Abstract
Episcleritis is an irritation of the episclera of our eyes. Episclera is a thin layer of tissue present between the conjunctiva and sclera. There are mainly four causes of episcleritis: an allergic response, autoimmune, vascular disease, or infections. The symptoms are redness, erythema, discomfort in the eyes, and clear discharge. It can sometimes be painful as well. In this case presentation, we will discuss the role of vitamin c in the prevention and reoccurrence of autoimmune episcleritis.
Keywords: eye discharge, eye pain, vitamin - c, inflammation of eye, episcleritis
Introduction
Most cases of episcleritis are idiopathic and usually resolve on their own. However, the rest of the cases of episcleritis are usually associated with systemic disorders, for example, rheumatoid arthritis, Crohn's disease, systemic lupus erythematosus, etc. There are some infectious causes as well associated with episcleritis, such as syphilis, Lyme disease, herpes virus, etc., but they are less common when compared to systemic and vascular disorders [1-5].
Case presentation
The patient is a 60-year-old male who presents to my outpatient clinic with a chief complaint of redness, irritation, and watery eyes. He states that this has happened multiple times in the past since the age of 45 years. The patient states that the symptoms are abrupt, and they typically take about one to two weeks to resolve. He has tried multiple medications, including steroids, NSAIDs, etc., which work, but these symptoms always return back in two to three months. He has a past medical history only significant for hypertension for which he takes amlodipine 5 mg daily. He does not smoke, does not drink, and has never used any drugs. He has normal vision and does not use spectacles. The patient's family history is only significant for coronary artery disease in both parents. He has a desk job in a bank and is not exposed to any chemicals. The patient saw an ophthalmologist two years ago for inflammation of his eyes. He was referred to a rheumatologist because of recurring inflammation of the eyes. He had extensive lab work done, which included checking for autoimmune diseases like systemic lupus erythematosus, Sjögren's syndrome, rheumatoid arthritis, etc., which were all negative. The patient was also tested for herpes zoster and Lyme disease, which were negative. He even had a chest x-ray and CT chest performed by his rheumatologist, which all turned out to be negative. The patient states that he does not take any supplements. He has tried taking herbal supplements like honey to help with his eye, but they have never worked. He occasionally uses over-the-counter artificial tear drops to prevent recurring inflammation of his eye, but it does not help. The patient changed his soap and shampoo and relocated to a new city over the past 15 years (since his symptoms started) but has had no relief in his symptoms.
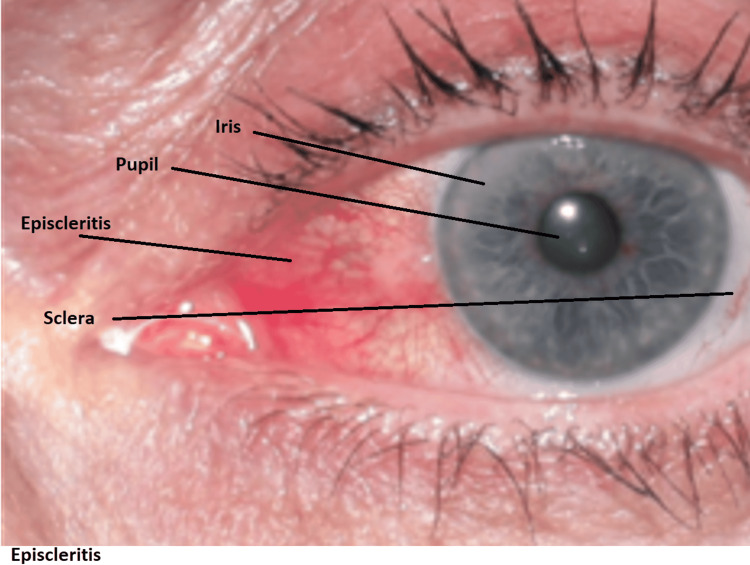
A physical exam reveals red episclera and slight swelling of the episclera without any swelling or edema in the sclera, as shown in Figure 1. The patient underwent laboratory evaluations and results in Table 1.
Table 1. Laboratory evaluations and results.
| Labs Test | Results | Normal Range |
| Complete Blood Count (CBC) | All within normal range | Normal |
| Comprehensive Metabolic Panel (CMP) | All within normal range | Normal |
| Rheumatoid Factor | Negative | Negative |
| Antinuclear Antibody | negative | Negative |
| Urinary analysis | Negative | Negative |
| Thyroid-Stimulating Hormone (TSH) | 1 | 0.35-5.0 |
Figure 1. Red episclera and slight swelling of the episclera without any swelling or edema in the sclera.
He was started on over-the-counter artificial tears and oral Ibuprofen - 400mg three times daily for seven days which resolved the patient's symptoms. However, the patient returned to my clinic again in two months with the same symptoms. Because of the patient's recurrence and multiple episodes in the past, I prescribed the same dose of Ibuprofen, but this time I also prescribed 500mg of Vitamin C daily. I advised the patient to continue taking Vitamin C daily for the rest of his life even after his symptoms completely resolved. The patient returned to me after seven months for his regular physical exam and stated that since starting his daily dose of Vitamin C, he had not had any more episodes of episcleritis.
Discussion
The immune system of our body can eventually become dysregulated during our lifecycle, which causes autoimmune attacks on parts of our body, for example, Inflammatory bowel disease, Hashimoto's disease, juvenile arthritis, etc. Similarly, the eyes can also be affected, leading to diseases like episcleritis. Studies have shown an association between oxidative stress and inflammation. Inflammation causes an increase in oxidative stress by elevating reactive oxygen species (ROS) [6,7]. Increased oxidative stress and ROS have been associated with inflammatory responses and autoimmune diseases, including keratoconjunctivitis sicca [8,9].
As we know, Vitamin C is a strong antioxidant that protects our tissue from oxidative damage. The total amount of Vitamin C in the human retina is 20 times higher than in the plasma [8]. Other Vitamins, which are also antioxidants, include Vitamin A and E. In autoimmune episcleritis, we suspect that the antioxidant system somehow gets weak, which causes damage to the episclera and causes inflammation and disease [8]. Vitamin C deficiency has been known to be associated with corneal inflammation, with some patients presenting with dry, irritated eyes [10]. Vitamin C supplementation can also be beneficial in undiagnosed cases of deficiency, as well as for its role in reducing oxidative stress, thereby resolving recurrent symptoms [11].
Regular Vitamin C intake is associated with minimal side effects, even at high intravascular doses [12]. There have been reports of kidney stones or other complications in patients with glucose-6-phosphate dehydrogenase deficiency or those with poor renal function receiving supraphysiological doses of vitamin C, and caution is recommended in such clinical situations [13,14]. These adverse effects could be minimized with patient education and by limiting daily intake within the upper limits of daily intake of 2000mg/day for adults [15].
Conclusions
Episclera is a highly vascular tissue that lies above the sclera and beneath the conjunctiva. Episcleritis is an inflammatory response likely caused by oxidative stress, which causes tissue inflammation. In this case, increasing the effectiveness of our body's antioxidant system could contain inflammation and disease. There are different kinds of antioxidants available in our diet and also available as synthetic supplements such as Vitamin C, which has been shown to prevent ocular inflammation. We conclude that Vitamin C can be considered a preventive and therapeutic measure in patients with recurrent episcleritis, which also has an excellent safety profile. Still, additional rigorous investigations with case-controlled studies or trials are needed for a more definitive conclusion.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Severity of episcleritis and systemic disease association. Akpek EK, Uy HS, Christen W, Gurdal C, Foster CS. Ophthalmology. 1999;106:729–731. doi: 10.1016/S0161-6420(99)90157-4. [DOI] [PubMed] [Google Scholar]
- 2.Clinical characteristics of a large cohort of patients with scleritis and episcleritis. de la Maza MS, Molina N, Gonzalez-Gonzalez LA, Doctor PP, Tauber J, Foster CS. Ophthalmology. 2012;119:43–50. doi: 10.1016/j.ophtha.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 3.Treatment and management of scleral disorders. Diaz JD, Sobol EK, Gritz DC. Surv Ophthalmol. 2016;61:702–717. doi: 10.1016/j.survophthal.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Scleritis and episcleritis. Watson PG, Hayreh SS. Br J Ophthalmol. 1976;60:163–191. doi: 10.1136/bjo.60.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Severity of scleritis and episcleritis. de la Maza MS, Jabbur NS, Foster CS. Ophthalmology. 1994;101:389–396. doi: 10.1016/s0161-6420(94)31325-x. [DOI] [PubMed] [Google Scholar]
- 6.Involvement of reactive oxygen species in toll-like receptor 4-dependent activation of NF-kappa B. Asehnoune K, Strassheim D, Mitra S, Kim JY, Abraham E. J Immunol. 2004;172:2522–2529. doi: 10.4049/jimmunol.172.4.2522. [DOI] [PubMed] [Google Scholar]
- 7.Inflammatory cells and oxygen radicals. Nagata M. Curr Drug Targets Inflamm Allergy. 2005;4:503–504. doi: 10.2174/1568010054526322. [DOI] [PubMed] [Google Scholar]
- 8.Emerging role of antioxidants in the protection of uveitis complications. Yadav UC, Kalariya NM, Ramana KV. Curr Med Chem. 2011;18:931–942. doi: 10.2174/092986711794927694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dry eye disease and oxidative stress. Seen S, Tong L. Acta Ophthalmol. 2018;96:0–20. doi: 10.1111/aos.13526. [DOI] [PubMed] [Google Scholar]
- 10.Sjögren's syndrome in scurvy. Hood J, Burns CA, Hodges RE. N Engl J Med. 1970;282:1120–1124. doi: 10.1056/NEJM197005142822003. [DOI] [PubMed] [Google Scholar]
- 11.Maxfield L, Crane JS. Treasure Island, FL: StatPearls Publishing; 2022. Vitamin C deficiency. [PubMed] [Google Scholar]
- 12.Harm of IV high-dose vitamin C therapy in adult patients: a scoping review. Yanase F, Fujii T, Naorungroj T, et al. Crit Care Med. 2020;48:0–8. doi: 10.1097/CCM.0000000000004396. [DOI] [PubMed] [Google Scholar]
- 13.Ascorbic acid supplements and kidney stones incidence among men and women: a systematic review and meta-analysis. Jiang K, Tang K, Liu H, Xu H, Ye Z, Chen Z. Urol J. 2019;16:115–120. doi: 10.22037/uj.v0i0.4275. [DOI] [PubMed] [Google Scholar]
- 14.High dose vitamin C induced methemoglobinemia and hemolytic anemia in glucose-6-phosphate dehydrogenase deficiency. Lo YH, Mok KL. Am J Emerg Med. 2020;38:2488–2485. doi: 10.1016/j.ajem.2020.05.099. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Washington, DC: National Academy Press; 2000. Food and nutrition Board. Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. [PubMed] [Google Scholar]