Key Points
Question
Is neighborhood opportunity differentially associated with health outcomes by race and ethnicity among US children with diabetic ketoacidosis?
Findings
In this cross-sectional study including 72 726 pediatric encounters for diabetic ketoacidosis, the probability of readmission within 365 days was significantly higher among non-Hispanic Black children compared with Hispanic children and non-Hispanic White children at the same level of opportunity. Within racial and ethnic groups, children with very low opportunity had significantly greater probability of readmission compared with those with very high opportunity.
Meaning
These findings suggest that despite having similar measures of neighborhood opportunity, non-Hispanic Black children with type 1 diabetes experience disparities in health outcomes compared with children in other racial and ethnic groups.
This cross-sectional study assesses whether neighborhood opportunity is associated with type 1 diabetes–related outcomes by race and ethnicity, including readmissions for diabetic ketoacidosis and co-occurring acute kidney injury and cerebral edema.
Abstract
Importance
The Child Opportunity Index 2.0 (COI) assesses neighborhood resources and conditions that influence health. It is unclear whether the COI scores are associated with health outcomes by race and ethnicity among children with type 1 diabetes (T1D).
Objective
To determine whether COI categories are associated with diabetes-related outcomes by race and ethnicity, including readmissions for diabetic ketoacidosis (DKA) and co-occurring acute kidney injury (AKI) or cerebral edema (CE).
Design, Setting, and Participants
This cross-sectional study included children discharged with a primary diagnosis of T1D with DKA between January 1, 2009, and December 31, 2018. Merged data were obtained from the Pediatric Health Information System and COI. Participants included children and adolescents younger than 21 years with an encounter for DKA. Data were analyzed from April 29, 2021, to January 5, 2022.
Exposures
Neighborhood opportunity, measured with the COI as an ordered, categorical score (where a higher score indicates more opportunity), and race and ethnicity.
Main Outcomes and Measures
The primary outcome was readmission for DKA within 30 and 365 days from an index visit. Secondary outcomes included the proportion of encounters with AKI or CE. Mixed-effects logistic regression was used to generate probabilities of readmission, AKI, and CE for each quintile of COI category by race and ethnicity.
Results
A total of 72 726 patient encounters were identified, including 38 924 (53.5%) for girls; the median patient age was 13 (IQR, 9-15) years. In terms of race and ethnicity, 600 (0.8%) of the encounters occurred in Asian patients, 9969 (13.7%) occurred in Hispanic patients, 16 876 (23.2%) occurred in non-Hispanic Black (hereinafter Black) patients, 40 129 (55.2%) occurred in non-Hispanic White (hereinafter White) patients, and 5152 (7.1%) occurred in patients of other race or ethnicity. The probability of readmission within 365 days was significantly higher among Black children with a very low COI category compared with Hispanic children (risk difference, 7.8 [95% CI, 6.0-9.6] percentage points) and White children (risk difference, 7.5 [95% CI, 5.9-9.1] percentage points) at the same COI category. Similar differences were seen for children with very high COI scores and across racial groups. The COI category was not associated with AKI or CE. However, race and ethnicity constituted a significant factor associated with AKI across all COI categories. The probability of AKI was 6.8% among Black children compared with 4.2% among Hispanic children (risk difference, 2.5 [95% CI, 1.7-3.3] percentage points) and 4.8% among White children (risk difference, 2.0 [95% CI, 1.3-2.6] percentage points).
Conclusions and Relevance
These results suggest that Black children with T1D experience disparities in health outcomes compared with other racial and ethnic groups with similar COI categories. Measures to prevent readmissions for DKA should include interventions that target racial disparities and community factors.
Introduction
Diabetic ketoacidosis (DKA) is the leading cause of hospitalization, morbidity, and mortality in children with type 1 diabetes (T1D).1,2 Previous studies have identified racial and ethnic disparities among children with T1D, particularly regarding risk of DKA. A study from the Centers for Disease Control and Prevention3 found that non-Hispanic Black (hereinafter Black) children had a nearly 2-fold increased risk of diabetes-related mortality, which included deaths due to DKA, compared with non-Hispanic White (hereinafter White) children. Further, White children are less likely to require hospitalization for DKA compared with children of other races and ethnicities.2,4 Although socioeconomic factors—including lack of health insurance or public insurance,2,4,5,6,7,8,9,10,11,12 lower income or living in areas of poverty,2,4,9,10,12 and lower parental educational achievement10—have been associated with higher risk and severity of DKA, other community attributes may influence health outcomes.
The Child Opportunity Index 2.0 (COI) was developed in 2020 and is a novel instrument that provides a comprehensive assessment of neighborhood attributes that may elucidate structural inequities and provide a more robust and practical assessment of social factors that influence health outcomes.13 Studies have shown that greater neighborhood opportunity is associated with fewer acute care visits14 and hospitalizations for ambulatory care conditions.15,16 It is unclear whether neighborhood opportunity influences diabetes-related outcomes. To address this gap in knowledge, we evaluated whether COI categorical scores are associated with diabetes-related outcomes by race and ethnicity with regard to (1) readmissions for DKA and (2) complications of DKA, including acute kidney injury (AKI) and cerebral edema (CE).
Methods
Study Design, Participants, and Setting
We conducted a cross-sectional study of children and adolescents younger than 21 years who were discharged from inpatient, observation, or emergency department care with a primary diagnosis of T1D with ketoacidosis (International Classification of Diseases, Ninth Revision [ICD-9], codes 250.11 and 250.13 or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10], codes E10.10 and E10.11) from January 1, 2009, to December 31, 2019. We excluded encounters from 2019 because these were used to determine readmission for 2018, duplicate encounters (ie, 2 encounters with the same admission date), and encounters with missing COI categorical scores or demographic information. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline and was deemed exempt from review and the need for informed consent by the institutional review board of Childrens’ Minnesota.
Data Sources
Clinical data were obtained from the Pediatric Health Information System (PHIS), which is managed by the Children’s Hospital Association, Lenexa, Kansas, and includes data from the largest US children’s hospitals. Data quality and reliability are assured through a joint effort between the Children’s Hospital Association and participating hospitals. Participating hospitals provide encounter-level data, including demographics, diagnoses, procedures, and measures of resource use. Complex chronic conditions were identified using diagnoses, procedures, measures of resource use, and associated complex chronic conditions.17 Race and ethnicity were determined by site-specific practices at each participating PHIS hospital, including self-report by a child’s guardian. We categorized race and ethnicity into 5 groups: Asian, Black, Hispanic, White, and other (including American Indian, multiracial, other race, and missing).
The COI measures neighborhood resources and conditions across more than 72 000 US Census tracts (ie, neighborhoods) from all 50 states and Washington, DC, using data from numerous sources, including the National Center for Education Statistics and the US Department of Education, and is publicly available.13,18 The COI includes 29 indicators across 3 domains: (1) educational (eg, third grade math and reading proficiency, high school graduation rates), (2) health and environmental (eg, proximity to grocery stores, proximity to parks and open spaces), and (3) socioeconomic opportunities (eg, unemployment rate, proximity to employment). The COI provides scale scores (range, 1-100) and quintile categorical scores (very low, low, moderate, high, and very high, ) for each domain and a composite for all Census tracts and zip codes in the US. Because the PHIS only includes zip codes, we used the COI at the zip code level. Notably, zip codes were assigned at the encounter level and could change if a patient moved between encounters.
Outcomes
The primary outcomes were readmissions for DKA within 30 days and within 365 days of an index visit resulting in hospitalization. For children with multiple admissions, each hospitalization was considered an index admission regardless of the number of days since the previous DKA admission. Readmissions were coded as binary (yes or no) variables based on the number of days between the date of discharge and the date of the next admission with a primary diagnosis of DKA. Patients readmitted within 30 days were included among those readmitted within 365 days. Secondary outcomes included the proportion of encounters with codes for AKI (ICD-9: 584.5-584.9 and 586; ICD-10: N17.0-N17.2, N17.8, N17.9, and N19) or CE (ICD-9: 348.5; ICD-10: G93.6) at the index visit. Acute kidney injury and CE were selected as secondary outcomes given the commonality of AKI19,20,21,22 and the mortality associated with CE.17,23,24,25
Statistical Analysis
Data were analyzed from April 29, 2021, to January 5, 2022. We used descriptive statistics to summarize encounter-level demographics and clinical outcomes overall and by COI category (very low, low, moderate, high, and very high). Patient-level characteristics were defined with respect to the patient’s incident encounter.
We used mixed-effects logistic regression to estimate the association between neighborhood COI and our binary outcomes: (1) 30-day readmission, (2) 365-day readmission, (3) AKI, and (4) CE, with random intercepts for hospital and patient. Models for 30- and 365-day readmissions were adjusted for the following covariates: age, sex, payer, complex chronic condition, intensive care unit admission, concurrent diagnosis of AKI or CE, and discharge year. In addition, we tested the significance of the interaction between race and ethnicity and COI category using a Wald test for each outcome. Nonsignificant interaction terms were excluded from the final model. Results for our regression models are reported as probabilities standardized to the distribution of the covariates in our sample and percentage-point risk differences with 95% CIs using the postestimation margins command in Stata.26 To summarize the proportion of variation in our outcomes explained by hospital and patient random effects, we used intraclass correlation coefficients. All analyses were conducted using Stata, version 16 (StataCorp LLC), and 2-sided P < .05 was considered statistically significant.
Results
A total of 83 445 DKA encounters were identified, of which 72 726 were included in our analysis (median age, 13 [IQR, 9-15] years; 38 924 for girls [53.5%] and 33 802 for boys [46.5%]) (Table 1), representing 46 496 unique patients from 49 hospitals. In terms of race and ethnicity, 600 (0.8%) of the encounters occurred in Asian patients, 16 876 (23.2%) occurred in Black patients, 9969 (13.7%) occurred in Hispanic patients, 40 129 (55.2%) occurred in White patients, and 5152 (7.1%) occurred in patients of other race or ethnicity. Overall, 2931 encounters (4.0%) resulted in a readmission for DKA within 30 days and 17 850 (24.5%) within 365 days of the index encounter (Figure 1).
Table 1. Demographic and Encounter Characteristics by COI Category.
| Characteristic | Encounters by COI categorya | |||||
|---|---|---|---|---|---|---|
| All (N = 72 726) | Very low (n = 17 263) | Low (n = 15 271) | Moderate (n = 14 599) | High (n = 12 940) | Very high (n = 12 653) | |
| COI domain scores, mean (SD)b | ||||||
| Socioeconomic | 48 (29) | 11 (7) | 32 (8) | 52 (9) | 71 (9) | 90 (7) |
| Health and environment | 44 (28) | 16 (16) | 32 (19) | 47 (21) | 63 (20) | 76 (17) |
| Educational | 47 (29) | 15 (12) | 33 (15) | 48 (16) | 66 (15) | 86 (10) |
| Age, y | ||||||
| Median (IQR) | 13 (9-15) | 13 (10-16) | 13 (10-15) | 13 (9-15) | 12 (9-15) | 12 (9-15) |
| <6 | 7578 (10.4) | 1344 (7.8) | 1493 (9.8) | 1528 (10.5) | 1588 (12.3) | 1625 (12.8) |
| 6-11 | 21 789 (30.0) | 4787 (27.7) | 4448 (29.1) | 4301 (29.5) | 4018 (31.1) | 4235 (33.5) |
| >11 | 43 359 (59.6) | 11 132 (64.5) | 9330 (61.1) | 8770 (60.1) | 7334 (56.7) | 6793 (53.7) |
| Sex | ||||||
| Girls | 38 924 (53.5) | 9531 (55.2) | 8311 (54.4) | 7894 (54.1) | 6690 (51.7) | 6498 (51.3) |
| Boys | 33 802 (46.5) | 7732 (44.8) | 6960 (45.6) | 6705 (45.9) | 6250 (48.3) | 6155 (48.6) |
| Race and ethnicity | ||||||
| Asian | 600 (0.8) | 68 (0.4) | 83 (0.5) | 117 (0.8) | 103 (0.8) | 229 (1.8) |
| Black | 16 876 (23.2) | 8198 (47.5) | 3492 (22.9) | 2532 (17.3) | 1652 (12.8) | 1002 (7.9) |
| Hispanic | 9969 (13.7) | 3333 (19.3) | 2473 (16.2) | 1958 (13.4) | 1352 (10.4) | 853 (6.7) |
| White | 40 129 (55.2) | 4511 (26.1) | 8135 (53.3) | 9014 (61.7) | 8943 (69.1) | 9526 (75.3) |
| Otherc | 5152 (7.1) | 1153 (6.7) | 1088 (7.1) | 978 (6.7) | 890 (6.9) | 1043 (8.2) |
| Insurance | ||||||
| Government | 38 706 (53.2) | 12 757 (73.9) | 9478 (62.1) | 7644 (52.4) | 5334 (41.2) | 3493 (27.6) |
| Private | 31 734 (43.6) | 4010 (23.2) | 5387 (35.3) | 6379 (43.7) | 7218 (55.8) | 8740 (69.1) |
| Complex chronic condition | 3093 (4.3) | 864 (5.0) | 629 (4.1) | 598 (4.1) | 533 (4.1) | 469 (3.7) |
| Hospital LOS, median (IQR), d | 2 (1-3) | 2 (1-3) | 2 (1-3) | 2 (1-3) | 2 (1-3) | 2 (1-3) |
| ICU | ||||||
| Admission | 27 689 (38.1) | 6834 (39.6) | 6005 (39.3) | 5874 (40.2) | 4685 (36.2) | 4291 (33.9) |
| LOS, median (IQR), d | 1 (1-1) | 1 (1-1) | 1 (1-1) | 1 (1-1) | 1 (1-1) | 1 (1-1) |
| Outcomes | ||||||
| Readmission | ||||||
| Within 30 d | 2931 (4.0) | 1047 (6.1) | 601 (3.9) | 558 (3.8) | 445 (3.4) | 280 (2.2) |
| Within 365 d | 17 850 (24.5) | 5994 (34.7) | 4065 (26.6) | 3499 (24.0) | 2506 (19.4) | 1786 (14.1) |
| AKI | 3592 (4.9) | 884 (5.1) | 764 (5.0) | 776 (5.3) | 573 (4.4) | 595 (4.7) |
| CE | 1029 (1.4) | 254 (1.5) | 211 (1.4) | 217 (1.5) | 175 (1.3) | 172 (1.3) |
Abbreviations: AKI, acute kidney injury; CE, cerebral edema; COI, Child Opportunity Index 2.0; ICU, intensive care unit; LOS, length of stay; PHIS, Pediatric Health Information System.
Unless otherwise indicated, data are expressed as number (%) of encounters. Percentages have been rounded and may not total 100.
Scores range from 0 to 100, with higher scores indicating greater opportunity.
Includes American Indian, multiple races, listed as other when submitted to PHIS by participating hospital, and missing.
Figure 1. Study Flowchart.
COI indicates Child Opportunity Index 2.0; DKA, diabetic ketoacidosis. Encounters for which patients were readmitted within 30 days were included for those readmitted within 365 days in the analysis.
The probability of readmission for DKA was associated with COI category (eFigure in the Supplement). Readmission for DKA within 365 days was highest for children living in very low–opportunity neighborhoods (19.2% [95% CI, 17.8%-20.5%]) (Table 2). Comparatively, the probability of readmission for children in very high–opportunity neighborhoods was 5.4 percentage points lower (13.8% [95% CI, 12.6%-15.0%]). The interaction between racial and ethnic groups and COI category was statistically significant (P = .04).
Table 2. Probability of Readmission at 30 and 365 Days, Acute Kidney Injury, and Cerebral Edema by Race and Ethnicity and COI Category.
| Variable | Probability of outcome by COI category, % (95% CI) | |||||
|---|---|---|---|---|---|---|
| Very low | Low | Moderate | High | Very high | ||
| 30-d Readmissions | ||||||
| Overall | 3.7 (3.3 to 4.1) | 3.1 (2.7 to 3.5) | 3.2 (2.8 to 3.6) | 3.1 (2.7 to 3.5) | 2.5 (2.1 to 2.9) | |
| Race and ethnicity | ||||||
| Asian | 2.7 (−1.4 to 6.8) | 2.3 (−1.0 to 5.6) | 4.1 (0.2 to 8.0) | 1.3 (1.2 to 3.8) | 0.7 (−0.7 to 2.1) | |
| Black | 5.1 (4.3 to 5.9) | 3.9 (3.1 to 4.7) | 3.9 (3.1 to 4.7) | 4.0 (3.0 to 5.0) | 4.8 (3.4 to 6.2) | |
| Hispanic | 3.3 (2.5 to 4.1) | 2.6 (2.0 to 3.2) | 2.5 (1.7 to 3.3) | 3.2 (2.2 to 4.2) | 2.2 (1.2 to 3.2) | |
| White | 3.2 (2.6 to 3.8) | 2.8 (2.4 to 3.2) | 3.0 (2.6 to 3.4) | 2.8 (2.4 to 3.2) | 2.1 (1.7 to 2.5) | |
| Other | 2.0 (1.2 to 2.8) | 2.9 (1.9 to 3.9) | 2.5 (1.5 to 3.5) | 1.7 (0.7 to 2.7) | 1.7 (0.9 to 2.5) | |
| 365-d Readmissions | ||||||
| Overall | 19.2 (17.8 to 20.5) | 17.2 (16.0 to 18.4) | 16.2 (15.0 to 17.4) | 15.3 (14.1 to 16.8) | 13.8 (12.6 to 15.0) | |
| Race and ethnicity | ||||||
| Asian | 14.5 (5.9 to 23.1) | 11.4 (5.9 to 16.9) | 9.0 (3.1 to 14.9) | 4.5 (0.2 to 8.8) | 4.8 (1.5 to 8.1) | |
| Black | 24.9 (23.1 to 26.7) | 22.8 (20.8 to 24.8) | 21.1 (18.9 to 23.3) | 21.2 (18.8 to 23.6) | 20.4 (17.7 to 23.1) | |
| Hispanic | 17.1 (15.4 to 18.9) | 16.6 (14.8 to 18.5) | 15.5 (13.6 to 17.4) | 15.9 (13.7 to 18.2) | 13.9 (11.4 to 16.5) | |
| White | 17.4 (15.8 to 19.0) | 14.9 (13.5 to 16.3) | 14.6 (13.4 to 15.8) | 13.0 (11.8 to 14.2) | 11.2 (10.0 to 12.4) | |
| Other | 16.1 (13.7 to 18.5) | 16.6 (14.2 to 19.0) | 12.7 (10.3 to 15.1) | 11.0 (8.6 to 13.4) | 9.9 (7.7 to 12.2) | |
| Acute kidney injury | ||||||
| Overall | 5.6 (4.2 to 7.0) | 5.3 (3.9 to 6.7) | 5.4 (4.0 to 6.8) | 5.0 (3.6 to 6.4) | 4.8 (3.4 to 6.2) | |
| Race and ethnicity | ||||||
| Asian | 6.7 (0.4 to 13.3) | 2.8 (−0.7 to 6.3) | 5.1 (0.4 to 9.8) | 4.8 (0.7 to 8.9) | 5.8 (2.7 to 8.9) | |
| Black | 7.2 (5.4 to 9.0) | 7.1 (5.1 to 9.1) | 6.5 (4.7 to 8.3) | 6.9 (4.7 to 9.1) | 5.7 (3.7 to 7.7) | |
| Hispanic | 4.1 (2.7 to 5.5) | 4.2 (2.8 to 5.6) | 4.6 (3.0 to 6.2) | 4.7 (3.1 to 6.3) | 3.8 (2.2 to 5.4) | |
| White | 5.5 (3.9 to 7.1) | 4.9 (3.5 to 6.3) | 4.8 (3.4 to 6.2) | 4.4 (3.2 to 5.6) | 4.5 (3.3 to 5.7) | |
| Other | 5.4 (3.4 to 7.4) | 4.7 (2.9 to 6.5) | 6.4 (4.2 to 8.6) | 5.1 (3.1 to 7.1) | 4.3 (2.7 to 5.9) | |
| Cerebral edema | ||||||
| Overall | 1.9 (1.5 to 2.3) | 1.6 (1.2 to 2.0) | 1.7 (1.3 to 2.1) | 1.5 (1.1 to 1.9) | 1.4 (1.0 to 1.8) | |
| Race and ethnicity | ||||||
| Asian | 1.7 (−1.6 to 5.0) | 0.9 (−0.9 to 2.7) | 0.9 (−0.9 to 2.7) | 1.0 (−1.0 to 3.0) | 0.5 (−0.5 to 1.5) | |
| Black | 2.1 (1.5 to 2.7) | 2.0 (1.2 to 2.8) | 1.4 (0.8 to 2.4) | 1.8 (1.0 to 2.6) | 1.5 (0.5 to 2.5) | |
| Hispanic | 1.6 (1.0 to 2.2) | 1.3 (7.0 to 1.9) | 1.4 (0.8 to 2.0) | 1.4 (0.8 to 2.0) | 1.1 (0.3 to 1.9) | |
| White | 1.8 (1.2 to 2.4) | 1.6 (1.2 to 2.0) | 1.8 (1.2 to 2.4) | 1.4 (1.0 to 1.8) | 1.5 (1.1 to 1.9) | |
| Other | 1.8 (1.0 to 2.6) | 1.8 (0.8 to 2.85) | 1.5 (0.7 to 2.3) | 1.6 (0.8 to 2.4) | 1.3 (0.5 to 2.1) | |
Abbreviation: COI, Child Opportunity Index 2.0.
At all levels of overall COI, Black children had a greater probability of readmission compared with Hispanic children and White children (Figure 2 and Table 2). Across racial groups, the probability of readmission within 365 days of an index encounter was significantly higher among Black children with an overall very low COI category compared with White children (risk difference, 7.5 [95% CI, 5.9-9.1] percentage points) and Hispanic children (risk difference, 7.8 [95% CI, 6.0-9.6] percentage points) at the same level of COI (Table 2). Similar racial differences were seen for children with an overall very high COI category (risk difference for Black compared with White children, 9.3 [95% CI, 6.6-11.9] percentage points; risk difference for Black compared with Hispanic children, 6.5 [95% CI, 4.4-8.6] percentage points) (Table 2). Within racial groups, Hispanic (risk difference, 3.2 [95% CI, 0.4-5.9] percentage points), Black (risk difference, 4.5 [95% CI, 1.7-7.2] percentage points), and White (risk difference, 6.2 [95% CI, 4.9-7.6 percentage points]) children with an overall very low COI category had significantly greater probability of readmission within 365 days compared with those with an overall very high COI category. Patient random effects explained approximately 40% of the variation in 365-day readmission (intraclass correlation coefficient, 0.40 [95% CI, 0.38-0.41]). Only minor variation in our outcome was explained by hospital effects (intraclass correlation coefficient, 0.02 [95% CI, 0.01-0.04]).
Figure 2. Probabilities of the Main Outcomes of Readmission and Diabetes-Related Complications by Race and Ethnicity and Overall Neighborhood Child Opportunity.
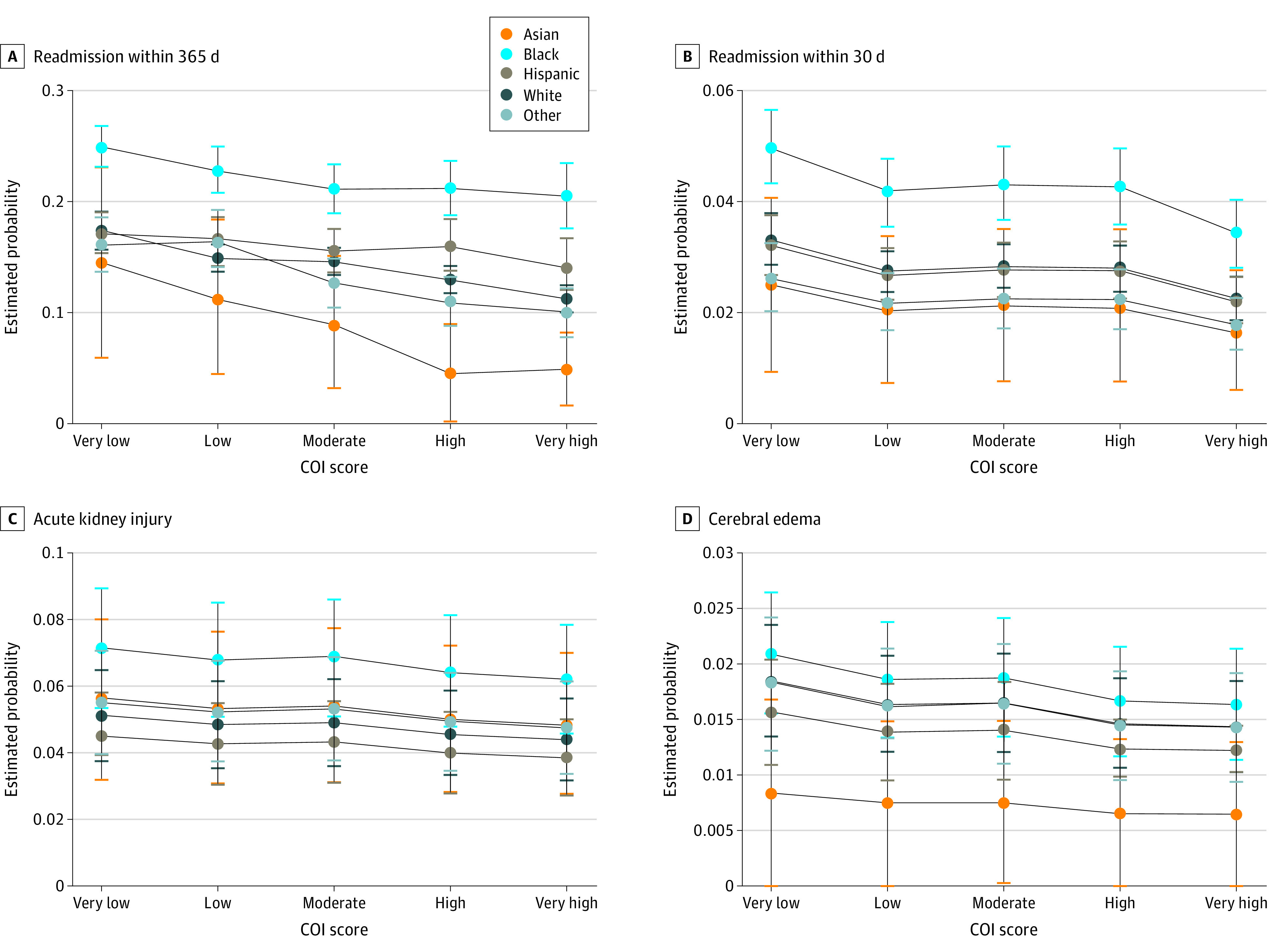
Child opportunity index 2.0 (COI) categorical scores at or below the 20th percentile were categorized as very low; greater than 20th to at or below the 40th percentile, as low; greater than 40th to at or below the 60th percentile, as moderate; greater than 60th to at or below the 80th percentile, as high; and greater than 80th percentile, as very high. Whiskers represent 95% CIs.
For each of the 3 COI domains, Black children had a greater probability of 365-day readmission at all COI categories compared with Hispanic children and White children (Figure 3). Among children with very low socioeconomic COI domains, the probability of readmission within 365 days was significantly higher compared with that of White children (risk difference, 6.2 [95% CI, 4.0-8.4] percentage points) and Hispanic children (risk difference, 6.7 [95% CI, 4.1-9.3] percentage points) with very low socioeconomic COI domains (eTable in the Supplement). The interaction between racial and ethnic group and COI domain was statistically significant for the socioeconomic domain (Wald χ2 = 30.22; P = .02). Similar results were seen for the health and environment and educational domains.
Figure 3. Probability of Readmissions Within 365 Days by Race and Ethnicity and Neighborhood Child Opportunity Domains.
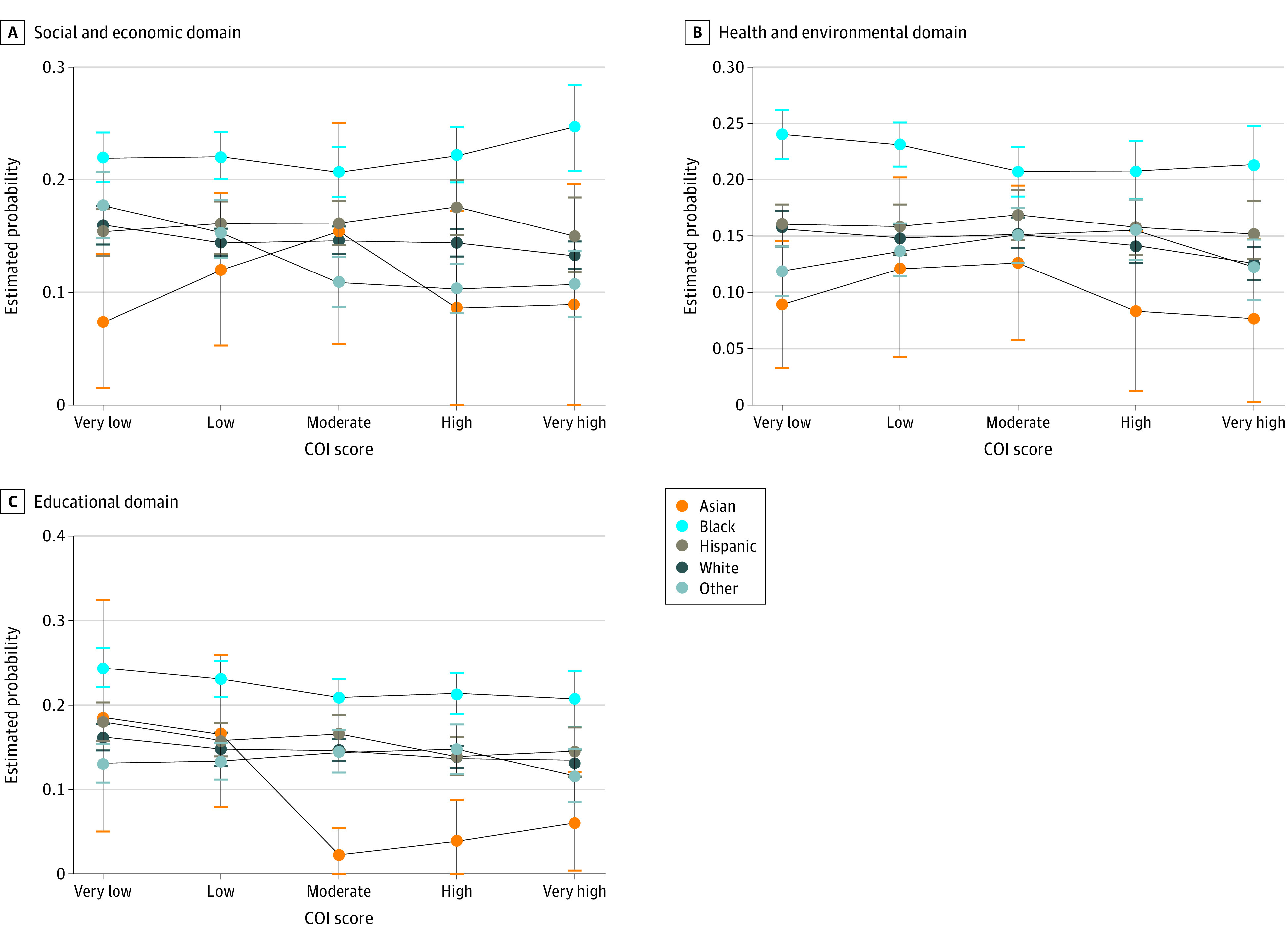
Child opportunity index 2.0 (COI) categorical scores at or below the 20th percentile were categorized as very low; greater than 20th to at or below the 40th percentile, as low; greater than 40th to at or below the 60th percentile, as moderate; greater than 60th to at or below the 80th percentile, as high; and greater than 80th percentile, as very high. Whiskers represent 95% CIs.
Category of COI was not associated with AKI; the probability of AKI was 5.6% among children with an overall very low COI category compared with 4.8% among those with an overall very high COI category (risk difference, 0.8 [95% CI, 0-1.3] percentage points); frequency was 4.9% among all categories. Race and ethnicity did not modify the association between COI category and AKI (Wald χ2 = 13.4; P = .65). However, race and ethnicity were independently associated with AKI (Figure 2 and Table 2). The probability of AKI was 6.8% among Black children compared with 4.8% among White children (risk difference, 2.0 [95% CI, 1.3-2.6] percentage points) and 4.2% among Hispanic children (risk difference, 2.5 [95% CI, 1.7-3.3] percentage points). Neither COI nor race and ethnicity were significantly associated with CE, and there was no evidence of effect modification (Wald χ2 = 6.82; P = .96) (Figure 2 and Table 2).
Discussion
Our findings suggest that Black children experience disparities in T1D care despite having similar measures of neighborhood opportunity when compared with other racial groups. Using data from 49 US children’s hospitals, we observed that Black children had greater probability of readmission for DKA compared with Hispanic children and White children at all COI categories. Within racial and ethnic groups, children with an overall very low COI category had significantly greater probability of readmission compared with those with an overall very high COI category. Our results have implications for health systems seeking to reduce disparities.
Hospital readmissions are commonly used as a quality indicator, in part because they may be avoidable with appropriate care during the index hospitalization and sufficient ambulatory care after discharge. This concept is the motivation for financial penalties associated with pay-for-performance strategies, such as the Centers for Medicare & Medicaid Services Hospital Readmission Reduction Program27 for adults and the Potentially Preventable Readmission measure used for pediatric readmissions.28,29 Although the use of readmissions as a quality indicator is controversial,30,31 the burden to families and health systems is undeniable. It has been estimated that 30-day pediatric readmissions account for $678 million dollars of all annual health care costs.32 For children with T1D, the median charge for a DKA readmission is greater than $12 000,1 and pediatric intensive care unit charges are even higher.33 Children who are readmitted also experience length of stays more than double those of patients who are not readmitted,34 making the burden on families even greater as they spend more time away from work and incur personal expenses. Further, the burden of readmission may disproportionately affect families who identify as Black and/or have public insurance, both of which are associated with increased readmission rates.35,36,37
Investigation has shown that there is widespread variation in readmissions for DKA across US children’s hospitals.1 A 2017 study38 showed that 365-day readmissions were significantly higher for Black children with T1D (21.7%) compared with children of other races (13.4%). In another study using PHIS data from 2004 to 2012,7 365-day readmissions for DKA occurred in 28% of children, and factors associated with readmission included public insurance and Black race. Both findings are consistent with our results. Further, the authors of one of these studies7 showed that Black race was associated with higher odds of 365-day readmission in 59% of hospitals, suggesting variation in DKA admission frequency across hospitals. It is unclear what drives this variation, although a number of factors likely contribute, including implicit biases39,40 and possibly neighborhood factors. More recently, Maxwell et al9 conducted a retrospective population-based cohort study using data from Cincinnati Children’s Hospital from 2011 to 2017 and examined whether Census tract poverty, race, and insurance status were associated with hospitalization for DKA in children. The authors conducted a subanalysis among children who were readmitted and found that Black race, public insurance status, and greater Census tract poverty were significantly associated with readmission.9 However, this study was limited in that the number of readmissions was low, with only 42 children (10%) being readmitted during the study period.9
Several studies14,15,16 have begun to explore the association among neighborhood opportunity, acute care use, and hospitalizations. One study found that residing in an area in the very low COI category was associated with significantly greater odds of having multiple acute care visits for conditions amenable to outpatient care compared with children who live in areas in the very high COI category.14 A similar study found that the hospitalization rate for asthma was significantly higher at 9.1 per 1000 children living in areas in the very low COI category compared with 1.8 per 1000 for those living in areas in the very high COI category.15 Area deprivation, a measure of neighborhood opportunity derived from American Community Survey data, has recently been associated with greater odds of hospital admission for recurrent DKA.41 However, that study was limited to a single state, which reduces generalizability. Only 1 previous study16 has evaluated use of diabetes resources in association with COI categories. Krager et al16 found that the hospitalization rate for children with diabetes and associated complications was significantly higher at 2.8 per 1000 children for those living in areas with a very low COI category compared with 1.5 per 1000 children in areas with a very high COI category.16 In the present study, we expand on these findings, using data from the largest children’s hospitals merged with COI data.
Our results provide an equity-focused evaluation of disparities as they are associated with diabetes-related outcomes. The COI includes measures such as reading and math proficiency, adult educational attainment, and access to healthy food, all of which are particularly important for children living with T1D because they must calculate insulin dosing, manage diabetes technology (eg, insulin pumps), and find healthy food choices. The importance is further supported by previous work showing that the risk of DKA and glycemic excursions are associated with lower parental educational level10,11,42 and unhealthy dietary intake choices.43,44,45,46 In addition, household food insecurity has been associated with higher hemoglobin A1c values and hospitalization rates in children with T1D,47 which is notable because children with lower COI categories have more limited access to healthy food choices compared with those with higher COI categories.13,48,49 Less frequent use of diabetes technology, particularly continuous glucose monitoring devices, has also been associated with worse health outcomes in children with T1D, including higher rates of DKA50 and time spent in hyperglycemia.51 In a recent study of 1500 children, Lai et al52 showed that 54% of White children with T1D started continuous glucose monitoring in the outpatient setting compared with 31% of Black and 33% of Hispanic children. It is unclear why individuals from racial and ethnic minority groups less frequently start continuous glucose monitoring, but it is notable that this disparity persisted even after adjusting for insurance status,52 suggesting that lack of coverage may not be a driving factor. The COI includes many socioeconomic measures; however, there are other unmeasured factors that may also contribute to disparities. For instance, lack of reliable transportation and concern for missing work, which disproportionally affect individuals from racial and ethnic minority groups and those with lower socioeconomic status,53 may influence a family’s ability to attend clinic visits.54,55,56 Previous studies have shown that children with at least 2 missed clinic visits have significantly higher hemoglobin A1c levels compared with children with 1 or no missed visits,57,58 and missing endocrinology visits has been shown to be associated with higher odds of hospitalization for DKA.59 With these factors in mind, it is not surprising that children with lower COI levels, and particularly Black children, are at risk for DKA readmissions.
We also found that diabetes-related AKI was associated with race and ethnicity but not COI category. Although studies among adults with T1D have demonstrated racial differences in AKI60,61,62 and recent work among children has highlighted the frequency of AKI in children with DKA,19,20,21,22 no studies to our knowledge have explicitly studied the association between race and ethnicity and diabetes-related AKI risk in the pediatric population. Thus, our finding that race and ethnicity constituted a significant factor associated with AKI across all levels of COI is novel, and future research should focus on racial and ethnic disparities in AKI among children with DKA. In terms of CE risk, we found no association between COI category or race and ethnicity and risk of CE. To our knowledge, no studies have explicitly examined the association between race and ethnicity and CE risk in children with DKA, likely because CE is a rare event, and large sample sizes would be needed to detect any differences.
Limitations
Our study has several limitations. First, we could not account for readmissions to non-PHIS hospitals, which precluded our ability to evaluate patient-level data. Second, factors not included in the COI may contribute to readmissions. For instance, exposure to adverse childhood experiences has been shown to have an association with hospitalization rates.63 It is also possible that other patient or clinician factors contribute to readmissions. We were unable to account for the presence of coexisting mental health conditions, which have been shown to be associated with readmissions for DKA in children.7,64 Implicit bias by clinicians may further influence treatment decisions, including hospitalization.39,65 Third, we were unable to reliably account for use of diabetes technology, which has been associated with lower rates of DKA.50,66,67 For example, the prevalence of the ICD-10 code for insulin pump use (Z96.41) in PHIS was only 3% and varied significantly by hospital from less than 1% to 18%. Documentation of insulin pump use has also been an issue in other administrative data sets.67 Fourth, the COI uses Census tract data, which may not align with how individuals perceive their neighborhood boundaries. This factor is important to recognize as interventions aimed at addressing health disparities are designed and implemented. Fifth, the frequency of AKI in our cohort was found to be 4.9%, which is lower in comparison with recent reports.20,21,22 This lower rate is likely due to ascertainment of AKI by ICD-9 and ICD-10 coding because we did not have access to laboratory values, whereas other studies were able to use creatinine data to define AKI.
Conclusions
Our study revealed significant disparities in DKA health outcomes associated with neighborhood opportunity. Readmissions were higher in patients with low COI categories, adding strain to already disadvantaged populations. The results of our study may be useful both for clinicians and health care systems as they seek ways to reduce health disparities and advocate for patients and families as well as for policy makers and community leaders who seek to enact change on a population level.
eTable. Estimated Probability of Readmission for Each COI Domain by Race and Ethnicity
eFigure. Projective Margins for DKA Readmission at 365 Days by Overall Neighborhood Child Opportunity, Adjusted for Race and Ethnicity
References:
- 1.Tieder JS, McLeod L, Keren R, et al. ; Pediatric Research in Inpatient Settings Network . Variation in resource use and readmission for diabetic ketoacidosis in children’s hospitals. Pediatrics. 2013;132(2):229-236. doi: 10.1542/peds.2013-0359 [DOI] [PubMed] [Google Scholar]
- 2.Everett EM, Copeland TP, Moin T, Wisk LE. National trends in pediatric admissions for diabetic ketoacidosis, 2006-2016. J Clin Endocrinol Metab. 2021;106(8):2343-2354. doi: 10.1210/clinem/dgab287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saydah S, Imperatore G, Cheng Y, Geiss LS, Albright A. Disparities in diabetes deaths among children and adolescents—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2017;66(19):502-505. doi: 10.15585/mmwr.mm6619a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keenan HT, Foster CM, Bratton SL. Social factors associated with prolonged hospitalization among diabetic children. Pediatrics. 2002;109(1):40-44. doi: 10.1542/peds.109.1.40 [DOI] [PubMed] [Google Scholar]
- 5.Jensen ET, Stafford JM, Saydah S, et al. Increase in prevalence of diabetic ketoacidosis at diagnosis among youth with type 1 diabetes: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2021;44(7):1573-1578. doi: 10.2337/dc20-0389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis KR, Clark C, Velarde MC. Socioeconomic factors associated with pediatric diabetic ketoacidosis admissions in Southern West Virginia. Clin Endocrinol (Oxf). 2014;81(2):218-221. doi: 10.1111/cen.12350 [DOI] [PubMed] [Google Scholar]
- 7.Malik FS, Hall M, Mangione-Smith R, et al. Patient characteristics associated with differences in admission frequency for diabetic ketoacidosis in United States children’s hospitals. J Pediatr. 2016;171:104-110. doi: 10.1016/j.jpeds.2015.12.015 [DOI] [PubMed] [Google Scholar]
- 8.Maniatis AK, Goehrig SH, Gao D, Rewers A, Walravens P, Klingensmith GJ. Increased incidence and severity of diabetic ketoacidosis among uninsured children with newly diagnosed type 1 diabetes mellitus. Pediatr Diabetes. 2005;6(2):79-83. doi: 10.1111/j.1399-543X.2005.00096.x [DOI] [PubMed] [Google Scholar]
- 9.Maxwell AR, Jones NY, Taylor S, et al. Socioeconomic and racial disparities in diabetic ketoacidosis admissions in youth with type 1 diabetes. J Hosp Med. Published online August 18, 2021. doi: 10.12788/jhm.3664 [DOI] [PubMed] [Google Scholar]
- 10.Rewers A, Klingensmith G, Davis C, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics. 2008;121(5):e1258-e1266. doi: 10.1542/peds.2007-1105 [DOI] [PubMed] [Google Scholar]
- 11.Usher-Smith JA, Thompson MJ, Sharp SJ, Walter FM. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ. 2011;343:d4092. doi: 10.1136/bmj.d4092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Everett E, Mathioudakis NN. Association of socioeconomic status and DKA readmission in adults with type 1 diabetes: analysis of the US National Readmission Database. BMJ Open Diabetes Res Care. 2019;7(1):e000621. doi: 10.1136/bmjdrc-2018-000621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acevedo-Garcia D, Noelke C, McArdle N, et al. Racial and ethnic inequities in children’s neighborhoods: evidence from the New Child Opportunity Index 2.0. Health Aff (Millwood). 2020;39(10):1693-1701. doi: 10.1377/hlthaff.2020.00735 [DOI] [PubMed] [Google Scholar]
- 14.Kersten EE, Adler NE, Gottlieb L, et al. Neighborhood child opportunity and individual-level pediatric acute care use and diagnoses. Pediatrics. 2018;141(5):e20172309. doi: 10.1542/peds.2017-2309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck AF, Huang B, Wheeler K, Lawson NR, Kahn RS, Riley CL. The Child Opportunity Index and disparities in pediatric asthma hospitalizations across one Ohio metropolitan area, 2011-2013. J Pediatr. 2017;190:200-206.e1. doi: 10.1016/j.jpeds.2017.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krager MK, Puls HT, Bettenhausen JL, et al. The Child Opportunity Index 2.0 and hospitalizations for ambulatory care sensitive conditions. Pediatrics. 2021;148(2):e2020032755. doi: 10.1542/peds.2020-032755 [DOI] [PubMed] [Google Scholar]
- 17.Edge JA, Hawkins MM, Winter DL, Dunger DB. The risk and outcome of cerebral oedema developing during diabetic ketoacidosis. Arch Dis Child. 2001;85(1):16-22. doi: 10.1136/adc.85.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noelke C, McArdle N, Baek M, et al. How we built it: the nuts and bolts of constructing the Child Opportunity Index 2.0. January 21, 2020. Accessed October 28th, 2021. https://www.diversitydatakids.org/research-library/research-brief/how-we-built-it
- 19.Huang JX, Casper TC, Pitts C, et al. Association of acute kidney injury during diabetic ketoacidosis with risk of microalbuminuria in children with type 1 diabetes. JAMA Pediatr. 2022;176(2):169-175. doi: 10.1001/jamapediatrics.2021.5038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang SK, Huang CY, Lin CH, et al. Acute kidney injury is a common complication in children and adolescents hospitalized for diabetic ketoacidosis. PLoS One. 2020;15(10):e0239160. doi: 10.1371/journal.pone.0239160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hursh BE, Ronsley R, Islam N, Mammen C, Panagiotopoulos C. Acute kidney injury in children with type 1 diabetes hospitalized for diabetic ketoacidosis. JAMA Pediatr. 2017;171(5):e170020. doi: 10.1001/jamapediatrics.2017.0020 [DOI] [PubMed] [Google Scholar]
- 22.Myers SR, Glaser NS, Trainor JL, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) DKA FLUID Study Group . Frequency and risk factors of acute kidney injury during diabetic ketoacidosis in children and association with neurocognitive outcomes. JAMA Netw Open. 2020;3(12):e2025481. doi: 10.1001/jamanetworkopen.2020.25481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edge JA, Jakes RW, Roy Y, et al. The UK case-control study of cerebral oedema complicating diabetic ketoacidosis in children. Diabetologia. 2006;49(9):2002-2009. doi: 10.1007/s00125-006-0363-8 [DOI] [PubMed] [Google Scholar]
- 24.Glaser N, Barnett P, McCaslin I, et al. ; Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics . Risk factors for cerebral edema in children with diabetic ketoacidosis. N Engl J Med. 2001;344(4):264-269. doi: 10.1056/NEJM200101253440404 [DOI] [PubMed] [Google Scholar]
- 25.Lawrence SE, Cummings EA, Gaboury I, Daneman D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J Pediatr. 2005;146(5):688-692. doi: 10.1016/j.jpeds.2004.12.041 [DOI] [PubMed] [Google Scholar]
- 26.Stata.com. Marginal means, predictive margins, and marginal effects. Accessed November 1, 2021. https://www.stata.com/manuals/rmargins.pdf
- 27.McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796-1803. doi: 10.1161/CIRCULATIONAHA.114.010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Auger KA, Harris JM, Gay JC, et al. Progress (?) toward reducing pediatric readmissions. J Hosp Med. 2019;14(10):618-621. doi: 10.12788/jhm.3210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toomey SL, Peltz A, Loren S, et al. Potentially preventable 30-day hospital readmissions at a children’s hospital. Pediatrics. 2016;138(2):e20154182. doi: 10.1542/peds.2015-4182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160(8):1074-1081. doi: 10.1001/archinte.160.8.1074 [DOI] [PubMed] [Google Scholar]
- 31.Fischer C, Lingsma HF, Marang-van de Mheen PJ, Kringos DS, Klazinga NS, Steyerberg EW. Is the readmission rate a valid quality indicator? a review of the evidence. PLoS One. 2014;9(11):e112282. doi: 10.1371/journal.pone.0112282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heslin KC, Owens PL, Simpson LA, Guevara JP, McCormick MC. Annual report on health care for children and youth in the United States: focus on 30-day unplanned inpatient readmissions, 2009 to 2014. Acad Pediatr. 2018;18(8):857-872. doi: 10.1016/j.acap.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 33.Kane JM, Hall M, Cecil C, et al. Resources and costs associated with repeated admissions to PICUs. Crit Care Explor. 2021;3(2):e0347. doi: 10.1097/CCE.0000000000000347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Markham JL, Hall M, Gay JC, Bettenhausen JL, Berry JG. Length of stay and cost of pediatric readmissions. Pediatrics. 2018;141(4):e20172934. doi: 10.1542/peds.2017-2934 [DOI] [PubMed] [Google Scholar]
- 35.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372-380. doi: 10.1001/jama.2012.188351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bucholz EM, Toomey SL, Schuster MA. Trends in pediatric hospitalizations and readmissions: 2010-2016. Pediatrics. 2019;143(2):e20181958. doi: 10.1542/peds.2018-1958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682-690. doi: 10.1001/jama.2011.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parikh K, Berry J, Hall M, et al. Racial and ethnic differences in pediatric readmissions for common chronic conditions. J Pediatr. 2017;186:158-164.e1. doi: 10.1016/j.jpeds.2017.03.046 [DOI] [PubMed] [Google Scholar]
- 39.FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19. doi: 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trent M, Dooley DG, Dougé J; Section on Adolescent Health; Council on Community Pediatrics; Committee on Adolescence . The impact of racism on child and adolescent health. Pediatrics. 2019;144(2):e20191765. doi: 10.1542/peds.2019-1765 [DOI] [PubMed] [Google Scholar]
- 41.Everett E, Mathioudakis N. Association of area deprivation and diabetic ketoacidosis readmissions: comparative risk analysis of adults vs children with type 1 diabetes. J Clin Endocrinol Metab. 2019;104(8):3473-3480. doi: 10.1210/jc.2018-02232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sadauskaite-Kuehne V, Samuelsson U, Jasinskiene E, et al. ; DEBS Study Group . Severity at onset of childhood type 1 diabetes in countries with high and low incidence of the condition. Diabetes Res Clin Pract. 2002;55(3):247-254. doi: 10.1016/S0168-8227(01)00328-X [DOI] [PubMed] [Google Scholar]
- 43.Ahola AJ, Harjutsalo V, Thomas MC, Forsblom C, Groop PH. Dietary intake and hospitalisation due to diabetic ketoacidosis and hypoglycaemia in individuals with type 1 diabetes. Sci Rep. 2021;11(1):1638. doi: 10.1038/s41598-021-81180-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahola AJ, Harjutsalo V, Forsblom C, Saraheimo M, Groop PH; Finnish Diabetic Nephropathy Study . Associations of dietary macronutrient and fibre intake with glycaemia in individuals with type 1 diabetes. Diabet Med. 2019;36(11):1391-1398. doi: 10.1111/dme.13863 [DOI] [PubMed] [Google Scholar]
- 45.Buyken AE, Toeller M, Heitkamp G, et al. ; EURODIAB IDDM Complications Study Group . Relation of fibre intake to HbA1c and the prevalence of severe ketoacidosis and severe hypoglycaemia. Diabetologia. 1998;41(8):882-890. doi: 10.1007/s001250051003 [DOI] [PubMed] [Google Scholar]
- 46.Seckold R, Howley P, King BR, Bell K, Smith A, Smart CE. Dietary intake and eating patterns of young children with type 1 diabetes achieving glycemic targets. BMJ Open Diabetes Res Care. 2019;7(1):e000663. doi: 10.1136/bmjdrc-2019-000663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marjerrison S, Cummings EA, Glanville NT, Kirk SF, Ledwell M. Prevalance and associations of food insecurity in children with diabetes mellitus. J Pediatr. 2011;158(4):607-611. doi: 10.1016/j.jpeds.2010.10.003 [DOI] [PubMed] [Google Scholar]
- 48.Acevedo-Garcia D, McArdle N, Hardy EF, et al. The Child Opportunity Index: improving collaboration between community development and public health. Health Aff (Millwood). 2014;33(11):1948-1957. doi: 10.1377/hlthaff.2014.0679 [DOI] [PubMed] [Google Scholar]
- 49.Jutte DP, Badruzzaman RA, Thomas-Squance R. Neighborhood poverty and child health: investing in communities to improve childhood opportunity and well-being. Acad Pediatr. 2021;21(8S):S184-S193. doi: 10.1016/j.acap.2021.04.027 [DOI] [PubMed] [Google Scholar]
- 50.Tauschmann M, Hermann JM, Freiberg C, et al. ; DPV Initiative . Reduction in diabetic ketoacidosis and severe hypoglycemia in pediatric type 1 diabetes during the first year of continuous glucose monitoring: a multicenter analysis of 3553 subjects from the DPV Registry. Diabetes Care. 2020;43(3):e40-e42. doi: 10.2337/dc19-1358 [DOI] [PubMed] [Google Scholar]
- 51.Laffel LM, Kanapka LG, Beck RW, et al. ; CGM Intervention in Teens and Young Adults with T1D (CITY) Study Group; CDE10 . Effect of continuous glucose monitoring on glycemic control in adolescents and young adults with type 1 diabetes: a randomized clinical trial. JAMA. 2020;323(23):2388-2396. doi: 10.1001/jama.2020.6940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lai CW, Lipman TH, Willi SM, Hawkes CP. Racial and ethnic disparities in rates of continuous glucose monitor initiation and continued use in children with type 1 diabetes. Diabetes Care. 2021;44(1):255-257. doi: 10.2337/dc20-1663 [DOI] [PubMed] [Google Scholar]
- 53.Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res. 2007;7:40. doi: 10.1186/1472-6963-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119-1125. doi: 10.1001/archpedi.152.11.1119 [DOI] [PubMed] [Google Scholar]
- 55.Samuels RC, Ward VL, Melvin P, et al. Missed appointments: factors contributing to high no-show rates in an urban pediatrics primary care clinic. Clin Pediatr (Phila). 2015;54(10):976-982. doi: 10.1177/0009922815570613 [DOI] [PubMed] [Google Scholar]
- 56.Yang S, Zarr RL, Kass-Hout TA, Kourosh A, Kelly NR. Transportation barriers to accessing health care for urban children. J Health Care Poor Underserved. 2006;17(4):928-943. doi: 10.1353/hpu.2006.0137 [DOI] [PubMed] [Google Scholar]
- 57.Markowitz JT, Volkening LK, Laffel LM. Care utilization in a pediatric diabetes clinic: cancellations, parental attendance, and mental health appointments. J Pediatr. 2014;164(6):1384-1389. doi: 10.1016/j.jpeds.2014.01.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaufman FR, Halvorson M, Carpenter S. Association between diabetes control and visits to a multidisciplinary pediatric diabetes clinic. Pediatrics. 1999;103(5, pt 1):948-951. doi: 10.1542/peds.103.5.948 [DOI] [PubMed] [Google Scholar]
- 59.Crossen SS, Wilson DM, Saynina O, Sanders LM. Outpatient care preceding hospitalization for diabetic ketoacidosis. Pediatrics. 2016;137(6):e20153497. doi: 10.1542/peds.2015-3497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ginde AA, Pelletier AJ, Camargo CA Jr. National study of US emergency department visits with diabetic ketoacidosis, 1993-2003. Diabetes Care. 2006;29(9):2117-2119. doi: 10.2337/dc06-0627 [DOI] [PubMed] [Google Scholar]
- 61.Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421-1426. doi: 10.2337/diacare.26.5.1421 [DOI] [PubMed] [Google Scholar]
- 62.Mathioudakis NN, Giles M, Yeh HC, Haywood C Jr, Greer RC, Golden SH. Racial differences in acute kidney injury of hospitalized adults with diabetes. J Diabetes Complications. 2016;30(6):1129-1136. doi: 10.1016/j.jdiacomp.2016.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hargreaves MK, Mouton CP, Liu J, Zhou YE, Blot WJ. Adverse childhood experiences and health care utilization in a low-income population. J Health Care Poor Underserved. 2019;30(2):749-767. doi: 10.1353/hpu.2019.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sildorf SM, Breinegaard N, Lindkvist EB, et al. Poor metabolic control in children and adolescents with type 1 diabetes and psychiatric comorbidity. Diabetes Care. 2018;41(11):2289-2296. doi: 10.2337/dc18-0609 [DOI] [PubMed] [Google Scholar]
- 65.Raphael JL, Oyeku SO. Implicit bias in pediatrics: an emerging focus in health equity research. Pediatrics. 2020;145(5):e20200512. doi: 10.1542/peds.2020-0512 [DOI] [PubMed] [Google Scholar]
- 66.Karges B, Schwandt A, Heidtmann B, et al. Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis, and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA. 2017;318(14):1358-1366. doi: 10.1001/jama.2017.13994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Everett EM, Copeland TP, Moin T, Wisk LE. Insulin pump related inpatient admissions in a national sample of youth with type 1 diabetes. J Clin Endocrinol Metab. Published online February 23, 2022. doi: 10.1210/clinem/dgac047 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Estimated Probability of Readmission for Each COI Domain by Race and Ethnicity
eFigure. Projective Margins for DKA Readmission at 365 Days by Overall Neighborhood Child Opportunity, Adjusted for Race and Ethnicity