Abstract
Background
Individuals with autism spectrum disorder (ASD) are more likely to use healthcare than their counterparts without disabilities, which imposes high medical costs to families and health systems. This study aimed to investigate healthcare costs and its determinants among individuals with ASD.
Methods
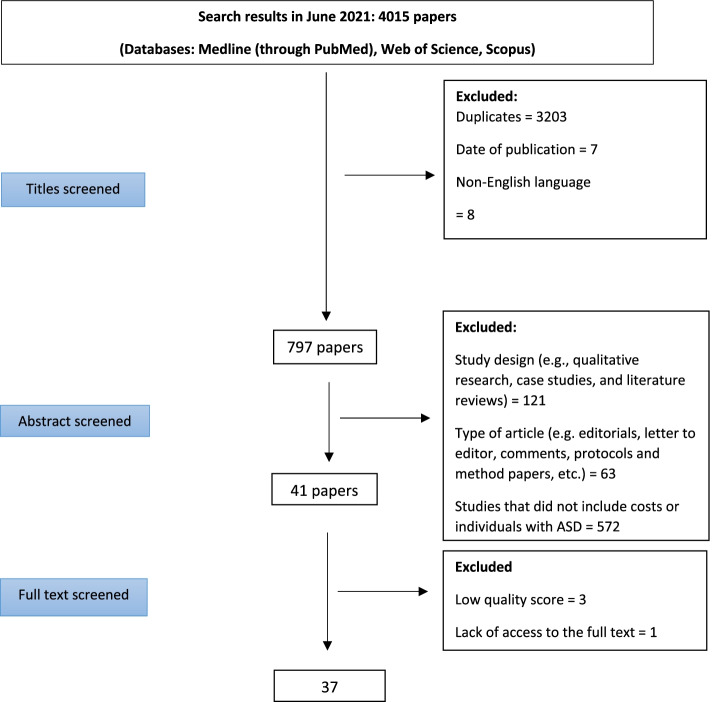
In this systematic review, we searched online databases (Web of Science, Medline through PubMed and Scopus) for observational and experimental studies that included data on service use and costs associated with ASD and published between January 2000 and May 2021. Exclusion criteria included non-English language articles, duplicates, abstracts, qualitative studies, gray literature, and non-original papers (e.g., letters to editors, editorials, reviews, etc.).
Results
Our searches yielded 4015 articles screened according to PRISMA guidelines. Of 4015 studies identified, 37 articles from 10 countries were eligible for final inclusion. Therapeutic interventions, outpatient visits and medications constituted the largest proportion of direct medical expenditure on individuals with ASD. Included studies suggest lack of health insurance, having associated morbidities, more severe symptoms, younger age groups and lower socioeconomic status (SES) are associated with higher medical expenditure in individuals with ASD.
Conclusions
This systematic review identified a range of factors, including lower SES and lack of health insurance, which are associated with higher healthcare costs in people with ASD. Our study supports the formulation of policy options to reduce financial risks in families of individuals with ASD in countries which do not have a tax-based or universal health coverage system.
Keywords: Autism, Healthcare costs, Out of pocket payments, Determinants, Systematic review
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that affects social abilities, communication skills and behavioral patterns among people with ASD [1]. This disorder occurs in all racial, ethnic and socioeconomic groups and its prevalence has grown rapidly in the last few decades [2]. According to the Centers for Disease Control and Prevention, about 1 in 54 children have been diagnosed with ASD [3]. Some studies have reported the prevalence of ASD to be approximately 1–2% in Asia, Europe and North America [4].
Individuals with ASD require behavioral interventions and specialty health services to improve social interactions, communication skills and daily functioning. Evidence suggests that individuals with ASD are more likely to have higher rates of utilization of both acute care (e.g. hospitalization and emergency department visits) and specialty care (e.g. psychiatric and neurology visits) than their counterparts without ASD [5, 6]. For example, Croen and colleagues found that children with ASD experienced a higher percentage of inpatient (3% vs 1%) and outpatient (5% vs 2%) hospitalizations compared to children without ASDs [7]. In addition, people with ASDs tend to use more psychotherapeutic medications than people without ASDs that impose considerable costs on families and health systems [8, 9].
Studies show a strong relationship between co-occurring conditions and healthcare cost among individuals with ASD. Of these, mental health problems have a major effect on medical care costs. Peacock et al. found that children with ASD and intellectual disability incurred expenditures 2.7 times higher than children with ASD and no co-occurring condition [10]. Similarly, a study by Zerbo et al. indicated that adults with ASD had a significantly higher mean number of visits for mental health (43.3% vs 5.4%) and speech therapy (0.8% vs 0.07%) compared with the general population [11].
The economic burden associated with ASD has been investigated in various studies. Studies have reported higher healthcare costs among individuals with ASD compared to the general population. For example, a study by Lavelle et al. indicated that annual costs of healthcare among children with ASDs were more than four times higher (14,061 USD vs 3020 USD) than those without ASDs [12]. Higher utilization of healthcare among individuals with ASDs may additionally impose higher direct costs on families, particularly in countries where out of pocket payment (OPP) for health services is common, and higher indirect costs, as a result of lost or disrupted employment for individuals and their parents/carers. We should note that healthcare is only one element of costs relevant to people with an ASD; other relevant costs include day care, respite care and education, including specialist education [13].
Some factors, such as age, place of residence, the level of disability, and associated comorbidities, can intensify the economic burden carried by individuals with ASDs. For example, Knapp et al. in the UK, found that lifetime costs are substantially higher for individuals with both ASD and intellectual disability than for those with ASD alone (£1.23 million vs £0.80 million) [13]. Similarly, Horlin et al. in Australia, noted that each additional symptom adds around 1400 USD per annum to the cost of an individual with ASD [14]. Timing of diagnosis also influences cost, with studies demonstrating that delayed diagnosis and access to specialty healthcare can increase associated comorbidities in people with disabilities which consequently leads to higher healthcare costs [15–17].
Overall, the consequences of ASD can potentially affect employment, family relationships, standards of living, social interactions, personal functioning, and quality of life for individuals and their families. In this systematic review, we aimed to identify factors associated with healthcare costs among individuals with ASD. Total costs associated with ASD can vary between individuals and between countries, as a result of a number of different factors. However, identification and quantification of the healthcare, and other, costs associated with ASD can provide a comprehensive picture of the financial impact on families and health systems and can help to identify factors affecting those costs, which may be amenable to change or policy intervention. To ensure appropriate planning of the afore-mentioned services and allocation of resources, it is essential to identify the major contributors to healthcare costs among individuals with ASD. Therefore, the present study aimed to identify determinants of healthcare costs among individuals with ASD.
Method
Search strategy
Our study was a systematic review that adheres to the PRISMA guidelines [18]. Three online bibliographic databases were used to search English language articles from January 1, 2000 to May 31, 2021: Web of Science, Medline through PubMed and Scopus. Two main foci were used to search for studies: (1) autism; and (2) cost; we used a combination of keywords to search for studies meeting our inclusion criteria and the search strategy is shown in Table 1. In addition, we searched the references of all included studies to identify additional studies.
Table 1.
Search strategy in the included databases
| Databases | Number of abstracts |
|---|---|
| Web of science | 1191 |
| TITLE: (autis*) AND TOPIC: (expen*) | 215 |
| TITLE: (autis*) AND TOPIC: (cost*) | 500 |
| TITLE: (autis*) AND TOPIC: (econom*) | 249 |
| TITLE: (autis*) AND TOPIC: (spen*) | 94 |
| TITLE: (autis*) AND TOPIC: (financ*) | 133 |
| Medline through PubMed | 1333 |
| (autis*[Title/Abstract]) AND (expen*[Title/Abstract]) | 183 |
| (autis*[Title/Abstract]) AND (cost*[Title/Abstract]) | 617 |
| (autis*[Title/Abstract]) AND (econom*[Title/Abstract]) | 285 |
| (autis*[Title/Abstract]) AND (spend*[Title/Abstract]) | 97 |
| (autis*[Title/Abstract]) AND (financ*[Title/Abstract]) | 151 |
| Scopus | 1474 |
| TITLE-ABS (autis* AND expen*) | 199 |
| TITLE-ABS (autis* AND cost*) | 665 |
| TITLE-ABS (autis* AND econom*) | 313 |
| TITLE-ABS (autis* AND spend*) | 124 |
| TITLE-ABS (autis* AND financ*) | 173 |
We included observational (cross-sectional studies, case-control studies, and cohort studies) and experimental (randomized control trial, quasi experimental) studies. As shown in Table 2, inclusion criteria were defined according to the Patient, Intervention, Comparator, Outcome, Study design (PICOS) framework. Our primary outcomes were factors associated with healthcare costs in individuals with ASD. In health economics, healthcare costs are categorized into direct and indirect costs. Direct costs are defined as those costs that are directly attributable to an illness or disorder, including direct medical costs (the cost of healthcare interventions) and direct non-medical costs (additional costs as a result of accessing healthcare interventions, such as accommodation, meals, and transportation costs) [19]. Indirect costs are costs (or ‘losses’) incurred due to the cessation of or reduction in work productivity as a result of the morbidity associated with an ASD [20]. In this study, total costs were the sum of direct and indirect costs.
Table 2.
PICOS inclusion criteria
| PICOS | Criteria |
|---|---|
| Population | Individuals with ASD |
| Intervention | N/A |
| Comparator | N/A |
| Outcome | Contributing factors to healthcare costs in individuals with ASD |
| Study design | Observational and experimental studies |
Inclusion criteria
Individuals with ASD
Studies reporting healthcare costs for individuals with ASD
Observational studies (cross-sectional studies, case-control studies, and cohort studies) or experimental studies (randomized control trial, quasi experimental) Published in English between January 1, 2000 and May 31, 2021
Full-text articles
Exclusion criteria
Published before January 1, 2000 and after May 31, 2021
Qualitative research, case studies, and literature reviews (e.g. scoping and systematic reviews)
Abstracts, editorials, letter to editor, and comments
Protocols and method papers
Grey literature (e.g. books, conference abstracts, theses, research reports, policy documents)
Non-English language studies
Data analysis
We developed a data extraction form to extract information such as authors, year, country, study design, study sample, costs, study perspective (for example: patient, healthcare sector, payer, societal or institutional perspective [21]), and patient characteristics hypothesized to be determinants of healthcare costs (for example, co-morbidities, severity of illness, age, health insurance status, socioeconomic status) from the included studies. Three main steps of title screening, abstract screening and full-text screening were performed to select the included studies. At the first step of title screening, we searched titles using the keywords outlined in Table 1 and then removed duplicate records. At the abstract screening stage, two authors independently checked the titles and abstracts for relevance (AK and MS), removed those clearly meeting exclusion criteria and retained all potentially relevant abstracts for full-text review. Full-text papers were similarly screened independently by two authors to ensure they met the inclusion criteria and did not meet the exclusion criteria (AK and MS). Data were extracted from all included studies using a pre-specified checklist of key study items. The corresponding author checked the accuracy of the data by comparing and adapting the extracted data with the information contained in the included articles. All disagreements were resolved by consensus after discussion. Where the full-text of papers could not be accessed, corresponding authors were contacted by email to request access. We used EndNote X9.3 to screen the papers and extract data.
Regarding the design of the included studies, we applied JBI Critical Appraisal Checklists for cross sectional studies and cohort studies to assess the quality of the studies included in the review [22]. Quality assessment was carried out by two authors independently (AK and MS).
Results
The process of study selection is shown in Fig. 1. In total, our search yielded 4015 papers (including manual searching of reference lists of included papers). In the first step of screening (title screening), 3218 articles were excluded because of language (not English), date of publication outside the dates of interest or because they were duplicates. In the second step of screening (abstract screening), 756 articles were excluded from the study because of study design (qualitative studies or an excluded design), participants (not ASD), type of article (letter to the editor, editorial and review), or for not reporting heath care costs. In the final step (full text screening), a further 4 articles were excluded because of lack of access to the full text or low quality score. Thus 37 articles met criteria for inclusion.
Fig. 1.
The process of systematic review of the literature
The 37 included studies, which are summarized in Table 3, were carried out in 10 countries: the United states of America (USA; n = 21), the United Kingdom (UK; n = 6); both USA and UK (n = 1),Taiwan (n = 2), Ireland (n = 1), Germany (n = 1), Israel (n = 1), China (n = 1), Australia (n = 1), Oman (n = 1), and South Korea (n = 1). The age of participants ranged between 1 and 89 years and the majority of studies focused on ASD or ASD with and without intellectual disability.
Table 3.
Study characteristics
| Authous (Year) | Country | Study aim | Data source | Sample size (age) |
Study perspective | Type of health services | Costs included in the study | Period of the study | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Average direct costs per person | Average indirect costs per person | Average total costs per person | ||||||||
| Jarbrink and Knapp (2001) [23] | UK | To estimate the economic consequences of autism in the UK | Secondary analysis of data | Autism with additional learning disabilities |
Patient Provider |
Hospital/inpatient services Medication use Other |
OOP: $67,098 Provider spending: $221,027 |
NR | NR | Lifetime |
| High functioning autism |
OOP: NR Provider spending: $152,717 |
$298,256 | NR | |||||||
| Jarbrink (2003) [24] | USA |
To show the major cost drivers among children with ASD |
Survey (Respondents: parents) |
N = 17 (4–10 years) |
Provider |
Early intervention Health services Medication use |
Provider spending: $416 | NR | NR | Weekly |
| Liptak et al. (2006) [25] | USA | To compare healthcare expenditures between children with ASD and other children with and without disabilities |
Survey (Respondents: parents) |
N = 100 (< 17 years old) |
Patient | Home/community-based/outpatient services Hospital/inpatient services Medication use Respite care | OOP: $898 | NR | NR | Annual costs |
| Flanders (2007) [26] | USA | To compare direct costs of treatment of children with ASD, asthma, and diabetes | Secondary analysis of data (California Medicaid Medical database) |
N = 731 (3–17 years) |
Payer |
Hospital/inpatient services Outpatient services Medication use |
Insurer spending: $6436 | NR | NR | Annual costs |
| Jarbrink (2007) [27] | UK | To show the major cost drivers among children with ASD |
Survey (Respondents: parents) |
N = 55 (< 18 years old) |
Provider |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Provider spending: $3996 | NR | NR | Annual costs |
| Leslie et al. (2007) [28] | USA | To examine the healthcare expenditures associated with ASDs in medical care settings | Secondary data analysis (Administrative claims database) | N = 613 (< 17 years old) |
Payer Patient |
Hospital/inpatient services Outpatient services Medication use |
OOP + Insurer spending: $8531 |
NR | NR | Annual costs |
| Sharpe and Baker (2007) [29] | USA | To identify factors associated with financial problems in families that have a child with autism |
Survey (Respondents: parents and care givers) |
N = 333 (< 19 years old) |
Patient |
Hospital/inpatient services Outpatient services Respite care Medication use Other |
NR | NR | NR | Annual costs |
| Shimabukuro et al. (2008) [30] | USA | To estimate medical expenditures for children with ASD who receive employer-based health insurance |
Secondary analysis of data (employer-based health insurance claims: the MarketScan research databases) |
N = 3481 (1–21 years) |
Payer Patient |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
OOP: $805 Insurer spending: $10,006 |
NR | NR | Annual costs |
|
Knapp et al. (2009) [13] |
UK | To estimate the costs of ASDs in the UK | Secondary analysis of data | Children with intellectual disability | Provider |
Hospital/inpatient services Respite care Other |
Provider spending: $11,946 | NR | NR | Annual costs |
| Children without intellectual disability | Provider spending: $30,936 | NR | NR | |||||||
| Young et al. (2009) [31] | USA | To examine the healthcare expenditures associated with ASDs in medical care settings. | Survey |
N = 113 (2.5–21 years) |
Patient |
Hospital/inpatient services Outpatient services Respite care Medication use Other |
OOP: $882 | NR | NR | Annual costs |
| Wang et al. (2010) [32] | USA | To examine trends in health care expenditures associated with ASDs in state Medicaid programs | Secondary analysis of data (Medicaid data) |
N = 69,542 (> 17 years old) |
Payer |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Insurer spending: $33,360 |
NR | NR | Annual costs |
| Barrett et al. (2012) [33] | UK | To determine family out-of-pocket expenses and productivity losses, and explore the relationship between family characteristics and costs. | Randomized controlled trial |
N = 152 (2–4 years) |
Patient Provider |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
OOP: $446 Provider spending: $2240 |
$539 | $3792 | 6 months |
| Parish et al. (2012) [34] | USA | To investigate the association between state Medicaid spending for children with disabilities and the financial burden reported by families of children with autism. | Secondary analysis of data (National Survey of Children with Special Healthcare Needs) |
N = 2082 (< 18 years old) |
Patients | NR | OOP: $690 | NR | NR | Annual costs |
| Peacock et al. (2012) [10] | USA | To compare medical expenditures between children with ASDs and without ASDs | Secondary analysis of data (Health insurance claims: MarketScan Medicaid Multi-State Databases) |
N = 8398 (2–17 years) |
Payer |
Hospital/inpatient services outpatient services Medication use |
Insurer spending: $14,777 |
NR | NR | Annual costs |
| Wang et al. (2012) [35] | China | To determine the health expenses incurred by families of children with ASD and those expenses in relation to total patient income and expenditures | Survey (Respondents: parents) |
N = 290 (1–15 years) |
Patient |
Home/community-based/outpatient services Respite care Medication use Other |
OOP: $2936 | NR | NR | Annual costs |
| Al-Farsi et al. (2013) [36] | Oman | To measure medical expenditures in children with ASDs | Survey (Respondents: parents) |
N = 150 (< 15 years old) |
Patient |
Home/community-based/outpatient services Respite care Medication use Other |
OOP:$346 | $961 | NR | Monthly |
| Van Steensel et al. (2013) [37] | USA |
To measure the societal costs of children with high-functioning ASD and comorbid anxiety disorder(s) |
Survey (Respondents: parents) |
N = 194 (7–18 years) |
Patient |
Home/community-based/outpatient services Respite care Medication use Other |
OOP: $16,806 | NR | NR | Annual costs |
| Raz et al. (2013) [38] | Israel | To measure the level of OOP expenditure for health services by families with autistic children | Survey (Respondents: parents) |
N = 204 (4–10 years) |
Patient |
Home/community-based/outpatient services Respite care Medication use Other |
OOP: $9930 | NR | NR | Annual costs |
| Buescher et al. (2014) [9] | UK | To estimate lifetime societal economic costs among individuals with ASD | NR | NR | Patient | Medical services |
Adults with ID: $8738 Adults without ID:$27,265 |
NR | NR | Annual costs |
| NR | Patient | Medical services |
Children with ID:$1578 Children without ID: $1030 |
NR | NR | Annual costs | ||||
| USA | NR | Patient | Medical services |
Adults with ID: $32,630 Adults without ID:$16,316 |
NR | NR | Annual costs | |||
| NR | Patient | Medical |
Children with ID: $18,645 Children without ID: $9323 |
NR | NR | Annual costs | ||||
| Horlin et al. (2014) [14] | Australia | To compare expenses between families whose children receiving immediate versus delayed diagnoses | Survey (Respondents: parents) |
N = 521 (< 18 years old) |
Patient | All healthcare | OOP: $6937 |
30,422 (loss of income of the parents and caregivers) |
35,593 | Annual costs |
| Lavelle et al. (2014) [12] | USA | To estimate the associations between ASD diagnoses and service use, caregiver time, and cost outcomes | Secondary analysis of data (National Health Interview Survey) and a study-specific survey |
N = 258 (3–17 years old) |
Patient Payer |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Insurer spending: $3618 OOP: $218 |
NR | NR | Annual costs |
| Thomas et al. (2014) [39] | USA | To investigate the association between school transition age and healthcare expenditures for children with ASD | Secondary analysis of data (Pooled data from the Medical Expenditure Panel Survey) |
N = 337 (< 21 years old) |
Patient | All healthcare |
Median OOP: $490 |
NR | NR | Annual costs |
| Barrett et al. (2015) [40] | UK | To describe the services and associated costs for individual with ASD and | Cohort of adolescents with ASD and other special needs |
N = 51(adolescents with autistic disorder) (9–14 years) |
Provider |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Provider spending: $1231 | NR | NR | 6 months |
|
N = 45 (adolescents with other ASDs) (9–14 years) |
Provider spending: $1999 | NR | NR | |||||||
| Byford et al. (2015) [41] | UK | To investigate the cost-effectiveness of a communication-focused therapy for pre-school children with ASD | Cohort study |
N = 77 (PACT+ treatment as usual) (2–4 years) |
Provider Patient |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
OOP: $2896 Provider spending: $16,523 |
$1223 | $20,645 | 13 months |
|
N = 75 (treatment as usual) (2–4 years) |
Provider Patient |
OOP: $1990 Provider spending: $5180 |
$842 | $7923 | ||||||
| Parish et al. (2015) [42] | USA | To investigate the relationship between family financial burden and children’s health | Secondary analysis of data (Pooled 2000–2009 Medical Expenditure Panel Survey data) |
N = 316 (< 18 years old) |
Patient | NR | OOP: $904 | NR | NR | Annual costs |
| Thomas et al. (2016) [43] | USA | To examine expenditures according to types of health insurance included private alone, Medicaid alone, and combined private and wrap-around Medicaid | Secondary analysis of data (Pooled data from the Medical Expenditure Panel Survey) |
N = 346 (< 18 years old) |
Patient |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
OOP for Medicaid insured children: $156 OOP for private insured children: $1579 Medicaid spending: $8383 Private insurance spending: $3736 |
NR | NR | Annual costs |
| Barry et al. (2017) [44] | USA | To measure whether implementing autism mandates altered service use or spending among commercially insured children with ASD | Secondary analysis of data (Health insurance claim: Data from three national insurers) |
N = 106,977 (< 21 years old) |
Payer |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Mandate eligible: $767 Mandate ineligible: $600 |
NR | NR | Monthly |
| Chang et al. (2018) [45] | Taiwan | To compare the differences in dental utilization and expenditure between children and adolescents with and without ASD | Secondary analysis of data (Health insurance claim: The database of the National Health Research Institutes) |
N = 1305 (< 18 years old) |
Payer | Dental treatment | Insurer spending: $110 | NR | NR | Annual costs |
| Vohra et al. (2017) [46] | USA | To investigate the prevalence and association of comorbidities with healthcare utilization and expenditures of fee-for service enrolled adults with and without ASD | Secondary analysis of data (Health insurance claim: Medicaid data) |
N = 1772 (22–64 years) |
Payer |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Insurer spending: $16,928 |
NR | NR | Annual costs |
| Candon et al. (2019) [47] | USA | To investigate whether mandates have heterogeneous effects on healthcare expenditure by insures and individuals with ASD | Secondary analysis of data (Health insurance claim) | N = 106,977 (< 21 years old) | Patient Payer | NR |
OOP: $124 Insurer spending: $453 |
NR | NR | Monthly |
| Hong et al. (2019) [48] | South Korea | To estimate the economic burden of ASD in South Korea | Secondary analysis of data (Health insurance claim: The National Health Insurance Service) |
N = 5653 (1–89 years) |
Patient |
Hospital/inpatient services Home/community-based/outpatient services |
NR | NR | $2496 | Annual costs |
| Li et al. (2019) [49] | Taiwan | To examine the cost and utilization of rehabilitation resources among children with ASD | Secondary analysis of data (Health insurance claim: The National Health Insurance Research Database) |
N = 3227 (3–12 years) |
Payer | Home/community-based/outpatient services | Insurer spending: $2100 | NR | NNRM | Annual costs |
| Roddy and O’Neill (2019) [50] | Ireland | To measure the societal cost of childhood ASDs | Survey (Respondents: parents) |
N = 222 (2–18 years) |
Patient |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
OOP: $2756 | NR | NR | Annual costs |
| Zerbo et al. (2019) [11] | USA | To compare healthcare utilization patterns and cost among insured adults with ASD, adults with ADHD and adults with neither condition | Secondary analysis of data (Administrative claim data: The Kaiser Permanente Northern California (KPNC) database |
N = 1507 (> 18 years) |
Provider |
Hospital/inpatient services Home/community-based/outpatient services Respite care Other |
Provider spending: $7889 | NR | NNRM | Annual costs |
| Zuvekas et al. (2021) [51] | USA | To estimate healthcare costs for US children with ASD | Secondary analysis of data (Two different surveys) |
N = 45,944 (3–17 years) |
Patient |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Medical Expenditure Panel Survey (MEPS: $4163 National Health Interview Survey (NHIS): $5955 |
NR | NR | Annual costs |
| Höfer et al. (2022) [52] | Germany | To estimate health service use and associated costs in children, adolescents and adults with ASD with and without intellectual disability | Survey (Respondents: parents) |
N = 385 (4–67 years) |
Patients |
Hospital/inpatient services Home/community-based/outpatient services Respite care Other |
$4208 | NR | NR | Annual costs |
| Ames et al. (2021) [53] | USA | To calculate healthcare service utilization and cost among transition-age youth with ASD and other special healthcare needs | Secondary analysis of data (Administrative claim: Kaiser Permanente Northern California) |
N = 4123 (14–25 years) |
Provider |
Hospital/inpatient services Home/community-based/outpatient services Respite care Medication use Other |
Provider spending: $5302 | NR | NR | Annual costs |
All costs are in U.S. dollars and are adjusted to reflect 2021 USD
ADHD Attention-Deficit and Hyperactivity Disorder; ASD Autism spectrum disorder; NR Not reported; UK United Kingdom; USA United States of America; OPP out of pocket payment
Direct healthcare costs
Included costs varied between studies, as illustrated in Table 3. Focusing on direct healthcare costs only, a number of studies reported that rehabilitation and psychological therapies constitute the greatest proportion of total healthcare-related expenditure for individuals with ASD. In the study by Wang et al., carried out in the USA, the highest percentage of healthcare expenditures was devoted to behavioral therapies (54.3%), followed by transportation and accommodation (18.4%), outpatient care (15.9%), and medication (8.2%) [54]. Similarly, Ganz et al., in the USA, estimated that behavioral therapies were the largest part of lifetime per capita direct medical expenditures (206,337 USD) of which was highest for children aged 3–7 years [55]. Mosadeghrad et al. also reported that rehabilitation services comprised the largest component (70%) of the annual ASD direct medical costs in their study conducted in Iran [56].
Outpatient and community-based services, such as physician appointments, were more commonly used than inpatient care and thus these services would impose a high economic burden on families of individuals with ASD in countries where such services are paid out of pocket. The study by Barrett et al. (2012), in the UK, reported a higher proportion of the included sample utilizing outpatient and community-based appointments, with 60, 57 and 48% of children with ASD having at least one contact with community pediatricians, general practitioners, and health visitors (nurses or midwives who have undertaken additional training in community public health nursing), respectively, over a 6 month period, compared to 10% of participants reporting an inpatient episode of care [33]. Similarly, the findings of Vohra et al., in the USA, indicated that following prescription drugs, outpatient visits were the second major contributor to healthcare expenditure [46].
The included studies suggest that prescription drugs make a major contribution to expenditure for households. Mosadghrad et al., in Iran, for example, estimated the average annual direct medical costs of ASD? were approximately 2215 USD of which 16% consisted of medication, compared to 7 and 6.5% for outpatient and inpatient visits, respectively [56]. Similarly, Flanders et al., in the USA, estimated the mean annual healthcare costs of prescription medication at 827 USD per person, compared to 222 USD per person for inpatient services [26], whilst Vorha et al. found prescription drugs to be the largest contributor to healthcare expenditure [56].
Eight studies (24.24% of included studies) reported that inpatient services, equipment and emergency room visits constituted a smaller proportion of total healthcare costs compared to outpatient services. For example, a study by Thomas et al. (2014), in the USA, showed that inpatient services constitute only 0.5% of expenditure compared to outpatient services (27.7%) [39]. Young et al. (2009), in the USA, reported that only 5 and 12.5% of individuals with ASD with public and private insurance coverage had used inpatient care but more than 70% of the participants had received rehabilitation services such as speech-language therapy and occupational therapy [31]. Of these, privately insured children unexpectedly had lower expenditure than those with public insurance. Additionally, in the study by Vohra and colleagues conducted in the USA, the mean annual cost of inpatient care constituted a lower proportion (10.99%) of total healthcare expenditure compared to outpatient visits (14.76%), prescription drug (20.47%), and emergency room visits (53.76%) [46].
Indirect costs
Indirect costs were commonly estimated in studies involving children and young people and were focused on lost productivity for parents and carers. Three studies (9.09% of included studies) showed that indirect costs constitute a greater proportion of total costs (direct + indirect) compared to healthcare expenditures in families of individuals with ASD. Accordingly, a study by Al-Farsi et al., in Oman, indicated a higher monthly indirect cost (924 USD; 8.92% of total costs) in contrast to direct healthcare expenditure (328 USD; 2.99% of total costs) [36]. In their study, the mean loss of income due to lost employment opportunity in middle-high income families (978 USD) was greater than low-income families (254 USD). Similarly, in the study by Horlin et al., in Australia, loss of income of parents and caregivers made a substantially larger contribution to the total cost of ASD per person (30,000 USD; 47%) compared to healthcare expenditure (4800 USD; 13.67%) [14]. They also reported that loss of income for the first income quartile (19,500 USD) was lower than the third income quartile (48,700 USD).
In contrast, Mosadeghrad et al., carried out in Iran, reported mean annual indirect costs due to productivity loss of 1118 USD, which was a smaller contribution to total expenditure (16%) compared to direct medical costs (32%) and direct non-medical costs (52%) [19]. In the study by Hong et al., carried out in South Korea, indirect costs for individuals with ASD in the age group of 20–29 years were lower than direct costs per capita (863 USD; 40.12% of total costs), but were higher than direct costs in older age groups [48].
Key determinants of healthcare costs among individuals with ASD
Table 4 summarises the major contributing factors to healthcare costs among individuals with ASD, and the direction of the relationship, as reported by included studies.
Table 4.
Contributing factors to healthcare costs in individuals with ASD
| Determinants of healthcare costs | Study |
|---|---|
| Severity of ASD (+) | (Järbrink and Knapp 2001), (Sharpe and Baker 2007), (Barrett, Byford et al. 2012), (Barrett, Byford et al. 2012), (Raz, Lerner-Geva et al. 2013), (Horlin, Falkmer et al. 2014), (Roddy and O’Neill 2019) |
| Associated disabilities (+) | (Järbrink and Knapp 2001), (Järbrink 2007), (Peacock, Amendah et al. 2012), (Lavelle, Weinstein et al. 2014), (Thomas, Parish et al. 2014), (Vohra, Madhavan et al. 2017), (Roddy and O’Neill 2019), (Page, McKenzie et al. 2021), (Buescher, Cidav et al. 2014) |
| Utilizing medical interventions (+) | (Sharpe and Baker 2007) |
| Age (+) | (Barrett, Byford et al. 2012), (Lavelle, Weinstein et al. 2014), (Thomas, Parish et al. 2014), (Parish, Thomas et al. 2015), (Chang, Wang et al. 2018), (Hong, Lee et al. 2020), (Buescher, Cidav et al. 2014) |
| Age (−) | (Barrett, Mosweu et al. 2015), (Barry, Epstein et al. 2017), (Li, Chen et al. 2019), (Page, McKenzie et al. 2021), (Research Ethics Committees Certificate 2019) |
| Being male (+) | (Hong, Lee et al. 2020), |
| Being female (+) | (Li, Chen et al. 2019), (Page, McKenzie et al. 2021), (Research Ethics Committees Certificate 2019) |
| Income (−) | (Sharpe and Baker 2007), (Thomas, Parish et al. 2014), |
| Income (+) | (Raz, Lerner-Geva et al. 2013), (Parish, Thomas et al. 2015), (Candon, Barry et al. 2019) |
| Health insurance (−) | (Parish, Thomas et al. 2012), (Thomas, Williams et al. 2016) |
| Rural residence (+) | (Wang, Zhou et al. 2012) |
| Rural residence (−) | (Parish, Thomas et al. 2015) |
| Parents’ education (+) | (Raz, Lerner-Geva et al. 2013), (Thomas, Parish et al. 2014), (Page, McKenzie et al. 2021) |
| Education level among adults with ASD (−) | (Page, McKenzie et al. 2021) |
| Living with parents (+) | (Raz, Lerner-Geva et al. 2013) |
| Living with a single mother head of household (−) | (Thomas, Parish et al. 2014) |
| Having at least one older sibling (−) | (Raz, Lerner-Geva et al. 2013) |
| Delay in diagnosis (+) | (Horlin, Falkmer et al. 2014), |
| Prescription medication (+) | (Lavelle, Weinstein et al. 2014), (Thomas, Parish et al. 2014) |
| Private insurance (+) | (Parish, Thomas et al. 2015), |
| Household size (−) | (Parish, Thomas et al. 2015) |
| Being visited in teaching hospital (+) | (Li, Chen et al. 2019) |
Associated morbidities
In some included studies, associated morbidities were one of the significant contributors to total healthcare expenditures in children with ASD. Van Steensel et al., in the USA, estimated the cost of children with ASD and comorbid anxiety disorder were four times higher than anxiety disorder alone, and 27 times higher than typically developing children [37]. Similarly, Peacock et al., in the USA, found that co-occurring conditions such as intellectual disability, Attention Deficit/Hyperactivity Disorder (ADHD) and seizure disorders can increase the overall costs in children with ASD [10]. For example, they report that average annual expenditures for children with ASD without associated conditions was only 7200 USD per person compared with 19,190 USD for children with ASD and an intellectual disability.
Symptom severity
A number of included studies showed that increasing symptom severity was associated with increased costs. Raz et al., in Israel, suggests that individuals with a clinically more severe condition have a higher likelihood of very high costs (OR = 3.31; 95% CI 1.40–7.83) [38]. However, Van Steense et al., in the USA, found no significant relationship [37]. The findings of Horlin et al., in Australia, indicated that each additional symptom adds nearly 1400 USD per annum to the cost of ASD [14]. The authors also report that delay in diagnosis could lead to an increase in the number of ASD symptoms which in turn was associated with higher healthcare costs. Furthermore, a study by Barrett et al., in the UK, showed that fulfilling three functional domains concerning communication, social and repetitive impairments, cost an additional £125 per month, in comparison to children who met only two of the three criteria [33].
Health insurance
Some included studies found that families in receipt of public health insurance, such as Medicaid, were more likely to demonstrate lower out of pocket costs compared with those in receipt of private insurance. A study by Parish et al., in the USA, showed that the median annual out of pocket costs in low-income families of Medicaid–insured individuals with ASD was 7 USD, compared with 160 USD for low-income families with private insurance coverage [42].
Studies also suggest that a lack of insurance coverage increases the probability of high out of pocket expenditures [1, 2]. Thomas et al., in the USA, found that out of pocket expenditures were significantly different by type of insurance such that children covered by private insurance had higher odds of high out of pocket spending compared with their counterparts covered by Medicaid [43]. In their study, the annual out of pocket per person expenditure for Medicaid insured children was estimated to be 150 USD compared to 1335 USD for those with private insurance coverage. In contrast, they found that the mean annual expenditures paid by Medicaid (per person) (7088 USD) was higher than private insurance companies (3151 USD). Similarly, Barry at al., in the USA, who investigated the role of commercial insurance in out of pocket expenditures, found commercial insurance to be associated with a 3.4% increase in out of pocket expenditure on health services and a 77 USD increase in monthly costs for ASD-specific services compared with public insurance [44].
Age
Seven studies showed a positive association and three studies indicated a negative association between age and healthcare costs among individuals with ASD. In adults, Zerbo et al., in the USA, found that the annual heath care cost in adults aged 50 years and older (12,000 USD) was higher than for the 18–25 age group (5000 USD) [9].
In younger populations, some studies showed that younger age groups were associated with higher costs than older age groups. For example, Barrett et al. (2015), in the UK, found that for every one-year increase in age, total health, education and social care costs fell by £4917 among adolescents with autism and autism spectrum disorder aged between 14 and 17 [40]. Similarly, Shimabukuro et al., in the USA, reported that children with ASD in the age group 1–4 years had a higher mean annual cost (8040 USD) compared with older age groups [30]. In contrast, Barrett et al. (2012), in the UK, in another study focused on very young children with autism aged between 2 and 4 years, estimated that young children in higher ages (45–60 months) were likely to use more resources than those in lower ages (24–45 months) [33]. Their study showed that for every 1 month increase in age, healthcare costs increased by £7 per month.
Socioeconomic status
Included studies suggest that households with higher socioeconomic status (SES) were more likely to pay out of pocket for healthcare in comparison to those with lower SES. For instance, Raz et al., in Israel, and Thomas et al., in the USA, reported that higher parental education and higher household income were associated with higher out of pocket expenditure in families of children with ASD [38, 39]. On the other hand, Parish et al., in the USA, cited that in middle and upper-income households, the financial strain was considerably higher for privately insured individuals compared to those with public insurance [42].
Discussion
This systematic review aimed to identify factors contributing to healthcare costs among individuals with ASD. Our findings showed that therapy services, outpatient visits, and medications made the largest contributions to total direct healthcare costs of ASD compared to inpatient care in the included studies, suggesting ASD is primarily managed in the community. Studies show that individuals with ASD are more likely to use therapy services (such as behavioral, occupational and speech therapy) than those without ASD which in turn imposes high costs on families and health systems [10, 25].
Insurance coverage was an important factor influencing the use of services like psychological and rehabilitation therapies, which are known to be important for improving competencies and facilitating social and economic participation in individuals with intellectual disabilities [57]. For example, in countries like Iran, there is no insurance coverage for occupational and speech therapies and thus families of children with intellectual disabilities have to pay out of pocket, with rehabilitation services constituting over 70% of direct medical expenditure among children with ASD [58]. Similarly, behavioral therapies for individuals with ASD are not covered by the Chinese national health insurance program, which imposes a large economic burden on families [35]. There is, therefore, a need to consider public funding of such services in order to protect individuals with ASD and their families from catastrophic health expenditures in countries where such services are paid out of pocket [59, 60].
In countries with public insurance, such as the USA, included studies suggest that -children in receipt of public insurance had a lower out of pocket financial burden compared to uninsured and privately insured children [42]. Our review showed that public insurance can have a major role in protecting families, particularly those on low income, against high direct medical costs associated with ASD. It is important to note that some private insurance companies do cover the cost of therapeutic services for individual with ASD, but low-income families may be unable afford to purchase private coverage. In addition, private insurance companies tend to shift healthcare costs to patients through high copayments or deductibles which in turn increases out of pocket expenses for patients and their families [61] and increases the risk that families cannot afford to purchase insurance.
Included studies showed that outpatient visits and medications constituted a major share of direct medical costs among individuals with ASD [9, 25, 29]. Literature indicates individuals with ASD have higher rates of poorer physical and mental health conditions than their counterparts without ASD which require further healthcare utilization to address these problems [5]. The present review showed that associated comorbidities predict higher healthcare costs [10, 12, 27]. For example, Zebro et al. in the USA, showed that people with ASD had significantly higher utilization of outpatient visits for primary care (74.2% vs. 66.6%), mental health (43.3% vs. 33.2%), and laboratory services (60.9% vs. 54.4%) compared to peers with ADHD [11].
The impact of age on healthcare costs was conflicting, with some suggesting a positive association and others suggesting a negative association. For adults, older age was associated with higher costs. However, the opposite was true in some studies focused on children and young people, with evidence that younger ages are associated with higher physician visits, prescription medication and related costs among individuals with ASD [27, 38, 40, 44].
Whilst the focus of the current paper was on healthcare costs, some included studies took a broader perspective and investigated societal costs among individuals with ASD [27, 37, 50]. In these studies, education made a larger contribution to total annual costs compared to healthcare. For example, the findings of Jarbrink et al., in the UK, showed that the contribution of local government services, schooling and community support comprised 78% of the total cost, while the cost for healthcare was marginal and accounted for less than 5% of the total societal cost [27]. The findings indicate that severe learning disabilities not only are associated with higher healthcare costs, but also with higher education costs (e.g. specialized schooling, transportation etc.) for children with ASD that should be taken into consideration by policy makers.
A number of included studies estimated indirect costs, in addition to direct healthcare costs, and these studies suggest that indirect costs constitute a major part of the total cost of individuals with ASD [14, 24, 33]. In particular, productivity losses (reduced productivity whilst at work or time off work due to illness or caring responsibilities) were found to constitute a substantial proportion of total societal costs, with one study reporting a contribution of almost 10% for productivity losses compared to 7% for out of pocket expenses (7.36%) [33]. Similarly, Al–Farsi et al., in Oman, estimated monthly income loss due to lost employment opportunity at 830 USD, which was higher than monthly out-of-pocket expenses per child (295 USD) [36]. The findings suggest that families spend a considerable amount of time seeking treatment and providing informal (unpaid) care for their family members with ASD. Family plays a central role in the treatment plan of children with ASD through encouraging collaboration, sharing information, reducing emotional distress, empowerment, and joint decision making [62, 63]. Some studies show that accompaniment by family members or parents helps to reduce anxiety and provide comfort in children with ASD [64]. Consequently, households commonly shift a major part of their resources (e.g., time and money) towards providing needed interventions for their children with ASD which subsequently may have a detrimental impact on the family finances, as employment, and thus household income, is reduced whilst healthcare expenditures increases. This suggests that the wellbeing of families’ with children with ASD, including quality of life, employment status, income, education, and physical and mental health, needs to be addressed by policy makers and researchers, alongside the wellbeing of people with ASD.
Limitations
Our study faced some limitations. Firstly, we were not able to compare total healthcare costs and out of pocket expenses between included studies because of heterogeneity in the cost components included in each study. Second, healthcare delivery and financing schemes varied across the included studies, making it difficult to compare healthcare costs between countries. Third, we did not include grey literature and non-English language articles which may have affected the findings and the generalizability of the present study. Finally, we only included studies that reported individual costs per person; aggregate medical and non-medical costs for individuals with ASD should be investigated at local and/or national levels in future studies.
Conclusion
This systematic review showed that therapy services, outpatient visits and medications constituted a major share of total direct healthcare costs among individuals with ASD. Indirect costs were also considerable, being higher than direct healthcare costs in some studies. Key determinants of healthcare costs in the included studies were health insurance, associated morbidities, symptom severity, age and socioeconomic status. Our study supports the formulation of policy options to reduce financial risks in families of individuals with ASD.
Acknowledgments
Not applicable.
Abbreviations
- ASD
Autism spectrum disorder
- SES
Socioeconomic status
- UK
United Kingdom
- USA
United States of America
- USD
United States Dollar
- OPP
Out of pocket payment
- PICOS
Patient, Intervention, Comparator, Outcome, Study design
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- NR
Not reported
Authors’ contributions
S.R., B.K.M. and S.S. contributed in the conception and design of the study. S.S., S.TR, and S. B, wrote and revised the manuscript text. E.Z. and Z.A. Contributed in collecting data. PJ and Z.A. searched articles. A.K.K. and M.S. analyzed data. B.K.M., and S.B. supervised and guided analytical work. All authors read and approved the final manuscript.
Funding
The present study was funded by the Kermanshah University of Medical Sciences through proposal grant number 990902. The funder had no role beyond the funding call in the design of the study, data collection, analysis, data interpretation, or writing the manuscript.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Ethics approval and consent to participate
This study was approved by the ethics committee of Kermanshah University of Medical Sciences (IR.KUMS.REC.1398.491) [65]. The systematic review was not registered.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Behzad Karami Matin, Email: bkm_1344@yahoo.com.
Sarah Byford, Email: sarah.byford@kcl.ac.uk.
Shahin Soltani, Email: shahin.soltani@kums.ac.ir.
Ali Kazemi-Karyani, Email: alikazemi.k20@gmail.com.
Zahra Atafar, Email: zahra_atafar@yahoo.com.
Ehsan Zereshki, Email: ehsanzereshki@gmail.com.
Moslem Soofi, Email: moslemsoofi@yahoo.com.
Satar Rezaei, Email: satarrezaei@gmail.com.
Shiva Tolouei Rakhshan, Email: toloui74482@gmail.com.
Parvin Jahangiri, Email: jhangiry713@gmail.com.
References
- 1.Association AP . Diagnostic and statistical manual of mental disorders (DSM-5®): American psychiatric pub. 2013. [DOI] [PubMed] [Google Scholar]
- 2.Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. The epidemiology of autism spectrum disorders. Annu Rev Public Health. 2007;28:235–258. doi: 10.1146/annurev.publhealth.28.021406.144007. [DOI] [PubMed] [Google Scholar]
- 3.The Centers for Disease Control and Prevention. [cited 2020 July 19]. Available from: https://www.cdc.gov/ncbddd/autism/facts.html.
- 4.Raina SK, Chander V, Bhardwaj AK, Kumar D, Sharma S, Kashyap V, et al. Prevalence of autism Spectrum disorder among rural, urban, and tribal children (1-10 years of age) J Neurosci Rural Pract. 2017;8(3):368–374. doi: 10.4103/jnrp.jnrp_329_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cummings JR, Lynch FL, Rust KC, Coleman KJ, Madden JM, Owen-Smith AA, et al. Health services utilization among children with and without autism Spectrum disorders. J Autism Dev Disord. 2016;46(3):910–920. doi: 10.1007/s10803-015-2634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiss JA, Isaacs B, Diepstra H, Wilton AS, Brown HK, McGarry C, et al. Health concerns and health service utilization in a population cohort of Young adults with autism Spectrum disorder. J Autism Dev Disord. 2018;48(1):36–44. doi: 10.1007/s10803-017-3292-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):e1203–e1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- 8.Chasson GS, Harris GE, Neely WJ. Cost comparison of early intensive behavioral intervention and special education for children with autism. J Child Fam Stud. 2007;16(3):401–413. doi: 10.1007/s10826-006-9094-1. [DOI] [Google Scholar]
- 9.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism Spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168(8):721–728. doi: 10.1001/jamapediatrics.2014.210. [DOI] [PubMed] [Google Scholar]
- 10.Peacock G, Amendah D, Ouyang L, Grosse SD. Autism spectrum disorders and health care expenditures: the effects of co-occurring conditions. J Dev Behav Pediatr. 2012;33(1):2–8. doi: 10.1097/DBP.0b013e31823969de. [DOI] [PubMed] [Google Scholar]
- 11.Zerbo O, Qian Y, Ray T, Sidney S, Rich S, Massolo M, et al. Health care service utilization and cost among adults with autism spectrum disorders in a US integrated health care system. Autism in Adulthood. 2019;1(1):27–36. doi: 10.1089/aut.2018.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA. Economic burden of childhood autism spectrum disorders. Pediatrics. 2014;133(3):e520–e529. doi: 10.1542/peds.2013-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knapp M, Romeo R, Beecham J. Economic cost of autism in the UK. Autism. 2009;13(3):317–36. 10.1177/1362361309104246. [DOI] [PubMed]
- 14.Horlin C, Falkmer M, Parsons R, Albrecht MA, Falkmer T. The cost of autism Spectrum disorders. PLoS One. 2014;9(9):e106552. doi: 10.1371/journal.pone.0106552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soltani S, Takian A, Akbari Sari A, Majdzadeh R, Kamali M. Financial barriers to access to health Services for Adult People with disability in Iran: the challenges for universal health coverage. Iran J Public Health. 2019;48(3):508–515. [PMC free article] [PubMed] [Google Scholar]
- 16.Smith KT, Monti D, Mir N, Peters E, Tipirneni R, Politi MC. Access Is Necessary but Not Sufficient: Factors Influencing Delay and Avoidance of Health Care Services. MDM Pol Pract. 2018;3(1):2381468318760298. doi: 10.1177/2381468318760298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taghaddosi M, Dianati M. Fath Gharib Bidgoli J, Bahonaran J. delay and its related factors in seeking treatment in patients with acute myocardial infarction. ARYA Atheroscler. 2010;6(1):35–41. [PMC free article] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed) 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boccuzzi SJ. Indirect health care costs. In: Weintraub WS, editor. Cardiovascular health care economics. Totowa: Humana Press; 2003. pp. 63–79. [Google Scholar]
- 20.Weintraub WS. Cardiovascular health care economics: Springer Science & Business Media. 2003. [Google Scholar]
- 21.Tai B-WB, Bae YH, Le QA. A systematic review of health economic evaluation studies using the Patient’s perspective. Value Health. 2016;19(6):903–908. doi: 10.1016/j.jval.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 22.JBI. Critical Appraisal Tools 2020 [cited 2022 March 22]. Available from: https://jbi.global/sites/default/files/2021-10/Checklist_for_Analytical_Cross_Sectional_Studies.docx.
- 23.Järbrink K, Knapp M. The economic impact of autism in Britain. Autism. 2001;5(1):7–22. doi: 10.1177/1362361301005001002. [DOI] [PubMed] [Google Scholar]
- 24.Jarbrink K, Fombonne E, Knapp M. Measuring the parental, service and cost impacts of children with autistic spectrum disorder: a pilot study. J Autism Dev Disord. 2003;33(4):395–402. doi: 10.1023/A:1025058711465. [DOI] [PubMed] [Google Scholar]
- 25.Liptak GS, Stuart T, Auinger P. Health care utilization and expenditures for children with autism: data from U.S. national samples. J Autism Dev Disord. 2006;36(7):871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- 26.Flanders SC, Engelhart L, Pandina GJ, McCracken JT. Direct health care costs for children with pervasive developmental disorders: 1996-2002. Adm Policy Ment Health Ment Health Serv Res. 2007;34(3):213–220. doi: 10.1007/s10488-006-0098-3. [DOI] [PubMed] [Google Scholar]
- 27.Järbrink K. The economic consequences of autistic spectrum disorder among children in a Swedish municipality. Autism. 2007;11(5):453–463. doi: 10.1177/1362361307079602. [DOI] [PubMed] [Google Scholar]
- 28.Leslie DL, Martin A. Health care expenditures associated with autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161(4):350–355. doi: 10.1001/archpedi.161.4.350. [DOI] [PubMed] [Google Scholar]
- 29.Sharpe DL, Baker DL. Financial issues associated with having a child with autism. J Fam Econ Iss. 2007;28(2):247–264. doi: 10.1007/s10834-007-9059-6. [DOI] [Google Scholar]
- 30.Shimabukuro TT, Grosse SD, Rice C. Medical expenditures for children with an autism spectrum disorder in a privately insured population. J Autism Dev Disord. 2008;38(3):546–552. doi: 10.1007/s10803-007-0424-y. [DOI] [PubMed] [Google Scholar]
- 31.Young A, Ruble L, McGrew J. Public vs. private insurance: cost, use, accessibility, and outcomes of services for children with autism spectrum disorders. Res Autism Spectr Disord. 2009;3(4):1023–1033. doi: 10.1016/j.rasd.2009.06.006. [DOI] [Google Scholar]
- 32.Wang L, Leslie DL. Health care expenditures for children with autism spectrum disorders in Medicaid. J Am Acad Child Adolesc Psychiatry. 2010;49(11):1165–1171. doi: 10.1016/j.jaac.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett B, Byford S, Sharac J, Hudry K, Leadbitter K, Temple K, et al. Service and wider societal costs of very young children with autism in the UK. J Autism Dev Disord. 2012;42(5):797–804. doi: 10.1007/s10803-011-1306-x. [DOI] [PubMed] [Google Scholar]
- 34.Parish SL, Thomas KC, Rose R, Kilany M, Shattuck PT. State Medicaid spending and financial burden of families raising children with autism. Intellectual Dev Disabil. 2012;50(6):441–451. doi: 10.1352/1934-9556-50.06.441. [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Zhou X, Xia W, Sun CH, Wu LJ, Wang JL, et al. Parent-reported health care expenditures associated with autism spectrum disorders in Heilongjiang province, China. BMC Health Serv Res. 2012;12:7. doi: 10.1186/1472-6963-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Farsi YM, Waly MI, Al-Sharbati MM, Al-Shafaee M, Al-Farsi O, Al-Fahdi S, et al. Variation in socio-economic burden for caring of children with autism Spectrum disorder in Oman: caregiver perspectives. J Autism Dev Disord. 2013;43(5):1214–1221. doi: 10.1007/s10803-012-1667-9. [DOI] [PubMed] [Google Scholar]
- 37.Van Steensel FJA, Dirksen CD, Bögels SM. A cost of illness study of children with high-functioning autism spectrum disorders and comorbid anxiety disorders as compared to clinically anxious and typically developing children. J Autism Dev Disord. 2013;43(12):2878–2890. doi: 10.1007/s10803-013-1835-6. [DOI] [PubMed] [Google Scholar]
- 38.Raz R, Lerner-Geva L, Leon O, Chodick G, Gabis LV. A survey of out-of-pocket expenditures for children with autism spectrum disorder in Israel. J Autism Dev Disord. 2013;43(10):2295–2302. doi: 10.1007/s10803-013-1782-2. [DOI] [PubMed] [Google Scholar]
- 39.Thomas KC, Parish SL, Williams CS. Healthcare expenditures for autism during times of school transition: some vulnerable families fall behind. Matern Child Health J. 2014;18(8):1936–1944. doi: 10.1007/s10995-014-1439-6. [DOI] [PubMed] [Google Scholar]
- 40.Barrett B, Mosweu I, Jones CRG, Charman T, Baird G, Simonoff E, et al. Comparing service use and costs among adolescents with autism spectrum disorders, special needs and typical development. Autism. 2015;19(5):562–569. doi: 10.1177/1362361314536626. [DOI] [PubMed] [Google Scholar]
- 41.Byford S, Cary M, Barrett B, Aldred CR, Charman T, Howlin P, et al. Cost-effectiveness analysis of a communication-focused therapy for pre-school children with autism: results from a randomised controlled trial. BMC Psychiatr. 2015;15:316. doi: 10.1186/s12888-015-0700-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parish SL, Thomas KC, Williams CS, Crossman MK. Autism and families' financial burden: the association with health insurance coverage. Am J Intellectual Dev Disabil. 2015;120(2):166–175. doi: 10.1352/1944-7558-120.2.166. [DOI] [PubMed] [Google Scholar]
- 43.Thomas KC, Williams CS, DeJong N, Morrissey JP. Examination of parent insurance ratings, child expenditures, and financial burden among children with autism: a mismatch suggests new hypotheses to test. Pediatrics. 2016;137:S186–SS95. doi: 10.1542/peds.2015-2851Q. [DOI] [PubMed] [Google Scholar]
- 44.Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Candon MK, Xie M, et al. Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Aff. 2017;36(10):1754–1761. doi: 10.1377/hlthaff.2017.0515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chang KC, Wang LY, Wang JH, Shaw CK, Hwang MJ, Wu CH, et al. Dental utilization and expenditures by children and adolescents with autism spectrum disorders: A population-based cohort study. Ci ji yi xue za zhi = Tzu-chi Med J. 2018;30(1):15–19. doi: 10.4103/tcmj.tcmj_185_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vohra R, Madhavan S, Sambamoorthi U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism. 2017;21(8):995–1009. doi: 10.1177/1362361316665222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Candon MK, Barry CL, Marcus SC, Epstein AJ, Kennedy-Hendricks A, Xie M, et al. Insurance mandates and out-of-pocket spending for children with autism spectrum disorder. Pediatrics. 2019;143:1. doi: 10.1542/peds.2018-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hong M, Lee SM, Park S, Yoon SJ, Kim YE, Oh IH. Prevalence and economic burden of autism Spectrum disorder in South Korea using National Health Insurance Data from 2008 to 2015. J Autism Dev Disord. 2020;50(1):333–339. doi: 10.1007/s10803-019-04255-y. [DOI] [PubMed] [Google Scholar]
- 49.Li HJ, Chen CY, Tsai CH, Kuo CC, Chen KH, Chen KH, et al. Utilization and medical costs of outpatient rehabilitation among children with autism spectrum conditions in Taiwan. BMC Health Serv Res. 2019;19(1):354. doi: 10.1186/s12913-019-4193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roddy A, O’Neill C. The economic costs and its predictors for childhood autism spectrum disorders in Ireland: how is the burden distributed? Autism. 2019;23(5):1106–1118. doi: 10.1177/1362361318801586. [DOI] [PubMed] [Google Scholar]
- 51.Zuvekas SH, Grosse SD, Lavelle TA, Maenner MJ, Dietz P, Ji X. Healthcare Costs of Pediatric Autism Spectrum Disorder in the United States, 2003-2015. J Autism Dev Disord. 2021;51(8):2950–8. 10.1007/s10803-020-04704-z. [DOI] [PMC free article] [PubMed]
- 52.Höfer J, Hoffmann F, Dörks M, Kamp-Becker I, Küpper C, Poustka L, et al. Health Services Use and Costs in Individuals with Autism Spectrum Disorder in Germany: Results from a Survey in ASD Outpatient Clinics. J Autism Dev Disord. 2022;52(2):540–52. [DOI] [PMC free article] [PubMed]
- 53.Ames JL, Massolo ML, Davignon MN, Qian Y, Croen LA. Healthcare service utilization and cost among transition-age youth with autism spectrum disorder and other special healthcare needs. Autism. 2021;25(3):705–18. [DOI] [PubMed]
- 54.Outlook: Obesity. 2012.
- 55.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- 56.Mosadeghrad AM, Pourreza A, Akbarpour N. Economic burden of autism spectrum disorders in Iran. Tehran University Med J. 2018;76(10):665–671. [Google Scholar]
- 57.Sechoaro EJ, Scrooby B, Koen DP. The effects of rehabilitation on intellectually-disabled people - a systematic review. Health SA Gesondheid (Online) 2014;19:1–9. [Google Scholar]
- 58.Mosadeghrad AM, Pourreza A, Akbarpour N. Economic burden of autism spectrum disorders in Iran. Tehran University Medical Journal. 2019;76(10):665–671. [Google Scholar]
- 59.Fang Y, Tao Q, Zhou X, Chen S, Huang J, Jiang Y, et al. Patient and Family Member Factors Influencing Outcomes of Poststroke Inpatient Rehabilitation. Archives of Physical Medicine and Rehabilitation. 2017;98(2):249–55.e2. [DOI] [PubMed]
- 60.Markussen S, Røed K. The impacts of vocational rehabilitation. Labour Econ. 2014;31:1–13. doi: 10.1016/j.labeco.2014.08.001. [DOI] [Google Scholar]
- 61.Reddy SR, Ross-Degnan D, Zaslavsky AM, Soumerai SB, Wharam JF. Impact of a high-deductible health plan on outpatient visits and associated diagnostic tests. Med Care. 2014;52(1):86–92. doi: 10.1097/MLR.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Clin Child Fam Psychol Rev. 2012;15(3):247–277. doi: 10.1007/s10567-012-0119-6. [DOI] [PubMed] [Google Scholar]
- 63.Helps S. Systemic psychotherapy with families where someone has an autism spectrum condition. NeuroRehabilitation. 2016;38(3):223–230. doi: 10.3233/NRE-161314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gabovitch EM, Curtin C. Family-centered Care for Children with Autism Spectrum Disorders: a review. Marriage Fam Rev. 2009;45(5):469–498. doi: 10.1080/01494920903050755. [DOI] [Google Scholar]
- 65.Research Ethics Committees Certificate. Investigation of health care expenditures for people with autism Spectrum disorders in the world: a systematic review 2019 [cited 2022 March 24]. Available from: https://ethics.research.ac.ir/ProposalCertificateEn.php?id=74099&Print=true&NoPrintHeader=true&NoPrintFooter=true&NoPrintPageBorder=true&LetterPrint=true.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.