Abstract
Orthognathic surgery has an undeniable functional effect, but the aesthetic result must not be disregarded, especially since many patients visit the surgeon precisely because of an aesthetic complaint and ignore the practical benefits. The aim of this paper is to discuss about an ideal treatment that combines this functional improvement with facial aesthetics and improves it after the operation. In order to predict which aesthetic deficits may occur, a facial analysis is essential. As precise as the virtual planning may be, there is still no exact predictability of soft tissue behavior. Some non-surgical procedures can help the surgeon achieve a result that better meets the patients' expectations. Imaging exams, photographs, facial analyzes, and patient complaints are essential to assess the possibility of any postoperative refinement. The entire surgical planning is discussed with the patient; the possibility of refinement must be part of the treatment plan. The surgeon's focus is on the functional correction of the dentofacial deformity, but the aesthetic outcome is essential for the patient. The results of this study suggest that refinement should be part of the treatment plan.
Keywords: Dermal fillers, Lifting, Orthognathic surgery, Rejuvenation, Sutures
الملخص
تعتبر جراحة تقويم الفكين ذات تأثير وظيفي لا يمكن إنكاره. ومع ذلك، يجب عدم تجاهل الجانب الجمالي لجراحة تقويم الفكين، حيث يستشير العديد من المرضى الجراحين على وجه التحديد للحصول على علاج جمالي ويتجاهلون فوائدها العملية. تناقش هذه الورقة العلاج المثالي الذي يجمع بين التحسينات الوظيفية وجماليات الوجه في جراحة تقويم الفكين. من أجل التنبؤ بالعجز الجمالي الذي قد يحدث، من الضروري إجراء تحليل للوجه. رغم دقة التخطيط الافتراضي، لا يوجد حتى الآن إمكانية للتنبؤ الدقيق بسلوك الأنسجة الرخوة. حيث يمكن لبعض الإجراءات غير الجراحية أن تساعد الجراحين في تحقيق نتيجة تلبي توقعات المرضى عن كثب. تعد فحوصات التصوير، والصور وتحليلات الوجه، وشكاوى المرضى ضرورية لتقييم إمكانية أي تعديلات بعد الجراحة. كما يجب مناقشة التخطيط الجراحي بالكامل مع المريض ويجب أن تكون إمكانية التعديل بعد الجراحة جزءا لا يتجزأ من خطة العلاج. يركز الجراحون بشكل أساسي على التصحيح الوظيفي لتشوه الوجه السني، ولكن النتيجة الجمالية مهمة للمريض. تشير نتائج هذه الدراسة إلى أنه يجب مراعاة التحسين كجزء من خطة العلاج.
الكلمات المفتاحية: حشو جلدي, رفع, جراحة تقويم الفكين, تجديد, الغرز
Introduction
Facial aesthetics play a significant role in human mental health; notably, even small changes can have a significant impact on a person's daily life. Thus, when several variables are involved, the requirements for a more beautiful face follow a certain pattern, albeit with some differences between genders and cultures. Points, angles, lines, and proportions are established as references for facial harmony, and the modification of these parameters can lead to the results desired by the patients.
Orthognathic surgery is a procedure aimed at balancing the facial bones of the skull, with significant effects on the patient's chewing, breathing, and phonation functions, thus resulting in significant improvement in their quality of life.1 Patients undergoing orthognathic surgery also strive for aesthetic improvements2, as many of them are victims of prejudice and bullying and they believe that their appearance does not meet the aesthetic standards of society. Against this background, what about the cases in which orthognathic surgery does not resolve the aesthetic complaints of these patients? What if, in order to achieve the aesthetic result the patient wants, we have to perform more aggressive osteotomies, which makes the operation riskier and more complicated?
The list of surgical and non-surgical facial procedures that exist today enables for alternatives to be planned in order to maximise gains and reduce morbidity. Therefore, the purpose of this article is to discuss some non-surgical techniques that can help surgeons achieve aesthetics that are as faithful to the patient as possible without altering the function that has already been improved by orthognathic surgery. Unfortunately, the literature on this subject is scarce. In fact, the few published articlesrequire constant updating as popular non-surgical products and facial aesthetic procedures continue to evolve.
Materials and Methods
This was a retrospective case series of patients undergoing orthognathic surgery and aesthetic non-surgical refinements that followed the Consensus-based Clinical Case Reporting (CARE) guidelines.3 As a private case report, this article is exempt from ethical approval. Furthermore, the patients’ written consent was obtained.
Three patients who underwent orthognathic surgery and later aesthetic refinement were included in this study. Each one was also presented with a different type of non-surgical procedure, including botulinum toxin injection, dermal fillers, and suspension threads. Specifically, the participants were two women and one man, all Caucasian, aged between 31 and 48 years. Two patients complained of aesthetic outcomes and the other one of pain in the lower jaw angle and bone resorption. There was no history of comorbidities as well as smoking or alcohol abuse in their backgrounds. Additionally, a bibliographic search was carried out, but literature on the subject is scarce. One of the main goals of this article is to expand the number of articles devoted to the refinement of orthognathic surgery.
Case studies
Botulinum toxin
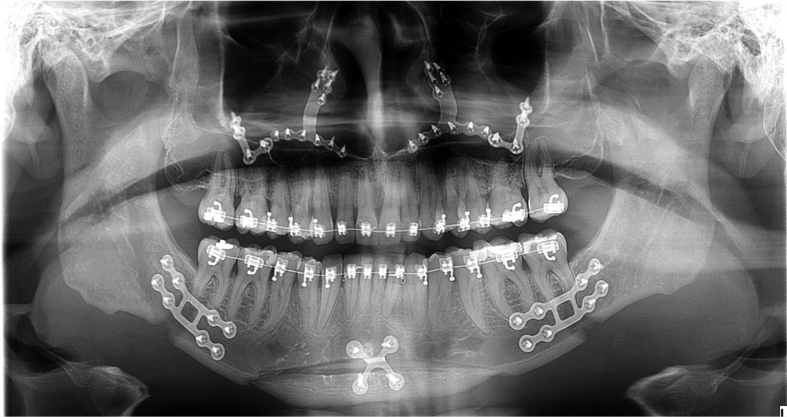
The male patient, 32 years old, with standard II class II dentofacial deformity (Figure 1), underwent orthognathic surgery, bimaxillary advancement, and advancement genioplasty. The postoperative imaging follow-up examinations revealed reabsorption of the mandibular angle (Figure 2) with aetiology caused by benign masseter hypertrophy and bruxism as well as constant complaints of myalgia in the temporal and masseteric areas. Subsequently, fiftyU of botulinum toxin was divided between the masseter (10U in each muscle in 2 points) and the temporal (15U in each muscle in 3 points). The patient is under control without an increase in resorption and without pain symptoms in the masticatory muscles with only the application of botulinum toxin annually without further medication or clinical treatment. Despite no massive change in the facial aspect, the panoramic x-ray showed that the case is under control without bone loss progression.
Figure 1.
Preoperative radiography. Note the irregularity in the bilateral mandibular angle region.
Figure 2.
Radiograph after two years of orthognathic surgery where it is possible to observe bone resorption at an angle of the mandible due to extreme muscle action.
Dermal filler
A 52-year-old female patient underwent orthognathic surgery 12 years ago with complaints about thin lips and no contour. Her lips were filled with 1 ml of hyaluronic acid of medium consistency (Figure 3).
Figure 3.
Lip filling (A). Note the better contour and volume of the upper lip and the proportion with the lower lip (B).
Facial sutures
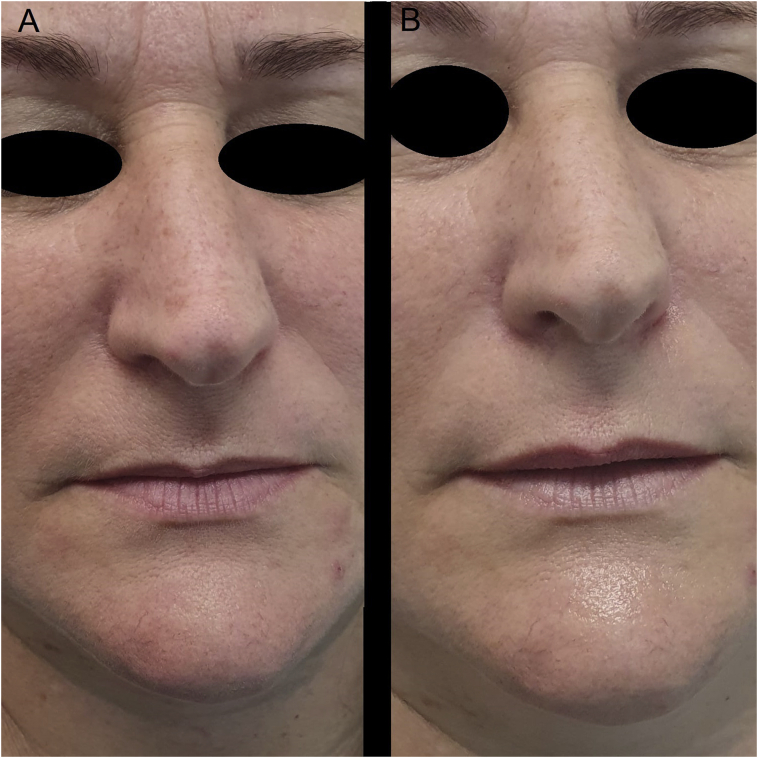
A 47-year-old female patient underwent orthognathic surgery 17 years ago. She had significant facial sagging with loss of mandibular contour and ptosis of the facial tissues. She had no bone changes that would justify a second orthognathic surgery. Therefore, six double needle sutures of eight cones made of polylactic acid (Silhouette Soft ®, Sinclair Pharma) were installed.
Even the immediate postoperative phase shows tissue repositioning with an improved mandibular contour (Figure 4). The face with an oval-shaped soft tissue ptosis became triangular, which gives it a more youthful appearance.
Figure 4.
Frontal view (A). Notice the changed face shape with improved facial aesthetics and rejuvenation (B).
The patients have returned to normal activities without incident. All of them are satisfied with the results and would undergo the same procedures again. The sample size was not critical, resulting in limited statistical power; consequently, additional patients would have strengthened the study.
Discussion
Although orthognathic surgery has evolved into a virtual planning process through computed tomography and specific software, facial analysis of patients remains of paramount importance. The literature shows that the three-dimensional correction of bone structures of any dentofacial deformity alone does not always achieve the proposed aesthetic result. Hence, soft tissue analysis is essential to improve these results.
Regardless of the facial analysis technique to be used, two points are essential. First, the facial analysis must be directly done on the patient's face and not through photographs, as the minimal tilt of the head and the intensity and type of light that is on the face can alter the doctor's vision. Second, the survey and consideration of the patients' complaints is another crucial detail – whether functional and/or aesthetic – because the treatment must try to resolve as many complaints as possible.
Among the features to be clinically analysed, we can mention the proportionality between the horizontal thirds of the face and the symmetry of the face as critical requirements. In the upper third, the eyebrow balance and/or ptosis should be assessed. The width of the mandible is more pronounced in female patients, even with more anteroposterior projection, which gives the patients a more youthful appearance. The male mandible tends to be square in shape with better lateral projection of the mandibular angle and goniac angle; in contrast, this is not as blunt as seen in women, making the male face more square and the female face more like an inverted-base triangle. In a profile view, a balance must be established between the tip of the nose and chin with a sufficient projection of the upper and lower lips. The well-defined cervico-mandibular angle also demonstrates youthfulness and health.
Botulinum toxin
Patients with dentofacial deformities have a three-dimensional change in bone position. After orthognathic surgery, the muscles, regardless of whether chewing or facial expression, must be adjusted if the bone base is correctly adjusted4; thus, postoperative physiotherapy is important. Owing to the excessive compensatory chewing effort because of their bone deformity, some patients develop a certain level of hypertrophy in the temporal muscle, which is more noticeable in the masseter.
One of the treatment methods for benign masseter hypertrophy with great acceptance and patient satisfaction is the use of botulinum toxin type A.5 This particular toxin acts on acetylcholine and paralyses the muscles. This paralysis and the resulting loss of muscle tone leads to a decrease in muscle volume, thus reducing the lateral projection of the lower jaw angle. In addition to its aesthetic function, the toxin can also be used functionally in other muscles to reduce muscle tension in the postoperative phase, prevent fracture or displacement of the fixation material,6 and reduce the likelihood of recurrences caused by muscle hyperactivity.7,8
Dermal filler
The virtual planning of orthognathic surgery increases the predictability of the surgical procedure and helps the patient to more efficiently visualise the final aesthetic result.9 Further, today there are only a few surgical procedures that require reoperation.10 However, even with all the available planning technology and sophisticated surgical techniques, some aesthetic deficits can occur.
The same filler used in rejuvenation and congenital disabilities11 can also be used in these situations. Applied by supraperiosteal injections, they give back a person's face its volume, outline it, and achieve an aesthetic result desired by the patient with a categorically lower risk of complications than with operations,12 be it a reoperation of orthognathic surgery or reparative plastics.
The central anatomical regions where the filling can be used to refine orthognathic surgeries are the infraorbital area, which gives an anteroposterior projection, and the zygomatic arch, which makes the middle third wider than the lower one in female patients. Male patients usually do not need refinement in the middle third. The area of the canine pit can be filled in cases where orthognathic surgery was unable to project the upper jaw into the anterior area in the desired amplitude. This filler projects the premaxilla and nose forward to raise the tip of the nose.
A filler can be used in the chin area in the lower third, which projects it forward and gives it a more harmonious shape based on the gender of the patient. Generally, this shape would be triangular for women and square for men. In some cases, orthognathic surgery cannot create volume in the mandibular angle area because of hypoplasia. In these cases, the patient, especially males, can fill in the region or install a facial implant to make the jaw more square with well-defined angles and edges that add youthfulness and masculinity to the face.
The anteroposterior projection and the lip contour can also be improved during the postoperative period.13 Even certain manoeuvres performed in the postoperative period are aimed at better anteroposterior projection of the lips, such as the VY suture, resulting in a lip projection considered adequate by many patients. The lip filling manages to improve this projection and gives the lips more volume and contour.
The cervico-mandibular angle has an important aesthetic aspect. When patients have a more defined border between their neck and jaw, the more youthful and healthier they appear; accordingly, a lack of this border is a common complaint from them. It can be treated with liposuction, which removes fat from the lower jaw region, or dermal filling, which more strongly marks the basal area of the lower jaw. In some cases, both procedures are required at different times.
With advancing age, bone resorption also occurs in patients without pathology or for those on medication. This resorption leads to a rounding of the mandibular edges, and what was pronounced in young patients is rounded off with age, thereby resulting in a loss of the mandibular contour, thus causing a connection between the neck and the face. This type of change in the cervical area can be treated with a dermal filling (i.e. hyaluronic acid, polycaprolactone) that restores the contour and makes the face look younger.
Another change is sagging in the front of the neck, which is caused not only by drooping tissue but also by the presence of fat. Fat can also be present in patients with a low body mass index (BMI). In this situation, one of the most effective treatments is performing liposuction of this submandibular fat, which brings back the contour to the neck when the cervico-mandibular angle is changed. Although a surgical treatment, it can be done simultaneously with orthognathic surgery, which increases the aesthetic result desired by the patient. Another treatment aimed at treating such facial aging is facial filling, which can be achieved with a variety of materials, either permanent types such as facial implants or temporary types such as hyaluronic acid, polycaprolactone, and calcium hydroxyapatite.
Facial sutures
Patients with some dentofacial deformity who are undergoing orthognathic surgery have a change in facial development with a resulting change in the overall homeostasis of the region. The change in this homeostasis is not permanent, and after the repair phase the soft and bone tissues return to their equilibrium. However, over the years there is soft tissue ptosis compatible with the age and habits of each patient. There is no evidence in the literature that orthognathic surgery causes any kind of acceleration in the sagging of the face.14,15
For many years, the only alternative treatment to hanging facial tissues has been surgical facial lifting. It is a surgery with excellent results, but with some disadvantages such as high cost and the patients’ need to stop daily activities for a while.
There are several treatments available for performing a non-surgical facelift. The greatest effect, however, are facial sutures, which manage to lift and hold the flaccid soft tissues by mechanical pulling, thereby anchoring them in a higher area of the face. The suspension of the tissues is immediately noticeable after the procedure. Nevertheless, because of the adaptation of the skin and the biostimulation provided by the thread itself, the end result should appear after about 90 days.
Conclusions
The procedures for aesthetic refinement after orthognathic surgery are becoming increasingly accessible. The surgeon needs to continually review these new procedures and know when to indicate them to achieve a superior aesthetic outcome. The refinement in no way replaces orthognathic surgery, as it is a purely aesthetic intervention without any functional advantage.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The authors confirm that this study has been prepared in accordance with the rules and regulations of the Committee on Publication Ethics (COPE). Given the nature of the letter, Institutional Review Board (IRB) review was not required.
Consent
Informed consent was obtained from all participants included in the study.
Authors contributions
RG conceived and designed the study, conducted research, collected and organised data, and wrote the article's draft. AMB, APCBL, and RV conducted research, provided research materials, and collected and organised data. MCP conceived and designed the study, analysed and interpreted data, and wrote the draft of the article. CRPJ collected, organised, and interpreted data and wrote the draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Bensoussan J.C., Bolton M.A., Pi S., Powell-Hicks A.L., Postolova A., Razani B., et al. Quality of life before and after cosmetic surgery. CNS Spectr. 2014 Aug;19(4):282–292. doi: 10.1017/S1092852913000606. https://doi: 10.1017/S1092852913000606 [DOI] [PubMed] [Google Scholar]
- 2.Nocini P.F., Chiarini L., Bertossi D. Cosmetic procedures in orthognathic surgery. J Oral Maxillofac Surg. 2011 Mar;69(3):716–723. doi: 10.1016/j.joms.2009.07.043. https://doi: 10.1016/j.joms.2009.07.043 [DOI] [PubMed] [Google Scholar]
- 3.Gagnier J.J., Kienle G., Altman D.G., Moher D., Sox H., Riley D., CARE Group The CARE guidelines: consensus-based clinical case reporting guideline development. BMJ Case Rep. 2013 Oct 23 doi: 10.1136/bcr-2013-201554. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wollina U., Goldman A. Botulinum toxin A and/or soft tissue fillers for facial rehabilitation. Wien Med Wochenschr. 2017 Mar;167(3–4):92–95. doi: 10.1007/s10354-016-0512-8. https://doi: 10.1007/s10354-016-0512-8 [DOI] [PubMed] [Google Scholar]
- 5.Arikan O.K., Tan F.U., Kendi T., Koc C. Use of botulinum toxin type A for the treatment of masseteric muscle hypertrophy. J Otolaryngol. 2006 Feb;35(1):40–43. doi: 10.2310/7070.2005.4108. https://doi: 10.2310/7070.2005.4108 [DOI] [PubMed] [Google Scholar]
- 6.Shin S.H., Kang Y.J., Kim S.G. The effect of botulinum toxin-A injection into the masseter muscles on prevention of plate fracture and postoperative relapse in patients receiving orthognathic surgery. Maxillofac Plast Reconstr Surg. 2018 Nov 25;40(1):36. doi: 10.1186/s40902-018-0174-0. https://doi: 10.1186/s40902-018-0174-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang Y.J., Cha B.K., Choi D.S., Jang I.S., Kim S.G. Botulinum toxin-A injection into the anterior belly of the digastric muscle for the prevention of postoperative open bite in class II malocclusions: a case report and literature review. Maxillofac Plast Reconstr Surg. 2019 Apr 26;41(1):17. doi: 10.1186/s40902-019-0201-9. https://doi: 10.1186/s40902-019-0201-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mücke T., Löffel A., Kanatas A., Karnezi S., Rana M., Fichter A., et al. Botulinum toxin as a therapeutic agent to prevent relapse in deep bite patients. J Cranio-Maxillo-Fac Surg. 2016 May;44(5):584–589. doi: 10.1016/j.jcms.2016.01.021. https://doi: 10.1016/j.jcms.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 9.Willinger K., Guevara-Rojas G., Cede J., Schicho K., Stamm T., Klug C. Comparison of feasibility, time consumption, and costs of three virtual planning systems for surgical correction of midfacial deficiency. Maxillofac Plast Reconstr Surg. 2021 Jan 7;43(1):2. doi: 10.1186/s40902-020-00284-1. https://doi: 10.1186/s40902-020-00284-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bowe C.M., Gurney B., Sloane J., Johnson P., Newlands C. Operative time, length of stay and reoperation rates for orthognathic surgery. Br J Oral Maxillofac Surg. 2020 Dec 15 doi: 10.1016/j.bjoms.2020.08.124. https://doi: 10.1016/j.bjoms.2020.08.124 S0266-4356(20)30959-1. [DOI] [PubMed] [Google Scholar]
- 11.Bertossi D., Nocini P.F., Rahman E., Heydenrych I., Kapoor K.M., de Maio M. Non surgical facial reshaping using MD Codes. J Cosmet Dermatol. 2020 Sep;19(9):2219–2228. doi: 10.1111/jocd.13596. https://doi: 10.1111/jocd.13596 [DOI] [PubMed] [Google Scholar]
- 12.Olivieri P., Uribe F.A., Quereshy F.A. Aesthetic facial surgery and orthodontics: common goals. Oral Maxillofac Surg Clin North Am. 2020 Feb;32(1):153–165. doi: 10.1016/j.coms.2019.09.004. https://doi: 10.1016/j.coms.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 13.Mohamed W.V., Perenack J.D. Aesthetic adjuncts with orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2014 Nov;26(4):573–585. doi: 10.1016/j.coms.2014.08.010. https://doi: 10.1016/j.coms.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 14.Bailey L.J., Collie F.M., White R.P., Jr. Long-term soft tissue changes after orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1996;11(1):7–18. [PubMed] [Google Scholar]
- 15.Raffaini M., Pisani C., Conti M. Orthognathic surgery "again" to correct aesthetic failure of primary surgery: report on outcomes and patient satisfaction in 70 consecutive cases. J Cranio-Maxillo-Fac Surg. 2018 Jul;46(7):1069–1078. doi: 10.1016/j.jcms.2017.09.026. https://doi: 10.1016/j.jcms.2017.09.026 [DOI] [PubMed] [Google Scholar]