Abstract
Children in foster care are at high risk for developmental delay. In this retrospective cohort study of young children presenting to a foster care clinic, 77% were not receiving developmental services and 75% failed developmental screening. Of those potentially eligible, 60% were not referred for developmental services.
Nationally, there are approximately 440 000 children in child protective custody (ie, foster care), of which 24% (~104 000) are under the age of 3 years.1 Young children in foster care usually have 2 placement options while in protective custody: (1) nonrelative foster caregivers—individuals who are recruited, trained, and credentialed to provide full-time care to the child in their home and receive a monetary stipend for this role or (2) kinship caregivers—relatives or family friends who agree to provide full-time care to the child in their home, with oversight from the child protection agency. Kinship caregivers tend to be older and are more likely to experience poverty.2 Child protection agencies give preference to kinship caregivers when placing a child in out-of-home care.3 As a result, the number of children placed with kinship caregivers has increased over the past decade,1 and the number of children placed with nonrelative foster caregivers has remained stable.
Most children enter foster care as a result of maltreatment, including neglect and abuse.4,5 This history of maltreatment, along with other risks, places them at higher risk for developmental delay compared with nonabused children,6 with prevalence of developmental delay as high as 45%−62%7–11 vs 13%−15%, respectively.12–15 Early identification of developmental delay is important because of the opportunity for early developmental interventions, such as Early Intervention and private therapy including speech therapy (ST), physical therapy (PT), and occupational therapy (OT) to yield developmental catch-up. The importance of identifying developmental delay among children in foster care is reflected in both federal legislation (Child Abuse Prevention and Treatment Act) and in American Academy of Pediatrics guidelines.16 Despite the presence of Child Abuse Prevention and Treatment Act and American Academy of Pediatrics guidelines, many children in foster care with developmental delay are not adequately identified8,17,18 nor do they successfully access early intervention or other developmental services.7,19 This study sought to better understand developmental screening, service referral, and service completion rates for young children in foster care to identify opportunities for intervention to improve developmental outcomes in this population.
Methods
We performed a retrospective cohort study from 2012 to 2017, with approval from the Institutional Review Board at Cincinnati Children’s Hospital Medical Center. A waiver of consent was granted. Subjects were included if they were less than 36 months old, in the custody of the local county child welfare system, seen at the Cincinnati Children’s Hospital Medical Center CHECK Foster Care Center, and received developmental screening as part of that visit.
Setting of Screening
The Cincinnati Children’s Hospital Medical Center CHECK Foster Care Center (CHECK Center) is an evaluation model clinic,20 designed in collaboration with the local county child welfare agency to consult on every child entering foster care in a single county in Ohio before referring back to primary care. Children are seen within 5 business days of entering foster care and again in 1–2 months for follow-up if still in care. The process repeats with every placement change. Children receive a developmental screening as part of the follow-up visit, 1–2 months after the placement visit, to allow the child a period of transition and the caregiver a period for observation.
Measures
Developmental screening at the CHECK Center is completed with the Ages and Stages Questionnaire (ASQ). Seventeen age-appropriate paper questionnaires are available, ranging from 0 to 36 months. The caregiver responds “yes,” “sometimes,” or “not yet” to 30 questions capturing 5 domains of development, including communication, gross motor, fine motor, problem solving, and adaptive behavior. These responses are then converted to scores of 10, 5, and 0 respectively. The total scores for each domain are compared with established screening cut-offs. If a score falls below this set cut-off, the child is considered to be at risk for developmental delay and warrants further assessment or intervention. For the purposes of this study, ASQ results were divided into “fail,” when the child was borderline or failed at least 1 domain, and “pass,” when the child passed all domains. The ASQ takes 10–15 minutes to complete and 5 minutes to score. Concurrent validity ranges from 76% to 91% in general pediatric population.21 There were children who received more than 1 ASQ over the study period due to multiple CHECK Center follow-up visits with different placement changes. For these children, we included the first administered ASQ.
Data Collection
The hospital has an enterprise electronic health record installed in 2009. All order entries and referrals are electronic. We extracted demographic data, including age, sex, race, and placement type (nonrelative foster family or kinship foster family), ASQ results, and data on enrollment in developmental services at baseline (ie, the time of ASQ screening), referrals for developmental services (including early intervention referrals and private PT, OT, and ST referrals), and completed referrals, defined as receiving a full evaluation from the referral service.
Results
Developmental Screening Results
From 2012 to 2017, there were 235 children (42% female, 25% White, 42% with kinship caregivers, mean age = 1.57, SD = 0.79) seen at the CHECK Center who were eligible for inclusion, indicating they were <36 months of age and completed developmental screening with an ASQ (Figure). Thirty-four children received more than 1 ASQ (range 2–3) over the study period because of rescreening for changes in placement and only had their first ASQ included in the data set.
Figure.
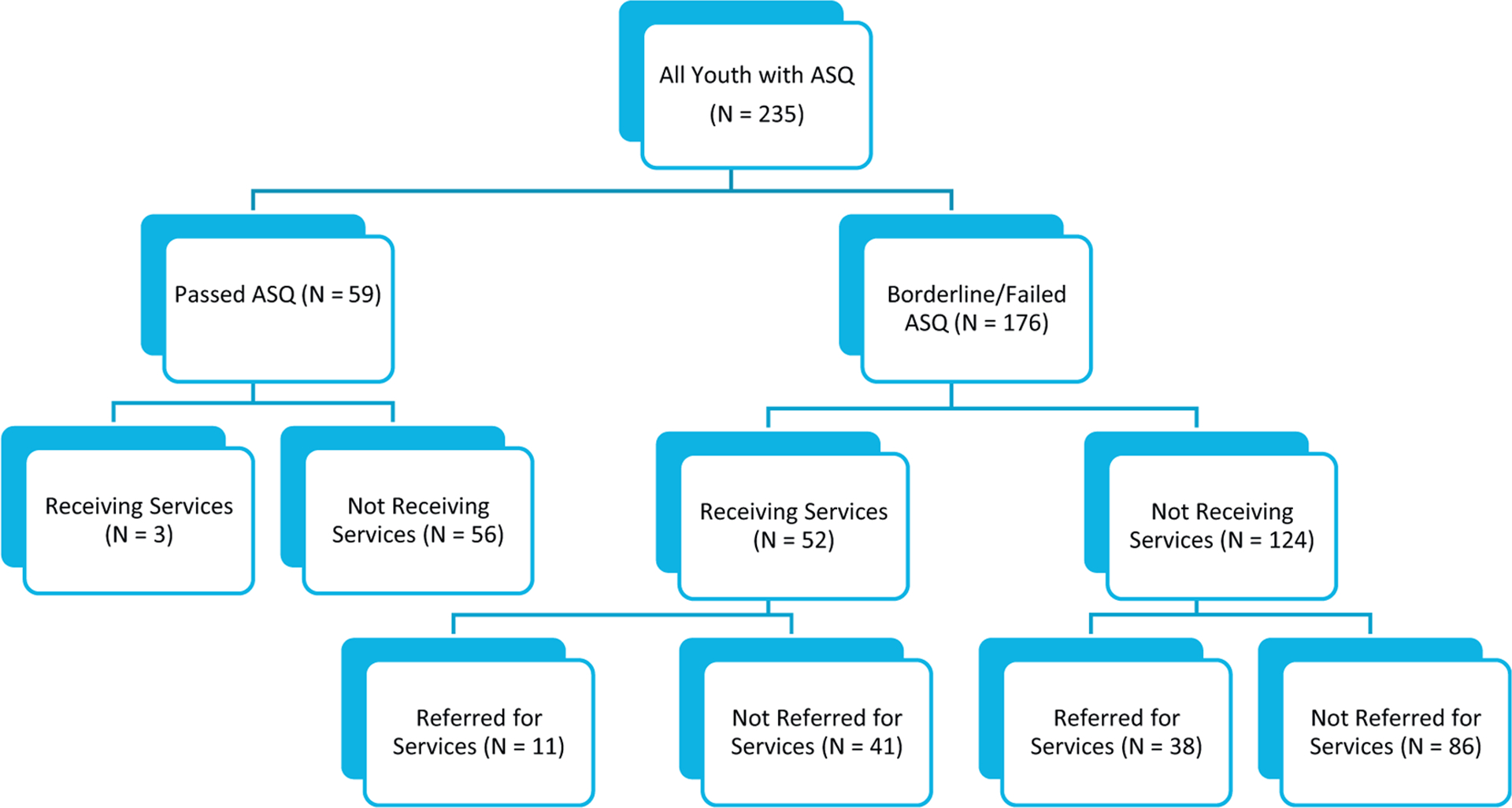
Breakdown of ASQ results and referrals for young children presenting to foster care clinic.
Of this group of 235 children, 59 (25%) passed their ASQ in all domains. The remaining 176 children (75%) had at least 1 borderline or failing score. The most commonly passed domain was gross motor, which was passed by 152 children (65%). Among those who failed the screening, the most commonly failed domain was problem-solving, which was borderline or failed by 129 children (55%). Among those who failed the screening, 39 (22%) failed 1 domain, 35 (20%) failed 2 domains, and 102 (58%) failed 3 or more domains (Table I; available at www.jpeds.com). In multivariate logistic regression model 1 predicting whether or not a child failed any ASQ domain, children (n = 235) were more likely to fail an ASQ when they were male (Table II). There were no other significant demographic differences. Children in kinship placements and nonrelative placements were equally likely to fail the ASQ.
Table I.
Descriptive statistics for children who failed the ASQ, by number of domains and which domains were failed
| Variables | Passed all domains (n = 59) | Failed any domain (n = 176) | Failed more than 1 domain (n = 137) | Failed communication (n = 97) | Failed fine motor (n = 113) | Failed gross motor (n = 81) | Failed personal-social (n = 114) | Failed problem-solving (n = 129) |
|---|---|---|---|---|---|---|---|---|
| Mean age (SD) | 1.52 (0.81) | 1.59 (0.78) | 1.62 (0.82) | 1.66 (0.76) | 1.59 (0.83) | 1.46 (0.77) | 1.56 (0.81) | 1.55 (0.79) |
| % Female | 32 (54%) | 67 (38%) | 54 (39%) | 39 (40%) | 45 (40%) | 32 (40%) | 41 (36%) | 51 (40%) |
| % White | 15 (25%) | 44 (25%) | 34 (25%) | 24 (25%) | 25 (22%) | 18 (22%) | 27 (24%) | 29 (22%) |
| % Kinship placement | 31 (53%) | 67 (38%) | 51 (37%) | 33 (34%) | 38 (34%) | 24 (30%) | 42 (37%) | 50 (39%) |
Table II.
Results of multiple regression models examining ASQ screening results, referrals for developmental services, and completion of referrals
| Variables | ASQ failure (model 1) | Enrollment in any developmental services at baseline (model 2) | Number of failed domains | Referred to any developmental services (model 3) | Referred for EI (model 4) | Completed any developmental service referral (model 5) | Completed EI referral (model 6) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI | OR | CI | B | SE | OR | CI | OR | CI | OR | CI | OR | CI | |
| Intercept | – | – | – | – | 2.13 | 0.35 | – | – | – | – | – | – | – | – |
| Age | 1.03 | 0.69–1.54 | 1.41 | 0.95–2.09 | −0.11 | 0.14 | 1.17 | 0.76–1.79 | 0.01* | 0.00–0.61 | 1.41 | 0.61–3.27 | 0.75 | 0.28–2.03 |
| Race | 0.99 | 0.69–1.41 | 0.91 | 0.63–1.31 | −0.13 | 0.13 | 0.95 | 0.64–1.40 | 0.33 | 0.07–1.65 | 1.04 | 0.50–2.18 | 0.86 | 0.37–1.96 |
| Sex | 0.53* | 0.29–0.99 | 0.83 | 0.44–1.57 | −0.22 | 0.22 | 1.01 | 0.51–1.99 | 0.15 | 0.01–3.61 | 1.36 | 0.35–5.27 | 0.84 | 0.17–4.05 |
| Placement type | 1.45 | 0.78–2.71 | 2.55** | 1.30–5.04 | 0.35 | 0.23 | 0.87 | 0.44–1.73 | 7.70 | 0.31–194.05 | 2.97 | 0.84–10.53 | 4.30 | 1.09–16.88 |
| Service enrollment | 7.19** | 2.12–24.30 | – | – | 1.74** | 0.27 | 0.40* | 0.17–0.92 | 0.95 | 0.06–16.40 | – | – | – | – |
| Failed ASQ | – | – | – | – | – | – | 4.63 | 0.90–23.96 | – | – | – | – | – | – |
| Number of failed domain | – | – | – | – | – | – | 1.42** | 1.11–1.82 | 0.21* | 0.04–0.97 | 0.97 | 0.58–1.57 | 0.84 | 0.49–1.43 |
B, regression coefficient; CI, ±95% confidence interval; EI, Early Intervention; OR, odds ratio.
Age was entered into all regression models as a continuous variable. Race was coded as White (3), Black (1), or Other (2). Sex was coded as female (1) or male (0). Placement type was coded as kinship (0) or nonrelative caregiver (1). Enrollment in any developmental services at baseline refers whether the child was already receiving EI or private therapy (OT, PT, or ST) at the time the ASQ was completed (1) or not (0). Failed ASQ refers to whether the child failed any domains (1) or passed all domains (0). Number of failed domains refers to a count of ASQ domains failed. Referral to any developmental services refers to whether a child received a referral to either EI or private therapy (1) or no referral (0). Referral to EI specifically compares receiving a EI referral (2) vs a private therapy referral (1). Completed developmental referral refers to whether the child engaged with either EI or private therapy (1) or failed to engage in services (0). Completed EI referral refers to whether the child engaged with EI specifically (1) or not (0). Number of failed domains was examined as an outcome using multiple linear regression; all other outcomes were evaluated in logistic regression models.
P < .05.
P < .01.
Established Developmental Services
The majority (77%) of the 235 children in this study were not receiving developmental services at the time of their CHECK Center visit and developmental screening. Among children who passed the ASQ (n = 59), only 3 (5%) were already receiving developmental services at the time of screening. Among children who failed the ASQ (n = 176), 52 (30%) were already receiving developmental services at the time of screening. In multivariate logistic regression model 2 predicting enrollment into developmental services at baseline, children (n = 235) receiving developmental services at the time of screening were more likely to be in nonrelative placement (Table II).
Referrals
Among the 124 children who failed the ASQ and were not receiving services, 38 (30.6%) were referred to developmental services, including early intervention or private therapies (PT, OT, and/or ST). In multivariate logistic regression model 3 predicting referral to services, children (n = 176) with multiple failed domains were more likely to get a referral to developmental services and children already enrolled in services were less likely to get a referral (Table II). Children referred to developmental services were otherwise not demographically different than children who were not referred to developmental services, and there was no variation by placement type. Younger children and children failing fewer ASQ domains were more likely to be referred to Early Intervention when compared with private therapy (OT, PT, ST), regardless of placement type (model 4, Table II).
Referral Completion
Among children referred to services who failed at least 1 domain on the ASQ (n = 49), 22% were already receiving developmental services. Thirty-two completed a referral, including 10 who were already enrolled in services. Seventeen did not complete a referral. In multivariate logistic regression model 5 predicting whether or not a child completed a referral for developmental services, children’s (n = 49) demographic characteristics and placement type were not associated with the completed referrals (Table II). Of those completing a referral, 7 were seen for evaluation for private therapy and 26 completed a referral to Early Intervention; 1 completed a referral to both service types. In multivariate logistic regression model 6 predicting whether or not a child completed an Early Intervention referral, licensed nonrelative caregivers were 4.3 times more likely to complete a referral to Early Intervention than kinship caregivers; no other demographic characteristics were significant. The most common reason for not completing a referral was “unknown” regardless of placement type. Other common reasons for not completing the Early Intervention referral for kinship families included caregiver declined (24%) and unable to contact family (18%). Other common reasons for not completing the Early Intervention referral for nonrelative foster families included unable to contact family (15%) and caregiver declined (7%). Finally, among those receiving an Early Intervention evaluation, 12 (46%) met criteria for enrollment and were engaged in Early Intervention services, and 14 were determined ineligible for Early Intervention services.
Discussion
In this study, we identified that a majority of young children in foster care failed development screening and were not referred for further developmental evaluation, regardless of placement type. This is particularly concerning as children in foster care are identified as a particularly vulnerable group for developmental delay and academic challenges.7,11 Seventy-five percent of foster children in this study had a borderline or failing ASQ. However, only 51% of this group were either already in services or referred to services. This means that almost one-half of the children had concerns on the ASQ did not receive further evaluation to determine if developmental delays were present. The most commonly failed domain in our population was problem-solving. Previous report of ASQ utilization in a general pediatrics clinic found communication as the most commonly failed domain. Further study is warranted to evaluate this as a meaningful difference for this population.22
Among the characteristics we examined, there were no trends associated with whether a child was referred to developmental services, and importantly, children in kinship placements and nonrelative foster placements were equally likely to need a referral and be referred for services. Our study did not collect how often developmental services were discussed and declined, or it did not allow us to delve into the qualitative aspects of the referral process. We also did not examine medical decision-making on referrals to private therapy vs Early Intervention.
We did find, however, that despite equal referral rates and rates of referral completion overall, foster caregivers were 4.3 times more likely to complete referrals to Early Intervention than kinship caregivers. Further, percentage of declined services was higher in kinship caregivers compared with nonrelative foster families. Nonrelative foster families had higher percentages of referrals closed because of being unable to contact the family, and these may represent passively declined services. More research is needed to inform implementation of intervention services and how to engage nonrelative foster and kinship caregivers in services.
In previous studies of kinship caregivers compared with nonrelative foster caregivers, kinship caregivers were more likely to be single, older, unemployed, and to have more health problems, in addition to being significantly more likely to have incomes below 100% of the federal poverty line.2,23,24 Yet, they generally received fewer services and less help from their local child welfare agency, in addition to little or no training.23–25 Further, past research has found that kinship caregivers have a more positive attitude toward the child’s behaviors and are more inclined to deny behavior problems.23,24 If a similar phenomenon is happening with their impression of the child’s developmental needs, they may be less inclined to follow through on a referral when made by the health care provider. Given the different trend in referral completion rates for private therapy referrals, which occurred less frequently and was high in both kinship caregivers and nonrelative licensed caregivers, it is also possible that some kinship families are uncomfortable with the home-based delivery method for Early Intervention and do not want service providers coming to their homes. Nonrelative foster caregivers may be more used to professionals coming to their homes because of their experiences with the nonrelative foster care system, which sets home visitation as a norm. It could also be that children referred to private therapies had higher developmental needs which were more concerning to the caregivers.
Our findings suggest that a different approach may be required to manage possible developmental delays with licensed and kinship caregivers. This may include partnering with the local child welfare and early intervention agencies to address barriers to getting evaluations completed and services in place. It may be that giving caregivers a choice between home-based therapies or nonhome-based therapies may increase referral completion rates. A lower threshold for referral to developmental services after a failed developmental screening may be needed. Watchful waiting may be an effective approach for children in traditional families, but placement changes and other challenges make children in foster care difficult to follow.
The strengths of this study include being able to utilize clinical data from a well-established consultative foster care clinic that has standard practices around use of developmental screeners. There are several limitations to this study. ASQs, especially completed by foster caregivers who are generally unfamiliar with children when they are first placed with them, may or may not accurately reflect likelihood of diagnosed developmental delay. Our data did not include when developmental service referrals were offered but declined or reasons a provider may have chosen watchful waiting for an individual child rather than referral or one referral type over another. Finally, this data set only included referrals from our hospital system. Although most caregivers seek referrals for these services through our foster care clinic, others may seek such referrals from private agencies in the area and not be reflected in our data. Finally, other systems may have automated referral processes in place and these results may not be generalizable to those settings.
Research in this area should focus on the qualitative aspects of why there may be hesitancy to refer to developmental services and why foster and kinship caregivers are not completing developmental evaluations despite identifying concerns on standardized screening and receiving referrals for developmental services, in particular for home-based Early Intervention services. The emerging role for telehealth will also need to be evaluated. This deeper understanding will facilitate development of concrete interventions to improve developmental outcomes in this high-risk population. More research is also needed on the efficacy of watchful waiting to follow development in young children in foster care.
Acknowledgments
S.B.’s time was supported through the National Institute of Drug Abuse (1K01DA041620). The authors declare no conflicts of interest.
We thank Vikash Patel, Jennifer Duma, and Nina Grau for their help with data collection and entry. We acknowledge Lorena Ferreira Corzo, MD for contributions in study design and data collection and Katherine Bowers, PhD, MPH, for efforts in early data analysis.
Glossary
- ASQ
Ages and Stages Questionnaire
- OT
Occupational therapy
- PT
Physical therapy
- ST
Speech therapy
References
- 1.U.S. Department of Health and Human Services AfCaF, Administration on Children, Youth and Families, Children’s Bureau. The AFCARS Report. Preliminary FY 2018 estimates as of August 22, 2019. 26th ed., 2018. p. 1–6. Washington. D.C: The Department of Health and Human Services (HHS), Administration for Children and Families (ACF), Children’s Bureau (CB). [Google Scholar]
- 2.Ehrle J, Geen R. Kin and non-kin foster care-findings from a national survey. Child Youth Serv Rev 2002;24:15–35. [Google Scholar]
- 3.Szilagyi M The pediatric role in the care of children in foster and kinship care. Pediatr Rev 2012;33:496–507. quiz 8. [DOI] [PubMed] [Google Scholar]
- 4.Takayama JI, Wolfe E, Coulter KP. Relationship between reason for placement and medical findings among children in foster care. Pediatrics 1998;101:201–7. [DOI] [PubMed] [Google Scholar]
- 5.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics 2000;106:909–18. [PubMed] [Google Scholar]
- 6.Osofsky JD. The impact of violence on children. The Future of Children (Center for the Future of Children, the David and Lucile Packard Foundation; ) 1999;9:33–49. [PubMed] [Google Scholar]
- 7.Stahmer AC, Leslie LK, Hurlburt M, Barth RP, Webb MB, Landsverk J, et al. Developmental and behavioral needs and service use for young children in child welfare. Pediatrics 2005;116:891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leslie LK, Gordon JN, Ganger W, Gist K. Developmental delay in young children in child welfare by initial placement type. Infant Mental Health J 2002;23:496–516. [Google Scholar]
- 9.Hochstadt NJ, Jaudes PK, Zimo DA, Schachter J. The medical and psychosocial needs of children entering foster care. Child Abuse Negl 1987;11:53–62. [DOI] [PubMed] [Google Scholar]
- 10.Ringeisen H, Casanueva C, Urato M, Cross T. Special health care needs among children in the child welfare system. Pediatrics 2008;122:e232–41. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg SA, Smith EG. Rates of Part C eligibility for young children investigated by child welfare. Top Early Child Spec 2008;28:68–74. [Google Scholar]
- 12.Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics 2011;127:1034–42. [DOI] [PubMed] [Google Scholar]
- 13.Rosenberg SA, Zhang D, Robinson CC. Prevalence of developmental delays and participation in early intervention services for young children. Pediatrics 2008;121:e1503–9. [DOI] [PubMed] [Google Scholar]
- 14.King TM, Tandon SD, Macias MM, Healy JA, Duncan PM, Swigonski NL, et al. Implementing developmental screening and referrals: lessons learned from a national project. Pediatrics 2010;125:350–60. [DOI] [PubMed] [Google Scholar]
- 15.Simpson GA, Colpe L, Greenspan S. Measuring functional developmental delay in infants and young children: prevalence rates from the NHIS-D. Paediatr Perinat Epidemiol 2003;17:68–80. [DOI] [PubMed] [Google Scholar]
- 16.Task Force on Health Care for Children in Foster Care. Fostering Health: Health Care for Children and Adolescents in Foster Care, Healthy Foster Care America (HFCA) is an initiative of the American Academy of Pediatrics (AAP): Itasca, IL. In: Pediatrics AAo. 2 ed, 2005. [Google Scholar]
- 17.Jee SH, Szilagyi M, Ovenshire C, Norton A, Conn AM, Blumkin A, et al. Improved detection of developmental delays among young children in foster care. Pediatrics 2010;125:282–9. [DOI] [PubMed] [Google Scholar]
- 18.Leslie LK, Hurlburt MS, Landsverk J, Rolls JA, Wood PA, Kelleher KJ. Comprehensive assessments for children entering foster care: a national perspective. Pediatrics 2003;112:134–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmer MH, Panko LM. Developmental status and service use among children in the child welfare system: a national survey. Arch Pediatr Adolesc Med 2006;160:183–8. [DOI] [PubMed] [Google Scholar]
- 20.AAP. In: Pediatrics AAo. 2016. https://www.aap.org/_layouts/15/aap/forms/pages/HFCAModelDefinitions.htm. Accessed April 2, 2021
- 21.Squires J, Bricker D, Potter L. Revision of a parent-completed development screening tool: Ages and Stages Questionnaires. J Pediatr Psychol 1997;22:313–28. [DOI] [PubMed] [Google Scholar]
- 22.Rydz D, Srour M, Oskoui M, Marget N, Shiller M, Birnbaum R, et al. Screening for developmental delay in the setting of a community pediatric clinic: a prospective assessment of parent-report questionnaires. Pediatrics 2006;118:e1178–86. [DOI] [PubMed] [Google Scholar]
- 23.Berrick JD, Barth RP, Needell B. A comparison of kinship foster homes and foster family homes: implications for kinship foster-care as family preservation. Child Youth Serv Rev 1994;16:33–63. [Google Scholar]
- 24.Gebel TJ. Kinship care and nonrelative family foster care: a comparison of caregiver attributes and attitudes. Child Welfare 1996;75:5–18. [Google Scholar]
- 25.Leslie LK, Landsverk J, Ezzet-Lofstrom R, Tschann JM, Slymen DJ, Garland AF. Children in foster care: Factors influencing outpatient mental health service use. Child Abuse Neglect 2000;24:465–76. [DOI] [PubMed] [Google Scholar]


