Abstract
Objective:
To identify the most appropriate threshold for disruptive mood dysregulation disorder (DMDD) diagnosis and the impact of potential changes in diagnostic rules on prevalence levels in the community.
Method:
Trained psychologists evaluated 3,562 preadolescents/early adolescents from the 2004 Pelotas Birth Cohort with the Development and Well-Being Behavior Assessment (DAWBA). The clinical threshold was assessed in 3 stages: symptomatic, syndromic, and clinical operationalization. The symptomatic threshold identified the response category in each DAWBA item, which separates normative misbehavior from a clinical indicator. The syndromic threshold identified the number of irritable mood and outbursts needed to capture preadolescents/early adolescents with high symptom levels. Clinical operationalization compared the impact of AND/OR rules for combining irritable mood and outbursts on impairment and levels of psychopathology.
Results:
At the symptomatic threshold, most irritable mood items were normative in their lowest response categories and clinically significant in their highest response categories. For outbursts, some indicated a symptom even when present at only a mild level, while others did not indicate symptoms at any level. At the syndromic level, a combination of 2 out of 7 irritable mood and 3 out of 8 outburst indicators accurately captured a cluster of individuals with high level of symptoms. Analysis combining irritable mood and outbursts delineated nonoverlapping aspects of DMDD, providing support for the OR rule in clinical operationalization. The best DMDD criteria resulted in a prevalence of 3%.
Conclusion:
Results provide information for initiatives aiming to provide data-driven and clinically oriented operationalized criteria for DMDD.
Keywords: child/adolescent, developmental psychopathology, disruptive mood dysregulation disorder, irritability, temper outbursts
Temper outbursts and irritable mood are common manifestations of typical development. When outbursts and irritable mood are intense, are frequent, last for significant periods, occur in several contexts, and are associated with behaviors not seen in typically developing children, they often require clinical attention.1–3 Disruptive mood dysregulation disorder (DMDD) is a new diagnosis designed to capture pathological manifestations of irritable mood and temper outbursts.4 Given the newness of DMDD, data-driven approaches based on epidemiological evidence are needed to evaluate appropriate thresholds for DMDD and consider the need to refine criteria. The current report provides such data.
DMDD has its origins in the mid-2000s when Leibenluft et al.5,6 defined a syndrome called severe mood dysregulation (SMD). SMD involved severe, chronic grouchy mood and heightened reactivity, along with symptoms of hyperarousal.6 The syndrome was defined to distinguish children with severe irritability from children with classic bipolar disorder (BD), in light of increasing numbers of children diagnosed with BD.7,8 The results of those studies converged to differentiate SMD from classic BD based on course and familial aggregation.9–11 For DSM-5, SMD was modified to create DMDD.
Alternative thresholds for defining DMDD have been only partially considered in the current literature. Some previous studies have focused on irritability as a dimensional trait, which is broader than DMDD as a diagnostic entity. These studies provide an important framework for investigating clinically relevant thresholds for specific behaviors. Wakschlag et al.12 used item response theory analysis to disentangle normative misbehavior from clinically significant problems by studying the symptomatic threshold, ie, investigating which response category in each item from a questionnaire separates normative misbehavior from a clinical indicator. They found that some behaviors are normative and represent problems only when their frequency is high or very high, whereas other behaviors always indicate a significant problem that requires clinical attention. This and similar research efforts in preschoolers13 inform attempts to evaluate varying boundaries for the definition of DMDD. Other studies focused more specifically on varying DSM-5 criteria for DMDD in preadolescents14,15 and adolescents.14–16 They found the prevalence of temper outbursts and negative mood are much lower than what is found in preschoolers and that applying exclusion criteria such as frequency and hierarchical diagnostic rules affects DMDD prevalence rates considerably.14–16 There was no evidence that clinical markers changed between preadolescence/early adolescence (9–12 years of age) and middle adolescence (13–16 years of age).15 Nonetheless, it is important to continue to identify appropriate diagnostic thresholds for distinct developmental periods, given that normative levels of irritability clearly vary across the life span.14–16
Another important step toward evaluating such varying boundaries involves quantifying the number of abnormal behaviors required to characterize a valid diagnosis, ie, identifying the syndromic threshold for a given diagnosis. Data-driven clustering approaches such as latent class analysis (LCA) derive groups that differ in the number of clinical indicators endorsed17 and thus inform attempts to set syndromic thresholds. Such efforts need to be balanced with clinical applicability in real-world settings, which require practical decisions such as how to combine clinical indicators from distinct domains (ie, irritable mood and outbursts). The latter can be achieved by investigating whether domains explain overlapping or distinct aspects of DMDD latent structure and related impairment, thus determining whether AND rules or OR rules should be used to provide a clinical operationalization of the diagnosis. Previous research in preadolescents and adolescents suggests irritable mood and temper outbursts predict each other over time. However, while each of them are associated with increased risk for disrupted functioning in adolescents,15 current criteria require both to be present for a diagnosis to be assigned.
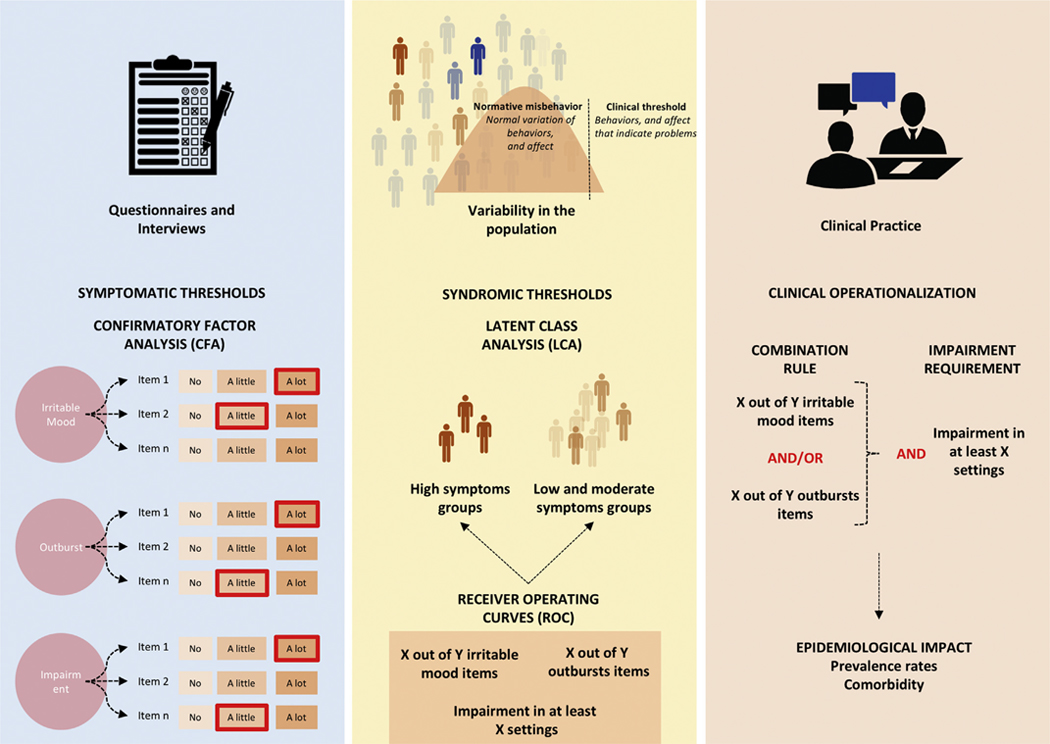
The aim of this study was to evaluate alternative clinical thresholds for the DMDD diagnosis (see Figure 1 for an overview of the analytic strategy and “Method” for details). We investigated 3562 preadolescents/early adolescents 10 to 12 years of age. First, we used confirmatory factor analysis (CFA) to identify item-level thresholds differentiating normative from clinical problems (the symptomatic threshold). This was used to dichotomize response levels as clinically significant or not. We next used these binary clinical indicators as input to LCA that assigned individuals into clusters with high and low levels of clinical indicators for each domain. This was followed by receiver operating characteristic (ROC) curves to detect the number of clinical indicators needed to predict class membership from LCA and to translate the data-driven results to DSM-5 symptom counts (the syndromic threshold). We then compared the impact of AND/OR rules on impairment and dimensional levels of psychopathology (clinical operationalization). Finally, we investigated the impact of varying definitions on DMDD prevalence and comorbidity profiles in a population-based sample.
FIGURE 1.
Symptomatic and Syndromic Thresholds and Clinical Operationalizations
METHOD
Participants
Participants of this study were preadolescents/early adolescents 10 to 12 years of age from the 2004 Pelotas Birth Cohort Study. All births occurring in the city of Pelotas, from January 1 to December 31, 2004, were enrolled and followed over time. Pelotas is in southern Brazil and has a population of 328,000. For a full description of the methods, see Santos et al.18 Briefly, all 4,231 live births in the city in 2004 whose mothers lived in the urban area and agreed to participate in the longitudinal study were considered eligible. Follow-up home visits were performed when the subjects had reached the ages of 3.0 months (SD = 0.1), 11.9 months (SD = 0.2), 23.9 months (SD = 0.4), and 49.5 months (SD = 1.7). When the subjects were, on average, 6.8 years old (SD = 0.3) and 11.0 years old (SD = 0.4), additional follow-up visits were conducted at a research clinic run by the Postgraduate Program of Epidemiology (Faculty of Medicine, Federal University of Pelotas, Brazil). Of the 4,231 subjects in the original birth cohort, 3,562 (84.1%) were included in our analysis, which used all available data from the 10 to 12 years of age assessment. The sample comprised 2,353 participants aged 10, 1,206 aged 11, and 4 aged 12. The prevalence of DMDD in this sample using current criteria associated with clinical ratings was 2.5% (95% CI 2.0–3.0).19 The study was approved by the Research Ethics Committee of the Federal University of Pelotas and by the Research Committee of the University of São Paulo School of Medicine. Written informed consent was obtained from all subjects.
Instruments and Diagnostic Assessment
The parent version of the DMDD section from the Development and Well-Being Assessment (DAWBA) questionnaire20 was administered by certified psychologists. This questionnaire uses open- and closed-ended questions to identify the occurrence of clinical indicators in children and adolescents 5 to 17 years of age based on the DSM criteria. The closed-ended questions start with 2 skip questions about the frequency of temper outbursts and irritable mood. Parents who answered that temper outbursts and/or irritable mood occurred at least once a week were probed to answer specific questions that characterize all DSM-5 criteria for DMDD.
A total of 593 parents of participants answered the DMDD section on irritable mood, representing the top 17% of irritable mood frequency. This section includes 9 items characterizing the threshold for experiencing anger, intensity of anger compared with peers of the same age, duration of anger during the day, whether irritable mood is perceived by others, setting in which anger occurs (at home, at school, with peers), and number of anger weeks throughout the year. A total of 425 parents answered the DMDD section on outbursts, representing the top 12% of frequency of outbursts. This section includes 15 items describing behavior during outbursts (slamming doors, shouting, swearing, saying mean things to others, saying negative things about self, physical aggression to others, deliberate self-harm, breaking things), setting in which outbursts occurred (at home, at school, with peers), and triggers (recognizable and easily triggered). We did not use the item “outbursts free-gap in the last year” in our analysis (DSM requires that there is not a period higher than ≥3 consecutive months without irritable mood and temper outbursts). The rationale for excluding this item is that it is unclear whether we would expect this item to be monotonically related to the overall latent construct given that short periods of irritability with large gaps could also inform episodes of irritability (a marker of severity and BD).
Lastly, 686 mothers or caregivers who completed either the outburst or the irritable mood sections were asked to also complete 4 items about impairment (impact on family life, friendship, learning, and leisure activities). After the impairment questions, mothers or caregivers answered the open-ended questions that allow qualitative description of the symptoms, frequency, and other characteristics of the disorder. All questions and response categories from the DMDD section are depicted in Table S1, available online.
The DAWBA was administered to mothers or caregivers by trained psychologists. The 40-hour training included lectures, role playing, and supervised clinical interviews with pediatric and mental health outpatients at the Federal University of Pelotas. The clinical evaluation of the total sample was performed by a psychologist, and a second independent psychologist evaluated 10% of the study sample. Both were trained in how to apply the DAWBA, in a standardized manner, by the child psychiatrist who had translated and validated the questionnaire for use in Brazil.21 Rating procedures were used for assigning comorbidities given that DMDD diagnosis was performed a posteriori. The interrater agreement was 91.2% for the presence of any psychiatric disorder, 75.9% for any anxiety disorder, 73.5% for any depressive disorder, 72.7% for attention-deficit/hyperactivity disorder, 72.9% for conduct disorder, 85.6% for any autism spectrum disorder, 59.5% for any eating disorder, and 52.4% for any tic disorder. Details of the questionnaire can be found online and in other studies.22
The Strengths and Difficulties Questionnaire (SDQ) was used to measure dimensional psychopathology. The SDQ is a 25-item behavioral screening questionnaire with 5 domains, each of which contains 5 items (emotional, conduct, hyperkinetic, peer relationships, prosocial behaviors, and impact scores). The overall SDQ total scores had a Cronbach a of .82, which is considered high. Internal consistency for the SDQ subscales was low to moderate ranging from 0.48 (peer relationships) to 0.78 (hyperkinetic). Despite low reliability, we maintained results from subscales for their descriptive nature in Supplement 1, available online.
Statistical Analysis
Symptomatic Threshold.
The 14 items on outbursts, 8 items on irritable mood, and 4 items on impairment were included in 3 CFAs testing unidimensional models for each construct (n = 593, n = 425, and n = 685, respectively). Details about the estimators and the model fit used in this study can be found in Table S2, available online, which provides the fit indexes of the unidimensional models for irritability, outbursts, and impairment items. CFA models estimate item level factor loadings (λ) and response category thresholds. Factor loadings represent the strength of the relationship between the latent trait and the item, ie, they indicate how well each item discriminates different severity levels of a given construct. Category thresholds indicate the expected value of the latent factor at which there is a 50% probability of endorsing a given category or higher, ie, the category threshold indicates the severity level at which the transition from 1 response category to the next is likely to happen (eg, from “no” to “a little” or higher, or from “a little” to “a lot”).
To distinguish normative misbehavior from behavior that would meet a diagnostic criterion, we used category thresholds from the CFA. CFAs were performed only in subjects with a frequency of irritable mood and outbursts greater than once a week. In this sample, a value of 0.5 represents a half SD above the mean of the distribution of subjects with a frequency of irritable mood and outbursts greater than once a week. Therefore, we interpreted values <0.5 as typical development (normative) and values ≥0.5 as clinical indicators (a proxy for symptoms or problem indicators). The latter represents an approximation to the top 5% most symptomatic preadolescents/early adolescents in the population, which is a threshold used in other diagnostic investigations.12 For details about the CFA, see Supplement 1, available online.
Syndromic Threshold.
Before data analysis, each questionnaire item was dichotomized at the value of the category threshold defined in the above-described symptomatic threshold analysis in subjects with at least 1 clinical indicator. Dichotomized items were chosen to enter the LCA because our intention was not to characterize varying levels of irritability in the community, but rather to identify groups that differ in their number of clinical indicators. Three LCAs were used to create empirically derived groups with different levels of clinical indicators for irritable mood, outbursts, and impairment. Next, we used 3 ROC curves to predict the most accurate number of clinical indicators for detecting participants with high levels of symptoms (as defined by LCA) with regard to irritable mood, outburst, and impairment. ROC curve analysis was used as a way to translate results from the syndromic thresholds of the LCA to the reality of clinical practice, which uses symptom counts. Thus, the ROC curve identifies a simple rule to allow the identification of patients who are likely to be members of the cluster that exhibit a high level of clinical indicators. The optimal cutoff was estimated using the Youden’s J statistic, which maximizes both sensitivity and specificity.23
Clinical Operationalization.
Four analytical strategies were used to determine the most appropriate rule for clinical operationalization: the OR rule versus the AND rule. First, we compared the fit of CFA models (n = 398), putting the selected dichotomized clinical indicators into a unidimensional model of irritability and a correlated model of irritability with 2 domains (irritable mood and outbursts). Second, we tested whether meeting criteria for the irritable mood group and/or for the outbursts group have distinct or overlapping associations with the impaired functioning group using a multiple logistic regression. Third, we used left censored regressions to compare skewed SDQ dimensional scores between subjects meeting criteria only for irritable mood, only for outbursts, either, or both and compared with a group of participants with other DSM disorders except for DMDD and typically developing comparisons. Fourth, for both OR groups and AND groups, we used a matching procedure to compare levels of SDQ scores between a group that differed in DMDD status (yes versus no DMDD) but were otherwise fully matched for comorbidities.
Epidemiological Impact.
Finally, using the relative frequency, we investigated the impact of these AND/OR rules and combinations for impairment requirements on the prevalence rates of DMDD in the community and on the comorbidity profile.
All analyses were performed in R version 3.6.1,24 including applications implemented in the packages lavaan 0.6–5,25 poLCA 1.4.1,26 pROC 1.15.3,27 CensReg 0.5–26,28 and MatchIt 3.0.2.29 The R markdown codes for the symptomatic, syndromic and clinical operationalization thresholds of current analysis can be found in Supplement 1, available online.
RESULTS
Symptomatic Threshold
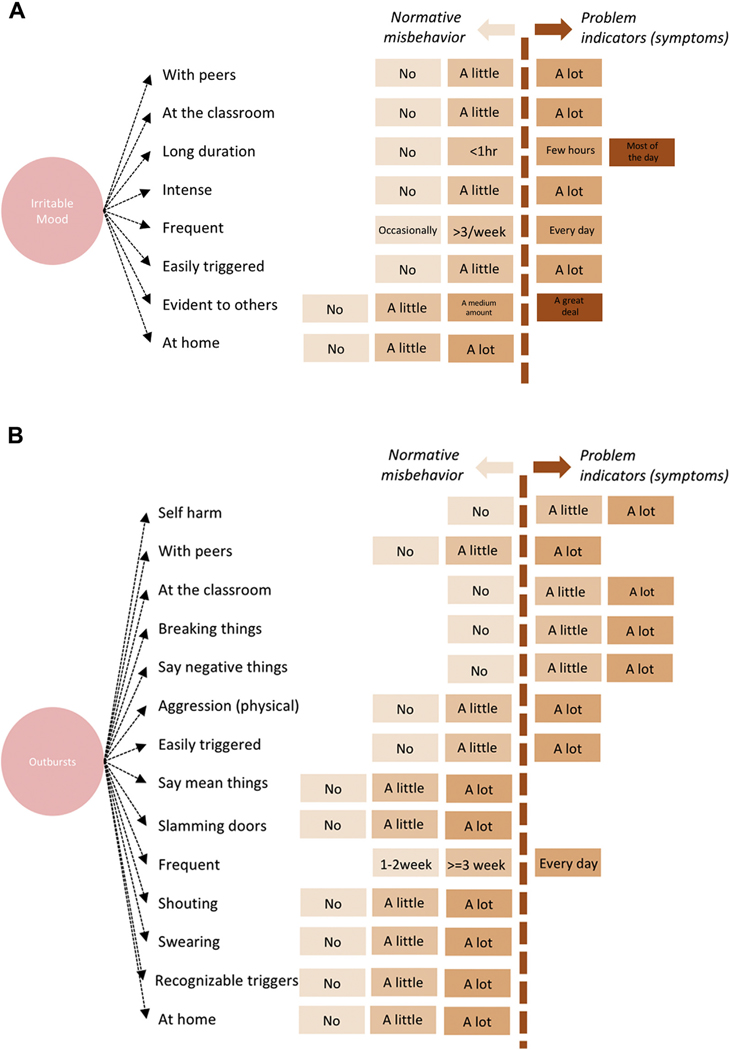
All 8 items of irritable mood were found to be normative in their lowest thresholds and clinical indicators (proxy for symptoms) in the highest thresholds except “irritable mood that happens at home,” which was found to be normative in all response categories. For the 6 items that describe intensity, the response option “a little” indicated normative behavior, while the response option “a lot” or “a great deal” indicated a symptom. For the duration item, irritable mood lasting <1 hour indicated normative behavior, whereas irritability lasting a few hours or most of the day indicated a symptom. For the frequency item, irritable mood occurring fewer than 3 times a week indicated normative behavior, whereas irritable mood occurring every day indicated a symptom (Table S3, available online).
For outbursts, threshold varied substantially across items. For some items, their occurrence even at mild levels indicated a symptom, whereas other items did not indicate a symptom at any level. Outbursts that included self-harm, breaking things, or saying negative things about self or those that occurred in the classroom were indicative of a symptom if they occurred at any level (ie, “a little” or “a lot”). Outbursts that occurred with peers, included physical aggression, or were easily triggered indicated a symptom when they occurred “a lot” but were normative when they occurred “a little.” Outbursts that occurred at home and included the preadolescents/early adolescents saying mean things, slamming doors, shouting, or swearing did not indicate a symptom regardless of the level endorsed. Also, whether the triggers were recognizable or not was not relevant to symptom designation. Regarding frequency, only outbursts that occurred daily indicated a symptom (Table S4, available online).
For impairment, “impact on family life” was normative when “a little” and indicated a symptom when “a medium amount” or “a lot.” Impairment that occurred in the other settings (friendship, learning, or leisure) indicated a symptom at any level (Figure 2 and Table S5, available online).
FIGURE 2. Symptomatic Threshold for Each Irritable Mood and Outbursts Item in the Confirmatory Factor Analysis.
Note: (A) Irritable mood. (B) Outbursts.
Syndromic Threshold
The prevalence of each clinical indicator is presented in Table 1. The 3 LCAs (irritable mood, outbursts, and impairment) indicated that the two-class solution was the best for each of the 3 domains (Table S6, available online). This indicates that in each of the 3 domains, the population was divided into 2 groups characterized by high versus low symptoms (Figure S1, available online). We next performed 3 ROC curve analyses (irritable mood, outburst, impairment) to determine the best number of clinical indicators (ie, items identified by the CFA) to use to predict membership in the high versus low symptom classes identified by the LCA. Youden’s J demonstrated that subjects in the high symptom irritable mood and outburst classes were most accurately characterized by 2 out of 7 irritable mood symptoms and 3 out of 8 outburst symptoms. As for impairment, the subjects with high level of symptoms in LCAs were most accurately characterized by significant impairment in at least 2 settings (Table 2 and Figure S2, available online).
TABLE 1.
Prevalencea of Each Disruptive Mood Dysregulation Disorder Item Written in Combination With the Response Category That Defines a Clinical Indicator
| Irritable mood/temper outbursts | Prevalence estimation of clinical indicators (%) | |
|---|---|---|
| Irritable mood | ||
| Frequency/duration | ||
| 1 | Irritable mood occurring every dayb | 2.1 |
| 2 | Irritable mood that lasts more than a few hoursb | 2.7 |
| Characteristics | ||
| 3 | Easily irritated, annoyed or angry a lotb | 3.6 |
| 4 | Intense irritable mood a lotb | 2.8 |
| Settings | ||
| 5 | Irritable mood occurs in the classroom a lotb | 1.1 |
| 6 | Irritable mood occurs with peers a lotb | 0.9 |
| 7 | Irritable mood is evident to others a great dealb | 1.7 |
| Temper outbursts | ||
| Frequency/duration | ||
| 1 | Outbursts occurring every dayb | 1.5 |
| Characteristics of outbursts | ||
| 2 | Saying any negative thing about selfb | 3.1 |
| 3 | Any physical aggression to othersb | 1.7 |
| 4 | Any form of deliberate self-harmb | 1.3 |
| 5 | Breaking things (any)b | 3.4 |
| Settings | ||
| 6 | Any outburst in the classroomb | 3.3 |
| 7 | Outbursts occurs with peers a lotb | 0.7 |
| Triggers | ||
| 8 | Easily triggered a lotb | 2.6 |
Note:
Prevalence estimates assume that preadolescents/early adolescents whose irritable mood and outbursts occurred less than once per week (and who therefore did not complete these items) do not have any of these problems to a significant degree.
Indicates the categories of responses necessary for each item to be considered a clinical indicator.
TABLE 2.
Receiver Operating Characteristic Curves Parameters Investigating the Best Number of Clinical Indicators to Capture Latent Class Groups
| Prediction of latent class groups |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Irritable mood |
Outbursts |
Severity of impairment |
||||||||||||||||
| Threshold | ACC | Sens | Spe | PPV | NPV | YI | ACC | Sens | Spe | PPV | NPV | YI | ACC | Sens | Spe | PPV | NPV | YI |
| 0 | 0.25 | 1.00 | 0.00 | 0.25 | — | 0 | 0.12 | 1.00 | 0.00 | 0.12 | — | 0 | 0.36 | 1.00 | 0.00 | 0.12 | — | 0 |
| 1 | 0.56 | 1.00 | 0.41 | 0.36 | 1.00 | 0.4 | 0.40 | 1.00 | 0.32 | 0.17 | 1.00 | 0.32 | 0.73 | 1.00 | 0.58 | 0.57 | 1.00 | 0.58 |
| 2 | 0.86 | 0.95 | 0.83 | 0.65 | 0.98 | 0.78 | 0.69 | 1.00 | 0.64 | 0.28 | 1.00 | 0.64 | 0.93 | 1.00 | 0.89 | 0.83 | 1.00 | 0.89 |
| 3 | 0.90 | 0.64 | 0.99 | 0.95 | 0.89 | 0.63 | 0.90 | 1.00 | 0.88 | 0.54 | 1.00 | 0.88 | 0.90 | 0.72 | 1.00 | 1.00 | 0.87 | 0.87 |
| 4 | 0.83 | 0.32 | 1.00 | 1.00 | 0.82 | 0.32 | 0.98 | 0.86 | 0.99 | 0.98 | 0.98 | 0.85 | 0.74 | 0.28 | 1.00 | 1.00 | 0.71 | 0.28 |
| 5 | 0.78 | 0.11 | 1.00 | 1.00 | 0.77 | 0.11 | 0.93 | 0.43 | 1.00 | 1.00 | 0.92 | 0.43 | — | — | — | — | — | — |
| 6 | 0.76 | 0.04 | 1.00 | 1.00 | 0.76 | 0.04 | 0.89 | 0.14 | 1.00 | 1.00 | 0.89 | 0.14 | — | — | — | — | — | — |
| 7 | 0.75 | 0.00 | 1.00 | — | 0.75 | 0 | 0.89 | 0.12 | 1.00 | 1.00 | 0.89 | 0.12 | — | — | — | — | — | — |
| 8 | 0.88 | 0.02 | 1.00 | 1.00 | 0.88 | 0.02 | — | — | — | — | — | — | ||||||
Note: Boldface types indicates the best number of clinical indicators to capture latent class groups. ACC = accuracy; NPV = negative predictive value; PPV = positive predictive value; Sens = sensitivity; Spe = specificity; YI = Youden’s index.
Clinical Operationalization
First, a model with 2 correlated domains (irritable mood and outbursts) provided a better fit than a unidimensional model encompassing both domains (χ2diff = 7.3, df = 1, p = .007) (Table S7, available online). Second, both irritable mood and outbursts were associated with clinical impairment in univariate models (irritable mood odds ratio = 41.71, p < .001; outbursts odds ratio = 76.1, p < .001) and in multiple models adjusted for the effects of including both predictors in the same model (irritable mood adjusted odds ratio = 18.2, p < .001; outbursts adjusted odds ratio = 23.63, p < .001). Third, comparisons between irritable only, outbursts only, and combined groups with typically developing comparisons and with a group of patients with other DSM disorders (except for DMDD) showed all 3 DMDD groups had higher scores on all SDQ scales than typically developing comparisons and higher total SDQ total scores than subjects with other DSM diagnosis (Figure S3 and Table S8, both available online). Fourth, left-censored regressions comparing groups matched for comorbidity (any anxiety, any mood, any hyperkinetic, and any disruptive behavior disorder) showed that, using either the OR rule or the AND rule, the DMDD group showed higher total, emotional, conduct, hyperactivity, peer relationship, and impact scores than the non-DMDD group with matched comorbidities (Figures S4 and S5, available online).
Epidemiological Impact
When using an OR rule, the optimal criteria from the ROC curve analysis (2 of 7 irritable mood symptoms, 3 of 8 outburst symptoms, impairment in at least 2 settings) resulted in a prevalence of 3.0%: 1.12% had only irritable mood, 0.64% had only outbursts, and 1.23% had both irritable mood and outbursts (Table 3). Both the OR rule and the AND rule resulted in higher levels of psychiatric comorbidities compared with the current DMDD clinical criteria (Table S9, available online).
TABLE 3.
Impact of Different Rules for Combining Irritable Mood and Temper Outburst Clinical Indicators and Impairment Requirements on Prevalence Rates of Disruptive Mood Dysregulation Disorder
| Irritable mood | Outbursts | AND rule | OR rule | |
|---|---|---|---|---|
| No impairment requirement | 2.41 | 0.9 | 1.63 | 4.94 |
| At least 1 setting | 1.80 | 0.70 | 1.46 | 3.96 |
| At least 2 settings (optimal) | 1.12 | 0.64 | 1.23 | 3.00 |
| At least 3 settings | 0.61 | 0.48 | 0.87 | 1.96 |
| All 4 settings | 0.17 | 0.17 | 0.53 | 0.87 |
Note: Boldface types indicates the optimal solution (impairment in at least 2 settings). Settings: 1 = impact on family life; 2 = impact on friendship; 3 = impact on learning; 4 = impact on leisure.
DISCUSSION
This study provides important information to guide a revision of the diagnostic criteria for DMDD. Using CFA, we found that 7 of the 8 irritable mood items were normative when endorsed in the low response categories and clinical indicators in the high response categories. The one exception was “irritable mood that happens at home,” which was always normative. For outbursts, the threshold for a clinical indicator varied substantially across items. For some items, such as outbursts with self-harm, their presence indicated a problem even at only mild levels. Others, such as shouting, were not clinical indicators even when present at the highest threshold. ROC curve analyses indicated that a combination of 2 of 7 irritable mood symptoms, 3 of 8 outburst symptoms, and significant impairment in at least 2 settings would best predict membership in the high versus low LCA-based symptom classes. The 4 clinical operationalization analyses converge to demonstrate that the 2 domains differ from a latent perspective, they are independently associated with impairment, and OR rule groups show comparable or even higher levels of impairment than other DSM disorders. Matched analysis showed that results cannot be attributed to comorbidity. The most accurate solution resulted in a prevalence of 3% in the fully automated operationalized criteria (1.12% only irritable mood, 0.64% only outbursts, and 1.23% combined).
Our findings are consistent with the limited literature examining irritability dimensionally in the population. Each set of findings suggests that normative outbursts differ from clinical indicators in frequency, duration, quality, context, and triggering events.30–33 Wakschlag et al.12 found that outbursts characterized by high frequency, “long duration,” or “aggressive components” or those that occurred “with nonparental adults” or “out of the blue” were clinical indicators. Wiggins et al.13 also used an empirical approach to identify irritable behaviors indicative of problems in preschoolers. They examined 22 temper loss behaviors from the criteria for oppositional defiant disorder, DMDD, and other depressive disorders in the DSM-5 and found 2 informative items. Similar to our work, the item “easily frustrated” indicated a symptom only when present nearly every day, but the item “break/destroy” indicated a symptom even when at lower frequencies. Nevertheless, those thresholds might vary substantially in distinct age ranges and cultures, which highlights the need for developmentally sensitive studies.
Clinical operationalization analysis suggests that an OR rule is most appropriate to capture cases in need of treatment. This algorithm identified preadolescents/early adolescents with either irritable mood or outbursts who manifested associated impairment, elevated symptoms, and functional impairment. This resulted in a prevalence rate of 3%, which is higher than the prevalence rate of 2.5% by the current diagnostic criteria. It is not possible to identify the “true” prevalence of DMDD in the population with 1 study; rather the current analyses inform nosologists’ attempts to weigh the strengths and weaknesses of various diagnostic thresholds.
Advancing understanding about DMDD diagnostic criteria is a major concern in the practice of child and adolescent psychiatrists. Our findings are a first step toward defining parameters to alert the clinician when to be (and when not to be) concerned with irritable mood and outbursts. Our approach suggests several refinements to the DSM-5 criteria. First, the new criteria provide a list of behaviors and a threshold for each behavior that specifies when to consider that behavior to be a clinical indicator. This is more descriptive, precise, and data-based than the current criteria and provide a way calibrate the severity of each clinical indicator composing the syndrome. Second, we suggest a syndromic threshold for the combination of such behaviors. This is a more practical way to separate normal from abnormal behaviors and considers that DMDD might manifest with distinct clinical indicators. Third, our data support an OR rule when combining irritable mood and outbursts rather than the AND rule currently in the manual. Finally, our results support the importance of requiring 2 settings for the diagnosis, as in DSM-5. Specifically, our data indicate that while the impact of symptoms on function needs to be at medium levels in family life to be considered a clinical indicator, mild levels of impairment in friendship, learning, or during leisure activities should suffice as a clinical indicator for the DMDD impairment criteria.
Our study has important strengths. First, we relied on a large representative population sample and implemented assessment methods that could mimic clinical assessment in the real world, as far as possible in an epidemiological investigation. Second, we applied CFA, LCA, and ROC curve analysis, applying a similar framework used in other disorders34,35 to a new syndrome that lacks empirical investigations to guide operationalization. However, this work has also some important limitations. First, our analysis is focused on internal validators. Further studies investigating course, family history, treatment response, and other external validators are needed to demonstrate the validity of the operationalized syndrome. As associations between symptoms and irritability-related impairment were investigated using the same DAWBA DMDD section, the size of the associations is likely to be overestimated. However, the value of these odds ratios may be helpful in understanding whether the 2 aspects of irritability capture distinct or overlapping aspects of irritability-related impairment. Second, our subjects were all 10 to 12 years old, and our data might not be generalized to other developmental stages. Third, because of the skip rule questions, the CFA parameters were estimated for subjects with irritable mood or outbursts that occurred at least once a week. Analyses were modeled to consider these characteristics, but this might have biased the parameter estimates for some items. Also, our approach assumes irritable mood, outbursts, and impairment are distinct domains, which is still an empirical question to be further tested. Fourth, our analysis is restricted to parent reports, and no information was acquired from preadolescents/early adolescents themselves. Lastly, our approach is restricted to a single sample, and it is unclear whether those results can be replicated in other samples.
In conclusion, this is the first study in the field with this intent in this age range and thus is a first step toward refining the diagnostic criteria of DMDD. Future research should include replicating these findings, extending similar approaches to diagnostic instruments other than the DAWBA, examining symptomatic thresholds using measures that do not have skipping rules and are designed specifically to differentiate normative versus nonnormative behaviors, investigating interrater reliability, and including developmentally sensitive items and external validators. Furthermore, prospective longitudinal investigation that applies this framework beginning at earlier ages can elucidate the origins of pathologic irritability, thus guiding the development of novel interventions and developmentally based prevention.
Supplementary Material
Acknowledgments
The Pelotas 2004 Birth Cohort is conducted by the Graduate Program in Epidemiology of Universidade Federal de Pelotas, supported by Associação Brasileira de Saúde Coletiva (ABRASCO-Brazilian Association of Public Health). From 2009 to 2013, the 2004 birth cohort was funded by the Wellcome Trust (United Kingdom). The 11-year follow-up was funded by the Sao Paulo Research Foundation-FAPESP (grant number 2014/13864–6). Previous phases of the study were funded by by the World Health Organization, Programa de Apoio a Núcleos de Excelência (PRONEX-Support Program for Excellence Centers), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq-National Council for Scientific and Technological Development), the Brazilian Ministry of Health, and Pastoral da Criança (Child’s Pastoral).
This work has been previously posted on a preprint server: https://doi.org/10.1101/19002436.
The authors thank the children and families for their participation, which made this research possible. The authors also thank the research team from the Pelotas 2004 Birth Cohort.
Disclosure: Drs. Laporte, Santos, Barros, and Salum have received support from the National Council for Scientific and Technological Development (CNPq). Dr. Rohde has received support from the CNPq. He has served on the speakers’ bureau/advisory board and/or acted as consultant for Eli Lilly and Company, Janssen-Cilag, Novartis, Medice, and Shire (a Takeda company) in the last 3 years. He has received authorship royalties from Oxford Press and ArtMed. He has received travel award for taking part in 2017 WFADHD and 2018 APA meetings from Novartis and Shire, respectively. The ADHD Disorder Outpatient Program chaired by him received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Janssen-Cilag, Novartis, and Shire. Drs. Matijasevich, Munhoz, Pine, and Leibenluft have reported no biomedical financial interests or potential conflicts of interest.
Contributor Information
Paola Paganella Laporte, Universidade Federal do Rio Grande do Sul, Graduate Program in Psychiatry and Behavioral Sciences, Brazil; the Section on Negative Affect and Social Processes, Hospital de Clínicas de Porto Alegre, Brazil; and the National Institute of Developmental Psychiatry for Children and Adolescents, CNPq, Brazil..
Alicia Matijasevich, Postgraduate Program in Epidemiology, Federal University of Pelotas, Brazil; Faculty of Medicine FMUSP, University of São Paulo, Brazil.
Tiago N. Munhoz, Postgraduate Program in Epidemiology, Federal University of Pelotas, Brazil; Faculty of Psychology, Federal University of Pelotas, Brazil.
Iná S. Santos, Postgraduate Program in Epidemiology, Federal University of Pelotas, Brazil.
Aluísio J.D. Barros, Postgraduate Program in Epidemiology, Federal University of Pelotas, Brazil.
Daniel S. Pine, Intramural Research Program, National Institute of Mental Health, Bethesda, Maryland.
Luis Augusto Rohde, Universidade Federal do Rio Grande do Sul, Graduate Program in Psychiatry and Behavioral Sciences, Brazil; the Section on Negative Affect and Social Processes, Hospital de Clínicas de Porto Alegre, Brazil; and the National Institute of Developmental Psychiatry for Children and Adolescents, CNPq, Brazil..
Ellen Leibenluft, Intramural Research Program, National Institute of Mental Health, Bethesda, Maryland.
Giovanni Abrahão Salum, Universidade Federal do Rio Grande do Sul, Graduate Program in Psychiatry and Behavioral Sciences, Brazil; the Section on Negative Affect and Social Processes, Hospital de Clínicas de Porto Alegre, Brazil; and the National Institute of Developmental Psychiatry for Children and Adolescents, CNPq, Brazil..
REFERENCES
- 1.Wakschlag LS, Estabrook R, Petitclerc A, et al. Clinical implications of a dimensional approach: the normal:abnormal spectrum of early irritability. J Am Acad Child Adolesc Psychiatry. 2015;54:626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petitclerc A, Briggs-Gowan MJ, Estabrook R, et al. Contextual variation in young children’s observed disruptive behavior on the DB-DOS: implications for early identification. J Child Psychol Psychiatry. 2015;56:1008–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perlman SB, Jones BM, Wakschlag LS, Axelson D, Birmaher B, Phillips ML. Neural substrates of child irritability in typically developing and psychiatric populations. Dev Cogn Neurosci. 2015;14:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 5.Leibenluft E Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168:129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leibenluft E, Blair RJR, Charney DS, Pine DS. Irritability in pediatric mania and other childhood psychopathology. Ann N Y Acad Sci. 2003;1008:201–218. [DOI] [PubMed] [Google Scholar]
- 7.Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996–2004. Biol Psychiatry. 2007;62:107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006;63:679–685. [DOI] [PubMed] [Google Scholar]
- 9.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166:1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16:456–466. [DOI] [PubMed] [Google Scholar]
- 11.Stringaris A, Baroni A, Haimm C, et al. Pediatric bipolar disorder versus severe mood dysregulation: risk for manic episodes on follow-up. J Am Acad Child Adolesc Psychiatry. 2010;49:397–405. [PMC free article] [PubMed] [Google Scholar]
- 12.Wakschlag LS, Choi SW, Carter AS, et al. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. J Child Psychol Psychiatry. 2012;53:1099–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiggins JL, Briggs-Gowan MJ, Estabrook R, et al. Identifying clinically significant irritability in early childhood. J Am Acad Child Adolesc Psychiatry. 2018;57:191–199.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 2013;170: 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Copeland WE, Brotman MA, Costello EJ. Normative irritability in youth: developmental findings from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2015;54:635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Althoff RR, Crehan ET, He J-P, Burstein M, Hudziak JJ, Merikangas KR. Disruptive mood dysregulation disorder at ages 13–18: results from the National Comorbidity Survey-Adolescent Supplement. J Child Adolesc Psychopharmacol. 2016;26:107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borsboom D, Rhemtulla M, Cramer AOJ, van der Maas HLJ, Scheffer M, Dolan CV. Kinds versus continua: a review of psychometric approaches to uncover the structure of psychiatric constructs. Psychol Med. 2016;46:1567–1579. [DOI] [PubMed] [Google Scholar]
- 18.Santos IS, Barros AJD, Matijasevich A, et al. Cohort profile update: 2004 Pelotas (Brazil) Birth Cohort Study. Body composition, mental health and genetic assessment at the 6 years follow-up. Int J Epidemiol. 2014;43:1437–1437a-f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munhoz TN, Santos IS, Barros AJD, Anselmi L, Barros FC, Matijasevich A. Perinatal and postnatal risk factors for disruptive mood dysregulation disorder at age 11: 2004 Pelotas Birth Cohort Study. J Affect Disord. 2017;215:263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41: 645–655. [PubMed] [Google Scholar]
- 21.Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry. 2004;43:727–734. [DOI] [PubMed] [Google Scholar]
- 22.La Maison C, Munhoz TN, Santos IS, Anselmi L, Barros FC, Matijasevich A. Prevalence and risk factors of psychiatric disorders in early adolescence: 2004 Pelotas (Brazil) birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2018;53:685–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. [DOI] [PubMed] [Google Scholar]
- 24.R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna,Austria; https://www.r-project.org/. [Google Scholar]
- 25.Rosseel Y lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48: 1–36; http://www.jstatsoft.org/v48/i02/. [Google Scholar]
- 26.Linzer DA, Lewis JB. poLCA: An R package for polytomous variable latent class analysis. J Stat Softw. 2011;42:1–29. [Google Scholar]
- 27.Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henningsen A censReg: Censored Regression (Tobit) Models. R package version 0.5. 2017; http://CRAN.R-Project.org/package=censReg. [Google Scholar]
- 29.Ho DE, Imai K, King G, Elizabeth A, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42:1–28; http://www.jstatsoft.org/v42/i08/. [Google Scholar]
- 30.Belden AC, Thomson NR, Luby JL. Temper tantrums in healthy versus depressed and disruptive preschoolers: defining tantrum behaviors associated with clinical problems. J Pediatr. 2008;152:117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhatia MS, Dhar NK, Singhal PK, Nigam VR, Malik SC, Mullick DN. Temper tantrums. Prevalence and etiology in a non-referral outpatient setting. Clin Pediatr (Phila). 1990;29:311–315. [DOI] [PubMed] [Google Scholar]
- 32.Osterman K, Björkqvist K. A cross-sectional study of onset, cessation, frequency, and duration of children’s temper tantrums in a nonclinical sample. Psychol Rep. 2010;106: 448–454. [DOI] [PubMed] [Google Scholar]
- 33.Wakschlag LS, Briggs-Gowan MJ, Carter AS, et al. A developmental framework for distinguishing disruptive behavior from normative misbehavior in preschool children. J Child Psychol Psychiatry. 2007;48:976–987. [DOI] [PubMed] [Google Scholar]
- 34.Kessler RC, Green JG, Adler LA, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Arch Gen Psychiatry. 2010;67:1168–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matte B, Anselmi L, Salum GA, et al. ADHD in DSM-5: a field trial in a large, representative sample of 18- to 19-year-old adults. Psychol Med. 2015;45:361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.