Learning objectives.
By reading this article, you should be able to:
-
•
Outline the reasons for the increased rate of occupational musculoskeletal disorders in anaesthetists.
-
•
Identify areas of your practice that would benefit from modifications to improve ergonomic conditions.
-
•
Describe the value of teaching ergonomics to anaesthetists early in their career to prevent injury and improve task performance.
Key points.
-
•
Occupational musculoskeletal injury is common amongst anaesthetists.
-
•
Musculoskeletal disorders cause pain, functional deficit and lost working days, and they can lead to early retirement.
-
•
Many of the procedures that anaesthetists perform daily can be hazardous to musculoskeletal health.
-
•
The experience of physical injury can be compounded by fatigue, emotional burden and cognitive strain.
-
•
Knowledge of ergonomics can prevent musculoskeletal injury and improve task performance.
Musculoskeletal disorders affect muscles, bones and joints throughout the body and can develop acutely or chronically and episodically. These disorders can progress from mild to severe and can impair quality of life.1 In healthcare, this progression can have a detrimental impact on practitioners' well-being, robustness of the workforce and patients' safety.
Musculoskeletal injury is a common occupational disorder; work-related musculoskeletal disorder (WRMSD) develops from the physical tasks necessitated by normal work activities. Specific factors increasing the risk of WRMSDs include fixed body positions or continuous repetition of movement, force on small body parts (such as the wrist) and a work schedule that does not include sufficient rest periods.1
Epidemiology of WRMSDs in anaesthetists in the UK
Neck and upper limb disorders
Healthcare workers in the UK have an above-average prevalence of musculoskeletal injury at 1420 per 100,000 workers (compared with the average of 1130 per 100,000).1 This accounts for 40% of sickness absence in the NHS compared with 27% of workdays lost to ill health nationally.1,2 The neck is the site affected most commonly, accounting for 44% of all cases of WRMSDs in the UK. Disorders affecting the neck and upper limbs together cause 50% of working days lost as a result of occupational musculoskeletal injury.
In one survey, 34% of anaesthetists had a formally diagnosed upper limb disorder, most commonly affecting the shoulder and neck.2 Cervical disc prolapse or degeneration and rotator cuff tendinitis were the most common single diagnoses identified. An association was found between the presence of upper limb disorders and years since beginning work in anaesthesia but not with the respondent's age, suggesting that occupational exposure is a risk factor.
Low back pain
Low back pain is the next most common WRMSD, with a prevalence of 520 cases per 100,000 workers in 2019–20 amongst all workers in the UK. Low back pain accounts for less than half of the days lost to sickness compared with neck and upper limb problems.1
Almost half the anaesthetists surveyed in one study reported low back pain related to working in clinical anaesthesia.3 This survey used the Oswestry Disability Index, a self-reporting tool, which is the basis of a diagnosis of chronic back pain. It is uncommon to have a definitive diagnosis. The practitioners subjectively attributed their low back pain to their clinical practice. Amongst those practitioners reporting pain, 44% had to make alterations to their working practice and 9.8% reported missing at least 1 day of work because of low back pain.
Epidemiology of WRMSDs amongst other operating theatre workers
Operating theatre personnel
Globally, the prevalence of musculoskeletal disorders amongst all operating theatre personnel was found to be highest for lower back pain (61% prevalence), followed by disorders of the ankle and foot (57%) and neck and shoulder conditions (both 56%).4 There was high heterogeneity between the results and a variety of diagnostic methods used in this meta-analysis. The lowest prevalence was for elbow disorders (23%) and hip pain (27%), which, nevertheless, represents a considerable burden of morbidity.4
Surgeons
The risk of musculoskeletal disorders is also increased amongst surgeons. Working in awkward or tiring positions is a common risk factor for developing a WRMSD and is arguably more relevant to surgical work than anaesthesia.1 A survey of UK plastic surgery consultants found a 32% prevalence of morbidity related to the cervical spine.5 A survey of UK ENT surgeons found a 47% prevalence of WRMSDs, but it used wider symptom criteria and had a lower response rate.6 The impact on productivity was highlighted, with 23% losing days to sickness and six surgeons retiring early.
The overall data suggest that neck and upper limb pain in operating theatre staff is actually less common than in the general population, and low back pain is the most common WRMSD in operating room personnel. The reasons behind this are not explained in the literature.
Ergonomic considerations for anaesthetists
The Health and Safety Executive ranks the most common reasons for musculoskeletal disorders at work as manual handling, working in awkward or tiring positions and repetitive actions (such as using a keyboard).1 This is relevant to anaesthetists because of the repetitive nature of certain tasks. Ignorance of correct posture and ergonomics dictated by the patient's position, clinical status and equipment is common and contributes to the increased risk of WRMSDs. Greater awareness of ergonomics, which is an applied science concerning the adaptation of a job or workplace to the needs of the workers to allow them to perform tasks safely and efficiently, could potentially negate this risk.
Airway management and tracheal intubation
Performing airway manoeuvres and tracheal intubation can require the anaesthetist to adopt potentially hazardous postures.
A task analysis study of simulated laryngoscopy using a Macintosh blade in groups at different stages of training showed that the less experienced group had a shallower line of sight when visualising the glottis, necessitating more levering of the laryngoscope and a reduction of the anaesthetist's height.7 This is often achieved by stooping or peering forward, which produces cervical shear forces and increases forces through lumbar soft tissue (Fig. 1A).
Fig 1.
(A) Levering rather than lifting the laryngoscope requires a ‘peering’ posture, which produces cervical shear forces. (B) Adjusting the bed height and rolling the head down maintains cervical alignment.
This potentially hazardous posture is analogous to that adopted by plastic surgeons wearing magnifying loupes. The increased cervical flexion and neck muscle tension needed to maintain the ‘peering forward’ position are associated with an increased risk of neck injury.5
More experienced practitioners perform tracheal intubation with improved ergonomics.8 Despite taking the same time and achieving the same success rate, experienced anaesthetists showed lower acceleration in the head and left hand, suggesting smoother motion. This implies a reduced potential for injury, or perhaps experienced practitioners have modified their movements in response to already-acquired musculoskeletal injury.
Compared with direct laryngoscopy, videolaryngoscopy has been shown to result in smaller deflections of all analysed postural angles except the wrist, and an objective measurement is that this posture is less likely to result in musculoskeletal injury.9 In many centres, videolaryngoscopy has replaced direct laryngoscopy as the primary technique for tracheal intubation.
The position of the anaesthetic machine and reservoir bag is often suboptimal, requiring the practitioner to overreach with shoulder angles of more than 120 degrees (Fig. 2A).10 Increasing the forces through the shoulder and exerting rotational forces through the cervical spine are potential causes of the increased prevalence of upper limb disorders in anaesthetists. This rotation of the cervical spine is further necessitated when the monitor is positioned to the side of or behind the anaesthetist (Fig. 2A). This disorder affects surgeons too, with excessive neck rotation to see the monitor being demonstrated in a time-and-motion study of surgeons performing laparoscopic surgery.11 An improvement would be to position the monitor such that end-range cervical motion is not required to be able to see the monitor. This could be achieved by aligning the head of the trolley with the edge of the monitor or using a slave screen linked to the original monitor if necessary. The position of the reservoir bag should be within the comfortable range of motion of the anaesthetist's shoulder, ideally close to the patient's head. This can be achieved by ergonomic anaesthetic room design or by using extension tubing that will decrease the risk of overextending the shoulder (Fig. 2B). Using the ventilator to ventilate the patient's lungs while holding the mask can also help to reduce the risk of musculoskeletal injury. Rolling the head down rather than peering forwards during laryngoscopy reduces unnecessary strain on the cervical spine (Fig. 1B). For neonatal intubation, sitting in an optimal position with the forearms horizontal is recommended.12
Fig 2.
(A) Overextension of the shoulder is seen when reaching to squeeze the bag for ventilation because the trolley is positioned too far forward from the anaesthetic machine. This also shows excessive cervical motion because of the position of the monitor. (B) Using extension tubing allows close positioning of bag and mask to avoid overextension of the shoulder. The patient in this image is a volunteer and the son of one of the authors.
Ergonomics of the anaesthetic room
The ergonomics of the anaesthetic room can compound the risk of musculoskeletal injury. The reported association between right-handedness and upper limb disorders may be explained by such a phenomenon.2 Anaesthetic machines have historically been designed with the oxygen rotameter on the left, in affinity with Boyle's machine whose inventor was himself left-handed. Although most modern machines in use do not have mechanical rotameters, overreaching of the right-handed anaesthetist to a left-sided oxygen rotameter, repeatedly over the course of a career, may be one cause of the increased prevalence of musculoskeletal injury. Placing the instrument tray on the practitioner's dominant side is preferable, but it may not be possible because of the layout of the room.
Trolley height
The height of the trolley, bed or table can affect the anaesthetist's posture at various stages throughout airway management. Discomfort was higher during mask ventilation when the bed was raised (at the level of the anaesthetist's xiphoid or nipple) compared with the bed being lower (at the level of the anaesthetist's lower rib margin or umbilicus).13 The opposite was true during tracheal intubation. When the bed is higher, the arm is elevated during mask ventilation, causing increased shoulder strain; at lower heights, the shoulder is within its range of motion and sustains no increased forces. The discomfort during tracheal intubation when the bed is too low is caused by increased forces on lumbar soft tissues when stooping to gain an improved view of the glottis.
The goal of correct alignment is to achieve maximal muscle performance with minimal load. During bag-mask ventilation, the patient's face should be positioned at the level of the anaesthetist's umbilicus, and the bed is raised to the level of the anaesthetist's xiphoid process or nipple for laryngoscopy.13
Regional anaesthesia
During the performance of neuraxial anaesthesia, practitioners' discomfort was significantly increased when the patient's bed was at lower heights compared with being higher.14 This discomfort may be explained by the observed increase in knee, lower back and neck flexion at the lower operating table heights. Excessive rotation (>90°) and flexion (>60°) of the cervical, thoracic and lumbar spine have been observed during the process of giving spinal anaesthesia.15 The trolley height should be optimised and the instrument tray positioned on the practitioner's dominant side for regional and neuraxial procedures.
Ergonomic principles taught in performance of regional anaesthesia determine that the ultrasound monitor, the regional anaesthesia needle and the practitioner are aligned in the same plane, to improve performance. A head-mounted display has been developed, which aims to keep the ultrasound image in the practitioner's field of vision, with the aim of improving hand–eye coordination, ensuring the procedure is successful and reducing musculoskeletal injury.16
Seating
The type of accessible seating can influence ergonomics. A seat with adjustable height is important to optimise upper limb and neck position when performing tasks, such as regional analgesia and arterial line insertion. Sitting on a backless stool can result in sustained end-range lumbar flexion, adding extra load to the passive structures (Fig. 3A). Adjustable height chairs with wheels, back and elbow support are ideal (Fig. 3B).
Fig 3.
(A) Sitting on backless stools in theatre can result in sustained end-range lumbar flexion, adding extra load to the passive structures. (B) Ergonomic theatre chairs with back support prevent the spine hanging in an end-range flexion posture.
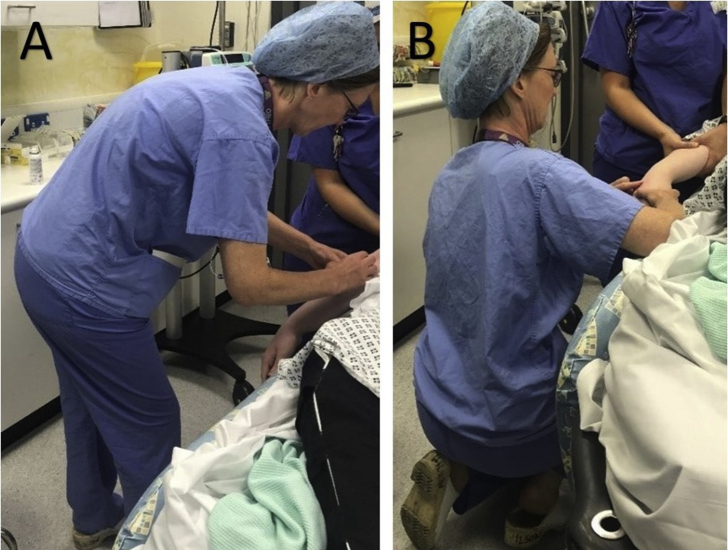
Vascular access and regional anaesthesia can all be performed more comfortably in sitting rather than standing positions, reducing forces through the cervical and lumbar spine and upper limbs (Fig. 4A). Kneeling is an alternative, but may be limited by knee pain (Fig. 4B).
Fig 4.
(A) Stooping during procedures, because the trolley is too low, increases forces on lumbar soft tissues (B) The height of the bed should be optimised for insertion of a spinal needle or vascular access, or sit or kneel to aim for a horizontal forearm without stooping.
Surgeons might be encouraged to sit when practicable too. Surgeons sitting rather than standing while performing vaginal surgery had less discomfort and spent less time with the shoulders in an unfavourable position, although this was at the expense of trunk flexion.17
Moving and handling aids
Moving and handling aids are used frequently in anaesthetic practice. Transfer slides and sheets facilitate moving anaesthetised patients and have been used safely to position patients prone in theatre and ICUs. In bariatric practice, an inflatable mattress uses airflow technology to ‘hover’ when transferring the patient, reducing physical strain on healthcare practitioners.
Task performance
The same principles apply to sporting achievement and task performance in anaesthesia. Time to completion of task, hand–eye coordination, fine motor control and psychomotor efficiency all improve with correct posture. Stooping and kneeling are both positions observed frequently in anaesthetic practice, for example when inserting an i.v. cannula or arterial line (Fig. 4A). Task performance is significantly faster when in an optimally seated position compared with kneeling or bending forward at the waist.12 Performance success, as measured by time taken, was shown to be proportional to comfort during the procedure; stooping and kneeling were both reported to be more painful than sitting. Kneeling in this study was on a carpet; therefore, it may be assumed to cause more pain on the hard floor of an anaesthetic room. Interestingly, the improvement in performance seen with sitting compared with stooping was the greatest in practitioners with poor manual dexterity, measured using predefined variables of hand–eye coordination, fine motor control and psychomotor efficiency. The improvement in performance was least in those practitioners with good manual dexterity. Posture makes the greatest improvement in task performance of inexperienced anaesthetists.
Biopsychosocial factors
Pain does not exist as a nociceptive phenomenon alone, but is experienced in the context of neurobiology, psychological distress, illness behaviour and social interactions. This describes the biopsychosocial model of pain.18 Psychological risk factors, such as stress and fatigue, can influence the perception of pain and the development of disability. Anaesthesia practitioners are frequently exposed to these risks because of long and unsocial hours and a greater emotional burden from the nature of their work. Stress and mental ill health are common amongst healthcare workers in general. In addition, 50% of the work-related ill health amongst healthcare workers in 2020 was stress, anxiety or depression.19
Consideration of the ergonomic structure of a workplace does not solely cover physical concerns but the interaction of multiple strains, which exist within occupations. Physical exertion and posture interact with the burdens of cognitive and emotional strain, and the demands of time, scheduling and hygiene protocols (Table 1).
Table 1.
Ergonomics of the workplace and interacting factors20
| Type | Factors |
|---|---|
| Personal factors | Age |
| Fitness | |
| Body mass index (BMI) | |
| Fatigue | |
| Health status | |
| Physical training and exercise habits | |
| Endurance | |
| Dexterity | |
| Strength | |
| Flexibility | |
| Circumstantial factors | Work organisation |
| Schedule | |
| Floor layout | |
| Equipment design | |
| Communication within the team | |
| Psychological support within the workplace | |
| Hygiene protocols | |
| Ambience | |
| Architecture | |
| Occupational factors | Physical workload |
| Working postures | |
| Emotional strain | |
| Cognitive burden |
Fatigue is prevalent amongst trainee anaesthetists.21 Fatigue can impair both cognitive function and psychomotor skills, increasing the risk of failure of task performance and of musculoskeletal injury.22 It can thus be considered a risk factor for anaesthetists developing musculoskeletal disorders.
Occupational injury is further influenced by factors outside the workplace. Upper limb disorders are more prevalent in anaesthetists with children, independent of the number of children or the sex of the anaesthetist.2 This could be explained by increased lifting and handling outside work, or the phenomenon of ‘double burden’, which describes the rigours of paid work alongside domestic and child-rearing work at home.23
Interventions to prevent WRMSD
Education
The finding that optimum posture improves the speed of task performance with the greatest effect in inexperienced practitioners suggests that teaching ergonomics to novice anaesthetists would improve success in clinical procedures. Furthermore, the consistent findings that novice anaesthetists in training display more hazardous postures present the opportunity for educating anaesthetists early in their careers regarding the correct postures to reduce musculoskeletal injury.
Managing stress and fatigue
Educational resources about fatigue and how to reduce the risks of musculoskeletal injury are available.24,25 These resources should be highlighted to trainees along with ergonomic training.
Preventative packages
Educational interventions should be delivered alongside robust occupational health and safety within a healthcare organisation, underpinned by an occupational health department undertaking preventative and reactive medicine. Early assessment, rehabilitation and work adjustment plans are recommended for any staff member who suffers a WRMSD.
There is evidence that preventative packages work. An intervention comparing the effectiveness of education in the operating theatre along with physiotherapy has been shown to reduce the incidence of lower back pain, analgesic use and quality of life in surgeons.26 It can be easier to notice potentially hazardous postures in others than in ourselves. A reminder about ergonomics in a preoperative checklist, for example about trolley height or monitor position, may be helpful. Each extreme position is not in itself dangerous, but total cumulative loading over a day and over a career can cause musculoskeletal injury. In some instances, the ideal alignment cannot be achieved, and this is acceptable.
Legislation
There is legislation in the Health and Safety at Work Act 1974.27 It describes the duty of the employer to protect the health and safety of their employees. This duty includes a risk assessment of tasks, such as manual handling, and a responsibility to reduce the risks of such tasks to as low as reasonably practicable. This can be achieved by staff training, the provision of manual handling aids and ergonomic workplace design, which includes consideration of lighting, non-slip floors and comfortable scrubs, for example. Employees have a reciprocal duty to take reasonable care of the health and safety of themselves and others by cooperating with the employer's regulations, following systems of work and using equipment designed to reduce musculoskeletal injury risk.
Conclusions
Knowledge of the practical application of sound ergonomic principles should be taught to anaesthetists early in their career to reduce the risk of musculoskeletal injury and improve task performance, with the greatest effect in inexperienced practitioners. Improving posture has the potential to have a positive impact on patients' safety and workforce productivity.
MCQs
The associated MCQs (to support CME/CPD activity) are accessible at www.bjaed.org/cme/home for subscribers to BJA Education.
Declaration of interests
The authors declare that they have no conflicts of interest.
Biographies
Catherine Riley MAFRCA MRCP is a specialty trainee in anaesthesia in Sheffield.
Catharine WilsonFRCA is a consultant paediatric anaesthetist at Sheffield Children's Hospital. She has organised departmental ergonomic training for anaesthetists and facilitated the purchase of improved seating for operating theatres.
Irralee Andrzejowska MCSP HCPC BApplSc is a senior associate physiotherapist with an interest in chronic back pain and has held back care workshops at the Doctors Updates Conferences in Portugal since 2013.
Prosenjit Giri DMRD MD MSc FFOM is a consultant occupational health physician in Sheffield, a health examiner and medical supervisor for the General Medical Council and training programme director in the Yorkshire and Humber Deanery. He sees and treats individuals with injuries related to anaesthesia in South Yorkshire as part of his professional practice.
Matrix codes: 1H02, 1I03, 2A01, 2D03, 2G02, 3J00, 3J02
References
- 1.Health and Safety Executive . 2021. Work-related musculoskeletal disorders statistics in Great Britain.https://www.hse.gov.uk/statistics/causdis/msd.pdf Available from: [Google Scholar]
- 2.Leifer S., Choi S.W., Asanati K., Yentis S.M. Upper limb disorders in anaesthetists—a survey of Association of Anaesthetists members. Anaesthesia. 2019;74:285–291. doi: 10.1111/anae.14446. [DOI] [PubMed] [Google Scholar]
- 3.Anson J.A., Mets E.J., Vaida S.J., Ochoa T., Gordin V., King T.S. Are we hurting ourselves?” What is the prevalence of back pain in anesthesia providers? J Clin Anesth. 2016;34:502–506. doi: 10.1016/j.jclinane.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 4.Tavakkola R., Kavib E., Hassanipourc S., Rabieie H., Malakoutikhah M. The global prevalence of musculoskeletal disorders among operating room personnel: a systematic review and meta-analysis. Clin Epidemiol Glob Health. 2020;8:1053–1061. [Google Scholar]
- 5.Godwin Y., Macdonald C.R., Kaur S., Zhelin L., Baber C. The impact of cervical musculoskeletal disorders on UK consultant plastic surgeons: can we reduce morbidity with applied ergonomics? Ann Plast Surg. 2017;78:602–610. doi: 10.1097/SAP.0000000000001073. [DOI] [PubMed] [Google Scholar]
- 6.Vijendren A., Yung M., Sanchez J., Duffield K. Occupational musculoskeletal pain amongst ENT surgeons—are we looking at the tip of an iceberg? J Laryngol Otol. 2016;130:490–496. doi: 10.1017/S0022215116001006. [DOI] [PubMed] [Google Scholar]
- 7.Walker J.D. Posture used during laryngoscopy. Br J Anaesth. 2002;89:772–774. [PubMed] [Google Scholar]
- 8.Sakakura Y., Kamei M., Sakamoto R., et al. Biomechanical profiles of tracheal intubation: a mannequin-based study to make an objective assessment of clinical skills by expert anesthesiologists and novice residents. BMC Med Educ. 2018;18:293–301. doi: 10.1186/s12909-018-1410-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grundgeiger T., Hurtienne J., Roewer N., Happel O., Grundgeiger J. Body posture during simulated tracheal intubation: GlideScope videolaryngoscopy vs Macintosh direct laryngoscopy for novices and experts. Anaesthesia. 2015;70:1375–1381. doi: 10.1111/anae.13190. [DOI] [PubMed] [Google Scholar]
- 10.Couldrey A., Ng E., Radhakrishna S. Ergonomics in anaesthesia: table height and body position during the induction of anaesthesia. Conference abstract. Anaesthesia. 2018;73:89. [Google Scholar]
- 11.Aitchison L.P., Cui C.K., Arnold A., Nesbitt-Hawes E., Abbott J. The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc. 2016;30:5068–5076. doi: 10.1007/s00464-016-4855-4. [DOI] [PubMed] [Google Scholar]
- 12.Buffington C., MacMurdo S.D., Ryan C.M. Body position affects manual dexterity. Anesth Analg. 2006;102:1879–1883. doi: 10.1213/01.ane.0000217124.94291.98. [DOI] [PubMed] [Google Scholar]
- 13.Lee H.C., Yun M.J., Hwang J.W., Na H.S., Kim D.H., Park J.Y. Higher operating tables provide better laryngeal views for tracheal intubation. Br J Anaesth. 2014;112:749–755. doi: 10.1093/bja/aet428. [DOI] [PubMed] [Google Scholar]
- 14.Sohn H.M., Kim H., Hong J.P., Lee K.M., Kim J. Higher operating table for optimal angle and less discomfort during spinal anaesthesia. Anesth Analg. 2018;26:1349–1352. doi: 10.1213/ANE.0000000000002534. [DOI] [PubMed] [Google Scholar]
- 15.Amjal M., Power S., Smith T., Shorten G. An ergonomic task analysis of spinal anaesthesia. Eur J Anaesthesiol. 2009;26:1037–1042. doi: 10.1097/EJA.0b013e3283317dc9. [DOI] [PubMed] [Google Scholar]
- 16.Udani A.D., Harrison T.K., Howard S.K., et al. Preliminary study of ergonomic behaviour during simulated ultrasound guided regional anaesthesia using a head mounted display. J Ultrasound Med. 2021;31:1277–1280. doi: 10.7863/jum.2012.31.8.1277. [DOI] [PubMed] [Google Scholar]
- 17.Singh R., Yurteri-Kaplan L.A., Morrow M.M., et al. Sitting versus standing makes a difference in musculoskeletal discomfort and postural load for surgeons performing vaginal surgery. Int Urogynecol J. 2019;30:231–237. doi: 10.1007/s00192-018-3619-1. [DOI] [PubMed] [Google Scholar]
- 18.Colvin L., Harrington L. In: Smith and Aitkenhead’s textbook of anaesthesia. Thompson J., Moppett I., Wiles M., editors. Elsevier; London: 2019. Pain; p. 508. [Google Scholar]
- 19.Health and Safety Executive . 2021. Human health and social work activities statistics in Great Britain.https://www.hse.gov.uk/statistics/industry/health.pdf Available from: [Google Scholar]
- 20.Encyclopaedia of Occupational Health & Safety . 2011. Hospital ergonomics: a review.https://www.iloencyclopaedia.org/part-xvii-65263/health-care-facilities-and-services/item/439-hospital-ergonomics-a-review Available from: [Google Scholar]
- 21.McClelland L., Holland J., Lomas J.P., Redfern N., Plunkett E. A national survey of the effects of fatigue on trainees in anaesthesia in the UK. Anaesthesia. 2017;72:1069–1077. doi: 10.1111/anae.13965. [DOI] [PubMed] [Google Scholar]
- 22.Health and Safety Executive. Human factors: fatigue. 2006. Available from: https://www.hse.gov.uk/humanfactors/topics/fatigue.htm (accessed 4 January 2021).
- 23.Vargas-Prada S., Macdonald E.B. Increased reporting of musculoskeletal pain in anaesthetists: is it an occupational issue? Anaesthesia. 2019;74:274–276. doi: 10.1111/anae.14537. [DOI] [PubMed] [Google Scholar]
- 24.Association of Anaesthetists. The culture of fatigue. 2014. Available from: https://anaesthetists.org/Home/Wellbeing-support/Fatigue/The-culture-of-fatigue (accessed 4 January 2021).
- 25.Association of Anaesthetists . 2021. Better musculoskeletal health for anaesthetists.https://anaesthetists.org/Home/Resources-publications/Guidelines/Better-musculoskeletal-health-for-anaesthetists Available from: [Google Scholar]
- 26.Giagio S., Volpe G., Gasparre G., Frizziero A., Pillastrini P., Squizzato F. A preventive program for work-related musculoskeletal disorders among surgeons: outcomes of a randomized controlled clinical trial. Ann Surg. 2019;270:969–975. doi: 10.1097/SLA.0000000000003199. [DOI] [PubMed] [Google Scholar]
- 27.Health and Safety Executive. The law on musculoskeletal disorders at work. 2020. Available from: https://www.hse.gov.uk/msd/legislation.htm (accessed 4 January 2021).