Abstract
BACKGROUND:
Microsurgical free flaps have largely supplanted pedicled flaps as the gold standard for head and neck cancer reconstruction. However, incidence of postoperative complications after accounting for patient comorbidities based on choice of reconstruction have not been well-defined in the literature in recent years.
METHODS:
Patients undergoing head and neck reconstruction were identified in the 2011–2016 ACS-NSQIP database and stratified into groups by free flap, myocutaneous pedicled flap, and other reconstruction. Demographics were analyzed and covariates balanced using overlap propensity score-based weighting. Logistic regression was used for binary outcomes and Gamma GLM was used for length of stay.
RESULTS:
4,712 patients met inclusion criteria. 1,297 patients (28%) underwent free flap, 208 patients (4%) pedicled flap, and 3,207 patients (68%) had other or no reconstruction performed. After adjusting for patient and disease-specific factors, pedicled flap reconstruction was associated with a higher risk of DVT (OR=2.64, CI 1.02–6.85, p=0.045), sepsis (OR=2.95, CI 1.52–5.71, p=0.001), and infection (OR=2.03, CI 1.39–2.96, p<0.001) compared to free flap reconstruction. Free flaps had the longest mean operative time compared to the other two groups (unadjusted 578 vs 440 vs 326, p<0.001). Pedicled flaps had a lower incidence of bleeding requiring transfusion (adjusted OR=0.65, CI 0.50–0.85, p=0.002), and lower incidence of prolonged mechanical ventilation (adjusted OR=0.33, CI 0.12–0.92, p=0.034) compared to free flaps. There was no difference in rates of reoperation, hospital readmission, or hospital length-of-stay between pedicled and free flaps.
CONCLUSION:
Myocutaneous pedicled flaps are associated with higher overall short-term postoperative complications compared to free flaps in head and neck reconstruction, which demonstrate a more favorable morbidity profile without significantly impacting hospital readmission, reoperation, or length-of-stay.
Keywords: Head and neck cancer reconstruction, free tissue transfer, pedicled flaps
Introduction
Head and neck cancers account for approximately 4% of all cancers in the United States.1 Treatment may vary considerably due to the structures involved, type of cancer, and patient factors. Because morbidity and mortality in these patients is typically due to local invasion rather than distant metastases, excision and/or radiation is a standard feature of successful treatment.2 Tumor location, stage, patient age, comorbidities, and other factors impact the reconstructive options that are available. Reconstruction for head and neck cancer is particularly difficult relative to other locations due to the complexity of facial anatomy and functional impairments that can result from establishing oncologically sound resection margins.3 Even small defects after resection can affect aesthetics, speech, and swallowing which makes their proper reconstruction especially important for improving quality of life2–5.
Reconstructive techniques have been refined over the last 40 years and can range from skin grafting to free tissue transfer. The advent of free flap procedures has been particularly revolutionary for head and neck reconstruction.6 Prior to the mid-1970s, pedicled myocutaneous flaps were the standard choice to achieve secondary closure of large defects resulting from ablative head and neck surgery.3 While the results from these procedures are still considered acceptable in certain circumstances, their bulk and inconsistent mobilization limits their utility for the uniquely challenging reconstruction of head and neck cancer.4, 7, 8 Since their introduction in the 1980s, free flaps have provided surgeons with a reconstructive option that results in better functional and aesthetic outcomes with lower complication rates.2, 7, 9 The increased size, variety of tissue, and ability to contour free flaps makes them an extremely flexible modality well-suited for head and neck reconstruction.9–12 While there has been an explosion in possible reconstructive techniques for head and neck cancer patients, there has been a paucity of studies on specific short term postoperative outcomes based on the type of reconstruction and the variety of pedicled and free flaps available. We sought to address how type of reconstruction influences the incidence of several postoperative complications in head and neck cancer by studying 30-day outcomes through the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) Database. This large, multi-institutional, nationally validated database that tracks surgical outcomes and has been used to correlate surgical and demographic factors with complication rates and impact institutional practices.13–16 We used NSQIP to compare postoperative outcomes in patients who underwent free flap, pedicled myocutaneous flap, or other reconstruction (i.e. primary closure, local tissue rearrangement) after head and neck cancer resection.
Methods
Data Source
Data was retrospectively reviewed from the ACS-NSQI database from 2011–2016 (http://www.acsnsqip.org/). The study was approved by Fox Chase Cancer Center with a waiver of the need for individual consent. ACS-NSQIP data including patient demographics, preoperative risk factors, baseline comorbidities, intraoperative risk factors, 30-day postoperative morbidity and mortality were obtained. Our search query identified International Classification of Disease (ICD) codes for Head and Neck cancer diagnosis (Appendix 1). These were then cross-referenced with resection current procedural terminology (CPT) codes corresponding to laryngectomy, maxillectomy, mandibulectomy, glossectomy and floor of mouth excisions (Table 1). We grouped patients based on type of reconstruction performed, which was classified into free flap or pedicled myocutaneous flap reconstruction (Figure 1). We excluded patients for whom BMI, sex, operative time, estimated probability of morbidity or mortality could not be determined, patients that received preoperative transfusion within 72 hours of operation, those who met criteria for sepsis preoperatively, patients with wound class of dirty/infected, and patients who were in renal failure or required ventilator support preoperatively. Those who had combined free flap and pedicled flap reconstruction were also excluded to limit potential confounding. We also evaluated a subgroup of patients who underwent pedicled myocutaneous flap as a salvage procedure after free flap by searching the database for free flaps that were associated with a reoperative code for a myocutaneous pedicled flap within 30 days of initial procedure. Patients that had other or no reconstruction (primary closure, adjacent tissue rearrangement, skin grafting, etc) were included in the other reconstruction group. Codes for free flap reconstruction included anterolateral thigh, radial forearm, latissimus dorsi, and free fibular flaps. Codes for pedicled myocutaneous reconstruction included pectoralis, temporalis muscle, and submental artery perforator flaps.
Appendix:
ICD Codes for Head and Neck Cancer Diagnosis
| ICD Codes | |
|---|---|
| 140 | Malignant neoplasm of lip |
| 140.0 | Malignant neoplasm of upper lip, vermilion border |
| 140.1 | Malignant neoplasm of lower lip, vermilion border |
| 140.3 | Malignant neoplasm of upper lip, inner aspect |
| 140.4 | Malignant neoplasm of lower lip, inner aspect |
| 140.5 | Malignant neoplasm of lip, unspecified, inner aspect |
| 140.6 | Malignant neoplasm of commissure of lip |
| 140.8 | Malignant neoplasm of other sites of lip |
| 140.9 | Malignant neoplasm of lip, unspecified, vermilion border |
| 141 | Malignant neoplasm of tongue |
| 141.0 | Malignant neoplasm of base of tongue |
| 141.1 | Malignant neoplasm of dorsal surface of tongue |
| 141.2 | Malignant neoplasm of tip and lateral border of tongue |
| 141.3 | Malignant neoplasm of ventral surface of tongue |
| 141.4 | Malignant neoplasm of anterior two-thirds of tongue, part unspecified |
| 141.8 | Malignant neoplasm of other sites of tongue |
| 141.9 | Malignant neoplasm of tongue, unspecified |
| 142.0 | Malignant neoplasm of parotid gland |
| 142.1 | Malignant neoplasm of submandibular gland |
| 142.2 | Malignant neoplasm of sublingual gland |
| 142.8 | Malignant neoplasm of other major salivary glands |
| 142.9 | Malignant neoplasm of salivary gland, unspecified |
| 143 | Malignant neoplasm of gum |
| 143.0 | Malignant neoplasm of upper gum |
| 143.1 | Malignant neoplasm of lower gum |
| 143.9 | Malignant neoplasm of gum, unspecified |
| 144 | Malignant neoplasm of floor of mouth |
| 144.0 | Malignant neoplasm of anterior portion of floor of mouth |
| 144.1 | Malignant neoplasm of lateral portion of floor of mouth |
| 144.8 | Malignant neoplasm of other sites of floor of mouth |
| 144.9 | Malignant neoplasm of floor of mouth, part unspecified |
| 145 | Malignant neoplasm of other and unspecified parts of mouth |
| 145.0 | Malignant neoplasm of cheek mucosa |
| 145.1 | Malignant neoplasm of vestibule of mouth |
| 145.2 | Malignant neoplasm of hard palate |
| 145.3 | Malignant neoplasm of soft palate |
| 145.5 | Malignant neoplasm of palate, unspecified |
| 145.6 | Malignant neoplasm of retromolar area |
| 145.8 | Malignant neoplasm of other specified parts of mouth |
| 145.9 | Malignant neoplasm of mouth, unspecified |
| 146 | Malignant neoplasm of oropharynx |
| 146.0 | Malignant neoplasm of tonsil |
| 146.1 | Malignant neoplasm of tonsillar fossa |
| 146.2 | Malignant neoplasm of tonsillar pillars (anterior) (posterior) |
| 146.3 | Malignant neoplasm of vallecula epiglottica |
| 146.4 | Malignant neoplasm of anterior aspect of epiglottis |
| 146.6 | Malignant neoplasm of lateral wall of oropharynx |
| 146.7 | Malignant neoplasm of posterior wall of oropharynx |
| 146.8 | Malignant neoplasm of other specified sites of oropharynx |
| 146.9 | Malignant neoplasm of oropharynx, unspecified site |
| 147.1 | Malignant neoplasm of posterior wall of nasopharynx |
| 147.3 | Malignant neoplasm of anterior wall of nasopharynx |
| 147.8 | Malignant neoplasm of other specified sites of nasopharynx |
| 148 | Malignant neoplasm of hypopharynx |
| 148.0 | Malignant neoplasm of postcricoid region of hypopharynx |
| 148.1 | Malignant neoplasm of pyriform sinus |
| 148.2 | Malignant neoplasm of aryepiglottic fold, hypopharyngeal aspect |
| 148.3 | Malignant neoplasm of posterior hypopharyngeal wall |
| 148.8 | Malignant neoplasm of other specified sites of hypopharynx |
| 148.9 | Malignant neoplasm of hypopharynx, unspecified site |
| 149.0 | Malignant neoplasm of pharynx, unspecified |
| 149.8 | Malignant neoplasm of other sites within the lip and oral cavity |
| 149.9 | Malignant neoplasm of ill-defined sites within the lip and oral cavity |
| 150 | Malignant neoplasm of esophagus |
| 150.0 | Malignant neoplasm of cervical esophagus |
| 160 | Malignant neoplasm of nasal cavities middle ear and accessory sinuses |
| 160.0 | Malignant neoplasm of nasal cavities |
| 160.1 | Malignant neoplasm of auditory tube, middle ear, and mastoid air cells |
| 160.2 | Malignant neoplasm of maxillary sinus |
| 160.3 | Malignant neoplasm of ethmoidal sinus |
| 160.4 | Malignant neoplasm of frontal sinus |
| 160.8 | Malignant neoplasm of other accessory sinuses |
| 160.9 | Malignant neoplasm of accessory sinus, unspecified |
| 161 | Malignant neoplasm of larynx |
| 161.0 | Malignant neoplasm of glottis |
| 161.1 | Malignant neoplasm of supraglottis |
| 161.3 | Malignant neoplasm of laryngeal cartilages |
| 161.2 | Malignant neoplasm of subglottis |
| 161.8 | Malignant neoplasm of laryngeal cartilages |
| 161.9 | Malignant neoplasm of larynx, unspecified |
| 170 | Malignant neoplasm of bone and articular cartilage |
| 170.0 | Malignant neoplasm of bones of skull and face, except mandible |
| 170.1 | Malignant neoplasm of mandible |
| 170.6 | Malignant neoplasm of pelvic bones, sacrum, and coccyx |
| 171.0 | Malignant neoplasm of connective and other soft tissue of head, face, and neck |
| 172.0 | Malignant melanoma of skin of lip |
| 172.1 | Malignant melanoma of skin of eyelid, including canthus |
| 172.2 | Malignant melanoma of skin of ear and external auditory canal |
| 172.3 | Malignant melanoma of skin of other and unspecified parts of face |
| 172.4 | Malignant melanoma of skin of scalp and neck |
| 172 | Malignant melanoma of skin |
| 173.0 | Other and unspecified malignant neoplasm of skin of lip |
| 173.01 | Basal cell carcinoma of skin of lip |
| 173.02 | Squamous cell carcinoma of skin of lip |
| 173.1 | Other and unspecified malignant neoplasm of eyelid, including canthus |
| 173.10 | Unspecified malignant neoplasm of eyelid, including canthus |
| 173.11 | Basal cell carcinoma of eyelid, including canthus |
| 173.12 | Squamous cell carcinoma of eyelid, including canthus |
| 173.19 | Other specified malignant neoplasm of eyelid, including canthus |
| 173.2 | Other and unspecified malignant neoplasm of skin of ear and external auditory canal |
| 173.20 | Unspecified malignant neoplasm of skin of ear and external auditory canal |
| 173.21 | Basal cell carcinoma of skin of ear and external auditory canal |
| 173,22 | Squamous cell carcinoma of skin of ear and external auditory canal |
| 173.29 | Other specified malignant neoplasm of skin of ear and external auditory canal |
| 173.3 | Other and unspecified malignant neoplasm of skin of other and unspecified parts of face |
| 173.30 | Unspecified malignant neoplasm of skin of other and unspecified parts of face |
| 173.32 | Squamous cell carcinoma of skin of other and unspecified parts of face |
| 173.39 | Other specified malignant neoplasm of skin of other and unspecified parts of face |
| 173.4 | Other and unspecified malignant neoplasm of scalp and skin of neck |
| 173.40 | Unspecified malignant neoplasm of scalp and skin of neck |
| 173.41 | Basal cell carcinoma of scalp and skin of neck |
| 173.42 | Squamous cell carcinoma of scalp and skin of neck |
| 173.49 | Other specified malignant neoplasm of scalp and skin of neck |
| 190.1 | Malignant neoplasm of orbit |
| 190.2 | Malignant neoplasm of lacrimal gland |
| 190.3 | Malignant neoplasm of conjunctiva |
| 190.5 | Malignant neoplasm of retina |
| 190.7 | Malignant neoplasm of lacrimal duct |
| 190.9 | Malignant neoplasm of eye, part unspecified |
| 193 | Malignant neoplasm of thyroid gland |
| 194.1 | Malignant neoplasm of parathyroid gland |
| 194.3 | Malignant neoplasm of pituitary gland and craniopharyngeal duct |
| 195.0 | Malignant neoplasm of head, face, and neck |
| 196.0 | Secondary and unspecified malignant neoplasm of lymph nodes of head, face, and neck |
| 201.91 | Hodgkin’s disease, unspecified type, lymph nodes of head, face, and neck |
| 202.81 | Other malignant lymphomas, lymph nodes of head, face, and neck |
| 202.91 | Other and unspecified malignant neoplasms of lymphoid and histiocytic tissue, lymph nodes of head, face, and neck |
| 209.31 | Merkel cell carcinoma of the face |
| 209.32 | Merkel cell carcinoma of the scalp and neck |
| 210.0 | Benign neoplasm of lip |
| 210.1 | Benign neoplasm of tongue |
| 210.3 | Benign neoplasm of floor of mouth |
| 210.4 | Benign neoplasm of other and unspecified parts of mouth |
| 210.9 | Benign neoplasm of pharynx, unspecified |
| 212.1 | Benign neoplasm of larynx |
| 213.0 | Benign neoplasm of bones of skull and face |
| 213.1 | Benign neoplasm of lower jaw bone |
| 215.0 | Other benign neoplasm of connective and other soft tissue of head, face, and neck |
| 216.2 | Benign neoplasm of ear and external auditory canal |
| 216.3 | Benign neoplasm of skin of other and unspecified parts of face |
| 216.4 | Benign neoplasm of scalp and skin of neck |
| 226 | Benign neoplasm of thyroid glands |
| 227.1 | Benign neoplasm of parathyroid gland |
| 231.0 | Carcinoma in situ of larynx |
| 232.2 | Carcinoma in situ of skin of ear and external auditory canal |
| 232.4 | Carcinoma in situ of scalp and skin of neck |
| 234.0 | Carcinoma in situ of eye |
| 235.0 | Neoplasm of uncertain behavior of major salivary glands |
| 235.6 | Neoplasm of uncertain behavior of larynx |
| C13.9 | Malignant neoplasm of hypopharynx, unspecified |
| V10.01 | Personal history of malignant neoplasm of tongue |
| V10.02 | Personal history of malignant neoplasm of other and unspecified oral cavity and pharynx |
| V10.1 | Personal history of malignant neoplasm of trachea bronchus and lung |
| V10.21 | Personal history of malignant neoplasm of larynx |
| 141.9 | Malignant neoplasm of tongue, unspecified |
| 143.8 | Malignant neoplasm of other sites of gum |
| 148 | Malignant neoplasm of hypopharynx |
| 150.3 | Malignant neoplasm of upper third of esophagus |
| 162 | Malignant neoplasm of trachea bronchus and lung |
| 171 | Malignant neoplasm of connective and other soft tissue |
| 195 | Malignant neoplasm of other and ill-defined sites |
| 196 | Secondary and unspecified malignant neoplasm of lymph nodes |
| 200.11 | Lymphosarcoma, lymph nodes of head, face, and neck |
| 210.6 | Benign neoplasm of other parts of oropharynx |
| 210.7 | Benign neoplasm of nasopharynx |
| 212 | Benign neoplasm of respiratory and intrathoracic organs |
| 213 | Benign neoplasm of bone and articular cartilage |
| 213.9 | Benign neoplasm of bone and articular cartilage, site unspecified |
| 227.1 | Benign neoplasm of parathyroid gland |
| 235.1 | Neoplasm of uncertain behavior of lip, oral cavity, and pharynx |
| 238 | Neoplasm of uncertain behavior of other and unspecified sites and tissues |
Table 1:
Resection/Reconstruction CPT Codes Used in Study
| Procedure | CPT Code | Description |
|---|---|---|
| Laryngectomy | 31368 | laryngectomy; subtotal supraglottic, with radical neck dissection |
| 31367 | laryngectomy; subtotal supraglottic, without radical neck dissection | |
| 31365 | laryngectomy; total, with radical neck dissection | |
| 31360 | laryngectomy; total, without radical neck dissection | |
| 31382 | partial laryngectomy (hemilaryngectomy); antero-latero-vertical | |
| 31380 | partial laryngectomy (hemilaryngectomy); anterovertical | |
| 31370 | partial laryngectomy (hemilaryngectomy); horizontal | |
| 31375 | partial laryngectomy (hemilaryngectomy); laterovertical | |
| 31395 | pharyngolaryngectomy, with radical neck dissection; with reconstruction | |
| 31390 | pharyngolaryngectomy, with radical neck dissection; without reconstruction | |
| Glossectomy | 41145 | glossectomy; complete or total, with or without tracheostomy, with unilateral radical neck dissection |
| 41140 | glossectomy; complete or total, with or without tracheostomy, without radical neck dissection | |
| 41150 | glossectomy; composite procedure with resection floor of mouth and mandibular resection, without radical neck dissection | |
| 41155 | glossectomy; composite procedure with resection floor of mouth, mandibular resection, and radical neck dissection (commando type) | |
| 41153 | glossectomy; composite procedure with resection floor of mouth, with suprahyoid neck dissection | |
| 41130 | glossectomy; hemiglossectomy | |
| 41120 | glossectomy; less than one-half tongue | |
| 41135 | glossectomy; partial, with unilateral radical neck dissection | |
| 41112 | excision of lesion of tongue with closure; anterior two-thirds | |
| 41113 | excision of lesion of tongue with closure; posterior one-third | |
| 41114 | excision of lesion of tongue with closure; with local tongue flap | |
| 41110 | excision of lesion of tongue without closure | |
| 41116 | excision, lesion of floor of mouth | |
| Maxillectomy | 31225 | maxillectomy; without orbital exenteration |
| 31230 | maxillectomy; with orbital exenteration (en bloc) | |
| Mandibulectomy | 21046 | excision of benign tumor or cyst of mandible; requiring intra-oral osteotomy (eg, locally aggressive or destructive lesion[s]) |
| 21040 | excision of benign tumor or cyst of mandible, by enucleation and/or curettage | |
| 21044 | excision of malignant tumor of mandible, removal of malignant growth of lower jaw bone | |
| 21045 | excision of malignant tumor of mandible; radical resection | |
| Pedicled Myocutaneous Flap | 15734 | muscle, myocutaneous, or fasciocutaneous flap; trunk |
| 15730 | midface flap (ie, zygomaticofacial flap) with preservation of vascular pedicle(s) | |
| 15733 | muscle, myocutaneous, or fasciocutaneous flap; head and neck with named vascular pedicle (ie, buccinators, genioglossus, temporalis, masseter, sternocleidomastoid, levator scapulae) | |
| Free Tissue Transfer | 15757 | free skin flap with microvascular anastomosis |
| 15758 | free fascial flap with microvascular anastomosis | |
| 15756 | free muscle or myocutaneous flap with microvascular anastomosis | |
| 20955 | bone graft with microvascular anastomosis; fibula | |
| 20956 | bone graft with microvascular anastomosis; iliac crest | |
| 20969 | free osteocutaneous flap with microvascular anastomosis; other than iliac crest, metatarsal, or great toe | |
| 20970 | free osteocutaneous flap with microvascular anastomosis; iliac crest | |
| Other Reconstruction | Absence of reconstruction code listed above |
Figure 1.
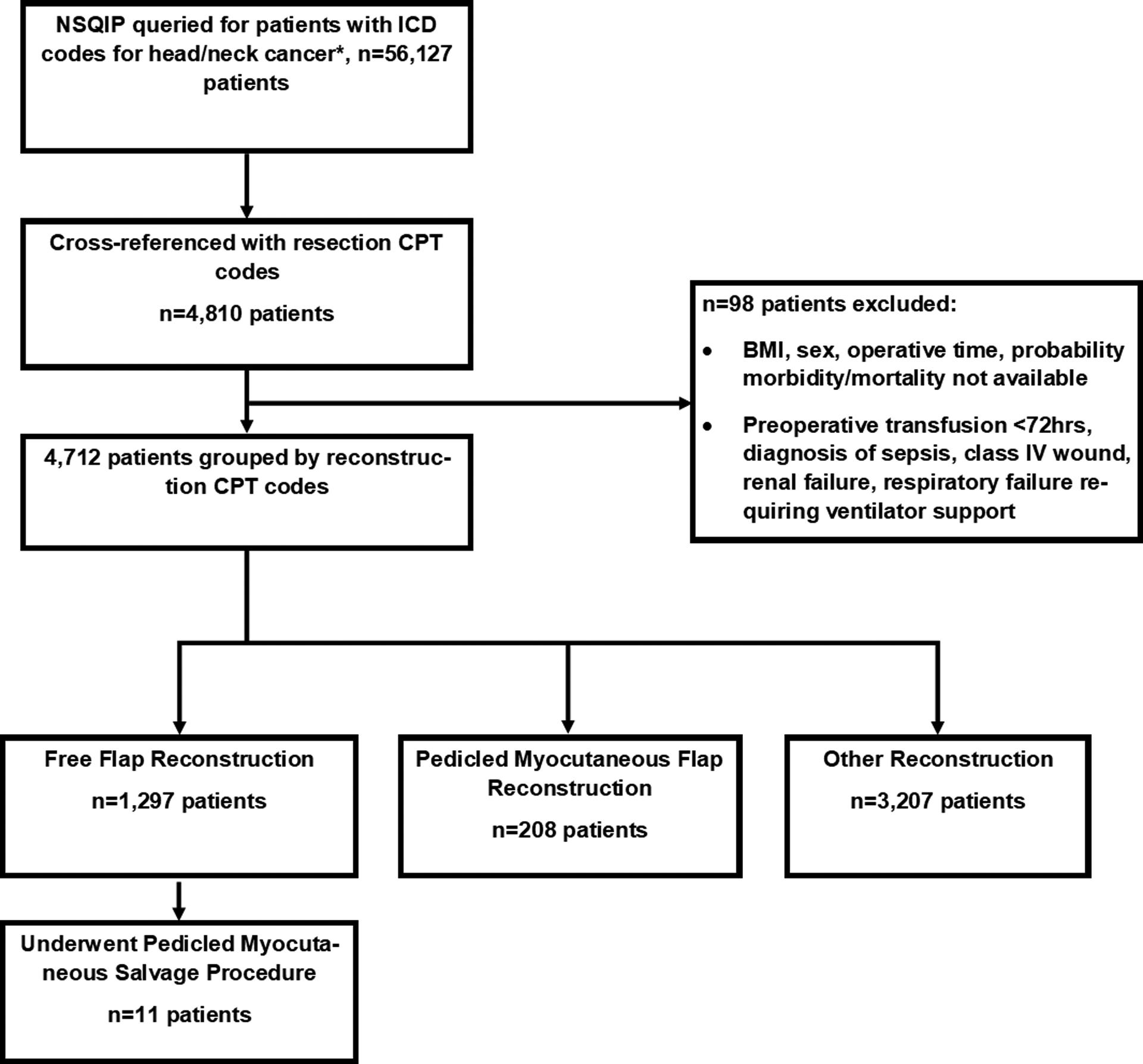
Flow chart of patients included from ACS-NSQIP database and group stratification.
Statistical Methods
All descriptive statistics were summarized using averages, standard deviations, and proportions. We used logistic regression models to compare binary outcomes and a generalized linear model (GLM) assuming a Gamma family and log link to compare length of stay (LOS). Given that patients undergoing pedicled flap reconstruction were more likely to have underlying comorbidities (Table 2), covariates were balanced using overlap propensity score weighting.17, 18 We estimated a propensity score from a multivariable logistic regression model containing the following defined ACS-NSQIP variables: age, body mass index (BMI), race, ethnicity, estimated probability of morbidity and mortality, diabetes, smoking, dyspnea, weight loss, preoperative functional health status, systemic sepsis, history of COPD, disseminated cancer, open wound/wound infection, steroid use, bleeding disorder, wound class, congestive heart failure (CHF) in 30 days before surgery and ASA class. We performed hypothesis testing bootstrap standard errors with fifty iterations. The bootstrap method accounted for the fact that the propensity score model was estimated and not known. We used free flap reconstruction as a reference category for all outcomes. P-values were based on comparison of odds ratios between pedicled flap and no or other reconstruction versus free flap. The odds ratio for pedicled flap versus other or no reconstruction can be obtained by division of their respective odds ratios with respect to free flap. Wilcoxon and Fisher’s exact test was used to compare outcomes between index pedicled flaps and pedicled flaps performed as a reoperative procedure. Results were considered significant if p-value was less than 0.05. SAS (V9.4) and STATA (Statacorp, College Station, TX) were used for analyses.
Table 2:
Unadjusted Patient Demographics
| Age | <0.001 | |||
| Mean (SD) | 60.74 (12.34) | 64.06 (10.75) | 62.61 (13.16) | |
| Median (Q1, Q3) | 61.0 (53.0, 69.0) | 65.0 (56.5, 71.0) | 63.0 (54.0, 71.0) | |
| BMI | <0.001 | |||
| Mean (SD) | 26.00 (6.42) | 24.15 (4.75) | 27.19 (6.40) | |
| Median (Q1, Q3) | 25.2 (21.6, 29.0) | 23.6 (20.7, 27.3) | 26.3 (22.9, 30.4) | |
| Estimated Probability of Mortality | 0.627 | |||
| Mean (SD) | −15.94 (36.42) | −15.22 (35.81) | −14.81 (35.33) | |
| Estimated Probability of Morbidity | 0.666 | |||
| Mean (SD) | −15.78 (36.49) | −15.04 (35.89) | −14.73 (35.36) | |
| Median (Q1, Q3) | 0.2 (0.1, 0.2) | 0.2 (0.1, 0.3) | 0.0 (0.0, 0.1) | |
| Ethnicity | 0.058 | |||
| Asian | 42 (3.2%) | 7 (3.4%) | 110 (3.4%) | |
| Black | 101 (7.8%) | 17 (8.2%) | 230 (7.2%) | |
| White | 969 (74.7%) | 172 (82.7%) | 2448 (76.3%) | |
| Other | 185 (14.3%) | 12 (5.8%) | 419 (13.1%) | |
| Diabetes | 0.012 | |||
| Insulin-Dependent | 44 (3.4%) | 8 (3.8%) | 148 (4.6%) | |
| Non-Insulin Dependent | 108 (8.3%) | 14 (6.7%) | 345 (10.8%) | |
| Smoking | 459 (35.4%) | 98 (47.1%) | 927 (28.9%) | <0.001 |
| Dyspnea | 118 (9.1%) | 40 (19.2%) | 289 (9.0%) | <0.001 |
| Independent Functional Status | 1273 (98.1%) | 200 (96.2%) | 3109 (96.9%) | 0.051 |
| >10% loss body weight in last 6 months | 155 (12.0%) | 22 (10.6%) | 146 (4.6%) | <0.001 |
| Preoperative SIRS Criteria | 9 (0.7%) | 3 (1.4%) | 33 (1.0%) | 0.440 |
| History of Severe COPD | 100 (7.7%) | 48 (23.1%) | 276 (8.6%) | <0.001 |
| Disseminated Cancer | 96 (7.4%) | 13 (6.3%) | 169 (5.3%) | 0.022 |
| Open wound/wound infection | 44 (3.4%) | 11 (5.3%) | 70 (2.2%) | 0.004 |
| Steroid use for chronic condition | 45 (3.5%) | 11 (5.3%) | 127 (4.0%) | 0.418 |
| Bleeding Disorder | 28 (2.2%) | 4 (1.9%) | 90 (2.8%) | 0.383 |
| CHF in 30d before surgery | 6 (0.5%) | 2 (1.0%) | 24 (0.7%) | 0.503 |
| ASA Class | <0.001 | |||
| 1 | 23 (1.8%) | 3 (1.4%) | 92 (2.9%) | |
| 2 | 245 (18.9%) | 17 (8.2%) | 1035 (32.3%) | |
| 3 | 922 (71.1%) | 158 (76.0%) | 1862 (58.1%) | |
| 4 | 107 (8.2%) | 30 (14.4%) | 218 (6.8%) |
Outcomes
Major surgical complications within 30 postoperative days included deep surgical site infections (fascia, muscle, or organ space infections), unplanned return to the operating room, and bleeding occurrences. Wound related complications were defined as wound dehiscence, superficial surgical site infections, deep wound infections, and organ space infections. Additionally, medical complications as defined by ACS-NSQIP endpoints included pneumonia, pulmonary embolism or deep venous thrombosis, postoperative renal insufficiency, urinary tract infections, stroke or cerebrovascular accidents, myocardial infections, deep, and sepsis or septic shock. We also compared mean operative time in minutes, hospital length-of-stay in days, days of postoperative mechanical ventilation greater than 48 hours, and hospital readmission within 30 days.
Results
Demographic Characteristics Associated with Type of Reconstruction
A total of 4,712 patients met inclusion criteria; 1,297 patients underwent reconstruction with a free flap, 208 patients had reconstruction with a myocutaneous pedicled flap, and 3,207 patients had other or no reconstruction performed. A total of 11 patients underwent pedicled flap within 30 days after free flap. The distribution of unadjusted patient demographic characteristics, functional status, and medical comorbidities is shown in Table 2 and 3. Patients who underwent pedicled flap reconstruction had a slightly higher mean age of 64 (60.7 for free flap and 62.6 for other reconstruction, p<0.001), lower BMI of 24±4.8 (26±6.42 for free flap, 27.2±6.4 for other reconstruction, p<0.001) , and were more likely to be smokers (<0.001), have a history of severe COPD (p<0.001), dyspnea (p<0.001), a higher ASA class of 3 or 4 (p<0.001), and more likely to have an open wound or wound infection preoperatively (5.3% for pedicled flap, 3.4% for free flap, and 2.2% for other reconstruction, p<0.01). There were no significant differences in terms of age, BMI, or comorbidities between patients who had a pedicled flap or a reoperative pedicled flap after free flap (Table 3). Patients who underwent free flap reconstruction were more likely to have disseminated cancer (7.4% vs 6.3% for pedicled flap and 5.3% for other reconstruction, p=0.022), or a >10% loss of body weight in the 6 months before surgery (12% vs 10.6% for pedicled, 4.6% for other reconstruction, p<0.001). Demographic characteristics after propensity score weighting were not significantly different between the three groups (Table 4).
Table 3:
Comparison Demographics and Outcomes Reoperative and Index Pedicled Flaps
| Age | 0.781 | ||
| Mean (SD) | 62.55 (12.24) | 64.06 (10.75) | |
| Median (Q1, Q3) | 65.0 (58, 68) | 65.0 (56.5, 71.0) | |
| BMI | 0.042 | ||
| Mean (SD) | 26.91 (4.50) | 24.15 (4.75) | |
| Median (Q1, Q3) | 26.2 (23.7, 31.7) | 23.6 (20.7, 27.3) | |
| Ethnicity | 0.749 | ||
| Asian | 0 (0%) | 7 (3.4%) | |
| Black | 1 (9.1%) | 17 (8.2%) | |
| White | 9 (81.8%) | 172 (82.7%) | |
| Other | 1 (9.1%) | 12 (5.8%) | |
| Diabetes | 0.147 | ||
| Insulin-Dependent | 1 (9.1%) | 8 (3.8%) | |
| Non-Insulin Dependent | 2 (18.3%) | 14 (6.7%) | |
| Smoking | 4 (36.4%) | 98 (47.1%) | 0.549 |
| Dyspnea | 1 (9.1%) | 40 (19.2%) | 0.694 |
| Independent Functional Status | 11 (100%) | 200 (96.2%) | 1.000 |
| >10% loss body weight in last 6 months | 3 (27.3%) | 22 (10.6%) | 0.117 |
| Preoperative SIRS Criteria | 0 (0%) | 3 (1.4%) | 1.000 |
| History of Severe COPD | 0 (0%) | 48 (23.1%) | 0.127 |
| Disseminated Cancer | 0 (0%) | 13 (6.3%) | 1.000 |
| Open wound/wound infection | 0 (0%) | 11 (5.3%) | 1.000 |
| Steroid use for chronic condition | 2 (18.2%) | 11 (5.3%) | 0.132 |
| Bleeding Disorder | 0 (0%) | 4 (1.9%) | 1.000 |
| CHF in 30d before surgery | 1 (9.1%) | 2 (1.0%) | 0.144 |
| ASA Class | 0.130 | ||
| 1 | 0 (0%) | 3 (1.4%) | |
| 2 | 3 (27.3%) | 17 (8.2%) | |
| 3 | 8 (72.7%) | 158 (76.0%) | |
| 4 | 0 (0%) | 30 (14.4%) | |
| Total Operative Time (min) | 0.011 | ||
| Mean (SD) | 541.73 (137.88) | 439.61 (146.34) | |
| Median (Q1, Q3) | 581.0 (454.0, 655.0) | 428.5 (344.5, 505.5) | |
| Wound classification | 0.778 | ||
| Clean | 0 (0%) | 19 (9.1%) | |
| Clean/Contaminated | 11 (100%) | 178 (85.6%) | |
| Contaminated | 0 (0.0%) | 11 (5.3%) | |
| Superficial Incisional SSI | 2 (18.2%) | 17 (8.2%) | 0.245 |
| Deep Incisional SSI | 1 (9.1%) | 12 (5.8%) | 0.498 |
| Organ Space SSI | 1 (9.1%) | 10 (4.8%) | 0.440 |
| Wound dehiscence | 5 (45.5%) | 18 (8.7%) | 0.003 |
| Pneumonia | 3 (27.3%) | 21 (10.1%) | 0.106 |
| Unplanned Intubation | 0 (0%) | 6 (2.9%) | 1.000 |
| Pulmonary Embolism | 1 (9.1%) | 1 (0.5%) | 0.098 |
| Mechanical Ventilation>48hrs | 1 (9.1%) | 5 (2.4%) | 0.269 |
| Progressive Renal Insufficiency | 0 (0.0%) | 1 (0.5%) | 1.000 |
| Urinary Tract Infection | 0 (0.0%) | 3 (1.4%) | 1.000 |
| Occurrences CVA | 0 (0.0%) | 1 (0.5%) | 1.000 |
| Cardiac Arrest | 2 (18.2%) | 3 (1.4%) | 0.021 |
| Myocardial Infarction | 1 (9.1%) | 2 (1.0%) | 0.144 |
| Bleeding requiring transfusion | 2 (18.2%) | 60 (28.8%) | 0.732 |
| DVT/Thrombophlebitis | 2 (18.2%) | 6 (2.9%) | 0.055 |
| Sepsis | 1 (9.1%) | 17 (8.2%) | 1.000 |
| Septic Shock | 0 (0.0%) | 5 (2.4%) | 1.000 |
| Composite DVT outcome | 3 (27.3%) | 7 (3.4%) | 0.009 |
| Composite Cardiac Outcome | 3 (27.3%) | 5 (2.4%) | 0.005 |
| Composite Infection Outcome | 3 (27.3%) | 49 (23.6%) | 0.725 |
|
Unplanned Reoperation
|
11 (100%) | 40 (19.2%) | <0.001 |
|
Hospital Readmission
|
6 (54.5%) | 29 (14.1%) | <0.001 |
Table 4:
Adjusted Demographics
| Age | |||
| Mean (SD) | 63.35 (11.45) | 63.48 (10.92) | 64.15 (11.68) |
| Median (Q1, Q3) | 63.0 (56.0, 71.0) | 64.0 (56.0, 70.0) | 64.0 (56.0, 72.0) |
| BMI | |||
| Mean (SD) | 24.54 (5.45) | 24.48 (4.70) | 24.61 (5.74) |
| Median (Q1, Q3) | 24.0 (20.8, 27.3) | 23.8 (21.0, 27.7) | 23.8 (20.7, 27.6) |
| Estimated Probability of Mortality | |||
| Mean (SD) | −18.10 (38.29) | −15.21 (35.80) | −16.03 (36.50) |
| Estimated Probability of Morbidity | |||
| Mean (SD) | −17.95 (38.37) | −15.05 (35.87) | −15.86 (36.57) |
| Median (Q1, Q3) | 0.2 (0.1, 0.2) | 0.2 (0.1, 0.2) | 0.2 (0.0, 0.3) |
| Ethnicity | |||
| Asian | 3.6% | 3.2% | 3.1% |
| Black | 8.7% | 8.4% | 8.7% |
| White | 6.6% | 6.9% | 7.4% |
| Other | 81.1% | 81.5% | 80.7% |
| Diabetes | |||
| Insulin-Dependent | 3.9% | 3.5% | 4.2% |
| Non-Insulin Dependent | 7.1% | 7.6% | 7.5% |
| Smoking | 43.4% | 42.8% | 44.1% |
| Dyspnea | 16.0% | 15.6% | 15.3% |
| Independent Functional Status | 97.2% | 96.8% | 96.5% |
| >10% loss body weight in last 6 months | 10.8% | 10.6% | 11.2% |
| Preoperative SIRS Criteria | 1.1% | 1.2% | 1.7% |
| History of Severe COPD | 17.7% | 16.4% | 17.5% |
| Disseminated Cancer | 7.3% | 6.5% | 5.7% |
| Open wound/wound infection | 4.5% | 3.7% | 4.4% |
| Steroid use for chronic condition | 4.6% | 4.5% | 5.7% |
| Bleeding Disorder | 2.2% | 1.7% | 2.4% |
| CHF in 30d before surgery | 0.7% | 0.8% | 0.8% |
| ASA Class | |||
| 1 | 1.6% | 1.4% | 1.4% |
| 2 | 10.9% | 10.5% | 9.5% |
| 3 | 75.7% | 75.9% | 77.0% |
| 4 | 11.9% | 12.2% | 12.1% |
Postoperative Outcomes
Unadjusted postoperative outcomes are reported in Table 5. Patients undergoing pedicled myocutaneous flaps were more likely to have a contaminated wound class (5.3% vs 2.2% for free flap, 2.5% for other reconstruction) and had a higher incidence of all three types of surgical site infection, wound dehiscence, pneumonia, DVT, sepsis, septic shock, and hospital readmission compared with those undergoing a free flap or other reconstruction (p<0.001, Figure 2). In comparison to index pedicled flaps, patients who had a reoperative pedicled flap after initial free flap had a longer mean operative time (541.73±137.88 vs 439.61±146.34 min, p=0.011), higher rate of wound dehiscence (45.5% vs 8.7%, p=0.003), cardiac arrest (18.2% vs 1.4%, p=0.021), DVT (18.2% vs 2.9%, p=0.055), and hospital readmission (54.5% vs 14.1%, p<0.001). After propensity score weighting, patients undergoing pedicled flap reconstruction were found to be at higher risk of developing a DVT or thrombophlebitis (OR=2.64, p=0.045), sepsis (OR=2.95, p=0.001), or developing any infection (OR=2.03, p<0.01, Figure 3) compared to those undergoing free flap reconstruction. However, patients who underwent pedicled flaps had a lower incidence of mechanical ventilation after 48hrs (OR=0.33, p=0.035) or having bleeding complications requiring a transfusion (OR=0.65, p=0.002) compared to those undergoing free flap reconstruction. Patients who underwent free flap reconstruction had a longer adjusted mean operative time compared to those who underwent pedicled flaps or other reconstruction (578.3±165.8 for free flap vs 440.1±147.8 pedicled flap, 326.1±198.7 for other, p<0.001, Figure 4).
Table 5:
Unadjusted Postoperative Outcomes
| Total Operative Time (min) | <0.001 | |||
| Mean (SD) | 573.91 (168.99) | 439.61 (146.34) | 232.96 (189.75) | |
| Median (Q1, Q3) | 562.0 (458.0, 675.0) | 428.5 (344.5, 505.5) | 194.0 (70.0, 343.0) | |
| Wound classification | 0.038 | |||
| Clean | 114 (8.8%) | 19 (9.1%) | 335 (10.4%) | |
| Clean/Contaminated | 1155 (89.1%) | 178 (85.6%) | 2791 (87.0%) | |
| Contaminated | 28 (2.2%) | 11 (5.3%) | 81 (2.5%) | |
| Superficial Incisional SSI | 83 (6.4%) | 17 (8.2%) | 91 (2.8%) | <0.001 |
| Deep Incisional SSI | 58 (4.5%) | 12 (5.8%) | 53 (1.7%) | <0.001 |
| Organ Space SSI | 29 (2.2%) | 10 (4.8%) | 29 (0.9%) | <0.001 |
| Wound dehiscence | 65 (5.0%) | 18 (8.7%) | 71 (2.2%) | <0.001 |
| Pneumonia | 92 (7.1%) | 21 (10.1%) | 89 (2.8%) | <0.001 |
| Unplanned Intubation | 44 (3.4%) | 6 (2.9%) | 34 (1.1%) | <0.001 |
| Pulmonary Embolism | 8 (0.6%) | 1 (0.5%) | 8 (0.2%) | 0.169 |
| Mechanical Ventilation>48hrs | 88 (6.8%) | 5 (2.4%) | 55 (1.7%) | <0.001 |
| Progressive Renal Insufficiency | 3 (0.2%) | 1 (0.5%) | 3 (0.1%) | 0.247 |
| Urinary Tract Infection | 22 (1.7%) | 3 (1.4%) | 29 (0.9%) | 0.071 |
| Occurrences CVA | 4 (0.3%) | 1 (0.5%) | 5 (0.2%) | 0.416 |
| Cardiac Arrest | 15 (1.2%) | 3 (1.4%) | 12 (0.4%) | 0.004 |
| Myocardial Infarction | 11 (0.8%) | 2 (1.0%) | 9 (0.3%) | 0.023 |
| Bleeding requiring transfusion | 427 (32.9%) | 60 (28.8%) | 199 (6.2%) | <0.001 |
| DVT/Thrombophlebitis | 17 (1.3%) | 6 (2.9%) | 14 (0.4%) | <0.001 |
| Sepsis | 45 (3.5%) | 17 (8.2%) | 48 (1.5%) | <0.001 |
| Septic Shock | 6 (0.5%) | 5 (2.4%) | 8 (0.2%) | <0.001 |
| Composite DVT outcome | 24 (1.9%) | 7 (3.4%) | 20 (0.6%) | <0.001 |
| Composite Cardiac Outcome | 27 (2.1%) | 5 (2.4%) | 23 (0.7%) | <0.001 |
| Composite Infection Outcome | 186 (14.3%) | 49 (23.6%) | 199 (6.2%) | <0.001 |
| Unplanned Reoperation | 266 (20.5%) | 40 (19.2%) | 213 (6.6%) | <0.001 |
| Hospital Readmission | 141 (11.1%) | 29 (14.1%) | 252 (8.0%) | <0.001 |
Figure 2.
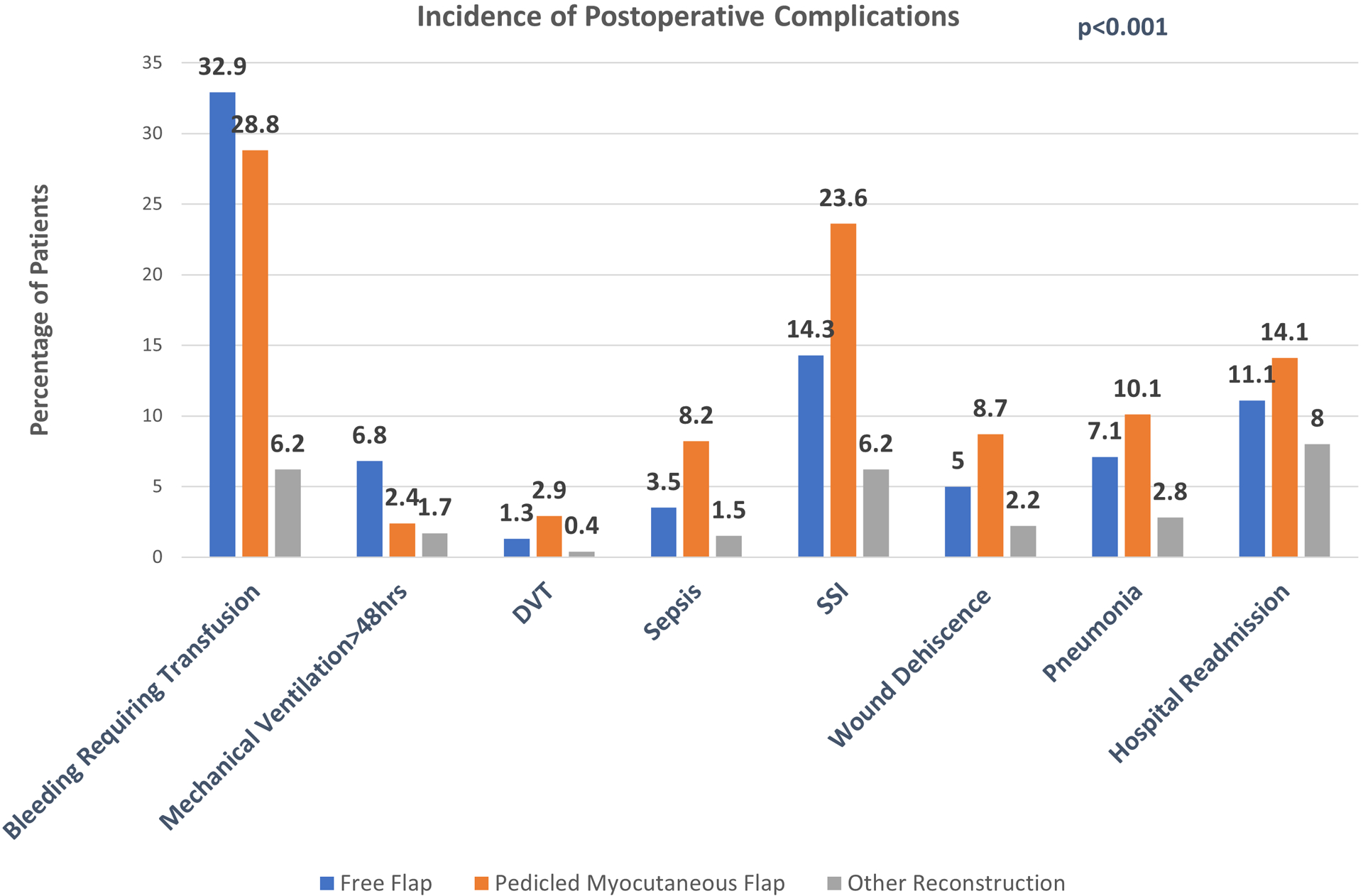
Unadjusted postoperative complication rates of three reconstructive groups.
Figure 3.
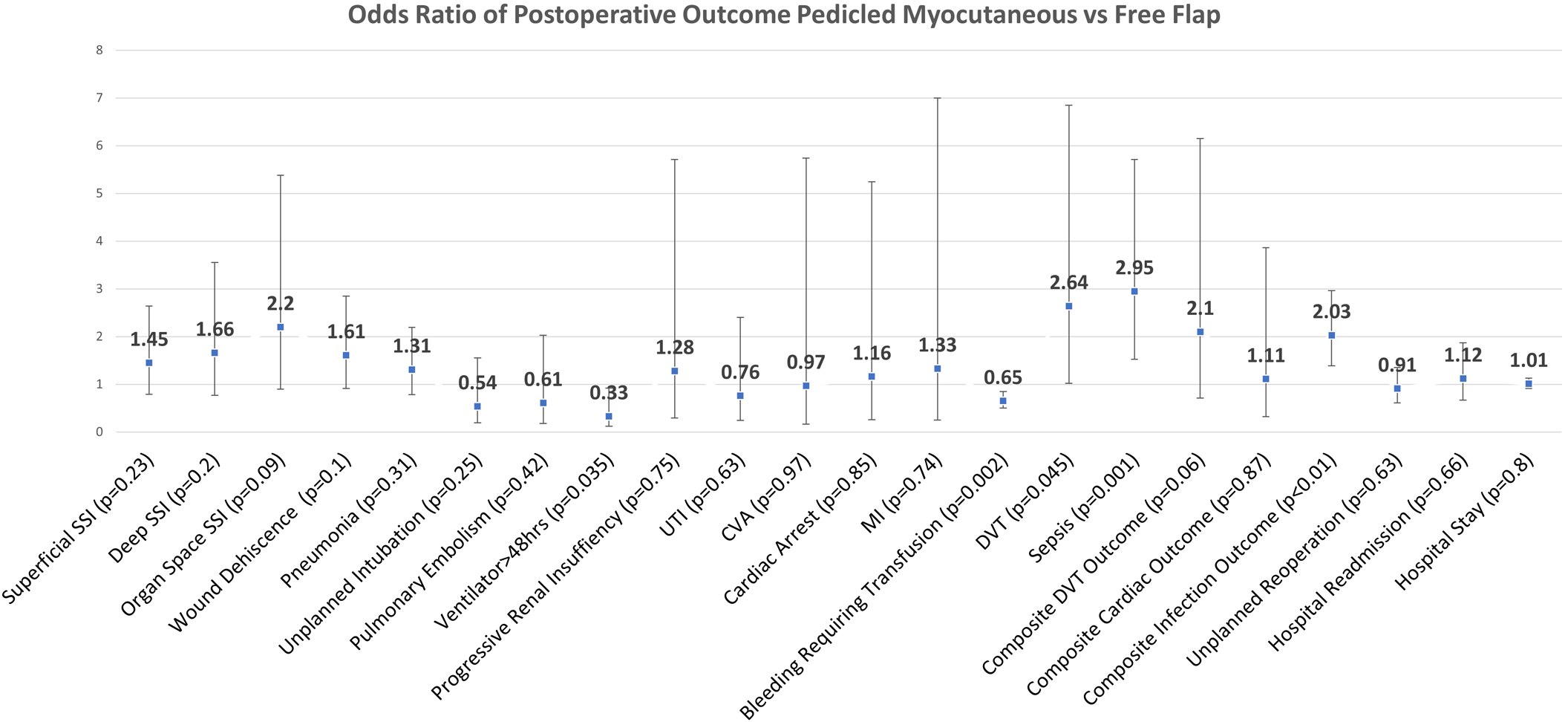
Odds ratios of postoperative complications for pedicled flap compared to free flap after propensity score matching.
Figure 4.
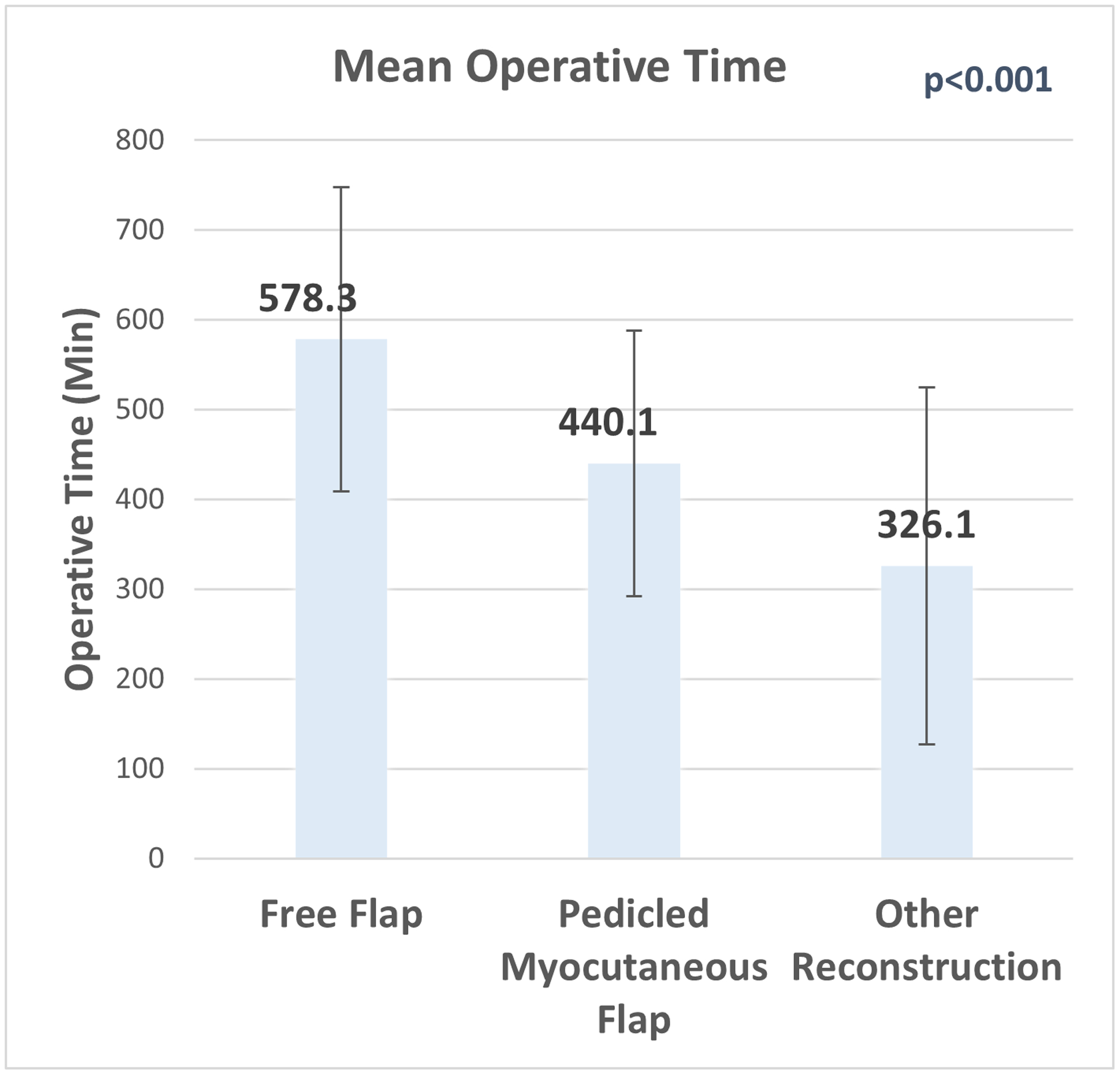
Mean operative time of three reconstructive groups.
Discussion
Advances in plastic surgery in the past two decades have allowed radical resection of head and neck cancer to be performed with the realistic expectation of returning form and function.19 Patients with head and neck cancer present distinct challenges to reconstruction, as local tissue for primary closure or rearrangement is often scarce and many patients require aggressive irradiation, emphasizing the need for a well-vascularized tissue reconstruction to minimize wound complications.19, 20 In this study, we compared postoperative outcomes between patients with head and neck cancer who underwent a major resection and reconstruction with free tissue transfer, pedicled myocutaneous flap reconstruction or non-flap based reconstruction. Options for myocutaneous pedicled flap reconstruction in the groups defined by CPT code included muscle flaps such as pedicled pectoralis major flap, temporalis muscle flap as well as fasciocutaneous flaps such as submental artery perforator and subclavicular flap.21, 22 Primary closure and adjacent tissue transfer were captured in the “other reconstruction” group. Previous literature supports free tissue transfer as the gold standard for hemiglossectomy, laryngectomy, maxillectomy, segmental mandibulectomy and other large composite defects22, and these typically include options such as the anterolateral thigh flap, radial forearm flap, rectus abdominis flap, latissimus dorsi flap, free fibula flap and several others.11 However, some centers continue to report a high success rate and good functional outcomes with certain pedicled flaps such as the supraclavicular artery and submental island flaps, especially elderly patients with severe medical comorbidities.23–26 Although defects can both be treated by combination of pedicled flaps or free tissue transfer, however these patients were excluded to prevent potential confounding of our postoperative outcome analysis.9 Factors affecting decision making in these cases include surgeon preference, facility capability and patient factors.
In this study, we found several important demographic differences between the three reconstruction groups. Patients who underwent pedicled myocutaneous flap reconstruction were typically slightly older and had more medical comorbidities, most notably higher incidence of smoking, COPD, higher ASA class, and open wound or wound infection. These factors likely play an important role in patient selection for myocutaneous vs free flap reconstruction based on the ability of the patient to tolerate a longer, more complex procedure. Additionally, patients that had free flap reconstruction were more likely to have disseminated cancer or weight loss in the six months preceding surgery, likely correlating to a greater disease burden that would require more extensive resection and reconstruction of a larger defect.
Patients who underwent pedicled flap reconstruction had a higher incidence of DVT, surgical site infection, wound dehiscence, pneumonia, sepsis, septic shock, and hospital readmission compared to free flap patients. Though this is at least partly explained by the higher medical comorbidity status of the pedicled flap group, after matching for patient and disease-specific factors, we found that patients who underwent pedicled flap reconstruction continued to have nearly twice the risk of developing DVT, sepsis, or any infection compared to patients undergoing free flap reconstruction. Though the reasons for this are not entirely clear, it is likely that patients undergoing pedicled flaps in this patient population had other disease-specific factors which influence flap selection and are not accounted for by our propensity score analysis, such as chemotherapy, radiation status, cancer recurrence, or previous flap failure. In a study by Mathieu et al, patients who underwent pedicled flap reconstruction after were more likely to a have unsuitable vessels for a microsurgical anastomosis as a result of prior treatment for head and neck cancer or radiation, were usually older and had more comorbidities.27 Previous reports comparing incidence of postoperative complications between free flaps and pedicled flaps for head and neck cancer reconstruction have generally focused on specific flap types and donor or recipient site complications, without reporting differences in specific outcome measures such as DVT, pneumonia, or sepsis.12, 28–32 A study of the NSQIP database from 2005–2011 by Kim et al found that among 213 patients undergoing reconstruction for pharyngolaryngeal defects, 162 of whom had free flaps and 51 who had pedicled flaps, incidence of complications such as PE, prolonged intubation time, renal failure, MI, transfusion or sepsis was higher among the pedicled flap group while there was no difference in pneumonia, reintubation, UTI or DVT.33 Importantly, this study predominantly focused on comparing outcomes between flap and non-flap based reconstruction groups and excluded osseous and osteocutaneous flaps for mandibulectomy and maxillary defects, while also grouping complications into either major or minor types rather than evaluating differences in specific 30 day outcomes. Nonetheless, the authors generally found increased wound and post-surgical morbidity associated with pedicled flaps, which was substantiated in prior single-institution studies.34–36
Free flap reconstruction was associated with a higher incidence of prolonged mechanical ventilation and bleeding requiring transfusion compared to pedicled flaps. These differences likely attest to the higher complexity of the case, longer operative time, possible need for tracheostomy with reconstruction of large defects, and technical considerations of performing a microvascular anastomosis in free flap reconstruction. Increased operative time has been shown to be an independent predictor of both increased transfusion requirement and prolonged need for mechanical ventilation in other studies of the NSQIP database.14, 37, 38 Despite the increased complexity of the procedure however, it is important to note that the risk of a large number of important outcomes we studied, including second unplanned operation, reintubation, wound dehiscence, cardiac complications, 30 day hospital readmission, and hospital length of stay were not significantly different between free flap and pedicled flap reconstruction. This data further confirm that free tissue transfer is superior to pedicled flap reconstruction and can be safely performed without increased morbidity in experienced hands.
There are several limitations to our study inherent to its reliance on a large national database. We have already noted that selection bias has the potential to cause differences in patient risk factors between groups in this study. Patients who are healthier, can tolerate longer surgeries, have larger defects, or require more complex reconstructions are more likely to have been selected for free flap reconstruction over myocutaneous flap or other reconstruction. Propensity score weighting was used to account for differences in patient comorbidities but cannot not fully address factors that are missing in the NSQIP database such as size and exact location of defect, if patients had chemotherapy/radiation, or the experience of the facility where patients were treated in regard to free tissue reconstruction. Such factors undoubtedly play a role in the choice of reconstruction based on surgical risk and goals in terms of restoration of tissue integrity versus optimizing form and function. Additionally, surgeon experience, case volume, and specialty have been found to profoundly affect overall outcomes with free tissue transfer, with 30-day complications such as SSI, wound dehiscence, and bleeding complications notably lower for patients treated by plastic surgeons.39, 40 Myocutaneous flaps may in some cases serve as a salvage procedure after free tissue transfer. We narrowed the terms of our query to select pedicled flaps based on CPT code for the index operation, however it is possible that some flaps were misclassified as an index rather than a salvage procedure by clinical reviewers or occurred as a salvage procedure after 30 days. However, a previous study suggested that the majority of reoperations for head and neck free flaps occur early on from 4.9 days for hematoma to 13.5 days for dehiscence, so it is reasonable that our query was able to identify a majority of cases where a pedicled flap was used to salvage a failed free flap.41 Moreover, the overall incidence of wound dehiscence among free flaps in our study was relatively low at 5%, comparable to prior studies.33, 34, 36, 42 Given the limited number of patients we identified in the database that had a pedicled flap after free flap, it is difficult to draw definite conclusions about this particular group. Nonetheless, despite these limitations, we were able to use a large, multi-institutional patient cohort that offers standardized data on postoperative outcomes and provides a high level of statistical power for comparing outcomes among different reconstruction types while adjusting for patient and disease-specific morbidities.
Conclusion
Our data highlights some of the important differences in complication rates between patients undergoing free versus pedicled flap reconstruction for head and neck reconstruction. The optimal reconstruction choice for any given patient will require consideration of many patient-specific and systemic factors. This study makes use of a large, multi-institutional database to substantiate established data on the safety profile of free tissue transfer compared to other types of reconstruction, and more importantly it highlights areas for continued improvement such as optimizing system-based practices to decrease operative time and the importance of DVT prophylaxis.
Table 6:
Adjusted Postoperative Outcomes
| Total Operative Time (min) | |||
| Mean (SD) | 578.30 (165.76) | 440.14 (147.76) | 326.08 (198.73) |
| Median (Q1, Q3) | 569.0 (468.0, 674.0) | 428.0 (345.0, 500.0) | 309.0 (170.0, 455.0) |
| Wound classification | |||
| Clean | 10.9% | 9.8% | 9.7% |
| Clean/Contaminated | 85.3% | 86.3% | 86.5% |
| Contaminated | 3.8% | 3.9% | 3.9% |
| Superficial Incisional SSI | 5.4% | 7.7% | 4.6% |
| Deep Incisional SSI | 3.8% | 6.1% | 3.9% |
| Organ Space SSI | 2.3% | 4.9% | 1.8% |
| Wound dehiscence | 4.9% | 7.7% | 4.9% |
| Pneumonia | 7.5% | 9.6% | 5.8% |
| Unplanned Intubation | 3.9% | 2.1% | 1.5% |
| Pulmonary Embolism | 0.5% | 0.3% | 0.2% |
| Mechanical Ventilation>48hrs | 6.9% | 2.4% | 3.8% |
| Progressive Renal Insufficiency | 0.2% | 0.3% | 0.1% |
| Urinary Tract Infection | 1.6% | 1.2% | 1.4% |
| Occurrences CVA | 0.3% | 0.3% | 0.3% |
| Cardiac Arrest | 1.0% | 1.2% | 1.1% |
| Myocardial Infarction | 0.6% | 0.8% | 0.4% |
| Bleeding requiring transfusion | 36.3% | 27.0% | 14.5% |
| DVT/Thrombophlebitis | 1.0% | 2.7% | 0.7% |
| Sepsis | 3.1% | 8.7% | 3.1% |
| Septic Shock | 0.5% | 2.3% | 0.7% |
| Composite DVT outcome | 1.5% | 3.0% | 0.9% |
| Composite Cardiac Outcome | 1.8% | 2.0% | 1.8% |
| Composite Infection Outcome | 13.0% | 23.3% | 11.8% |
| Unplanned Reoperation | 19.8% | 18.3% | 10.6% |
Acknowledgements:
Statistical work for this project was supported through the National Institutes of Health National Cancer Institute (Grant #P30CA006927)
Footnotes
Conflict of Interest: The authors report no conflicts of interest and have no relevant disclosures regarding this manuscript. The manuscript represents original work that is not being considered or has been accepted for publication elsewhere. All authors have reviewed and approved the final version of this manuscript.
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Presented At:
American Society of Plastic Surgeons, Virtual Plastic Surgery The Meeting, October 16–18th, 2020
Robert H. Ivy Society of Plastic Surgery, Annual Virtual Scientific Meeting, November 7th, 2020
References:
- 1.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. Jan 2017;67(1):7–30. doi: 10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- 2.Gurtner GC, Evans GR. Advances in head and neck reconstruction. Plast Reconstr Surg. Sep 2000;106(3):672–82; quiz 683. [PubMed] [Google Scholar]
- 3.Chim H, Salgado CJ, Seselgyte R, Wei FC, Mardini S. Principles of head and neck reconstruction: an algorithm to guide flap selection. Semin Plast Surg. May 2010;24(2):148–54. doi: 10.1055/s-0030-1255332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel SA, Chang EI. Principles and practice of reconstructive surgery for head and neck cancer. Surg Oncol Clin N Am. Jul 2015;24(3):473–89. doi: 10.1016/j.soc.2015.03.005 [DOI] [PubMed] [Google Scholar]
- 5.Hurvitz KA, Kobayashi M, Evans GR. Current options in head and neck reconstruction. Plast Reconstr Surg. Oct 2006;118(5):122e–133e. doi: 10.1097/01.prs.0000237094.58891.fb [DOI] [PubMed] [Google Scholar]
- 6.Abouyared M, Katz AP, Ein L, et al. Controversies in free tissue transfer for head and neck cancer: A review of the literature. Head Neck. 09 2019;41(9):3457–3463. doi: 10.1002/hed.25853 [DOI] [PubMed] [Google Scholar]
- 7.Wong CH, Wei FC. Microsurgical free flap in head and neck reconstruction. Head Neck. Sep 2010;32(9):1236–45. doi: 10.1002/hed.21284 [DOI] [PubMed] [Google Scholar]
- 8.Lyons AJ. Perforator flaps in head and neck surgery. Int J Oral Maxillofac Surg. Mar 2006;35(3):199–207. doi: 10.1016/j.ijom.2005.07.015 [DOI] [PubMed] [Google Scholar]
- 9.Kim EK, Evangelista M, Evans GR. Use of free tissue transfers in head and neck reconstruction. J Craniofac Surg. Nov 2008;19(6):1577–82. doi: 10.1097/SCS.0b013e3181897376 [DOI] [PubMed] [Google Scholar]
- 10.McCarthy CM, Cordeiro PG. Microvascular reconstruction of oncologic defects of the midface. Plast Reconstr Surg. Dec 2010;126(6):1947–59. doi: 10.1097/PRS.0b013e3181f446f1 [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal E, Carroll W, Dobbs M, Scott Magnuson J, Wax M, Peters G. Simplifying head and neck microvascular reconstruction. Head Neck. Nov 2004;26(11):930–6. doi: 10.1002/hed.20076 [DOI] [PubMed] [Google Scholar]
- 12.Gabrysz-Forget F, Tabet P, Rahal A, Bissada E, Christopoulos A, Ayad T. Free versus pedicled flaps for reconstruction of head and neck cancer defects: a systematic review. J Otolaryngol Head Neck Surg. Mar 2019;48(1):13. doi: 10.1186/s40463-019-0334-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American College of Surgeons Quality Improvement Program Participant Data Use File. www.facs.org/quality-programs/acsnsqip)
- 14.Brady JS, Desai SV, Crippen MM, et al. Association of Anesthesia Duration With Complications After Microvascular Reconstruction of the Head and Neck. JAMA Facial Plast Surg. May 2018;20(3):188–195. doi: 10.1001/jamafacial.2017.1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brady JS, Govindan A, Crippen MM, et al. Impact of diabetes on free flap surgery of the head and neck: A NSQIP analysis. Microsurgery. Jul 2018;38(5):504–511. doi: 10.1002/micr.30276 [DOI] [PubMed] [Google Scholar]
- 16.Raval MV, Pawlik TM. Practical Guide to Surgical Data Sets: National Surgical Quality Improvement Program (NSQIP) and Pediatric NSQIP. JAMA Surg. August 2018;153(8):764–765. doi: 10.1001/jamasurg.2018.0486 [DOI] [PubMed] [Google Scholar]
- 17.Thomas LE, Li F, Pencina MJ. Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial. JAMA. Jun 16 2020;323(23):2417–2418. doi: 10.1001/jama.2020.7819 [DOI] [PubMed] [Google Scholar]
- 18.Li F, Thomas LE, Li F. Addressing Extreme Propensity Scores via the Overlap Weights. Am J Epidemiol. Jan 1 2019;188(1):250–257. doi: 10.1093/aje/kwy201 [DOI] [PubMed] [Google Scholar]
- 19.McCarthy JG, Galiano RD, Boutros SG. Current therapy in plastic surgery. 1st ed. Saunders/Elsevier; 2006:xxii, 710 p. [Google Scholar]
- 20.Jose B, Banis J, Flynn M, et al. Irradiation and free tissue transfer in head and neck cancer. Head Neck. 1991 May-Jun 1991;13(3):213–6. doi: 10.1002/hed.2880130308 [DOI] [PubMed] [Google Scholar]
- 21.Liu M, Liu W, Yang X, Guo H, Peng H. Pectoralis Major Myocutaneous Flap for Head and Neck Defects in the Era of Free Flaps: Harvesting Technique and Indications. Sci Rep. 04 2017;7:46256. doi: 10.1038/srep46256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cordeiro PG, Santamaria E. A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg. Jun 2000;105(7):2331–46; discussion 2347–8. doi: 10.1097/00006534-200006000-00004 [DOI] [PubMed] [Google Scholar]
- 23.Paydarfar JA, Patel UA. Submental island pedicled flap vs radial forearm free flap for oral reconstruction: comparison of outcomes. Arch Otolaryngol Head Neck Surg. Jan 2011;137(1):82–7. doi: 10.1001/archoto.2010.204 [DOI] [PubMed] [Google Scholar]
- 24.Anand AG, Tran EJ, Hasney CP, Friedlander PL, Chiu ES. Oropharyngeal reconstruction using the supraclavicular artery island flap: a new flap alternative. Plast Reconstr Surg. Feb 2012;129(2):438–441. doi: 10.1097/PRS.0b013e31823aebce [DOI] [PubMed] [Google Scholar]
- 25.Chiu ES, Liu PH, Friedlander PL. Supraclavicular artery island flap for head and neck oncologic reconstruction: indications, complications, and outcomes. Plast Reconstr Surg. Jul 2009;124(1):115–123. doi: 10.1097/PRS.0b013e3181aa0e5d [DOI] [PubMed] [Google Scholar]
- 26.Deganello A, Gitti G, Parrinello G, et al. Infrahyoid flap reconstruction of oral cavity and oropharyngeal defects in elderly patients with severe general comorbidities. Head Neck. Sep 2012;34(9):1299–305. doi: 10.1002/hed.21913 [DOI] [PubMed] [Google Scholar]
- 27.Mahieu R, Colletti G, Bonomo P, et al. Head and neck reconstruction with pedicled flaps in the free flap era. Acta Otorhinolaryngol Ital. Dec 2016;36(6):459–468. doi: 10.14639/0392-100X-1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geiger EJ, Basques BA, Chang CC, et al. Pedicle versus free flap reconstruction in patients receiving intraoperative brachytherapy. J Plast Surg Hand Surg. Aug 2016;50(4):227–32. doi: 10.3109/2000656x.2016.1152974 [DOI] [PubMed] [Google Scholar]
- 29.Zhang S, Chen W, Cao G, Dong Z. Pedicled Supraclavicular Artery Island Flap Versus Free Radial Forearm Flap for Tongue Reconstruction Following Hemiglossectomy. J Craniofac Surg. Sep 2015;26(6):e527–30. doi: 10.1097/scs.0000000000002031 [DOI] [PubMed] [Google Scholar]
- 30.Kroll SS, Reece GP, Miller MJ, Schusterman MA. Comparison of the rectus abdominis free flap with the pectoralis major myocutaneous flap for reconstructions in the head and neck. Am J Surg. Dec 1992;164(6):615–8. doi: 10.1016/s0002-9610(05)80719-6 [DOI] [PubMed] [Google Scholar]
- 31.Mallet Y, El Bedoui S, Penel N, Ton Van J, Fournier C, Lefebvre JL. The free vascularized flap and the pectoralis major pedicled flap options: comparative results of reconstruction of the tongue. Oral Oncol. Dec 2009;45(12):1028–31. doi: 10.1016/j.oraloncology.2009.05.639 [DOI] [PubMed] [Google Scholar]
- 32.Howard BE, Nagel TH, Barrs DM, Donald CB, Hayden RE. Reconstruction of Lateral Skull Base Defects: A Comparison of the Submental Flap to Free and Regional Flaps. Otolaryngol Head Neck Surg. 06 2016;154(6):1014–8. doi: 10.1177/0194599816634296 [DOI] [PubMed] [Google Scholar]
- 33.Kim K, Ibrahim AM, Koolen PG, Frankenthaler RA, Lin SJ. Analysis of the NSQIP database in 676 patients undergoing laryngopharyngectomy: the impact of flap reconstruction. Otolaryngol Head Neck Surg. Jan 2014;150(1):87–94. doi: 10.1177/0194599813511785 [DOI] [PubMed] [Google Scholar]
- 34.Bertino G, Spasiano R, Mazzola I, Benazzo M. The use of pedicled and free flaps in laryngeal cancer recurrences: postoperative considerations and functional results. Ann Plast Surg. Oct 2005;55(4):384–8. doi: 10.1097/01.sap.0000178814.73683.30 [DOI] [PubMed] [Google Scholar]
- 35.Clark JR, Gilbert R, Irish J, Brown D, Neligan P, Gullane PJ. Morbidity after flap reconstruction of hypopharyngeal defects. Laryngoscope. Feb 2006;116(2):173–81. doi: 10.1097/01.mlg.0000191459.40059.fd [DOI] [PubMed] [Google Scholar]
- 36.Teknos TN, Myers LL, Bradford CR, Chepeha DB. Free tissue reconstruction of the hypopharynx after organ preservation therapy: analysis of wound complications. Laryngoscope. Jul 2001;111(7):1192–6. doi: 10.1097/00005537-200107000-00011 [DOI] [PubMed] [Google Scholar]
- 37.Cannady SB, Hatten KM, Bur AM, et al. Use of free tissue transfer in head and neck cancer surgery and risk of overall and serious complication(s): An American College of Surgeons-National Surgical Quality Improvement Project analysis of free tissue transfer to the head and neck. Head Neck. 04 2017;39(4):702–707. doi: 10.1002/hed.24669 [DOI] [PubMed] [Google Scholar]
- 38.Offodile AC, Aherrera A, Wenger J, Rajab TK, Guo L. Impact of increasing operative time on the incidence of early failure and complications following free tissue transfer? A risk factor analysis of 2,008 patients from the ACS-NSQIP database. Microsurgery. Jan 2017;37(1):12–20. doi: 10.1002/micr.22387 [DOI] [PubMed] [Google Scholar]
- 39.Drinane JJ, Drinane J, Nair L, Patel A. Head and Neck Reconstruction: Does Surgical Specialty Affect Complication Rates? J Reconstr Microsurg. Sep 2019;35(7):516–521. doi: 10.1055/s-0039-1688711 [DOI] [PubMed] [Google Scholar]
- 40.Zhang JX, Wan M, Ding Y, et al. Do Microsurgical Outcomes Differ Based on Which Specialty Does the Operation? A NSQIP Analysis. Plast Reconstr Surg Glob Open. Apr 2020;8(4):e2769. doi: 10.1097/GOX.0000000000002769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chattha AS, Baltodano PA, Chen AD, Ata A, Patel A. Analysis of Post-Operative Reoperation Timing and Risk Factors for Post-Operative Free Flap Compromise in Head and Neck Reconstruction: A National Retrospective Cohort. Plast Reconstr Surg Glob Open. 2017;5(9 Suppl):9–10. [Google Scholar]
- 42.van der Putten L, Spasiano R, de Bree R, Bertino G, Leemans CR, Benazzo M. Flap reconstruction of the hypopharynx: a defect orientated approach. Acta Otorhinolaryngol Ital. Oct 2012;32(5):288–96. [PMC free article] [PubMed] [Google Scholar]


