burden.36 Centers with higher COVID-19 inpatient volumes were noted to have more decline in stroke care. In addition, the stroke care centers with high and midvolumes demonstrated a more profound volume decline in stroke hospitalization, potentially “related to the fact that larger centers were more likely to become the preferred destination for COVID-19 referrals leading to capacity issues.”36 (p578) The scarcity of resources further limited access to stroke care to patients with COVID-19 and stroke. This has created increased stress to families, caregivers, and stroke health care professionals to provide optimal medical care and rehabilitation services.
Home and community
Adults with stroke often need supplementary support to optimize their independence in their home and to promote safe and successful community reentry. These necessary supports in the home and community include postacute care, paid and family caregivers, alternative options for transportation, social support groups, and other accessible community areas integrated into daily routines. The COVID-19 pandemic affected various levels of participation in daily routines and access in both home and community environments for those surviving strokes37; closing nonessential businesses, social distancing, and reducing face-to-face contact were among chief contributors to disadvantaged access and participation.
Caregivers, both paid and unpaid, afford people living with the effects of stroke the opportunity to live in preferred and less restrictive environments. During the pandemic, caregivers received inadequate training on procedures to minimize transmission and experienced limited communication with health care professionals as they assumed varied roles secondary to reduced home- and community access.38 Caregivers experienced high levels of depression and stress, sometimes more frequently than people with stroke.39 Less support from external sources, increased roles and care demands, and stress of the pandemic all coalesce to reduce overall quality of care for people with stroke.
Potential problems related to public health efforts
People surviving stroke during the pandemic may experience additional unanticipated complications during their recovery as a result of pandemic-related social distancing guidelines, mask mandates, and community lockdowns. These public health efforts, albeit necessary, have likely restricted recovery and community reintegration for various reasons. The Centers for Disease Control and Prevention in the US defined guidelines within community, work, and school settings to reduce transmission of the disease.40 Clear guidelines and restrictions in community gatherings, compounded by increased risk of transmission for those with reduced immunity, presented barriers for community reentry and engagement for those with stroke. These restrictions, including closing of businesses, restrictions on public transportation, and reduction of free community-based services, resulted in a vast and abrupt change to community-based routines and patterns and greater isolation from social interactions.41
Increasing community engagement after stroke presents a myriad of challenges,42 including barriers to engagement because of changes in mobility and self-efficacy with balance,43 cognitive44, language and visual impairment; reduced access to transportation; and psychosocial factors, such as reduced confidence with self-image.45 However, community reentry is often a goal for people with stroke and is valued as a mark of independence as well as a modality for continuity of holistic maintenance and remediation of various personal functions.
Closure of nonessential businesses and distancing mandates, varying by geographic location and times of increased transmission, further reduced opportunities for community activities such as exercising at a gym, attending in-person support groups, and physician office visits are all means of secondary prevention for stroke and other health conditions. Although technology became increasingly available to compensate for social distancing requirements, lacking device access and difficulty navigating different platforms further reduced accessibility to varied social circles and resources outside of the home. Complications associated with unmet needs and desires in any of these areas are correlated with greater risk of depression and social isolation as well as increased mortality rate, specifically among people living with the effects of stroke.46 , 47
Ongoing efforts to reduce the spread of the virus may be contributing to the exacerbation of disability for individuals with stroke. For instance, mask wearing may contribute to challenges for people with (1) communication impairments after stroke such as aphasia or apraxia of speech; and (2) heightened risk of falls post stroke where visual fields may be obstructed by the mask itself. Another example is the effect of social distancing and isolating on function. For instance, approximately 84% of people with stroke experience significant cognitive impairment 4 years post onset.48 , 49 Although this area needs further study, it is critical that health care providers are aware of the potential double threat people with stroke may have for developing dementia during the pandemic because of neurocognitive impairments paired with social isolation. With fewer opportunities for participation, people returning to community living after stroke may be living more sedentary and isolated lifestyles, in turn creating negative health effects.50
Because of the ongoing pandemic waves and global public health efforts, our taskforce posits that people with stroke may encounter the following challenges: (1) decreased social and instrumental support; (2) loss or decrease of financial resources; (3) less opportunities to engage with peers or support groups focused on supporting life after stroke; (4) stress-related shifts in housing affordability with increased costs and moratoriums ending;(5) decreased physical health because of restrictions or fear for personal safety in public places such as gyms or other venues aiming at health and wellness; and (6) increased anxiety and depression.
Call for action
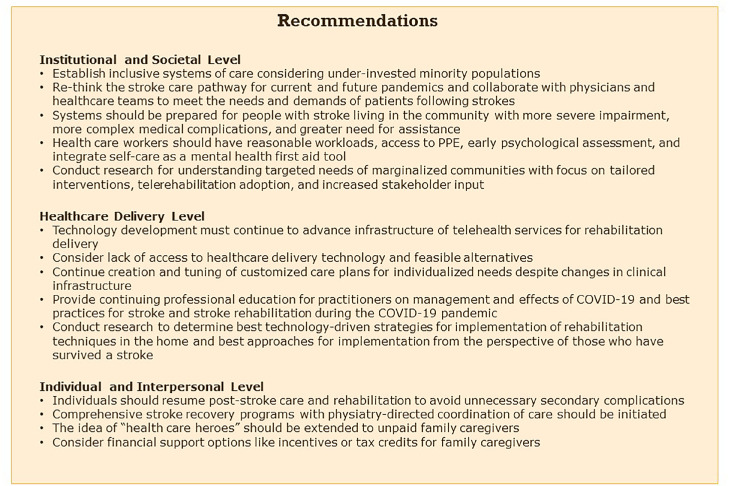
Our task force has identified several opportunities to address the needs of this population at the (1) institutional and societal level, (2) health care delivery level, and (3) individual and interpersonal level.
Institutional and societal level
Social determinants of health
The importance of achieving health equity for people living with the effects of stroke cannot be underestimated. “Social determinants of health are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”51 (p1) Factors of social determinants of health include access to clean air and water, nutritious foods, physical activity opportunities, safe housing, modes of transportation, education, job opportunities, income, language and literacy skills. In addition, racism, discrimination, and other violence can also negatively affect a person's health, well-being, and quality of life. Those persons from underinvested groups often experience economic and social systemic barriers that are harmful to achieving full health equity (eg, racial and ethnic minority groups, individuals with disabilities, non-English speaking language).52 Intersectional identities may experience even more health inequities.
The COVID-19 pandemic has laid bare the gaps in the health care system that continue to contribute to worsening health inequities. Racial differences in stroke incidence were documented where the age-adjusted incidence of first ischemic stroke per 1000 was 0.88 in White individuals, 1.91 in Black individuals, and 1.49 in Hispanic individuals.53 Racial and ethnic disparities were also noted with respect to poststroke disability assessment tools and outcomes.54 It is apparent that COVID-19 disproportionately affects underinvested racial and ethnic minority groups across multiple domains.55, 56, 57 Rate ratios of COVID-19 cases compared with non-Hispanic White persons were 1.5 × in American Indian or Alaska Native persons, 0.7 × in Asian persons, 1.0 × in Black persons, and 1.5 × in Hispanic or Latino persons. Rate ratios of deaths related to COVID-19 compared with non-Hispanic White persons were 2.2 × in American Indian or Alaska Native persons, 0.8 × in Asian persons, 1.7 × in Black persons, and 1.9 × in Hispanic or Latino persons.58 The American Heart Association highlighted the need to adequately recognize structural racism as a fundamental cause of poor health and disparities in cardiovascular disease.59 As we work to establish a more inclusive system of care for survivors of stroke, “a growing body of evidence requires us to expand our understanding of the sociopolitical influences affecting social determinants of health, which impact the overall health status of patients from disproportionately impacted communities.”60 (p439) Increased research is critical for understanding specific and targeted needs of specific marginalized communities, including tailored stroke interventions, telerehabilitation adoptions, and increased stakeholder input from marginalized communities in research development.
Health authority and health care system opportunities
The COVID-19 pandemic has had a major effect on stroke care, including disruption to hospital stays (shortened or lengthened), patients presenting with greater severity strokes both related and unrelated to COVID-19 infection, and increased mortality rates of stroke in the first wave of the pandemic.61 During the subsequent waves of the pandemic, the burden eased slightly, including decreases in hospital stays, severity of stroke symptoms, and mortality rates in stroke.33
In response to rapid changes, health authorities who are responsible for regional health services should prepare and rethink the stroke care pathway for present and future pandemics and collaborate with physician leaders and allied health care teams to meet the needs and demands of patients after strokes. Health authorities should focus on long-term complications and sequelae management of survivors of stroke in the context of the COVID-19 pandemic because the neglect of care could exacerbate poor patient outcomes, increasing burden to the already stressed health care system.
Frontline health care workers have faced extreme challenges during the pandemic. Many stress factors, such as the fears of transmission, increased workload, inadequate PPE, the need of making ethically difficult decisions on the level of care, physical exhaustion, and even increased family responsibilities because of closed school and day care, may result in significant negative effects on health care workers’ physical and mental well-being. A recent meta-analysis suggests that prevalence rates of anxiety and depression among the health care workers are 23.2% and 22.8%, respectively,62 while insomnia prevalence is reaching 38.9% during the COVID pandemic. Nurses and female physicians are vulnerable to anxiety and depression.62
An urgent need exists to support health care workers’ emotional well-being and mental health during the pandemic. Reasonable workload and access to PPE are requisite needs. Evidence from previous pandemics suggests that early psychological assessment and intervention are particularly useful.63 , 64 Further, self-care as a mental health first aid tool may help health care workers to process stress and anxiety in the current era of the COVID pandemics.65
Be prepared for people with more severe impairments and needs in the community
Referral patterns and access to traditional poststroke care models were altered because of the COVID-19 pandemic. “Admission for stroke during the COVID-19 pandemic was associated with a significantly lower probability of being discharged to an inpatient rehabilitation facility.”66 (p1) As a result of rapid reductions in the immediate availability of health care providers and facilities, survivors of stroke may have experienced delayed care, shortened length of stay during inpatient care, and deviations from the standard of care according to established care models.67 Subsequently, survivors of stroke in the community may have more severe impairment, more complex medical complications, and greater needs for assistance.
Health care delivery level
Change in delivery after acute hospitalization
Changes in health care have created opportunities to advance secondary prevention and empower patients to self-manage after hospitalization. Focusing on self-management has been trending in stroke rehabilitation in recent years and can be addressed face-to-face, via telehealth or remote communication technologies, or through a hybrid approach where technology is complementary to skilled provider training.68 , 69
These remote communication technologies are regarded as effective options to support the delivery of health care interventions for neurorehabilitation. Examples of technologies leading these efforts include telemedicine, wearable sensors, smartphones, virtual reality, augmented reality, and rehabilitative games.26 , 70 In addition, strategy training intervention delivery was adapted for remote delivery integrating mobile health technology.70 Further research is warranted to determine best strategies for implementation of rehabilitation techniques in the home setting.
Increase the integration of evidence-based intervention programs and strategies such as telemedicine, telerehabilitation, and telepsychology across the continuum of care
Prior to the COVID-19 pandemic, remote telestroke services in the setting of acute stroke were frequently being used.71 , 72 Further down the continuum, a Cochrane Review published in 2020 found that telerehabilitation programs for stroke showed a reduction in depressive symptoms, enhanced quality of life, and improved independence in activities of daily living compared with usual care. Furthermore, outcomes were not inferior to face-to-face rehabilitation and telerehabilitation were cost-effective compared with traditional rehabilitation services.73 Telehealth and telerehabilitation were viable alternatives to in-person visits during the height of the COVID-19 pandemic for individuals with stroke.26 Isolation precautions during the pandemic forced the rapid expansion and integration of remote clinical care services through platforms such as video conferencing and mobile applications. Although patients with stroke-related deficits may require assistance to use the technology, advances in telehealth show the potential to provide access to health care that was once only offered in person.
While individuals are relatively satisfied with telehealth use, telehealth is not a panacea, and effective implementation approaches have not been established.26 A common barrier to use of telehealth is difficulty with technology use.26 , 74 Adaptation for remote delivery should be done with consideration to methods for training end users on new technology use and the intervention.75 Concerns about the Digital Divide, the gulf between individuals or groups who can access internet and those who cannot,76 further exacerbate what services may be available to patients. Health care providers must not overlook existing health care disparities that limit access to this technology. Social determinants that affect telehealth access include economic stability (ability to access internet-capable devices), education (literacy and digital literacy), social and community contexts (expectations of the person to use electronic internet devices), and the built environment (infrastructure for free or paid internet service).77
Nonetheless, technology to support telehealth services after stroke is becoming ubiquitous as the population continues to own smartphones and use applications frequently throughout the day.69 , 78 In multiple studies, remote telehealth services have proven easy to use, have used less resources (eg, transportation, time off from work), and have been well received by patients, caregivers, and clinical staff under the appropriate circumstances.79 , 80 Whether in person or virtual, support to be encouraged includes stroke rehabilitation therapies, maintaining a healthy lifestyle, physical activity, and preserving social networks.27 , 67 , 81 , 82 It is necessary that technology development teams continue to advance the infrastructure of telehealth services to provide opportunities for high-quality rehabilitation service delivery. Hospitals and clinics should continue to invest in state-of-the-art and state-of-the-science technologies, particularly because future pandemic waves are expected. Providers should continue to familiarize themselves with up-to-date advances in the technology and service delivery to provide high-quality care to people surviving stroke during and after the pandemic. Future research is needed to understand the best approaches to implement telerehabilitation from the perspective of those that have survived stroke.
Stroke and disability management, infection control, customization of care plan
Stroke care delivery during the COVID-19 pandemic has been challenged to incorporate infection control protocols across different settings to maintain safety of patients and clinical personnel. PPE such as masks, gloves, goggles, face shields, nonporous gowns, caps, shoe covers, and filtering respirator have been used as a standard practice for personal safety during clinical interaction. Prehospital and hospital stroke clinical care teams adjusted to use of diagnostic testing, incorporating extra time for sanitizing between patients, requiring patients to wear masks if medically stable, and varying clinical staff work schedules because of redeployment, sickness, and quarantine. Changes in clinical infrastructure required frequent monitoring to remain compliant but also to provide stroke specific care to persons with deficits such as weakness, aphasia, vision deficits, and cognitive deficits.67 It is imperative to continue the creation and modification of a customized care plan specific to the needs of each individual.
Professional development at all health care levels
With the rapid changes in knowledge brought on by the pandemic, it is important that continuing professional education be intentionally incorporated within professional knowledge requirements that provides updates on the management of patient with and living with the effects of COVID-19. Multidisciplinary teams involved in stroke care including physicians, physician assistants, nurses, physical therapists, occupational therapists, speech-language pathologists, psychologists, recreational therapists, vocational therapists, dieticians, and social workers will require advanced knowledge and adjustments to health care delivery in the setting of a pandemic. Professional societies and stroke-specific organizations have invested in developing resources for patients, caregivers, and professional staff.67 Additional research will help elucidate best practices for stroke and stroke rehabilitation during the COVID-19 pandemic.
Individual and interpersonal level
If decline in function is observed, actively pursue/resume therapy services
Many individuals with stroke had a decline in function across multiple domains during the COVID-19 pandemic because of quarantine isolation, closure of outpatient rehabilitation or fitness center facilities, and absence of available community resources.67 When possible, individuals should resume poststroke care and rehabilitation as soon as possible to continue stroke recovery and avoid unnecessary secondary complications (eg, worsening spasticity, diminished balance increasing fall risk). A comprehensive stroke recovery program including physiatry-directed coordination of care and “integrating modified cardiac rehabilitation may potentially benefit from reductions in all-cause mortality and improvements in cardiovascular performance and function.”74 , 83 (p953)
Support persons and caregivers as health care heroes
The idea of “health care heroes” should extend to caregivers who had to suddenly shift and take on or adjust to a system that was already strained with little additional resources. With the need for social distancing, many survivors of stroke found themselves in a position where they were unable to (1) have hired help enter their home; or (2) leave their home to access community services.67 The result was that family or friends suddenly had to take on the role of “caregiver” or “care partner” to fill the gap of required care. These nonprofessional caregivers were challenged with performing activities such as toileting, dressing, grooming, bathing, transfers, ambulation, meal preparation, medication management, and laundry services. During the pandemic and lockdown periods, many transportation options were not available. Tasks such as grocery shopping, attending medical and dental visits, and assistance to participate in social activities were also thrust on nonprofessional caregivers. Prior to the pandemic, individuals with chronic health conditions found the health care system under stress and difficult to navigate. Often not acknowledged, these caregivers should also be recognized as “health care heroes” for their sacrifice and courage to navigate a cumbersome health care system with few resources.67 Additional financial support options for caregivers supporting persons with stroke during the pandemic should be explored. For instance, advocacy for policies focused on providing monetary incentives or tax credits for family caregivers is important to support these “health care heroes.” Furthermore, additional research is needed on approaches to decrease caregiver burden and stress among this population (fig 1 ).
Fig 1.
Multi-level recommendations and interdisciplinary approaches.
Conclusions
People continue to endure stroke during the COVID-19 pandemic, and despite adaptations in health care, this population may be met with health care, policy, and social changes that influence their recovery. A generation of people who survived a stroke during this time may be living with additional fallout from the pandemic, which may include additional unmet and long-term needs. Practitioners must be prepared to meet the anticipated demand among this generation of survivors of stroke. It is critical that interdisciplinary health care providers are prepared to identify and address additional problems this population may encounter at any point across the care continuum but particularly within the context of the community. The work of the Health and Wellness Task Force propose recommendations for addressing the needs of this population at the (1) institutional and societal level; (2) health care delivery level; and (3) individual and interpersonal level. Future research is necessary to better understand the short- and long-term needs of people who survived a stroke during the COVID-19 pandemic.
Footnotes
Emily Kringle was supported by the National Heart Lung and Blood Institute of the National Institutes of Health under award no. K23 159240 during the development of this publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures: none.
References
- 1.Cadilhac DA, Prvu Bettger J. Health policy and health services delivery in the era of COVID-19. Stroke. 2021;52:2177–2179. doi: 10.1161/STROKEAHA.121.033292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Abajobir AA, Abate KH, et al. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38:208–211. doi: 10.1055/s-0038-1649503. [DOI] [PubMed] [Google Scholar]
- 4.Kim J, Thayabaranathan T, Donnan GA, et al. Global stroke statistics 2019. Int J Stroke. 2020;15:819–838. doi: 10.1177/1747493020909545. [DOI] [PubMed] [Google Scholar]
- 5.Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerotziafas GT, Catalano M, Colgan MP, et al. Guidance for the management of patients with vascular disease or cardiovascular risk factors and COVID-19: position paper from VAS-European Independent Foundation in Angiology/Vascular Medicine. Thromb Haemost. 2020;120:1597–1628. doi: 10.1055/s-0040-1715798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wijeratne T, Gillard Crewther S, Sales C, Karimi L. COVID-19 pathophysiology predicts that ischemic stroke occurrence is an expectation, not an exception—a systematic review. Front Neurol. 2021;11:1759. doi: 10.3389/fneur.2020.607221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi JY, Lee HK, Park JH, et al. Altered COVID-19 receptor ACE2 expression in a higher risk group for cerebrovascular disease and ischemic stroke. Biochem Biophys Res Commun. 2020;528:413–419. doi: 10.1016/j.bbrc.2020.05.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mayo NE, Wood-Dauphinee S, Ahmed S, et al. Disablement following stroke. Disabil Rehabil. 1999;21:258–268. doi: 10.1080/096382899297684. [DOI] [PubMed] [Google Scholar]
- 10.VanGilder JL, Hooyman A, Peterson DS, Schaefer SY. Post-stroke cognitive impairments and responsiveness to motor rehabilitation: a review. Curr Phys Med Rehabil Rep. 2020;8:461–468. doi: 10.1007/s40141-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: a systematic review and meta-analysis. Int J Stroke. 2021;16:137–149. doi: 10.1177/1747493020972922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walsh S, Brisson A, Flaherty R, Geller D, Tokash J, Kim GJ. Application of the ICF and the OTPF-4 to conceptualize the dual diagnosis of COVID-19 and stroke: implications for occupational therapy practice in acute and inpatient rehabilitation. Occup Ther Health Care, 2022; in press. [DOI] [PubMed]
- 13.Demain S, Wiles R, Roberts L, McPherson K. Recovery plateau following stroke: fact or fiction? Disabil Rehabil. 2006;28:815–821. doi: 10.1080/09638280500534796. [DOI] [PubMed] [Google Scholar]
- 14.Gittins M, Lugo-Palacios DG, Paley L, et al. How do patients pass through stroke services? Identifying stroke care pathways using national audit data. Clin Rehabil. 2020;34:698–709. doi: 10.1177/0269215520907654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walters R, Collier JM, Carvalho LB, et al. Exploring post acute rehabilitation service use and outcomes for working age stroke survivors (≤ 65 years) in Australia, UK and South East Asia: data from the international AVERT trial. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2019-035850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alquézar-Arbé A, Piñera P, Jacob J, et al. Impact of the COVID-19 pandemic on hospital emergency departments: results of a survey of departments in 2020 - the Spanish ENCOVUR study. Emergencias. 2020;32:320–331. [PubMed] [Google Scholar]
- 17.Cao Y, Li Q, Chen J, et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020;27:309–311. doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coughlan C, Nafde C, Khodatars S, et al. COVID-19: lessons for junior doctors redeployed to critical care. Postgrad Med J. 2021;97:188–191. doi: 10.1136/postgradmedj-2020-138100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakken BK, Winn AN. Clinician burnout during the COVID-19 pandemic before vaccine administration. J Am Pharm Assoc. 2021;61:e71–e77. doi: 10.1016/j.japh.2021.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wira CR, Goyal M, Southerland AM, et al. Pandemic guidance for stroke centers aiding COVID-19 treatment teams. Stroke. 2020;51:2587–2592. doi: 10.1161/STROKEAHA.120.030749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bersano A, Pantoni L. On being a neurologist in Italy at the time of the COVID-19 outbreak. Neurology. 2020;94:905–906. doi: 10.1212/WNL.0000000000009508. [DOI] [PubMed] [Google Scholar]
- 22.Srivastava PK, Zhang S, Xian Y, et al. Treatment and outcomes of patients with ischemic stroke during COVID-19. Stroke. 2021;52:3225–3232. doi: 10.1161/STROKEAHA.120.034414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiss P, Carcel C, Hockham C, Peters SAE. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7:18–27. doi: 10.1093/ehjqcco/qcaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bersano A, Kraemer M, Touzé E, et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020;27:1794–1800. doi: 10.1111/ene.14375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim GJ, Kim H, Fletcher J, et al. The differential impact of the COVID-19 pandemic on healthcare utilization disruption for community-dwelling individuals with and without acquired brain injury. Arch Rehabil Res Clin Transl. 2022;4 doi: 10.1016/j.arrct.2021.100176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markus HS, Brainin M. COVID-19 and stroke—a global World Stroke Organization perspective. Int J Stroke. 2020;15:361–364. doi: 10.1177/1747493020923472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perrin N, Iglesias J, Rey F, et al. Impact of the COVID-19 pandemic on acute coronary syndromes. Swiss Med Wkly. 2020;150:w20448. doi: 10.4414/smw.2020.20448. [DOI] [PubMed] [Google Scholar]
- 29.Rudilosso S, Laredo C, Vera V, et al. Acute stroke care is at risk in the era of COVID-19. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sama SR, Quinn MM, Galligan CJ, et al. Impacts of the COVID-19 pandemic on home health and home care agency managers, clients, and aides: a cross-sectional survey, March to June, 2020. Home Health Care Manag Pract. 2021;33:125–129. [Google Scholar]
- 31.Jones AL, Valverde R. Characteristics and use of home health care by men and women aged 65 and over. Natl. Health Stat Report. 2012;(52):8. [PubMed] [Google Scholar]
- 32.Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. MedRxiv. 2020 Feb 25 doi: 10.1101/2020.02.22.20026500. [Epub ahead of print] [DOI] [Google Scholar]
- 33.Fuentes B, Alonso de Leciñana M, Rigual R, et al. Fewer COVID-19-associated strokes and reduced severity during the second COVID-19 wave: the Madrid Stroke Network. Eur J Neurol. 2021;28:4078–4089. doi: 10.1111/ene.15112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qin C, Zhou L, Hu Z, et al. Clinical characteristics and outcomes of COVID-19 patients with a history of stroke in Wuhan. China. Stroke. 2020;51:2219–2223. doi: 10.1161/STROKEAHA.120.030365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fifi JT, Mocco J. COVID-19 related stroke in young individuals. Lancet Neurol. 2020;19:713–715. doi: 10.1016/S1474-4422(20)30272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nogueira RG, Abdalkader M, Qureshi MM, et al. Global impact of COVID-19 on stroke care. Int J Stroke. Published online. 2021;16:573–584. doi: 10.1177/1747493021991652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goverover Y, Kim G, Chen MH, et al. The impact of the COVID-19 pandemic on engagement in activities of daily living in persons with acquired brain injury. Brain Inj. 2022;36:183–190. doi: 10.1080/02699052.2022.2043441. [DOI] [PubMed] [Google Scholar]
- 38.Reckrey JM. COVID-19 confirms it: paid caregivers are essential members of the healthcare team. J Am Geriatr Soc. 2020;68:1679–1680. doi: 10.1111/jgs.16566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Towfighi A, Cheng EM, Ayala-Rivera M, et al. Randomized controlled trial of a coordinated care intervention to improve risk factor control after stroke or transient ischemic attack in the safety net: secondary stroke prevention by uniting community and chronic care model teams early to end disparities (SUCCEED) BMC Neurol. 2017;17:24. doi: 10.1186/s12883-017-0792-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. COVID-19 and your health. Available at: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/index.html. Accessed February 18, 2022.
- 41.Fama ME, Hatfield B, Coyle S, Richman MS, Georgeadis AC. The impact of the COVID-19 public health crisis on communication and quality of life: insights from a community of stroke and brain trauma survivors. Am J Speech Lang Pathol. 2021;30:1805–1818. doi: 10.1044/2021_AJSLP-20-00297. [DOI] [PubMed] [Google Scholar]
- 42.Teasell R, Salbach NM, Foley N, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke; Update 2019. Int J Stroke. 2020;15:763–788. doi: 10.1177/1747493019897843. [DOI] [PubMed] [Google Scholar]
- 43.Cohen JW, Ivanova TD, Brouwer B, Miller KJ, Bryant D, Garland SJ. Do performance measures of strength, balance, and mobility predict quality of life and community reintegration after stroke? Arch Phys Med Rehabil. 2018;99:713–719. doi: 10.1016/j.apmr.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 44.Kimonides S, Cavuoto MG, De Silva L, Kinsella GJ. The role of subjective cognitive complaints and depressive symptoms in social re-integration following stroke: a mediation explanation in a cross-sectional sample. Top Stroke Rehabil. 2018;25:514–520. doi: 10.1080/10749357.2018.1489570. [DOI] [PubMed] [Google Scholar]
- 45.Glickman LB. Clients with stroke and non-stroke and their guardians’ views on community reintegration status after in-patient rehabilitation. Malawi Med J. 2018;30:174–179. doi: 10.4314/mmj.v30i3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Olaiya MT, Cadilhac DA, Kim J, et al. Community-based intervention to improve cardiometabolic targets in patients with stroke. Stroke. 2017;48:2504–2510. doi: 10.1161/STROKEAHA.117.017499. [DOI] [PubMed] [Google Scholar]
- 47.Hakulinen C, Pulkki-Råback L, Virtanen M, Jokela M, Kivimäki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. 2018;104:1536–1542. doi: 10.1136/heartjnl-2017-312663. [DOI] [PubMed] [Google Scholar]
- 48.Mahon SP. Auckland University of Technology; Auckland, New Zealand: 2018. The long-term impact of stroke on cognition: prevalence, predictors, and assessment. [PhD thesis] [Google Scholar]
- 49.Mahon S, Theadom A, Barker-Collo S, et al. The contribution of vascular risk factors in prevalence of fatigue four years following stroke: results from a population-based study. J Stroke Cerebrovasc Dis. 2018;27:2192–2199. doi: 10.1016/j.jstrokecerebrovasdis.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 50.Tieges Z, Mead G, Allerhand M, et al. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil. 2015;96:15–23. doi: 10.1016/j.apmr.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 51.U.S. Department of Health and Human Services. Healthy People 2030. Available at: https://health.gov/healthypeople. Accessed January 21, 2022.
- 52.Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of health disparities, health inequities, and social determinants of health to support the advancement of health equity. J Public Health Manag Pract. 2016;22(Suppl 1):S33–S42. doi: 10.1097/PHH.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Virani SS, et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143:254–743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 54.Burns SP, White BM, Magwood G, et al. Racial and ethnic disparities in stroke outcomes: a scoping review of post-stroke disability assessment tools. Disabil Rehabil. 2019;41:1835–1845. doi: 10.1080/09638288.2018.1448467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lekoubou A, Pelton M, Ba DM, Ssentongo P. Racial disparities in ischemic stroke among patients with COVID-19 in the United States. J Stroke Cerebrovasc Dis. 2021;30 doi: 10.1016/j.jstrokecerebrovasdis.2021.105877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72:703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Havenon A, Ney JP, Callaghan B, et al. Impact of COVID-19 on outcomes in ischemic stroke patients in the United States. J Stroke Cerebrovasc Dis. 2021;30 doi: 10.1016/j.jstrokecerebrovasdis.2020.105535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Available at:https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed January 21, 2022.
- 59.Churchwell K, Elkind MS, Benjamin RM, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 60.Fleming TK. Letter to the editor on “African American patient disparities in COVID-19 outcomes, a call to action for physiatrists to provide rehabilitation care to Black survivors. Am J Phys Med Rehabil. 2021;100:439–440. doi: 10.1097/PHM.0000000000001725. [DOI] [PubMed] [Google Scholar]
- 61.Katsanos AH, Tsivgoulis G. Stroke mortality during the second wave of the COVID-19 pandemic: is it getting any better? Eur J Neurol. 2021;28:3881–3882. doi: 10.1111/ene.15135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee SH, Juang YY, Su YJ, Lee HL, Lin YH, Chao CC. Facing SARS: psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen Hosp Psychiatry. 2005;27:352–358. doi: 10.1016/j.genhosppsych.2005.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smith MW, Smith PW, Kratochvil CJ, Schwedhelm S. The psychosocial challenges of caring for patients with Ebola virus disease. Health Secur. 2017;15:104–109. doi: 10.1089/hs.2016.0068. [DOI] [PubMed] [Google Scholar]
- 65.Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9:241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thau L, Siegal T, Heslin ME, et al. Decline in rehab transfers among rehab-eligible stroke patients during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021;30 doi: 10.1016/j.jstrokecerebrovasdis.2021.105857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Venketasubramanian N, Anderson C, Ay H, et al. Stroke care during the COVID-19 pandemic: international expert panel review. Cerebrovasc Dis. 2021;50:245–261. doi: 10.1159/000514155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Burns SP, Terblanche M, Perea J, et al. mHealth intervention applications for adults living with the effects of stroke: a scoping review. Arch Rehabil Res Clin Transl. 2021;3 doi: 10.1016/j.arrct.2020.100095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burns SP, Terblanche M, MacKinen A, DeLaPena C, Fielder JDP. Smartphone and mHealth use after stroke: results from a pilot survey. OTJR (Thorofare N J) 2022;42:127–136. doi: 10.1177/15394492211068851. [DOI] [PubMed] [Google Scholar]
- 70.Kim GJ, Parnandi A, Eva S, Schambra H. The use of wearable sensors to assess and treat the upper extremity after stroke: a scoping review. Disabil Rehabil. 2021 Jul 30 doi: 10.1080/09638288.2021.1957027. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Patel UK, Malik P, DeMasi M, Lunagariya A, Jani VB. Multidisciplinary approach and outcomes of tele-neurology: a review. Cureus. 2019;11:e4410. doi: 10.7759/cureus.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwamm LH, Chumbler N, Brown E, et al. Recommendations for the implementation of telehealth in cardiovascular and stroke care: a policy statement from the American Heart Association. Circulation. 2017;135:e24–e44. doi: 10.1161/CIR.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 73.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2020;1 doi: 10.1002/14651858.CD010255.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tyagi S, Lim DSY, Ho WHH, et al. Acceptance of tele-rehabilitation by stroke patients: perceived barriers and facilitators. Arch Phys Med Rehabil. 2018;99:2472–2477. doi: 10.1016/j.apmr.2018.04.033. [DOI] [PubMed] [Google Scholar]
- 75.Kringle EA, Setiawan IMA, Golias K, Parmanto B, Skidmore ER. Feasibility of an iterative rehabilitation intervention for stroke delivered remotely using mobile health technology. Disabil Rehabil Assist Technol. 2020;15:908–916. doi: 10.1080/17483107.2019.1629113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sanders CK, Scanlon E. The digital divide is a human rights issue: advancing social inclusion through social work advocacy. J Hum Rights Soc Work. 2021;6:130–143. doi: 10.1007/s41134-020-00147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27:1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim H, Kim GJ. Attitudes and use patterns for mobile technology and upper extremity home exercises in stroke survivors in the United States. Br J Occup Ther. 2022 Feb 14 [Epub ahead of print] [Google Scholar]
- 79.Halbert K, Bautista C. Telehealth use to promote quality outcomes and reduce costs in stroke care. Crit Care Nurs Clin North Am. 2019;31:133–139. doi: 10.1016/j.cnc.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 80.Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020;94:30–38. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 81.Caughlin S, Mehta S, Corriveau H, et al. Implementing telerehabilitation after stroke: lessons learned from Canadian trials. Telemed J E Health. 2020;26:710–719. doi: 10.1089/tmj.2019.0097. [DOI] [PubMed] [Google Scholar]
- 82.Piran P, Thomas J, Kunnakkat S, et al. Medical mobile applications for stroke survivors and caregivers. J Stroke Cerebrovasc Dis. 2019;28 doi: 10.1016/j.jstrokecerebrovasdis.2019.104318. [DOI] [PubMed] [Google Scholar]
- 83.Cuccurullo SJ, Fleming TK, Kostis WJ, et al. Impact of a stroke recovery program integrating modified cardiac rehabilitation on all-cause mortality, cardiovascular performance and functional performance. Am J Phys Med Rehabil. 2019;98:953–963. doi: 10.1097/PHM.0000000000001214. [DOI] [PubMed] [Google Scholar]