Abstract
Objective:
Irritability is a multifaceted construct in pediatric psychopathology. It has been conceptualized as having a phasic dimension and a tonic dimension. Disruptive mood dysregulation disorder is defined by the presence of both dimensions. Severe irritability, or disruptive mood dysregulation disorder, is highly comorbid with attention-deficit/hyperactivity disorder (ADHD). However, it is unknown whether the presence of ADHD modulates the expression of phasic and tonic irritability.
Method:
A data-driven, latent variable approach was used to examine irritability and ADHD symptoms in a transdiagnostic pediatric sample (N = 489) with primary disruptive mood dysregulation disorder, ADHD, subclinical irritability symptoms, or no diagnosis. Using latent profile analyses, we identified 4 classes: high levels of both irritability and ADHD symptoms, high levels of irritability and moderate levels of ADHD symptoms, moderate levels of irritability and high levels of ADHD symptoms, and low levels of both irritability and ADHD symptoms. Confirmatory factor analysis operationalized phasic irritability and tonic irritability.
Results:
As expected, the 2 latent classes characterized by high overall irritability exhibited the highest levels of both phasic and tonic irritability. However, between these 2 high irritability classes, highly comorbid ADHD symptoms were associated with significantly greater phasic irritability than were moderately comorbid ADHD symptoms. In contrast, the 2 high irritability groups did not differ on levels of tonic irritability.
Conclusion:
These findings suggest that phasic, but not tonic, irritability has a significant association with ADHD symptoms and that phasic and tonic might be distinct, though highly related, irritability dimensions. Future research should investigate potential mechanisms underlying this differential association.
Keywords: ADHD, aggression, DMDD, irritability, latent variable analysis
Irritability, defined as an increased proneness to anger relative to peers, is a common symptom in pediatric psychopathology.1 While irritability cuts across many diagnoses in youths, disruptive mood dysregulation disorder (DMDD)2 classifies youths with the most severe, chronic, and impairing irritability.3 Specifically, DMDD conceptualizes irritability as including both a phasic dimension, ie, severe and developmentally inappropriate outbursts, and a tonic dimension, ie, persistent irritable mood between outbursts. Clinical samples of youths with DMDD exhibit high rates of co-occurring attention-deficit/hyperactivity disorder (ADHD).4,5 Conversely, irritability is a common symptom in youths with ADHD.6–8 However, it is unknown whether or how the presence of ADHD modulates the expression of irritability, particularly phasic vs tonic irritability, which has implications for treatment. To address this question, the current study adopted a data-driven, latent variable approach to examine patterns of phasic and tonic irritability and ADHD symptoms in a transdiagnostic sample of youths.
Children with ADHD often present with significant emotional lability,9,10 including chronic irritability.1,5 Previous research in community samples indicates that 4.3%–23.5% of youths with ADHD meet diagnostic criteria for DMDD,3,11 with estimates as high as 35.8% in children with a diagnosis with ADHD combined type.8 Indeed, in patients with ADHD, increased anger and irritability are associated with greater severity of core ADHD symptoms12 and increased risk for negative outcomes, including peer rejection, substance abuse, and depression.8,13,14 In fact, based on physiological data, ADHD with severe co-occurring irritability, as seen in DMDD, has been proposed to represent a distinct subtype of ADHD.7
The conceptualization of irritability as a construct in general as well as its presentation in DMDD specifically includes both phasic and tonic dimensions. Phasic irritability involves a rapid onset of angry affect and associated behaviors, such as verbal and sometimes physical aggression (eg, physically pushing, shoving, slapping, or kicking another person), typically in response to identifiable environmental triggers, such as frustration. Tonic irritability captures longer-lasting but less intense grouchiness, crankiness, and annoyance in between outbursts.1,15 Phasic and tonic symptoms of irritability are the 2 core dimensions of observable behavior underlying the clinical definition of DMDD and thus represent the clearest target for translational research and development of precision-based treatments of DMDD.16
Although the conceptualization of irritability and DMDD include both phasic and tonic dimensions, few studies have parsed these dimensions, and it is unclear whether they have differential clinical, behavioral, or biological correlates.17–22 Despite the high comorbidity of ADHD and irritability, no study has examined how ADHD symptoms may relate differentially to phasic and tonic irritability. In treatment studies of ADHD, following administration of stimulant medication, a reduction in irritability symptoms broadly has been observed.20,23–25 However, this literature did not assess changes in phasic and tonic symptoms specifically. Indirect evidence for differential associations comes from a recent treatment study, in which the optimization of stimulant medication before the initiation of selective serotonin reuptake inhibitor vs placebo in the treatment of DMDD significantly reduced ADHD symptoms and temper outbursts, but not irritable mood.26 Thus, ADHD symptoms may be differentially associated with phasic vs tonic irritability, perhaps reflecting greater shared mechanisms (ie, impaired top-down prefrontal control of subcortical regions).27
The current study used latent variable methods to investigate ADHD symptoms as a potential modulator of phasic vs tonic irritability in a large, well-characterized transdiagnostic sample of youths. First, we used latent profile analysis (LPA) to derive classes of youths characterized by distinct patterns of irritability and ADHD symptoms. This approach involved a data-driven evaluation of patterns of irritability and ADHD symptoms. In contrast to median-split approaches, LPA statistically evaluates whether and what distinct patterns of irritability and ADHD symptoms emerge in the sample. Next, we used confirmatory factor analysis (CFA) to quantify separate indices of phasic irritability and tonic irritability. With respect to phasic irritability, we included indices of both temper outbursts and aggression, given that both represent behavioral manifestations of underlying trait anger.28 We then examined whether the LPA-derived classes differed in their patterns of phasic and tonic irritability.
Given indirect evidence for the reduction of phasic irritability symptoms following stimulant medication administration,24–26 we predicted that, in the context of high irritability, high vs low levels of ADHD symptoms would be related to greater phasic, but not tonic, irritability. Finally, given the common co-occurrence of anxiety and oppositionality28 with irritability, we performed additional analyses controlling for anxiety and oppositionality to test for any confounding effects of these common comorbidities. Together, these analyses provide the first direct examination of ADHD symptoms in relation to phasic and tonic irritability.
METHOD
Participants
The sample consisted of 489 youths ages 7–18 years (mean [SD] age = 12.03 [2.41] years) who were recruited from the community to participate in research at the National Institute of Mental Health (NIMH). The sample was predominantly White (63.60%) and upper-middle class (income >90,000; 70.69%). Full demographic characteristics are presented in Table 1.
TABLE 1.
Sample Characteristics
| Variable | Value | |
|---|---|---|
| Mean | (SD) | |
| Age, years | 12.03 | (2.41) |
| IQ | 110.46 | (12.66) |
| n | (%) | |
| Sex, malea | 268 | (54.81) |
| Race | ||
| White | 311 | (63.60) |
| American Indian or Alaskan Native | 3 | (0.61) |
| Asian | 23 | (4.70) |
| Black or African American | 84 | (17.18) |
| Multiple races | 45 | (9.20) |
| Other | 1 | (0.20) |
| Unknown | 22 | (4.50) |
| Ethnicity | ||
| Latino or Hispanic | 52 | (10.63) |
| Not Latino or Hispanic | 423 | (86.50) |
| Unknown | 14 | (2.86) |
| Socioeconomic status | ||
| Highest education level | ||
| Graduate professional degree (master’s or above) | 195 | (39.88) |
| 4-year college graduate | 65 | (13.29) |
| Partial college (≥1 year) | 41 | (8.38) |
| High school graduate | 10 | (2.04) |
| Partial high school (grade 10 or 11) | 7 | (1.43) |
| Junior high school (grades 7–9) | 4 | (0.82) |
| <7 years of school | 8 | (1.64) |
| Unknown | 159 | (32.52) |
| Income | ||
| >$180,000 | 95 | (28.70) |
| $90,000–$179,999 | 139 | (41.99) |
| $60,000–$89,999 | 35 | (10.57) |
| $40,000–$59,999 | 21 | (6.34) |
| $25,000–$39,999 | 13 | (3.93) |
| $15,000–$24,999 | 8 | (2.42) |
| $10,000–$14,999 | 2 | (0.60) |
| $5,000–$9,999 | 0 | (0) |
| <$5,000 | 1 | (0.30) |
| Unknown | 175 | (35.79) |
| Mean | (SD) | |
| Symptom measure scores | ||
| ARI | 4.38 | (4.15) |
| CBRS Inattentive | 10.55 | (8.53) |
| CBRS Hyperactive/Impulsive | 7.88 | (7.42) |
| n | (%) | |
| Research group b | ||
| ADHD | 102 | (20.86) |
| DMDD | 191 | (39.06) |
| Sub-DMDD | 19 | (3.89) |
| Healthy volunteer | 177 | (36.20) |
| Diagnosis c | ||
| ADHD | 251 | (51.33) |
| Anxiety disorderd | 108 | (22.09) |
| CD | 3 | (0.61) |
| DMDD | 191 | (39.06) |
| MDD | 21 | (4.29) |
| ODDe | 24 | (4.91) |
| None | 177 | (36.20) |
| Medication f | ||
| AED | 25 | (5.11) |
| ADHD medicationsg | 136 | (27.81) |
| SGA | 52 | (10.63) |
| SSRI | 70 | (14.31) |
| None | 314 | (64.21) |
Note: ADHD = attention-deficit/hyperactivity disorder; AED = antiepileptic drug; ARI = Affective Reactivity Index; CBRS Hyperactive/Impulsive = DSM Hyperactive/Impulsive Subscale scores of the Conners Comprehensive Behavior Ratings Scale; CBRS Inattentive = DSM Inattentive Subscale scores of the Conners Comprehensive Behavior Ratings Scale; CD = conduct disorder; DMDD = disruptive mood dysregulation disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder; SGA = second-generation antipsychotic; SSRI = selective serotonin reuptake inhibitor; Sub-DMDD = subthreshold disruptive mood dysregulation disorder.
One participant declined to indicate sex. This participant was coded as sex unspecified for analyses including sex in the model.
Percentage of total sample in each research group. Research group refers to the primary group or diagnosis for which participants were recruited for research purposes. Participants could have comorbid diagnoses.
Percentage of total sample with a diagnosis of each disorder. Participants could have multiple diagnoses.
Anxiety disorder includes generalized anxiety disorder, separation anxiety disorder, social anxiety disorder, and specific phobias.
Following DSM-5 exclusion rules, ODD cannot be diagnosed with DMDD.
Percentage of total sample taking each medication type. Participants could be taking more than one type of medication.
Includes stimulants, anti-ADHD medication, and nonstimulant anti-ADHD medication.
The sample was recruited to represent full ranges of irritability and ADHD symptoms, including youths with a primary diagnosis of DMDD (n = 191) or ADHD (n = 102), youths with clinically significant irritability that did not meet thresholds required for DMDD (subthreshold DMDD [sub-DMDD], n = 19), and youths with no psychiatric diagnosis (Table 1). Youths with sub-DMDD exhibited temper outbursts at least once per month, irritable mood at least 1 day per week for most of the day, and irritability-related impairment in at least one setting (home, school, peers); all other criteria for sub-DMDD were the same as those for DMDD. Before participation, diagnoses were confirmed by a doctoral- or master’s-level clinician using the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime version (K-SADS-PL)29 including a DMDD module.30 All diagnoses were reviewed by a board-certified psychiatrist or psychologist (D.S.P., M.A.B., or E.L.). Additional clinical characteristics are presented in Table 1. Exclusionary criteria were IQ <70; diagnosis of autism spectrum disorder, past and/or current posttraumatic stress disorder, schizophrenia, or depression; use of any substance with psychoactive effects within 3 months; and neurological disorder. Parents provided written informed consent and youths provided written assent before participation. All study procedures were approved by the NIMH Institutional Review Board. Participants received monetary compensation.
Measures
Latent Profiles of Irritability and ADHD Symptoms.
Overall levels of irritability were assessed using the parent-report Affective Reactivity Index (ARI).31 The ARI is one of the most widely used measures of irritability and has been used in samples comparable to the current one.32 Scores ranged across all possible scores from a minimum of 0 to a maximum of 12 (mean [SD] = 4.38 [4.15]). Internal consistency of the ARI was high in the current study (α = .94). Total scores on the ARI were z-transformed before analysis.
ADHD symptoms were assessed using the parent-report Conners Comprehensive Behavior Ratings Scale (CBRS) DSM Inattentive and Hyperactive/Impulsive subscales.33 Scores ranged across all possible scores from a minimum of 0 to a maximum of 27 on the Inattentive subscale (mean [SD] = 10.55 [8.53]) and the Hyperactive/Impulsive subscale (mean [SD] = 7.88 [7.42]). Internal consistency of both the Inattentive (α = .96) and the Hyperactive-Impulsive (α = .93) subscale was high in the current study. Again, all scores were z-transformed before analysis.
Phasic and Tonic Irritability and Aggression.
For assessment of phasic irritability, the observed variables used to index temper outbursts included parent-, child-, and clinician-rated measures. Specifically, we used the clinician-rated Temper Outbursts item (ie, “Do you get angry a lot? Do you have blow-ups or lose your temper? Do little things get you mad? When you get really angry do you yell and scream, stomp around, throw or break things?”) from either the DMDD module or severe mood dysregulation module of the K-SADS-PL,30 the Explosiveness subscale of the parent-report Screen for Children’s Affective Reactivity–Home (SCAR-H) (eg, “Being ‘hot-blooded’ and quick tempered”),34 and the Anger Expression-Out subscale (expression of angry feelings toward other persons or objects in the environment) of the child-report State-Trait Anger Expression Inventory–Child/Adolescent (STAXI-CA) (eg, “I do things like slam doors”).35 Responses to the K-SADS-PL Temper Outburst item ranged from 1 to 3 (mean [SD] = 2.54 [0.75]), with 1 indicating not present, 2 indicating subthreshold level, and 3 indicating threshold level (temper outbursts occur at least 3 times a week and are grossly disproportionate to the stressor and inconsistent with developmental level). SCAR-H Explosiveness subscale scores were computed as participants’ mean response across all items, which were scored on 3-point Likert scales. Scores ranged from 1 to 3 (mean [SD] = 1.69 [0.65]). STAXI-CA Anger Expression-Out subscale sum scores ranged from 5 to 15 (mean [SD] = 9.30 [2.55]).
To index aggression, we used 3 aggression subscales from the parent-report Retrospective Modified Overt Aggression Scale (RMOAS)36: Verbal Aggression (ie, “How many times did your child threaten to hurt someone?”), Aggression Against Property (ie, “How many times did your child break things, smash windows, or damage or deface property on purpose?”), and Aggression Towards Others (ie, “How many times did your child hit someone with hands or an object, kick, push, scratch, or pull hair?”) as well as the Aggression subscale from the parent-report SCAR-H (eg, “Making threatening gestures, like swinging at people or grabbing at others”). For RMOAS, subscale scores were calculated using a summed score. Scores ranged from 0 to 20 on the RMOAS Verbal Aggression subscale (mean [SD] = 3.15 [4.23]), 0 to 44 on the Aggression Against Property subscale (mean [SD] = 5.07 [7.09]), and 0 to 52 on the Aggression Towards Others (mean [SD] =7.22 [11.20]). SCAR-H Aggression subscale scores were computed using the mean response on a 3-point Likert scale across all items. Scores ranged from 1 to 3 (mean [SD] = 1.49 [0.49]).
Critically, the SCAR-H and RMOAS Aggression subscales include items that broadly capture aggressive behaviors and do not differentiate between reactive and proactive aggression. For example, the RMOAS Verbal Aggression subscale includes both “How many times did your child threaten to hurt someone?” and “How many times did your child shout angrily, curse, or insult people in a repetitive, out-of-control way?”; these items could capture more proactive and more reactive forms of verbal aggression, respectively. Given that these measures capture a more global assessment of aggression than typically characteristic of phasic irritability, we modeled aggression separately from temper outbursts as 2 independent latent factors.
Similar to phasic irritability, the observed variables used to index irritable mood between outbursts included parent-, child-, and clinician-rated measures. Specifically, we used the clinician-rated Mood Between Outbursts item (ie, “Do you often feel irritable, cranky, or angry? Do you feel this way most of the day nearly every day?”) from the DMDD and severe mood dysregulation modules of the K-SADS-PL, item 12 (ie, “Being kinda grouchy”) from the parent-report SCAR-H, and item 16 (ie, “I feel grouchy”) from the child-report STAXI-CA. Responses to the DMDD module ranged from 1 to 3 (mean [SD] = 2.51 [0.75]) where 1 indicates not present, 2 indicates subthreshold levels of irritable mood between outbursts, and 3 indicates irritable mood between meets/exceeds threshold (present most of the day and nearly every day). Responses to SCAR-H item 12 were given on a 3-point Likert scale and ranged from 1 to 3 (mean [SD] = 1.85 [0.78]). Responses to STAXI-CA item 16 were given on a 3-point Likert scale and ranged from 1 to 3 (mean [SD] = 1.54 [0.61]).
Global Impairment.
Overall severity of impairment resulting from psychiatric symptoms was measured by the Children’s Global Assessment Scale (CGAS).37 The CGAS is a well-established clinician-rated measure scored on the basis of clinical interviews with both the parent and the child. Scores on the CGAS ranged from 1 to 100 (mean [SD] = 59.71 [18.04]), with lower CGAS scores reflecting greater levels of impairment.
Comorbid Symptoms.
In a subset of participants (n = 483), anxiety symptoms were measured using the parent-report Screen for Child Anxiety Related Emotional Disorders (SCARED) total score.38 Scores ranged from 0 to 58 (mean [SD] = 13.45 [12.89]), indicating variability in levels of anxiety through the clinical range (scores >25). Oppositionality was measured using 4 items from the Conners CBRS (ie, “Argues with adults,” “Actively defies or refuses to comply with adults’ requests,” “Blames others for his/her mistakes or misbehavior,” Spiteful“ or vindictive”) that were not confounded with irritability. A summed Conners CBRS Oppositionality score was calculated for each participant. Scores ranged across all possible scores (0–12) (mean [SD] = 4.18 [3.61]).
Data Analysis
Latent Profile Analysis.
LPA was conducted in R Version 3.6.0 using the tidyLPA package to assess latent classes as a function of irritability and ADHD symptoms. Successive solutions were fit to the data by increasing the number of classes by 1 until the best-fitting solution was found. Models were evaluated using the Bayesian information criterion, Akaike information criterion, entropy, and bootstrapped parametric likelihood ratio test. Indices of good model fit include lower Bayesian information criterion and Akaike information criterion values, entropy >0.80, and a significant bootstrapped parametric likelihood ratio test (< 0.05). We also evaluated models based on the size of the smallest derived class, using a cutoff of 5% for the smallest derived class. These model selection criteria were consistent with prior work done with similar populations.32,39 There were no missing data on the ARI or Conners CBRS. Participants were subsequently categorized according to their most likely class.
Confirmatory Factor Analysis.
We conducted CFAs using the lavaan package40 in R to extract estimates of temper outbursts, aggression, and irritable mood between outbursts. Three independent models were fit using full information maximum likelihood to handle missing data. A single latent variable each for temper outbursts, aggression, and irritable mood between outbursts was estimated using the observed variables described above. For the aggression latent variable, model fit was assessed using the comparative fit index, Tucker Lewis index, and root mean square error of approximation. For comparative fit index and Tucker Lewis index, values >0.950 indicate strong model fit. For root mean square error of approximation, values <0.05 indicate good model fit and values <0.08 indicate adequate model fit. Because temper outbursts and irritable mood between outbursts models were estimated using only 3 observed variables each, they were just-identified models with insufficient degrees of freedom to estimate fit. Importantly, path coefficients are still valid, allowing for assessment of the degree to which observed variables contribute to the latent variable. Factor scores were extracted for each latent variable for each participant. In contrast to summed scores, factor scores capture the shared variance among measured variables within each model. Therefore, factor scores are less susceptible to measure-specific variance or impurities.
Comparison Between Classes.
To examine associations of classes with phasic and tonic irritability, we conducted an analysis of covariance (ANCOVA) with class entered as a between-subjects factor and age and sex entered as covariates. Effect sizes are reported for all analyses. For omnibus effects, we report partial eta-squared (ηp2), and for pairwise comparisons, we report d.
RESULTS
LPA of Irritability and ADHD Symptoms
Results of the LPA supported a 4-class solution (Figure 1; Table 2; Table S1, available online). A 5-class solution failed to converge and exhibited a very low probability (< .1%) of some classes being assigned cases. The 4 classes all differed significantly from one another on ARI scores (F3,485 = 1075.94, p < .001, ηp2 = 0.87), Conners CBRS Inattentive scores (F3,485 = 577.89, p < .001, ηp2 = 0.78), and Conners CBRS Hyperactive-Impulsive scores (F3,485 = 424.00, p < .001, ηp2 = 0.72) (all pairwise comparisons p < 0.01).
FIGURE 1. Mean Scores on the Symptom Measures for Each Class in the 4-Class Solution.
Note: Irritability as measured by the parent report Affective Reactivity Index (ARI), CBRS Inattentive and CBRS Hyperactive/Impulsive as measured by the DSM Inattentive and Hyperactive/Impulsive subscales of the Conners Comprehensive Behavior Rating Scale. z-score of 1 = ARI Parent score of 8.52, Conners CBRS Inattentive score of 19.08, and Conners CBRS Hyperactive/Impulsive score of 15.29; z-score of 0 = ARI Parent score of 4.38, Conners CBRS Inattentive score of 10.55, Conners CBRS Hyperactive/Impulsive score of 7.88; z-score of −1 = ARI Parent score of 0.23, Conners CBRS Inattentive score of 2.02, and Conners CBRS Hyperactive/Impulsive score of 0.46. ADHD = attention-deficit/hyperactivity disorder.
TABLE 2.
Fit Information for Latent Profile Analysis Models With 2–5 Classes
| Classes | Log likelihood | AIC | BIC | Entropy | BLRT | Smallest class proportion, % |
|---|---|---|---|---|---|---|
| 2 | −1659.09 | 3338.18 | 3380.10 | 0.91 | < 0.01 | 49.08 |
| 3 | −1567.36 | 3162.71 | 3221.40 | 0.88 | < 0.01 | 24.72 |
| 4 | −1490.02 | 3016.04 | 3091.50 | 0.89 | < 0.01 | 12.68 |
| 5 | −1490.01 | 3024.02 | 3116.26 | 0.73 | 0.36 | < 0.01 |
Note: AIC = Akaike information criterion; BIC = Bayesian information criterion; BLRT = bootstrapped parametric likelihood ratio test.
For ease of interpretation, each class was characterized using ARI raw scores and Conners CBRS T scores (Table 3). For Conners CBRS T scores, published cutoffs are33 ≥70 = very elevated, 65–69 = elevated, 60–64 = high average, 40–59 = average, and <40 = low. For ARI scores, the current classes’ levels are <1 = low, <3 = moderate, and ≥8 = high.32 Based on these criteria, we characterized the 4 classes as high levels of both irritability and ADHD symptoms (n [%] = 130 [26.58%]), high levels of irritability and moderate levels of ADHD symptoms (n [%] = 87 [17.79%]), moderate levels of irritability and high levels of ADHD symptoms (n [%] = 62 [12.68%]), and low levels of both irritability and ADHD symptoms (n [%] = 210 [42.94%]).
TABLE 3.
Demographics and Symptom Measures by Each Class in the 4-Class Solution
| High irritability + high ADHD | High irritability + moderate ADHD | Moderate irritability + high ADHD | Low irritability + low ADHD | Omnibus p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age | 11.08 | (1.90)a | 10.91 | (1.98)a | 12.34 | (2.20)b | 13.00 | (2.55)c | < .001 |
| IQ | 110.31 | (13.52) | 110.81 | (12.32) | 110.94 | (13.07) | 110.27 | (12.28) | .98 |
| Sex, n (% female) | 43 | (33.07)a | 40 | (45.98)a,c | 14 | (22.58)b | 123 | (58.85)c | < .001 |
| Race, (%) | < .001 | ||||||||
| White | 98 | (75.38)a | 65 | (74.71)a | 48 | (77.42)a | 100 | (47.62)b | |
| American Indian or Alaskan Native | 1 | (0.77)a | 0 | (0.00)a | 1 | (1.61)a | 1 | (0.48)a | |
| Asian | 5 | (3.85)a,b | 6 | (6.90)b | 0 | (0.00)a | 12 | (5.71)a,b | |
| Black or African American | 11 | (8.46)a,b | 3 | (3.45)b | 9 | (14.52)a | 61 | (29.05)c | |
| Multiple races | 12 | (9.23)a | 8 | (9.20)a | 3 | (4.84)a | 22 | (10.48)a | |
| Other | 0 | (0.00)a | 0 | (0.00)a | 0 | (0.00)a | 1 | (0.48)a | |
| Unknown | 3 | (2.31)a | 5 | (5.75)a | 1 | (1.61)a | 13 | (6.19)a | |
| Ethnicity, n (%) | .46 | ||||||||
| Latino or Hispanic | 15 | (11.54) | 8 | (9.20) | 8 | (12.90) | 21 | (10.00) | |
| Not Latino or Hispanic | 114 | (87.69) | 74 | (85.06) | 53 | (85.48) | 182 | (86.67) | |
| Unknown | 1 | (0.77) | 5 | (5.75) | 1 | (1.61) | 7 | (3.33) | |
| Impairmente | 47.06 | (7.61)a | 51.69 | (11.89)b | 61.58 | (11.33)c | 82.25 | (13.74)d | < .001 |
| ARI Parent | 8.99 | (1.70)a | 8.09 | (1.93)b | 2.52 | (1.79)c | 0.53 | (1.00)d | < .001 |
| CBRS Inattentive T score | 74.45 | (8.96)a | 58.95 | (8.98)b | 70.97 | (8.75)c | 46.54 | (5.94)d | < .001 |
| CBRS Hyperactive/Impulsive T score | 79.24 | (9.04)a | 62.54 | (10.27)b | 69.26 | (13.18)c | 46.99 | (5.50)d | < .001 |
Note: Values are reported as mean (SD) unless otherwise noted. Cells marked with different superscript letters (a, b, c, d) are significantly different.
ADHD = attention-deficit/hyperactivity disorder; ARI = Affective Reactivity Index; CBRS Hyperactive/Impulsive = DSM Hyperactive/Impulsive Subscale scores of the Conners Comprehensive Behavior Ratings Scale; CBRS Inattentive = DSM Inattentive Subscale scores of the Conners Comprehensive Behavior Ratings Scale.
Children’s Global Assessment Scale scores range from 1 to 100, with lower scores reflecting greater impairment.
Demographic Variables and Global Impairment
Examination of demographic variables by derived class showed that the 4 classes differed significantly in age (F3,484 = 28.74, p < .001, ηp2 = 0.15), sex (χ26 = 37.61, p < .001, φ = 0.28), race (χ218 = 60.88, p < .001, φ = 0.20), and overall severity of impairment (F3,294 = 161.70, p < .001, ηp2 = 0.63) (for pairwise comparisons see Table 3). The classes did not differ in IQ (F3,392 = 0.06, p = .98, ηp2 = 0.00) or ethnicity (χ26 = 5.72, p = .46, φ = 0.08).
Associations of Classes With Phasic and Tonic Irritability
Phasic Irritability.
For temper outbursts, CFA estimated a single latent variable using the 3 observed variables (Figure 2). Because the model was just-identified, fit statistics could not be computed. All 3 observed variables loaded significantly on the temper outburst latent variable (all ps < .001). Of note, the loading of the SCAR-H Explosiveness subscale was very high (0.94), both in absolute terms and relative to the loadings for the STAXI-CA Anger Expression-Out subscale and the K-SADS Temper Outbursts item (0.52 and 0.72, respectively). Participants’ factor scores were extracted (N = 456: high levels of both irritability and ADHD symptoms, n = 129; high levels of irritability and moderate levels of ADHD symptoms, n = 85; moderate levels of irritability and high levels of ADHD symptoms, n = 61; low levels of both irritability and ADHD symptoms, n = 181).
FIGURE 2. Confirmatory Factor Analysis Models for Temper Outbursts, Aggression, and Irritable Mood Between Outbursts.
Note: (A) temper outbursts, (B) aggression, and (C) irritable mood between outbursts. Path coefficients represent the loading of each item onto the latent factor. DMDD = disruptive mood dysregulation disorder; RMOAS = Retrospective Modified Overt Aggression Scale; SCAR-H = Screen for Children’s Affective Reactivity–Home; STAXI = State-Trait Anger Expression Inventory.
***p < .001.
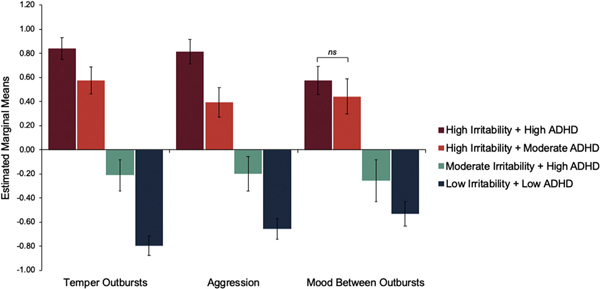
An ANCOVA examined temper outbursts factor scores by class, covarying age and sex. Classes differed significantly in temper outbursts (F3,450 = 211.91, p < .001, ηp2 = 0.59. Post hoc pairwise comparisons using the estimated marginal means indicated that temper outbursts differed significantly between all classes (all ps < .002, ds = 0.46–2.81), with the highest temper outburst score in the high levels of both irritability and ADHD symptoms class, followed by the high levels of irritability and moderate levels of ADHD symptoms class, then the moderate levels of irritability and high levels ADHD symptoms class, and last the low levels of irritability and ADHD symptoms class (Figure 3; Table S2, available online).
FIGURE 3. Estimated Marginal Means for Temper Outbursts, Aggression, and Irritable Mood Between Outbursts Factor Scores Across Each Class in the 4-Class Solution.
Note: Error bars represent 95% CI. The only nonsignificant pairwise comparison was for irritable mood between outbursts scores between the high irritability + high ADHD and high irritability + moderate ADHD groups. ADHD = attention-deficit/hyperactivity disorder; ns = nonsignificant.
For aggression, CFA estimated a single latent variable using the 4 observed variables (Figure 2). Model fit indices indicated good model fit (Tucker Lewis index = 1.00; comparative fit index = 1.00; root mean square error of approximation = 0, 90% CI [0, 0.08]; χ22 = 1.38, p = .50). All 4 observed variables loaded significantly on the latent factor (all ps < .001). Participants’ factor scores were extracted (N = 452: high levels of both irritability and ADHD symptoms, n = 125; high levels of irritability and moderate levels of ADHD symptoms, n = 83; moderate levels of irritability and high levels of ADHD symptoms, n = 57; low levels of both irritability and ADHD symptoms, n = 187).
An ANCOVA examined aggression factor scores by class, covarying age and sex. Classes differed significantly in aggression (F3,446 = 114.53, p < .001, ηp2 = 0.44). Post hoc pairwise comparisons using the estimated marginal means indicated that aggression differed significantly between all classes (all ps < .001, ds = 0.63–2.13), with the highest aggression score in the high levels of both irritability and ADHD symptoms class followed by the high levels of irritability and moderate levels of ADHD symptoms class, then the moderate levels of irritability and high levels of ADHD symptoms class, and last the low levels of both irritability and ADHD symptoms class (Figure 3; Table S2 available online).
Tonic Irritability.
CFA estimated a single latent variable using the 3 observed variables (Figure 2). Because the model was just-identified, fit statistics could not be computed. All 3 observed variables loaded significantly on the latent variable (all ps < .001). Of note, the loading for STAXI-CA item 16 (0.30) was somewhat lower than the loadings for the K-SADS Mood Between item and SCAR-H item 12 (0.69 and 0.65, respectively). Participants’ factor scores were extracted (N = 456: high levels of both irritability and ADHD symptoms, n = 129; high levels of irritability and moderate levels of ADHD symptoms, n = 85; moderate levels of irritability and high levels of ADHD symptoms, n = 61; low levels of both irritability and ADHD symptoms, n = 181).
An ANCOVA examined irritable mood factor scores by class, covarying age and sex. Classes differed significantly in irritable mood (F3,450 = 120.16, p < .001, ηp2 = 0.45). Post hoc pairwise comparisons using the estimated marginal means indicated that irritable mood did not differ significantly between the high irritability and high ADHD symptoms class vs the high irritability and moderate ADHD symptoms class (mean difference = 0.13, 95% CI [−0.01, 0.27], p = .06, d = 0.25) (Figure 3). All other pairwise comparisons were significant (all ps < .001, ds = 0.52–2.08) (Table S2, available online).
Given the high correlations between phasic and tonic irritability (rs = 0.58–0.79) (Table S3, available online), we repeated analyses for temper outbursts and aggression controlling for irritable mood (F3,449 = 59.20, p < .001, ηp2 = 0.28 and F3,436 = 41.19, p < .001, ηp2 = 0.22, respectively) and for irritable mood between outbursts controlling for temper outbursts (F3,436 = 6.25, p < .001, ηp2 = 0.04) or aggression (F3,436 = 46.96, p < .001, ηp2 = 0.24). The findings remained unchanged with one exception: irritable mood did not differ significantly between the low levels of both irritability and ADHD symptoms class vs the moderate levels of irritability and high levels of ADHD symptoms class when controlling for temper outbursts (mean difference = 0.03, 95% CI [−0.11, 0.16], p = .69, d = 0.05). All pairwise comparisons are in Tables S4 and S5, available online.
Last, we repeated the analyses to address potential confounding effects of co-occurring anxiety and oppositionality.28 Overall, the pattern of findings did not change when either anxiety or oppositionality was entered as a covariate in the models. Critically, when comparing the 2 high-irritability classes, high relative to moderate co-occurring ADHD symptoms were associated with larger effects for temper outbursts and aggression than irritable mood. See Supplement 1 (Tables S6–S9), available online, for a full discussion of these analyses.
DISCUSSION
The present study is the first to use data-driven methods to identify profiles of irritability and ADHD symptoms in a large, transdiagnostic sample of youths. Using LPA, we identified 4 symptom classes: high levels of both irritability and ADHD symptoms, low levels of both irritability and ADHD symptoms, and 2 opposing, intermediate profiles characterized by high levels of irritability and moderate levels of ADHD symptoms vs moderate levels of irritability and high levels of ADHD symptoms. With respect to phasic and tonic components of irritability, as expected across the 2 classes characterized by high overall irritability, we observed significant levels of temper outbursts, irritable mood between outbursts, and aggression in both groups. However, when comparing these 2 high-irritability classes, high relative to moderate co-occurring ADHD symptoms were associated with significantly greater temper outbursts and aggression, but not irritable mood between outbursts. This clinically important pattern of findings suggests that while phasic and tonic irritability are strongly related constructs, they are potentially dissociable through their associations with comorbid ADHD symptoms.
The best fit solution of our LPA indicated classes characterized by differing levels of irritability and ADHD symptoms. Of note, no classes emerged with high levels of one clinical dimension and low levels of the other. This suggests that in a clinical sample, irritability and ADHD symptoms co-occur to some extent in all classes where symptoms are present. The 2 classes characterized by high irritability demonstrated poorer overall functioning, converging with prior findings that irritability is associated with considerable impairment.3,11,41 Moreover, the class with high levels of both irritability and ADHD symptoms demonstrated the poorest overall functioning. Thus, for treatment-seeking youths with severe irritability, co-occurring ADHD symptoms appears to be associated with increased impairment.
Prior research has focused on identifying an irritable subtype of ADHD.7,8,42 Conversely, our analyses extend previous work by probing the effect of co-occurring ADHD symptoms on different dimensions of irritability. Using CFA, we were able to extract novel indices of phasic and tonic irritability across parent-, child-, and clinician-informant reports. These indices could be used in further research. Interestingly, factor scores for the resulting latent variables were highly correlated with one another, supporting that tonic and phasic irritability symptoms are strongly related. Future factor analytic studies could compare models of phasic and tonic irritability that vary in factor structure and associations between latent variables. This would allow for a direct test of the degree to which phasic and tonic irritability symptoms are correlated. Such an approach would require additional measured variables, particularly for irritable mood between outbursts, which in the current study relied on only 3 item-level variables. Further rigorous work on disentangling these constructs relies on the development of additional measures of tonic irritability. Additionally, the current study included temper outbursts and aggression as separate latent variables capturing behavioral manifestations of underlying trait anger. These constructs were modeled separately owing to the broad measures of aggression included in the study. Future work might examine further whether measures of reactive aggression specifically and temper outbursts constitute a shared overarching construct of phasic irritability.
Critically, despite high correlations between tonic and phasic irritability symptoms, when comparing the 2 high-irritability classes that differed in levels of co-occurring ADHD symptoms, ie, high vs moderate, we observed large between-group effect sizes for temper outbursts and aggression, but only a small effect size for irritable mood that was not statistically significant. This differential association may arise from shared mechanisms between ADHD symptoms and phasic irritability. In particular, the differential association of ADHD symptoms with temper outbursts and aggression may implicate shared alterations in top-down, prefrontal modulation of subcortical brain processes, such as prepotent or automatic behavioral responses to stimuli.27,43 Deficits in cognitive control have been viewed as central to the construct of ADHD.44 Prior research implicates aberrant frontostriatal activity and associated cognitive control deficits45 as a potential endophenotype for ADHD.46 Temper outbursts and aggression may reflect underlying impairments in cognitive control, consistent with evidence that normative levels of temper outbursts and reactive aggression decrease across development as prefrontal cortex maturation occurs.47,48 In contrast, there may be less mechanistic overlap between irritable mood between outbursts and ADHD.
The current study has several limitations. First, our analyses adopted a classify-then-analyze approach. With this approach, LPA was used to first identify classes based on patterns of irritability and ADHD symptoms. We then compared phasic and tonic irritability across these classes. This approach treats class assignment as precise and does not capture its uncertain or probabilistic nature. Second, most participants were treatment-seeking, contributing to the relatively high rates of comorbidity, impairment, and medication use. The sample was recruited to include clinical groups characterized by primary irritability and/or ADHD symptoms. Although this enabled a fine-grained approach to clinical phenotyping of irritability and ADHD, it will be important to examine associations of phasic and tonic irritability with ADHD in community samples and across a wider range of psychiatric comorbidities.49 Thus, these findings may be relevant only for clinical samples characterized primarily by irritability and/or ADHD symptoms. Third, when possible, we included measured variables across parent, child, and clinician informants to balance potential informant effects. However, the measures of irritability and ADHD used in the LPA were limited to parent report. Given known cross-informant variations in the assessment of psychiatric symptoms in youths,50 future work might fruitfully expand this latter approach to include additional informants. In addition, the development of measures specifically aimed at differentiating phasic and tonic irritability would greatly benefit from inclusion of multiple informants. Fourth, because the current study is cross-sectional, causal pathways could not be assessed. Future longitudinal studies delineating developmental trajectories of irritability and ADHD symptoms are needed to explicate the nature of the relationships among symptoms. Fifth, the current findings suggest distinct mechanisms for phasic and tonic irritability as they relate to ADHD symptoms; however, analyses were limited to the clinical data. Future work examining neural and behavioral correlates of phasic and tonic irritability will be essential to testing purported mechanisms. Finally, the sociodemographic composition of the sample was predominantly White and of high socioeconomic status. In further research in this area, more diverse samples should be recruited.
Despite these limitations, the current study is the first to leverage data-driven methods to identify patterns of irritability and ADHD symptoms in a large, well-characterized, transdiagnostic sample of youths. The novel findings suggest that phasic and tonic irritability are differentially associated with co-occurring ADHD symptoms. These findings suggest that highly comorbid irritability and ADHD symptoms represent an increased risk for clinical impairment. Future work investigating temper outbursts and irritable mood holds promise for disentangling dimensions of irritability with potentially distinct correlates and mechanisms. Identifying and targeting potential common mechanisms underlying irritability and ADHD, such as impaired cognitive control, may serve as a promising intervention for DMDD with comorbid ADHD. However, additional work is needed directly interrogating cognitive control deficits in irritable youths with varying levels of ADHD symptoms.
Supplementary Material
Acknowledgments
This work is supported by the National Institute of Mental Health (NIMH) Intramural Research Program (ZIAMH002781), conducted under National Institutes of Health Clinical Study Protocols 01-M-0192 (ClinicalTrials.gov identifier: NCT00018057) and a Bench-to-Bedside Award (479969).
Footnotes
Publisher's Disclaimer: Disclosure: Drs. Cardinale, Brotman, Pine, Leibenluft, Kircanski, and Ms. Freitag have reported no biomedical financial interests or potential conflicts of interest.
REFERENCES
- 1.Leibenluft E Pediatric irritability: A systems neuroscience approach. Trends Cogn Sci. 2017;21:277–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 3.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 2013;170:173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leibenluft E Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168:129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16:456–466. [DOI] [PubMed] [Google Scholar]
- 6.Liu L, Chen W, Vitoratou S, et al. Is emotional lability distinct from “angry/irritable mood,” negative“ affect,” or other subdimensions of oppositional defiant disorder in children with ADHD? J Atten Disord. 2019;23:859–868. [DOI] [PubMed] [Google Scholar]
- 7.Karalunas SL, Gustafsson HC, Fair D, Musser ED, Nigg JT. Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychol Assess 2019;31:236–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eyre O, Langley K, Stringaris A, Leibenluft E, Collishaw S, Thapar A. Irritability in ADHD: Associations with depression liability. J Affect Disord. 2017;215: 281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw P, Stringaris A, Nigg J, Leibenluft E. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 2014;171:276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother. 2009;9:489–503. [DOI] [PubMed] [Google Scholar]
- 11.Mulraney M, Schilpzand EJ, Hazell P, et al. Comorbidity and correlates of disruptive mood dysregulation disorder in 6–8-year-old children with ADHD. Eur Child Adolesc Psychiatry. 2016;25:321–330. [DOI] [PubMed] [Google Scholar]
- 12.Sobanski E, Banaschewski T, Asherson P, et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): Clinical correlates and familial prevalence: Emotional lability in ADHD. J Child Psychol Psychiatry 2010;51:915–923. [DOI] [PubMed] [Google Scholar]
- 13.Eyre O, Riglin L, Leibenluft E, Stringaris A, Collishaw S, Thapar A. Irritability in ADHD: Association with later depression symptoms. Eur Child Adolesc Psychiatry. 2019;28:1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maedgen JW, Carlson CL. Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol. 2000;29:30–42. [DOI] [PubMed] [Google Scholar]
- 15.Moore CC, Hubbard JA, Bookhout MK, Mlawer F. Relations between reactive and proactive aggression and daily emotions in adolescents. J Abnorm Child Psychol. 2019; 47:1495–1507. [DOI] [PubMed] [Google Scholar]
- 16.Insel T, Cuthbert B, Garvey M, et al. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. Am J Psychiatry 2010;167: 748–751. [DOI] [PubMed] [Google Scholar]
- 17.Roberson-Nay R, Leibenluft E, Brotman MA, et al. Longitudinal stability of genetic and environmental influences on irritability: From childhood to young adulthood. Am J Psychiatry. 2015;172:657–664. [DOI] [PubMed] [Google Scholar]
- 18.Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: A conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. 2016;55:556–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Copeland WE, Brotman MA, Costello EJ. Normative irritability in youth: Developmental findings from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2015;54:635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blader JC, Pliszka SR, Kafantaris V, et al. Prevalence and treatment outcomes of persistent negative mood among children with attention-deficit/hyperactivity disorder and aggressive behavior. J Child Adolesc Psychopharmacol. 2016;26:164–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlson GA, Danzig AP, Dougherty LR, Bufferd SJ, Klein DN. Loss of temper and irritability: The relationship to tantrums in a community and clinical sample. J Child Adolesc Psychopharmacol. 2016;26:114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore AA, Lapato DM, Brotman MA, et al. Heritability, stability, and prevalence of tonic and phasic irritability as indicators of disruptive mood dysregulation disorder. J Child Psychol Psychiatry. 2019;60:1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernáandez de la Cruz L, Simonoff E, McGough JJ, Halperin JM, Arnold LE, Stringaris A. Treatment of children with attention-deficit/hyperactivity disorder (ADHD) and irritability: Results from the Multimodal Treatment Study of Children With ADHD (MTA). J Am Acad Child Adolesc Psychiatry 2015;54:62–70.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Posner J, Kass E, Hulvershorn L. Using stimulants to treat ADHD-related emotional lability. Curr Psychiatry Rep. 2014;16:478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waxmonsky J, Pelham WE, Gnagy E, et al. The efficacy and tolerability of methylphenidate and behavior modification in children with attention-deficit/hyperactivity disorder and severe mood dysregulation. J Child Adolesc Psychopharmacol. 2008;18:573–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Towbin K, Vidal-Ribas P, Brotman MA, et al. A double-blind randomized placebo-controlled trial of citalopram adjunctive to stimulant medication in youth with chronic severe irritability. J Am Acad Child Adolesc Psychiatry. 2020;59:350–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beauchaine TP, Zisner AR, Sauder CL. Trait impulsivity and the externalizing spectrum. Annu Rev Clin Psychol. 2017;13:343–368. [DOI] [PubMed] [Google Scholar]
- 28.Leibenluft E, Stoddard J. The developmental psychopathology of irritability. Dev Psychopathol 2013;25(4 Pt 2):1473–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980–988. [DOI] [PubMed] [Google Scholar]
- 30.Wiggins JL, Brotman MA, Adleman NE, et al. Neural correlates of irritability in disruptive mood dysregulation and bipolar disorders. Am J Psychiatry. 2016;173: 722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stringaris A, Goodman R, Ferdinando S, et al. The Affective Reactivity Index: A concise irritability scale for clinical and research settings. J Child Psychol Psychiatry 2012;53: 1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kircanski K, Zhang S, Stringaris A, et al. Empirically derived patterns of psychiatric symptoms in youth: A latent profile analysis. J Affect Disord. 2017;216:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conners C, Pitkanen J, Rzepa S. Conners Comprehensive Behavior Rating Scale. In: Kreutzer JS, DeLuca J, Caplan B, eds. Encyclopedia of Clinical Neuropsychology. New York, NY: Springer; 2011. [Google Scholar]
- 34.Kolko DJ, Baumann BL, Bukstein OG, Brown EJ. Internalizing symptoms and affective reactivity in relation to the severity of aggression in clinically referred, behavior-disordered children. J Child Fam Stud. 2007;16:745–759. [Google Scholar]
- 35.Brunner T, Spielberger C. The State Trait Anger Expression Inventory-2 Child and Adolescent. Odessa, FL: Psychological Assessment Resources; 2009. [Google Scholar]
- 36.Blader JC, Pliszka SR, Kafantaris V, et al. Stepped treatment for attention-deficit/hyperactivity disorder and aggressive behavior: A randomized, controlled trial of adjunctive risperidone, divalproex sodium, or placebo after stimulant medication optimization. J Am Acad Child Adolesc Psychiatry. 2021;60:236–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaffer D A Children’s Global Assessment Scale (CGAS). Arch Gen Psychiatry 1983; 40:1228. [DOI] [PubMed] [Google Scholar]
- 38.Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 1997;36:545–553. [DOI] [PubMed] [Google Scholar]
- 39.Versella MV, Piccirillo ML, Potter CM, Olino TM, Heimberg RG. Anger profiles in social anxiety disorder. J Anxiety Disord. 2016;37:21–29. [DOI] [PubMed] [Google Scholar]
- 40.Rosseel Y Lavaan: An R package for structural equation modeling. J Stat Softw. 2012; 48:1–36. [Google Scholar]
- 41.Dougherty LR, Smith VC, Bufferd SJ, Kessel E, Carlson GA, Klein DN. Preschool irritability predicts child psychopathology, functional impairment, and service use at age nine. J Child Psychol Psychiatry. 2015;56:999–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mick E, Spencer T, Wozniak J, Biederman J. Heterogeneity of irritability in attention-deficit/hyperactivity disorder subjects with and without mood disorders. Biol Psychiatry. 2005;58:576–582. [DOI] [PubMed] [Google Scholar]
- 43.Kircanski K, Craske MG, Averbeck BB, Pine DS, Leibenluft E, Brotman MA. Exposure therapy for pediatric irritability: Theory and potential mechanisms. Behav Res Ther. 2019;118:141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biol Psychiatry. 2005;57:1336–1346. [DOI] [PubMed] [Google Scholar]
- 45.Chevrier A, Schachar RJ. BOLD differences normally attributed to inhibitory control predict symptoms, not task-directed inhibitory control in ADHD. J Neurodev Disord 2020;12:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Durston S, de Zeeuw P, Staal WG. Imaging genetics in ADHD: A focus on cognitive control. Neurosci Biobehav Rev. 2009;33:674–689. [DOI] [PubMed] [Google Scholar]
- 47.Brame B, Nagin DS, Tremblay RE. Developmental trajectories of physical aggression from school entry to late adolescence. J Child Psychol Psychiatry. 2001; 42:503–512. [PubMed] [Google Scholar]
- 48.Wiggins JL, Mitchell C, Stringaris A, Leibenluft E. Developmental trajectories of irritability and bidirectional associations with maternal depression. J Am Acad Child Adolesc Psychiatry. 2014;53:1191–1205.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Snyder HR, Friedman NP, Hankin BL. Transdiagnostic mechanisms of psychopathology in youth: Executive functions, dependent stress, and rumination. Cogn Ther Res. 2019; 43:834–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Los Reyes A, Augenstein TM, Wang M, et al. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull. 2015;141: 858–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.