Abstract
Background
COVID-19 pandemic has affected people with multiple sclerosis (PwMS) on various levels. Pandemic lockdown influenced the access to typical measures of physical activity such as out-door training or gym exercises.
Methods
We performed a survey assessing physical activity during pandemic lockdown among PwMS treated in our MS center. The questionnaire encompassed questions regarding physical activity before and during lockdown, including the employment of online technologies.
Results
The survey was completed by 262 PwMS. Physical activity before lockdown was declared by 74.4% of PwMS, regular exercises were declared by 30.9% of participants. Among physically active PwMS 50.5% limited their physical activity during the COVID-19 lockdown. The decrease in physical activity was reported more frequently by PwMS with higher levels of disability, particularly declaring regular exercises before lockdown. In the opinion of 39,7% of PwMS online training could replace standard exercises, however only 19,9% of PwMS were actively looking for online training during the lockdown. The interest in online exercise was greatest in the group ≤30 years of age and EDSS ≤2. Synchronous exercises were the preferred online training, particularly among PwMS with EDSS≥4.
Conclusion
Our findings indicate a need for systematic educational and organizational measures, promoting physical activity among PwMS and acknowledging pandemic conditions.
Keywords: Multiple sclerosis, Physical activity, COVID-19, Online training
1. Introduction
Multiple sclerosis (MS) is a chronic autoimmune disease of central nervous system (CNS) affecting young and middle aged people all around the world. Poland is a high prevalence region of MS (Kapica-Topczewska et al., 2018). Coronavirus disease (COVID-19) pandemic quarantine limited access to health care, rehabilitation and physical activity outside the home for many patients.
Clinical efficacy of physical activity and rehabilitation has been increasingly well documented in MS (Centonze et al., 2020). Numerous functional parameters, important for the everyday living, were shown to be positively influenced by physical exercises in MS patients, including: muscular fitness, ambulatory performance, balance, spasticity, cardiovascular fitness (Platta et al., 2016; Barclay et al., 2019; Yazgan et al., 2019). Also pain, mood disorders, fatigue and cognitive functions can be improved by physical exercises in MS patients (Barclay et al., 2019; Yazgan et al., 2019; Ozkul et al., 2020; Demaneuf et al., 2019). In general, multiple reports indicate that physical activity exerts beneficial effects on quality of life of people with MS (PwMS) (Centonze et al., 2020; Barclay et al., 2019; Yazgan et al., 2019). The biological mechanisms underlying the effects of physical activity have been investigated in experimental models of MS as well as in clinical settings. The influence on numerous processes in the CNS have been suggested, including demyelination, remyelination, neuroprotective activity and axonal regeneration as well as modulation of immune regulatory and metabolic mechanisms (Afzal et al., 2020; Di Liegro et al., 2019; Guo et al., 2020; Kjølhede et al., 2018).
Despite the evidence of the safety and beneficial effects of physical activity on many clinical aspects of the disease, PwMS are less active than the healthy controls (Kinnett-Hopkins et al., 2017). Currently, it can be assumed that the quarantine enforced by the governmental regulations could exacerbate this undesirable situation.
Recent recommendations for physical activity of PwMS include different exercise strategies, depending on the degree of disability (Kalb et al., 2020; Casey et al., 2018). These recommendations include many different forms of physical activity dedicated to MS patients, such as aerobic activity (e.g., walking, rowing, jogging, aquatic activities), resistance training (e.g., free weights, resistance bands) and neuromotor training (e.g. exercises focusing on balance, coordination, gait) (Mostert and Kesselring, 2002; Kierkegaard et al., 2016). Recently, wide range of innovative systems delivering rehabilitation outside of a hospital and home have been evaluated. Several systematic reviews indicated that telerehabilitation was effective for patients with many musculoskeletal (Cottrell et al., 2017) and neurological conditions including MS (Yeroushalmi et al., 2019). It was concluded that technology based distance physical rehabilitation interventions including internet training increase physical activity of patients with MS (Rintala et al., 2018) and improve motor symptoms (Di Tella et al., 2020; Dlugonski et al., 2012). Participants of online synchronous (real-time) and asynchronous trainings reported a high acceptance and satisfaction, however lower compliance (Tallner et al., 2012).
The COVID-19 pandemic has impacted all aspects of health care delivery. Beginning on March 24, 2020 to the end of May 2020 inhabitants of Poland were not allowed to leave home unless necessary. The gyms, swim pools, outdoor playing areas as well as rehabilitation clinics were closed. Ten weeks of lockdown restriction, due to COVID-19 pandemic, forced some PwMS to looking for new space and type of physical activity. In our study, we analyzed the impact of pandemic lockdown on physical activity of PwMS including their opinions and behavior concerning the use of internet tools in their daily physical activity under the completely new and unexpected conditions of lockdown.
2. Materials and methods
2.1. Participants and procedures
Participants with relapsing-remitting MS (RRMS) diagnosed according to McDonald criteria 2010 were recruited among the patients treated with disease modifying therapy (DMT) in MS center in Department of Neurology Medical University of Lodz, one of the largest MS centers in Poland, following over 700 PwMS across the country. The physical activity questionnaire was collected after 10 weeks of country lockdown due to COVID-19 pandemic. All the patients coming to the Neurology Outpatient Clinic for their routine visits associated with MS therapy program in the period from June to August 2020 were asked to complete the questionnaire. The survey questionnaire was anonymous and participation was voluntary. Ethical review and approval were waived for this study. All the patients participating in the study declared unlimited access to Internet. All the patients recruited into the study were neurologically stable during the past 3 months. Participants were divided according to age and Expanded Disability Status Scale score (EDSS) for more detailed analysis.
The physical activity questionnaire was designed for this study and consisted of eight questions :
-
1
Before the pandemic lockdown, did you do any physical activity?
-
2
Please mark the type of activity: running; cycling; gym; Nordic walking; yoga/gymnastics; others.
-
3
Before the pandemic lockdown, did you participate in the rehabilitation due to disability associated with MS ?
-
4
Before the pandemic lockdown, did you participate in the rehabilitation / physical activity online? Was the training conducted in real time?
-
5
Did the pandemic lockdown limited your physical activity?
-
6
Did you look for online training during the pandemic lockdown?
-
7
In your opinion, could online training replace the traditional training?
-
8
Would you prefer training at home with the use of the internet in the form of: recorded exercises or real time contact with the trainer?
Regular physical activity was defined as training at least three times a week. Analyses were performed with Statistica 13, Statsoft (Cracow, Poland). Data are expressed as absolute scores and percentage distribution, based on the total responses. The questionnaires did not contain missing values.
3. Results
3.1. Study population
Participants ranged in age from 18 to 67 years; the mean age of the MS patients was 42,5 years (SD=11,8). In regard to gender identity, 191 (72,9%) were women and 71 (27,1%) were men. Mean disease duration was 10,41 years (SD=7,51) and mean EDSS score was 2,58 (SD=1,5). 9,2% of patients had comorbidities, the most common was hypertension (25% of all comorbidities). See Table 1 for demographic data.
Table 1.
Study population demographics.
| Total number of patients | N = 262 |
|---|---|
| Age (years), mean (SD); median | 42,5 (11,8); 43 |
| Female/ Male ratio | 191/71 |
| Disease duration (years), mean (SD); median | 10,41 (7,51); 10 |
| EDSS, mean (SD); median | 2,74 (3,01); 2,5 |
| Age ≤30 | 44 (16,8%) |
| Age 31–50 | 151 (57,5%) |
| Age ≥51 | 67 (25,8%) |
| EDSS 0–2 | 117 (44,7%) |
| EDSS 2.5–3.5 | 84 (32,0%) |
| EDSS ≥4 | 61 (23,3%) |
SD – standard deviation.
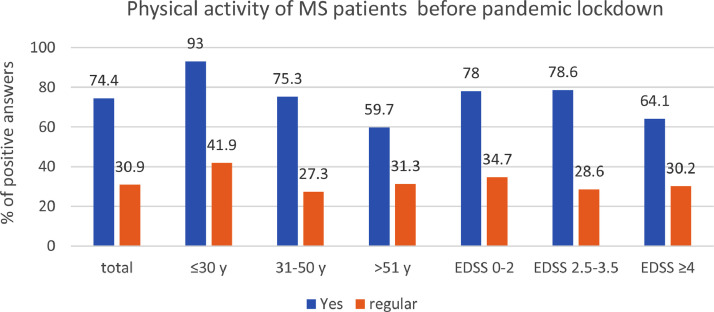
3.2. Physical activity of PwMs before COVID-19 pandemic lockdown in Poland
Two hundred sixty two (262) PwMS filled out the questionnaire during their routine visits in the MS center. 74.4% of surveyed PwMS declared physical activity before the lockdown, whereas regular exercises, defined as training at least three times a week, were declared by 30.9% of participants (Fig. 1 ). The youngest patients (up to 30 years of age) were the most physically active. According to the survey, exercises were performed before the start of the pandemic lockdown by 93% of patients in this age group. Also the regular physical activity was the most frequent among the youngest MS patients, however it was declared only by 41.9% of participants in this age group (as compared to 27.3% and 31.3% in groups 31–50 years and ≥ 51 years, respectively). The lowest physical activity was observed in patients older than 50 years (59.7%) and in the group with the level of physical disability described as EDSS≥4 (64.1%).
Fig. 1.
Physical activity of PwMS before COVID-19 pandemic lockdown according to age and EDSS status. 74.4% of MS patients declared performing physical activity; 30.9% of MS patients declared regular exercises before lockdown. PwMS up to 30 years of age were the most active (93% of patients declared physical activity), the lowest physical activity was declared by patients over 51 years of age (59.7%) and in the group with EDSS ≥4 (64.1%).
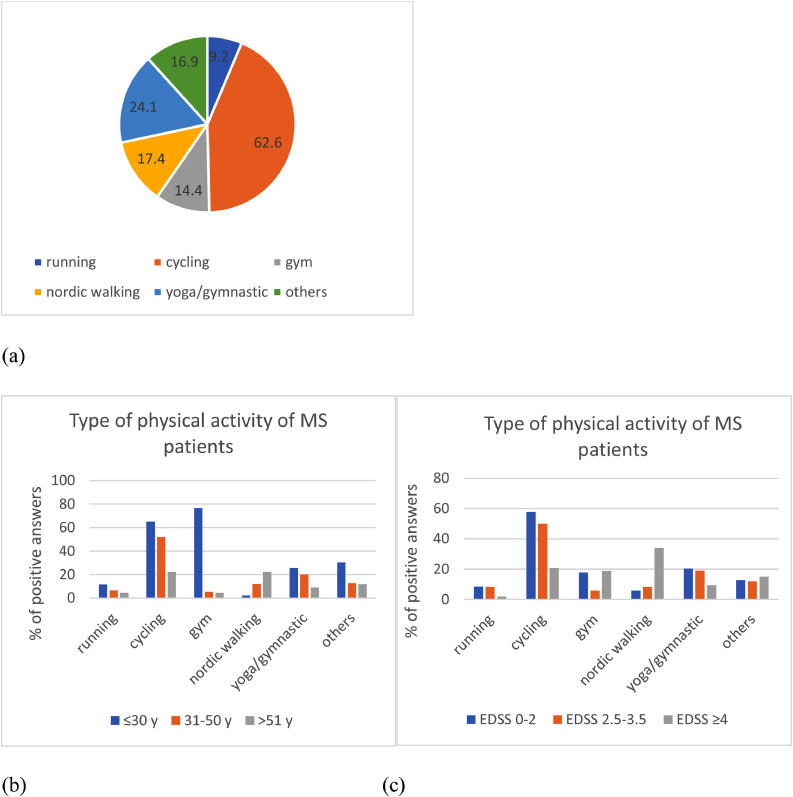
Independently of age, the most popular form of physical activity was cycling (62.6% of PwMS). Notably, younger PwMS were more likely to choose exercises at the gym (76.7% of patients ≤30 years). Nordic walking was preferred form of physical activity in the groups with more advanced physical disability (EDSS≥4) and age (≥51 years) – 34% and 22.3%, respectively (Fig. 2 ).
Fig. 2.
Structure of physical activity of PwMS before the COVID-19 pandemic lockdown. (a) The types of preferred physical activity declared in the whole group of surveyed PwMS. (b) Preferred physical activity according to age. (c) Preferred physical activity according to the level of neurological disability as measured by EDSS.
Only 9.5% of total PwMS participated in physical activity online before the COVID-19 pandemic. Among them usage of real time (synchronous) form of online exercises was declared by small proportion of participants (1.9% of the whole group). In the youngest group of patients (≤30 years) participation in the online training was the highest and reached 20.9% before lockdown.
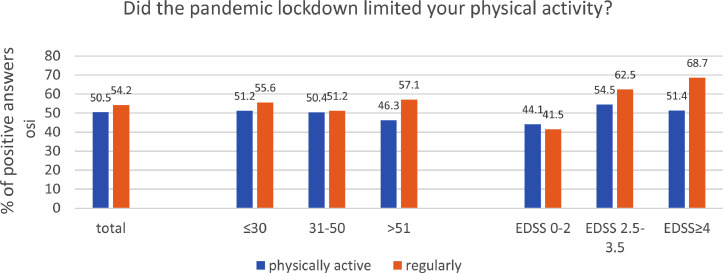
3.3. Impact of lockdown restrictions on physical activity of PwMs
According to our survey 44.7% of the whole group of PwMS, 50.5% of physically active PwMS and 54.2% of PwMS performing regular exercises limited their physical activity during the COVID-19 lockdown. The influence of pandemic restriction on physical activity was similar in particular age groups. However, the negative effects were more pronounced in patients with higher levels of disability, particularly among PwMS declaring regular exercises (Fig. 3 ).
Fig. 3.
The impact of the COVID-19 lockdown restrictions on PwMS physical activity; according to PwMS age and EDSS score.
3.4. The role of online training during the COVID-19 lockdown
Nearly one fifth (19.9%) of PwMS answered that they were looking for training online during the lockdown. The active interest in online exercise was greatest in the group ≤30 years of age (32.6%) and with EDSS ≤2 (28%). Importantly, in the opinion of 39.7% of PwMS online training could replace standard exercises. This opinion was the most popular among the youngest patients with MS (53.4%). Synchronous online exercises were preferred by more participants of the survey than the asynchronous online training (53.8% vs. 31.7%, respectively). The difference was particularly pronounced in the group of MS patients with neurological disability defined as EDSS≥4. 64.2% of these patients chose synchronous training, whereas 18.9% preferred asynchronous training (Table 2 ).
Table 2.
The role of online training in the physical activity of PwMS during COVID-19 pandemic.
| Survey question(% of positive answers) | Total | ≤30 y. | 31–50 y. | >50 y. | EDSS 0–2 | EDSS 2.5–3.5 | EDSS≥4 |
|---|---|---|---|---|---|---|---|
| Before the pandemic, did you participate in online training? | 9.5% | 20.9% | 7.3% | 7.5% | 14.4% | 3.6% | 5.7% |
| Did the pandemic lockdown limited your physical activity? | 44.7% | 51.2% | 43.3% | 44.8% | 42.4% | 46.4% | 45.3% |
| Did you look for online training during the lockdown? | 19.4% | 32.6% | 18% | 14.8% | 28% | 10.7% | 13.2% |
| In your opinion, could online training replace the standard exercises? | 39.7% | 53.4% | 36.7% | 35.8% | 44.1% | 32.1% | 43.4% |
| Preferred type of online trainings: -synchronous -asynchronous |
53.8% 31.7% |
44.2% 44.2% |
57.3% 26.7% |
53.7% 32.7% |
53.4% 38.2% |
47.6% 32.1% |
64.2% 18.9% |
4. Discussion
In our study we analyzed the self-reported physical activity of PwMS before and during the social restrictions introduced in Poland due to the COVID-19 pandemic. Significant proportion of PwMS (74.4%) declared physical activity in general before the pandemic. However, less than one third of the group admitted performing the exercises regularly, at least three times a week. The questionnaire used in our study does not allow for the detailed quantitative analysis of the level of physical activity. Nevertheless, we believe that our data stay in line with earlier findings including a study demonstrating that the rate of physical activity was insufficient in almost 60% of a group of over 1500 PwMS (Motl et al., 2015).
Moreover, the results of our study indicate that half of the physically active PwMS reduced their physical activity under the COVID-19 lockdown conditions. This observation is analogous to the results published most recently by Kalron and colleagues (Kalron et al., 2021). Based on the online survey filled out by 120 Israeli PwMS, the authors demonstrated that ca. 50% of responders ceased or decreased their physical activity during the COVID-19 pandemic (Kalron et al., 2021). Importantly, the mean age in this PwMS group was very close to our patients. Due to the lack of EDSS data in the Israeli group the direct comparison of neurological status is not possible. However, the high proportion of patients who did not use any walking assistance, suggests also similar level of disability to our population. Since as yet there are no other publications on this topic, these similarities seem to strengthen mutually the importance of the results presented in both reports.
In our study the self-reported physical activity was the lowest among the oldest patients and patients with the highest level of neurological disability (≥50 years and EDSS≥4, respectively). Interestingly, the most prominent influence of pandemic restrictions was observed on regular physical exercises in the group of patients with EDSS≥4. Most probably, this observation can be at least partially related to the structure of declared physical activity. Nordic walking was preferred form of exercise in the group with EDSS≥4 and exactly this form of activity was particularly hampered by the enforced lockdown conditions. The decrease in physical activity may be also associated with broad psychological effects of COVID-19 pandemic, including increase in anxiety, depression and fatigue levels, which have been demonstrated in various populations of PwMS (Naser Moghadasi, 2020; Costabile et al., 2021; Motolese et al., 2020). In the recent study analyzing the relationship between mental distress, disability and coping strategies under COVID-19 lockdown in Italy, the authors found that 70% of PwMS perceived higher risk of SARS-COV-2 infection than general population (Costabile et al., 2021). In the context of our observations it is worth to indicate, that the mental distress in MS may be additionally potentiated by dysfunctional coping, especially in patients with significant mental and physical disability (Costabile et al., 2021; Holland et al., 2019). Additionally, the newly published post-hoc analysis of the data obtained in the aforementioned Italian group demonstrates, that physical exercise may protect from the detrimental effects of disability on mental health of PwMS (Carotenuto et al., 2021).
The negative change in physical activity behavior reported by the significant proportion of PwMS in our group might potentially bear important clinical consequences. As described earlier, physical exercise is associated with multiple beneficial effects in MS (Centonze et al., 2020; Yazgan et al., 2019; Ozkul et al., 2020; Demaneuf et al., 2019). The recently published meta-analysis of studies evaluating the role of different kinds of non-pharmacological interventions in the symptomatic treatment of MS patients, showed that physical exercise had the greatest influence, improving fatigue, function, and balance (Byrnes and Whillier, 2019). A potential involvement of exercises in the control and modulation of disease activity have been also discussed (Pilutti et al., 2014; Dalgas et al., 2019), including MRI outcomes (Kjølhede et al., 2018). Most importantly however, discontinuation of physical activity seems to be associated with a return to pre-intervention functional status (Charron et al., 2018). Additionally, it has been postulated that adjuvant therapeutic role of physical exercises in MS may be subjected to similar “window of opportunity” as pharmacological treatment (Riemenschneider et al., 2018). This fact seems to be of particular meaning in the planning of MS patients care in the era of pandemic restrictions, when any constrictions of physical activity may be potentially associated with long lasting consequences. Of great importance in the aforementioned context are the recently published results of the study assessing the impact of COVID-19 home confinement on physical and psychological characteristics of PwMS (Andreu-Caravaca et al., 2021). The analysis revealed a worsening in functional capacity as well as a lower physical self-perception and a greater anxiety state in group of 17 PwMS after 2 months of home confinement (Andreu-Caravaca et al., 2021). One of the possible solutions in this situation is the employment of tele-rehabilitation techniques, especially programs that have been developed specifically for PwMS (Centonze et al., 2020; Dlugonski et al., 2011). In our study nearly 40% of responders expressed positive opinion regarding online training as a replacement for traditional exercises. However, the percentage of patients, who in fact looked for this kind of physical activity during pandemic restrictions, was much lower. The active search for online tele-rehabilitation was declared more frequently in patients younger and with lower disability levels. The level of interest in receiving telerehabilitation by Belgian PwMS reported recently by Remy and colleagues was ca. 50% higher than in our group (Remy et al., 2020). Although the mean age and EDSS score of PwMS in our study were similar to the Belgian group, there are multiple other factors not included in our analysis which could be potentially responsible for this discrepancy. Possible differences include: available telecommunication technologies (even among PwMS declaring an access to Internet), education and employment status, other socioeconomic factors as well as intensity of mood disorders and cognitive disability. Importantly, in accordance with our observations, PwMS with higher level of disability in the Belgian group were less likely to be interested in a program of physical exercises provided via online technologies (Remy et al., 2020). The lower interest in online training in the case of older and more physically disabled PwMS may reflect an existence of more pronounced deficits in social engagement in this group of patients. In agreement with this assumption, synchronous online exercises, offering a live contact with the trainer, were clearly more popular among PwMS in our study, and this preference was particularly manifested in patients with the highest neurological disability (EDSS≥4). Similarly, social advantages may account also for the preference of “Nordic walking” declared in our study by PwMS with more advanced physical disability and age. Another explanation for the age- and neurological disability- dependent level of interest in online training among PwMS may be the difference in the awareness of such solutions and/or differences in general abilities to use electronic devices.
Our results are based on the survey filled out by RRMS patients treated in a single academic center, thus it is impossible to extrapolate the findings on the whole population of Polish PwMS. This limitation is of particular importance in the case of patients without DMT, patients with progressive forms of MS as well as older PwMS with multiple comorbidities. Although the survey was performed relatively shortly after the COVID-19 lockdown and the questionnaire was filled out anonymously, the influence of the recall bias and social desirability bias have to be also acknowledged during interpretation of the presented findings. However, we believe that the relatively large and homogenous cohort of efficiently treated, clinically stable RRMS patients allow us to regard the observations as significant for the understanding of the influence of pandemic conditions on PwMS and also other groups of patients with chronic diseases.
5. Conclusions
The results of our study demonstrate a negative influence of pandemic restrictions on the physical activity of PwMS. Importantly, a greater interest in online training was observed among PwMS under lockdown conditions, although the real engagement in online exercises increased to lesser extent. These observations deserve to be further investigated in more detailed analyses performed on bigger populations of PwMS and patients with other chronic neurological diseases. However, already at this point, our findings indicate an urgent need for systematic educational and organizational measures, promoting physical activity among PwMS.
Funding
This research received no external funding.
CRediT authorship contribution statement
Mariola Matysiak: Conceptualization, Methodology, Investigation, Writing – original draft. Małgorzata Siger: Investigation. Agata Walczak: Investigation. Agnieszka Ciach: Investigation. Mateusz Jonakowski: Formal analysis. Mariusz Stasiołek: Conceptualization, Methodology, Writing – original draft, Supervision.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kapica-Topczewska K., Brola W., Fudala M., Tarasiuk J., Chorazy M., Snarska K., Kochanowicz J., Kulakowska A. Prevalence of multiple sclerosis in Poland. Mult. Scler. Relat. Disord. 2018;21:51–55. doi: 10.1016/j.msard.2018.02.016. [DOI] [PubMed] [Google Scholar]
- Centonze D., Leocani L., Feys P. Advances in physical rehabilitation of multiple sclerosis. Curr. Opin. Neurol. 2020;33(3):255–261. doi: 10.1097/WCO.0000000000000816. [DOI] [PubMed] [Google Scholar]
- Platta M., Pilutti L.A., Motl R.W., Pilutti L.A. The effect of exercise training on fitness in multiple sclerosis: a meta-analysis. Arch. Phys. Med. Rehabil. 2016;97:1564–1572. doi: 10.1016/j.apmr.2016.01.023. [DOI] [PubMed] [Google Scholar]
- Barclay A., Paul L., MacFarlane N., McFadyen A.K. The effect of cycling using active-passive trainers on spasticity, cardiovascular fitness, function and quality of life in people with moderate to severe Multiple Sclerosis (MS); a feasibility study. Mult. Scler. Relat. Disord. 2019;34:128–134. doi: 10.1016/j.msard.2019.06.019. [DOI] [PubMed] [Google Scholar]
- Yazgan Y.Z., Tarakci E., Tarakci D., Ozdincler A.R., Kurtuncu M. Comparison of the effects of two different exergaming systems on balance, functionality, fatigue, and quality of life in people with multiple sclerosis: a randomized controlled trial. Mult. Scler. Relat. Disord. 2019;39 doi: 10.1016/j.msard.2019.101902. [DOI] [PubMed] [Google Scholar]
- Ozkul C., Guclu-Gunduz A., Eldemir K., Apaydin Y., Yazici G., Irkec C. Combined exercise training improves cognitive functions in multiple sclerosis patients with cognitive impairment: a single-blinded randomized controlled trial. Mult. Scler. Relat. Disord. 2020;45 doi: 10.1016/j.msard.2020.102419. [DOI] [PubMed] [Google Scholar]
- Demaneuf T., Aitken Z., Karahalios A., Leong T.I., De Livera A.M., Jelinek G.A., Weiland T.J., Marck C.H. Effectiveness of exercise interventions for pain reduction in people with multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. Arch. Phys. Med. Rehabil. 2019;100(1):128–139. doi: 10.1016/j.apmr.2018.08.178. [DOI] [PubMed] [Google Scholar]
- Afzal R., Dowling J.K., McCoy C.E. Impact of Exercise on Immunometabolism in Multiple Sclerosis. J. Clin. Med. 2020;21(9):3038. doi: 10.3390/jcm9093038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Liegro C.M., Schiera G., Proia P., Di Liegro I. Physical Activity and Brain Health. Genes (Basel) 2019;10(9):720. doi: 10.3390/genes10090720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L.Y., Lozinski B., Yong V.W. Exercise in multiple sclerosis and its models: focus on the central nervous system outcomes. J. Neurosci. Res. 2020;98(3):509–523. doi: 10.1002/jnr.24524. [DOI] [PubMed] [Google Scholar]
- Kjølhede T., Siemonsen S., Wenzel D., Stellmann J.P., Ringgaard S., Pedersen B.G., Stenager E., Petersen T., Vissing K., Heesen C. Dalgas, U. Can resistance training impact MRI outcomes in relapsing-remitting multiple sclerosis? Mult. Scler. 2018;24(10):1356–1365. doi: 10.1177/1352458517722645. [DOI] [PubMed] [Google Scholar]
- Kinnett-Hopkins D., Adamson B., Rougeau K., Motl R.W. People with MS are less physically active than healthy controls but as active as those with other chronic diseases: an updated meta-analysis. Mult. Scler. Relat. Disord. 2017;13:38–43. doi: 10.1016/j.msard.2017.01.016. [DOI] [PubMed] [Google Scholar]
- Kalb R., Brown T.R., Coote S., Costello K., Dalgas U., Garmon E., Giesser B., Halper J., Karpatkin H., Keller J., et al. Exercise and lifestyle physical activity recommendations for people with multiple sclerosis throughout the disease course. Mult. Scler. J. 2020;26:1459–1469. doi: 10.1177/1352458520915629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey B., Coote S., Galvin R., Donnelly A. Objective physical activity levels in people with multiple sclerosis: meta-analysis. Scand. J. Med. Sci. Sports. 2018;28(9):1960–1969. doi: 10.1111/sms.13214. [DOI] [PubMed] [Google Scholar]
- Mostert S., Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult. Scler. J. 2002;8:161–168. doi: 10.1191/1352458502ms779oa. [DOI] [PubMed] [Google Scholar]
- Kierkegaard M., E Lundberg I., Olsson T., Johansson S., Ygberg S., Opava C., Holmqvist L.W., Piehl F. High-intensity resistance training in multiple sclerosis—An exploratory study of effects on immune markers in blood and cerebrospinal fluid, and on mood, fatigue, health-related quality of life, muscle strength, walking and cognition. J. Neurol. Sci. 2016;362:251–257. doi: 10.1016/j.jns.2016.01.063. [DOI] [PubMed] [Google Scholar]
- Cottrell M.A., Galea O.A., O'Leary S.P., Hill A.J., Russell T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin. Rehabil. 2017;31:625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- Yeroushalmi S., Maloni H., Costello K., Wallin M.T. Telemedicine and multiple sclerosis: a comprehensive literature review. J. Telemed. Telecare. 2019 doi: 10.1177/1357633X19840097. 1357633×19840097. [DOI] [PubMed] [Google Scholar]
- Rintala A., Hakala S., Paltamaa J., Heinonen A., Karvanen J., Sjögren T. Effectiveness of technology-based distance physical rehabilitation interventions on physical activity and walking in multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. Disabil. Rehabil. 2018;40(4):373–387. doi: 10.1080/09638288.2016.1260649. [DOI] [PubMed] [Google Scholar]
- Di Tella S., Pagliari C., Blasi V., Mendozzi L., Rovaris M., Baglio F. Integrated telerehabilitation approach in multiple sclerosis: a systematic review and meta-analysis. J. Telemed. Telecare. 2020;26(7–8):385–399. doi: 10.1177/1357633X19850381. [DOI] [PubMed] [Google Scholar]
- Dlugonski D., Motl R., Mohr D., Sandroff B. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol. Health Med. 2012;17:636–651. doi: 10.1080/13548506.2011.652640. [DOI] [PubMed] [Google Scholar]
- Tallner A., Mäurer M., Pfeifer K. An internet-based at home training protocol enhances muscle strength and lung function in multiple sclerosis patients. Mult. Scler. 2012;18:S15–S24. [Google Scholar]
- Motl R.W., McAuley E., Sandroff B.M., Hubbard E.A. Descriptive epidemiology of physical activity rates in multiple sclerosis. Acta Neurol. Scand. 2015;131(6):422–425. doi: 10.1111/ane.12352. [DOI] [PubMed] [Google Scholar]
- Kalron A., Dolev M., Greenberg-Abrahami M., Menascu S., Frid L.;., Avrech-Shezifi S., Harari G., Magalashvili D., Achiron A. Physical activity behavior in people with multiple sclerosis during the COVID-19 pandemic in Israel: results of an online survey. Mult. Scler. Relat. Disord. 2021;47 doi: 10.1016/j.msard.2020.102603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser Moghadasi A. One Aspect of Coronavirus disease (COVID-19) Outbreak in Iran: high Anxiety among MS Patients. Mult. Scler. Relat. Disord. 2020;41 doi: 10.1016/j.msard.2020.102138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costabile T., Carotenuto A., Lavorgna L., Borriello G., Moiola L., Inglese M., Petruzzo M., Trojsi F., Ianniello A., Nozzolillo A. COVID-19 pandemic and mental distress in multiple sclerosis: implications for clinical management. Eur. J. Neurol. 2021;28:3375–3383. doi: 10.1111/ene.14580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motolese, F.; Rossi, M.; Albergo, G.; Stelitano, D.; Villanova, M.; Di Lazzaro, V.; Capone, F. The Psychological Impact of COVID-19 Pandemic on People With Multiple Sclerosis. Front. Neurol..2020, 11:580507. [DOI] [PMC free article] [PubMed]
- Holland D.P., Schlüter D.K., Young C.A., Mills R.J., Rog D.J., Ford H.L., Orchard K. TONiC study group. Use of coping strategies in multiple sclerosis: association with demographic and disease-related characteristics. Mult. Scler. Relat. Disord. 2019;27:214–222. doi: 10.1016/j.msard.2018.10.016. [DOI] [PubMed] [Google Scholar]
- Carotenuto A., Scandurra C., Costabile T., Lavorgna L., Borriello G., Moiola L., Inglese M., Trojsi F., Petruzzo M., Ianniello A., et al. Physical Exercise Moderates the Effects of Disability on Depression in People with Multiple Sclerosis during the COVID-19 Outbreak. J. Clin. Med. 2021;10:1234. doi: 10.3390/jcm10061234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes K.L., Whillier S. Effects of Nonpharmaceutical Treatments on Symptom Management in Adults With Mild or Moderate Multiple Sclerosis: a Meta-analysis. J. Manipulative Physiol. Ther. 2019;42(7):514–531. doi: 10.1016/j.jmpt.2018.12.010. [DOI] [PubMed] [Google Scholar]
- Pilutti L., Platta M.E., Motl R.W., Latimer-Cheung A.E. The safety of exercise training in multiple sclerosis: a systematic review. J. Neurol. Sci. 2014;343(1–2):3–7. doi: 10.1016/j.jns.2014.05.016. [DOI] [PubMed] [Google Scholar]
- Dalgas U., Langeskov-Christensen M., Stenager E., Riemenschneider M., Hvid L.G. Exercise as Medicine in Multiple Sclerosis-Time for a Paradigm Shift: preventive, Symptomatic, and Disease-Modifying Aspects and Perspectives. Curr. Neurol. Neurosci. Rep. 2019;19(11):88. doi: 10.1007/s11910-019-1002-3. [DOI] [PubMed] [Google Scholar]
- Charron S., McKay K.A., Tremlett H. Physical activity and disability outcomes in multiple sclerosis: a systematic review (2011-2016) Mult. Scler. Relat. Disord. 2018;20:169–177. doi: 10.1016/j.msard.2018.01.021. [DOI] [PubMed] [Google Scholar]
- Riemenschneider M., Hvid L.G., Stenager E. Dalgas, U. Is there an overlooked "window of opportunity" in MS exercise therapy? Perspectives for early MS rehabilitation. Mult. Scler. 2018;24(7):886–894. doi: 10.1177/1352458518777377. [DOI] [PubMed] [Google Scholar]
- Andreu-Caravaca L., Ramos-Campo D.J., Chung L.H., Manonelles P., Abellán-Aynés O., Rubio-Arias J.Á. The impact of COVID-19 home confinement on neuromuscular performance, functional capacity, and psychological state in Spanish people with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2021;53 doi: 10.1016/j.msard.2021.103047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dlugonski D., Motl R.W., McAuley E. Increasing physical activity in multiple sclerosis: replicating Internet intervention effects using objective and self-report outcomes. J. Rehabil. Res. Dev. 2011;48(9):1129–1136. doi: 10.1682/jrrd.2010.09.0192. [DOI] [PubMed] [Google Scholar]
- Remy C., Valet M., Stoquart G., El Sankari S., Van Pesch V., De Haan A., Lejeune T. Telecommunication and rehabilitation for patients with multiple sclerosis: access and willingness to use. A cross-sectional study. Eur. J. Phys. Rehabil. Med. 2020;56(4):403–411. doi: 10.23736/S1973-9087.20.06061-X. [DOI] [PubMed] [Google Scholar]