Abstract
Objective
Little is known regarding the reactogenicity and related SARS–CoV‐2 vaccine response in patients with chronic inflammatory disease (CID). Our objective was to characterize the adverse event profile of CID patients following SARS–CoV‐2 vaccination and understand the relationship between reactogenicity and immunogenicity of SARS–CoV‐2 vaccines.
Methods
CID patients and healthy controls eligible to receive messenger RNA (mRNA) SARS–CoV‐2 vaccines participated in 3 study visits (pre‐vaccine, after dose 1, and after dose 2) in which blood and clinical data were collected. Assessment of adverse events were solicited within 7 days of receiving each dose. Serum anti–SARS–CoV‐2 spike IgG ± antibody titers were quantified following vaccination. Statistical analysis was performed utilizing mixed models and tobit regressions, with adjustment for covariates.
Results
The present study included 441 participants (322 CID patients and 119 control subjects). Compared to controls, CID patients reported greater symptom severity after dose 1 (P = 0.0001), including more myalgia and fatigue (P < 0.05). For immunogenicity, a higher symptom severity after dose 1 and a higher number of symptoms after dose 2 was associated with higher antibody titers (P ≤ 0.05). Each increase of 1 symptom was associated with a 15.1% increase in antibody titer. Symptom association was strongest with site pain after dose 1 (105%; P = 0.03) and fatigue after dose 2 (113%; P = 0.004).
Conclusion
Patients with CID have a distinct reactogenicity profile following SARS–CoV‐2 vaccination compared to controls. Furthermore, there is an association between increased reactogenicity and increased vaccine response. This finding may speak to the more variable immunogenicity in CID patients and may be an important indicator of vaccine response to the novel SARS–CoV‐2 vaccines.
INTRODUCTION
The COVID‐19 pandemic caused by the SARS–COV‐2 virus is a global health emergency that has affected tens of millions of individuals worldwide. To address this crisis, the US Food and Drug Administration has approved several vaccines for emergency use, including novel messenger RNA (mRNA)–based and adenovirus‐based approaches (1, 2, 3). Patients with chronic inflammatory diseases (CIDs) have dysregulation of their immune system and often require long‐term use of immunosuppressive medications that may increase their risk of developing severe illness from SARS–CoV‐2 infection (4, 5). Therefore, the importance of immunization in this population is particularly high.
SIGNIFICANCE & INNOVATIONS.
Patients with chronic inflammatory disease (CID) have a distinct reactogenicity profile compared to healthy controls following SARS–CoV‐2 vaccination and demonstrate an association between reactogenicity and immunogenicity.
The unique relationship of reactogenicity and immunogenicity in CID patients following vaccination with the messenger RNA SARS–CoV‐2 vaccines has not been demonstrated in the general population.
Concerns regarding the side effect profile and novelty of the mRNA SARS–CoV‐2 vaccines have been shown to influence attitudes toward the vaccines and contribute to vaccine hesitancy in the general population (6, 7). The clinical trials of 2 mRNA‐based vaccines and 1 adenovirus‐based vaccine identified that most participants reported at least 1 local or systemic reaction, with very few reactions characterized as severe (1, 2, 3). Follow‐up data from the Centers for Disease Control and Prevention (CDC) V‐safe active surveillance system have confirmed these initial findings and helped provide reassurance to providers and patients regarding vaccine safety (8, 9). Yet, while the side effects profile of the general population to the SARS–CoV‐2 vaccines continues to be studied, little is known regarding the reactogenicity of patients with CIDs following SARS–CoV‐2 vaccination (10, 11).
While rheumatic disease–specific reactogenicity studies are limited, the safety profile of the several vaccines in immunocompromised patients, including HIV and renal transplant patients, have been examined (12, 13, 14, 15). Given the presence of immune dysregulation and use of chronic immunosuppression, it is plausible that patients with CID may have a unique reactogenicity profile to the novel SARS–CoV‐2 vaccines. In addition, many of the reported adverse events to the SARS–CoV‐2 vaccine, including arthralgias, myalgias, fatigue, and even fever, mimic symptoms of CID flare (9). It is therefore crucial to better understand the reactogenicity of CID patients following SARS–CoV‐2 vaccination to better inform physicians and patients regarding expectations.
Another pressing question has been the relationship between immunogenicity and reactogenicity to the SARS–CoV‐2 vaccines. It has been hypothesized that increased symptomatology following vaccination would be indicative of a more robust vaccine response; however, this has yet to be demonstrated in the general population (16). One explanation could be the robustness of the vaccine response in the immunocompetent host that has been demonstrated to occur in nearly all individuals. However, in patients with CID and other immunocompromised states, it has been shown that immune response may be blunted in certain groups (17, 18). Therefore, understanding the relationship of immunogenicity and reactogenicity in the CID patient population may be of particular clinical importance.
The primary objective of this study was to characterize the adverse event profile of patients with CID after receiving SARS–CoV‐2 vaccines and to better understand the relationship between reactogenicity and immunogenicity of the SARS–CoV‐2 vaccines in patients with CID. We were interested in understanding the degree of severity and individual symptoms experienced by CID patients as well as the impact of immunosuppressive medications. We hypothesized patients with CID would have a reactogenicity profile unique to that of the general population and that increased symptomatology would be associated with increased vaccine response.
PATIENTS AND METHODS
Study design and participants
This substudy within the COVID‐19 Vaccine Responses in Patients with Autoimmune Disease (COVARIPAD) study examined the magnitude and quality of immune response to the SARS–COV‐2 vaccines. COVARIPAD is a longitudinal, prospective, observational study taking place at 2 large academic centers, Washington University in St. Louis and University of California, San Francisco. This study was approved by the Washington University in St. Louis and University of California, San Francisco institutional review boards.
Participants with confirmed CID and healthy controls who were eligible to receive the SARS–CoV‐2 vaccine were recruited for this study from the faculty, staff, employees, and patients at Washington University School of Medicine and BJC health care system (St. Louis, Missouri) and UCSF, UCSF Health, and Zuckerberg San Francisco General Hospital (San Francisco, California). All participants provided informed consent. As part of the COVARIPAD study, participants were assessed in standardized intervals (pre‐vaccine, post‐vaccine dose 1, and post‐vaccine dose 2) to answer questionnaires and provide blood samples. Prior to first vaccine dose, demographic data and clinical data, including disease classification, and current and previous medication history were collected. When enrolling, control participants had the option to only complete questionnaires and not provide blood for immunogenicity studies; these participants provided demographic characteristics, verification of the absence of CID, and reactogenicity information only.
Assessment of SARS–CoV‐2 vaccine response
Humoral response quantification was performed for patients and controls who had completed baseline and post‐vaccination blood draws. As previously described, anti‐spike IgG quantification was performed utilizing enzyme‐linked immunosorbent assay, and direct ex vivo enzyme‐linked immunosorbent spot (ELISpot) assays were performed to quantify recombinant S protein–binding IgG secreting cells (17).
Assessment of reactogenicity
For assessment of adverse events, the outcomes of interest included overall severity of symptoms (0–3 ordinal scale), number of symptoms, and each individual symptom present (yes/no) following both doses of vaccine. We used an online administered survey showing severity on an ordinal scale (0 = no symptoms, 1 = mild symptoms, 2 = moderate symptoms, and 3 = severe symptoms) and solicited symptoms presented in list format (injection site pain, injection site redness, headache, fever, rash, myalgia, arthralgia, fatigue, nausea, and diarrhea). Due to differences in initial protocol, healthy controls from the Washington University in St. Louis site did not provide information on graded severity. Participants were asked to respond with their symptoms up to 7 days post‐vaccination.
Statistical analysis
Demographic differences between CID patients and healthy subjects were assessed using t‐tests and chi‐square tests. Differences in reactogenicity outcomes between CID patients and healthy controls were analyzed using mixed models, with site as a random effect and adjustment for age, sex, and vaccine (Stata meologit command for ordinal regression of severity, mixed‐effects modeling for linear regression of number of symptoms, and melogit command for logistic regression of the presence/absence of symptoms). Within CID patients, differences in reactogenicity were examined among 1) different CID disease states and 2) medications of interest by comparing exposed and nonexposed groups (for example, inflammatory bowel disease versus non–inflammatory bowel disease CID, and tumor necrosis factor [TNF] inhibitor medication versus no TNF inhibitor). We did not stratify or adjust for medications within disease states or vice versa due to small sample sizes. Severity and number of symptoms were evaluated using mixed models as above; diseases and medications for each individual symptom were assessed using chi‐square tests.
Study site was incorporated as a random effect in our mixed models as there were site differences in adverse events and correlated demographic characteristics (e.g., age) (Supplementary Table 1, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24894). To further account for these study site differences, sensitivity analysis of reactogenicity in CID patients versus healthy controls was performed using a subset of patients in homogeneous matched groups. Nonoverlapping groups were selected so that they contained 1 or more CID subjects, 1 or more healthy subjects, and so that all group members had the same vaccine exposure, sex, and age (within 5 years). Some subjects were excluded when there were no corresponding CID/healthy controls with the match criteria. A total of 397 patients were included in 31 groups. These were analyzed using the mixed model functions above but with the matched group as the random effect.
For assessment of reactogenicity impact on vaccine antibody response, the outcome of interest was anti–SARS–CoV‐2 spike IgG ± antibody titer. Differences in antibody titers were examined with reactogenicity as a predictor, using graded symptom severity, number of symptoms, and individual symptoms among CID patients and healthy controls. Tobit regressions adjusted for participant status, age, sex, and vaccine type were used to account for left‐censoring below the response detect limit (1:30) (19, 20). Vaccine type and site were not shown to be of significance and were removed from these models.
RESULTS
Study participants and clinical characteristics
A total of 441 participants were included in the study, including 322 patients with CID and 119 healthy controls. The mean ± SD age was 47.3 ± 15.9 years, with 18% of participants being ≥65 years old. The majority of participants were female (68%) and White (82%). Vaccine distribution included 74% receiving the BNT162b2 vaccine and 26% receiving the mRNA‐1273 vaccine. The most common diagnoses among CID patients included inflammatory bowel disease (32%) and rheumatoid arthritis (23%). Demographic information, clinical characteristics, and medications used by study participants are shown in Tables 1 and 2.
Table 1.
Demographic and clinical characteristics of study participants*
| Demographic data | Patients with CID (n = 322) | Control subjects (n = 119) | P |
|---|---|---|---|
| Age, mean ± SD years | 48.5 ± 15.7 | 44.2 ± 15.8 | 0.01 |
| <65 years, % | 80.4 | 85.9 | 0.18 |
| 65+ years, % | 19.6 | 15.1 | – |
| Female sex, % | 71.4 | 59.9 | 0.02 |
| White race, % | 85.7 | 73.9 | 0.01 |
| Vaccine type, % | |||
| BNT162b2 | 73.9 | 73.1 | 0.86 |
| mRNA‐1273 | 26.1 | 26.9 | – |
| Site, % | |||
| WUSTL | 65.5 | 39.5 | <0.001 |
| UCSF | 35.5 | 60.5 | – |
CID = chronic inflammatory disease; UCSF = University of California, San Francisco; WUSTL = Washington University in St. Louis.
Table 2.
Clinical characteristics and medication use of study participants*
| No. (%) | |
|---|---|
| Immunologic diagnosis | |
| Inflammatory bowel disease | 105 (32.6) |
| Rheumatoid arthritis | 74 (23.0) |
| Spondyloarthritis | 46 (14.3) |
| Systemic lupus erythematosus | 36 (11.2) |
| Sjögren's syndrome | 18 (5.6) |
| Other CTD | 18 (5.6) |
| Uveitis | 22 (6.8) |
| Multiple sclerosis | 20 (6.2) |
| Hidradenitis suppurativa | 16 (5.0) |
| Vasculitis | 7 (2.2) |
| Autoinflammatory syndrome | 3 (1.0) |
| IgG4‐related disease | 3 (1.0) |
| NMO | 2 (0.6) |
| Other | 8 (2.5) |
| Medications | |
| Prednisone | 41 (12.7) |
| DMARDs | |
| Methotrexate | 58 (18.0) |
| Hydroxychloroquine | 60 (18.6) |
| Azathioprine | 20 (6.2) |
| Sulfasalazine | 19 (5.9) |
| Mycophenolate mofetil | 17 (5.3) |
| Leflunomide | 11 (3.4) |
| JAK inhibitors | 18 (5.6) |
| Biologic therapies | |
| TNF inhibitors | 99 (30.7) |
| B cell–depleting therapies | 29 (9.0) |
| Belimumab | 4 (1.2) |
| Vedolizumab | 26 (8.1) |
| IL‐12/23 or IL‐23 inhibitors | 22 (6.8) |
| Abatacept | 5 (1.6) |
| Other | 4 (1.2) |
| NSAIDs | 59 (18.3) |
CTD = connective tissue disease; DMARDs = disease‐modifying antirheumatic drugs; IL‐12 = interleukin‐12; NMO = neuromyelitis optica; NSAIDs = nonsteroidal antiinflammatory drugs; TNF = tumor necrosis factor.
Adverse event profile
Solicited adverse events occurred frequently in both the CID and control groups following the first and second dose of the SARS–CoV‐2 vaccine. In CID patients, the most common symptoms following both first and second dose of vaccine included injection site pain, fatigue, headaches, and myalgias (Figure 1). When compared to healthy controls, CID patients had significantly more severe symptoms following the first dose of vaccine after adjustment for age, sex, and vaccine type, with an odds ratio (OR) of 3.7 (95% confidence interval [95% CI] 1.91, 7.12], P = 0.0001) per severity level (i.e., the odds of a CID patient experiencing severe symptoms 1 level higher was 3.7 times that of a healthy patient with other covariates equal). With random‐effects mixed modeling of the combined sites, there was more fatigue (OR 1.85 [95% CI 1.01, 3.37], P = 0.045) and myalgias (OR 1.95 [1.03, 3.67], P = 0.04) in patients with CID following the first dose compared to healthy controls. Following the second dose, CID patients had more instances of reported headache compared to healthy controls (OR 1.68 [95% CI 1.06, 2.66], P = 0.03) but other differences in symptoms severity, and number of symptoms did not vary significantly between CID patients and control subjects. A sensitivity analysis with matched groups for sex, age, and vaccine type yielded similar results to original combined analysis (Supplementary Table 1, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24894).
Figure 1.
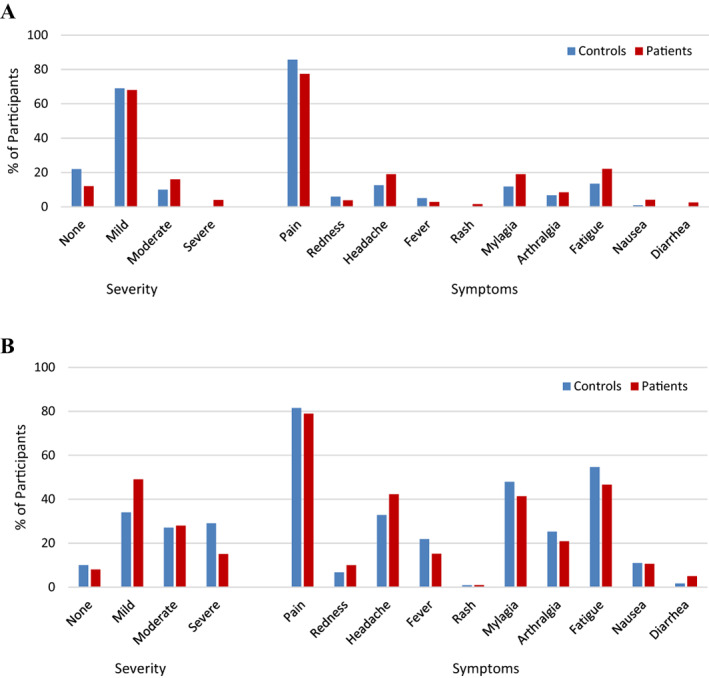
Severity of symptoms and solicited symptoms in control subjects versus patients with chronic inflammatory disease. Percentage of participants from each group who had endorsed symptom severity and solicited adverse events within 7 days after doses 1 (A) and 2 (B) of SARS–CoV‐2 vaccine is shown.
Among CID patients, no specific disease group was associated with increased symptomatology following mixed‐model regression analysis adjusted for age, sex, and vaccine. There was suggestive evidence of increased reactogenicity in spondyloarthritis (SpA) patients with increased severity following the second dose (OR 1.98 [95% CI 1.08, 3.64], P = 0.03). The strongest individual symptom associations included SpA patients with increased fatigue following the second vaccine dose (OR 2.35 [95% CI 1.24, 4.51], P = 0.005) and the first vaccine dose (OR 2.27 [95% CI 1.14, 4.15], P = 0.009) and connective tissue disease patients with increased nausea following the first dose (OR 4.69 [95% CI 1.23, 16.99], P = 0.004). Among medications used in CID patients, methotrexate (OR 1.54 [95% CI 0.89, 2.68], P = 0.13) had the strongest adjusted association with increased symptom severity following the second dose of vaccine. B cell–depleting agents, including rituximab and ocrelizumab, had suggestive protective effects for site pain following the first dose (OR 0.39 [95% CI 0.16, 0.97], P = 0.02). Among other more prevalent medications, hydroxychloroquine was most associated with arthralgia after the second dose (OR 2.03 [95% CI 1.01, 3.95], P = 0.03), and TNF inhibitor was most associated with less redness after dose 1 (OR 0.19 [95% CI 0.004, 1.37], P = 0.08).
When examining additional factors influencing reactogenicity, we found age and sex influenced reactogenicity (Figure 2). In multivariable models, being older than 65 years of age was associated with significantly less symptom severity (OR 0.51 [95% CI 0.31, 0.83], P = 0.006) and was also associated with fewer reported symptoms following the second dose of vaccine (OR −0.81 [95% CI −1.27, −0.34] per symptom, P = 0.001). We also found that female sex was associated with increased symptom severity when compared to male sex, with an OR of 2.028 (95% CI 1.33, 3.10) after second vaccine dose (P = 0.001). Those receiving the BNT162b2 mRNA vaccine demonstrated a trend toward less severe symptoms following second dose compared to those receiving the mRNA‐1273 vaccine; however, this was not statistically significant (OR 0.66 [95% CI 0.43, 1.01], P = 0.06). Complete results are shown in Supplementary Table 2, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24894.
Figure 2.
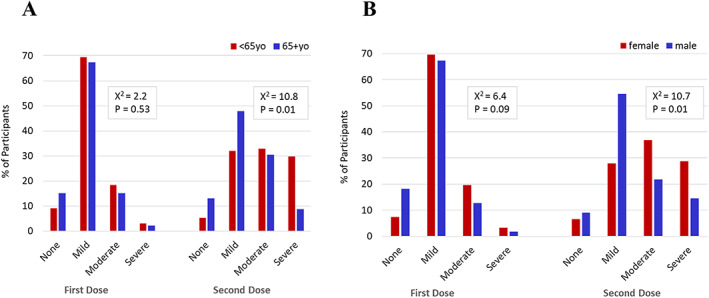
Symptom severity among participants by age and sex. Comparison of endorsed symptom severity following doses 1 and 2 of SARS–CoV‐2 vaccine by age groups (A) and by sex (B).
Reactogenicity and immunogenicity
Regarding reactogenicity and its relationship to vaccine response, we found certain adverse event characteristics were associated with higher spike protein antibody titer to the SARS–CoV‐2 vaccine in both CID patients and control subjects. Specifically, after adjustment for covariates, increased symptom severity following the first dose of vaccine and a higher number of reported symptoms after the second dose of vaccine was associated with higher antibody titers (Table 3). Each increase in degree of severity following the first dose was associated with a 68% increase of antibody titer (range 4.6%, 170%) (P = 0.03). Each increase of 1 endorsed symptom following the second dose of vaccine was associated with a 15.1% increase in antibody titer (range 0%, 32.4%) (P = 0.05) in our regression model (Figure 3). Complete results are shown in Supplementary Table 3, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24894.
Table 3.
Top reactogenicity predictors (P ≤ 0.05) of increase in antibody titer*
| Reactogenicity predictors | β (log10 titer) | % change (increase) | % change (95% CI) | P |
|---|---|---|---|---|
| Severity per level with first dose | 0.226 | 68.1 | (4.6, 170.2) | 0.03 |
| Number of symptoms per symptom with second dose | 0.061 | 15.1 | (0.0, 32.4) | 0.05 |
| Site pain with first dose | 0.313 | 105.6 | (7.9, 291.8) | 0.03 |
| Fever with second dose | 0.309 | 103.6 | (3.1, 301.9) | 0.04 |
| Fatigue with second dose | 0.329 | 113.5 | (27.8, 256.8) | 0.004 |
Shown are the reactogenicity attributes and their associated changes in anti–SARS–CoV‐2 spike IgG+ antibody titers that, when present, predicted the largest increase in antibody titers compared to when attribute was not present; analysis was performed using tobit regression for each predictor, with adjustment for chronic inflammatory disease/healthy status, age, sex, and vaccine type. 95% CI = 95% confidence interval.
Figure 3.
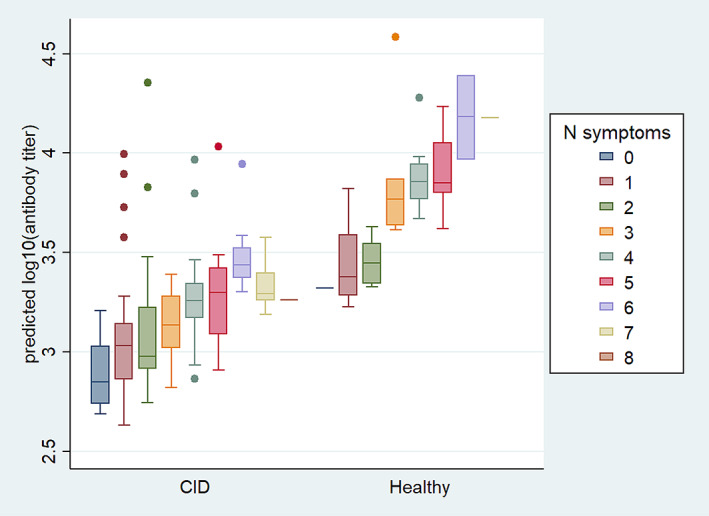
Predicted antibody titers following second dose by number of symptoms in patients with chronic inflammatory disease (CID) and healthy control subjects. The regression model depicts change in anti–SARS–CoV‐2 spike IgG ± antibody titer with each increase of 1 endorsed symptom following second dose of vaccine in CID patients and healthy controls.
Among all individual symptoms, the symptom with the strongest association after each dose of vaccine was site pain after first dose and fatigue after second dose. The presence of site pain following the first dose of vaccine demonstrated an increase of 105% (range 7.9%, 292%) (P = 0.03) in antibody titer compared to the antibody response associated with absence of site pain, and presence of fatigue after the second dose demonstrated an increase of 114% (range 27.8%, 257%) (P = 0.004) in antibody titer. Notably in CID patients, the presence of fatigue following the second dose of vaccine was associated with the greatest increase in antibody titer compared to other symptoms (138% [range 27%, 346%]; P = 0.007).
DISCUSSION
This study is one of the first to examine reactogenicity of the novel mRNA SARS–CoV‐2 vaccines among patients with CID and the relationship between reactogenicity and vaccine response. In the present work, we found patients with CID experienced more adverse events and more severe adverse events following the first dose of the novel SARs–COV‐2 mRNA vaccines but overall had a similar adverse event profile as healthy controls following the second dose. Most notably, we found the number of adverse events reported was associated with increased antibody titer, demonstrating a link between reactogenicity and immunogenicity in patients with CID as well as healthy controls. The findings from this study will help provide the much‐needed information on the adverse event profile of the novel SARS–CoV‐2 vaccines and help to better inform patients and providers.
Concerns regarding side effect profile of the novel mRNA vaccines have been shown to be a contributor to vaccine hesitancy in not only the general population, but also in patients with CID (21, 22, 23). In this study, we demonstrate differences in reactogenicity profile between the general population and CID patients following the first dose of vaccine. This finding could be potentially due to the existing underlying immune dysregulation in patients with CID or possible alterations in disease activity. Overall, however, when compared to healthy controls, there were not significant differences among CID patients following the second dose of vaccine, which has been associated with more severe adverse events than the first dose. Also reassuringly, burden of severe adverse events experienced by patients with CID following vaccination mirrored those reported on a national level (8, 9).
While we were unable to determine significant differences in reactogenicity among specific CID diseases or medications due to small, stratified sample sizes, the data did show a trend suggesting increased reactogenicity in SpA patients, specifically with increased severity of symptoms following second dose of vaccine and increased fatigue following both doses. This finding may be attributed to SpA patients temporarily suspending use of nonsteroidal antiinflammatory drugs, which is first‐line treatment for axial SpA, around time of vaccination (11). This in turn could lead to increased disease activity, including fatigue. In both CID patients and control subjects, similar to prior studies, we demonstrate that younger patients and female patients had higher adverse event burden than their older and male counterparts (15, 24, 25). Differences in immune system competency, hormone status, as well as recognition and reporting of symptoms may explain some of these variations among age and sex (16, 25).
It has been previously hypothesized that increased symptomatology following vaccination may be indicative of increased immune response; however, to date, that has yet to be demonstrated in vaccine studies. In this study, we demonstrate a link between reactogenicity and immunogenicity with increased adverse events and certain specific adverse events associated with increased antibody titers. This finding, present among CID patients and control subjects, mechanistically supports the underlying physiology of vaccination with immunity emerging via stimulation of the immune system (26). While it is still unclear what clinical significance these differences in antibody titers may have, reactogenicity may be a signal for robustness of immune response in certain populations.
There were both strengths and limitations of the present study. This was one of the first studies to examine reactogenicity and its link with immunogenicity of the novel mRNA SARS–CoV‐2 vaccines in patients with CID. We applied prospective data to a relatively large and well‐characterized cohort of patients from 2 different centers with a diverse number of CIDs. Limitations of the present study include the control population, which was notably different in age and sex between study sites and distinct from the CID cohort. While we attempted to control for these variables using multivariable models, residual confounding cannot be excluded. There were also differences with regard to reactogenicity between the 2 study sites, which may be reflective of the population eligible for vaccination at each site. Additionally, given differences in initial protocol between sites, there was a reduction in sample size for symptom severity, which could imply less power for analyses. However, given there was a highly significant difference at dose 1, and an effect size close to 1 for dose 2, sample size alone is unlikely to affect these conclusions. We did lack the ability to compare across cohorts and therefore rule out latent site‐specific effects for severity. Overall, it was important to include these 2 sites to include a more representative study population. Additionally, given our CID patients included multiple disease states and varying medication regimens, including combination therapy, it was difficult to isolate differences based on specific disease states or medication exposures.
In conclusion, we examined the reactogenicity and subsequent immunogenicity of patients with CID and found that although CID patients had more symptoms following the first dose of SARS–CoV‐2 vaccine, their reactogenicity following full vaccination was similar to healthy controls and the general public. The presence of more symptoms and select adverse events following vaccination was associated with increased SARS–CoV‐2 antibody titers. Overall, this study serves to provide much needed safety data for patients with CID and as an initial step to better understand the link between reactogenicity and immunogenicity following SARS–CoV‐2 vaccines.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Yang had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Yang, W. Kim, Ellebedy, Ciorba, Paley, Deepak, A. Kim, Katz, Matloubian, Nakamura, Gensler.
Acquisition of data
Yang, Paez, Carividi, Demissie, Pawar, El‐Qunni, McMorrow, Schriefer, Huang, Kinnett, Klebert, Haile, Ellebedy, Ciorba, Paley, Deepak, A. Kim, Katz, Matloubian, Nakamura, Gensler.
Analysis and interpretation of data
Yang, Taylor, O'Halloran, Presti, W. Kim, Ellebedy, Ciorba, Paley, Deepak, A. Kim, Katz, Matloubian, Nakamura, Gensler.
Supporting information
Disclosure Form
Supplementary Table 1: Outcomes in CID patients vs. Healthy controls combined and by study site, adjusted for age, gender and vaccine*
Supplementary Table 2: Mixed models of age 65+, gender, and vaccine, with site as random effect*
Supplementary Table 3: Reactogenicity predictors* of increase in antibody titer
Primarily supported by The Leona M. and Harry B. Helmsley Charitable Trust, Marcus Program in Precision Medicine Innovation, NIH grant UL1TR002345 from the National Center for Advancing Translational Sciences, and NIH grants P30‐AR‐070155 and T32‐AR‐079068 from the National Institutes of Arthritis and Musculoskeletal and Skin Diseases (on behalf of the University of California, San Francisco).
Author disclosures are available at https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1002%2Facr.24894&file=acr24894‐sup‐0001‐Disclosureform.pdf.
REFERENCES
- 1. Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid‐19 vaccine. N Engl J Med 2020;383:2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA‐1273 SARS‐CoV‐2 vaccine. N Engl J Med 2021;384:403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single‐dose Ad26.COV2.S vaccine against Covid‐19. N Engl J Med 2021;384:2187–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gao Y, Chen Y, Liu M, Shi S, Tian J. Impacts of immunosuppression and immunodeficiency on COVID‐19: a systematic review and meta‐analysis. J Infect 2020;81:e93–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Strangfeld A, Schäfer M, Gianfrancesco MA, Lawson‐Tovey S, Liew JW, Ljung L, et al. Factors associated with COVID‐19‐related death in people with rheumatic diseases: results from the COVID‐19 Global Rheumatology Alliance physician‐reported registry. Ann Rheum Dis 2021;80:930–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pogue K, Jensen JL, Stancil CK, Ferguson D, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential COVID‐19 vaccination in the United States. Vaccines (Basel) 2020;8:582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, et al. Factors associated with US adults' likelihood of accepting COVID‐19 vaccination. JAMA Netw Open 2020;3:e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gee J, Marquez P, Su J, et al. First month of COVID‐19 vaccine safety monitoring: United States, December 14, 2020–January 13, 2021. MMWR Morb Mortal Wkly Rep 2021;70:283–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chapin‐Bardales J, Gee J, Myers T. Reactogenicity following receipt of mRNA‐based COVID‐19 vaccines. JAMA 2021;325:2201–2. [DOI] [PubMed] [Google Scholar]
- 10. Connolly CM, Ruddy JA, Boyarsky BJ, Barbur I, Werbel WA, Geetha D, et al. Disease flare and reactogenicity in patients with rheumatic and musculoskeletal diseases following two‐dose SARS–CoV‐2 messenger RNA vaccination. Arthritis Rheumatol 2022;74:28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Botwin GJ, Li D, Figueiredo J, Cheng S, Braun J, McGovern DP, et al. Adverse events after SARS‐CoV‐2 mRNA vaccination among patients with inflammatory bowel disease. Am J Gastroenterol 2021;116:1746–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berkowitz EM, Moyle G, Stellbrink HJ, Schürmann D, Kegg S, Stoll M, et al. Safety and immunogenicity of an adjuvanted herpes zoster subunit candidate vaccine in HIV‐infected adults: a phase 1/2a randomized, placebo‐controlled study. J Infect Dis 2015;211:1279–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vink P, Ramon Torrell JM, Sanchez Fructuoso A, Kim SJ, Kim S, Zaltzman J, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in chronically immunosuppressed adults following renal transplant: a phase III, randomized clinical trial. Clin Infect Dis 2020;70:181–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ou MT, Boyarsky BJ, Chiang TP, Bae S, Werbel WA, Avery RK, et al. Immunogenicity and reactogenicity after SARS‐CoV‐2 mRNA vaccination in kidney transplant recipients taking belatacept. Transplantation 2021;105:2119–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Miraglia JL, Abdala E, Hoff PM, Luiz AM, Oliveira DS, Saad CG, et al. Immunogenicity and reactogenicity of 2009 influenza A (H1N1) inactivated monovalent non‐adjuvanted vaccine in elderly and immunocompromised patients. PloS One 2011;6:e27214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hervé C, Laupèze B, Del Giudice G, Didierlaurent AM, Tavares Da Silva F. The how's and what's of vaccine reactogenicity. NPJ Vaccines 2019;4:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Deepak P, Kim W, Paley MA, Yang M, Carvidi AB, Demissie EG, et al. Effect of immunosuppression on the immunogenicity of mRNA vaccines to SARS‐CoV‐2: a prospective cohort study. Ann Intern Med 2021;174:1572–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boyarsky BJ, Werbel WA, Avery RK, Tobian AA, Massie AB, Segev DL, et al. Antibody response to 2‐dose SARS‐CoV‐2 mRNA vaccine series in solid organ transplant recipients. JAMA 2021;325:2204–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tobin J. Estimation of relationships for limited dependent variables. Econometrica 1958;26:24. [Google Scholar]
- 20. Amemiya T. Tobit models: a survey. J Econom 1984;24:3–61. [Google Scholar]
- 21. Priori R, Pellegrino G, Colafrancesco S, Alessandri C, Ceccarelli F, Di Franco M, et al. SARS‐CoV‐2 vaccine hesitancy among patients with rheumatic and musculoskeletal diseases: a message for rheumatologists. Ann Rheum Dis 2021;80:953–4. [DOI] [PubMed] [Google Scholar]
- 22. Gaur P, Agrawat H, Shukla A. COVID‐19 vaccine hesitancy in patients with systemic autoimmune rheumatic disease: an interview‐based survey. Rheumatol Int 2021;41:1601–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ko T, Dendle C, Woolley I, Morand E, Antony A. SARS‐COV‐2 vaccine acceptance in patients with rheumatic diseases: a cross‐sectional study. Hum Vaccines Immunother 2021:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cook IF. Sex differences in injection site reactions with human vaccines. Hum Vaccin 2009;5:441–9. [DOI] [PubMed] [Google Scholar]
- 25. Klein SL, Jedlicka A, Pekosz A. The Xs and Y of immune responses to viral vaccines. Lancet Infect Dis 2010;10:338–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moser M, Leo O. Key concepts in immunology. Vaccine 2010;28 Suppl 3:C2–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure Form
Supplementary Table 1: Outcomes in CID patients vs. Healthy controls combined and by study site, adjusted for age, gender and vaccine*
Supplementary Table 2: Mixed models of age 65+, gender, and vaccine, with site as random effect*
Supplementary Table 3: Reactogenicity predictors* of increase in antibody titer


