Abstract
Background
The global outbreak of COVID-19 has created a challenging situation, especially for the frontline Health Care Professionals (HCPs), who are routinely exposed and thus are at a higher risk of infection. Pranayama, a component of Yoga, is known to improve immune function and reduce infection. However, no clinical trial on the efficacy of Pranayama in preventing COVID-19 has yet been conducted.
Aim and objective
This quasi-randomized clinical trial assessed the efficacy of Pranayama in preventing COVID-19 infection in HCPs routinely exposed to COVID-19.
Methodology
The study was conducted at 5 different COVID-19 hospitals, India in year 2020. The inclusion criteria were being an HCP exposed to COVID-19 patients and being negative on antibody tests. 280 HCPs were recruited sequential and assigned to intervention and control groups. Of these, 250 HCPs completed the study. The intervention was twice daily practice, for 28 days, of specially designed Pranayama modules under the online supervision of Yoga instructors. The HCPs in the control group were advised to continue their normal daily routine, but no pranayama sessions. Participants who developed symptoms suggestive of COVID-19 were subjected to Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) or Point of Care Rapid Antigen Test (RAT) for confirmation of the diagnosis. All the participants were tested for antibodies to COVID-19 on 28th day of the intervention to detect any asymptomatic infection.
Results
The intervention (123) and control (127) groups had comparable demographics and baseline characteristics. At end of 28 days of intervention, nine participants in the control group and one in the intervention group developed COVID-19 (P-value: 0.01, Odds Ratio: 0.107, 95% CI: 0.86; Risk Ratio: 0.11, 95% CI: 0.89).
Conclusion
The intervention of twice daily practice of the Pranayama module for 28 days in HCPs might have made a noteworthy contribution and may have helped in preventing COVID-19 infection.
Keywords: COVID-19, Pranayama, Health care professionals, Yoga
1. Introduction
COVID-19 pandemic is a global challenge to public health [1]. Among other measures, most countries have enforced lock-downs or stay-at-home orders [1] as a mitigation measure. Health Care Professionals (HCPs) being exposed to cases as a part of their professional duties have been in particular susceptible to COVID-19 infection.
HCPs being on the front lines of COVID-19 crisis, have reported psychological stress [2], tiredness, sleep problems [2] because of fear, and interruption of normal life due to heavy patient loads [3]. HCPs are under extreme stress due to their long working hours, wearing of Personal Protective Equipment (PPE), lack of specific drugs and being away from their families [4,5].
At present, there is no definite treatment for COVID-19. However, researchers and clinicians are working on various antibiotics and antiviral agents, like monoclonal antibodies, oseltamivir, ganciclovir, ribavirin, molnupiravir, favipiravir, nelfinavir, arbidol, remdesivir and galidesivir [[6], [7], [8], [9]]. Since immunity plays an important role in COVID-19 infection, Non-Pharmacological Interventions which have an immune-modulatory effect, could serve as a preventive as well as a therapeutic measure for patients with COVID-19 infection [[10], [11], [12], [13], [14]]. During this outbreak, numerous herbal products have also been explored as alternative therapies [15,16].
Yoga, which originated in ancient India, is also recognized as a form of a Complementary Medicine, as well as an alternative therapy that can positively influence the mind-body continuum [17]. Yoga has been practiced since times immemorial for the prevention of disease and promotion of health. Substantial research has already been done on the effectiveness of Yoga in the management of lifestyle disorders, preventing infection and accelerating healing and recovery. Yoga has two key practices – one of rhythmic, controlled breathing called Pranayama and another is effortless concentration of mind called Dhyana. The former helps to improve lung capacity, cardio-respiratory functions, neuro-endocrine activity and also mental activity [17,18]. Several other studies suggest the effects of various components of Yoga in infectious diseases. A study conducted in a Bangalore sanatorium showed efficacy of Integrated Yoga (IY) protocol as an add-on to Anti Tuberculosis Treatment in reducing symptoms of Tuberculosis [17]. One month of practice of integrated Yoga in patients suffering from HIV-1 infection led to a significant reduction in viral load, increase in the number of CD4 immune cells and improvement in psychological state [18]. Several clinical trials have suggested an overall positive effect of Yoga in improving pulmonary and immune functions in patients with tuberculosis [17], HIV-1 infection [18] and anxiety [19].
Therefore, the present study was conducted to assess the efficacy of Pranayama, which is a part of yoga, in preventing COVID 19 infection in the HCPs exposed to COVID-19 infection [20].
2. Methodology
2.1. Ethical considerations
After obtaining approval of the Institutional Ethics Committee, the study was registered on Clinical Trials Registry of India (CTRI No. CTRI/2020/07/026667). Five hospitals dedicated for handling COVID-19 cases were included for the study. HCPs meeting inclusion criteria of exposure to COVID-19 suspects or cases, were in quarantine and ready to practice Pranayama, but did not have co-morbidities that avert practice of Pranayama or Severe cardiac disease were enrolled for the study and their informed consent obtained. One Yoga instructor was assigned to each of the five identified hospitals to train and guide the study participants in twice daily practice of Pranayama, supervise its practice and collect data on the intervention. The HCPs in the control group were advised to continue their normal daily routine, but no pranayama sessions.
2.2. Sample size
Sample size was estimated on the assumption of a prevalence of COVID-19 infection of 10% in the population of HCPs, and expectation that our treatment group will have a 90% lower prevalence i.e. 1%. For a power of 80%, alpha of 0.05, 95% confidence interval, the sample size estimate was 121 in each arm (Table 3).
Table 3.
Sample size calculation In Stata sampsi 0.1 0.01, power (0.8).
| Estimated sample size for two-sample comparison of proportions |
| Test Ho: p1 = p2, where p1 is the proportion in population 1 and p2 is the proportion in population 2 |
| Assumptions: |
| alpha = 0.0500 (two-sided) |
| power = 0.8000 |
| p1 = 0.1000 |
| p2 = 0.0100 |
| n2/n1 = 1.00 |
| Estimated required sample sizes: |
| n1 = 121 |
| n2 = 121 |
2.3. Study sample
Inclusion criterion was HCPs (age range: 19–65 years, any gender), being on COVID-19 duty (duty cards were taken as proof), not previously infected with COVID-19 (negative antibody test) but with a recent history of exposure to COVID-19 suspects or cases and who were in quarantine. 288 HCPs were registered for the study. Out of these, 8 were found positive on rapid Antibody tests at baseline. Positive rapid antibody test of HCPs indicates previous infection of COVID-19; therefore, such HCPs were excluded from the study. HCPs like doctors, nursing staff, housekeeping staff/caretaker and Yoga instructors who were directly in contact with COVID-19 positive patients were classed as “directly exposed”. Others like Medical Superintendent, Chief Medical Officers, Pharmacists, Lab technician, Hospital administration staff like Managers, Supervisors, DEO, MTS who were not in close contact with COVID-19 cases were classed as “indirectly (remotely) exposed”.
2.4. Randomization
Medical in-charge of the hospitals/COVID-19 care units were authorized to enroll study participants but had no other role in the trial. Eligible HCPs were quasi-randomized on admission through alternate allocation (ratio 1:1) into two groups. Subsequently, the two groups were designated as ‘Intervention group’ and the ‘Control group’ by the coordinator of the study, who was blinded to the initial allocation.
2.5. Masking
It is difficult to assess yoga/pranayama practices in double blind trials because the intervention requires active participation of the participants and hence their identities become known after allocation. Soon after enrollment, antibody test was administered by a lab staff who did not otherwise participate in the trial and was blinded to the study groups. In addition, the outcome assessor was blinded to the group of study.
2.6. Study groups
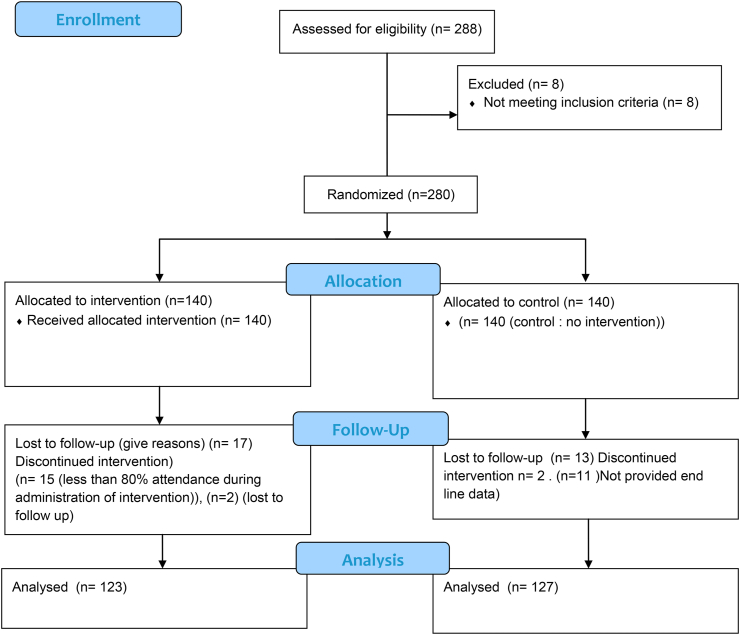
Of the 280 enrolled participants, 17 (Intervention – 15, Control – 2) did not adhere to the 80% attendance requirement, and 13 (Intervention – 2, Control – 11) did not give their post-intervention data, and thus 30 study participants (Intervention – 17, Control – 13) were excluded. Thus, 250 participants completed the study which included 123 in the intervention group (administered Pranayama protocols) and 127 in the control group. Profession wise break up of 250 participants was: Resident Doctors-29, Nursing staff-63, Caretakers/House-keeping staff-82, Lab technicians-22, CMOs/Medical Superintendent −20, Pharmacist-15, Yoga Instructors-4, Hospital Administration staff like Accountants, Multi-Tasking Staff, Data Entry Operator, Receptionists-15.
2.7. Study parameters and tools
Basic demographic information, medical history and dietary habits were collected at baseline. Antibody test for COVID-19 was done on all the study participants at baseline and on completion of the study at end-line.
2.8. Antibody test
An antibody serology test (Accucare COVID-19 kit) approved by ICMR; was used to detect prior COVID-19 infection in all study participants. This test detects two types of antibodies – IgM and IgG. During the study, the participants who developed COVID-19 symptoms were also administered the Rapid Antigen Test/RT-PCR for confirmation of a diagnosis of COVID-19.
2.9. The intervention: administration of pranayama protocols
Two Pranayama modules lasting 30 min for the morning (Table 1) and 15 min for the evening (Table 2), were developed by the principal investigator., . Participants in the intervention group were trained and guided through Video-Conference by Yoga Instructors to practice Pranayama twice a day for 28 days. A daily attendance record was maintained. All the participants were closely monitored by the Yoga Instructors for confirmation to the protocol.
Table 1.
Pranyama (breathing) protocol for the morning session (30 min).
| S. no | Practices | Name of practice | Rounds | Duration (in minutes) |
|---|---|---|---|---|
| 1 | Preparatory Practices for Pranayama (9 min) |
Prayer | 3 deep breathing or prayer of individual | 1 |
| 2 | Vaata-Neti | 3 roundsa (30 s/round) | 2.5 | |
| 3 | Kapalabhati | 3 roundsa (30 s/round) | 2.5 | |
| 4 | Deep breathing | 10 rounds | 3 | |
| 5 | Pranayama practices (16 min) | Nadi-shodhana | 10 rounds | 8 |
| 6 | Ujjaayee | 10 rounds | 4 | |
| 7 | Bhramari | 10 rounds | 4 | |
| 9 | Meditation (5 min) | Dhyana | Awareness of breathing, thoughts and emotions | 5 |
| Total duration | 30 |
This Pranayama protocol was administered with increased intensity gradually to achieve 6:3:6:3 ratio (6 inhalations: 3 retentions: 6 exhalations: 3 retentions).
Day 1: subjects were practiced Inhalation (4 s): Exhalation (4 s).
Day 2: I: E ratio (5 s:5 s).
Day 3: I: E ratio (6 s:6 s).
Day 4 & 5: I: RI:E ratio (6 s:3 s:6 s).
Day 6 & 7: I: RI: E: RO ratio (6 s:3 s:6 s:3 s).
8th day onwards they continuously practiced with 6 s of inhalations: 3 s of retentions: 6 s of exhalations: 3 s of retention ratios.
(2 &3) Each practice of vaataneti/kapalbhanti has suitable rest/gap time of 20 s to become normal and to experience the impact of the practice.
Table 2.
Pranyama (breathing) protocol for the evening session (15 min).
| S. no | Name of practice | Rounds | Duration (in minutes) |
|---|---|---|---|
| 1 | Shavasana (corpse pose) (with palm upwards) Pristhabhumi Tadasana |
1 | |
| 2 | Abdominal breathing | 15 Roundsa | 3 |
| 3 | Thoracic breathing | 15 Roundsa | 3 |
| 4 | Clavicular breathing | 15 Roundsa | 3 |
| 5 | Deep breathing (lying down position) | 15 Roundsa | 3 |
| 6 | Relaxation in Shavasana with awareness on abdominal breathing | 2 | |
| Total duration | 15 | ||
Each breathing comprises 6 s inhalation and 6 s exhalation.
There is no retention of breathing in the evening session. For the breathing practices in the evening yoga sessions were designed as follows.
Day 1& 2: subjects were practiced Inhalation (4 s): exhalation ratio (4 s).
Day 3& 4: inhalation (5 s): exhalation ratio (5 s).
Day 5 & 6: inhalation (6 s): exhalation ratio (6 s).
Rest/gap has been given between each pranayama.
Initially the practice of all 4 breathing practices started with 10 rounds each and gradually over a period of 5–7 days increased to 15 rounds each.
2.10. Modules
Specially designed Pranayama modules included preparatory Yoga practices for 9 min, Pranayama practice for 16 min and meditation for 5 min each in the morning session, and 15 min of breathing exercises in the evening session. Detailed procedure to perform the protocol has been provided as supplementary data (Annexure-1)
These modules were also publicly hosted (https://www.youtube.com/watch?v=RD1huWS_7w8&feature=youtu.be). The intervention group was provided this link from the beginning for their better understanding and aid in practice.
2.11. Statistical analysis
Data collected was entered in Microsoft Excel and cleaned. In bivariate analysis, categorical variables were presented as frequencies (%), continuous data as mean (with Standard Deviation) or median. Mean difference in pre-post intervention was examined for statistical significance using Fisher's exact test. A P-value of 0.01 was considered significant. Data was analyzed using IBM Statistical Package for the Social Sciences (SPSS) Version 20.0 (Armonk, NY: IBM Corp).
3. Results
Flowchart diagram of recruitment process of participants and design of the study has been provided in Fig. 1.
Fig. 1.
Flow chart.
Two groups of HCPs had comparable age, socio demographic characteristics, exposure status and comparable co-morbidities (Table 4).
Table 4.
Baseline socio demographic profile of 250 HCPs.
| Variables | Experimental Grp N (%) |
Control Grp N (%) |
|---|---|---|
| Total | 123 (100.00%) | 127 (100.00%) |
| Age (in years) | ||
| 18–35 | 74 (60.16%) | 70 (55.12%) |
| 36–50 | 40 (32.52%) | 49 (38.58%) |
| 51–65 | 9 (7.32%) | 8 (6.30%) |
| Gender | ||
| Male | 67 (54.47%) | 65 (51.18%) |
| Female | 56 (45.53%) | 62 (48.82%) |
| Diet | ||
| Veg. | 69 (56.10%) | 52 (40.94%) |
| Mixed diet | 54 (43.90%) | 75 (59.06%) |
| Exposure | ||
| In-directly exposed | 86 (69.92%) | 87 (68.50%) |
| Admin staff | 4(3.3%) | 11 (8.7%) |
| Lab technician | 14 (11.4%) | 8 (6.3%) |
| Pharmacist | 5(4.1%) | 10 (7.9%) |
| Senior officers/CMO | 11(8.9%) | 9 (7.1%) |
| Directly exposed | 37 (30.08%) | 40 (31.50%) |
| Doctor | 17 (13.8%) | 12 (9.4%) |
| Nursing staff | 30 (24.4%) | 33 (26.0%) |
| Caretaker/housekeeping | 39 (31.7%) | 43 (33.9%) |
| Yoga instructor | 3 (2.4%) | 1 (0.8%) |
| Health status | ||
| HCPs (healthy) | 102 (83%) | 106 (84%) |
| HCPs (with co-morbidities) | 21 (17%) | 21 (16%) |
Grp: group; N: number; Veg.: vegetarian.
During the period of the study, three participants from the control group developed symptoms suggestive of COVID-19 such as fever, cough, etc. They tested positive on Rapid Antigen test/RT-PCR. At the end of the study, one participant from the intervention group and 9 from the control group (including three symptomatic participants who had tested positive on Rapid Antigen Test/RTCPR) tested positive on COVID-19 Antibody Test. This difference was statistically significant (P-value: 0.01), indicating a protective effect of the intervention of Pranayama in preventing COVID-19 infection (odds ratio: 0.107, 95% CI: 0.86; risk ratio: 0.11, 95% CI: 0.89) (Table 5). The 10 HCPs who tested positive with COVID-19 at the end line showed no particular socio-demographic pattern (Table 6). They belonged to both genders, diverse age and professional groups with 80% of them being middle-aged. Of the 10 HCPs (4 females, 6 males) who contracted COVID-19 infection, nine were from the highly exposed group and 8 were healthy with no comorbidities (Table 6). The lone participant from the experimental group who tested positive on antibody testing at the end of intervention probably had asymptomatic COVID 19 infections.
Table 5.
Post-intervention COVID-19 assessment results in intervention vs. control groups.
| Total no. of HCPs | COVID-19 positive cases | COVID-19 negative cases | Fisher's exact test score | P-value | Effect size | |
|---|---|---|---|---|---|---|
| Experimental grp N (%) |
123 (100%) | 1 (0.8%) | 122 (99.2%) | 0.0192 | 0.01a | Odd's ratio: 9.00, CI: (1.14, 71.03) |
| Control Grp N (%) |
127 (100%) | 9 (7.1%) | 118 (92.9%) | Risk ratio: 1.83, CI (1.43, 2.3) |
Indicate level of significance.
Table 6.
Socio-demographic profile of HCPs infected with COVID-19 at post-intervention.
| HCPs | Group | Gender | Dietary habits | Age group | Exposure (COVID-19) | Duty in COVID-19 wards |
|---|---|---|---|---|---|---|
| SUB 012 | Control | F | Veg | 18–35 | Direct | Asha worker/care taker/housekeeping |
| SUB 034 | Control | M | Veg | 51–65 | Direct | Care taker/housekeeping |
| SUB 084 | Control | F | Non-veg | 36–50 | Direct | Care taker/housekeeping |
| SUB 114 | Control | F | Non-veg | 36–50 | Direct | Nursing off |
| SUB 164 | Control | M | Veg | 36–50 | Indirect | Courier boy/admin staff |
| SUB 171 | Control | M | Veg | 18–35 | Indirect | Lab tech |
| SUB 173 | Control | M | Non-veg | 51–65 | Direct | Doctor |
| SUB 186 | Control | F | Veg | 18–35 | Direct | Care taker/housekeeping |
| SUB 196 | Control | M | Non-veg | 18–35 | Direct | Care taker/housekeeping |
| SUB 227 | Experimental | M | Veg | 36–50 | Direct | Care taker/housekeeping |
4. Discussion
The present study was conducted in 5 different hospitals dedicated for COVID-19 patients with a reasonable (250) sample size. To the best of our knowledge, this is the first study to assess the effect of Pranayama in preventing COVID-19. The results of our study suggesting a role of Pranayama in infection is in agreement with earlier studies [11,17,18]. The only participant in the Intervention group who developed COVID-19 was a caretaker (male) in the 35–50 years age group, with no comorbidity, who was in contact with COVID-19 patients. He had no regular exercise routine, but was practicing the Pranayama intervention.
The biological processes underlying the protective effects of Pranayama remain to be fully investigated. Each component of the Pranayama module would have played a role in preventing COVID-19 infection. Vaata-neti helps to clean the nasal passages and maintain the sinuses and helps to get rid of pathogens. Kapalabhati kriya is a process of forceful exhalation and normal inhalation which help to improve pulmonary function and clean the frontal sinuses, removing congestion in nasal and respiratory tract [22] and easing movement of the diaphragm [21]. These two are very useful preparatory practices for Pranayama. Deep breathing helps to improve lung's vital capacity. Nadi-shodhana pranayama helps to reduce sympathetic activity and stimulate the vagal (parasympathetic activity) [23]. It helps to reduce stress and anxiety, thus balancing autonomic function. Ujjayi pranayama increase oxygen (O2) saturation in the body, removal of congestion from the throat and strengthens the larynx and pharynx [23]. Bhramari pranayama is similar to humming that increases nasal Nitric Oxide (NO) by improving blood flow to the ciliary epithelium [24,25]. Meditation helps to reduce stress & anxiety by reducing cortisol levels in the blood and enhances alpha (α) waves in the brain. The above pranayama and Dhyana practices make the body comfortable, keep the mind calm and help to balance the neuro-endocrine system, and thereby the immune system. The preparatory practices for pranayama (eg. Vaataneti & kapalabhati) performed at the rate of one breathing per sec and pranayama practices in the morning session involved a ratio of 6 (inhalation):3 (retention): 6 (exhalation):3 (retention), while those in the evening session followed a breathing ratio of 6:6. At rest, one breath normally lasts 3 s, which gets extended to 18 s during pranayama. In our protocol, emphasis was on deep, slow, rhythmic breath with awareness. The breathing practices for the evening followed by shavasana (with the palm upwards) would have given relaxation to body and mind and improved the quality of sleep. In thoracic breathing, the chest expands and contracts with each breath while the abdominal area does not. The subjects were encouraged to breathe in more oxygen by slow and deep thoracic breathing with total awareness [26]. Practice of thoracic breathing immediately after performing abdominal breathing helps the practitioner to adapt to more chest expansion, before doing the clavicular breathing. Thus, in the next step, i.e., the practice of deep breathing, the subject naturally and effectively expands thorax for effective ventilation. The selected combination of Pranayama modules makes it a comprehensive intervention for the purpose of reducing the possibility of contracting COVID-19 infection.
There is strong evidence on the positive effects of Yoga practice on stress management among HCPs [27]. Stress is known to suppress immune function and increase susceptibility to infections [28]. Chronic stress is associated with global immuno-suppression, as well as decreases in almost all immune measures. Increased duration of stress can result in a shift from potentially adaptive changes to potentially detrimental changes, initially in cellular immunity and then in broad immune function [29]. Pranayama practices have been found to have a direct impact on reduction in vaata aggravation and Vagus Nerve stimulation [31,32]. Vagus Nerve Stimulation has been found to have a direct effect in managing stress and diseases born out of it [30]. A strong host immune response to the novel coronavirus is a key factor for protection against infection. The efficacy of our especially designed Pranayama protocol could be because of the above-mentioned mechanisms, whose modalities of action need further exploration. This study has also revealed that COVID-19 infection in the intervention group tends to be mild and asymptomatic, thus strengthening the conclusion of a positive, preventive effect of Pranayama.
4.1. Strength, limitations and future recommendations
This study has some limitations. Due to pandemic conditions, the Pranayama protocols could be administered through online mode only. Yoga Practices like Pranayama need Guru-Shishya (Yoga teacher – Yoga student) interaction. HCPs could have had a lowered interest in Pranayama classes due to prolonged working hours. As the control group was not administered with any comparable practice, they might not have had any expectation of a lower chance of contracting the infection. Future studies are required with a set of comparable practices for the control group also. Since the Antibody test alone was used for pre-test assessment of COVID-19 infection, there could be a theoretical probability in both the groups of a prior infection with COVID-19, but without any detectable antibodies. Of the 10 HCPs (9 Control +1 Experimental group) who contacted COVID-19 at the end-line, 6 were from the lower Socio-economic groups. Only 2 of the 10 participants turning covid-19 positive were from the doctors/nurse category, while the rest were from allied and support staff, whose household and social conditions like food intake, home environment, stress of life might not be comparable. The study has not investigated the effect of confounding variables like environmental factors (such as food intake, home environment, stress of life). This is an area of further research. Our intervention lasted 28 days, which is a relatively short length for the study and longer periods of practice of the intervention are critical to knowing the lasting benefits and efficacy of the intervention. Hence, a multi-centric study with a larger sample and longer duration/period is recommended for further testing of our Pranayama Protocol. The pranayama protocol can also be compared to and supplemented with other yoga/pranayama programs. Considering the implications of the study for Health care professionals and the general public living in fear of COVID-19, larger studies across different geographical, ethnic and cultural backgrounds are needed to verify its generalizability.
Despite limitations, the data presented in this study draws attention to the benefits of our Pranayama modules to prevent COVID-19 in HCPs routinely exposed to the virus.
The intervention of twice daily practice of Pranayama administered by trained Yoga instructors in HCPs exposed to active cases might have helped and made a noteworthy contribution in significantly preventing COVID-19 infection. The present study suggests that the Pranayama modules can be promoted among all sections of the population to prevent COVID-19.
Funding agency
Funded by Morarji Desai National Institute of Yoga, Ministry of Ayush, Govt. of India.
Declaration of competing interest
No conflicts of interest.
Acknowledgments
The authors would like to thank Vaidya Rajesh Kotecha, Secretary, Ministry of AYUSH and Chairman, Governing Council, MDNIY for his support and guidance. We would also like to extend our thanks to Shri P.N. Ranjit Kumar, Joint Secretary, AYUSH and Chairperson, Scientific Advisory Committee (SAC), MDNIY and all other members of SAC for their valuable inputs and encouragement. We also thank Dr. Shivam Pandey, Scientist-1, Dept. of Biostatistics, AIIMS for his help in doing statistical analysis of the research work. We would also like to offer our special thanks to Dr. R.K. Manchanda, Director, Directorate of AYUSH Govt. of NCT Delhi for his support in arranging the much-needed participants for the study and Dr. I.N. Acharya, Program Officer (YT) of MDNIY for helping supervise the administration of the modules. The authors also thank medical superintendents, doctors and staff of all 5 hospitals for their active cooperation. We would like to thank 5 yoga instructors (Mr. Sahil, Mr. Sandeep, Ms. Aishwarya, Ms. Sunita and Ms. Kranti) and Data entry operator (Ms. Nishu) for administration of yoga modules and entry of data respectively.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2022.100586.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.WHO . 2020. WHO director-general's opening remarks at the media briefing on COVID-19 – 11 March 2020.https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available from: [Google Scholar]
- 2.Wu W., Zhang Y., Wang P., Zhang L., Wang G., Lei G., et al. Psychological stress of medical staff during outbreak of COVID-19 and adjustment strategy. J Med Virol. 2020;92:1962–1970. doi: 10.1002/jmv.25914. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suryavanshi N., Kadam A., Dhumal G., Nimkar S., Mave V., Gupta A., et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;10 doi: 10.1002/brb3.1837. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson W., Raj J.P., Rao S., Ghiya M., NedunjalaiParambil N.M., Mundra H., et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J Psychol Med. 2020;42:353–358. doi: 10.1177/0253717620933992. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li W., Yang Y., Liu Z.-H., Zhao Y.-J., Zhang Q., Zhang L., et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caly L., Druce J.D., Catton M.G., Jans D.A., Wagstaff K.M. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antivir Res. 2020;178:104787. doi: 10.1016/j.antiviral.2020.104787. ISSN 0166-3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheahan T.P., Sims A.C., Leist S.R., Schäfer A., Won J., Brown A.J., et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11 doi: 10.1038/s41467-019-13940-6. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu Z., Peng C., Shi Y., Zhu Z., Mu K., Wang X., et al. 2020. Nelfinavir was predicted to be a potential inhibitor of 2019-nCov main protease by an integrative approach combining homology modelling, molecular docking and binding free energy calculation. Available from: [DOI] [Google Scholar]
- 9.Li G., De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV) Nat Rev Drug Discov. 2020;19:149–150. doi: 10.1038/d41573-020-00016-0. Available from: [DOI] [PubMed] [Google Scholar]
- 10.Koca Adam B., Şanlier N. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit Rev Food Sci Nutr. 2015;57:2889–2895. doi: 10.1080/10408398.2015.1077195. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Eda N., Ito H., Shimizu K., Suzuki S., Lee E., Akama T. Yoga stretching for improving salivary immune function and mental stress in middle-aged and older adults. J Women Aging. 2017;30:227–241. doi: 10.1080/08952841.2017.1295689. Available from: [DOI] [PubMed] [Google Scholar]
- 12.Ren J.-L., Zhang A.-H., Wang X.-J. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res. 2020;155:104743. doi: 10.1016/j.phrs.2020.104743. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L., Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagendra H. Yoga for COVID-19. Int J Yoga. 2020;13:87. doi: 10.4103/ijoy.IJOY_27_20. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma M., Anderson S.A., Schoop R., Hudson J.B. Induction of multiple pro-inflammatory cytokines by respiratory viruses and reversal by standardized Echinacea, a potent antiviral herbal extract. Antivir Res. 2009;83:165–170. doi: 10.1016/j.antiviral.2009.04.009. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Nugraha R.V., Ridwansyah H., Ghozali M., Khairani A.F., Atik N. Traditional herbal medicine candidates as complementary treatments for COVID-19: a review of their mechanisms, pros and cons. evidence-based complementary and alternative medicine. Evid Based Complement Altern Med. 2020;2020:1–12. doi: 10.1155/2020/2560645. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visweswaraiah N.K., Telles S. Randomized trial of yoga as a complementary therapy for pulmonary tuberculosis. Respirology. 2004;9:96–101. doi: 10.1111/j.1440-1843.2003.00528.x. Available from: [DOI] [PubMed] [Google Scholar]
- 18.Metri K., Naoroibam R., Bhargav H., Nagaratna R., Nagendra H. Effect of Integrated Yoga (IY) on psychological states and CD4 counts of HIV-1 infected patients: a randomized controlled pilot study. Int J Yoga. 2016;9:57. doi: 10.4103/0973-6131.171723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varambally S., Philip M., Gangadhar B., Umadevi P., Ramachandra S. Effect of yoga therapy on anxiety and depressive symptoms and quality-of-life among caregivers of in-patients with neurological disorders at a tertiary care center in India: a randomized controlled trial. Indian J Psychiatry. 2013;55:385. doi: 10.4103/0019-5545.116304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahendra J. Effect of pranayama on Ppar-γ, Nf-κB expressions and red complex microorganisms in patients with chronic periodontitis – a clinical trial. J Clin Diagn Res. 2017 doi: 10.7860/JCDR/2017/27846.10108. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patra S. Physiological effect of kriyas: cleansing techniques. Int J Yoga Philos Psychol Parapsychol. 2017;5:3. doi: 10.4103/ijny.ijoyppp_31_17. Available from: [DOI] [Google Scholar]
- 22.Dhanvijay A.D., Bagade A.H., Choudhary A.K., Kishanrao S.S., dhokne N. Alternate nostril breathing and autonomic function in healthy young adults. 2015. https://www.iosrjournals.org/iosr-jdms/papers/Vol14-issue3/Version-6/M014366265.pdf Available from:
- 23.Saoji A.A., Raghavendra B., Manjunath N. Effects of yogic breath regulation: a narrative review of scientific evidence. J Ayurveda Integr Med. 2019;10:50–58. doi: 10.1016/j.jaim.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maniscalco M., Sofia M., Weitzberg E., de Laurentiis G., Stanziola A., Rossillo V., et al. Humming-induced release of nasal nitric oxide for assessment of sinus obstruction in allergic rhinitis: pilot study. Eur J Clin Investig. 2004;34:555–560. doi: 10.1111/j.1365-2362.2004.01384.x. Available from: [DOI] [PubMed] [Google Scholar]
- 25.Maniscalco M., Weitzberg E., Sundberg J., Sofia M., Lundberg J. Assessment of nasal and sinus nitric oxide output using single-breath humming exhalations. Eur Respir J. 2003;22:323–329. doi: 10.1183/09031936.03.00017903. Available from: [DOI] [PubMed] [Google Scholar]
- 26.Saraswati S.S. In: Thoracic breathing in pranayama. 3rd ed. Asana Pranayama, Mudra Bandha., editors. Yoga Publication Trust; Munger, Bihar, India: 2004. pp. 363–378. [Google Scholar]
- 27.Michalsen A., Grossman P., Aci A., Langhorst J., Lüdtke R., Esch T., et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. 2005. https://pubmed.ncbi.nlm.nih.gov/16319785/ Available from: [PubMed]
- 28.Dhabhar F.S. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16:300–317. doi: 10.1159/000216188. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Segerstrom S.C., Miller G.E. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130:601–630. doi: 10.1037/0033-2909.130.4.601. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bremner J.D., Gurel N.Z., Wittbrodt M.T., Shandhi M.H., Rapaport M.H., Nye J.A., et al. Application of noninvasive vagal nerve stimulation to stress-related psychiatric disorders. J Pers Med. 2020;10:119. doi: 10.3390/jpm10030119. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chu I.-H., Wu W.-L., Lin I.-M., Chang Y.-K., Lin Y.-J., Yang P.-C. Effects of yoga on heart rate variability and depressive symptoms in women: a randomized controlled trial. J Altern Complement Med. 2017;23:310–316. doi: 10.1089/acm.2016.0135. Available from: [DOI] [PubMed] [Google Scholar]
- 32.Howland R.H. Vagus nerve stimulation. Curr Behav Neurosci Rep. 2014;1:64–73. doi: 10.1007/s40473-014-0010-5. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.