A 75‐year‐old man with a history of chronic ischemic heart disease with a previously normal blood count, presented to the emergency room with fever and tachycardia. There was no hepatosplenomegaly or lymphadenopathy. An electrocardiogram showed a left bundle branch block. Oxygen saturation was 95%. Because of the fever, the patient was tested for SARS‐CoV‐2; the reverse transcriptase‐polymerase chain reaction was positive. A diagnosis of COVID‐19 was made.
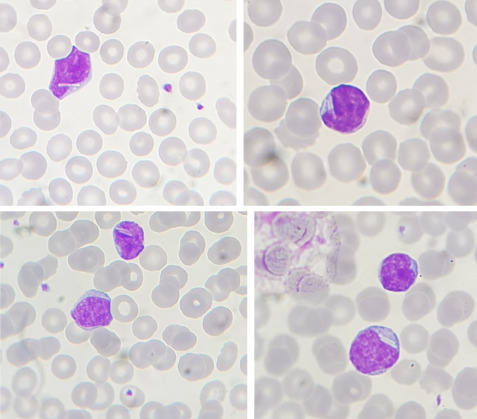
The patient's blood count showed a white blood cell count (WBC) of 10.46 × 109/L, lymphocytes 4.51 × 109/L, hemoglobin 129 g/L, and platelet count 233 × 109/L. D‐dimer was 659 μg/L (normal range < 500) and interleukin 6 was 76.3 pg/ml (normal range < 6.4). A computed tomography scan of the chest showed bilateral interstitial infiltrates associated with multiple enlarged mediastinal lymph nodes. Following a rapid and unexpected increase of the WBC to 17.49 × 109/L and of the lymphocyte count to 8.37 × 109/L over the next 48 h, a blood film and immunophenotyping were performed. The film showed small and medium‐sized lymphocytes, with a variable N:C ratio and moderately basophilic cytoplasm. Smear cells were present. A quarter of the lymphocytes showed the negative images of one to three rod‐shaped crystals (average two per cell). There were some immature monocytes and some neutrophils showed mild toxic granulation or abnormal nuclear shapes, consistent with COVID‐19. Flow cytometric immunophenotyping showed an increased number of circulating B cells (93% of lymphocytes, 7.78 × 109/L) with lambda light chain restriction and expressing CD19, CD5, CD23, weak CD20, CD43, and CD200; the cells were negative for CD10, CD79b, CD81, FMC7, and CD38. The matutes score was 5/5. At this stage, the condition could not be distinguished from chronic lymphocytic leukemia (CLL).
Two months later the WBC and lymphocyte count had returned to normal and repeated immunophenotyping showed only 0.63 × 109/L CD5‐positive clonal B cells. However, lymphocytes with cytoplasmic crystals were still present. A diagnosis of monoclonal B‐cell lymphocytosis (MBCL) was made. Patients with CLL in whom COVID‐19 led to a marked but transient increase in the lymphocyte count have been reported. In this case, COVID‐19 in a patient with MBCL led to an increase in the lymphocyte count to a level simulating CLL with follow‐up indicating the correct diagnosis. In addition, we report here the observation of the negative images of crystals, attributable to crystallization of immunoglobulin, in MCBL. This phenomenon has previously been reported in CLL.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Lanza L, Koroveshi B, Barducchi F, et al. A new diagnosis of monoclonal B‐cell lymphocytosis with cytoplasmic inclusions in a patient with COVID‐19. Am J Hematol. 2022;97(10):1372‐1373. doi: 10.1002/ajh.26582
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


