Abstract
Background and aim
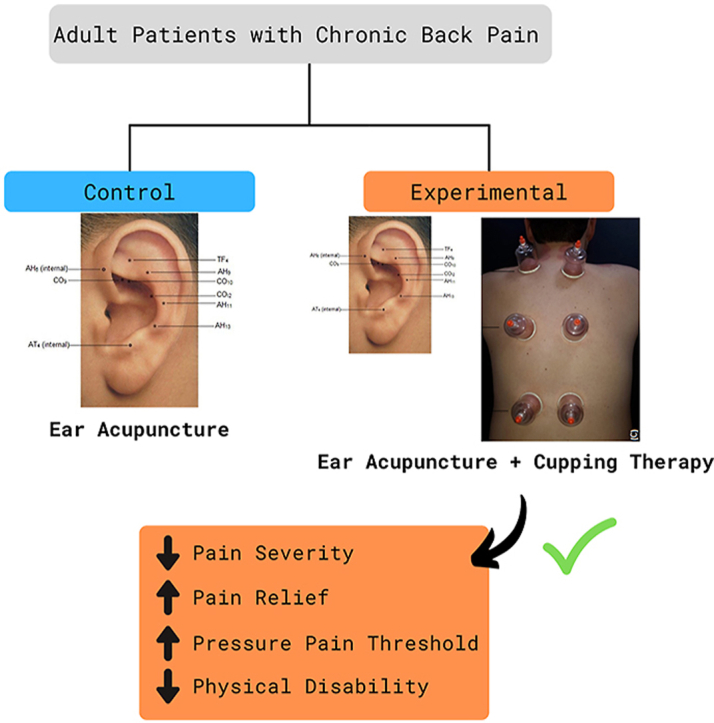
Chronic back pain causes physical, functional, and emotional disabilities. Traditional Chinese Medicine therapies have been shown as interventions to treat chronic back pain. The present study aimed to clinically evaluate the effects of ear acupuncture combined with cupping therapy on people with chronic back pain.
Experimental procedure
We conducted an open-label, randomized, parallel-group controlled clinical trial. Following the CONSORT statement recommendations, 198 participants were randomized into ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups. Data were collected in three different points; before the first session (initial) with the patient, after the last session (final), and seven days after the end of the treatment (follow-up). The Brief Pain Inventory, a digital algometer, and the Rolland Morris Disability Questionnaire were used for data collection. Generalized Estimation Equation model was used to examine the association between the interventions and the primary outcome pain severity.
Results
Pain severity, pressure pain threshold, and physical disability improved over time in both groups. However, for the patients being treated with both ear acupuncture and cupping therapy, significant changes were seen in pain severity, pain relief, and physical disabilities between the initial and final sessions. For the ‘ear acupuncture and cupping therapy’ group, significant changes were also seen for pain relief and physical disability in the follow-up session.
Conclusion
Ear acupuncture combined with cupping therapy was shown to be more effective in the treatment of chronic back pain when compared to treatment using only ear acupuncture.
Keywords: Chronic pain, Back pain, Clinical trial, Ear acupuncture, Cupping therapy
Graphical abstract
Highlights
-
•
Ear acupuncture plus cupping therapy is effective to treat chronic back pain.
-
•
Patients treated with both interventions achieved positive changes in all variables.
-
•
These are interventions that can be implemented in clinical practice.
List of abbreviations
- AH
Antihelix
- AH6
Sympathetic Nerve
- AH13
Cervical Vertebrae
- AH11
Thoracic Vertebrae
- AH9
Lumbosacral Vertebrae
- AT
Antitragus
- AT4
Subcortex
- BL
Bladder
- BPI
Brief Pain Inventory
- CI
Confidence interval for difference set at 95 %
- CG
control group
- CO
Conchae
- CO10
Kidney
- CO9
Bladder
- COI2
Liver
- CONSORT
Consolidated Standards of Reporting Trials
- C
Cupping
- EA
Ear acupuncture
- EG
Experimental group
- GB
Gall Bladder
- IMMPACT
Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials
- LR
Liver
- Qic
Quasi Likelihood Under Independence Model Criterion
- RMDQ
Roland–Morris Disability Questionnaire
- RMASS2
Repeated Measures with Attrition: Sample Sizes for 2 Groups
- TF
Triangular fossa
- TF4
Shenmen
1. Introduction
Chronic back pain is considered a major public health problem worldwide.1 It is associated with physical, functional, and emotional disabilities, in addition to affecting productivity and quality of life of those affected and generating economic burden at the personal, family, business, and government levels.2
Chronic pain is characterized as a pain that lasts longer than three months3 and has a complex clinical presentation.4 The side effects of chronic pain vary substantially across people. In some cases, people with chronic pain experience minimal disruptions in their lives, while in other cases, people become severely disabled and are not able to fulfill work obligations and participate in social and family activities.5
Currently, chronic pain has no cure.5 However, there are interventions available focused on pain relief and improving physical and functional disabilities, which enable people with chronic pain to return to performing activities of daily living and also treat other side effects of long-term chronic pain, such as depression.5,6
Non-pharmacological therapies are more often used in the treatment of chronic pain when compared to the management of acute pain.5 For example, the American College of Physicians strongly recommends the implementation of non-pharmacological therapies, such as acupuncture, as the first choice of treatment for chronic pain.7
Ear acupuncture (耳鍼) and cupping therapies (拔罐) are low-cost treatments with minimal risks to the patient.2,8 Ear acupuncture is used to relieve physical and psychosomatic dysfunctions, by stimulating specific points in the ear.2 Neurological reflexes are a consequence of the stimulation of the ear points, which leads to the release of neurotransmitters and endogenous opioids (endorphins), contributing to pain and inflammation relief.2 Results from a systematic review and meta-analysis showed that ear acupuncture is a nonpharmacological treatment suggested for chronic pain, including back chronic pain.9
Cupping therapy involves the application of cups of various types of materials to an acupoint or area of pain and uses heat or suction to create subatmospheric pressure at the site.10 The underlying processes of pain reduction through cupping therapy are still unclear.10,11 It is believed that the application of the cups similarly stimulates nerve fibers as does acupuncture analgesia. The nerve fibers when stimulated send impulses to the spinal cord and from there to the brain and pituitary gland which, when activated, release chemical transmitters, such as monoamines and endorphins, blocking pain messages.12 The cupping therapy also promotes an increase in peripheral blood circulation, blood detoxification, and activation of the immune system, which can act in relieving the pain.11,13 A systematic review and meta-analysis revealed that cupping therapy is a promising method for the treatment of chronic back pain in adults.14 However, the high heterogeneity and median methodological quality of the clinical trials included in the review limited the findings.14.
Ear acupuncture and cupping therapy can be used alone or combined with other treatments. However, to this date, no study has investigated the effect of ear acupuncture combined with cupping therapy on the treatment of chronic back pain. Therefore, our study aimed to explore the effect of ear acupuncture combined with cupping therapy on back chronic pain. We hypothesized that the participants in the ‘ear acupuncture and cupping therapy’ group would report a decrease in back chronic pain severity, an increase in pain threshold, and improvement in physical disability compared to the ‘ear acupuncture’ group.
2. Materials and methods
2.1. Study design and study population
We conducted an open-label, randomized, parallel-group controlled clinical trial, following the CONSORT statement checklist recommendation.15,16 Our study population consisted of patients aged between 18 and 70 years, presenting chronic back pain (cervical, thoracic, and/or lumbar). The target population was on the waiting list for physical therapy services offered by the outpatient Family Health Strategies program (Estratégias de Saúde da Família) at a town in Brazil, from November 2017 to December 2018.
Patients with a referral to physical therapy services due to the diagnosis of back pain were recruited. Potential participants were contacted via phone calls and screened for chronic back pain that was lasting at least three months.3 As part of the initial screening, the chronic back pain could be of any origin and the patients had to report their pain as moderate to severe (higher than 4 points in a numerical scale from 1 to 11) in the past seven days.3
2.2. Participant eligibility criteria
Patients recruited for the study met the following inclusion criteria: 1) aged between 18 and 70 years; 2) had preserved cognitive function score, according to the 6 Item Cognitive Impairment Test17; 3) were available to participate at the scheduled time for the treatment sessions; 4) were not making continuous use of prescribed adjuvant drugs, such as antidepressants, anxiolytics, anticonvulsants, antipsychotics, and/or muscle relaxants5; 5) were not doing physical therapy at the same time as the study interventions; 6) were not being treated with other energy therapies in the last 3 months previous to the study enrollment; 7) had no infection, inflammation or injury to the ear; 8) were not allergic to metal or microporous tape; 9) did not have any piercings in the ear, for the exception of earrings in the ear lobe; 10) did not present decrease in skin turgor, lesions, inflammation or skin diseases in the dorsal region; 11) did not have other chronic diseases, such as cancer, hemophilia, anemia, neurological or psychiatric disorders10; 12) did not use pacemakers and/or anticoagulants; 10 and 13) were not pregnant or in postpartum period.10
Patients were excluded from the study if 1) they were hospitalized during the study period, 2) used non-opioid analgesics, opioids, nonsteroidal anti-inflammatory drugs, and/or muscle relaxants, orally 24 h or via injections 72 h before the sessions, 3) developed an allergic and/or inflammatory reaction in the ear or the suction cup application site, 4) presented intense pain (pain scored as 8 or higher in a scale from 1 to 11) at the place where the needles were applied in the ear and or where the suction cups were applied, 5) chose to withdraw from the study, or 6) missed two consecutive sessions or exceeded an interval greater than 10 days between them.
2.3. Interventions
In this study, the protocols for implementation of the ear acupuncture by itself and ear acupuncture combined with cupping therapy were developed according to the recommendations from the Standards for Reporting Interventions in Clinical Trials of Acupuncture18 and the Standards for Reporting Interventions in Clinical Trials of Cupping,19 respectively. Both therapies were delivered by a nurse with a specialty in acupuncture and six years of experience in the field. The nurse conducted five sessions of therapies each in the ‘ear acupuncture and cupping therapy’ and ‘ear acupuncture’ groups. The sessions were conducted once a week for each group, for 6 weeks.20,21 In week 6, a follow-up session was conducted to measure the lasting effect of the interventions. No therapy was delivered in week 6.
2.3.1. Ear acupuncture (耳鍼)
For the ear acupuncture therapy, we used semi-permanent, sterile, and disposable needles, of size 0.20 × 1.5 mm, from the brand Complementary Agulhas®. During the therapy, we alternated the ears in each session.20
We started each ear acupuncture session by cleaning the patient's ears with cotton and ethyl alcohol 70 %. We proceed to locate the ear acupoints using the Chinese map recommended by the World Federation of Acupuncture-Moxibustion Societies.22 For greater precision during the insertion of the needles, we used an acupoint finder (EL30 Finder NKL Basic®). The acupoint finder detects changes in the electrical resistance of the acupoint. In the presence of a pathological condition, the acupoint has decreased electrical resistance compared to normal conditions.23 To detect the ear acupoint, we used the finder's option G (Gold points - low impedance or electrical resistance). During the process, the patient would use one hand to hold the reference electrode (2 cm diameter metal rod) while the nurse would slide the finder's red differential pen over the patient's ear to detect the acupoint. The finder device was calibrated using the lowest sensitivity voltage (approximately four in this study) to detect first the Shenmen acupoint and then the other ear acupoints.
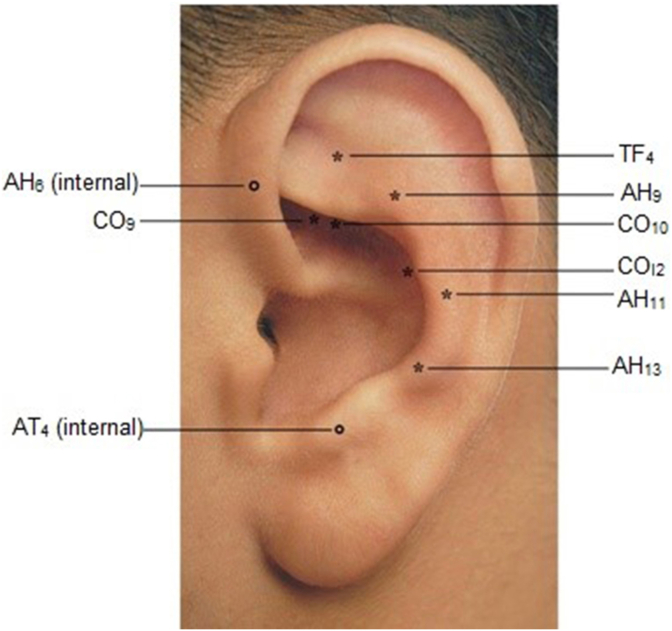
The ear acupoints detected were Shénmén (TF4 - Shenmen), Shèn (CO10 – Kidney), Jiaogan (AH6 - Sympathetic Nerve), Pizhixia (AT4 – Subcortex), Pangguang (CO9 – Bladder), Gan (COI2 – Liver), Jlngzhui (AH13 - Cervical Vertebrae), Xiongzhui (AH11 - Thoracic Vertebrae), and Yaodfzhui (AH9 - Lumbosacral Vertebrae).20 The location of each acupoint in an ear can be seen in Fig. 1.
Fig. 1.
Location of the acupoints for ear acupuncture therapy. Abbreviations: TF - Triangular fossa; AH – Antihelix; CO - Conchae; AT – Antitragus; TF4 – Shenmen; CO10 – Kidney; AH6 – Sympathetic Nerve; AT4 – Subcortex; CO9 – Bladder; COI2 – Liver; AH13 – Cervical Vertebrae; AH11 – Thoracic Vertebrae; AH9 – Lumbosacral Vertebrae. Authors' archive.
The six acupoints TF4, CO10, AH6, AT4, CO9, and COI2 were used for all patients in all sessions. The three acupoints AH13, AH11, and AH9 were used according to the patient's pain complaint site, which varied by patient. Therefore, in each session, between 7 and 9 acupuncture needles were used per patient on the six basic acupoints and one or more of the three acupoints according to the patient's pain site.
The semi-permanent needles were fixated in the patient's ear with a micropore tape and stayed in place for one week. Participants were instructed to not press the needles, as it was not needed due to the non-invasive nature of the needles.
2.3.2. Cupping therapy (拔罐)
We used the non-invasive dry and fixed cupping therapy,12 which promotes stimulation of the acupoints in the same way as the acupuncture needles.24 Acrylic cups of 4.5, 3, or 2.3 cm in diameter (DongYang®) were used according to the location of the application site. A manual suction pump was used to rise the skin inside the cup up to 1.5 cm.25
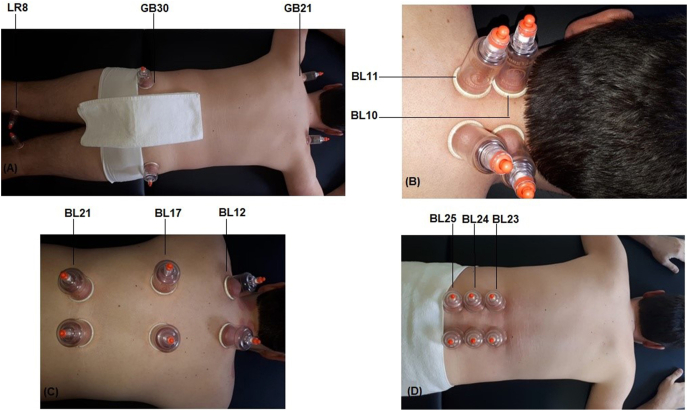
We started each cupping therapy session by cleaning the patient's dorsal region with cotton and ethyl alcohol 70 %. The suction cups were then applied bilaterally to the dorsal region and fixed for 10 min12 on the acupoints Jianjing (Gall Blader 21), Huantiao (Gall Blader 30) e Ququan (Liver 8).26 Depending on the patient's pail location, suction cups were also applied to the acupoints a)Tianzhu (Bladder 10) and Dazhu (Bladder 11) in the cervical region, b) Fengmen (Bladder 12), Geshu (Bladder 17), and Weishu (Bladder 21) in the thoracic region or c) Shenshu (Bladder 23), Qihaishu (Bladder 24), and Dachangshu (Bladder 25) in the lumbar region26 (Fig. 2).
Fig. 2.
Location of the acupoints for cupping therapy. (A) systemic acupoints – for all participants; (B) cervical region acupoints – if the pain was located in the cervical region; (C) thoracic region acupoints – if the pain was located in the thoracic region; (D) lumbar region acupoints – if the pain was located in the lumbar region. Abbreviations: LR – Liver; GB – Gall Bladder; BL – Bladder. Authors' archive.
If the pain was located in the cervical region, the patient received cupping therapy in the following five bilateral acupoints Jianjing (Gall Blader 21), Huantiao (Gall Blader 30), Ququan (Liver 8), Tianzhu (Bladder 10), and Dazhu (Bladder 11). If the pain was located in the thoracic region, the cupping therapy was applied in the following six bilateral acupoints Jianjing (Gall Blader 21), Huantiao (Gall Blader 30), Ququan (Liver 8), Fengmen (Bladder 12), Geshu (Bladder 17), and Weishu (Bladder 21). If the patient had pain in the lumbar region, the cupping therapy was applied bilaterally to the acupoints Jianjing (Gall Blader 21), Huantiao (Gall Blader 30), Ququan (Liver 8), Shenshu (Bladder 23), Qihaishu (Bladder 24), and Dachangshu (Bladder 25). Finally, if the pain was located in the entire dorsal region, the cupping therapy was applied bilaterally to all 11 acupoints.
2.3.2.1. Primary outcome
Our primary outcome was pain severity. We used the Brief Pain Inventory (BPI) Short Form27 to assess the outcome. The BPI has been translated and psychometrically and linguistically validated to Brazilian Portuguese and adapted to the Brazilian culture.28 This instrument uses a numerical scale (from 0 – no pain to 10 – pain as bad as you can imagine) to describe the patient's pain at 1) its worst in the last 24 h, 2) its least in the last 24 h, 3) on average, and the patient's pain 4) at the moment it is being assessed. The median from the results for the four items was used as a measure for the pain severity.29
2.4. Secondary outcomes
The secondary outcomes were pain relief through the interventions,27 pressure pain threshold, and physical disability.30 Pain relief was assessed using the question from the BPI instrument27 that measures how much pain relief pain treatments or medications have been provided to the patient on a scale from 0 % (no relief) to 100 % (complete relief).29
To assess the pressure pain threshold, defined as the minimum amount of pressure that induces pain or sensitivity,31 we used a digital pressure algometer with a capacity of 20 kg-force (kgf) (digital dynamometer model DDK, for tensile and compression tests - Kratos®). The algometer measures the responsiveness of peripheral nociceptors by applying pressure to surfaces on which they are found. The pressure is a measure of the exerted force (weight) upon an area of square centimeters (kilopascal or kilogram/cm2). A protocol developed by Moura et al.32 was used to guide the patient's positioning and the pressure pain threshold assessment. The patient was positioned in a stretcher in the prone position, with their arms extended alongside the body.
Physical disability was measured using the Roland–Morris Disability Questionnaire (RMDQ).30 This questionnaire was developed to assess self-rated physical disability caused by chronic low back pain. The RMDQ has 24 statements that are scored as 0 or 1 (yes/no). The total score ranges from 0 (no physical disability) to 24 points (severe physical disability).33 Clinical improvement in physical disability is identified when there is a reduction of 30 % in RMDQ follow-up scores compared to baseline.34 The RMDQ was translated, adapted, and psychometrically validated to Brazilian Portuguese.30
2.5. Sample size
To estimate sample size, a pilot test was conducted with 20 patients (10 each in the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups). Pain severity was assessed using the BPI instrument.27 The mean difference in pain severity score between groups was 1.42 points at the initial and 0.93 points at the final assessment. Based on the results from the pilot test, the software RMASS2®: Repeated Measures with Attrition: Sample Sizes for 2 Groups35 was used to calculate the sample size. An estimated sample of 77 participants for each group was calculated using a significance level of 5 %, power of 95 %, and effect size of 0.5. To account for potential loss of participants (e.g., dropout, hospitalization, death, or exclusion from the study), the initially estimated sample was corrected by 30 %, which increased the minimal sample size to 99 participants per group (198 participants total).
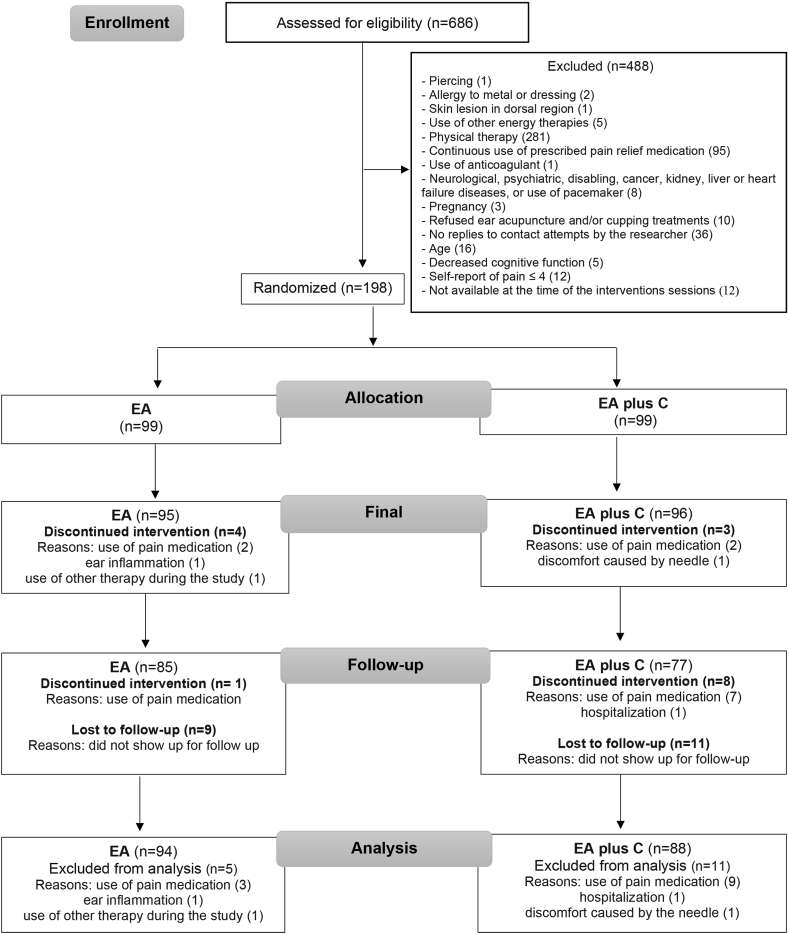
The initial study population consisted of 686 patients with a referral to physical therapy services due to the diagnosis of back pain. Of the 686 patients assessed for eligibility, 488 did not meet the study inclusion criteria. The resulting sample of 198 patients was randomized into the ‘ear acupuncture’ or ‘ear acupuncture + cupping therapies’ groups (Fig. 3).
Fig. 3.
Flowchart illustrating the phases of the study, following the Consolidated Standards of Reporting Trials (CONSORT) recommendations for nonpharmacological interventions. Abbreviations: EA: ear acupuncture; C: cupping.
2.6. Randomization
Randomization of the patients was conducted by a researcher blinded to the study design, using generators from the website Randomization.com (http://www.randomization.com/). A 1:1 ratio was used in the randomization. Each number in the random sequence list was placed in an opaque envelope and given to the nurse only at the patient's initial intervention session.
2.7. Data collection
Data measuring the primary and secondary outcomes were collected by three researchers at 1) the beginning of the patient's first (initial) intervention session, 2) the end of the last (final) intervention session, and 3) seven days after the final intervention session (follow-up). In addition to the instruments used to assess the primary and secondary outcomes, baseline sociodemographic and clinical information were collected at the beginning of the initial intervention session for the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups. The form used was developed by the researchers in this study and evaluated by three pain experts (two nurses and a post-doctoral physical therapist). The same three researchers that collected the outcomes data also collected the baseline sociodemographic and clinical information. For each patient, sex, age, education level, and occupation were collected, along with pain duration (in months), type of pain (ongoing, recurrent), if the patient was unable to practice physical activities due to the pain, fear of moving the body due to the pain, fatigue related to the pain, if the patient had seen a clinician due the complaint of pain, and the frequency of use of pain relief medications (per week/month). Age, education level, and pain duration were treated as continuous variables, while the remaining as categorical variables.
2.8. Statistical analyses
Two of the researchers independently entered the data collected into Microsoft Office Excel sheets. The data entered were checked for consistency and then analyzed using the Statistical Package for the Social Sciences software, version 23.0.
The homogeneity between the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups was verified through the analysis of the demographic and clinical variables. The Shapiro-Wilk test was performed first to test whether the variables followed the normal distribution at a 0.05 significance level. Given the absence of normality, the non-parametric Chi-Square and Mann-Whitney tests were performed at a significance level of 0.05 to compare the distribution of the categorical and continuous variables in the two groups, respectively.
Generalized Estimating Equation models were used to estimate and test the effect of group allocation, adjusting for the effect of time (initial, final, and follow-up sessions) and interaction (group ∗ time), on the outcome variables. The variables were treated assuming a gamma distribution and logarithmic link function. The model with the lowest Quasi Likelihood Under Independence Model Criterion (QIC) and the best fit was considered as the final model (unstructured or interchangeable). Statistical significance was set at p ≤ .05. The Bonferroni posthoc test was used to compare the means of the significant correlations between the predictors and the outcomes.
2.9. Ethical considerations
The present study was registered in a Clinical Trials Registry and approved by an Institutional Ethical Committee (CEAE registration number 75281317.3.0000.5149). Written informed consent was obtained for all patients participating in the study.
3. Results
In total, 198 patients were included and randomized into the ‘ear acupuncture’ or ‘ear acupuncture combined with cupping therapy’ groups. Data from sixteen participants (8.1 %) were excluded from the analyses for the primary and secondary outcomes. These patients were discontinued from the intended treatments due to use of pain medication (n = 12), ear inflammation (n = 1), hospitalization (n = 1), use of other therapy during the study (n = 1), and discomfort caused by the needle (n = 1) (Fig. 3).
Table 1 shows baseline demographic and clinical characteristics for each group. No statistically significant differences at baseline were found between groups. The mean age was 47 years for the ‘ear acupuncture’ group and 48 years for the ‘ear acupuncture and cupping therapy’ group. About 16 and 17 % of patients were male in the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups, respectively. Patients in the ‘ear acupuncture’ group reported back chronic pain lasting an average of 96 months, compared to 102 months for patients in the ‘ear acupuncture and cupping therapy’ group (Table 1).
Table 1.
Participants baseline sociodemographic and clinical information.
| Variables | EA (n = 94) | EA plus C (n = 88) | p-value | |
|---|---|---|---|---|
| Age ( ± sd) | (in years) | 47.87 ± 13.18 | 48.20 ± 11.62 | 0.885a |
| Education level ( ± sd) | (in years) | 8.03 ± 3.94 | 8.48 ± 4.35 | 0.451a |
| Gender (%) | Male | 16.00 | 16.90 | 0.870b |
| Female | 84.00 | 83.10 | ||
| Has an occupation (%) | 58.50 | 55.1 | 0.637b | |
| Pain duration ( ± sd) | (in months) | 96.37 ± 117.47 | 102.19 ± 116.25 | 0.566a |
| Pain type (%) | Ongoing | 41.50 | 44.90 | 0.637b |
| Recurrent | 58.50 | 55.10 | ||
| Cause of pain (as reported by the participant) (%) | Fall | 12.80 | 10.10 | 0.573b |
| Sedentary lifestyle | 3.20 | 4.50 | 0.646b | |
| Physical effort | 57.40 | 61.80 | 0.549b | |
| Otherc | 7.40 | 12.40 | 0.487b | |
| Pathologies diagnosed through imaging testsd | 73.40 | 60.70 | 0.067b | |
| Unable to practice physical activities (%) | 59.60 | 68.50 | 0.207b | |
| Fear of moving the body (%) | 53.20 | 42.70 | 0.156b | |
| Fatigue (%) | 57.40 | 64.00 | 0.361b | |
| Sees a clinician due to the complaint of pain (%) | Never | 44.70 | 47.20 | 0.099b |
| Sporadically | 52.00 | 44.80 | ||
| 1 or more times a week | 3.20 | 7.80 | ||
| Frequency of analgesic/anti-inflammatory and/or muscle relaxant consumption for pain relief (%) | Never | 13.80 | 14.60 | 0.277b |
| Sporadically | 39.40 | 46.10 | ||
| 1 or 2 per month | 10.70 | 2.50 | ||
| 1 or more times a week | 36.20 | 34.90 | ||
: mean; sd: standard deviation.
Abbreviations: EA: ear acupuncture; C: cupping.
Mann-Whitney test.
Qui-Square test.
Emotional factor, age, and overweight/obesity.
Intervertebral disc degeneration, vertebral axis rotational changes, degenerative spine conditions, nerve root compression.
Table 2 shows the mean differences in pain severity (primary outcome) scores for the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups over time. The primary outcome of pain severity was significantly changed by both types of treatments. However, this change was more significant for patients in the ‘ear acupuncture and cupping therapy’ group and statistically different from the patients in the ‘ear acupuncture’ group in the final session. For example, pain severity was 0.8-point lower in the ‘ear acupuncture and cupping therapy’ group when compared to the ‘ear acupuncture’ group. The comparison between sessions within each group revealed statistically significant changes in pain severity from the initial to the final sessions and from the initial to the follow-up session for both the ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups. However, the changes in pain severity scores over time were larger for those patients in the ‘ear acupuncture and cupping therapy’ group.
Table 2.
Changes in pain severity outcome in the two groups over time.
| Pain severity | Group | Mean Difference (CIa) | |||||
| Sessions | |||||||
| Initial | Final | Follow-up | Initial-Final | Final-Follow-up | Initial-Follow-up | ||
| EA (n = 94) | −0.03b (−0.49; 0.42) | 0.80b (0.15; 1.44)∗ | 0.38b (−0.46; 1.21) | 2.15 (1.59; 2.71)∗ | −0.59 (−1.43; 0.24) | 1.56 (0.81; 2.30)∗ | |
| EA plus C (n = 88) | 2.99 (2.33; 3.65)∗ | −1.02 (−0.18;-1.85)∗ | 1.97 (1.30; 2.63)∗ | ||||
∗ Statistical significance.
Abbreviations: EA: ear acupuncture; C: cupping.
Confidence interval for difference set at 95 %.
Mean Difference: Control Group vs Experimental Group.
A statistically significant difference in pain relief was also be seen for both groups in the final and follow-up sessions. The ‘ear acupuncture and cupping therapy’ group reported larger pain relief when compared to the ‘ear acupuncture’ group (Table 3). We did not compare pain relief differences from the initial-final and initial-follow-up sessions because the patients in both groups did not present pain relief before the treatments.
Table 3.
Changes in pain relief outcome in the two groups over time.
| Pain relief | Group | Mean Difference (CIa) | |||||
| Sessions | |||||||
| Initial | Final | Follow-up | Initial-Final | Final-Follow-up | Initial-Follow-up | ||
| EA (n = 94) | – | −5.44b (−10.45; −0.43)∗ | −6.18b (−11.08; −0.72)∗ | – | 0.36 (−3.31; 4.04) | – | |
| EA plus C (n = 88) | – | −0.37 (−3.21; 2.45) | – | ||||
∗ Statistical significance.
Abbreviations: EA: ear acupuncture; C: cupping.
Confidence interval for difference set at 95 %.
Mean Difference: Control Group vs Experimental Group.
We observed a statistically significant increase in pressure pain threshold for both ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups from initial to final sessions, and initial and follow-up sessions. However, there were no statistically significant differences in pressure pain threshold between groups at initial, final, or follow-up sessions (Table 4).
Table 4.
Changes in pain threshold in the two groups over time.
| Pain threshold | Group | Mean Difference (CIa) | |||||
| Sessions | |||||||
| Initial | Final | Follow-up | Initial-Final | Final-Follow-up | Initial-Follow-up | ||
| EA (n = 94) | 0,16b (−0.12; 0.45) | 0,15b (−0.20; 0.51) | 0,08b (−0.26; 0.43) | −0,41 (−0.58; −0.23)∗ | 0.12 (0.04; 0.28) | −0.29 (−0.46; −0.11)∗ | |
| EA plus C (n = 88) | −0.42 (−0.57; −0.26)∗ | 0.05 (−0.11; 0.20) | −0.37 (−0.56; −0.17)∗ | ||||
∗ Statistical significance.
Abbreviations: EA: ear acupuncture; C: cupping.
Confidence interval for difference set at 95 %.
Mean Difference: Control Group vs Experimental Group.
A decrease in physical disability was seen in both groups from initial to final sessions and from initial to follow-up sessions. Patients in the ‘ear acupuncture and cupping therapy’ group had a larger decrease in physical disability scores when compared to the ‘ear acupuncture’ group. Physical disability was on average 1.78 points lower in the ‘ear acupuncture and cupping therapy’ group in the final session and 2.78 points lower in the follow-up session, when compared to the ‘ear acupuncture’ group. Only for the patients in the ‘ear acupuncture’ group, a statistically significant decrease in physical disability was seen from the final to the follow-up sessions (Table 5).
Table 5.
Changes in physical disability in the two groups over time.
| Physical Disability | Group | Mean Difference (CIa) | |||||
| Sessions | |||||||
| Initial | Final | Follow-up | Initial-Final | Final-Follow-up | Initial-Follow-up | ||
| EA (n = 94) | −0.44b (−2.08; 1.20) | 1.78b (0.02; 3.58)∗ | 2.68b (0.65; 4.71)∗ | 5.94 (4.31; 7.57)∗ | −1.65 (−3.18; −0.11)∗ | 4.29 (2.73; 5.84)∗ | |
| EA plus C (n = 88) | 8.17 (6.44; 9.88)∗ | −0.75 (−2.03; 0.54) | 7.42 (5.42; 9.41)∗ | ||||
∗ Statistical significance.
Abbreviations: EA: ear acupuncture; C: cupping.
Confidence interval for difference set at 95 %.
Mean Difference: Control Group vs Experimental Group.
4. Discussion
The results of the present study showed that both ear acupuncture by itself or the combination of ear acupuncture and cupping are favorable therapeutic options for the treatment of chronic back pain. Statistically significant changes in pain severity, pain relief, pressure pain threshold and physical disability from baseline to follow-up were seen for both ‘ear acupuncture’ and ‘ear acupuncture and cupping therapy’ groups over time. However, patients in the ‘ear acupuncture and cupping therapy’ group reported a greater decrease in the primary and secondary outcomes when compared to the ‘ear acupuncture’ group.
Only a few studies have measured and reported improvement in chronic back pain associated with ear acupuncture2,20,21 and cupping therapies.14 A meta-analysis revealed cupping as a promising therapy for the treatment of chronic back pain in adults, showing statistically significant associations between this therapy and a decrease in pain severity and pressure pain threshold.14 Also, randomized clinical trials have shown positive effects of cupping therapy on cervical chronic pain36 and lumbar chronic pain.37 However, our study is the first to compare the effects of ear acupuncture and cupping therapy on chronic pain outcomes.
Our study showed a statistically significant decrease in pain severity in both groups. In the ‘ear acupuncture’ group, we identified a decrease of 38 % in pain severity scores between the initial to the final sessions and 27 % when comparing the initial and follow-up sessions. In the ‘ear acupuncture and cupping therapy’ group, a decrease of 52 % in pain severity was reported from the initial to the final sessions, and of 35 % from the initial pain severity score to the follow-up score. According to the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT),38 our study showed a moderately important improvement in pain severity (≥30 %) for the ‘ear acupuncture’ group and a substantially better improvement for the ‘ear acupuncture and cupping therapy’ group (≥50 %) at the final sessions. A comparison of both groups in the follow-up sessions demonstrated a minimally important improvement in the ‘ear acupuncture’ group (10–20 %) and a moderately important improvement in the ‘ear acupuncture and cupping therapy’ group (≥30 %).
Similar to our results for the ‘ear acupuncture’ group, a study reported a significant reduction in pain severity associated with ear acupuncture, which lasted for seven days.39 As for the cupping therapy, another study investigated the impact of cupping associated with laser therapy on non-specific chronic lumbar pain and reported that five sessions of the combined therapy are effective in decreasing pain.40
Patients in both groups reported pain relief associated with the treatment received. However, patients in the ‘ear acupuncture and cupping therapy’ group reported pain relief 6 % greater by the final and follow-up sessions when compared to patients in the ‘ear acupuncture’ group.
An increase in pressure pain threshold was also seen for patients in both groups. However, there was not a statistically significant difference between groups. People with chronic back pain have a lower pressure pain threshold compared to healthy people.41 The continuous nociceptive stimulus in the spinal cord42 related to chronic pain alters the normal processing of nociceptive and non-nociceptive information and reduces the pressure pain threshold.
A randomized clinical trial did not find a statistically significant increase in pressure pain threshold associated with ear acupuncture for people with musculoskeletal disorders.43 The authors reported that the number of ear acupuncture sessions or the stimulus exerted by the needles in the ear might have not been enough to cause a change in the pressure pain threshold. In contrast, other studies reported an increase in pressure pain threshold associated with cupping therapy for chronic cervical pain36 and chronic lumbar pain.44 Our study was novel in measuring changes to pressure pain threshold for chronic back pain associated with ear acupuncture combined with cupping therapy.
In our study, patients in the ‘ear acupuncture’ group had a significant decrease of 45 % in physical disability by the final treatment session and 32 % when comparing the initial session to the follow-up. Interestingly, the patients in the ‘ear acupuncture and cupping therapy’ group had a significant decrease of 60 % in physical disability by the final treatment session, and of 54 % between the initial and follow-up sessions. Other studies have reported a reduction in physical disability associated with chronic back pain after treatment with ear acupuncture or cupping therapy.1,21,36,37
Finally, our results showed that the combination of ear acupuncture and cupping therapy is effective in the treatment of chronic back pain. The cupping therapy enhanced the effects of ear acupuncture on pain outcomes by 24 % by the final session and 30 % by the follow-up. These results are innovative and emphasize the benefits of combining ear acupuncture and cupping therapies in the treatment of chronic back pain to improve, especially, physical disability resulting from pain.
This study is not without limitations. The use of standardized protocols for the application of the interventions is contrary to the basic precepts of Traditional Chinese Medicine and can be seen as a limitation for the applicability and relevance of our results. Nonetheless, the use of standardized protocols allows for the reproducibility of our methods and results.
It is important to note that the participant losses (4.95 % in the ‘ear acupuncture’ and 10.89 % in the ‘ear acupuncture and cupping therapy’ groups) during the study were accounted for by the 30 % increase in the initially estimated sample. Thus, the minimal estimated sample size needed to avoid bias in our analysis was still achieved and the intention-to-treat analysis was not needed.45
Future studies investigating the effects of ear acupuncture combined with cupping therapies in different health care settings are needed to contribute with more consistent scientific evidence about the effectiveness of the therapies on pain control for chronic back pain, which is considered one of the major health challenges today. We believe it is also important to extend this investigation to other types of pain, since different forms of pain may respond differently to these therapies. In addition, the effects of ear acupuncture combined with cupping therapy should be explored for other physiological biomarkers, such as inflammatory markers and tissue temperature.
5. Conclusion
In conclusion, the antinociceptive effects of ear acupuncture and cupping therapies combined in our study caused a greater decrease in pain severity for the patients in the ‘ear acupuncture and cupping therapy’ group. Chronic back pain can cause physical disability to varying degrees,5 which consequently negatively impacts the quality of life, performance of daily activities, sleep patterns, in addition to leading to absenteeism, presenteeism, and early retirement.46 Thus, these two interventions can be potentially considered alternative therapies, which can help in the treatment, rehabilitation, and prevention of chronic back pain, and improvement of quality of life.
Taxonomy (classification by EVISE)
Acupuncture; Pain Disorder; Traditional Chinese Medicine; Clinical Trial.
Funding
This work was supported by the Research Support Foundation of the State of Minas Gerais (FAPEMIG) [grant number: APQ-01681-18]; the National Council of Technological and Scientific Development [grant number: 443826/2018-8]; and Coordination for the Improvement of Higher Education Personnel (CAPES) [Financing Code 001], Brazil.
Clinical trial registration
RBR-9h77k7, Brazilian Clinical Trials Registry.
Declaration of competing interest
The authors confirm they have no conflict of interest.
Acknowledgments
This manuscript is part of a thesis by Caroline de Castro Moura for her Ph.D. in Nursing degree from the Federal University of Minas Gerais, Brazil.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Contributor Information
Caroline de Castro Moura, Email: caroline.d.moura@ufv.br.
Erika de Cássia Lopes Chaves, Email: echaves@unifal-mg.edu.br.
Denismar Alves Nogueira, Email: denismar.nogueira@unifal-mg.edu.br.
Denise Hollanda Iunes, Email: deniseiunes@unifal-mg.edu.br.
Hérica Pinheiro Corrêa, Email: hericapc@yahoo.com.br.
Gabriela Aparecida Pereira, Email: gabrielaaparecida100@yahoo.com.br.
Higor Magalhães Silvano, Email: higormagalhaes19@gmail.com.
Cissa Azevedo, Email: cissa.ufsj@gmail.com.
Tamara Goncalves Rezende Macieira, Email: tmacie2@ufl.edu.
Tânia Couto Machado Chianca, Email: tchianca@enf.ufmg.br.
References
- 1.Moura C.C., Chaves E.C.L., Chianca T.C.M., et al. Contribution of Chinese and French ear acupuncture for the management of chronic back pain: a randomized controlled trial. J Clin Nurs. 2019;28:3796–3806. doi: 10.1111/jocn.14983. [DOI] [PubMed] [Google Scholar]
- 2.Artioli D.P., Tavares A.L., Bertolini G.R. Auriculotherapy: neurophysiology, points to choose, indications and results on musculoskeletal pain conditions: a systematic review of reviews. Br J Pain. 2019;2(4):356–361. doi: 10.5935/2595-0118.20190065. [DOI] [Google Scholar]
- 3.Treede R.D., Rief W., Barke A., et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11) Pain. 2019;160:19–27. doi: 10.1097/j.pain.0000000000001384. [DOI] [PubMed] [Google Scholar]
- 4.Barker A. 2019. Chronic Pain has arrived in the ICD-11. Retrieved from https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=8340&navItemNumber=643. [Google Scholar]
- 5.Maher C., Underwood M., Buchbinder R. Non-specific low back pain. Lancet. 2017;389:736–747. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 6.Lim T.K., Ma Y., Berger F., et al. Acupuncture and neural mechanism in the management of low back pain-an update. Medicine. 2018;5:1–34. doi: 10.3390/medicines5030063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qaseem A., Wilt T.J., McLean R.M., et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 8.Chi L.M., Lin L.M., Chen C.L., et al. The effectiveness of cupping therapy on relieving chronic neck and shoulder pain: a randomized controlled trial. Evid Based Complement Alternat Med. 2016;2016:1–7. doi: 10.1155/2016/7358918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vieira A., Reis A.M., Matos L.C., et al. Does auriculotherapy have therapeutic effectiveness? An overview of systematic reviews. Compl Ther Clin Pract. 2018;33:61–70. doi: 10.1016/j.ctcp.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Aboushanab T.S., Alsanad S. Cupping therapy: an overview from a modern medicine perspective. J Acupunct Meridian Stud. 2018;11:83–87. doi: 10.1016/j.jams.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Al-Bedah A.N.M., Elsubai I.S., Qureshi N.A., et al. The medical perspective of cupping therapy: effects and mechanisms of action. J Tradit Complement Med. 2019;9:90–97. doi: 10.1016/j.jtcme.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rozenfeld E., Kalichman L. New is the well-forgotten old: the use of dry cupping in musculoskeletal medicine. J Bodyw Mov Ther. 2016;20:173–178. doi: 10.1016/j.jbmt.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Zeng K., Wang J.W. Clinical application and research progress of cupping. J Acupunct Tuina Sci. 2016;14:300–304. doi: 10.1007/s11726-016-0940-4. [DOI] [Google Scholar]
- 14.Moura C.C., Chaves E.C.L., Cardoso A.C.L., et al. Cupping therapy and chronic back pain: systematic review and meta-analysis. Rev Lat Am Enfermagem. 2018;26:1–9. doi: 10.1590/1518-8345.2888.3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Consort . 2010. The CONSORT flow diagram. Retrieved from http://www.consort-statement.org/consort-statement/flow-diagram. [Google Scholar]
- 16.Consort . 2010. CONSORT 2010 checklist of information to include when reporting a randomised trial. Retrieved from http://www.consort-statement.org/consort-2010. [Google Scholar]
- 17.Brooke P., Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatr. 1999;14:936–940. doi: 10.1002/(SICI)1099-1166(199911)14:11<936::AID-GPS39>3.0.CO;2–1. [DOI] [PubMed] [Google Scholar]
- 18.Macpherson H., Altman D.G., Hammerschlag R., et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7:1–11. doi: 10.1371/journal.pmed.1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X., Tian R., Lam W.C., et al. Standards for reporting interventions in clinical trials of cupping (STRICTOC): extending the CONSORT statement. Chin Med. 2020;15:1–15. doi: 10.1186/s13020-020-0293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moura C.C., Chaves E.C.L., Cardoso A.C.L., et al. Auricular acupuncture for chronic back pain in adults: a systematic review and metanalysis. Rev. Esc. Enferm. USP. 2019;53:1–13. doi: 10.1590/S1980-220X2018021703461. [DOI] [PubMed] [Google Scholar]
- 21.Moura C.C., Iunes D.H., Ruginsk S.G., et al. Action of ear acupuncture in people with chronic pain in the spinal column: a randomized clinical trial. Rev Lat Am Enfermagem. 2018;26:1–9. doi: 10.1590/1518-8345.2678.3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Federation of Acupuncture-Moxibustion Societies WFAS Auricular acupuncture point (WFAS STANDARD-002: 2012) World J Tradit Chin Med. 2013;23:12–21. doi: 10.1016/S1003-5257(13)60055-0. [DOI] [Google Scholar]
- 23.Suen L.K.P., Wong T.S.K., Chung J.W.Y., et al. Auriculotherapy on low back pain in the elderly. Compl Ther Clin Pract. 2007;13:63–69. doi: 10.1016/j.ctcp.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Tham L.M., Lee H.P., Lu C. Cupping: from a biomechanical perspective. J Biomech. 2006;39:2183–2193. doi: 10.1016/j.jbiomech.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 25.Hekmatpou D., Moeini L., Haji-nadali S. The effectiveness of wet cupping vs. venesection on arterial O2 saturation level of cigarette smokers: a randomized controlled clinical trial. PaK J Med Sci. 2013;29:1349–1353. doi: 10.12669/pjms.296.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization WHO . World Health Organization; Manila: 2008. WHO Regional Office for the Western Pacific: WHO Standard Acupuncture Point Locations in the Western Pacific Region. [Google Scholar]
- 27.Daut R., Cleeland C., Flanery R. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17:197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- 28.Ferreira K.A., Teixeira M.J., Mondonza T.R., et al. Validation of brief pain inventory to Brazilian patients with pain. Support Care Canc. 2011;19:505–511. doi: 10.1007/s00520-010-0844-7. [DOI] [PubMed] [Google Scholar]
- 29.Cleeland C.S. 2009. The brief pain inventory - user guide. Retrieved from https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf. [Google Scholar]
- 30.Sardá Júnior J.J., Nicholas M.K., Pimenta C.A.M., et al. Validation of the Roland Morris disability questionnaire for general pain. Rev Dor. 2010;11:28–36. [Google Scholar]
- 31.Fischer A.A. Pressure threshold measurements for diagnosis of myofascial pain and evaluation of treatment results. Clin J Pain. 1987;2:207–211. [Google Scholar]
- 32.Moura C.C., Iunes D.H., Agostinho A.A.M., et al. Assessment and correlation between subjective and physiological variables of chronic spinal pain. Revista Dor. 2017;18:194–198. doi: 10.5935/1806-0013.20170102. [DOI] [Google Scholar]
- 33.Roland M., Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Jordan K., Dunn K.M., Lewis M., et al. A minimal clinically important difference was derived for the Roland-Morris Disability Questionnaire for low back pain. J Clin Epidemiol. 2006;59:45–52. doi: 10.1016/j.jclinepi.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 35.Hedeker D., Gibbons R.D., Waternaux C. Sample size estimation for longitudinal designs with attrition: comparing time-related contrasts between two groups. J Educ Behav Stat. 1999;24:70–93. doi: 10.3102/10769986024001070. [DOI] [Google Scholar]
- 36.Saha F.J., Schumann S., Cramer H., et al. The effects of cupping massage in patients with chronic neck pain - a randomised controlled trial. J Complement Med Res. 2017;24:26–32. doi: 10.1159/000454872. [DOI] [PubMed] [Google Scholar]
- 37.Volpato M.P., Breda I.C.A., Carvalho R.C., et al. Single cupping therapy session improves pain, sleep, and disability in patients with nonspecific chronic low back pain. J Acupunct Meridian Stud. 2020;13:48–52. doi: 10.1016/j.jams.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Dworkin R.H., Turk D.C., Wyrwich K.W., et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 39.Eberhardt T.D., Hofstätter L.M., Lopes S.M.S., et al. Analgesic comparison of Zen Shiatsu and auricular acupuncture in back pain among nursing professionals. Rev Enferm UFPI. 2015;23:324–330. doi: 10.12957/reuerj.2015.9616. [DOI] [Google Scholar]
- 40.Lin M.L., Wu J.H., Lin C.W., et al. Clinical effects of laser acupuncture plus Chinese cupping on the pain and plasma cortisol levels in patients with chronic nonspecific lower back pain: a randomized controlled trial. Evid Based Complement Alternat Med. 2017;2017:1–7. doi: 10.1155/2017/3140403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Farasyn A., Lassat B. Cross friction algometry (CFA): comparison of pressure pain thresholds between patients with chronic non-specific low back pain and healthy subjects. J Bodyw Mov Ther. 2016;20:224–234. doi: 10.1016/j.jbmt.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 42.Imamura M., Alfieri F.M., Filippo T.R.M., et al. Pressure pain thresholds in patients with chronic nonspecific low back pain. J Back Musculoskelet Rehabil. 2016;29:327–336. doi: 10.3233/BMR-150636. [DOI] [PubMed] [Google Scholar]
- 43.Moura C.C., Chaves E.C.L., Chianca T.C.M., et al. Effects of auricular acupuncture on chronic pain in people with back musculoskeletal disorders: a randomized clinical trial. Rev Esc Enferm USP. 2019;53:1–9. doi: 10.1590/S1980-220X2018009003418. [DOI] [PubMed] [Google Scholar]
- 44.Markowski A., Sanford S., Pikowski J., et al. A pilot study analyzing the effects of Chinese cupping as an adjunct treatment for patients with subacute low back pain on relieving pain, improving range of motion, and improving function. J Alternative Compl Med. 2014;20:113–117. doi: 10.1089/acm.2012.0769. [DOI] [PubMed] [Google Scholar]
- 45.Altman D.G., Schulz K.F., Moher D., et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663–694. doi: 10.20996/1819-6446-2011-7-1-110-116. [DOI] [PubMed] [Google Scholar]
- 46.Dueñas M., Ojeda B., Salazar A., et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–467. doi: 10.2147/JPR.S105892. [DOI] [PMC free article] [PubMed] [Google Scholar]