Abstract
Traditional medicine has the potential to boost the health and economies of many SSA countries, especially if regulatory mechanisms are deployed to govern their protection and utilisation. There is lack of knowledge regarding traditional medicines and their impact on pregnancy. This paper reviews the literature on traditional medicine utilisation among pregnant women in Sub-Saharan African countries. The paper, determined the proportion of pregnant women utilising traditional medicines in Sub-Saharan Africa, identified the different types of traditional medicine used during antenatal care and reasons for Use in Sub-Saharan Africa and also identified challenges that are faced by women who use traditional medicine in antenatal care. A systematic exploratory review was conducted guided by the PRISMA framework. The databases that were searched included Google Scholar, PubMed, Cochrane, HINARI and the World Health Organization. Forty-one literature sources were eligible and included in the review process. Reported traditional medicine utilisation ranged between 12 and 93% among pregnant women in Sub-Saharan Africa. Different types of traditional medicines have been utilised in Sub-Saharan Africa for different purposes. Safety and poor management of usage were reported to be some of the challenges associated with traditional medicine. There is a need to determine chemical components and mode of action of these herbs as some could be beneficial, whilst others harmful, leading to severe pregnancy complications.
Keywords: traditional medicine, utilisation, prevalence, pregnant women, sub-saharan Africa
Highlights
1) Traditional medicine utilisation during pregnancy is common in many Sub-Saharan African (SSA) countries.
2) There are still gaps in knowledge on how traditional medicine is utilised and for what purposes during pregnancy
3) This research provides a window of opportunity to explore the different types of traditional medicines utilised in different countries in SSA and document these for possible further studies to explore its safety and efficacy to strengthen health systems in managing pregnancies.
Background
Traditional medicines (TM) have been used in pregnancy management in many countries, even where modern health care is readily available 1 TM refers to plants, animals, or minerals taken either by injection, ingestion, adsorption or absorption by pregnant women 2 It focuses on the knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health and the prevention, diagnosis, improvement or treatment of physical and mental illnesses 2 There has been an increase of interest in the use and importance of TMs both by the WHO and many African countries 3 Pregnant women utilise TMs for several reasons: lack of foetal turning, overdue delivery, pregnancy breech and false labour, morning sickness, abdominal pain, constipation, heartburn, uterus being dirty or full of air, sexually transmitted diseases and high blood pressure4,5 The utilisation of TMs is diverse in maternal health. It can be used for different purposes depending on individuals the culture and beliefs of individuals and is based on locally available natural resources 6 The use is triggered by various practices, approaches, knowledge and beliefs about incorporating plant, animal and mineral-based medicines, spiritual therapies to maintain wellbeing and treat, diagnose or prevent illness2,7,8 However, it is reported in some studies that this increasing Use of TMs by pregnant women poses risks which in most cases are unknown ad could compete with other modernised medicines used, leading to complications 9
Treatment in the early stages of pregnancy is believed to prevent miscarriage and ensure proper growth of the foetus and stability of the woman’s health10,11 Treatment with TM at the later stages of pregnancy ensures safe delivery minimising chances of complications even after birth 12 Though most professional health practitioners are sceptical about the safety of TM usage, they agree that traditional healers play an important complementary role in the provision of effective prevention and treatment of diseases 13 The African continent is still developing, and several countries are classified as poor by the World Bank14,15 Poverty has negatively impacted health service provision due to poor infrastructure development and human resources exodus to developed countries16–18 Staff shortages in health institutions, among other challenges, have ensured that traditional health practitioners serve a large population and play an essential role in the health system19–21 There should, therefore, be an urgent need to recognise traditional practitioners and prioritise them in public health campaigns and health promotions as a mechanism to reduce maternal mortality 2 Studies in Sub-Saharan Africa (SSA) have shown that doctors are fewer than traditional healers aiding pregnant women to consult with the traditional system, which is more efficient2,22,23 Apart from the challenges mentioned above, sociocultural factors such as the knowledge passed from generation to generation, availability of TMs, unpleasant experiences with the formal health system, health beliefs and conceptualisation in most Africa settings also influence traditional medicine use in pregnant women SSA 4
Generally, several studies conducted on TMs utilisation tend to focus mainly on the factors that lead women to utilise the different types of TMs, with most focussing on the proportions of pregnant women that utilise these medicines during pregnancy9,24–28 Furthermore, most of these studies do not explore in-depth the challenges reported by these women who utilise TMs thus, this current study is critical in ensuring that challenges faced by women who utilise TMs are comprehensively documented through synthesising the different studies that have been published in SSA.
TM can boost the health and economies of many SSA countries, especially if regulatory mechanisms are deployed to govern their protection and utilisation 29 To reduce maternal deaths and pregnancy-related complications, TMs used during pregnancy need to be better known and thoroughly researched regarding their safety. Research into the TMs used will aid women in receiving adequate treatment, to identify potentially unsafe use, and also preserve valuable information about medicinal in the future as well as declare the different types of TMs they would have used in their health facilities to aid complementarity and better management of the pregnancies9,30 Therefore, this review explored TM utilisation during pregnancy in SSA. The following 3 specific objectives have guided this enquiry:
1) Determining the proportion of pregnant women utilising TMs in SSA
2) Identifying the different types of TM used during antenatal care and reasons for Use in SSA
3) Identifying challenges that are faced by women who use TM in antenatal care.
Methodology
Inclusion Criteria
Studies were included if they reported the Use of TMs by SSA women for reasons related to preparation for pregnancy, promoting fertility, treating pregnancy-related symptoms, maintenance of general wellbeing during pregnancy, inducing or assisting labour. Studies were also included if they described the views, attitudes and beliefs of women regarding TM utilisation. All studies published in English (up to 17 November 2021) in reputable peer-reviewed journals, and available open access were targeted.
Exclusion Criteria
The study excluded all published literature sources that addressed TM related issues but did not focus on SSA. Furthermore, literature sources that focused on women’s Use of TM for general purposes and other conditions other than pregnancy were excluded.
Keywords for Literature Search
The keywords for the literature search engines included traditional medicine utilisation, SSA pregnant women.
Search Strategy
The keywords (Traditional medicine; pregnant women; herbal medicines; phytotherapy, Sub-Saharan Africa complementary and alternative medicines) were used to search for literature on Google Scholar, PubMed, Cochrane, HINARI and the WHO website. The literature search was done up to 17 November 2021.
Methods of Review
We reviewed independently titles and abstracts of articles and reports that were relevant and qualified to be included in this study. Disagreements were resolved through dialogue between we and reaching an agreement based on issues arising and exchanged. The 2 authors reviewed full texts of these articles and reports that met the inclusion criteria, and findings were discussed, and an agreement was reached.
Data Extraction and Synthesis
We developed a data collection form as guided by the objectives to facilitate uniformity in data collection (by the authors). The we reviewed articles and reports and collected data. Discrepancies observed on collected data by the authors were resolved through dialogue and reaching a consensus. Findings from the articles and reports were then coded and thematically analysed in line with the specific objectives.
Quality Assessment
For this review, the quality was assessed using a purposive rating tool adapted from the AMSTAR checklist 31 This scale is a freely accessible, validated tool for evaluating the methodological quality of reviewed documents. AMSTAR items contain several aspects; therefore, only components relevant to the research scope were used 31 The primary purpose of this rating tool was to evaluate the scientific quality/rigour of systematic reviews in TM use, and question 1–6 was used in the checklist 31
Results
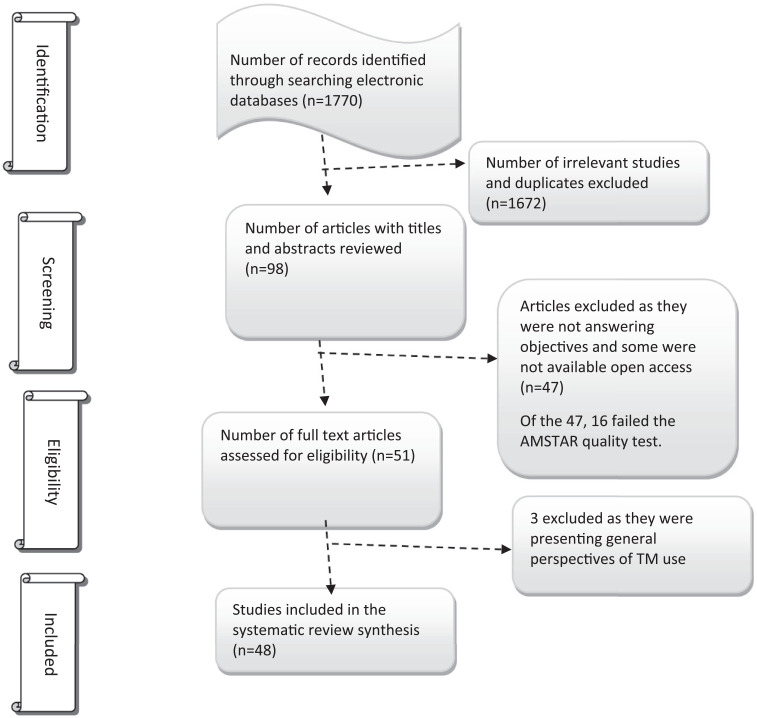
A total of 1770 literature sources were obtained from electronic databases. After excluding 1672 duplicates and irrelevant sources, 98 sources had their titles and abstracts screened. After screening, 47 articles were found not to address the objectives of this review, and some were not available open access, and some failed the quality test (16) and were excluded leaving 51 that underwent full manuscript review. Three of the 51 were excluded as they gave a general perspective of TM use, and the remaining 48 were eligible and included in this systematic review. The summary of this inclusion/exclusion process is shown in Figure 1.
Figure 1.
Document review process.
Proportion of Pregnant Women Utilising Traditional medicines in Sub-Saharan African
It is estimated that TM utilisation by women in SSA is estimated to be between 30 and 70% 4 Subsidising influences to increase the Use of TMs include culture and beliefs, poverty, long distance to health facilities, cost of modern medicines and acceptability of TM 32 Results from different studies indicate that prevalence varies depending on the country, and in SSA, it ranges from 12 to 93% among pregnant women, as influenced by different contextual settings in different countries. These findings are presented in Table 1.
Table 1.
Prevalence of Traditional Medicines Use in Sub-Saharan African.
| Country | Prevalence (%) | Citations |
|---|---|---|
| 1. South Africa | 33–93 | 4,56–58 |
| 2. Nigeria | 31.4–68 | 4,28,59,60 |
| 3. Mali | 80 | 30 |
| 4. Zimbabwe | 52–69.9 | 61–63 |
| 5. Tanzania | 55 | 32 |
| 6. Ethiopia | 48.6–50.4 | 64,65 |
| 7. Ghana | <50 | 66 |
| 8. Tanzania | 42 | 4 |
| 9. Cote d’ Ivoire | 35 | 4 |
| 10. Malawi | 25.7 | 67,68 |
| 11. Kenya | 12 | 69 |
| 12. Zambia | 21 | 70 |
| 13. Uganda | 20 | 71 |
Traditional medicines Used During pregnancy Among Sub-saharan African Women
A study conducted in South Africa cited ten species as frequently used for the treatment of common pregnancy-related problems such as oedema, indigestion, constipation, infection, high blood pressure and post-partum healing 33 Also, a study conducted in Zimbabwe identified 8 species of herbal medicines, with many being used to quicken labour 34 Table 2 shows some traditional remedies used in Sub-Saharan Africa during pregnancy with Asparagus Africanus used in South Africa and Zimbabwe.
Table 2.
Some Traditional Medicines used in Sub-Saharan Africa.
| Country | Traditional Medicine | Reasons and How it is Used | Citations |
|---|---|---|---|
| South Africa | Isihlambelo | Taken orally in the third trimester for a quick labour, foetal growth, and wellbeing and it is a mixture of different ingredients such as fish heads, snakeskin, crocodile parts and mercury | 33,72–74 |
| Imbelekisane and Inembe | Imbelekisane is used to treat prolonged labour whilst Inembe is used for labour induction but can cause severe complications such as abortions or uterine rupture | 33,46 | |
| Umchamo wemfene | This is solidified imbila (cape hyrax, dassie) urine and faeces is taken orally, to treat menstrual difficulties and to ease childbirth | 75,76 | |
| Kgaba remedies and crushed ostrich eggshell | These are taken orally; crushed ostrich eggshell is used to trigger labour even though its chemical properties are unknown and kgaba is a mixture of different plants such as kgaba etona (Rhoicissus tridentata) | 76 | |
| Usigidi | Drop of mercury given orally to induce labour and can be mixed with isihlambelo | 76 | |
| Gramophone record | Crushed and mixed with water to induce labour | 76 | |
|
Mpundulo
Mbheswana |
Mpundulo a herb taken orally daily in preparation for labour whilst Mbheswana is drunk to enhance labour and reduce foetal distress | 57,77 | |
| Asparagus africanus | Quickens labour | 78 | |
| Imbiza | Class of purgative medicines for internal cleansing so that uterus accept foetus | 79 | |
| Zimbabwe | Elephant’s dung Donkey placenta Eel fish |
Mix with water to quicken labour | 34,63 |
| Dicerocaryum zanguebarium | Soak in water lubricate vagina and widens it for baby to come out easy | 34,61 | |
| Sweet potato leaves | Boil and drink for 36–40 days till the onset of labour to quicken labour | 34 | |
| Asparagus africanus | Quickens labour | ||
| Snot leaves | Crushed and socked in water to induce labour | ||
| Pouzolzia mixta solms | Roots extract inserted into the vagina to expand birth canal | ||
| Ghana | Annona glauca | For easy delivery | 80 |
| Prosopis africana | Lower abdominal pain | 80,81 | |
| Moringa oleifera (moringa) | Blood pressure, bleeding and constipation | 82 | |
| Citrus limon (lemon) | Loss of appetite and body weakness | 80 | |
| Adansonia digitata (baobab) | Cardiovascular conditions such as hypertension | 83 | |
| Carica papaya (pawpaw) | Worm infestation and malaria | 84 | |
| Pennisitumn glaucum (millet) | Seeds are used to treat skin rashes and jaundice | 80 | |
| Securidaca longepedunculata | Root, bark, and leaves used for health purposes such as liver problems and food poisoning | ||
| boiled tealeaf and fenugreek herbs | Dizziness, fever and malaria | 4 | |
|
(Zingiber officinale), peppermint (Mentha × piperita), thyme (Thymus Lamiaceae), sage (Salvia officinalis), aniseeds (Pimpinella anisum), fenugreek (Trigonella foenum-graecum), green tea (Camellia sinensis), garlic (Allium sativum), tea leaf (Camellia sinensis), raspberry
(Rubus idaeus), and echinacea leaf (Echinacea purpurea) |
Used in combinations treat pregnancy-related complications such as relief of back pain, dizziness, stress and depression, cold, fever, malaria, vomiting and nausea reduction, as well as in the prevention of miscarriages | 4 | |
| Mali | Ximenia americana | Treat heartburn in pregnancy and prevent foetal diseases | 85 |
| Trichilia emetic | Should only be used externally as a wash to treat fever | ||
|
Euphorbia hirta
Ficus capensis |
Often recommended in pregnancy to increase breast milk production | 85,86 | |
| Cola cordifolia | Leaf and stem bark facilitate labour | 30 | |
| Adansonia digitata (baobab) | Infants are given barks to gain weight | 83 | |
| Cassia sieberiana | The root bark has a use as a purgative and has a strong bitter taste. The plant is also used against infertility | 85 | |
| Ethiopia | Zingiber officinale (ginger, Allium sativum (garlic), Ocimum lamiifolium (basil or damakasie, Hagenia abyssinica (koso), Taverniera abyssinica (emergency herb, Ruta chalepensis (rue or tena adam), Lepidium sativum (peppergrass or feto), Coffea arabica linn (altet), Eucalyptus globulus (eucalyptus leaf), Brassica nigra (mustard seed), Tenaadam (Rutachalenssis) | The accessed study did not report the reasons or purposes of using these specific TMs. However, it is generally reported that the herbs are used to treat nausea, morning sickness, vomiting, cough, deficiency in nutrition and malaria | 26,27 |
| Benin | Musaceae Bananier, Musa sapientum, Euphorbiaceae Plante corail, Jatropha multifida, Apocynaceae, Rauvolfia vomitoria Afzel, Annonaceae Pomme, Annona senegalensis, Macrosphyra longistyla, Newbouldia laevis, Holarrhena floribunda, Terminalia macroptera Guill, Crescentia cujete, Chassalia kolly Schumach, Ceiba pentandra, Entada africana Guill, Diospyros mespiliformis Hochst, Piliostigma thonningii Schumach, Carica papaya, Lawsonia inermis, Piliostigma reticulata, Ageratum conyzioïdes, Jatropha curcas, Strophanthus sarmentosus, Boerhavia diffusa, Acacia nilotica, Achyranthes aspera, Aloe buettneri, Annona muricate, Arachis hypogaea, Berlinia grandiflora Vahl, Bidens Pilosa, Bridelia micrantha Hochst, Bryophyllum pinnatum Lam, Cassia sieberiana, Combretum micranthum, Dialium guineense Willd, Eucalyptus camadulensis Dehn, Ficus exasperata Vahl, Ficus lutea Vahl, Guiera senegalensis, Hibiscus surattensis, Hyptis pectinate, Imperata cylindrica, Mangifera indica, Mirabilis jalapa, Moringa oleifera Lam, Nauclea latifolia, Paullinia pinnata, Pterocarpus erinaceus Poir, Spondias mombin, Stereospermum kunthianum Cham, Tamarindus indica, Terminalia avicennioides Guil, Terminalia laxiflora Engl, Uvaria chamae, Vernonia amygdalina Delile, Vernonia colorata Willd, Ximenia Americana | These were found to be used by pregnant women as Antihemorrhagic medicinal plants | 87 |
| Nigeria | Bitter leaf, Palm kernel oil, Bitter kola (Garcinia kola), Dogoyaro (Neeme leaf), Garlic, Jute leaves (Utazi), Ginger, Holy Basil leaf/scent leaf, Honey, Herbal mixture (Agbo), Calabash chalk (Nzu), Aloe Vera, Drum stick tree (Moringa), Palm wine, African teak (iroko seed), Bitter lemon/lime, Onion, Cod liver oil, Pumpkin leaves, Shea butter, Pepper/spice, Bark of cashew, lime juice (Alabukun) | There were a number of herbs that were used in Nigeria however the reasons for their use were not specified | 28 |
Challenges and pregnancy Complications Associated with Traditional Medicines Use
The review process revealed several challenges due to the utilisation of TMs during pregnancy. Themes that emerged included safety, regulation, adverse outcomes, inadequate monitoring, as indicated in Table 3
Table 3.
Challenges and Complication of Traditional Medicine Use in Pregnancy.
| Pregnancy Challenges and Complications | Explanation | Citations |
|---|---|---|
| Poor monitoring and safety | Several traditional remedies remain untested, and their mode of action or safety is unknown in pregnancy management. Also, their interactions with pharmaceuticals and food consumed by pregnant women are unknown | 45,73 |
| Regulation of TM | Some countries have put measures to regularise utilisation of TM even though they still run parallel with the modern system | 29,59,69,73 |
| Scanty data | Numerous studies focus on perceptions, prevalence and utilisation patterns of TM | 30,32,33,43,62 |
| Negative outcomes | Foetal distress is shown by the high frequency of meconium-stained liquor (MSL), caesarean section and uterine rupture uterine, hyper stimulation, and low neonatal birth weights, preclamsia, nausea, vomiting has been reported due to TM use | 32,73 |
| General pregnancy complications | Some pregnancy-related complications have been noted such as miscarriage, separation of the placenta, haemorrhage, obstructed labour and the retention of the placenta | 50 |
Note. TM = Traditional Medicine.
Discussion
The review indicated that the prevalence of TM utilisation during pregnancy is predominant and varies across different countries. Increasing prevalence is no longer debatable even though there is a previous misconception regarding herbal medicinal products as safe and raw consumption from their natural state. In several countries, herbal medicines and related products are introduced without any mandatory safety or toxicological evaluation, which makes patients have access to them 35 Studies conducted in Australia are within the range obtained by our review, with between 48% and 69% prevalence36,37 In Ghana, TM use in pregnancy is triggered by low education levels and long distances to the hospital and unpleasant interactions with health service providers in the modernised health facilities 4 The promotion of TM in society and the media is another contributing factor that increases prevalence in some Sub-Saharan countries 32 It should also be noted that TM utilisation is higher in countries that have poorly financed health systems that usually change significant amounts of monies from users, the majority of who would be poor and could barely afford the fees charged38,39
As our study indicated that prevalence varies, literature shows that increasing utilisation of traditional remedies is also caused by unease or discomfort about discussing their medical problems and fear of confidentiality in handling their health information 40 Influence of religion and a greater level of spiritual consciousness, many individuals tend to be increasingly disposed to accepting the therapeutic value based on faith or intuition rather than scientific reasoning 41 Numerous studies also indicate that traditional remedies usage is mostly recommended by traditional birth attendants, close relatives, and on rare occasions by health care providers. It is revealed that family members who advise on using herbal medicines may not have sufficient knowledge of the herbs and remedies 42
Confidence in herbal remedies is relatively high among primitive individuals, mainly those based in rural populations. It is associated with a lack of access to public healthcare, social and cultural values, perceived efficacy, beliefs about safety and general ease of access 43 However, though women have access to public healthcare facilities in urban areas, women still rely on alternative or traditional systems of care 43 In public health care, herbal medicines have been proved to impact the health-seeking behaviours of patients, prescribed drug use and health outcomes 44 Some women use herbal medicines secretively as compared to modern medications 44
Even though our review showed that Meconium-Stained Liquor (MLS) is a result of traditional remedies used but other scholars highlight that it can occur without any form of medications or if there is no foetal distress during pregnancies33,45, the review indicated Isihlambelo, which is commonly used in South Africa among Zulu that causes uterine contraction thereby quickening labour 46 Although some studies reveal adverse effects of traditional herbs, some highlights their benefit as some herbs have sugar components that can be the source of nutrition and energy to a pregnant woman, although others are antioxidants with health benefits, thereby boosting the immune system, preventing respiratory diseases and preventing birth defects47–49
Preeclampsia, nausea and vomiting have been noted in the review as complications among pregnant women who utilise traditional remedies. Other studies acknowledge that preeclampsia, vomiting and nausea are common during pregnancy and suggest modern ways of controlling such as regular intake of at least 1500 mg of calcium each day during pregnancy could significantly reduce the risk of preeclampsia and substantially lower blood pressure 50 It is also reported that hyperemesis gravidarum, Zingiber officinale (ginger) root is beneficial both in milder nausea and hyperemesis 51
Results revealed that several factors had triggered utilisation of TMs, and studies in different geographic setups indicate factors such as the belief that herbal products are superior to manufactured products 52 Furthermore, discontent with the results from approved modern medicines and the belief that herbal medicines might be helpful in the treatment of certain diseases where conventional therapies and medicines have proven to be ineffective. Some TMs are locally available and easily accessible in SSA. Accessibility and availability of TM in SSA are well documented and highlighted in the literature as an alternative remedy that promotes self-medication 52
The review also indicated that there are no formal regulations of this herbal medicines 29 The absence of these regulations is contrary to the European Union (EU), which implemented a directive to harmonise the management of traditional herbal medicinal products across the EU and establish a simplified licensing system to help the public make informed choices about the use of herbal products 53 It is expected that stakeholders producing herbal products have a product license or become registered as a traditional herbal medicinal dealer/distributor53,54 In developing countries, there is a lack of capacity to regulate manufacturing practices and enforce quality standards 50 These herbal products have been consistently made available to consumers without prescription, and in most cases, the potential hazards in a low-grade product are hardly recognised 52
This review indicated that different TM was used to ensure the sound development of the foetus, quicken labour, prevent or cure malaria and prevent miscarriages. Published sources from countries such as Ivory Coast, Nigeria, Zambia, Uganda, Tanzania, Benin and Gabon reveal extensive use of different types of TMs among women 55 In a study conducted in Uganda, Ivory Coast, Tanzania, Benin, Gabon study among women, 75, 75, 23, 248, 189 plant species were identified for use during pregnancy and labour, respectively 55
Limitations of the Study
We did not find some Latin Names for some of the TMs that different women in the literature used, and some literature just presented. It should also be noted that the environment we live in is dynamic, and new information comes through. Therefore, some studies may have been missed in this study. It should also be noted that this study was not funded; therefore, the literature search was limited to only those available sources open access from the databases.
Conclusion
There is proof that TM is widely used during pregnancy among Sub-Saharan African women. However, there is a gap as most studies focus on presenting general TMs utilisation patterns without paying particular attention to its application to maternal health-related issues and the complications associated with its use thereof. There is a need to determine the chemical components and mode of action of these herbs as some are beneficial, whilst others could be harmful, leading to severe maternal complications. Stakeholders within the domain of maternal health systems should design standardised guidelines and policies that might regulate the utilisation of traditional remedies by pregnant women.
Footnotes
Author’s Note: This review was part of a broader study on traditional medicine utilisation and maternal health-related issues.
Author Contributions: NM conceptualised the research idea and designed the methodology and data collection tools. WNN refined the idea and, together with NM drafted the manuscript. WNN performed the management, screening and data extraction in the review process. All the authors coordinated the manuscript writing process; they read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Wilfred N. Nunu  https://orcid.org/0000-0001-8421-1478
https://orcid.org/0000-0001-8421-1478
References
- 1. Biddlecom AE, Munthali A, Singh S, Woog V. Adolescents’ views of and preferences for sexual and reproductive health services in Burkina Faso, Ghana, Malawi and Uganda. Afr J Reprod Health. 2007;11(3):99. [PMC free article] [PubMed] [Google Scholar]
- 2. Bodeker G, Ong C-K. WHO Global Atlas of Traditional, Complementary and Alternative Medicine. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 3. Van Wyk B-E. A broad review of commercially important southern African medicinal plants. J Ethnopharmacol. 2008;119(3):342-355. [DOI] [PubMed] [Google Scholar]
- 4. Peprah P, Agyemang-Duah W, Arthur-Holmes F, et al. ‘We are nothing without herbs’: A story of herbal remedies use during pregnancy in rural Ghana. BMC Compl Alternative Med. 2019;19(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peltzer K. Utilization and practice of traditional/complementary/alternative medicine (TM/CAM) in South Africa. Afr J Tradit, Complement Altern Med. 2009;6(2):175. [PMC free article] [PubMed] [Google Scholar]
- 6. Kaingu CK, Oduma JA, Kanui TI. Practices of traditional birth attendants in Machakos District, Kenya. J Ethnopharmacol. 2011;137(1):495-502. [DOI] [PubMed] [Google Scholar]
- 7. WHO. Legal Status of Traditional Medicine and Complementary. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 8. WHO. Making Pregnancy Safer: The Critical Role of the Skilled Attendant: A Joint Statement by WHO, ICM and FIGO. Geneva, Switzerland: World health organization; 2004. [Google Scholar]
- 9. Aljofan M, Alkhamaiseh S. Prevalence and factors influencing use of herbal medicines during pregnancy in Hail, Saudi Arabia: A cross-sectional study. Sultan Qaboos Univ Med J. 2020;20(1):e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Broussard C, Louik C, Honein M, Mitchell A. Herbal use before and during pregnancy. Am J Obstet Gynecol. 2010;202:443. [DOI] [PubMed] [Google Scholar]
- 11. Malan D, Neuba R. Traditional practices and medicinal plants use during pregnancy by anyi-ndenye women (Eastern côte d’ivoire). Afr J Reprod Health. 2011;15:85-93. [PubMed] [Google Scholar]
- 12. Wreford J. Shaming and Blaming: Medical Myths, Traditional Health Practitioners and HIV/AIDS in South Africa. Cape Town, South Africa: OpenUCT; 2008. [Google Scholar]
- 13. Jones PW. Education, Poverty and the World Bank. Rotterdam, Netherlands: Sense Publishers; 2006. [Google Scholar]
- 14. Easterly W. What did structural adjustment adjust?: The association of policies and growth with repeated IMF and World Bank adjustment loans. J Dev Econ. 2005;76(1):1-22. [Google Scholar]
- 15. Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97-105. [PMC free article] [PubMed] [Google Scholar]
- 16. Wagstaff A. Research on Equity, Poverty and Health Outcomes: Lessons for the Developing World. Washington, DC: Oprn Knowledge Respository; 2000. [Google Scholar]
- 17. Duggal R. Poverty & health: Criticality of public financing. Indian J Med Res. 2007;126(4):309. [PubMed] [Google Scholar]
- 18. Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit, Complement Altern Med. 2011;8(suppl 5):115-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gyasi RM. Relationship between health insurance status and the pattern of traditional medicine utilisation in Ghana. Evid base Compl Altern Med. 2015;2015:717926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. James PB, Wardle J, Steel A, Adams J. Traditional, complementary and alternative medicine use in Sub-Saharan Africa: A systematic review. BMJ global health. 2018;3(5):e000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nunu WN, Munyewende PO. Patient satisfaction with nurse-delivery primary health care services in Free State and Gauteng provinces, South Africa: A comparative study. Afr J Prim Health Care Fam Med. 2017;9(1):e1-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nunu WN, Ndlovu V, Maviza A, Moyo M, Dube O. Factors associated with home births in a selected ward in Mberengwa District, Zimbabwe. Midwifery. 2019;68:15-22. [DOI] [PubMed] [Google Scholar]
- 23. Onyiapat J-l, Okafor C, Okoronkwo I, et al. Complementary and alternative medicine use: Results from a descriptive study of pregnant women in Udi local Government area of Enugu State, Nigeria. BMC Complement Altern Med. 2017;17(1):189-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Laelago T, Yohannes T, Lemango F. Prevalence of herbal medicine use and associated factors among pregnant women attending antenatal care at public health facilities in Hossana Town, Southern Ethiopia: Facility based cross sectional study. Arch Publ Health. 2016;74(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte Hospital, Western Ethiopia. Jundishapur J Nat Pharm Prod. 2014;9(4):e17368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Beyene KG, Beza SW. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health. 2018;46:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Duru CB, Uwakwe KA, Chinomnso NC, et al. Socio-demographic determinants of herbal medicine use in pregnancy among Nigerian women attending clinics in a tertiary hospital in Imo State, South-East, Nigeria. Am J Med. 2016;4(1):1-10. [Google Scholar]
- 28. Mposhi A, Manyeruke C, Hamauswa S. The importance of patenting traditional medicines in Africa: The case of Zimbabwe. Int J Humanit Soc Sci. 2013;3(2):236-246. [Google Scholar]
- 29. Nergard CS, Ho TPT, Diallo D, Ballo N, Paulsen BS, Nordeng H. Attitudes and use of medicinal plants during pregnancy among women at health care centers in three regions of Mali, West-Africa. J Ethnobiol Ethnomed. 2015;11(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sharif MO, Janjua-Sharif F, Ali H, Ahmed F. Systematic reviews explained: AMSTAR-how to tell the good from the bad and the ugly. Oral Health Dent Manag. 2013;12(1):9-16. [PubMed] [Google Scholar]
- 31. Godlove MJ. Prevalence of Herbal Medicine Use and Associated Factors Among Pregnant Women Attending Antenatal Clinic at Mbeya Refferal Hospital in 2010. Dar es Salaam, Tanzania: Muhimbili University of Health and Allied Sciences; 2011. [Google Scholar]
- 32. Varga CA, Veale D. Isihlambezo: Utilization patterns and potential health effects of pregnancy-related traditional herbal medicine. Soc Sci Med. 1997;44(7):911-924. [DOI] [PubMed] [Google Scholar]
- 33. Panganai T, Shumba P. The African pitocin-a midwife’s dilemma: The perception of women on the use of herbs in pregnancy and labour in Zimbabwe, Gweru. Pan Afr Med J. 2016;25:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Negi PS. Plant extracts for the control of bacterial growth: Efficacy, stability and safety issues for food application. Int J Food Microbiol. 2012;156(1):7-17. [DOI] [PubMed] [Google Scholar]
- 35. Frawley J, Adams J, Sibbritt D, Steel A, Broom A, Gallois C. Prevalence and determinants of complementary and alternative medicine use during pregnancy: Results from a nationally representative sample of Australian pregnant women. Aust N Z J Obstet Gynaecol. 2013;53(4):347-352. [DOI] [PubMed] [Google Scholar]
- 36. Xue CC, Zhang AL, Lin V, Da Costa C, Story DF. Complementary and alternative medicine use in Australia: A national population-based survey. J Altern Compl Med. 2007;13(6):643-650. [DOI] [PubMed] [Google Scholar]
- 37. Henderson S, Kendall E. Culturally and linguistically diverse peoples’ knowledge of accessibility and utilisation of health services: Exploring the need for improvement in health service delivery. Aust J Prim Health. 2011;17(2):195-201. [DOI] [PubMed] [Google Scholar]
- 38. Bigdeli M, Jacobs B, Tomson G, et al. Access to medicines from a health system perspective. Health Policy Plan. 2013;28(7):692-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Studdert DM, Eisenberg DM, Miller FH, Curto DA, Kaptchuk TJ, Brennan TA. Medical malpractice implications of alternative medicine. JAMA. 1998;280(18):1610-1615. [DOI] [PubMed] [Google Scholar]
- 40. Ziel HK. Complementary alternative medicine boon or boondoggle? Skeptic. 1999;7(1):86-86. [Google Scholar]
- 41. Chigora P, Masocha R, Mutenheri F. The role of Indigenous Medicinal Knowledge (IMK) in the treatment of ailments in rural Zimbabwe: The case of Mutirikwi communal lands. J Sustain Dev Afr. 2007;9(2):26-43. [Google Scholar]
- 42. Bamidele JO, Adebimpe WO, Oladele EA. Knowledge, attitude and use of alternative medical therapy amongst urban residents of Osun State, southwestern Nigeria. Afr J Tradit, Complement Altern Med. 2009;6(3):281-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Langlois-Klassen D, Kipp W, Jhangri GS, Rubaale T. Use of traditional herbal medicine by AIDS patients in Kabarole District, Western Uganda. Am J Trop Med Hyg. 2007;77(4):757-763. [PubMed] [Google Scholar]
- 44. Mupfumira R. An Assessment of African Traditional Medicines in Pregnancy and on Birth Outcomes: Pharmacists’ Perceptions of Complementary Medicines in Pregnancy. Grahamstown, South Africa: Rhodes University Grahamstown; 2012. [Google Scholar]
- 45. Veale D, Havlik I, Katsoulis L, et al. The pharmacological assessment of herbal oxytocics used in South African traditional medicine. Biomed Environ. 1998;2:216-222. [Google Scholar]
- 46. Chuang C-H, Doyle P, Wang J-D, Chang P-J, Lai J-N, Chen P-C. Herbal medicines used during the first trimester and major congenital malformations. Drug Safety. 2006;29(6):537-548. [DOI] [PubMed] [Google Scholar]
- 47. Essilfie-Appiah G, Hofmeyr G, Moodley J. Misoprostol in obstetrics and gynaecology—benefits and risks. S Afr J Obstet Gynaecol. 2005;11(1):9-10. [Google Scholar]
- 48. Graham K. The Collaborative randomised aminoinfusion for meconium project (CRAMP): 1. South Africa and 2. Zimbabwe. Br J Obstet Gynaecol. 1998;105(11):1238-1239. [DOI] [PubMed] [Google Scholar]
- 49. Bucher HC, Guyatt GH, Cook RJ, et al. Effect of calcium supplementation on pregnancy-induced hypertension and preeclampsia: a meta-analysis of randomized controlled trials. JAMA. 1996;275(14):1113-1117. [DOI] [PubMed] [Google Scholar]
- 50. Fischer-Rasmussen W, Kjær SK, Dahl C, Asping U. Ginger treatment of hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol. 1991;38(1):19-24. [DOI] [PubMed] [Google Scholar]
- 51. Bandaranayake WM. Quality control, screening, toxicity, and regulation of herbal drugs. Modern Phytomedicine. 2006;25-57. https://onlinelibrary.wiley.com/doi/book/10.1002/9783527609987#page=45 [Google Scholar]
- 52. Routledge PA. The European herbal medicines directive. Drug Safety. 2008;31(5):416-418. [DOI] [PubMed] [Google Scholar]
- 53. Raynor DK, Dickinson R, Knapp P, Long AF, Nicolson DJ. Buyer beware? Does the information provided with herbal products available over the counter enable safe use? BMC Medicine. 2011;9(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Towns AM. Fertility and Fontanels: Women’s Knowledge of Medicinal Plants for Reproductive Health and Childcare in Western Africa. Leiden, Netherlands: Universiteit Leiden; 2014. [Google Scholar]
- 55. Shewamene Z, Dune T, Smith CA. The use of traditional medicine in maternity care among African women in Africa and the diaspora: A systematic review. BMC Complement Altern Med. 2017;17(1):382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ngomane S, Mulaudzi FM. Indigenous beliefs and practices that influence the delayed attendance of antenatal clinics by women in the Bohlabelo district in Limpopo, South Africa. Midwifery. 2012;28(1):30-38. [DOI] [PubMed] [Google Scholar]
- 57. Singh V, Raidoo DM, Harries CS. The prevalence, patterns of usage and people’s attitude towards Complementary and Alternative Medicine (CAM) among the Indian community in Chatsworth, South Africa. BMC Compl Alternative Med. 2004;4(1):3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. TamunoOmole-Ohonsi IA, Fadare J. Use of herbal medicine among pregnant women attending a tertiary hospital in northern Nigeria. Int J Gynecol Obstet. 2010;15(2):1-8. [Google Scholar]
- 59. Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Compl Alternative Med. 2009;9(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mawoza T, Nhachi C, Magwali T. Prevalence of traditional medicine use during pregnancy, at labour and for postpartum care in a rural area in Zimbabwe. Clin Mother Child Health. 2019;16(2):321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mureyi DD, Monera TG, Maponga CC. Prevalence and patterns of prenatal use of traditional medicine among women at selected harare clinics: A cross-sectional study. BMC Complement Altern Med. 2012;12(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chamisa JA. Zimbabwean Ndebele Perspectives on Alternative Modes of Child Birth. Pretoria, South Africa: University of South Africa; 2013. [Google Scholar]
- 63. Kennedy DA, Lupattelli A, Koren G, Nordeng H. Herbal medicine use in pregnancy: Results of a multinational study. BMC Complement Altern Med. 2013;13(1):355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Mekuria AB, Erku DA, Gebresillassie BM, Birru EM, Tizazu B, Ahmedin A. Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at University of Gondar referral and teaching hospital, Ethiopia: A cross-sectional study. BMC Compl Altern Med. 2017;17(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Addo V. Herbal medicines: socio-demographic characteristics and pattern of use by patients in a tertiary obstetrics and gynaecology unit. J Sci Technol. 2007;27(3):149-155. [Google Scholar]
- 66. Zamawe C, King C, Jennings HM, Fottrell E. Associations between the use of herbal medicines and adverse pregnancy outcomes in rural Malawi: A secondary analysis of randomised controlled trial data. BMC Complement Altern Med. 2018;18(1):166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zamawe C, King C, Jennings HM, Mandiwa C, Fottrell E. Effectiveness and safety of herbal medicines for induction of labour: A systematic review and meta-analysis. BMJ Open. 2018;8(10):e022499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Mothupi MC. Use of herbal medicine during pregnancy among women with access to public healthcare in Nairobi, Kenya: A cross-sectional survey. BMC Compl Alternative Med. 2014;14(1):432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Banda Y, Chapman V, Goldenberg RL, et al. Use of traditional medicine among pregnant women in Lusaka, Zambia. J Alternative Compl Med. 2007;13(1):123-128. [DOI] [PubMed] [Google Scholar]
- 70. Nyeko R, Tumwesigye NM, Halage AA. Prevalence and factors associated with use of herbal medicines during pregnancy among women attending postnatal clinics in Gulu district, Northern Uganda. BMC Pregnancy Childbirth. 2016;16(1):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Brookes KB. Chemical Investigation of Isihlambezo or Traditional Pregnancy-Related Medicines. Durban, South Africa: University of KwaZulu-Natal; 2004. [Google Scholar]
- 72. Mabina M, Pitsoe S, Moodley J. The effect of traditional herbal medicines on pregnancy outcome. S Afr Med J. 1997;87(8):1008-1010. [PubMed] [Google Scholar]
- 73. Naidu M. Constructing patient and patient healthcare: indigenous knowledge and the use of isihlambezo. IAJIKS. 2013;12(2):252-262. [Google Scholar]
- 74. Alabi AA, O’Mahony D, Wright G, Ntsaba MJ. Why are babies born before arrival at health facilities in King Sabata Dalindyebo Local Municipality, Eastern Cape, South Africa? A qualitative study. Afr J Prim Health Care Fam Med. 2015;7(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Mkize GT. An Assessment of Use of Traditional Medicine in Pregnacy and Associated Factors Among Black South African Women Delivering in Bertha Gxowa Hospital. Johannesburg, South Africa: University of Witwatersrand; 2015. [Google Scholar]
- 76. Maldonado-Morales MX. Culture, pregnancy, and its challenges. In: Clinical Handbook of Transcultural Infant Mental Health. Springer; 2019:151-166. [Google Scholar]
- 77. Stafford GI, Pedersen ME, van Staden J, Jäger AK. Review on plants with CNS-effects used in traditional South African medicine against mental diseases. J Ethnopharmacol. 2008;119(3):513-537. [DOI] [PubMed] [Google Scholar]
- 78. Ndhlala A, Stafford G, Finnie J, Van Staden J. In vitro pharmacological effects of manufactured herbal concoctions used in KwaZulu-Natal South Africa. J Ethnopharmacol. 2009;122(1):117-122. [DOI] [PubMed] [Google Scholar]
- 79. Ameade E, Zakaria A, Abubakar L, Sandow R. Herbal medicine usage before and during pregnancy—a study in Northern Ghana. Int J Complement Alt Med. 2018;11(4):235-242. [Google Scholar]
- 80. Prabha DS, Dahms H-U, Malliga P. Pharmacological potentials of phenolic compounds from Prosopis spp.-a review. J coast life med. 2014;2:918-924. [Google Scholar]
- 81. Coppin J. A Study of the Nutritional and Medicinal Values of Moringa Oleifera Leaves from Sub-Saharan Africa: Ghana, Rwanda, Senegal and Zambia. Piscataway, NJ: Rutgers University-Graduate School-New Brunswick; 2008. [Google Scholar]
- 82. Zahra’u B, Mohammed A, Ghazali H, Karim R. Baobab tree (Adansonia digitata L) parts: Nutrition, applications in food and uses in ethno-medicine–a review. Ann Nutr Disord Ther. 2014;1(3):1011. [Google Scholar]
- 83. Agbagba C, Agongo E, Apeawini G, et al. Pharmacological Importance of Some Fruit Bearing Trees On Princefield University College. Ho, Ghana: Emerald Campus; 2017. [Google Scholar]
- 84. Nordeng H, Al-Zayadi W, Diallo D, Ballo N, Paulsen BS. Traditional medicine practitioners’ knowledge and views on treatment of pregnant women in three regions of Mali. J Ethnobiol Ethnomed. 2013;9(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Maiga A, Diallo D, Fane S, Sanogo R, Paulsen BS, Cisse B. A survey of toxic plants on the market in the district of Bamako, Mali: Traditional knowledge compared with a literature search of modern pharmacology and toxicology. J Ethnopharmacol. 2005;96(1):183-193. [DOI] [PubMed] [Google Scholar]
- 86. Klotoé JR, Dougnon TV, Koudouvo K, et al. Ethnopharmacological survey on antihemorrhagic medicinal plants in South of Benin. Eur J Med Plants. 2013;3(1):40. [Google Scholar]
- 87. Asowa-Omorodion FI. Women’s perceptions of the complications of pregnancy and childbirth in two Esan communities, Edo state, Nigeria. Soc Sci Med. 1997;44(12):1817-1824. [DOI] [PubMed] [Google Scholar]