Abstract
Background
In 2014, the Burkina Faso government launched the Seasonal Malaria Chemoprevention (SMC) programme. Expected benefit was a 75% reduction of all malaria episodes and a 75% drop of severe malaria episodes. This study assessed SMC efficiency on malaria morbidity in the country after 2 years of implementation.
Methods
Quasi-experimental design comparing changes in outcomes during the high transmission period (August–November) between SMC and non-SMC health districts before (2013–2014) and after intervention (two rounds in 2015 and 2016). Health indicators (number of uncomplicated malaria cases (UM) and severe malaria cases (SM)) from 19 health districts (8 in intervention and 11 in comparison group) were extracted from the District Health Information System (DHIS2)-based platform including health facilities data. Effect on incidence was assessed by fitting difference-in difference mixed-effects negative binomial regression model at a log scale.
Results
The two rounds of SMC were associated with a reduction of UM incidence (ratio of incidence rate ratio (IRR) 69% (95% CI 55–86%); p = 0.001) and SM incidence (ratio of IRR = 73% (55–95%), p = 0.018) among under five children.
Conclusion
The two rounds of SMC had a significant effect on the reduction of malaria cases in under five children. This additional evidence on the effectiveness of SMC, using routine data, support the need to sustain its implementation and consider expansion to eligible areas not yet covered.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12936-022-04172-z.
Keywords: Seasonal malaria chemoprevention, Evaluation, Impact, Malaria, Burkina Faso
Background
Malaria control has yielded rewarding achievements in reducing the disease burden in past 15 years due to global revived interest and significant increase in funding [1], which led to the scale-up of multiple control interventions in endemic countries. These control interventions include appropriate and prompt management of uncomplicated with effective and severe cases, the provision of insecticide-treated nets (ITN), indoor residual spraying (IRS), intermittent preventive treatment for pregnant women (IPTp) and, lately, seasonal malaria chemoprophylaxis (SMC) [2].
The World Health Organization (WHO) recommended SMC for malaria prevention in children under five living in markedly seasonal malaria transmission areas in the Sahel region for eligible countries in 2012 [3, 4]. The SMC is defined as “the intermittent administration of full treatment courses of an anti-malarial medicine during the malaria season to prevent malarial illness with the objective of maintaining therapeutic anti-malarial drug concentrations in the blood throughout the period of greatest malarial risk” [5]. As of 2019, twelve countries have been implementing SMC in the Sahel subregion [6], including Burkina Faso, which adopted and launched SMC with sulfadoxine-pyrimethamine + amodiaquine (SP-AQ) in 2014 [7], gradually deployed in health districts over a 6-year period until 2019 [8–12], alongside several other ongoing malaria control interventions, and strengthening of health surveillance system to better monitor and measure achievements.
The improved quality of malaria surveillance data provides an opportunity for assessing the impact of SMC country-wide. Most of the experimental studies supporting the recommendation of SMC in children were conducted in West Africa [13–17], but there is limited evidence for its effect in real-life large-scale conditions. Indeed, until recently few impact evaluations were conducted in the Sahel region, and they found results with different magnitude [18–20]. In Burkina Faso, an impact evaluation using point and period prevalence of parasitaemia, prevalence of moderate to severe anaemia, and history of reported fever in last 14 days as outcome measures was carried out and found a protective efficacy of 51% and 62%, respectively. However, this study was conducted in only one health district, and this could have limited its capacity to capture disparities between health districts in which the SMC was later deployed [9]. Recently, Access-SMC partnership [21] assessed the impact of SMC in the reduction of malaria incidence in seven countries including Burkina Faso. However, at the time of their impact evaluation, data on severe malaria cases were not available for the year 2016 in Burkina Faso and only cases in district hospitals attributed to malaria were considered. The 2016 severe malaria and deaths data in primary health facilities and district hospitals are now available in Burkina Faso, therefore, accounting for both cases and deaths in these primary health facilities and all cases in each year could provide more robust evidence of the effect of SMC in the country.
Given the extensive resources involved in SMC it is crucial to assess how well it works to better inform potential adjustments to optimize the impact of the intervention. This study evaluates the effect of the SMC in children under five living in Burkina Faso during two rounds of implementation using data from the routine health information system.
Methods
Country profile
Burkina Faso is a West African country covering an area of 274,200 km2 with an estimated population of 20,870,060 inhabitants in 2019. The country is located at a transitional zone between the arid Sahara in the north and the Sudanian zone in the south. The start, duration of rains, total number of rainy days are highly variable and defined by three ecoclimatic zones: Sahelian zone in the north, Sudanian zone in the south and Sudano-Sahelian zone in between with a total annual rainfall/average annual temperature of less than 600 mm/29 °C, 900–1200 mm/28 °C and 600–900 mm/27 °C, respectively [22–24]. The transmission of malaria is stable, occurring throughout the year with a peak during the rainy season (June–September).
Regarding the health system structure, there are currently three levels: the central level elaborates health policies, the regional level coordinates the implementation, and the district level is operational with a network of health centres in relation with district or regional hospitals. The doctor-nurse-midwife/population and primary health facility/population ratios were 8 and 0.9 per 10,000 inhabitants in 2018 [25], respectively. In the country, SMC started in 2014 in a few districts, then extended in 2015 and in 2016. In 2019, every district in Burkina Faso implemented SMC [7–12].
Study design
The present study is a two-group two-period quasi-experiment with a pre- and post-intervention observations in the country health districts. The intervention being SMC in children under five. In Burkina Faso, the SMC intervention consists in the administration of a monthly 3-day course of SP-AQ (a single dose of SP + 3 days-course of AQ) to children under five on a monthly basis in the rainy months (July–October). The SP-AQ doses are administered by community health workers under the supervision of health providers operating the primary health facility [2].
Selection of SMC and non-SMC health districts
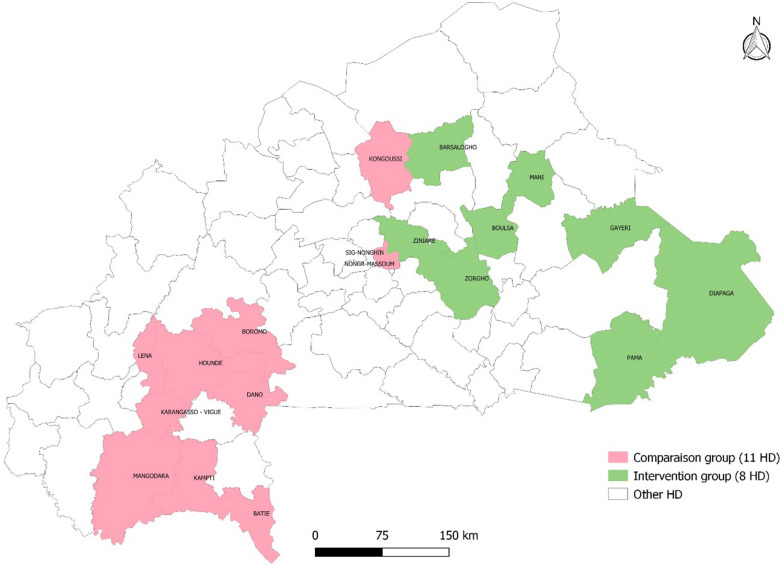
In 2013, the health statistics yearbook listed 70 health districts (primary health facilities and district hospitals data). The inclusion criteria for the intervention group were SMC implemented in 2015 and 2016 [8] and for the comparison group, no SMC before 2017 [7–9]. The exclusion criterion was the presence of a regional or teaching hospital in the district for both groups. Health districts with such hospitals were excluded because their data reported do not discriminate patients from SMC and no SMC districts. Diébougou health district in which IRS was conducted for 3 consecutive years from 2010 was excluded. Indeed, evidence from the Garki project suggests that malaria vector populations, and therefore transmission, may not surge back early after the end of spraying campaigns [6]. In this respect, the Diébougou health district might be different from the other health districts in terms of transmission intensity. The selection process and outcome are summarised in Figs. 1 and 2. Figure 2 presents SMC and non–SMC health districts.
Fig. 1.
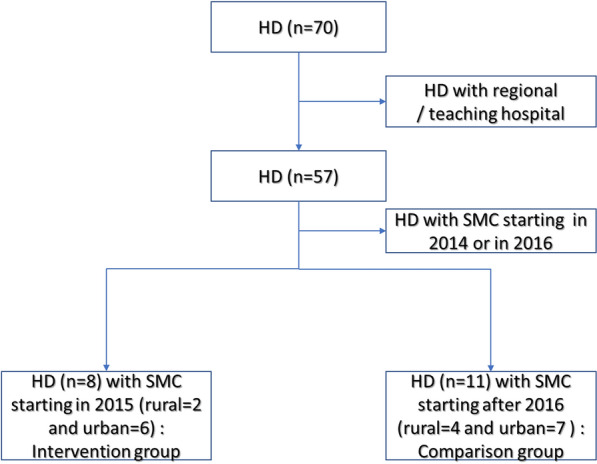
Health district selection flowchart. HD health district, SMC seasonal malaria chemoprophylaxis
Fig. 2.
Map of the selected health districts SMC in green and no-SMC in pink
Data sources
Data were extracted from the online national health data repository which is a District Health Information System (DHIS2)-based platform called ENDOS-BF (Entrepôt National de Données Sanitaires du Burkina Faso), operative as of 2013. The monthly data reports on primary health facilities and district hospitals activities sent to the health district, are aggregated in ENDOS-BF.
Selection of study variables
Among expected benefit of SMC, there was a 75% drop of the incidence of all malaria episodes and a 75% drop of the incidence of severe malaria episodes. The study investigated the effect of the SMC on malaria morbidity based on two outcomes variables collected from primary health facilities and district hospitals to comply with the national policy of malaria case definition: incidence of uncomplicated malaria (UM), i.e. all presumptive cases based on clinical symptoms or confirmed parasitological cases of a malaria rapid diagnostic tests (RDT) or microscopy and incidence of severe malaria cases in children (SM) i.e. confirmed cases of malaria with signs of severe illness and/or evidence of vital organ dysfunction who required hospitalization [7]. The incidence of UM in children under five is defined as the number of UM reported cases, relative to the total population of children under five living in the health district. The incidence of SM in children under five is defined as the number of SM reported cases, relative to the total population of children under five living in the health district. There were also the data for older age groups (5–14 years and 15 years and more) to control for confounding temporal trends.
Data quality assurance
Data quality audits are conducted periodically in public primary health care facilities by supervisory teams from the district level to check consistency between source data (registers) and data reported in the monthly activities reports. Besides, in parallel to the mandatory global monthly activity reports, each health facility produces a weekly telegram on key health indicators among which uncomplicated and severe malaria cases in children under five. The figures reported to the Health Statistics Directorate of the Ministry of Health should match those of the aggregated weekly telegrams reported to the disease surveillance directorate of the same ministry. ENDOS-BF has built-in quality, which enables central data managers to check several dimensions of quality in the course of data entry and generate queries intended for districts data managers [26]. An assessment of ENDOS-BF in 2017 reported data accuracy, data timeliness, data completeness, and data reliability of 83%, 80%, 78% and 87%, respectively [27]. Moreover, the data discrepancy index between the source and the reported data improved from 61% in 2013 to 80% in 2018 [28].
Data analysis
Background characteristics of health districts in intervention and comparison groups
The study health districts were comparable in many respects at baseline (2013). The differences in surface area is attributable to one significantly wider district (Diapaga) in the intervention group. There was no statistical difference in terms of average annual rainfall and average annual temperature (overlapping of 95% confidence interval). The ratio population per health worker, in the intervention districts is lower compared to comparison districts. The proportion of population living at less than 5 km away from a health facility is also substantially lower in the intervention districts. Globally, bed net ownership was lower in the SMC group compared to non-SMC group in 2014, and bed net use proportion are similar in both groups before SMC implementation (Table 1).
Table 1.
Summary of study health districts characteristics in 2013
| Background characteristics | SMC health districts (intervention) | Non-SMC health districts (comparison) |
|---|---|---|
| Total surface area (km2) | 46,785 | 33,833 |
| Average annual rainfall (mm) (95% CI) | 794 (640, 948) | 752 (629, 876) |
| Average monthly temperature (°C) (95% CI) | 28.1 (27.7, 28.6) | 28.0 (27.6, 28.4) |
| Total population | 2,042,236 | 2,133,367 |
| Total number of primary health facilities | 212 | 199 |
| Total health staff | 1150 | 2173 |
| Population/health facility ratio | 9633 | 10,720 |
| Population/health care worker ratio | 1776 | 981 |
| Population of children under five | ||
| Total | 422,272 | 382,191 |
| Proportion | 20.7% | 17.9% |
| Population at < 5 km away from the health facility | ||
| Total | 808,066 | 1,363,340 |
| Proportion | 39.6% | 63.9% |
| Insecticide treated nets in 2014a | ||
| Ownership | 75.4% | 82.2% |
| Use | 88.0% | 87.2% |
aWe obtained this information from the Malaria Indicator Survey (MIS) conducted in 2014. The MIS was not designed to provide estimates at health districts level. To address this issue, we fitted a Bayesian binomial model to the aggregated data on ITN ownership and use to estimate them at the district level
Statistical analysis (descriptive and regression)
For each outcome (uncomplicated malaria incidence and severe malaria incidence) and each group, the average difference between the post-(combining the data of first round August 1 to November 30, 2015, and second round August 1 to November 30, 2016) and pre-(August 1 to November 30, 2013, and August 1 to November 30, 2014) intervention periods were calculated as previously done [21]. The average change was then subtracted in the outcomes over time in health districts not implementing SMC from that of health districts implementing the SMC to single out effect of SMC. The parallel trend assumption guides the use of the difference in difference (DID) analysis and assumes that no time-varying differences exist between the SMC and comparison groups. For that purpose, a test was performed verifying whether variations in outcomes were equivalent between the two groups during the pre-intervention period. Due to overdispersion in the data, a mixed-effects negative binomial regression model was fitted. Given the geographic variation in malaria incidence, heath districts were included as random intercepts.
In 2016, Burkina Faso removed patient charges for children under 5 years and for pregnant women. This was associated with a marked increase in outpatient attendance and hence a marked increase in reported case of malaria. For that, the authors considered the variable as a control variable in the difference-in-difference analysis to estimate the impact of SMC accurately.
The validity of the regression was included by comparing Akaike Information Criterion (AIC) of Poisson regression and binomial negative Regression. With the lowest AIC, a mixed-effects negative binomial regression model was fitted to estimate the effect of SMC on incidence of uncomplicated malaria cases, and severe malaria cases. Each regression model included time variable (pre-SMC period vs post-SMC period), SMC variable (SMG group vs non-SMC group, the free healthcare variable (Free_Healthcare) and population size (children under five aged in each district) as an offset.
The empirical model estimated can be characterized as:
where Yit is number of cases of interest provided by district i in time period t (in months), time is a variable capturing the pre (2013–2014) and post-SMC period (2015 and 2016), SMC is an indicator for a health district being in a SMC group or non-SMC group, Free_healthcare variable for patient removing charges, SMC * Time the interaction that captures the DID estimator at log scale, the effect of the implementation of two rounds of SMC in 2015 and 2016 and the error term.
From the mixed-effects negative binomial regression models, ratio of incidence, rate ratio with 95% confidence interval and p-values were estimated. Statistical significance was met for p-values < 0.05. All analyses were performed using Stata (version 16; StataCorp, College Station, TX, USA).
Results
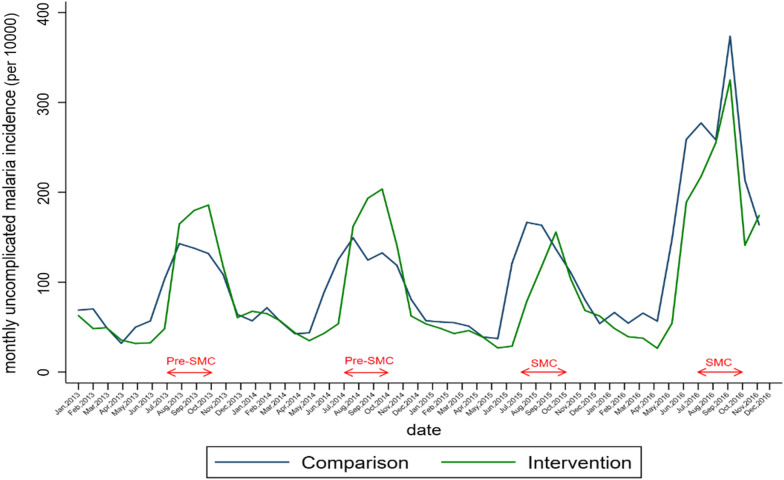
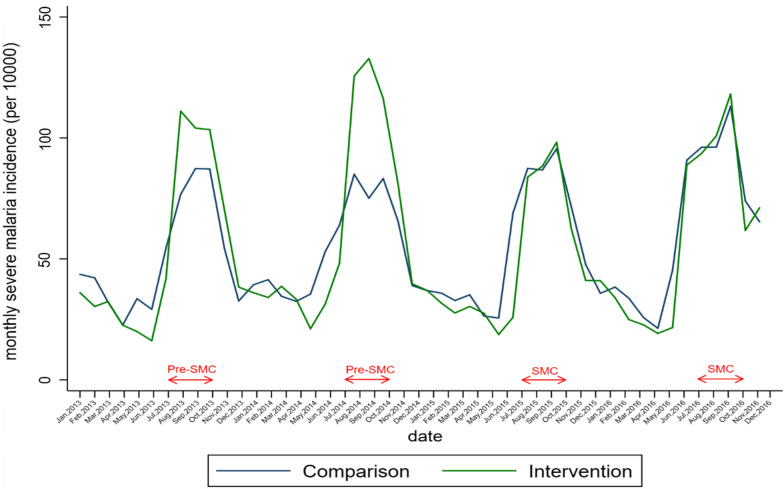
Crude trends in uncomplicated malaria and severe malaria monthly incidence
Table 2, Figs. 3 and 4 present the crude trends of uncomplicated malaria and severe malaria monthly incidence respectively. Before the introduction of SMC, the crude monthly uncomplicated malaria incidence during high transmission period was higher in SMC group decreased after the two rounds of SMC to the level of the comparison group (Table2, Fig. 3). Before the establishment of SMC, the SMC group showed a high evolution of crude monthly severe malaria incidence during the high transmission period to that of control. Following the first and the second round of SMC implementation, there was a decline in the SMC group. (Table 2, Fig. 4).
Table 2.
Number of uncomplicated and severe malaria cases, testing rate by group and year (August–November) among children under 5 years, 2013–2016
| 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|
| Uncomplicated malaria cases | ||||
| Comparison group | 209,816 | 216,047 | 244,386 | 487,104 |
| SMC group | 264,905 | 293,816 | 196,534 | 387,255 |
| Severe malaria cases | ||||
| Comparison group | 13,071 | 13,244 | 14,796 | 15,975 |
| SMC group | 14,887 | 17,483 | 12,746 | 14,360 |
| Malaria suspected cases | ||||
| Comparison group | 224,102 | 239,942 | 305,405 | 473,295 |
| SMC group | 279,499 | 311,299 | 209,756 | 364,534 |
| Suspected malaria cases tested | ||||
| Comparison group | 127,912 | 184,858 | 249,880 | 485,624 |
| SMC group | 166,575 | 259,008 | 219,637 | 351,972 |
| Malaria confirmed cases | ||||
| Comparison group | 115,702 | 168,142 | 221,919 | 394,583 |
| SMC group | 155,441 | 239,876 | 197,776 | 279,676 |
| Testing rates (%) | ||||
| Comparison group | 57.1 | 77.0 | 81.8 | 102.6 |
| SMC group | 59.6 | 83.2 | 104.7 | 96.6 |
| Test positivity rate (%) | ||||
| Comparison group | 90.5 | 91.0 | 88.8 | 81.3 |
| SMC group | 93.3 | 92.6 | 90.0 | 79.5 |
Fig. 3.
Monthly trends of uncomplicated malaria incidence in health districts before and after SMC implementation
Fig. 4.
Monthly trends of severe malaria incidence in health districts before and after SMC implementation
The crude trends in uncomplicated malaria and severe malaria monthly incidence for older age group was presented in Additional file 1: Figs. S1, S2. Malaria testing rates was higher in the SMC group compared to non-SMC group between 2013 and 2015, even in 2016 the proportion was higher in the comparison group compared to SMC group. However, the test positivity rate was similar for both groups during the study period 2013–2016 (Table 2).
Effect of seasonal malaria chemoprevention on malaria burden
Compared to the period before implementation and after the two rounds of SMC, incidence rates of UM increased in the comparison group [incidence rates ratio (IRR): 1.05 (95% CI 0.92–1.20)] while in the SMC group, the incidence rate was significantly lower [IRR: 0.72 (95% CI 0.63–0.82)]. The ratio of the IRR in SMC and comparison group [69% (95% CI 55–86%; p = 0.001)] reflects an important difference in the evolution of UM incidence rates between the two groups, in favour of the SMC group (Table 3). Compared to the period before implementation and that after the two rounds of SMC, incidence rates of SM increased in the comparison group [incidence rates ratio: 1.08 (95% CI 0.93–1.27)] while in the SMC group, the incidence rate was significantly lower [IRR: 0.79 (95% CI 0.68–0.91) 0.64–0.95)]. The ratio of the IRRs in SMC and comparison group [73% (95% CI 55–95%, p = 0.018)] reflects an important difference in the evolution of SM incidence rates between the two groups, in favour of the SMC group (Table3). The positive impact of SMC among children under five was not observed among older age group (Additional file 1: Tables S1, S2).
Table 3.
Effect of seasonal malaria chemoprevention on incidence of uncomplicated and severe malaria cases
| Period | Mean incidence rates (100 persons-months) | Comparison | Intervention | IRRa ratios (%) (95% CI) | p | |
|---|---|---|---|---|---|---|
| Comparison districts (n = 11) | Intervention districts (n = 8) | IRR (95% CI) | IRR (95% CI) | |||
| Uncomplicated malaria | ||||||
| Before | 12.7 | 15.0 | 1 | 1 | 1 | |
| After | 13.2 | 10.7 | 1.05 (0.92–1.20) | 0.72 (0.63–0.82) | 69 (55–86) | 0.001 |
| Severe malaria | ||||||
| Before | 7.0 | 8.9 | 1 | 1 | 1 | |
| After | 7.5 | 7.0 | 1.08 (0.93–1.27) | 0.79 (0.68–0.91) | 73 (55–95) | 0.018 |
IRR incidence rate ratio obtained from a mixed-effects negative binomial regression model with random intercept for health districts and robust standard error
aRatio of IRR intervention vs. IRR comparison
Discussion
This study assessed the effect of seasonal malaria chemoprevention in children under five on malaria morbidity using routine data in Burkina Faso from 2013 to 2016. After two rounds of SMC, we observed a significant decrease in the incidence of uncomplicated malaria cases and severe malaria cases.
These findings are in line with the well-documented effectiveness of SMC in reducing severe malaria incidence. In a quasi-experimental study based on one comparison district (Bafoulabe) and one intervention district in Kita, Mali, Diawara et al. found that the SMC reduced severe malaria incidence by 72% [18] in 2014 compared to 2013. A previous study conducted in one district (Kaya, Burkina Faso) at the early stage of the SMC implementation in the country showed that it could reduce febrile episodes by 46% but did not specifically investigate its effect on severe malaria [19]. The results also confirm the findings of ACCESS SMC on a large scale in Burkina Faso. By also using routine data in Burkina Faso, the associated reduction in SM cases with SMC estimated from Poisson regression was 27.4% in 2015 [21].
Moreover, a large-scale randomized trial published in 2021, in which the efficacy of SMC was estimated by comparing malaria incidence in children who received SMC plus the malaria vaccine with children who receive only the malaria vaccine [29]; and a re-analysis of large scale randomized trial of SMC combined with azithromycin [30] have shown results, are consistent with a high level of efficacy of SMC.
This study also observed an increase in malaria incidence in 2016. This calls for the exploration of new strategy like a combination of SMC with malaria vaccine, strengthening SP resistance monitoring, extend age group of target population, expending the period to at least 3 months after the high transmission period, active surveillance at the community level. A positive contribution of combination of malaria vaccine and SMC on malaria burden has been reported recently [31].
This study demonstrates the valued added of using routine data to effectively monitor and evaluate the effect on malaria interventions at the subnational level. This calls for a need to continuing strengthening routine information systems for improved quality of malaria surveillance data and use of these data to inform program implementation. In line with the High Burden High Impact Strategy (HBHI) regular subnational assessment of change in malaria burden, is necessary for defining appropriate intervention package targeted to specific area.
Limitations
There are a number of limitations to this study. The relative contribution of other ongoing interventions that could have an effect on malaria morbidity (e.g. ACT for effective treatment, use of ITNs and proper management of malaria cases) and SMC coverage was not assessed. Therefore, these results cannot be attributed solely to SMC because it is an additional intervention to others, such as IPTp with SP, the use of ITN (ITN. mass distribution campaign and routine distribution) and proper management of malaria cases in the selected area. Moreover, overdiagnosis is likely to be a feature of most programmatic data because diagnosis of malaria in the routine system relies on the use of RDTs. However, even if this burden were to be discounted to account for potential overdiagnosis, it would remain substantial.
Variation in the implementation of strategy between rounds and/or districts can occur and limit the external validity. According to research, repeated cycles of SMC could contribute to reduce overall malaria transmission [32]. In this study it was impossible to investigate this hypothesis because this only focused on the use of routine data to assess SMC impact. Also, the proportion of malaria cases (uncomplicated and severe) not captured by ENDOS-BF and exclusion of districts with regional or teaching hospitals can limit the SMC impact. Due to their attractiveness, they might have concentrated cases of severe malaria from selected districts, which do not have a regional or teaching hospital. Thus, this study can be insufficiently powered to detect SMC impact, especially on severe malaria.
However, despite its limitations, the authors have mostly looked at SMC impact from the data perspective because other context issues related SMC are already extensively documented in the literature. SMC is an effective strategy if well implemented with effective drug, perfect timing, and optimal coverage. Moreover, SMC in mainly for burden reduction, not elimination strategy. It is then critical to put in place a function data system to monitor SMC and measure its impact.
Conclusions
The two rounds of SMC implementation were associated with a reduction in uncomplicated and severe malaria cases among children under 5 years. This additional evidence on the effectiveness of SMC, using routine data, support the need to sustain its implementation and consider expansion to eligible areas not yet covered. There is also a need to continue efforts in strengthening routine health information system to provide quality data for monitor coverage and assess impact on malaria burden at the subnational level.
Supplementary Information
Additional file 1: Figure S1. Monthly trends of uncomplicated malaria incidence in health districts before and after SMC implementation among older age group (5–14 years old and 15 years and more). Figure S2. Monthly trends of severe malaria incidence in health districts before and after SMC implementation among older age group (5–14 years old and 15 years and more). Table S1. Effect of seasonal malaria chemoprevention on incidence of uncomplicated malaria cases among older age group (5–14 years old and 15 years and more). Table S2. Effect of seasonal malaria chemoprevention on incidence of severe malaria cases among older age group (5–14 years old and 15 years and more).
Acknowledgements
The authors thank Cheick Saïd Compaoré from the National Malaria Control Programme, Ministry of Health, Burkina Faso for facilitating SMC data collection. A special thanks to Tiga David Kangoye and Adama Gansané from the Centre National de Recherche et de Formation sur le Paludisme (CNRFP), Burkina Faso for data collection and logistic support about data collection and Sekou Samadoulougou and Michèle Wilmet-Dramaix for editing support and helpful advice regarding statistical aspects.
Abbreviations
- AIC
Akaike Information Criterion
- CI
Confidence interval
- CNRFP
Centre National de Recherche et de Formation sur le Paludisme
- DHIS
District Health Information System
- DID
Difference in Difference
- ENDOS-BF
Entrepôt National de Données Sanitaires du Burkina Faso
- INSD
Institut national de la statistique et de la démographie
- IPTp
Intermittent Preventive Treatment for pregnant women
- IRR
Incidence rate ratio
- ITN
Insecticides-treated bed nets
- LLIN
Long-lasting insecticidal nets
- RDT
Rapid diagnosis test
- SMC
Seasonal malaria chemoprevention
- SMC
Severe malaria
- SP–AQ
Sulfadoxine–pyrimethamine + amodiaquine
- ULB
Université libre de Bruxelles
- UM
Uncomplicated malaria
- WHO
World Health Organization
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Funding
No funding is dedicated to this study.
Availability of data and materials
All data were extracted from the national health information system as part of routine care. Data that support the findings of this study are available at the Ministry of Health in Burkina Faso.
Declarations
Ethics approval and consent to participate
The data used in the present study was collected in the course of routine healthcare provision and is aggregated with no personal information in the sources. This data, stored in the health data repository is ultimately made publicly available in the yearly health statistics book of the ministry of health. Consent was waived by the ethics committee; therefore, individual patient consent was not sought.
Consent for publication
Not applicable.
Competing interests
The authors do not have any conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haakenstad A, Harle AC, Tsakalos G, Micah AE, Tao T, Anjomshoa M, et al. Tracking spending on malaria by source in 106 countries, 2000–16: an economic modelling study. Lancet Infect Dis. 2019;19:703–716. doi: 10.1016/S1473-3099(19)30165-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministère de la Santé. Directives nationales pour la prise en charge du paludisme dans les formations sanitaires du Burkina Faso. Programme National de Lutte contre le Paludisme; 2014. https://www.severemalaria.org/sites/mmv-smo/files/content/attachments/2017-03-13/burkina%20faso%20treatment%20guidelines.pdf.
- 3.WHO. Policy recommendation: seasonal malaria chemoprevention (SMC) for Plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. Geneva: World Health Organization; 2012. https://apps.who.int/iris/handle/10665/337978.
- 4.WHO. Policy recommendation on intermittent preventive treatment during infancy with sulphadoxine–pyrimethamine (SP-IPTi) for Plasmodium falciparum malaria control in Africa. Geneva: World Health Organization; 2010. https://apps.who.int/iris/handle/10665/337977.
- 5.WHO. Report of the technical consultation on seasonal malaria chemoprevention (SMC)/Chimio-prévention saisonnière du paludisme (CSP). Geneva: World Health Organization; 2011. https://www.who.int/malaria/publications/atoz/smc_report_teg_meetingmay2011.pdf.
- 6.WHO. World malaria report 2019. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/330011. Accessed 30 Mar 2022.
- 7.Programme national de lutte contre le paludisme (PNLP). Rapport de l’atelier bilan de la chimio-prévention du paludisme saisonnier des sept (7) districts sanitaires pilotes en 2014 au Burkina Faso. Burkina Faso; 2014.
- 8.Programme national de lutte contre le paludisme (PNLP). Bilan de la mise en oeuvre de la campagne chimio-prevention du paludisme saisonnier en 2015 au Burkina Faso. Burkina Faso; 2015.
- 9.Programme national de lutte contre le paludisme (PNLP). Rapport synthèse de la mise en oeuvre de la campagne de chimio-prevention du paludisme saisonnier (CPS) en 2016 au Burkina Faso. Burkina Faso; 2016.
- 10.Programme national de lutte contre le paludisme (PNLP). Rapport bilan de la chimio-prévention du paludisme saisonnier (CPS) 2017, Burkina Faso. Burkina Faso; 2017.
- 11.Programme national de lutte contre le paludisme (PNLP). Rapport général de la campagne chimio-prévention du paludisme saisonnier (CPS) 2018, mise en oeuvre dans les 65 districts, Burkina Faso. Burkina Faso; 2018.
- 12.Programme national de lutte contre le paludisme (PNLP). Etat des lieux de la chimio-prévention du paludisme saisonnier 2014–2020, Burkina Faso; 2020.
- 13.Cissé B, Sokhna C, Boulanger D, Milet J, Bâ EH, Richardson K, et al. Seasonal intermittent preventive treatment with artesunate and sulfadoxine-pyrimethamine for prevention of malaria in Senegalese children: a randomised, placebo-controlled, double-blind trial. Lancet. 2006;367:659–667. doi: 10.1016/S0140-6736(06)68264-0. [DOI] [PubMed] [Google Scholar]
- 14.Dicko A, Diallo AI, Tembine I, Dicko Y, Dara N, Sidibe Y, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Mali: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8:e1000407. doi: 10.1371/journal.pmed.1000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konaté AT, Yaro JB, Ouédraogo AZ, Diarra A, Gansané A, Soulama I, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Burkina Faso: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8:e1000408. doi: 10.1371/journal.pmed.1000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kweku M, Liu D, Adjuik M, Binka F, Seidu M, Greenwood B, et al. Seasonal intermittent preventive treatment for the prevention of anaemia and malaria in Ghanaian children: a randomized, placebo controlled trial. PLoS ONE. 2008;3:e4000. doi: 10.1371/journal.pone.0004000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sesay S, Milligan P, Touray E, Sowe M, Webb EL, Greenwood BM, et al. A trial of intermittent preventive treatment and home-based management of malaria in a rural area of The Gambia. Malar J. 2011;10:2. doi: 10.1186/1475-2875-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diawara F, Steinhardt LC, Mahamar A, Traore T, Kone DT, Diawara H, et al. Measuring the impact of seasonal malaria chemoprevention as part of routine malaria control in Kita, Mali. Malar J. 2017;16:325. doi: 10.1186/s12936-017-1974-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Druetz T, Corneau-Tremblay N, Millogo T, Kouanda S, Ly A, Bicaba A, et al. Impact evaluation of seasonal malaria chemoprevention under routine program implementation: a quasi-experimental study in Burkina Faso. Am J Trop Med Hyg. 2018;98:524–533. doi: 10.4269/ajtmh.17-0599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moundine K, Moukenet Z, Clement K-H, Gaudard J. Impact of seasonal malaria chemoprevention on morbidity and mortality dues to malaria among children under five years in Chad. Int J Sci Technol Res. 2016;5:102–106. [Google Scholar]
- 21.Baba E, Hamade P, Kivumbi H, Marasciulo M, Maxwell K, Moroso D, et al. Effectiveness of seasonal malaria chemoprevention at scale in west and central Africa: an observational study. Lancet. 2020;396:1829–1840. doi: 10.1016/S0140-6736(20)32227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ibrahim B. Caractérisation des saisons de pluies au Burkina Faso dans un contexte de changement climatique et évaluation des impacts hydrologiques sur le bassin du Nakanbé [PhD thesis]. Université Pierre et Marie Curie, Paris VI; 2012. https://tel.archives-ouvertes.fr/tel-00827764. Accessed 30 Mar 2022.
- 23.De Longueville F, Hountondji Y-C, Kindo I, Gemenne F, Ozer P. Long-term analysis of rainfall and temperature data in Burkina Faso (1950–2013) Int J Climatol. 2016;36:4393–4405. doi: 10.1002/joc.4640. [DOI] [Google Scholar]
- 24.Ministère de l’environnement et du cadre de Vie. Programme d’Action National d’adaptation à la variabilité et aux changements climatiques (PANA); 2007
- 25.Ministère de la santé. Annuaire statististique 2018. Burkina Faso; 2018.
- 26.Ministry of health. National health information system and 2010–2020 strategic plan evaluation, Burkina Faso. 2020. https://static1.squarespace.com/static/548487dce4b08bf981fe60d5/t/60354eef1ec0a67d735b4a1f/1614106365430/BurkinaFaso_Report_Final.pdf.
- 27.Dodo M, Badolo O, Nebie S, Sawadogo Y, Yanogo P. Benefits and challenges of building a strong national HMIS using DHIS2: case of Burkina Faso malaria data collection system. 2021. http://content.dhis2.org.s3.amazonaws.com/experts%20academy%202017/BURKINA%20FASO%20F_reduced.pdf.
- 28.Mnistère de la santé. Rapport d’évaluation du système de gestion et de la qualité des données de routine du SNIS. Burkina Faso.
- 29.Chandramohan D, Zongo I, Sagara I, Cairns M, Yerbanga R-S, Diarra M, et al. Seasonal malaria vaccination with or without seasonal malaria chemoprevention. N Engl J Med. 2021;385:1005–1017. doi: 10.1056/NEJMoa2026330. [DOI] [PubMed] [Google Scholar]
- 30.Cairns ME, Sagara I, Zongo I, Kuepfer I, Thera I, Nikiema F, et al. Evaluation of seasonal malaria chemoprevention in two areas of intense seasonal malaria transmission: secondary analysis of a household-randomised, placebo-controlled trial in Houndé District, Burkina Faso and Bougouni District, Mali. PLoS Med. 2020;17:e1003214. doi: 10.1371/journal.pmed.1003214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greenwood B, Cairns M, Chaponda M, Chico RM, Dicko A, Ouedraogo J-B, et al. Combining malaria vaccination with chemoprevention: a promising new approach to malaria control. Malar J. 2021;20:361. doi: 10.1186/s12936-021-03888-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cissé B, Ba EH, Sokhna C, NDiaye JL, Gomis JF, Dial Y, et al. Effectiveness of seasonal malaria chemoprevention in children under ten years of age in Senegal: a stepped-wedge cluster-randomised trial. PLoS Med. 2016;13:e1002175. doi: 10.1371/journal.pmed.1002175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Monthly trends of uncomplicated malaria incidence in health districts before and after SMC implementation among older age group (5–14 years old and 15 years and more). Figure S2. Monthly trends of severe malaria incidence in health districts before and after SMC implementation among older age group (5–14 years old and 15 years and more). Table S1. Effect of seasonal malaria chemoprevention on incidence of uncomplicated malaria cases among older age group (5–14 years old and 15 years and more). Table S2. Effect of seasonal malaria chemoprevention on incidence of severe malaria cases among older age group (5–14 years old and 15 years and more).
Data Availability Statement
All data were extracted from the national health information system as part of routine care. Data that support the findings of this study are available at the Ministry of Health in Burkina Faso.